Abstract
Coronavirus disease 2019 (COVID-19) is an emerging infectious disease. Bilateral pneumonia, acute respiratory failure, systemic inflammation, endothelial dysfunction, and coagulation activation have been described as key features of severe COVID-19.
Fibrinogen and D-dimer are typically increased. Moreover, the risk for venous thromboembolism is markedly increased, especially in patients in the intensive care unit, often despite prophylactic-dose anticoagulation. Pulmonary microvascular thrombosis has also been described and the risk for arterial thrombotic diseases also appears to be increased. Bleeding is less common than thrombosis but can occur.
Evaluation for venous thromboembolism may be challenging because symptoms of pulmonary embolism overlap with COVID-19, and imaging studies may not be feasible in all cases. All inpatients should receive thromboprophylaxis unless contraindicated. In hospitalized patients with COVID-19, prophylactic dosing rather than more intensive (intermediate or therapeutic) dosing are suggested. On the other hand, therapeutic dose of anticoagulation is always appropriate to treat deep venous thrombosis or pulmonary embolism, unless contraindicated.
This article reviews evaluation and management of coagulation abnormalities in individuals with COVID-19.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
A novel coronavirus was identified in late 2019 that rapidly reached pandemic proportions. The World Health Organization has designated the disease caused by the virus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) as coronavirus disease 2019 (COVID-19). Bilateral pneumonia, acute respiratory failure (ARF), systemic inflammation, endothelial dysfunction, and coagulation activation has been described as key features of severe COVID-19 [1,2,3,4,5,6]. An increased risk of venous thromboembolism (VTE) in patients with COVID-19 pneumonia admitted to intensive care unit (ICU) [7,8,9,10,11] and in non-ICU wards has been reported despite adequate thromboprophylaxis. Thus, several authors [7, 8] suggested that higher anticoagulation targets than in usual critically ill patients should probably be taken into consideration for patients with COVID-19 pneumonia.
This review provides practical information for evaluation and management of coagulation abnormalities in individuals with COVID-19.
2 SARS-CoV-2 Clinical Feature
SARS-CoV-2 outcome seems to be determined by the extent of the host immune system imbalance. The primary immune response usually leads to viral clearance. However, for unclear reasons, the secondary immune response may be exaggerated and, in some cases, may lead to multiple organ failure, acute respiratory distress syndrome (ARDS), and death [12]. This exaggerated response is known as cytokine release syndrome (CRS), and it has an important role in the activation of coagulation.
The spectrum of symptomatic COVID-19 infection ranges from mild to critical; most infections are not severe. Specifically, in a report from the Chinese Center for Disease Control and Prevention, that included approximately 44,500 confirmed infections, an estimation of disease severity was described [13]. Mild disease (or mild pneumonia) was reported in 81%. Severe disease (e.g., with dyspnea, hypoxia, or >50% lung involvement on imaging within 24–48 h) was described in 14%. Critical disease (e.g., with respiratory failure, shock, or multiorgan dysfunction) was identified in 5%. The overall case fatality rate was 2.3%; no deaths were reported among noncritical cases. Among hospitalized patients, the proportion of critical or fatal disease is higher. In a study that included 2741 patients who were hospitalized for COVID-19 in a New York City health care system, 665 patients (24%) died or were discharged to hospice [14]. Of the 749 patients who received intensive care (27% of the total hospitalized cohort), 647 received invasive mechanical ventilation; of those patients, 60% died and 13% were still ventilated. In Italy, 12% of all detected COVID-19 cases and 16% of all hospitalized patients were admitted to the ICU; the estimated case fatality rate was 7.2% [15, 16].
Individuals of any age can acquire SARS-CoV-2 infection, although adults of middle age and older are most commonly affected, and older adults are more likely to have severe disease. Symptomatic infection in children and adolescents appears to be relatively uncommon; when it occurs, it is usually mild, although a small proportion (e.g., <2%) experience severe and even fatal disease. Severe illness can occur in otherwise healthy individuals, but it predominantly occurs in adults with underlying medical comorbidities. Comorbidities and other conditions that have been associated with severe illness and mortality include cardiovascular disease, diabetes mellitus, hypertension, chronic lung disease, cancer (in particular hematologic malignancies, lung cancer, and metastatic disease), chronic kidney disease, obesity, and smoking. In a report of 355 patients who died with COVID-19 in Italy, the mean number of pre-existing comorbidities was 2.7, and only three patients had no underlying condition [16].
