Abstract
Diabetes is characterized by early and extensive involvement of the vascular system and affects both the micro- and macrocirculation. Changes in the micro- and macrocirculation, both anatomical and functional, contribute to the development of diabetic neuropathy. On the other hand, the development of diabetic neuropathy also affects the vasodilatory capacity of the microcirculation. Thus, the interaction between changes in the vasculature and peripheral nerves is bidirectional and results in changes in both blood flow and neuronal function. The possible links between diabetic micro- and macrovascular alterations and nerve damage will be the focus of this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Diabetes is often defined a “vascular disease” because of the early and extensive involvement of the vascular tree observed in diabetic patients and, even, in those at risk of developing diabetes. Both the micro- and macrocirculation are affected, though the pathophysiology, histology, clinical history, and clinical sequelae at the two vascular levels appear to be quite different.
Historically, there have been two competing hypotheses regarding the origins of diabetic neuropathy. According to the first one, diabetic neuropathy is secondary to the impairment of nerve and Schwann cells, while the second one stated that diabetic neuropathy is mostly ascribed to microvascular disease. However, it is currently realized that nerve and microvascular injury are both among the factors that contribute to nerve dysfunction.
Chronic diabetic complications are the result of small vessel disease. Diabetic microangiopathy has been considered the main anatomic alteration leading to the development of retinopathy, nephropathy, and neuropathy. Nevertheless, macroangiopathy, i.e., atherosclerosis of peripheral arteries, is also a prominent feature of long-lasting diabetes and is characterized as involving predominantly distal arteries. The possible links between diabetic micro- and macrovascular alterations and nerve damage will be the focus of this chapter.
2 Microvascular Disease: Overview and Anatomic Changes
Lesions specific for diabetes have been observed in the arterioles and capillaries of the foot and other organs that are the typical targets of diabetic chronic complications. A nowadays-historical retrospective histological study demonstrated the presence of PAS-positive material in the arterioles of amputated limb specimens from diabetic patients [1]. Though it was believed for several years that the anatomic changes described were occlusive in nature, in 1984 LoGerfo and Coffmann recognized that, in diabetic patients, there is no evidence of an occlusive microvascular disease [2]. Subsequent prospective anatomic staining and arterial casting studies have demonstrated the absence of an arteriolar occlusive lesion, thus dispelling the hopeless notion of diabetic “occlusive small vessel disease” [3, 4].
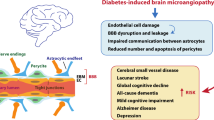
While there is no occlusive lesion in the diabetic microcirculation, other structural changes do exist. Arteriolar hyalinization, corresponding to the thickening of walls of arterioles, was observed in patients with diabetes, regardless of hypertension [5]. These abnormalities are characterized by hypertrophic remodeling and are associated with impaired endothelium-dependent vasodilation in vitro. Furthermore, endoneurial capillary density was also found to be increased in patients with diabetes, suggesting that capillary density may respond to diabetes-induced nerve ischemia [6]. The thickening of the capillary basement membrane, which is accompanied by pericyte degeneration and endothelial cell hyperplasia, is the dominant structural change in diabetic neuropathy. The composition of basement membrane in diabetes suggested that accumulation of glycosylated and cross-linked proteins contributed to the expanded membrane structure and impaired function. This can affect endothelial cell and extracellular matrix interactions and represents a response to the metabolic changes related to diabetes and hyperglycemia [7,8,9]. Furthermore, the thickness of basement membrane of skin and nerve correlates with the extent of neuropathy in diabetes [10]. However, this alteration does not lead to occlusion of the capillary lumen, and arteriolar blood flow may be normal or even increased despite these changes [11]. On the contrary, it might act as a barrier to the exchange of nutrients and/or increase the rigidity of the vessels further limiting their ability to dilate in response to different stimuli [12].
In the kidney, nonenzymatic glycosylation reduces the charge on the basement membrane, which may account for transudation of albumin, an expanded mesangium, and albuminuria [13]. Similar increases in vascular permeability occur in the eye and probably contribute to macular exudate formation and retinopathy [14]. In simplest terms, microvascular structural alterations in diabetes result in an increased vascular permeability and impaired autoregulation of blood flow and vascular tone.
