Abstract
Sunscreens are topical preparations designed to protect the skin from the negative effects of sun exposure. Their proven clinical benefits include the protection against sunburn erythema; attenuation of photoaging; the decreased incidence of some forms of skin cancers and precursors, namely cutaneous squamous cell carcinoma, actinic keratoses, and possibly invasive melanoma; and the treatment and prevention of various photo-induced and photo-aggravated dermatoses.
Sunscreens’ protecting effects depend on their ultraviolet radiation (UVR) filtering spectrum—comprising UVB filters measured by the sun protection factor (SPF) and UVA filters—and further on their properties of water resistance, photostability and cosmetic acceptability that condition compliance and correct use.
Current recommendations endorse the regular use of broad spectrum, UVB and UVA filtering sunscreens, with SPF > 15 (>30 by some guidelines), applied in amount of 2 mg/cm2, on UV-exposed skin, 20 min before and repeated at least every 2 h during sun exposure, in addition to other photoprotection measures like wearing protective clothing, seeking shade, and avoiding peak-hour sun exposure and artificial tanning devices (sunbeds).
Sunscreens alone do not appear to impact on the vitamin D levels of healthy individuals, but consistent photoprotection through sunscreens use combined with physical and behavioral measures of reducing UVR exposure warrants vitamin D status screening and oral supplementation in case of defficiency.
Topical sunscreens are generally well tolerated and safe when properly and reasonably used. Recent concerns on their long-term effects include the possible systemic transepidermal absorption at high doses and its impact on endocrine and developmental systems, the potential photo-oxidative tissue damage induced by photo-unstable, epidermis-penetrating UVR filters, and their potential effect on marine ecosystems following globally increased use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Topical sunscreens contain as active ingredients molecules able to reflect, scatter, or absorb the ultraviolet radiation (UVR) incident on the skin.
-
The proven clinical benefits of sunscreens include: the protection against sunburn erythema; the attenuation of photoaging; the decreased incidence of some forms of skin cancers and precursors including cutaneous squamous cell carcinoma, actinic keratoses, and possibly invasive melanoma; the treatment and prevention of various photo-induced and photo-aggravated dermatoses.
-
Current recommendations endorse the regular use of broad spectrum, UVB and UVA filtering sunscreens, with SPF > 15 (>30 by some guidelines), applied in amount of 2 mg/cm2, on UV-exposed skin, 20 min before and repeated at least every 2 h during sun exposure, in addition to other photoprotection measures like wearing protective clothing, seeking shade, and avoiding peak-hour sun exposure and artificial tanning devices.
General Principles
Ultraviolet radiation (UVR) of both natural solar and artificial origin has a wide range of effects on the human skin, depending on the radiation’s wavelength and the host’s sensitivity. While sunlight is necessary for health, excessive sun exposure, which is individually determined, has negative consequences. The immediate clinical effects of UVR include sunburn (ranging from mild erythema to painful blistering), pigmentation, cutaneous immunity modulation (suppression of acquired immunity, enhancement of innate immunity), and vitamin D synthesis in the skin. The chronic, cumulative UVR effects include the photoaging (with its clinical complex of skin dispigmentation, telangiectasia, fine and coarse wrinkles and elasticity loss) and, importantly, the development of skin cancers. UV exposure is considered the principal environmental factor of cutaneous oncogenesis, with about 90% of keratinocyte cancers and 65% of melanoma burden currently attributed to UV exposure(Robyn et al. 2006). In predisposed individuals, sunlight is also responsible for a vast array of photo-induced and photo-aggravated dermatoses.
These effects result from the molecular mechanisms of UVR action within the skin cells, which comprise: structural DNA damage, with formation of cyclobutane pyrimidine dimers (CPDs) and C-T, CC-TT mutations (mainly UVB effect); the generation of reactive oxygen species (ROS) toxic for DNA and other cell structures (mainly UVA effect); gene expression modulation; melanogenesis stimulation; induction of apoptosis; and depletion of skin immune cells. Vitamin D production is initiated by the UVB-induced conversion of epidermal 7-dehydrocholesterol into pre-vitamin D (Young et al. 2017; Suozzi et al. 2020).
These complex mechanisms are triggered by the interaction between the UVR and the UV-absorbing chromophore molecules within the skin, either endogenous like DNA, porphyrins, or melanins, or exogenous—derived from systemic or cutaneous exposure to various drugs or chemicals. The absorption of UVR induces energetic and structural changes in the chromophore molecules, resulting in the production of ROS and other potentially toxic metabolites, function alterations, or binding to other molecules and triggering chain effects.
Topical sunscreens are formulations applied on the skin in order to protect it from the various negative UVR effects. Their fundamental mechanism of action is to block the UVR from reaching its target molecules within the skin, either by reflecting or scattering the incident UVR away from the skin or by absorbing the UVR energy and converting it in the less harmful form of heat (Young et al. 2017; Mancuso et al. 2017).
In order to be effective protectors, the topical sunscreens must meet certain requirements. Principally, they must protect both against UVB (280–320 nm) and UVA (320–400 nm) radiation, taking into consideration that the solar UVR reaching the Earth surface is represented by 5% UVB and 95% UVA. While UVB is the main inducer of erythema, the other acute and chronic UV pathogenic effects, including photocarcinogenesis, may result from cumulative exposure to sub-erythemogenic doses of both UVB and UVA (Young et al. 2017). Further, topical sunscreens must be photostable, should be nontoxic to the skin and display negligible percutaneous systemic adsorption. They should be cosmetically acceptable for the general public, safe for humans and the environment, and must comply with the patent and marketing regulations relevant for their area of use.
As the skin protection from UVR exposure is now the cornerstone of prevention of skin cancers and photoaging, the topical sunscreens have become an important part of the preventive efforts, along with other physical protection methods like photoprotective clothing and sunglasses and behavioral measures of avoiding excessive sun exposure and artificial tanning.
Sunscreen Structure and Classification
Topical sunscreens exist in various forms of creams, gels, lotions, or sprays that incorporate molecules acting as UV filters by absorbing or/and scattering the UV radiation. UV filters fall into two broad categories: the organic filters, also called chemical filters, that penetrate within the epidermis and act at this level mainly by absorbing and redistributing the UVR energy; and the inorganic filters, also called physical or mineral filters, that remain largely at the surface of the epidermis and act mainly by reflecting or scattering the incident UVR away from the skin surface, in addition to also absorbing UVR. Sunscreen formulations can contain one or both filter types.
