Abstract
COVID-19 is primarily associated with acute infection, however, its presentation and degree of severity varies in individuals. Individuals at the greatest risk of long-COVID include those who experience severe symptoms of their initial infection and those who are aged >65 years, female, obese or smoke tobacco. Long-COVID presents anything up to 1-year post-initial infection and with a range of symptoms such as fatigue, muscle pain, and loss of smell. The exact cause of long-COVID is not fully conclusive but it is associated with viral tissue damage, immune, and inflammatory responses. It affects both children and adults, resulting in increased dependence on already stretched healthcare systems, negative patient outcomes and impacting on activities of daily living. Currently, there is no curative treatment for long-COVID rather symptomatic management but preventive measures via vaccination is deemed as beneficial.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- COVID-19
- Long-COVID
- COVID long-haulers
- Post-acute sequelae of COVID-19 (PASC)
- Post-COVID-19 condition
- Post-COVID-19 syndrome
- Chronic COVID-19 syndrome (CCS)
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak first occurred in late 2019 in China. The associated condition, coronavirus disease 2019 (COVID-19), causes a range of symptoms including fever, cough, loss of taste and smell, fatigue, headache, and breathing difficulties [1,2,3]. Although symptoms are mild in most affected individuals, COVID-19 is associated with severe illness in some patients, and has a case-fatality rate of around 1% [4]. In the absence of a specific cure for the condition, the initial management of patients consisted of symptomatic management, and the use of supportive technology available in the clinic such as ventilators [5, 6]. Although only a small proportion of infected individuals are severely affected, the widespread and rapid transmission of COVID-19 resulted in immense acute pressure on healthcare systems throughout the world. Various infection control measures, such as the mandatory wearing of face coverings, school closures, and lockdowns were implemented, in part to reduce this acute pressure on health systems.
Whilst the initial phases of the response to COVID-19 naturally focused on refining the acute management of the disease (lasting no more than 3 weeks in most individuals [7]), it quickly became apparent that, in common with many other viral diseases, recovery from COVID-19 was extremely delayed in some individuals [7], a phenomenon described as ‘post-acute sequelae of COVID-19 (PASC)’, ‘post-COVID-19 condition’, ‘post-COVID-19 syndrome’, ‘chronic COVID syndrome (CCS)’ or simply ‘long-COVID’ [8,9,10,11,12]. This syndrome affects multiple organs and systems, and symptoms include tiredness, weakness, shortness of breath, muscle aches and pains, prolonged loss of taste and smell, and difficulty concentrating (Fig. 22.1). Owing to the very high prevalence of COVID infections worldwide, long-COVID is likely to have substantial impacts on morbidity, and healthcare resource use for the foreseeable future. This chapter will summarize the current state of knowledge with respect to long-COVID, with a particular focus on the definition, epidemiology, and clinical implications of the condition.
Commonly reported symptoms of long-COVID. (Image created using Biorender.com)
Biological and Historical Context
Long-COVID must be understood in the context of the wider body of knowledge about recovery from viral illness, and, of post-viral syndromes [13]. The similar condition Severe Acute Respiratory Distress Syndrome (SARS), also caused by a coronavirus is associated with long terms symptoms characteristic of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) (fatigue, myalgia, and depression) [13]. Importantly, these symptoms are persistent and severe—preventing individuals from returning to work for up to 20 months post-infection. The mechanism behind these adverse effects is imperfectly understood, however, for SARS it was demonstrated that the virus could enter the brain via the olfactory route, resulting in activation of inflammatory pathways. Long-COVID has also been likened to post-Ebola syndrome which also manifests with joint and muscle pain, and fatigue [14].
Definitions of Long-COVID
Owing to the syndromic nature of long-COVID, its complex pathophysiology, variety of symptoms (in terms of nature, onset, and duration), and the absence of a biological test, long-COVID essentially becomes a diagnosis of exclusion in patients who have had a confirmed or suspected COVID-19 infection, and for which other causes for the clinical presentation cannot be found [15]. Formal definitions of long-COVID have been proposed by the National Institute for Health and Care Excellence (NICE) [11] in the United Kingdom (UK) and by the World Health Organization (WHO) [8] (Table 22.1). Importantly the definitions make clear that symptoms may be ongoing and unresolved from the initial infection or may recur (or appear for the first time) at some point after apparent recovery from the acute infection.