Previous studies have shown a correlation between the development of diabetic chronic complication and metabolic control with perhaps the strongest evidence coming from the Diabetes Control and Complications Trial (DCCT), which enrolled type 1 diabetic patients, and the United Kingdom Prospective Diabetes Study (UKPDS), which enrolled type 2 diabetic patients [15, 16]. The results from both clinical trials clearly showed a delay in the development and progression of retinopathy, nephropathy, and neuropathy with intensive glycemic control, thus supporting the direct causal relationship between hyperglycemia and microcirculation impairment. In contrast, there was less evident for macrovascular disease, which was assessed only in the UKPDS.
It should be emphasized hyperglycemia alone is not sufficient to trigger generalized diabetic microvascular pathologies. The Joslin Diabetes Center 50-year Medalist Study has shown that 30–35% patients with type 1 diabetes did not have significant microvascular complications [17]. This suggests that there may be unidentified genetic or other endogenous protective factors that diminish the adverse microvascular effects of hyperglycemia. It has been shown that multiple mechanisms are involved in the adverse effects of hyperglycemia with vascular complications, including nonenzymatic glycation and the formation of advanced glycation end products (AGEs); enhanced reactive oxygen production and actions; endoplasmic reticulum (ER) stress; and the activation of the polyol pathway, the diacylglycerol (DAG)–protein kinase C (PKC) pathway [5], Src homology-2 domain-containing phosphatase-1 (SHP-1), and the reninangiotensin system (RAS) and kallikrein-bradykinin (BK) systems (Fig. 1).
Although the structural alterations observed in diabetic capillaries do not affect the basal blood flow, some functional abnormalities of the microvascular circulation, which may eventually result in a relative ischemia, have been extensively documented. This aspect will be deeply discussed in the next section.
3 Pathophysiology of Microvascular Disease and Endothelial Dysfunction in Diabetes
3.1 Functional Changes
Diabetes mellitus, even in the absence of complications, impairs the vascular reactivity, that is the endothelium dependent and independent vasodilation, in the skin microcirculation [18]. Many glucose-related metabolic pathways can determine endothelium dysfunction: increased aldose reductase activity leading to the imbalance in nicotinamide adenine dinucleotide phosphate (NADP)/nicotinamide adenine dinucleotide phosphate, reduced form (NADPH); auto-oxidation of glucose leading to the formation of reactive oxygen species (ROS); “advanced glycation end-products” (AGEs) produced by nonenzymatic glycation of proteins; abnormal n6-fatty acid metabolism and inappropriate activation of protein kinase C. All these different pathways lead to an increase of oxidative stress which is responsible for a reduced availability of nitric oxide and, in turn, for a functional tissue hypoxia and the development of diabetic chronic complications [19] (Fig. 2).
3.2 Microvascular Dysfunction and Diabetic Neuropathy
Microvascular reactivity is further reduced at the foot level in the presence of peripheral diabetic neuropathy. Endothelial nitric oxide synthase (eNOS) is a key regulator of vascular nitric oxide production. Immunostaining of foot skin biopsies in our unit, with antiserum to human eNOS, glucose transporter I (GLUT I), which is a functional marker of the endothelium and von Willebrand factor, an anatomical marker, showed no difference among diabetic patients with or without peripheral neuropathy in the staining of GLUT I and von Willebrand factor, while the staining for the eNOS was reduced in neuropathic patients (Fig. 3) [20]. Another study documented increased levels of iNOS and reduced eNOS levels in skin from the foot of diabetic patients with severe neuropathy and foot ulceration [21].
Differences in the microcirculation between the foot and forearm levels have also been investigated, the main hypothesis being that increased hydrostatic pressure in distal microcirculatory beds, related to the orthostatic posture, affects the foot microcirculation more than at the forearm level. The endothelium-dependent and -independent vasodilation is, in fact, lower at the foot level when compared to the forearm in healthy subjects and both non-neuropathic and neuropathic diabetic patients [22]. This forearm–foot gradient exists despite a similar baseline blood flow at the foot and forearm level. Therefore, it is reasonable to believe that erect posture may be a contributing factor for the early development of the nerve damage at the foot, compared to the forearm.
Endoneurial microangiopathy was related to the severity of neuropathy, suggesting that there might be a causal relationship between impaired microvasculature and diabetic neuropathy [6, 23]. In a large observational study, it was found that endothelial function was a strong independent predictor of DPN [24]. Experimental data also showed that endothelium impairment could cause neuropathy through involvement of the Desert Hedgehog pathway [25].