Organic Filters
Organic filters are aromatic compounds that contain series of conjugated π-electron systems on their aromatic rings, giving them the ability to absorb UVR energy and subsequently dissipate it in the form of heat (Young et al. 2017; Mancuso et al. 2017). Several classes of organic filters exist (Table 156.1), with absorption properties in UVB, UVA spectrum, or both.
Organic filters penetrate within the epidermis and act at this level. Hence they are not visible on the skin surface after application, so they are cosmetically acceptable and the widest prescribed and used class of commercially available sunscreens (Maier and Korting 2005). At the same time, their interaction with the UVR within the living epidermis can generate neoantigens that may induce photoallergic reactions (Collaris and Frank 2008); thus organic filters cause more frequently photoallergic contact dermatitis than inorganic ones. Further, organic filters may degrade under UV irradiation, generating ROS that are toxic to the surrounding cells’ structures including DNA. The highly effective but highly photolabile UVA1 filter avobenzone is such an example. The paradoxical increased DNA damage through oxidative mechanisms induced by organic UV filters-derived ROS, despite the filters’ protective effect against UVB-signature CPD formation, has been proven in in vitro and in vivo studies (Bastien et al. 2010; Hanson et al. 2006). The photodegradation can be aggravated or, on the contrary, attenuated by particular filter combinations, and therefore modern commercial formulations focus on combining filters with reciprocal stabilizing effects and complementing UVB/UVA spectrum (Mancuso et al. 2017).
Inorganic Filters
Inorganic filters are metal oxides, like titanium dioxide (TiO2) or zinc oxide (ZnO). They are efficient filters for both the UVB and UVA radiation and are active also in the visible light (VL) spectrum. Their reflective properties and the fact that they remain at the epidermis surface make them less likely to induce photoallergic reactions or skin-toxic products by photodegradation, so they have been “generally recognized as safe and effective” (GRASE) by the U.S. Food and Drug Administration (FDA), unlike organic ones (FDA FaDA 2019). The main limitation of inorganic filters’ use has been the cosmetically unfavorable whitish hue they leave on the skin surface, which lowers them in consumers’ preference rankings (Varedi et al. 2019). The mitigation of this effect has been attempted by supplementing the filters with universal skin tone tints that counter the white color and bring a more skin-natural hue to the product applied on the skin. Another strategy to reduce their visibility on the skin consists in the micronization, and more recently in the nanosizing of the filter particles incorporated in the sunscreen formulation (Jansen et al. 2013). Nanosizing has potential downsides, as it may increase the filter’s penetrance within the living epidermis and hence the risk of photoallergic/phototoxic reactions (Sha et al. 2015; Crosera et al. 2015); it may also reduce the filter’s spectrum, changing the ratio between its UVR reflecting/scattering and UVR absorption properties. Micronization of TiO2 has been shown to increase its UVB absorption, but decrease the absorption in UVA range and lower its scattering and reflection of visible light (VL) spectrum, making it a less effective filter for UVA and VL (Jansen et al. 2013). These particle-size-dependent effects have not been shown though for ZnO (Cole et al. 2016).
Sunscreen Measurements and Regulation
Sunscreen formulations are classified and approved for consumers’ use primarily according to their UVR filtering performance and spectrum. Further parameters that influence their effects, marketing approval, and labeling include their resistance to water, their photostability and their cosmetic effect. These parameters are subject to different methods of measurement, labeling and regulation in different countries.
The UV Filtering Spectrum and Efficiency
The sun protection factor (SPF) was the first parameter introduced in the 1950s, as sunscreens were initially developed to protect against the sunburn erythema (Schulze 1956). SPF is calculated as the ratio between the doses of UVR needed to cause skin erythema with and without sunscreen applied. As erythema is induced mainly by UVB, SPF is primarily an indicator of the filtering efficiency in the UVB spectrum. Different methodologies of measuring SPF exist worldwide; the most widely used ones currently are the ISO 24444 standard methodology, published in 2010 by the International Standards Organization (Technical Committee ISO/TC 217 2010) and adopted in Europe, Australia, Canada, and Japan (Young et al. 2017), and the FDA standard methodology valid in the USA and many other countries (Young et al. 2017; FDA 2011). These methodologies are based on the same principle of SPF measurement in vivo, by irradiating the living skin of healthy volunteers with a standardized range of UVB doses, before and after applying a standardized dose of 2 mg/cm2 of sunscreen, and measuring the degree of ensuing erythema. There is no standardized in vitro method of measuring SPF to date and the in vivo testing has a certain degree of result variability, depending on the testing site, methodology, and volunteer subjects’ characteristics. In the European Union (EU) area and in the USA the regulatory bodies allow a superior limit of 50+ for the SPF labeling of sunscreens, justified by the attempt to avoid misleading the consumer, as the protective effect against sun damage does not increase linearly with the SPF, nor should, e.g., an SPF100 product be mistakenly considered to provide 100% blockage of UVR. This labeling cap has recently been proposed to be raised to SPF60+ in the USA (FDA FaDA 2019), acknowledging the increased benefit of using higher-SPF sunscreens, especially in the context of real-life application of suboptimal sunscreen amounts (Williams et al. 2018; Ou-Yang et al. 2012) and in the long term to protect against cumulative sun exposure.
The testing for measuring the degree of UVA protection of sunscreen products was developed later, as the photocarcinogenic and photoaging effects of UVA were being discovered and the necessity of broad-spectrum UVR protection was recognized. Modern sunscreens are required to have broad spectrum, UVB and UVA filtering properties (Cosmetics Europe 2005). The standardized UVA testing procedure mostly used at present is set out by the ISO 24443 methodology, issued in 2012 (International Organization for Standardization 2012). It consists of an in vitro procedure to determine the UVR spectral absorption curve, based on which further parameters can be calculated including the UVA protection factor (UVA PF), critical wavelength, and UVA absorbance proportionality (International Organization for Standardization 2012). These parameters are used by different market regulation authorities to evaluate the sunscreens claiming broad UVB/UVA protection spectrum. The FDA requires a critical wavelength of 370 nm (FDA 2011) and within the EU it is required the same critical wavelength and a UVA PF of at least 1/3 of the product’s SPF for the sunscreen to be labeled as providing broad-spectrum UV protection (Cosmetics Europe 2005). Earlier in vivo testing methods, based on the pigmenting effect of UVA on the living human skin (persistent pigment darkening, PPD), are still mandatory for market approval only in Japan and Korea (Young et al. 2017). The ISO 24443 UVA testing methodology requires prior in vivo measurement of SPF as the basis for the scaling of the UV absorbance curve.