Symptoms and Pathophysiological Mechanisms in Long-COVID
Whilst the pathophysiology of a diverse and complex syndrome is likely to be difficult to fully elucidate, it is nevertheless helpful to undertake efforts to understand the condition with a view to developing diagnostic tests and treatments for long-COVID. It has been suggested that the symptoms of long-COVID may result from direct damage to tissues as a result of the infection, thrombolysis, excessive unregulated inflammation or virus-induced activation of autoreactive T and B cells [16]. Recent investigations into viral persistence in COVID-19 and immune responses to infection have been extremely instructive in shedding light on mechanistic aspects of long-COVID.
Recent autopsy studies have clearly demonstrated widespread and persistent systemic infection with SARS-CoV-2. A study of 44 COVID-19 patients demonstrated that SARS-CoV-2 RNA could be detected in a range of anatomical sites (including the brain) for as long as 230 days. Interestingly, the study found little evidence of inflammatory responses to infection outside of the lung, and thus further investigation is necessary to better understand the causal links between prolonged infection with SARS-CoV-2, and the clinical symptoms of long-COVID [17].
Further light on the immune response to COVID-19 was shed by a larger prospective multicentre cohort study of 215 patients which compared immunoglobulin signatures in COVID-19 patients and healthy controls [16]. The investigators found that the development of long-COVID was associated with a distinct immunoglobulin signature (based on IgM and IgG3); and when this was combined with clinical and demographic information, it contributed to an effective risk stratification scoring system. This has important implications for identifying patients most likely to suffer from long-COVID but is also informative with respect to pathophysiological mechanisms—particularly with respect to specific inflammatory mediators which might prove to be therapeutic targets.
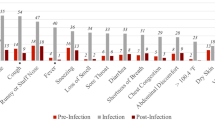
The wide range of symptoms reported and associated with long-COVID clearly demonstrates the systemic nature of the condition, and the range of organs affected. Studies of COVID-19 in large populations have reported a wide range of reported symptoms including tiredness, weakness, shortness of breath, muscle aches and pains, loss of taste and smell, and difficulty concentrating (Fig. 22.2).
Prevalence of long-COVID symptoms in the United Kingdom: Estimated percentage of people living in private households with self-reported long-COVID by symptom. Data current at February 2022, plotted using data released from the UK Office of National Statistics [18]
Clearly, different patients experience different symptoms, and the pathological mechanisms accounting for the symptoms are likely to represent a variety of responses to persistent SARS-CoV-2 infection in different organs and tissues.
It has been suggested that chronic fatigue following COVID-19 may result from inflammation and congestion in the glymphatic system, resulting in reduced drainage of cerebrospinal fluid within the central nervous system [19]. Dyspnoea is likely to result from damage to the lung tissues (particularly endothelial cells) during the acute infection, particularly in individuals with existing respiratory disorders. Loss of taste and smell may result from viral entry (via non-neuronal ACE2) into cells of the olfactory system, causing inflammation and impairing olfactory nerve function.
Cardiovascular abnormalities following COVID are clearly an important cause for concern in the management of patients [19], and biomarker manifestations of cardiac damage can be detected many weeks after infection [20]. However, as this topic is the subject of specifically focused chapters within this volume, the mechanisms will not be discussed further here.
Epidemiology of Long-COVID
As time has progressed, and more of the world’s population has been exposed to COVID-19 it is to be expected that the prevalence of long-COVID will increase proportionally. Indeed, this has been seen in health surveillance data. Interestingly, in the United Kingdom, data from the Office of National Statistics suggests that the incidence of reported long-COVID syndromes is increasingly steadily, both for individuals who have had a relatively recent COVID-19 infection (within 12 weeks), but also for those with much more temporally distant infections—up to 12 months previously (Fig. 22.3).