3.2.1 Endothelium Dysfunction
Previous studies have suggested that endothelium-dependent vasodilation is impaired in diabetes, regardless of the presence of long-term complications [26,27,28]. It has also been shown that endothelium dysfunction precedes the development of macro- and microvascular diabetic complications, indicating that endothelial impairment could be a critical factor toward the development of diabetic vascular complications [29]. However, these changes mainly involve the ability of microcirculation under stress, such as foot injury while they do not affect the baseline blood flow [20]. This feature, combined with the arteriovenous shunt that is present at the foot level due to autonomic neuropathy, can account for observations in clinical practice, in which, diabetic neuropathy with or without ulceration presents with a warm limb with distended veins and palpable pulses. The final result is that despite no reduction in the total lower extremity blood flow, there is functional ischemia that promoted injury and impairs wound healing.
3.3 Autonomic Denervation
Autonomic nerve fibers take part in the modulation of blood circulation. At rest, noradrenergic sympathetic nerves are tonically active in normothermic environments and increase their activity during cold exposure, releasing both norepinephrine and co-transmitters to decrease skin blood flow [30]. Autonomic neuropathy can compromise the diabetic microcirculation because of the development of arterio-venous shunting due to sympathetic denervation. The opening of these shunts leads to a maldistribution of blood between the nutritional capillaries and subpapillary vessels, and consequent aggravation of microvascular ischemia. Studies employing sural nerve photography and fluorescein angiography as well as other elegant techniques seem to support this concept [31, 32]. In addition to the above, these changes also result in impaired thermoregulation [33].
A loss of sympathetic tone is also responsible for an increased capillary permeability in diabetic patients with neuropathy [34, 35]. This might cause endoneurial edema, as demonstrated by employing magnetic resonance spectroscopy, which can in turn represent another mechanism leading to a reduction of endoneurial perfusion and a worsening of the nerve damage [35]. The increased lower extremity capillary pressure upon assuming the erect posture, due to early loss of postural vasoconstriction (mediated by the sympathetic fibers), might amplify this edematous effect.
3.4 Nerve Axon Reflex
Diabetic somatic neuropathy can further affect the skin microcirculation by the impairment of the axon reflex-related vasodilatation (Lewis’ flare). Under normal conditions, the stimulus of the c-nociceptive nerve fibers not only travels in the normal direction, centrally toward the spinal cord, but also peripherally (“antidromic conduction”) to local cutaneous blood vessels, causing a vasodilatation by the release of vasoactive substances, such as calcitonin gene-related peptide (CGRP), Neuropeptide Y, substance P, and bradykinin by the c fibers initiate neurogenic inflammation (Fig. 4). This short circuit, or nerve axon reflex, is responsible for the Lewis’ triple flare response to injury and plays an important role in increasing local blood flow when it is mostly needed, i.e., in condition of stress.
The nerve axon reflex-related vasodilation or neurovascular response: stimulation of the c-nociceptive nerve fibers by acetylcholine or other noxious stimuli leads to antidromic stimulation of the adjacent c-fibers, which secrete Calcitonin Gene-Related Peptide (CGRP) that causes vasodilation and increased local blood flow
This neurovascular (N-V) response is significantly reduced at the foot level in diabetic patients with peripheral somatic neuropathy, autonomic neuropathy, and peripheral artery disease compared to diabetic patients without complications and healthy control subjects (Fig. 5) [22, 36]. Moreover, local anesthesia significantly reduces the nerve axon reflex-related vasodilation at the foot of patients without peripheral neuropathy, while it has no effect on the amount of the pre-anesthesia N-V vasodilation—which is already very low—at the foot of neuropathic patients [37]. This suggests that the main determinant of the presence of the neurovascular vasodilation is c-fiber function and that its measurement could be used as a surrogate measure of the function of these fibers.