Asymptomatic infections have also been well documented [17]. The proportion of infections that are asymptomatic has not been systematically and prospectively studied. One literature review estimated that it is as high as 30 to 40%, based on data from two large cohorts that identified cases through population-based testing [17, 18].
The incubation period for COVID-19 is generally within 14 days following exposure, with most cases occurring approximately 4–5 days after exposure.
Pneumonia appears to be the most frequent serious manifestation of infection, characterized primarily by fever, cough, dyspnea, and bilateral infiltrates on chest imaging [3]. However, other features, including upper respiratory tract symptoms, myalgias, diarrhea, and smell or taste disorders, are also common. Although some clinical features (in particular smell or taste disorders) are more common with COVID-19 than with other viral respiratory infections, there are no specific symptoms or signs that can reliably distinguish COVID-19. Some patients with initially nonsevere symptoms may progress over the course of a week [19].
Common laboratory findings among hospitalized patients with COVID-19 include lymphopenia, elevated aminotransaminase levels, elevated lactate dehydrogenase levels, elevated inflammatory markers (e.g., ferritin, C-reactive protein, and erythrocyte sedimentation rate), and abnormalities in D-dimer levels (see Table 8.1). Several laboratory features, including high D-dimer levels and more severe lymphopenia, have been associated with critical illness or mortality [4].
Common abnormal radiograph findings in patients with COVID-19 most were consolidation and ground-glass opacities, with bilateral, peripheral, and lower lung zone distributions. Chest CT commonly demonstrates ground-glass opacification with or without consolidative abnormalities. Chest CT abnormalities are often bilateral, have a peripheral distribution, and involve the lower lobes. Among patients who clinically improve, resolution of radiographic abnormalities may lag behind improvements in fever and hypoxia.
Several complications of COVID-19 have been described. ARDS is the major complication in patients with severe disease. Other complications have included arrhythmias, acute cardiac injury, and shock. Thromboembolic complications, including pulmonary embolism and acute stroke, have also been reported. Other inflammatory complications and auto-antibody-mediated manifestations have been described. Guillain-Barré syndrome may occur, with onset 5–10 days after initial symptoms. A multisystem inflammatory syndrome with clinical features similar to those of Kawasaki disease and toxic shock syndrome has also been described in children with COVID-19.
The proportion of patients with COVID-19 who are diagnosed with ARDS on the basis of oxygenation criteria ranges between 20% and 67% in patients admitted to hospital and is 100% in mechanically ventilated patients [20, 21]. Grasselli et al. recently published a systematic analysis of clinical and laboratory features in patients with COVID-19-associated ARDS in 301 consecutive patients prospectively enrolled in 7 Italian hospitals [15]. They compared the pathophysiology of COVID-19-related ARDS with classical ARDS using two large historical datasets, showing that patients with COVID-19-associated ARDS have a form of injury that is similar to that of classical ARDS characterized by decreased compliance and increased lung weight. In many patients, this injury was complicated by increased dead space, which was probably related to diffuse microthrombi or emboli of the pulmonary vascular bed. In this study, patients with COVID-19-related ARDS had a median static compliance of the respiratory system 28% higher in patients with COVID-19 (n = 297; 41 mL/cm H2O [IQR 33–52]) than in those with classical ARDS (n = 960; 32 mL/cm H2O [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40], p < 0·0001). Moreover, they found that most of the patients had markedly increased D-dimer concentrations (median 1880 ng/mL [IQR 820–6243]). In this study, 28-day mortality was 36% (93 of 261 patients). In particular, when an easily identified phenotype of increased parenchymal damage (low static compliance) and increased D-dimer concentrations occurs together, mortality is extremely high.
Secondary infections including respiratory infections and bacteremia do not appear to be common complications of COVID-19 overall, although data are limited [41]. Several reports have described presumptive invasive aspergillosis among immunocompetent patients with ARDS from COVID-19, although the frequency of this complication is uncertain [42].
Recovery time appears to be around 2 weeks for mild infections and 3–6 weeks for severe disease based on early data from China. However, the recovery course is variable and depends on age and pre-existing comorbidities in addition to illness severity.
Systematic evaluation of the long-term sequelae of COVID-19 is lacking, but emerging data [43] suggest the potential for ongoing respiratory impairment. Moreover, cardiac imaging studies have suggested the potential for cardiac sequelae after COVID-19 [22].