Time course of the prevalence of long-COVID symptoms in the United Kingdom. Black Squares: Estimated percentage of people living in private households with self-reported long-COVID of any duration (4-week period prior to reporting date). Red Circles: Estimated percentage of people living in private households with self-reported long-COVID who first had (or suspected they had) COVID-19 at least 12 weeks previously (4-week period prior to reporting date). Blue Triangles: Estimated percentage of people living in private households with self-reported long-COVID who first had (or suspected they had) COVID-19 at least 12 months previously (4-week period prior to reporting date). Data current at February 2022, plotted using data released from the UK Office of National Statistics [18]
Clearly these data must be interpreted with caution, as symptoms are largely self-reported, and causality cannot be ascribed, nevertheless, the data do support the expected rise in the long-term complications of infection over time.
The REACT-2 study in the UK provided the opportunity for a large and detailed study of long-COVID symptoms. The investigators recruited over half a million participants and asked about their previous history of COVID infection and questioned in detail about 29 symptoms associated with long-COVID by previous researchers. The results highlighted the high prevalence of ongoing morbidity following acute COVID infection—nearly 15% of participants experienced at least one symptom which lasted 12 weeks or more. Multivariate analysis was conducted to identify independent predictors of long-COVID following acute infection. Long-COVID appeared to be associated with a more severe initial infection, female sex, increasing age, obesity, and smoking [21].
A smaller study of 4182 users of the ‘COVID Symptom Study’ app compared the attributes of patients with COVID symptoms which resolves in less than 10 days, with those whose symptoms lasted at least 28 days, 8 weeks, and 12 weeks. The findings were in accordance with the REACT-2 trial. Long-COVID symptoms included fatigue, headache, dyspnoea, and anosmia and were associated with severe acute illness (>five symptoms in the acute phase), and demographics outlined above female, older age and obesity. The authors were able to validate their findings by developing a predictive model and testing it in an independent sample, which was modestly predictive (area under the receiver operator characteristic curve was 76%) [22].
Importantly, it appears that vaccination reduces the reported incidence of long-COVID. A large cross-sectional study of 951 patients with PCR-confirmed COVID infections (67% of whom were vaccinated, predominantly with the BNT162b2 mRNA vaccine [23]) and 2437 controls allowed for the study of association between vaccination status and the development of long-COVID. Following adjustment for time and measured confounding demographic variables, there was a substantial and statistically significant reduction in a range of long-COVID symptoms: fatigue (RR = 0.36), headache (RR = 0.46), weakness (RR = 0.43), and persistent muscle pain (RR = 0.32). The effect was strongest in double-vaccinated individuals. The authors concluded that vaccination may prevent against the development of long-COVID. Clearly these results (which are currently only available as a pre-print) cannot tell us about the effects of other vaccines in different populations, but they clearly add another important piece of evidence supporting the overwhelming benefit/risk ratio for vaccination [24].
Clinical Implications of Long-COVID
The implications of long-COVID must be considered both on an individual and a population level. The most commonly reported symptoms (described above) are likely to have implications for individuals’ ability to work in the short term, and (based on the high reported prevalence) may have significant implications for healthcare resources. However, in otherwise healthy individuals, common long-COVID symptoms are unlikely to be life threatening. Nevertheless, particular consideration should be given to outcomes of long-COVID in particular at-risk groups.
The impact of COVID (and long-COVID) on individuals at high risk of cardiovascular disease is covered at length elsewhere in this volume, so will not be discussed in detail here. However, it is important to note that multiple factors related to COVID (ranging from direct cardiac damage in acute infections, thromboembolism, and delayed routine care) are likely to result in poor outcomes for those patients at high risk of cardiovascular events [25, 26]. Indeed, a large cohort study (153,750 individuals with COVID-19 and 5,637,647 non-infected controls), has demonstrated a substantial increase in the incidence of a range of cardiovascular events in the 12 months following acute infection with COVID-19 [26]. These findings are biologically plausible if widespread SARS-CoV-2 infection results in systemic inflammation, in light of recent advances in knowledge of the contribution of inflammation to the aetiology of atherosclerotic cardiovascular disease [2, 27,28,29,30,31,32,33].