The neurovascular response (expressed as percentage of blood flow increase over the baseline blood flow) is significantly reduced at the foot level of diabetic patients with peripheral somatic neuropathy (DN), autonomic neuropathy (DA), and peripheral artery disease (DV) compared to diabetic patients without complications (DC) and healthy controls (C) *p < 0.001
Neurovascular response is associated with measures of peripheral nerve function [37, 38]. Studies in our units have shown that an N-V response lower than 50% is highly sensitive (90%) and adequately specific (74%), in identifying diabetic patients with peripheral neuropathy [38]. Besides, the finding that this response is significantly reduced even in the early stages of peripheral neuropathy supports the hypothesis that small fiber damage is a precocious event in the clinical history of diabetic neuropathy—even preceding large fibers’ impairment (Fig. 6). This leads to impaired vasodilation under conditions of stress, such as injury or inflammation. Therefore, it is possible to speculate that small fiber neuropathy might further contribute to nerve hypoxic damage by the impairment of this hyperemic response, determining a vicious cycle of injury.
The nerve axon reflex-related vasodilation at the foot level in a diabetic population stratified on the basis of the degree of peripheral somatic neuropathy in patients without neuropathy (D), with mild neuropathy (DN mild), with moderate neuropathy (DN moderate), and with severe neuropathy (DN severe) compared to healthy controls (C). Median (25–75 percentile). The nerve axon reflex-related vasodilation is already significantly reduced in the early stages of neuropathy (subclinical neuropathy), supporting the belief that small fiber dysfunction might precede large fiber impairment in the natural history of diabetic nerve damage
The previous conclusions are supported by recent studies in experimental diabetes which have demonstrated that epineurial arterioles of the sciatic nerve are innervated by sensory nerves that contain CGRP and mediate a hyperemic response at this level [39]. Furthermore, it has been shown that in long-term diabetic rats the amount of CGRP present in epineurial arterioles is diminished, which could be due to a denervation process [40]. Exogenous CGRP-mediated vasodilation of these arterioles is also impaired in experimental diabetes, indicating a reduced CGRP bioactivity [40]. All these findings further support a role of small sensory nerve fibers’ impairment in the development and progression of diabetic neuropathy.
The impairment of the nerve axon reflex-related vasodilation is not affected by successful bypass surgery in patients with peripheral arterial disease. In addition, the endothelium-dependent and -independent vasodilation, which is not related to the nerve axon reflex, remains impaired after successful revascularization. Therefore, despite correction in obstructive lesions and restoration of normal blood flow in the large vessels, the changes in microcirculation continue to be present and cause tissue hypoxia under conditions of stress [41].
In summary, both the functional and structural changes observed in diabetic microcirculation contribute to the shift of blood flow away from the nutritive capillaries to low-resistance arteriovenous shunts, leading to functional ischemia of tissues including peripheral nerves and, consequently, to the development of diabetic peripheral neuropathy and other diabetic chronic complications.
4 Lower Extremity Arterial Disease and Diabetes
Smoking, diabetes mellitus, and dyslipidemia are the most associated risk factors of lower extremity artery disease [42]. Diabetes mellitus is estimated to be associated with two- to fourfold increase in the prevalence of peripheral arterial disease (PAD) [43]. The concomitant occurrence of atherosclerotic peripheral vascular disease and peripheral neuropathy in patients with diabetes is the main factor in the development of diabetic foot pathology. Furthermore, peripheral arterial disease (PAD) of the lower extremities is considered the major risk factor for lower-extremity amputation, and it is also accompanied by a high likelihood for cardiovascular and cerebrovascular diseases [44]. In a large, multinational meta-analysis, the presence of diabetes was associated with nearly a twofold increased odds for PAD [45]. The risk of amputation in patients with diabetes is 0.2–2.0/1000, which is 10–15 times greater in diabetes than in the nondiabetic population [46].
Although the underlying pathogenesis of atherosclerotic disease in diabetics is similar to that noted in nondiabetics, there are still some significant differences. Diabetic patients present with atherosclerotic disease at a significantly younger age than their nondiabetic counterparts, tend to present with more advanced disease and have a worse prognosis. The prevalence of concomitant of PAD and diabetes is high in patients with critical lower limb ischemia, with more than 50% patients with critical limb ischemia having diabetes [47]. In addition, diabetes is also associated with more severe below-the-knee PAD. The anterior tibial, posterior tibial, and peroneal arteries are most commonly affected and tend to have more diffuse lesions [48,49,50]. Equally important is the observation that the arteries of the foot, specifically the dorsalis pedis, are often spared of occlusive disease. This provides an excellent option for a distal revascularization target [51].