The topical sunscreens’ role for protection against solar visible light (VL) and infrared radiation (IR) was not addressed until recently. Visible light and IR have been shown to contribute to the cutaneous oxidative photodamage, as they induce up to 50% of the free radicals produced in the skin by sunlight exposure (Zastrow and Lademann 2016). Visible light induces persistent pigmentation, especially in darker skin phototypes (Mahmoud et al. 2010), may contribute to melasma and post-inflammatory hyperpigmentation induction (Regazzetti et al. 2018; Schalka 2017) and plays a triggering role for various photodermatoses (Nahhas et al. 2018). Currently, VL protection can be provided by the inorganic UV filters like zinc and titanium oxides, depending on their particle size (Moseley et al. 2001), and by iron oxides, which are not regulated as UV filters, but are highly effective in reflecting/scattering VL. They are available in less cosmetically acceptable tinted sunscreen formulations (Schalka 2017). There is currently no standardized method to measure the VL/IR protection and this parameter is not routinely measured or required on current sunscreens.
Water Resistance
In the EU and the USA the methods of testing the sunscreens’ water resistance are based on measuring the product’s SPF before and after immersion in water for a specified period. In the European Union, the labeling as “water resistant” and “very water resistant” is awarded to products that maintain at least 50% of their pre-immersion SPF value after 2 and respectively 4 periods of 20 minutes water immersion (Cosmetics Europe 2005). In the USA, the FDA has stricter requirements for the same labeling, as sunscreens need to maintain the same value of SPF before and after water immersion in the same conditions (FDA 2011). Water resistance has been increased in newer sunscreens by adding polymer molecules like acrylates.
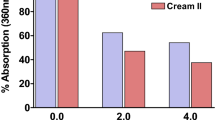
Photostability
The photostability of a sunscreen can be determined in vivo or in vitro, based on measuring the UVR filter amount contained in the tested sunscreen formulation before and after UV irradiation through high-performance liquid chromatography or spectrophotometry. The photostability is a critical characteristic of a topical sunscreen, however its testing is not mandatory for market licensing in the EU, Australia, or the USA. Nonetheless, a guideline for photostability testing of sunscreens has been issued by Cosmetics Europe (Guidelines on stability testing of cosmetic products Cosmetics Europe 2004) and in the USA the FDA requires the photostability evaluation as prerequisite for the critical wavelength testing for the UVA protection (FDA 2011). The photostability of a product in real-life use may however differ from in-laboratory testing, as it can be considerably impacted by the UV filter combinations, the interaction with the non-active sunscreen ingredients, and the exposure to environmental heat (Mancuso et al. 2017; Jung et al. 2012) among many other factors.
Sunscreen Regulation
The regulations for sunscreen testing, labeling and marketing vary worldwide. In the USA sunscreens are considered over the counter drugs, regulated by the FDA. Similarly, sunscreens are considered drugs in Canada (with the exception of mineral filters or para amino-benzoic acid (PABA)-containing products (Sunscreen Monograph 2013)) and therapeutic goods in Australia, if with SPF > 4 (Yap et al. 2017). In contrast, in the EU sunscreens are considered and regulated as cosmetics (Regulation (EC) No 1223/2009), as they are in South American Mercosur, Southeast Asian nations, in China, India, and Japan, with different criteria but with ensuing less strict regulation and scrutiny than medicine products (Mancuso et al. 2017). Consequently, the number of filters that are available and of new filters being approved in the USA and Canada is significantly lower than in the rest of the world, raising some concerns that new, more photostable and stronger UVA protectors are not available on North American markets. In 2019, the FDA has proposed a new ruling, where the inorganic filters have been “generally recognized as safe and effective” (GRASE), but the term was not granted also to 12 organic filters, on which the FDA is seeking additional safety testing (FDA FaDA 2019).
Clinical Benefits of Sunscreens
Developed initially to protect skin from sunburn erythema, sunscreens are currently developed, recommended and used for their benefits in protecting the skin against a wide range of negative effects of the UVR-exposure, most prominently the skin cancer development, but also the photoaging and the many photodermatoses and photo-aggravated disorders.
Benefits of Sunscreens in Preventing Skin Cancer
The benefit of sunscreens in preventing cutaneous oncogenesis is well grounded theoretically, and widely supported by in vitro and animal studies (Young et al. 2017; Suozzi et al. 2020; Mancuso et al. 2017), but is challenging to prove in clinical setting due to the large latency of skin cancer development after sun exposure and the many confounding variables, including behavior- and compliance-related, of the potential study participants.
The strongest evidence comes from the largest randomized clinical trial to date addressing the skin cancer prevention through sunscreen use—the Nambour Skin Cancer prevention Trial, carried out in Australia. In this study, 1621 randomly selected Nambour city residents were randomly assigned to daily application of an SPF 16 sunscreen to head and arms or discretionary sunscreen use and followed-up initially for up to 4.5 years between 1992 and 1996, and further until 2006 (Green et al. 1999; van der Pols et al. 2006). The study found that regular daily sunscreen use had no significant effect on the incidence of basal-cell carcinoma (BCC) but was associated with a significantly lower incidence of cutaneous squamous-cell carcinoma (cSCC) than in the discretionary sunscreen group (0.61 [0.46–0.81]) by 4.5 years follow-up. The effect was maintained after prolonged follow-up 8 years after study, with a nonsignificant decrease in BCC tumor rates and a significant decrease by 40% in incident cSCCs in people formerly randomized to daily sunscreen use compared with the control group.
The same study cohort revealed that ten years after the study’s end the regular sunscreen group had a nonsignificant lower incidence of melanoma, but a significant reduction (3 vs. 11 tumors) in invasive melanoma incidence (Green et al. 2011).