3 Coagulation Abnormalities in Patients with COVID-19
SARS-CoV-2 may predispose patients to thrombotic disease, both in the venous and arterial circulation, due to excessive inflammation, platelet activation, and endothelial dysfunction [23,24,25]. The predominant coagulation abnormalities in patients with COVID-19 are summarized in Table 8.2. Bleeding does not appear to be a major manifestation of COVID-19. However, patients may have bleeding for other reasons, including trauma and/or treatment with anticoagulation. If it occurs, treatment is similar to non-COVID-19 patients and may include transfusions, anticoagulant reversal or discontinuation, or specific products for underlying bleeding disorders.
Laboratory findings in COVID-19 are the following: prothrombin time (PT) and activated partial thromboplastin time (aPTT) normal or slightly prolonged, platelet counts normal or increased, fibrinogen increased, D-dimer increased, factor VIII activity increased, von Willebrand factor (VWF) antigen greatly increased, and minor changes in natural anticoagulants (i.e., small decreases in antithrombin and small increase in protein C) [26]. The presence of a lupus anticoagulant (LA) is common in individuals with a prolonged aPTT. Very elevated levels of D-dimer have been observed that correlate with illness severity, especially if levels are increased several-fold [27].
This state appears to be distinct from disseminated intravascular coagulation (DIC), even if some critical patients with COVID-19 have met criteria for probable DIC. Clinical findings of acute DIC include bleeding, thrombocytopenia, prolonged PT and aPTT, low plasma fibrinogen, elevated plasma D-dimer, and microangiopathic changes on peripheral blood smear. DIC is a clinical and laboratory diagnosis. The International Society on Thrombosis and Haemostasis (ISTH) has developed in 2009 a scoring system to be applied to individuals with an underlying disorder associated with DIC, which incorporates laboratory features including the PT, platelet count, fibrinogen level, and D-dimer [28]. The ISTH scoring system (see Table 8.3) is reported to have a sensitivity of 91% and a specificity of 97%, but is not widely used. COVID-19 has some similar laboratory findings to DIC, including a marked increase in D-dimer and in some cases, mild thrombocytopenia. However, other coagulation parameters in COVID-19 are distinct from DIC. In particular, the typical findings of high fibrinogen and high factor VIII activity suggest that major consumption of coagulation factors is not occurring [26]. As a matter of fact, in one of the largest series that reported thromboembolic events in subjects with COVID-19, none of the patients developed overt DIC [8].
The pathogenesis of hypercoagulability in COVID-19 is incompletely understood. However, we know that cytokine release syndrome (CRS) is thought to play an important role in disease severity [29]. CRS is associated with increased levels of inflammatory cytokines and activation of T lymphocytes, macrophages, and endothelial cells. In particular, interleukin 6 and tumor necrosis factor seems to hold a key role leading to vascular leakage and to activation of complement, tissue factor, and coagulation cascade [30, 31]. Moreover, all three of the major contributions of Virchow’s triad to clot formation (i.e., endothelial injury, stasis, and hypercoagulable state) apply to severe COVID-19 infection. There is evidence of direct invasion of endothelial cells by the SARS-CoV-2 virus, potentially leading to endothelial injury [32]. Other sources of endothelial injury include intravascular catheters and mediators of the acute systemic inflammatory response such as cytokines (e.g., interleukin 6) and other acute phase reactants [33]. The contribution of complement-mediated endothelial injury has also been suggested [34]. Immobilization can cause stasis of blood flow in all hospitalized and critically ill patients, regardless of whether they have COVID-19. Finally, a number of changes in circulating prothrombotic factors have been found in patients with severe COVID-19: elevated factor VIII, elevated fibrinogen, neutrophil extracellular traps (NETs), and hyperviscosity [26, 35].
These coagulation abnormalities in the direction of an underlying hypercoagulable state raise questions about appropriate evaluations and interventions to prevent or treat thrombosis.
4 Venous Thromboembolism in Critically Ill Patients
Critically ill patients have an increased risk of VTE of the upper and lower extremities. The risk factors include immobility associated with serious illness such as sepsis and trauma and invasive procedures such as central venous lines [36]. The most serious manifestation of VTE is pulmonary embolism (PE). Of all PEs, 90% are estimated to originate from deep venous thrombosis (DVT) of the lower limbs [37]. DVT and PE share common risk factors [38].