The clinical presentation and prognosis of PAD with diabetes is also implicated by the coexistence of peripheral neuropathy. Microvascular disease (i.e., retinopathy, nephropathy, neuropathy) independently associated with limb amputation after controlling for traditional atherogenic risk factors. Concomitant presence of microvascular disease and PAD synergistically amplifies the risk of amputation. Thus, it is imperative to take into consideration the importance of microvascular disease in consideration of limb salvage strategies [52]. In addition, diabetic patients are less likely to present with typical claudication symptoms than patients without diabetes. As a consequence, the development of tissue loss (foot ulceration or gangrene) may represent the first sign of lower limb ischemia and because of its limb-threatening potential, it is termed as critical limb ischemia. Therefore, diabetic patients with a foot ulcer should always be evaluated for ischemia, irrespective of their symptoms, particularly for the increased risk of limb-threatening infection and faulty healing related to PVD [53].
The observations that distal vessels (i.e., distal peroneal, dorsal pedal, and plantar arteries) are often spared from arterial occlusive disease had a crucial impact on the manner in which peripheral vascular disease is approached in the diabetic population. In the past, based upon the false presumption of small vessel disease, diabetics were not treated as aggressively with revascularization as is now standard. A more aggressive attempt to correct the vascular deficit in diabetic ischemic limbs in addition to more aggressive measures to control local infection has radically altered the prognosis of peripheral vascular disease in the diabetic extremity.
5 Conclusions
Changes in the micro- and macrocirculation, both anatomical and functional, contribute to the development of diabetic neuropathy. On the other hand, the development of diabetic neuropathy also affects the vasodilatory capacity of the microcirculation and can interfere with the clinical presentation of peripheral obstructive arterial disease. Thus, the interaction between changes in the vasculature and peripheral nerves is bidirectional and results in changes in both blood flow and neuronal function.
References
Goldenberg S, Alex M, Joshi RA, Blumenthal HT. Nonatheromatous peripheral vascular disease of the lower extremity in diabetes mellitus. Diabetes. 1959;8:261–73.
LoGerfo FW, Coffman JD. Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. N Engl J Med. 1984;311:1615–9.
Conrad MC. Large and small artery occlusion in diabetics and nondiabetics with severe vascular disease. Circulation. 1967;36:83–91.
Strandness DE Jr, Priest RE, Gibbons GE. Combined clinical and pathologic study of diabetic and nondiabetic peripheral arterial disease. Diabetes. 1964;13:366–72.
Rizzoni D, Porteri E, Guelfi D, Muiesan ML, Valentini U, Cimino A, Girelli A, Rodella L, Bianchi R, Sleiman I, Rosei EA. Structural alterations in subcutaneous small arteries of normotensive and hypertensive patients with non-insulin-dependent diabetes mellitus. Circulation. 2001;103:1238–44.
Thrainsdottir S, Malik RA, Dahlin LB, Wiksell P, Eriksson KF, Rosen I, Petersson J, Greene DA, Sundkvist G. Endoneurial capillary abnormalities presage deterioration of glucose tolerance and accompany peripheral neuropathy in man. Diabetes. 2003;52:2615–22.
LeBleu VS, Macdonald B, Kalluri R. Structure and function of basement membranes. Exp Biol Med. 2007;232:1121–9.
Haitoglou CS, Tsilibary EC, Brownlee M, Charonis AS. Altered cellular interactions between endothelial cells and nonenzymatically glucosylated laminin/type IV collagen. J Biol Chem. 1992;267:12404–7.
Williamson JR, Tilton RG, Chang K, Kilo C. Basement membrane abnormalities in diabetes mellitus: relationship to clinical microangiopathy. Diabetes Metab Rev. 1988;4:339–70.
Malik RA, Newrick PG, Sharma AK, Jennings A, Ah-See AK, Mayhew TM, Jakubowski J, Boulton AJ, Ward JD. Microangiopathy in human diabetic neuropathy: relationship between capillary abnormalities and the severity of neuropathy. Diabetologia. 1989;32:92–102.
Parving HH, Viberti GC, Keen H, Christiansen JS, Lassen NA. Hemodynamic factors in the genesis of diabetic microangiopathy. Metabolism. 1983;32:943–9.