The sunscreens’ protective effect against SCCs is clinically supported by studies in immunosuppressed organ transplant recipients (OTRs), who are at high risk of multiple and aggressive SCCs. In a single-center study, 60 OTRs who applied daily a broad-spectrum sunscreen (>50 SPF, high UVA filter) on sun-exposed areas for 24 months had a significant reduction in the number of actinic keratoses (AKs) (−120 vs. +82), and significantly less new SCCs (0 vs. 8) than the control group of OTR patients, matched for age, and type of and duration since transplant, who were using discretionarily sunscreens of their choice (Ulrich et al. 2009). The sunscreen intervention had a positive but not significant effect against BCC development.
The Nambour trial and a number of other studies showed that regular sunscreen application has a protective effect against the development of actinic keratoses, as patients in sunscreen-daily intervention groups manifested lower overall counts of AKs and lower rates of new AKs development after up to 24 months treatment than the control groups with placebo or discretionary sunscreen use (Green et al. 1999; van der Pols et al. 2006; Darlington et al. 2003).
In conclusion, the regular application of sunscreen has prolonged preventive effects against cSCC, may protect against invasive melanoma, but has no clear benefit in reducing BCC. Despite methodological concerns (Sanchez et al. 2016), this clinical evidence remains the strongest to date.
Benefits of Sunscreens in Preventing Photoaging
Few small clinical studies have shown a beneficial effect of regularly used broad spectrum, high UVB and UVA protection sunscreens in preventing photoaging. The benefit was measured either directly—as the reduction in clinical or histological signs of solar elastosis after up to two years of sunscreen use (Boyd et al. 1995)—or indirectly through the reduction in the cellular and molecular markers of photodamage, like the tissue expression of metalloproteinases MMP1, 9, number of sunburn cells, Langerhans cells depletion, and CPD formation or p53 expression in the UV-irradiated skin (Cole et al. 2014). The largest clinical trial addressing the issue was the Nambour study (Hughes et al. 2013), in 903 subjects, which showed 24% less clinical signs of skin aging over 4.5 years in the intervention group subjects using daily sunscreens, versus control subjects with discretionary sunscreen use.
Sunscreens’ Effect on the Number of Melanocytic Nevi
The number of melanocytic nevi is currently considered the strongest predictive marker for melanoma risk (Gandini et al. 2005; Olsen et al. 2010). A randomized controlled study in 309 white children, aged 6–10 years, showed a reduction in the median nevus count (24 vs. 28) in the study group that applied regularly broad spectrum, SPF 30 sunscreen on sun-exposed areas for 3 years, compared with the children who used no sunscreen (Gallagher et al. 2000). Based on this study, regular sunscreen use in children may prevent the later occurrence of estimatedly 30–40% of acquired nevi (Gallagher et al. 2000; Lee et al. 2005). Given the recognized connection between nevogenesis and melanogenesis (Bastian 2014), these results add arguments that regular sunscreen use started early in childhood may have additive benefit on melanoma prevention at adult age.
Benefits of Sunscreens in the Management of Photodermatoses
Photoprotection through sunscreens has a confirmed place in the treatment and prevention of a wide range of photo-induced and photo-aggravated dermatoses, ranging from genetic DNA repair disorder syndromes (e.g., xeroderma pigmentosum) and porphyrias to polymorphic light eruption and chronic actinic dermatitis, and from cutaneous lupus erythematosus and dermatomyositis to rosacea, seborrheic dermatitis and hyperpigmentation disorders (Schalka 2017; Nahhas et al. 2018; Bylaite et al. 2009; Kuhn et al. 2011; O’Gorman and Murphy 2014). Broad-spectrum sunscreens, with UVA protection and optimally with additional short-wavelength VL filters are the ones recommended in these situations (Lyons et al. 2020). The regular application of the correct amount and the integration of sunscreen use in a comprehensive photoprotection strategy (Bellutti Enders et al. 2017) including photoprotective clothing, seeking shade and avoiding artificial UVR exposure are essential and emphasized across all clinical practice recommendations.
Sunscreens Dosage and Use Recommendations
The protective effect of topical sunscreens depends critically on the correct use, in terms of both amount and frequency of application on the skin. For the sunscreens to achieve the filtering performance of their labeled SPF, the same amount must be applied on the skin as that used for the regulatory-required tests, i.e., 2 mg/cm2. This equals to approximately 30–35 mL (about the cream amount covering one’s palm) to cover the entire body surface (How to select a sunscreen 2020), or a teaspoon (~5 mL) for each body part (limb, front and back of the trunk, face-neck-head).
The amount applied by people in real life however is usually much less, estimatedly in the range 0.5–1 mg/cm2 (Petersen and Wulf 2014). The real SPF decreases with the reduction in the sunscreen amount applied, in a linear or even exponential manner (Petersen and Wulf 2014; Bimczok et al. 2007), so the actual SPF achieved by real-life users likely decreases to 20–50% of the labeled value (Petersen and Wulf 2014). Using a high-SPF (>50) sunscreen might compensate to a certain extent the underuse of suboptimal amounts (Ou-Yang et al. 2012), for limited periods of time, but the importance of applying the correct amount of sunscreen should be clarified to the consumers.
Sunscreens should be applied 20 minutes before the sun exposure and then reapplied every 2 hours when outdoors, more often after swimming, sweating, or using towels. This optimal frequency is also rarely observed in real life (Petersen and Wulf 2014). The development of highly water-resistant sunscreen formulations has helped to compensate to some degree this effect.
The correct application is strongly impacted by the sunscreen’s formulation and vehicle, as gels, lotions and sprays are easier and more comfortable to apply, even on large surfaces and for oily skin types, than creams and ointments, but they are usually applied in thin-layered, suboptimal amount.
The current recommendations by the World Health Organization (WHO), medical professional societies and clinical guidelines worldwide support in consensus the regular use of sunscreens with broad UVB and UVA spectrum, SPF >15 [or >30 by some recommendations (How to select a sunscreen 2020)], applied in 2 mg/cm2 amount, before and repeatedly during sun exposure, in conjunction with other physical and behavioral methods of sun protection like using photoprotective clothing including hats and sunglasses, seeking shade, and avoiding peak-hour sun exposures and artificial tanning devices (sunbeds).