The main clinical importance of DVT lies in its association with potentially life-threatening PE. In critically ill patients with impaired cardiopulmonary reserve, a small PE might have severe or fatal sequelae. In addition, evaluation for VTE in critical ill patients may be challenging. Thus, some mechanically ventilated patients with sudden episodes of hypotension, tachycardia, or hypoxia may have undetected PE [39].
PE is stratified into massive, sub-massive, and low risk based upon the presence or absence of hypotension and right ventricular dysfunction or dilation. This stratification is associated with mortality risk [40].
The prevalence of VTE in non-COVID-19 ICU patients ranged from 2 to 8% [7, 44, 45]. In a retrospective observational cohort study in 12 adult ICUs, including 12.338 medical-surgical critically ill patients, VTE appears to be an apparently infrequent problem, occurring also among patients receiving prophylaxis [44]. Indeed, only 1–2% of patients developed VTE. Across these 12 ICUs, the incidence of definite DVT or PE ranged from 0.1% to 2.6% and 0.2% to 2.4%, respectively. In particular, 252 (2.0%) patients had confirmed VTE (166 DVT events and 122 PE events). Most incident events occurred within 2 weeks of ICU admission. Two thirds of patients required mechanical ventilation and one third required vasopressors or inotropes at some point during their ICU stay. The proportion of patients with VTE who received thromboprophylaxis for 80% or more of their ICU stay was 65.8%. Thus, most VTE events were due to prophylaxis failure rather than failure to provide prophylaxis.
5 Venous Thromboembolism in Hospitalized Patients with COVID-19 Pneumonia
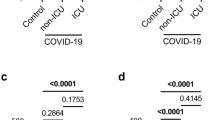
Among hospitalized COVID-19 patients, an increased risk of VTE has been reported despite adequate thromboprophylaxis [7,8,9,10,11, 46]. In particular, higher prevalence of VTE was found compared to non-COVID-19 ICU patients [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. Case series of ICU patients including more than 600 patients reported high rates of VTE (range 20 to 43%), mostly PE [8, 47,48,49]. Data regarding VTE rate outside the ICU are more limited but also suggest a possibly increased rate (range 3% to 6%) [24, 49]. Other studies focused on COVID-19 patients also show a higher rate of DVT (65–69% in ICU patients [50, 51] and 11.9–21% in general ward patients [11, 52, 53]).
In a retrospective study, 11 diagnoses of PE were described in a population of 62 patients with ARDS related to COVID-19 [9]. In all these patients, main pulmonary arteries were involved (Fig. 8.1).
Autopsy studies in small series of patients who have died from COVID-19 have also demonstrated microvascular thrombosis in the lungs [34, 54]. The universality and clinical implications of these observations require further research.
Several factors contribute to the increase in VTE risk in ICU patients. Recognized risk factors for DVT are related to one or more elements of Virchow’s triad: flow stasis, vessel injury, and hypercoagulability. Flow stasis, due to prolonged immobility, mechanical ventilation, use of sedatives, and neuromuscular block, plays a major role in ICU patients [55,56,57]. In addition, in this population vessel injury may be due to catheter insertion in central veins, and hypercoagulability may be induced by sepsis or dehydration [55, 56].
Evaluation for DVT or PE in these patients may be challenging because symptoms of PE overlap with COVID-19, and imaging studies may not be feasible in all cases [9]. The threshold for evaluation or diagnosis of DVT or PE should be low given the high frequency of these events and the presence of additional VTE risk factors in many individuals. In patients with suspected PE due to unexplained hypotension, tachycardia, worsening respiratory status, or other risk factors for thrombosis, computed tomography with pulmonary angiography is the preferred test to confirm or exclude the diagnosis. On the other hand, bilateral complete duplex ultrasound (CDUS) is the suggested test to screen for DVT.
Heparin resistance (requirement for very high doses of heparin to achieve a therapeutic aPTT or anti-factor Xa activity) might be another concern in acutely ill patients with COVID-19. In a French study, 43% of patients reported VTE despite thromboprophylaxis, and thrombotic complications occurred despite prophylactic or therapeutic anticoagulation, respectively, in 70% and 30% of patients [7]. In another series, among 74 patients, VTE was reported in 29 patients [49]. All of them were receiving anticoagulation, both at prophylactic and therapeutic levels. In addition, a series of 15 individuals in the ICU anticoagulated for VTE noted a very high requirement for unfractionated heparin or low molecular weight heparin. In particular, five patients receiving dalteparin had anti-factor Xa peak below expected (<0.6 international units/mL for twice daily dosing or <1 international units/mL for once daily dosing]) [58]. The reason for heparin resistance is not understood; the authors stated that heparin is negatively charged and can interact with a variety of positively charged plasma proteins, some of which behave like acute phase reactants and will compete for heparin binding. Furthermore, the suboptimal efficacy of higher anticoagulation dose could also be explained by the underlying pathophysiological mechanism which explains the presence of thrombotic material in pulmonary circulation [59, 60]. In the context of COVID-19, pulmonary thrombosis may develop via a distinctive mechanism and therefore may not respond adequately to intensified anticoagulation.