As the likelihood of long-COVID has been shown to increase with age [21, 22], the implications of the condition requires careful consideration in older adults. Indeed, the complications of long-COVID appear to be more severe in those aged over 65 years, than for other lower respiratory tract infections, with an increased risk of respiratory failure, dementia, and post-viral fatigue [34]. Therefore, older adults may require close monitoring and care following COVID to spot the early signs of clinical deterioration.
At the other extreme of life, the impact of long-COVID in children also requires specialist consideration. In many children, COVID is asymptomatic or mild, and symptoms are short-lived. In one large study, less than 2% of children reported symptoms after 56 days [35, 36]. However, rarely, children experience severe and life-threatening late effects of COVID, such as paediatric inflammatory multi-system syndrome temporally associated with SARS-CoV-2 (PIMS-TS) which can even occur after a mild or asymptomatic index infection [37]. Urgent attention is required in order to better predict those at risk of this devastating condition, and to manage recovery. Recent findings from the LATE-COVID-Kids study have identified younger age, higher levels of antithrombin III, and higher heart rate as being associated with increased risk of developing PIMS-TS [38]. These findings require validation in a range of populations to reach further conclusions and consensus.
Beyond the level of individual patients, long-COVID clearly has implications on the delivery of healthcare, from the specific management of patients with the condition, and that fact that healthcare professionals throughout the world are struggling to ‘catch up’ with routine healthcare screening and interventions which ceased or were dramatically scaled back during the pandemic [1]. Data on the prevalence of long-COVID suggests that health and social workers are more likely to be affected than individuals in any other professional group [18] (almost certainly reflecting the very high rates of COVID infection acquired by these individuals as a result of their patient-facing contact). Severe long-COVID (as with other post-viral conditions) clearly impacts upon an individual’s ability to return to work, therefore it is to be expected that a larger than usual level of illness absence of healthcare professionals will persist for the foreseeable future.
Inevitably in the context of a rapidly-developing body of knowledge, guidelines, and treatment recommendations will be continuously developed and refined. However, current guidelines mainly focus on the reactive management of specific symptoms, and supporting the patient to return to their activities of daily life [11, 12].
Conclusions and Future Directions
The ubiquitous worldwide spread of COVID-19 has resulted in an inevitable growing problem of the post-viral syndrome, known as long-COVID. The syndrome manifests in a variety of ways, but common symptoms include tiredness, weakness, shortness of breath, muscle aches and pains, loss of taste and smell, and difficulty concentrating. These symptoms result in significant morbidity, and there is, as yet, not cure for the condition. Whilst careful studies have shed some light onto the potential mechanisms of the disease (which may involve persistent systemic infection and the activation of specific inflammatory pathways), a much greater understanding of the pathophysiology of long-COVID, and of post-viral syndromes in general is necessary to allow fully validated risk prediction scores to be developed. This will enable identification of patients most at risk and inform optimal management of such patients. In the meantime, it must be remembered that ‘prevention is better than cure’, and promising data suggest that individuals who are vaccinated are less likely than unvaccinated individuals to experience long-term sequalae of COVID if they later develop an infection.
References
Banach M, Penson PE, Fras Z, Vrablik M, Pella D, Reiner Z, et al. Brief recommendations on the management of adult patients with familial hypercholesterolemia during the COVID-19 pandemic. Pharmacol Res. 2020;158:104891. https://doi.org/10.1016/j.phrs.2020.104891.
Ganjali S, Bianconi V, Penson PE, Pirro M, Banach M, Watts GF, et al. Commentary: statins, COVID-19, and coronary artery disease: killing two birds with one stone. Metabolism. 2020;113:154375. https://doi.org/10.1016/j.metabol.2020.154375.
Struyf T, Deeks JJ, Dinnes J, Takwoingi Y, Davenport C, Leeflang MM, et al. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19. Cochrane Database Syst Rev. 2021;2:CD013665. https://doi.org/10.1002/14651858.CD013665.pub2.