Adverse Effects of Sunscreens
The adverse effects reported after topical sunscreen application include irritative and allergic contact dermatitis, acne and acneiform rashes and photoallergic and phototoxic dermatitis (Heurung et al. 2014). The vast majority of these reactions are caused actually by the inactive ingredients within the sunscreen formulations. However, in rare cases phototoxic or photoallergic reactions may be caused by photo-absorbing, epidermis-penetrating active UV filters (Darvay et al. 2001). The benzophenones and dibenzoylmethanes are the UV filters most commonly implicated in allergic and photoallergic contact dermatitis reactions, with oxybenzone as the leading allergen and photoallergen within this class, frequently used in commercial formulations (Heurung et al. 2014). Nevertheless, taking into account the enormous increase in sunscreen use, the occurrence of true UV-filter-induced phototoxic/photoallergic reactions remains a very rare event (Darvay et al. 2001).
Sunscreens: Concerns and Controversies
Beyond the significant proven benefits of sunscreens and their good tolerance profile, some concerns have been raised lately over their potential longer-term harms for human users and the environment alike.
Increased Duration of Sun Exposure
An important concern is that widespread sunscreen use induces a false safety feeling and are actually increasing the photoexposure duration. It was indeed showed that the use of higher-SPF sunscreens that canceled the limiting erythema of the sunburn significantly increased the duration of recreational sun exposure, including sunbathing, of young white Europeans (Autier et al. 1999). This behavior has higher impact on photocarcinogenesis if the sunscreen used provides UVB but not adequate UVA protection. Hence the need to emphasize to the public the necessity to use regularly broad-spectrum sunscreens, with high SPF and UVA protection, in the correct amount, in addition to and not replacing sun-avoidance behaviors.
Paradoxical Increase in Skin Cancer Risk
Some earlier case-control studies associated sunscreen use with higher risk of melanoma (Westerdahl et al. 2000; Wolf et al. 1998). However, it is now considered that this effect was likely due to increased time spent in the sun by the sunscreen users who escaped the painful sunburn thanks to the UVB filters, to the use of earlier sunscreens without efficient UVA protection, or to the use of overall low-level protection (SPF < 10) sunscreens (Suozzi et al. 2020; Jansen et al. 2013).
Percutaneous Systemic Absorption
As organic UV filters are able to penetrate within the living epidermis, a major emerging concern is their potential systemic absorption and impact on human developmental and endocrine systems, as well as on carcinogenesis. Two very recent randomized clinical trials (Matta et al. 2019, 2020) showed that after maximal topical use (sunscreen application of 2 mg/cm2, covering 75% of the body surface, 4 times daily) seven of the FDA-approved organic filters had plasma levels exceeding the 0.5 ng/mL threshold above which FDA requires systemic safety testing. The plasma levels surpassed the threshold already after the first application, and remained higher than the threshold for as long as 4 days after the last application. The highest levels were noted for oxybenzone, which has also been linked with estrogenic effects in animal studies (Buck Louis et al. 2015; Watanabe et al. 2015). It is not known yet what the biological effects of these high plasma levels on human health are, nor how frequently they are attained in real-life use, where sunscreens are applied in amounts significantly lower than those employed in the trials. The FDA is currently seeking additional safety testing on the organic filters, without however deeming them unsafe (FDA FaDA 2019). In 2022 the (European Commission 2022), following the opinion of the Scientific Committee on Consumer Safety (SCCS) has amended the Annex VI to the EU Cosmetics Regulation — namely, the list of UV filters allowed in cosmetic products, to reduce the concentrations allowed in sunscreen formulations of two organic UV filters with potential endocrine disrupting properties: benzophenone-3 and octocrylene.
The systemic absorption and its impact are not a concern for inorganic filters, as both FDA and SCCS stated, although nanosized ZnO particles have been found within the epidermis and the pilosebaceous units have been linked, although without conclusive evidence, to frontal fibrosing alopecia (Robinson et al. 2020). Most animal and human studies showed that nano-TiO2 did not penetrate beyond the outer layers of stratum corneum to viable cells and did not reach the general circulation, either in healthy or in compromised skin (Dréno et al. 2019).
Oxidative Damage and Antioxidants
The addition to sunscreen formulations of natural antioxidants with reactive oxygen species (ROS)-scavenging properties, like vitamin E, vitamin C, or ubiquinone (coQ10) has been proposed as a strategy to enhance the protection against the UVR-induced oxidative damage. Topical antioxidants have been shown to decrease the amount of free oxygen radicals or the number of sunburn cells in the UV-irradiated skin and to enhance the measured SPF when combined with UV filters (Syring et al. 2016; Nichols and Katiyar 2010). Consequently, antioxidant-enriched sunscreen formulations became commercially available in Europe. However, recent studies in animal models found that antioxidants delayed the development of cSCC and melanoma in UV-irradiated mice, but once the melanoma occurred, the products accelerated the tumor growth (Cassidy et al. 2013; Burke et al. 2014). This raised the concern of a double-phased effect of antioxidants, as they appear to inhibit initially the tumorigenesis by reducing ROS-induced DNA damage, but once the tumorigenesis occurs, they may accelerate tumor growth by protecting tumor cells from the same ROS damage. Their true benefit in topical sunscreen formulations, especially in patients with already sun-damaged skin or field cancerization, remains thus to be determined.
Vitamin D Depletion
A heated, intensively media-covered debate is ongoing on the potential role of high-SPF sunscreens in inducing vitamin D depletion through inhibiting its UVB-mediated synthesis in the skin. These concerns have been augmented by the recent studies suggesting a possible link between vitamin D deficiency and immunosuppression, oncogenesis and unfavorable cancer outcomes, including for melanoma (Autier et al. 2017; Stucci et al. 2018; Vaughan-Shaw et al. 2017). The available evidence on the relationship between sunscreen use and vitamin D status has been reviewed recently and the studies concluded that daily, reasonable use of broad-spectrum sunscreens with high UVA protection in optimal amount will not negatively impact vitamin D status in healthy people (Neale et al. 2019; Passeron et al. 2019). It was noted at the same time that consistent photoprotection for people with photosensitivity disorders or skin cancer risk, which includes high-protection sunscreen use together with photoprotective clothing and sun-avoidance behavior, will likely cause vitamin D insufficiency. This insufficiency can be easily redressed however by diet and oral supplementation. Consequently, for patients with photosensitivity disorders or photocarcinogenic risk it is recommended to pursue the consistent photoprotection, including sunscreen use, which is crucial for disease prevention, in combination with screening for vitamin D status and oral vitamin D supplementation in case of defficiency.