Based on these reports, many physicians are advocating the empiric use of therapeutic anticoagulation even in patients who do not have a documented diagnosis of VTE [7, 61, 62]. On the other hand, the current position of the majority of medical societies still recommend using standard prophylactic doses of anticoagulation for hospitalized COVID-19 patients, similar to what is recommended for other acutely ill medical patients [63].
A small randomized trial (HESACOVID) randomly assigned 20 individuals with severe COVID-19 to receive therapeutic-dose anticoagulation (enoxaparin, 1 mg/kg twice daily) or prophylactic-dose anticoagulation (enoxaparin, 40 mg once daily or unfractionated heparin, 5000 units three times daily); adjustments were made for age, weight, and kidney function as appropriate [64]. Half the patients in the prophylactic group received unfractionated heparin and half enoxaparin. Compared with prophylactic dosing, therapeutic dosing led to fewer days on the ventilator and significant reductions in D-dimer levels. However, confidence in the results is hampered by the open-label design and small size of this study. Besides, in our general ICU, a high prevalence of PE was registered among the first 62 patients (19.3% cases) affected by COVID-19-related ARF, admitted from 1 March to 31 March 2020, despite a regular antithrombotic prophylaxis [9]. Thus, a protocol with increased doses of thromboprophylaxis was introduced in our hospital for these patients. Subsequently, we performed a prospective, observational study to assess thrombotic risk in COVID-19 pneumonia patients and to compare populations treated with three different antithrombotic prophylaxis protocols (Fig. 8.2) [10]. Seventy-four patients were enrolled (44 men and 30 women, average age 68.6). Diagnosis of venous thromboembolism was made in 21 cases (28.4%). Forty-seven out of 74 patients (63.5%) received intermediate or therapeutic dose of anticoagulation, while 27 patients (34.5%) received standard antithrombotic prophylaxis. Our analysis showed that an intermediate or therapeutic dose of anticoagulation did not decrease the prevalence of thrombotic events. On the other hand, six patients reported severe hemorrhagic complications (two cases with standard antithrombotic prophylaxis group and four cases with increased antithrombotic dose), with a hemorrhagic shock in three cases. In addition, mortality among patients receiving a higher dose of antithrombotic prophylaxis was three times higher than in subjects treated with standard prophylaxis. More recently, a randomized trial was stopped when the prespecified criterion for futility was met for therapeutic-dose anticoagulation after the inclusion of 1098 critical ill patients with COVID-19 [65]. The authors of this study concluded that in critically ill patients with COVID-19, an initial strategy of therapeutic-dose anticoagulation with heparin did not result in a greater probability of survival to hospital discharge or a greater number of days free of cardiovascular or respiratory organ support than did usual-care pharmacologic thromboprophylaxis.
Antithrombotic prophylaxis in Longhitano study [10]. Antithrombotic prophylaxis: molecules and doses
To date, VTE prophylaxis using at least prophylactic dosing is appropriate in all hospitalized medical, surgical, and obstetric patients with COVID-19, unless there is a contraindication to anticoagulation (e.g., active bleeding or serious bleeding in the prior 24–48 h) [66, 67]. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in hospitalized patients with COVID-19 suggested prophylactic dosing rather than more intensive (intermediate or therapeutic) dosing [68].
Low molecular weight (LMW) heparin is preferred for thromboprophylaxis, but unfractionated heparin can be used if LMW heparin is unavailable or if kidney function is severely impaired. In case of history of heparin-induced thrombocytopenia (HIT), an alternative agent such as fondaparinux may be used. The presence of a prolonged aPTT due to the lupus anticoagulant (LA) phenomenon does not reflect decreased risk of thromboembolic complications (in some individuals, it reflects increased risk) and is not a reason to avoid anticoagulation.
Therapeutic-dose (full-dose) anticoagulation for at least 3 months is always appropriate to treat DVT or PE, and tissue plasminogen activator (tPA) is appropriate for massive PE, unless there is a contraindication.