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/s1473-3099(20)30244-9.
Molhave M, Agergaard J, Wejse C. Clinical management of COVID-19 patients—an update. Semin Nucl Med. 2022;52(1):4–10. https://doi.org/10.1053/j.semnuclmed.2021.06.004.
Tobaiqy M, Qashqary M, Al-Dahery S, Mujallad A, Hershan AA, Kamal MA, et al. Therapeutic management of patients with COVID-19: a systematic review. Infect Prev Pract. 2020;2(3):100061. https://doi.org/10.1016/j.infpip.2020.100061.
Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. https://doi.org/10.1136/bmj.m3026.
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2021;22(4):e102–7. https://doi.org/10.1016/s1473-3099(21)00703-9.
Baig AM. Chronic COVID syndrome: need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol. 2021;93(5):2555–6. https://doi.org/10.1002/jmv.26624.
Centers for disease control and prevention: post-COVID conditions. 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Flong-term-effects.html. Accessed.
National Institute for Health and Care Excellence. NG188: COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2021.
National Institute for Health and Care Excellence, Scottish Intercollegiate Guidelines Network, Royal College of General Practitioners. COVID-19 rapid guideline: managing the longterm effects of COVID-19. 2022.
Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: post-viral syndrome post COVID-19. Med Hypotheses. 2020;144:110055. https://doi.org/10.1016/j.mehy.2020.110055.
Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021;27(1):28–33. https://doi.org/10.1038/s41591-020-01202-8.
Fernandez-de-Las-Penas C, Palacios-Cena D, Gomez-Mayordomo V, Cuadrado ML, Florencio LL. Defining post-COVID symptoms (post-acute COVID, long COVID, persistent post-COVID): an integrative classification. Int J Environ Res Public Health. 2021;18(5):2621. https://doi.org/10.3390/ijerph18052621.
Cervia C, Zurbuchen Y, Taeschler P, Ballouz T, Menges D, Hasler S, et al. Immunoglobulin signature predicts risk of post-acute COVID-19 syndrome. Nat Commun. 2022;13(1):446. https://doi.org/10.1038/s41467-021-27797-1.
Chertow D, Stein S, Ramelli S, Grazioli A, Chung J-Y, Singh M, et al. SARS-CoV-2 infection and persistence throughout the human body and brain. 2021. https://doi.org/10.21203/rs.3.rs-1139035/v1.
Office for National Statistics: prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/alldatarelatingtoprevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk. Accessed.
Crook H, Raza S, Nowell J, Young M, Edison P. Long Covid-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. https://doi.org/10.1136/bmj.n1648.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–73. https://doi.org/10.1001/jamacardio.2020.3557.
Whitaker M, Elliott J, Chadeau-Hyam M, Riley S, Darzi A, Cooke G, et al. Persistent symptoms following SARS-CoV-2 infection in a random community sample of 508,707 people. 2021. https://doi.org/10.1101/2021.06.28.21259452.
Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms 1 collected by the Covid symptoms study app. 2020. https://doi.org/10.1101/2020.10.19.20214494.
Muhsen K, Cohen D. COVID-19 vaccination in Israel. Clin Microbiol Infect. 2021;27(11):1570–4. https://doi.org/10.1016/j.cmi.2021.07.041.
Kuodi P, Gorelik Y, Zayyad H, Wertheim O, Wiegler KB, Jabal KA, et al. Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients tested between March 2020 and November 2021. 2022. https://doi.org/10.1101/2022.01.05.22268800.
Satterfield BA, Bhatt DL, Gersh BJ. Cardiac involvement in the long-term implications of COVID-19. Nat Rev Cardiol. 2021;19(5):332–41. https://doi.org/10.1038/s41569-021-00631-3.
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–90. https://doi.org/10.1038/s41591-022-01689-3.
Banach M, Penson PE. Colchicine and cardiovascular outcomes: a critical appraisal of recent studies. Curr Atheroscler Rep. 2021;23(7):32. https://doi.org/10.1007/s11883-021-00932-5.