Effects on the Environment
It is estimated that 4000–14,000 tons of UV filter residues are entering annually the planet’s oceans and seas, washing off from the touristic coastal areas (Downs et al. 2016). Additionally, UV filters were identified in natural and drinking water in some countries (da Silva et al. 2015). Several studies showed the bioaccumulation of organic UV filters, especially oxybenzone, within various species of fish worldwide, and this compound induced in laboratory setting toxic effect on corals, including coral bleaching, and impaired reproduction in fish species (Schneider and Lim 2019). Together, these findings raised increasing concerns for the consequences of widespread sunscreen use on the marine ecosystems, culminating with legislation passed in 2018 by the state of Hawaii followed by several other Atlantic and Pacific territories that banned the use of some UV filters potentially harmful for the coral reefs. To date, there is no evidence yet for harmful effects on human health from marine exposure to UV filter residues through the food chain, nor is it known to which degree these residues in oceans actually contribute to the coral reefs’ degradation (Galamgam et al. 2018). However, they may synergize with the other current threats to the marine ecosystems and life through climate change and pollution. Further studies are needed to classify the potential environmental effects of sunscreens.
Future Developments for Sunscreens
The topical sunscreens have undergone major development since their introduction six decades ago and the efforts continue to ameliorate these products, addressing the concerns of broad-spectrum protection, photostability, cosmesis and compliance, systemic absorption and effects, interference with the health-favorable UV effects such as immunomodulation and vitamin D synthesis and environmental impact. The main development strategies include the bioengineering of UV filter molecules to increase their photostability and decrease their tissue penetrance, like through the encapsulation of organic filter compounds in mesoporous silica, or into bioadhesive nanoparticles able to bind covalently to the stratum corneum (Suozzi et al. 2020). New molecules within UVC (220–280 nm) absorption capacities are also researched.
Another breakthrough development in this direction is the supplementation of traditional UV filters with new compounds able to counter the carcinogenic UV effects downstream, at molecular levels, including new ROS scavengers, DNA repair enzymes, or immune cytokine modulators (Suozzi et al. 2020).
Conclusion
Topical sunscreens with broad UVB and UVA filtering spectrum, regularly used in sufficient amount, have an established role in the prevention of skin cancers and photoaging and in the management of a wide range of photo-induced and photo-aggravated dermatoses. Their benefit/safety profile is optimal when used judiciously, in conjunction with other physical and behavioral methods of photoprotection. While more research is warranted on their intensive use’s effects on human and environment health, new products are continuously developed with improved stability, safety and protective properties.
References
Autier P, Dore JF, Negrier S, Lienard D, Panizzon R, Lejeune FJ, et al. Sunscreen use and duration of sun exposure: a double-blind, randomized trial. J Natl Cancer Inst. 1999;91(15):1304–9. Epub 1999/08/05
Autier P, Mullie P, Macacu A, Dragomir M, Boniol M, Coppens K, et al. Effect of vitamin D supplementation on non-skeletal disorders: a systematic review of meta-analyses and randomised trials. Lancet Diabetes Endocrinol. 2017;5(12):986–1004.
Bastian BC. The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annu Rev Pathol. 2014;9:239–71.
Bastien N, Millau JF, Rouabhia M, Davies RJ, Drouin R. The sunscreen agent 2-phenylbenzimidazole-5-sulfonic acid photosensitizes the formation of oxidized guanines in cellulo after UV-A or UV-B exposure. J Invest Dermatol. 2010;130(10):2463–71.
Bellutti Enders F, Bader-Meunier B, Baildam E, Constantin T, Dolezalova P, Feldman BM, et al. Consensus-based recommendations for the management of juvenile dermatomyositis. Ann Rheum Dis. 2017;76(2):329–40.
Bimczok R, Gers-Barlag H, Mundt C, Klette E, Bielfeldt S, Rudolph T, et al. Influence of applied quantity of sunscreen products on the sun protection factor--a multicenter study organized by the DGK Task Force Sun Protection. Skin Pharmacol Physiol. 2007;20(1):57–64.
Boyd AS, Naylor M, Cameron GS, Pearse AD, Gaskell SA, Neldner KH. The effects of chronic sunscreen use on the histologic changes of dermatoheliosis. J Am Acad Dermatol. 1995;33(6):941–6.
Buck Louis GM, Chen Z, Kim S, Sapra KJ, Bae J, Kannan K. Urinary concentrations of benzophenone-type ultraviolet light filters and semen quality. Fertil Steril. 2015;104(4):989–96.
Burke KE, Zhou X, Wang Y, Commisso J, Keen CL, Nakamura RM, et al. The effects of topical L-selenomethionine on protection against UVB-induced skin cancer when given before, during, and after UVB exposure. J Drugs Dermatol. 2014;13(10):1214–23.
Bylaite M, Grigaitiene J, Lapinskaite GS. Photodermatoses: classification, evaluation and management. Br J Dermatol. 2009;161(Suppl 3):61–8.
Cassidy PB, Fain HD, Cassidy JP Jr, Tran SM, Moos PJ, Boucher KM, et al. Selenium for the prevention of cutaneous melanoma. Nutrients. 2013;5(3):725–49.
Cole C, Appa Y, Ou-Yang H. A broad spectrum high-SPF photostable sunscreen with a high UVA-PF can protect against cellular damage at high UV exposure doses. Photodermatol Photoimmunol Photomed. 2014;30(4):212–9.
Cole C, Shyr T, Ou-Yang H. Metal oxide sunscreens protect skin by absorption, not by reflection or scattering. Photodermatol Photoimmunol Photomed. 2016;32(1):5–10.
Collaris EJ, Frank J. Photoallergic contact dermatitis caused by ultraviolet filters in different sunscreens. Int J Dermatol. 2008;47(Suppl 1):35–7.
Cosmetics Europe: Guidelines for evaluating sun product water resistance. Available from: https://cosmeticseurope.eu/publications-cosmetics-europe-association/guidelines.htmlview=item&id=18. (2005).