Flynn MD, Tooke JE. Aetiology of diabetic foot ulceration: a role for the microcirculation? Diabet Med. 1992;9:320–9.
Mogensen CE, Schmitz A, Christensen CK. Comparative renal pathophysiology relevant to IDDM and NIDDM patients. Diabetes Metab Rev. 1988;4:453–83.
Cunha-Vaz JG. Studies on the pathophysiology of diabetic retinopathy. The blood-retinal barrier in diabetes. Diabetes. 1983;32(Suppl 2):20–7.
Diabetes C, Complications Trial Research G, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Group UPDSU. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Keenan HA, Costacou T, Sun JK, Doria A, Cavellerano J, Coney J, Orchard TJ, Aiello LP, King GL. Clinical factors associated with resistance to microvascular complications in diabetic patients of extreme disease duration: the 50-year medalist study. Diabetes Care. 2007;30:1995–7.
Morris SJ, Shore AC, Tooke JE. Responses of the skin microcirculation to acetylcholine and sodium nitroprusside in patients with NIDDM. Diabetologia. 1995;38:1337–44.
Cameron NE, Eaton SE, Cotter MA, Tesfaye S. Vascular factors and metabolic interactions in the pathogenesis of diabetic neuropathy. Diabetologia. 2001;44:1973–88.
Veves A, Akbari CM, Primavera J, Donaghue VM, Zacharoulis D, Chrzan JS, DeGirolami U, LoGerfo FW, Freeman R. Endothelial dysfunction and the expression of endothelial nitric oxide synthetase in diabetic neuropathy, vascular disease, and foot ulceration. Diabetes. 1998;47:457–63.
Jude EB, Boulton AJ, Ferguson MW, Appleton I. The role of nitric oxide synthase isoforms and arginase in the pathogenesis of diabetic foot ulcers: possible modulatory effects by transforming growth factor beta 1. Diabetologia. 1999;42:748–57.
Arora S, Smakowski P, Frykberg RG, Simeone LR, Freeman R, LoGerfo FW, Veves A. Differences in foot and forearm skin microcirculation in diabetic patients with and without neuropathy. Diabetes Care. 1998;21:1339–44.
Malik RA, Tesfaye S, Thompson SD, Veves A, Sharma AK, Boulton AJ, Ward JD. Endoneurial localisation of microvascular damage in human diabetic neuropathy. Diabetologia. 1993;36:454–9.
Roustit M, Loader J, Deusenbery C, Baltzis D, Veves A. Endothelial dysfunction as a link between cardiovascular risk factors and peripheral neuropathy in diabetes. J Clin Endocrinol Metab. 2016;101:3401–8.
Chapouly C, Yao Q, Vandierdonck S, Larrieu-Lahargue F, Mariani JN, Gadeau AP, Renault MA. Impaired Hedgehog signalling-induced endothelial dysfunction is sufficient to induce neuropathy: implication in diabetes. Cardiovasc Res. 2016;109:217–27.
Williams SB, Cusco JA, Roddy MA, Johnstone MT, Creager MA. Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol. 1996;27:567–74.
Palmer RM, Ashton DS, Moncada S. Vascular endothelial cells synthesize nitric oxide from L-arginine. Nature. 1988;333:664–6.
Johnstone MT, Creager SJ, Scales KM, Cusco JA, Lee BK, Creager MA. Impaired endothelium-dependent vasodilation in patients with insulin-dependent diabetes mellitus. Circulation. 1993;88:2510–6.
Elhadd TA, Kennedy G, Hill A, McLaren M, Newton RW, Greene SA, Belch JJ. Abnormal markers of endothelial cell activation and oxidative stress in children, adolescents and young adults with type 1 diabetes with no clinical vascular disease. Diabetes Metab Res Rev. 1999;15:405–11.
Charkoudian N. Mechanisms and modifiers of reflex induced cutaneous vasodilation and vasoconstriction in humans. J Appl Physiol. 2010;109:1221–8.
Tesfaye S, Harris N, Jakubowski JJ, Mody C, Wilson RM, Rennie IG, Ward JD. Impaired blood flow and arterio-venous shunting in human diabetic neuropathy: a novel technique of nerve photography and fluorescein angiography. Diabetologia. 1993;36:1266–74.