6 Arterial Thrombosis
Arterial thrombotic events such as stroke, myocardial infarction, and limb ischemia are also increased, but to a lesser extent than venous thrombosis.
The largest study, which included 3334 individuals (829 ICU and 2505 non-ICU), reported stroke in 1.6% and myocardial infarction in 8.9% [69]. Risk factors for arterial thrombosis included older age, male sex, Hispanic ethnicity, history of coronary artery disease, and D-dimer >230 ng/mL on presentation. Arterial thrombotic events were associated with increased mortality.
A report described 20 patients with COVID-19 who developed acute limb ischemia at a single institution over a 3-month period [70]. This represented a significant increase in limb ischemia over the previous year (16%, versus 2% in early 2019). Most were male, and the average age was 75 years. Surgical revascularization procedures were performed in 17, of which 12 (71%) were successful, a lower-than-expected success rate. Individuals who received postoperative heparin did not require reintervention, although the benefits of postoperative heparin did not reach statistical significance.
7 Conclusion
COVID-19 is characterized with a hypercoagulable state associated with acute inflammatory changes and laboratory findings that are distinct from DIC, safe for some patients with very severe disease. The risk for VTE is markedly increased, especially in patients in the ICU, often despite prophylactic-dose anticoagulation. Pulmonary microvascular thrombosis and arterial thrombotic events such as stroke, myocardial infarction, and limb ischemia are also increased, but to a lesser extent than venous thrombosis. Bleeding is less common than thrombosis but can occur.
The threshold for evaluation or diagnosis of DVT or PE should be low given the high frequency of these events and the presence of additional VTE risk factors in many individuals. In patients with suspected PE, computed tomography with pulmonary angiography is the preferred test to confirm or exclude the diagnosis. CDUS is the suggested test to screen for DVT.
All inpatients should receive thromboprophylaxis unless contraindicated. In hospitalized patients with COVID-19, prophylactic dosing rather than more intensive (intermediate or therapeutic) dosing is suggested. Therapeutic dose of anticoagulation is always appropriate to treat DVT or PE, unless contraindicated.
References
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–8. https://doi.org/10.1007/s00134-020-05991-x.
Han H, Yang L, Liu R, Liu F, Wu KL, Li J, Liu XH, Zhu CL. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020;58(7):1116–20. https://doi.org/10.1515/cclm-2020-0188.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. https://doi.org/10.1016/S0140-6736(20)30211-7.
Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094–9. https://doi.org/10.1111/jth.14817.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–8. https://doi.org/10.1016/S0140-6736(20)30937-5.
Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, Merdji H, Clere-Jehl R, Schenck M, Fagot Gandet F, Fafi-Kremer S, Castelain V, Schneider F, Grunebaum L, Anglés-Cano E, Sattler L, Mertes PM, Meziani F. CRICS TRIGGERSEP group (clinical research in intensive care and sepsis trial Group for Global Evaluation and Research in sepsis). High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–98. https://doi.org/10.1007/s00134-020-06062-x.
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. https://doi.org/10.1016/j.thromres.2020.04.013.
Longhitano Y, Racca F, Zanza C, Piccioni A, Audo A, Muncinelli M, Santi R, Kozel D, Geraci C, Taverna M, Bonato V, Cassini F, Franceschi F. Venous thromboembolism in critically ill patients affected by ARDS related to COVID-19 in northern-West Italy. Eur Rev Med Pharmacol Sci. 2020;24(17):9154–60. https://doi.org/10.26355/eurrev_202009_22864.
Longhitano Y, Racca F, Zanza C, Muncinelli M, Guagliano A, Peretti E, Minerba AC, Mari M, Boverio R, Salio M, Chichino G, Franceschi F, Piccioni A, Abenavoli L, Salvini M, Artico M. Venous Thrombo-embolism in hospitalized SARS-CoV-2 patients treated with three different anticoagulation protocols: prospective observational study. Biology (Basel). 2020;9(10):310. https://doi.org/10.3390/biology9100310.
Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, Parra-Virto A, Toledano-Macías M, Toledo-Samaniego N, García-García A, García-Fernández-Bravo I, Ji Z, de-Miguel-Diez J, Álvarez-Sala-Walther LA, Del-Toro-Cervera J, Galeano-Valle F. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23–6. https://doi.org/10.1016/j.thromres.2020.05.018.