Crosera M, Prodi A, Mauro M, Pelin M, Florio C, Bellomo F, et al. Titanium dioxide nanoparticle penetration into the skin and effects on HaCaT cells. Int J Environ Res Public Health. 2015;12(8):9282–97.
da Silva CP, Emídio ES, de Marchi MR. The occurrence of UV filters in natural and drinking water in São Paulo State (Brazil). Environ Sci Pollut Res Int. 2015;22(24):19706–15.
Darlington S, Williams G, Neale R, Frost C, Green A. A randomized controlled trial to assess sunscreen application and beta carotene supplementation in the prevention of solar keratoses. Arch Dermatol. 2003;139(4):451–5.
Darvay A, White IR, Rycroft RJ, Jones AB, Hawk JL, McFadden JP. Photoallergic contact dermatitis is uncommon. Br J Dermatol. 2001;145(4):597–601.
Downs CA, Kramarsky-Winter E, Segal R, Fauth J, Knutson S, Bronstein O, et al. Toxicopathological effects of the sunscreen UV filter, oxybenzone (benzophenone-3), on coral planulae and cultured primary cells and its environmental contamination in Hawaii and the U.S. Virgin Islands. Arch Environ Contam Toxicol. 2016;70(2):265–88.
Dréno B, Alexis A, Chuberre B, Marinovich M. Safety of titanium dioxide nanoparticles in cosmetics. J Eur Acad Dermatol Venereol. 2019;33(Suppl 7):34–46.
European Commission. Commission Regulation (EU) 2022/1176 of 7 July 2022 amending Regulation (EC) No 1223/2009 of the European Parliament and of the Council as regards the use of certain UV filters in cosmetic products. 2022. Retrieved on 08/06/2023 from https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32022R1176&from=EN.
FDA. Labeling and effectiveness testing; sunscreen drug products for over-the-counter human use. Fed Regist. 2011;76:FR 35619.
FDA FaDA. Sunscreen drug products for over-the-counter human use: proposed rule. Fed Regis. 2019;84(38) Available from: https://www.federalregister.gov/documents/2019/04/18/2019-07712/sunscreen-drug-productsfor-over-the-counter-human-use-correction
Galamgam J, Linou N, Linos E. Sunscreens, cancer, and protecting our planet. Lancet Planet Health. 2018;2(11):e465–e6.
Gallagher RP, Rivers JK, Lee TK, Bajdik CD, McLean DI, Coldman AJ. Broad-spectrum sunscreen use and the development of new nevi in white children: a randomized controlled trial. JAMA. 2000;283(22):2955–60.
Gandini S, Sera F, Cattaruzza MS, Pasquini P, Abeni D, Boyle P, et al. Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi. Eur J Cancer. 2005;41(1):28–44.
Green A, Williams G, Neale R, Hart V, Leslie D, Parsons P, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet. 1999;354(9180):723–9.
Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29(3):257–63.
Guidelines on stability testing of cosmetic products Cosmetics Europe. 2004.
Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006;41(8):1205–12.
Heurung AR, Raju SI, Warshaw EM. Adverse reactions to sunscreen agents: epidemiology, responsible irritants and allergens, clinical characteristics, and management. Dermatitis. 2014;25(6):289–326.
How to select a sunscreen. July 2020. Available from: https://www.aad.org/public/spot-skin-cancer/learn-about-skincancer/prevent/how-to-select-a-sunscreen
Hughes MC, Williams GM, Baker P, Green AC. Sunscreen and prevention of skin aging: a randomized trial. Ann Intern Med. 2013;158(11):781–90.
International Organization for Standardization. ISO 24443: 2012. Determination of sunscreen UVA photoprotection in vitro. 2012.
Jansen R, Osterwalder U, Wang SQ, Burnett M, Lim HW. Photoprotection: part II. Sunscreen: development, efficacy, and controversies. J Am Acad Dermatol. 2013;69(6):867 e1–14. quiz 81–2
Jung GW, Ting PT, Salopek TG. Stability of sunscreens and sunblocks following exposure to extreme temperatures. J Am Acad Dermatol. 2012;66(6):1007–9.
Kuhn A, Ruland V, Bonsmann G. Cutaneous lupus erythematosus: update of therapeutic options part I. J Am Acad Dermatol. 2011;65(6):e179–93.
Lee TK, Rivers JK, Gallagher RP. Site-specific protective effect of broad-spectrum sunscreen on nevus development among white schoolchildren in a randomized trial. J Am Acad Dermatol. 2005;52(5):786–92.
Lyons AB, Trullas C, Kohli I, Hamzavi IH, Lim HW. Photoprotection beyond ultraviolet radiation: a review of tinted sunscreens. J Am Acad Dermatol. 2020;
Mahmoud BH, Ruvolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130(8):2092–7.
Maier T, Korting HC. Sunscreens - which and what for? Skin Pharmacol Physiol. 2005;18(6):253–62.
Mancuso JB, Maruthi R, Wang SQ, Lim HW. Sunscreens: an update. Am J Clin Dermatol. 2017;18(5):643–50.
Matta MK, Zusterzeel R, Pilli NR, Patel V, Volpe DA, Florian J, et al. Effect of sunscreen application under maximal use conditions on plasma concentration of sunscreen active ingredients: a Randomized Clinical Trial. JAMA. 2019;321(21):2082–91.
Matta MK, Florian J, Zusterzeel R, Pilli NR, Patel V, Volpe DA, et al. Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a Randomized Clinical Trial. JAMA. 2020;323(3):256–67.
Moseley H, Cameron H, MacLeod T, Clark C, Dawe R, Ferguson J. New sunscreens confer improved protection for photosensitive patients in the blue light region. Br J Dermatol. 2001;145(5):789–94.
Nahhas AF, Oberlin DM, Braunberger TL, Lim HW. Recent developments in the diagnosis and management of photosensitive disorders. Am J Clin Dermatol. 2018;19(5):707–31.
Neale RE, Khan SR, Lucas RM, Waterhouse M, Whiteman DC, Olsen CM. The effect of sunscreen on vitamin D: a review. Br J Dermatol. 2019;181(5):907–15.
Nichols JA, Katiyar SK. Skin photoprotection by natural polyphenols: anti-inflammatory, antioxidant and DNA repair mechanisms. Arch Dermatol Res. 2010;302(2):71–83.