Brie D, Sahebkar A, Penson PE, Dinca M, Ursoniu S, Serban MC, et al. Effects of pentoxifylline on inflammatory markers and blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Hypertens. 2016;34(12):2318–29. https://doi.org/10.1097/HJH.0000000000001086.
Bytyci I, Bajraktari G, Penson PE, Henein MY, Banach M, Lipid, et al. Efficacy and safety of colchicine in patients with coronary artery disease: a systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol. 2021;88(4):1520–8. https://doi.org/10.1111/bcp.15041.
Dyrbus K, Gasior M, Desperak P, Trzeciak P, Nowak J, Penson PE, et al. Risk-factors associated with extremely high cardiovascular risk of mid- and long-term mortality following myocardial infarction: analysis of the hyperlipidaemia therapy in tERtiary cardiological cEnTer (TERCET) registry. Atherosclerosis. 2021;333:16–23. https://doi.org/10.1016/j.atherosclerosis.2021.08.024.
Penson PE, Long DL, Howard G, Toth PP, Muntner P, Howard VJ, et al. Associations between very low concentrations of low density lipoprotein cholesterol, high sensitivity c-reactive protein, and health outcomes in the reasons for geographical and racial differences in stroke (REGARDS) study. Eur Heart J. 2018;39(40):3641–53. https://doi.org/10.1093/eurheartj/ehy533.
Ruscica M, Penson PE, Ferri N, Sirtori CR, Pirro M, Mancini GBJ, et al. Impact of nutraceuticals on markers of systemic inflammation: potential relevance to cardiovascular diseases–a position paper from the international lipid expert panel (ILEP). Prog Cardiovasc Dis. 2021;67:40–52. https://doi.org/10.1016/j.pcad.2021.06.010.
Shahbaz SK, Sadeghi M, Koushki K, Penson PE, Sahebkar A. Regulatory T cells: possible mediators for the anti-inflammatory action of statins. Pharmacol Res. 2019;149:104469. https://doi.org/10.1016/j.phrs.2019.104469.
Cohen K, Ren S, Heath K, Dasmarinas MC, Jubilo KG, Guo Y, et al. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2022;376:e068414. https://doi.org/10.1136/bmj-2021-068414.
Gurdasani D, Akrami A, Bradley VC, Costello A, Greenhalgh T, Flaxman S, et al. Long COVID in children. Lancet Child Adolescent Health. 2022;6(1):e2. https://doi.org/10.1016/S2352-4642(21)00342-4.
Molteni E, Sudre CH, Canas LS, Bhopal SS, Hughes RC, Antonelli M, et al. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolescent Health. 2021;5(10):708–18. https://doi.org/10.1016/s2352-4642(21)00198-x.
Ward JL, Harwood R, Smith C, Kenny S, Clark M, Davis PJ, et al. Risk factors for PICU admission and death among children and young people hospitalized with COVID-19 and PIMS-TS in England during the first pandemic year. Nat Med. 2022;28(1):193–200. https://doi.org/10.1038/s41591-021-01627-9.
Jatczak-Pawlik I, Lewek J, Czkwianianc E, Blomberg A, Krysiak N, Zeman K, et al. Biochemical and cardiovascular predictors of PIMS-TS risk in children after COVID-19 recovery: preliminary results of the LATE-COVID-kids study. Arch Med Sci. 2022;18(2):545–52. https://doi.org/10.5114/aoms/146827.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
P.E.P. owns four shares in AstraZeneca PLC and has received honoraria and/or travel reimbursement for events sponsored by AKCEA, Amgen, AMRYT, Link Medical, Mylan, Napp, Sanofi.
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
McCloskey, A.P., Penson, P.E. (2022). Long-COVID-19: Definition, Epidemiology, and Clinical Implications. In: Banach, M. (eds) Cardiovascular Complications of COVID-19. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-031-15478-2_22
Download citation
DOI: https://doi.org/10.1007/978-3-031-15478-2_22
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-031-15477-5
Online ISBN: 978-3-031-15478-2
eBook Packages: MedicineMedicine (R0)