Sarzi-Puttini P, Giorgi V, Sirotti S, Marotto D, Ardizzone S, Rizzardini G, Antinori S, Galli M. COVID-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. 2020;38:337–42.
Wu Z. McGoogan JM characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239.
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in new York City: prospective cohort study. BMJ. 2020;369:m1966. https://doi.org/10.1136/bmj.m1966.
Grasselli G, Pesenti A. Cecconi M critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545.
Onder G, Rezza G. Brusaferro S case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775.
Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection a narrative review. Ann Intern Med. 2020;173(5):362. Epub 2020 Jun 3
Lavezzo E, Franchin E, Ciavarella C, Cuomo-Dannenburg G, Barzon L, Del Vecchio C, Rossi L, Manganelli R, Loregian A, Navarin N, Abate D, Sciro M, Merigliano S, De Canale E, Vanuzzo MC, Besutti V, Saluzzo F, Onelia F, Pacenti M, Parisi SG, Carretta G, Donato D, Flor L, Cocchio S, Masi G, Sperduti A, Cattarino L, Salvador R, Nicoletti M, Caldart F, Castelli G, Nieddu E, Labella B, Fava L, Drigo M, Gaythorpe KAM, Brazzale AR, Toppo S, Trevisan M, Baldo V, Donnelly CA, Ferguson NM, Dorigatti I, Crisanti A, Imperial College COVID-19 Response Team. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature. 2020;584(7821):425. Epub 2020 Jun 30
Cohen PA, Hall LE, John JN, Rapoport AB. The early natural history of SARS-CoV-2 infection: clinical observations from an urban, ambulatory COVID-19 clinic. Mayo Clin Proc. 2020;95(6):1124. Epub 2020 Apr 20
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81. https://doi.org/10.1016/S2213-2600(20)30079-5.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. https://doi.org/10.1001/jama.2020.1585.
Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, Daniels CJ. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021;6(1):116–8. https://doi.org/10.1001/jamacardio.2020.4916.
Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH. Global COVID-19 thrombosis collaborative group, endorsed by the ISTH, NATF, ESVM, and the IUA, supported by the ESC working group on pulmonary circulation and right ventricular function. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(23):2950–73. https://doi.org/10.1016/j.jacc.2020.04.031.
Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, Kucher N, Studt JD, Sacco C, Bertuzzi A, Sandri MT, Barco S. Humanitas COVID-19 task force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. https://doi.org/10.1016/j.thromres.2020.04.024.
Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, Burdelski C, de Heer G, Nierhaus A, Frings D, Pfefferle S, Becker H, Bredereke-Wiedling H, de Weerth A, Paschen HR, Sheikhzadeh-Eggers S, Stang A, Schmiedel S, Bokemeyer C, Addo MM, Aepfelbacher M, Püschel K, Kluge S. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;173(4):268–77. https://doi.org/10.7326/M20-2003.
Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, Pesenti A, Peyvandi F, Tripodi A. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738–42. https://doi.org/10.1111/jth.14850.
Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z, Zhang Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost. 2020;18(6):1324–9. https://doi.org/10.1111/jth.14859.
Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145(1):24–33. https://doi.org/10.1111/j.1365-2141.2009.07600.x.
Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39(5):529–39. https://doi.org/10.1007/s00281-017-0629-x.
Shimabukuro-Vornhagen A, Gödel P, Subklewe M, Stemmler HJ, Schlößer HA, Schlaak M, Kochanek M, Böll B, von Bergwelt-Baildon MS. Cytokine release syndrome. J Immunother. Cancer. 2018;6(1):56. https://doi.org/10.1186/s40425-018-0343-9.
Levi M. Pathogenesis and diagnosis of disseminated intravascular coagulation. Int J Lab Hematol. 2018;40(Suppl 1):15–20. https://doi.org/10.1111/ijlh.12830.
Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20(7):389–91. https://doi.org/10.1038/s41577-020-0343-0.
Begbie M, Notley C, Tinlin S, Sawyer L, Lillicrap D. The factor VIII acute phase response requires the participation of NFkappaB and C/EBP. Thromb Haemost. 2000;84(2):216–22.
Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. https://doi.org/10.1016/j.trsl.2020.04.007.
Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, Falco M, Albano G, Menicanti L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18(7):1747–51. https://doi.org/10.1111/jth.14854.
Attia J, Ray JG, Cook DJ, Douketis J, Ginsberg JS, Geerts WH. Deep vein thrombosis and its prevention in critically ill adults. Arch Intern Med. 2001;161(10):1268–79. https://doi.org/10.1001/archinte.161.10.1268.
