Abstract
NREM parasomnias and nocturnal epileptic seizures (especially frontal lobe seizures) share clinical similarities which may lead to misdiagnosis and delayed treatment. Sleep-related hypermotor epilepsy (SHE), formerly termed nocturnal frontal lobe epilepsy (NFLE), is characterized by bizarre motor behavior and autonomic activation, appearing almost exclusively during sleep particularly N2 sleep stage. Night terrors typically begin after an arousal from N3 slow wave sleep, although occasionally may emerge from stage N2 sleep. Both are characterized by complex hypermotor, behavior, altered responsiveness and amnesia for the episode, with seizures exhibiting a more stereotypic motor pattern. NREM parasomnias as well as frontal lobe epilepsy (FLE) are more prevalent among children and young adults, but onset at any age can be seen especially with nocturnal frontal seizures. Stress, sleep deprivation, or irregular sleep-wake rhythm may provoke seizures as well as NREM parasomnias. A genetic predisposition plays an important role in disorders of arousals as well as in some nocturnal epilepsy types, such as SHE. There may be an occasional co-occurrence of focal seizures with new onset NREM related parasomnias (night terrors) making the diagnosis even more challenging. A Polysomnogram (PSG) with full electroencephalogram (EEG) montage is useful in differentiating between the two.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- NREM parasomnias
- Sleep terrors
- Confusional arousals
- Nocturnal seizures
- Hypermotor epilepsy
- Nocturnal panic attacks
- REM parasomnias
History
A 32-year-old man presented to the clinic after experiencing new onset of “night terrors”. The first episode occurred 1 year previously. His girlfriend observed the patient screaming during sleep, accompanied by hyperactive behaviors such as jumping and kicking. During the episode, the patient was observed to have his eyes open with an expression of fear and panic on his face. The event lasted approximately 5 min. The patient had no recollection of the event, but admits to feeling slightly confused afterwards, with a persistent sensation of fear and panic accompanied by fast heartbeat. He denied any dream associated with the event. A few weeks prior to the event the patient was started on lysdexamfetamine due to attention deficit hyperactive disorder (ADHD), which he stopped immediately after the episode. Patient denied sleep deprivation prior to the event or any precipitating factors except the fact that event occurred when sleeping out of his habitual place. The behaviors occurred during the first half of the night, within 1.5 h of falling asleep.
The patient experienced his second event, with similar clinical presentation, several months later while staying in a hotel. The event occurred 1.5 h after falling asleep, with no precipitating factors observed, except that both events occurred when sleeping in a new place.
The patient reported a childhood history of sleepwalking that resolved by age 11. He also admitted to snoring. He has a history of ADHD. The patient has no prior history of antidepressant exposure. There is no history of seizures or risk factors for epilepsy such as febrile seizures, head trauma with loss of consciousness, brain infections or family history of epilepsy. The patient denied smoking or illicit drug use and only reported occasional alcohol consumption. The relevant family history includes that his father and brother both have night terrors and obstructive sleep apnea (OSA), both using continuous positive airway pressure (CPAP) therapy with resulting decreased frequency of night terrors.
Examination
The patient was 6 ft. tall and weighed 180 lb., with a body mass index (BMI) 24.6 kg/m2 and neck circumference 15 inches. Nasal septum was midline, oropharyngeal examination showed Mallampati 2 with no evidence of tonsillar hypertrophy. He had normal neurological and musculoskeletal examination.
Investigations/Studies
Home sleep apnea test: apnea-hypopnea index (AHI) 1/h, with a respiratory disturbance index (RDI) of 10/h.
Magnetic resonance imaging (MRI) of the brain and routine electrocencephalogram (EEG) were normal.
Polysomnography (PSG) testing with prolonged video-EEG (vEEG):
Total seep time was 418 min, with 68.7% sleep efficiency. The patients sleep latency was 53.6 min. The REM latency was 54.5 min. The total AHI was 9.5/h. The periodic limb movements of sleep (PLMS) Index was 0/h. The mean oxygen saturation was 96.7%. There was normal muscle atonia during REM sleep stage.
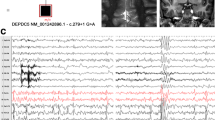
The prolonged video-EEG showed bi-synchronous frontal (R > L) potentially epileptogenic abnormalities (see Figs. 41.1 and 41.2) and also Frontal Intermittent Rhythmic Delta Activity (FIRDA).
Electroencephalogram, bipolar montage. EEG shows burst of mainly frontal epileptiform abnormalities (box). The international 10–20 system of electrode placement applied. Odd numbers, left; even numbers, right. Fp (frontopolar), F7 and F8 (anterior temporal), F3 and F4 (frontal), C3 and C4 (central), T3 and T4 (temporal), T5 and T6 (posterior temporal), P3 and P4 (parietal), O1 and O2 (occipital). ECGL-ECGR: Electrocardiogram. Sensitivity 7 μV/mm
Electroencephalogram, referential montage. EEG shows burst of mainly frontal epileptiform abnormalities (box). The international 10–20 system of electrode placement applied. Odd numbers, left; even numbers, right. Fp (frontopolar), F7 and F8 (anterior temporal), F3 and F4 (frontal), C3 and C4 (central), T3 and T4 (temporal), T5 and T6 (posterior temporal), P3 and P4 (parietal), O1 and O2 (occipital). ECGL-ECGR: Electrocardiogram. Sensitivity 7 μV/mm
Differential Diagnosis
The patient presented with new onset nocturnal episodes of paroxysmal motor behavior. The differential diagnosis of hyperactive nocturnal behavior includes NREM parasomnias (sleep terrors, confusional arousals and sleep walking), nocturnal seizures, rhythmic movement disorder, nocturnal panic attacks and REM behavior disorder (RBD).