Flynn MD, Tooke JE. Diabetic neuropathy and the microcirculation. Diabet Med. 1995;12:298–301.
Rutkove SB, Veves A, Mitsa T, Nie R, Fogerson PM, Garmirian LP, Nardin RA. Impaired distal thermoregulation in diabetes and diabetic polyneuropathy. Diabetes Care. 2009;32:671–6.
Lefrandt JD, Bosma E, Oomen PH, Hoeven JH, Roon AM, Smit AJ, Hoogenberg K. Sympathetic mediated vasomotion and skin capillary permeability in diabetic patients with peripheral neuropathy. Diabetologia. 2003;46:40–7.
Eaton RP, Qualls C, Bicknell J, Sibbitt WL Jr, King MK, Griffey RH. Structure-function relationships within peripheral nerves in diabetic neuropathy: the hydration hypothesis. Diabetologia. 1996;39:439–46.
Hamdy O, Abou-Elenin K, LoGerfo FW, Horton ES, Veves A. Contribution of nerve-axon reflex-related vasodilation to the total skin vasodilation in diabetic patients with and without neuropathy. Diabetes Care. 2001;24:344–9.
Caselli A, Rich J, Hanane T, Uccioli L, Veves A. Role of C-nociceptive fibers in the nerve axon reflex-related vasodilation in diabetes. Neurology. 2003;60:297–300.
Caselli A, Spallone V, Marfia GA, Battista C, Pachatz C, Veves A, Uccioli L. Validation of the nerve axon reflex for the assessment of small nerve fibre dysfunction. J Neurol Neurosurg Psychiatry. 2006;77:927–32.
Calcutt NA, Chen P, Hua XY. Effects of diabetes on tissue content and evoked release of calcitonin gene-related peptide-like immunoreactivity from rat sensory nerves. Neurosci Lett. 1998;254:129–32.
Yorek MA, Coppey LJ, Gellett JS, Davidson EP. Sensory nerve innervation of epineurial arterioles of the sciatic nerve containing calcitonin gene-related peptide: effect of streptozotocin-induced diabetes. Exp Diabetes Res. 2004;5:187–93.
Arora S, Pomposelli F, LoGerfo FW, Veves A. Cutaneous microcirculation in the neuropathic diabetic foot improves significantly but not completely after successful lower extremity revascularization. J Vasc Surg. 2002;35:501–5.
Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116:1509–26.
Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–81.
Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med. 1992;117:97–105.
Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, Norman PE, Sampson UK, Williams LJ, Mensah GA, Criqui MH. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–40.
Vadiveloo T, Jeffcoate W, Donnan PT, Colhoun HC, McGurnaghan S, Wild S, McCrimmon R, Leese GP. Scottish Diabetes Research Network Epidemiology G. Amputation-free survival in 17,353 people at high risk for foot ulceration in diabetes: a national observational study. Diabetologia. 2018;61:2590–7.
Dick F, Diehm N, Galimanis A, Husmann M, Schmidli J, Baumgartner I. Surgical or endovascular revascularization in patients with critical limb ischemia: influence of diabetes mellitus on clinical outcome. J Vasc Surg. 2007;45:751–61.
Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24:1433–7.
American Diabetes A. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26:3333–41.
Armstrong EJ, Waltenberger J, Rogers JH. Percutaneous coronary intervention in patients with diabetes: current concepts and future directions. J Diabetes Sci Technol. 2014;8:581–9.
Van Damme H. Crural or pedal artery revascularisation for limb salvage: is it justified? Acta Chir Belg. 2004;104:148–57.
Behroozian A, Beckman JA. Microvascular disease increases amputation in patients with peripheral artery disease. Arterioscler Thromb Vasc Biol. 2020;40:534–40.
Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, Sackett DL, Strandness DE Jr, Taylor LM. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a critical review. Circulation. 1996;94:3026–49.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chen, L., Veves, A. (2023). Micro- and Macrovascular Disease in Diabetic Neuropathy. In: Tesfaye, S., Gibbons, C.H., Malik, R.A., Veves, A. (eds) Diabetic Neuropathy. Contemporary Diabetes. Humana, Cham. https://doi.org/10.1007/978-3-031-15613-7_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-15613-7_19
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-031-15612-0
Online ISBN: 978-3-031-15613-7
eBook Packages: MedicineMedicine (R0)