O’Gorman SM, Murphy GM. Photoaggravated disorders. Dermatol Clin. 2014;32(3):385–98. ix
Olsen CM, Carroll HJ, Whiteman DC. Estimating the attributable fraction for cancer: A meta-analysis of nevi and melanoma. Cancer Prev Res (Phila). 2010;3(2):233–45.
Ou-Yang H, Stanfield J, Cole C, Appa Y, Rigel D. High-SPF sunscreens (SPF >/= 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67(6):1220–7.
Passeron T, Bouillon R, Callender V, Cestari T, Diepgen TL, Green AC, et al. Sunscreen photoprotection and vitamin D status. Br J Dermatol. 2019;181(5):916–31.
Petersen B, Wulf HC. Application of sunscreen − theory and reality. Photodermatol Photoimmunol Photomed. 2014;30(2-3):96–101.
Regazzetti C, Sormani L, Debayle D, Bernerd F, Tulic MK, De Donatis GM, et al. Melanocytes sense blue light and regulate pigmentation through opsin-3. J Invest Dermatol. 2018;138(1):171–8.
Regulation (EC) No 1223/2009 of the European Parliament and of the Council of 30 November 2009 on cosmetic products. OJ L 342. 2009(22.12.2009):59–209.
Robinson G, McMichael A, Wang SQ, Lim HW. Sunscreen and frontal fibrosing alopecia: a review. J Am Acad Dermatol. 2020;82(3):723–8.
Robyn L, McMichael T, Smith W, Armstrong B. Solar ultraviolet radiation: global burden of disease from solar ultraviolet radiation. World Health Organization; 2006.
Sanchez G, Nova J, Rodriguez-Hernandez AE, Medina RD, Solorzano-Restrepo C, Gonzalez J, et al. Sun protection for preventing basal cell and squamous cell skin cancers. Cochrane Database Syst Rev. 2016;7:CD011161.
Schalka S. New data on hyperpigmentation disorders. J Eur Acad Dermatol Venereol. 2017;31(Suppl 5):18–21.
Schneider SL, Lim HW. Review of environmental effects of oxybenzone and other sunscreen active ingredients. J Am Acad Dermatol. 2019;80(1):266–71.
Schulze R. Einige Versuche und Bemerkungen zum Problem der handelsüblichen Lichtschutzmittel. Parf Kosm. 1956;37:310–5.
Sha B, Gao W, Cui X, Wang L, Xu F. The potential health challenges of TiO2 nanomaterials. J Appl Toxicol. 2015;35(10):1086–101.
Stucci LS, D'Oronzo S, Tucci M, Macerollo A, Ribero S, Spagnolo F, et al. Vitamin D in melanoma: controversies and potential role in combination with immune check-point inhibitors. Cancer Treat Rev. 2018;69:21–8.
Sunscreen Monograph. 2013.
Suozzi K, Turban J, Girardi M. Cutaneous photoprotection: a review of the current status and evolving strategies. Yale J Biol Med. 2020;93(1):55–67.
Syring F, Weigmann HJ, Schanzer S, Meinke MC, Knorr F, Lademann J. Investigation of model sunscreen formulations comparing the sun protection factor, the universal sun protection factor and the radical formation ratio. Skin Pharmacol Physiol. 2016;29(1):18–23.
Technical Committee ISO/TC 217, Cosmetics. ISO 24444: 2010. Cosmetics -sun protection test methods - in vivo determination of the sun protection factor (SPF). 2010.
Ulrich C, Jurgensen JS, Degen A, Hackethal M, Ulrich M, Patel MJ, et al. Prevention of non-melanoma skin cancer in organ transplant patients by regular use of a sunscreen: a 24 months, prospective, case-control study. Br J Dermatol. 2009;161(Suppl 3):78–84.
van der Pols JC, Williams GM, Pandeya N, Logan V, Green AC. Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use. Cancer Epidemiol Biomark Prev. 2006;15(12):2546–8.
Varedi A, Wu YP, Klein SZ, Leachman SA, Grossman D. Mineral sunscreens not recommended by Consumer Reports: suggestions to improve the review process. J Am Acad Dermatol. 2019;80(3):832–3.
Vaughan-Shaw PG, O'Sullivan F, Farrington SM, Theodoratou E, Campbell H, Dunlop MG, et al. The impact of vitamin D pathway genetic variation and circulating 25-hydroxyvitamin D on cancer outcome: systematic review and meta-analysis. Br J Cancer. 2017;116(8):1092–110.
Watanabe Y, Kojima H, Takeuchi S, Uramaru N, Sanoh S, Sugihara K, et al. Metabolism of UV-filter benzophenone-3 by rat and human liver microsomes and its effect on endocrine-disrupting activity. Toxicol Appl Pharmacol. 2015;282(2):119–28.
Westerdahl J, Ingvar C, Masback A, Olsson H. Sunscreen use and malignant melanoma. Int J Cancer. 2000;87(1):145–50.
Williams JD, Maitra P, Atillasoy E, Wu MM, Farberg AS, Rigel DS. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78(5):902–10 e2.
Wolf P, Quehenberger F, Mullegger R, Stranz B, Kerl H. Phenotypic markers, sunlight-related factors and sunscreen use in patients with cutaneous melanoma: an Austrian case-control study. Melanoma Res. 1998;8(4):370–8.
Yap FH, Chua HC, Tait CP. Active sunscreen ingredients in Australia. Australas J Dermatol. 2017;58(4):e160–e70. Epub 2017/03/16
Young AR, Claveau J, Rossi AB. Ultraviolet radiation and the skin: Photobiology and sunscreen photoprotection. J Am Acad Dermatol. 2017;76(3S1):S100–S9.
Zastrow L, Lademann J. Light - instead of UV protection: new requirements for skin cancer prevention. Anticancer Res. 2016;36(3):1389–93.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Forsea, AM. (2023). Sunscreens. In: Katsambas, A.D., Lotti, T.M., Dessinioti, C., D'Erme, A.M. (eds) European Handbook of Dermatological Treatments. Springer, Cham. https://doi.org/10.1007/978-3-031-15130-9_156
Download citation
DOI: https://doi.org/10.1007/978-3-031-15130-9_156
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-15129-3
Online ISBN: 978-3-031-15130-9
eBook Packages: MedicineMedicine (R0)