NREM parasomnias such as sleep terrors, usually occur within the first half of the sleep period, as did patient’s events, and are characterized by abrupt terror, alarming frightening scream and are accompanied by intense fear and signs of autonomic arousals. Patients with sleep terrors are usually unresponsive to external stimuli, and if awakened are confused and disoriented, which goes along with patient’s clinical presentation. Sleep walking may occur in some cases. In contrast, patients with confusional arousals and sleep walking do not demonstrate autonomic changes such as tachycardia, tachypnea, mydriasis and diaphoresis during an episode [1].
Several types of epileptic syndromes predominantly manifest during sleep. Nocturnal frontal lobe epilepsy (NFLE), renamed sleep-related hypermotor epilepsy (SHE), considered in our patient (interictal potentially epileptogenic discharges: see Figs. 41.1 and 41.2), causes sleep disruption and may present as paroxysmal arousal with hyperactive movements, nocturnal paroxysmal dystonia or episodic nocturnal wandering. Seizures can look like simple arousal from sleep, at times confused as nightmare or night terror. More complex body movements like twisting, turning, pedaling, and vocalizations like screaming, moaning or crying may occur. Interictal EEG may show epileptiform activity in the frontal region, or may be normal. The seizure may last a few seconds to a few minutes, and are usually stereotyped. Frontal lobe seizures are most likely to occur during NREM sleep, especially stage N2 sleep; even during an episode epileptiform activity may not be apparent due to movement artifact.
Nocturnal panic attacks usually occur within the first half of the sleep period and can demonstrate autonomic changes. It usually occurs in individuals who have preexisting mood disorder, anxiety or panic attacks during wakefulness. Our patient has no prior history of mood disorders, but admits to ADHD. Even though ADHD and anxiety are separate conditions, about half of the adults with ADHD may also have anxiety disorder. However, patients can usually easily recognize the episode as a panic attack immediately after awakening.
Rhythmic movement disorder (RMD) is characterized by repetitive, stereotyped and rhythmic large muscle group body movements. Movements usually occur during drowsiness or sleep and are typically seen in infants and children, but may also occur in adults. In contrast to seizures this activity may be interrupted or stopped by environmental disturbance or being spoken to. Rhythmic movements have been reported in association with restless legs syndrome (RLS), narcolepsy, RBD, OSA and ADHD (last two being co-morbid conditions in our patient).
Idiopathic RBD usually affects older males. REM behaviors commonly occur during the later part of sleep. Episodes are often violent in nature, involving kicking and punching in addition to vocalization. The behavior emerges from REM sleep with PSG recording demonstrating REM sleep without atonia (RSWA). The individual usually reports a dream that corresponds to the observed sleep behavior. The eyes remain closed during the episode.
Discussion and Management
It is known that the clinical similarities between NREM parasomnias and nocturnal epileptic seizures (frontal and temporal lobe seizures) may lead to misdiagnosis. Both may occur only out of sleep with inappropriate or absent responsiveness and complete amnesia for the episode. The patients may appear confused and disoriented for several minutes afterwards.
NREM disorders of arousals are more prevalent among children and adults younger than 35 years, with the prevalence rate 2.3–2.6% in adults. Disorders of arousals that begin in adulthood are often more disruptive and require more clinical attention. With frontal lobe epilepsy (FLE), over 85% of people are diagnosed before 20 years old, usually around the age of 9. Our patient used to sleepwalk in childhood but a new type of events started at age 32, which is not very typical for NREM parasomnias like night terrors nor FLE [2].
Stress, sleep deprivation, irregular sleep-wake rhythm and other coexisting sleep pathologies (OSA in our case) as well as use of medications/drugs that modify sleep architecture may provoke NREM parasomnias as well as seizures. Travel and sleeping in unfamiliar surrounding have been associated with the onset of some disorders of arousals such as sleep walking.
PSG studies demonstrate that disorders of arousal typically begin after an arousal from slow wave sleep, occasionally may emerge from stage N2 sleep, while frontal lobe seizures are most likely to occur from stage N2 sleep.
In our case there seem to be a familial pattern with patient’s father and brother experiencing similar type of events. A genetic predisposition in disorders of arousals appear to play an important role. However, published research data is limited primarily to sleepwalking. There is known strong genetic predisposition reported in some nocturnal epilepsy types, such as SHE, with 70%–80% penetrance. It is usually a lifelong condition, with seizures controlled by medications. Most people are intellectually normal, but there may be associated mood disorders, behavioral problems or intellectual disability.
An admission for several days for EEG monitoring session may be useful should the events become more frequent. At times empiric treatment with anti-seizure medications may be considered, with events resolution favoring diagnosis of epilepsy.
Final Diagnosis
Possible frontal lobe epilepsy.
References
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
Bisulli F, Vignatelli L, Provini F, Leta C, Lugaresi E, Tinuper P. Parasomnias and nocturnal frontal lobe epilepsy (NFLE): lights and shadows--controversial points in the differential diagnosis. Sleep Med. 2011;12(Suppl 2):S27–32. https://doi.org/10.1016/j.sleep.2011.10.008.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Koziorynska, E.I. (2023). Case 41. Night Terrors Are Not Always What They Seem. In: Rodriguez, A.J. (eds) Sleepless and Sleepy . Springer, Cham. https://doi.org/10.1007/978-3-031-18374-4_41
Download citation
DOI: https://doi.org/10.1007/978-3-031-18374-4_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-18373-7
Online ISBN: 978-3-031-18374-4
eBook Packages: MedicineMedicine (R0)