Saeger W, Genzkow M. Venous thromboses and pulmonary embolisms in post-mortem series: probable causes by correlations of clinical data and basic diseases. Pathol Res Pract. 1994r;190(4):394–9. https://doi.org/10.1016/S0344-0338(11)80413-9.
Bruni-Fitzgerald KR. Venous thromboembolism: an overview. J Vasc Nurs. 2015;33(3):95–9. https://doi.org/10.1016/j.jvn.2015.02.001.
McKelvie PA. Autopsy evidence of pulmonary thromboembolism. Med J Aust. 1994;160(3):127–8.
Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK. American Heart Association Council on cardiopulmonary, critical care, perioperative and resuscitation; American Heart Association Council on peripheral vascular disease; American Heart Association Council on arteriosclerosis, thrombosis and vascular biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123:1788–830.
Sepulveda J, Westblade LF, Whittier S, Satlin MJ, Greendyke WG, Aaron JG, Zucker J, Dietz D, Sobieszczyk M, Choi JJ, Liu D, Russell S, Connelly C, Green DA. Bacteremia and blood culture utilization during COVID-19 surge in new York City. J Clin Microbiol. 2020;58(8):e00875–20. https://doi.org/10.1128/JCM.00875-20.
Koehler P, Cornely OA, Böttiger BW, Dusse F, Eichenauer DA, Fuchs F, Hallek M, Jung N, Klein F, Persigehl T, Rybniker J, Kochanek M, Böll B, Shimabukuro-Vornhagen A. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63(6):528. Epub 2020 May 15
Mo X, Jian W, Su Z, Chen M, Peng H, Peng P, Lei C, Chen R, Zhong N, Li S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;55(6):2001217. https://doi.org/10.1183/13993003.01217-2020.
Patel R, Cook DJ, Meade MO, Griffith LE, Mehta G, Rocker GM, Marshall JC, Hodder R, Martin CM, Heyland DK, Peters S, Muscedere J, Soth M, Campbell N, Guyatt GH. Burden of illness in venous ThromboEmbolism in critical care (BITEC) study investigators; Canadian critical care trials group. Burden of illness in venous thromboembolism in critical care: a multicenter observational study. J Crit Care. 2005;20(4):341–7. https://doi.org/10.1016/j.jcrc.2005.09.014.
Chi G, Gibson CM, Kalayci A, Cohen AT, Hernandez AF, Hull RD, Kahe F, Jafarizade M, Sharfaei S, Liu Y, Harrington RA, Goldhaber SZ. Extended-duration betrixaban versus shorter-duration enoxaparin for venous thromboembolism prophylaxis in critically ill medical patients: an APEX trial substudy. Intensive Care Med. 2019;45(4):477–87. https://doi.org/10.1007/s00134-019-05565-6.
Chi G, Lee JJ, Jamil A, Gunnam V, Najafi H, Memar Montazerin S, Shojaei F, Marszalek J. Venous thromboembolism among hospitalized patients with COVID-19 undergoing Thromboprophylaxis: a systematic review and meta-analysis. J Clin Med. 2020;9(8):2489. https://doi.org/10.3390/jcm9082489.
Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–4.
Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S. Lille ICU Haemostasis COVID-19 group. Pulmonary embolism in patients with COVID-19: awareness of an increased prevalence. Circulation. 2020;142(2):184–6. https://doi.org/10.1161/CIRCULATIONAHA.120.047430.
Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, Bouman CCS, Beenen LFM, Kootte RS, Heijmans J, Smits LP, Bonta PI, van Es N. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1995–2002. https://doi.org/10.1111/jth.14888.
Nahum J, Morichau-Beauchant T, Daviaud F, Echegut P, Fichet J, Maillet JM, Thierry S. Venous thrombosis among critically ill patients with coronavirus disease 2019 (COVID-19). JAMA Netw Open. 2020;3(5):e2010478. https://doi.org/10.1001/jamanetworkopen.2020.10478.
Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, Merouani K. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18(7):1743–6. https://doi.org/10.1111/jth.14869.
Santoliquido A, Porfidia A, Nesci A, De Matteis G, Marrone G, Porceddu E, Cammà G, Giarretta I, Fantoni M, Landi F, Gasbarrini A, Pola R. GEMELLI AGAINST COVID-19 group, D'Alfonso ME, lo Monaco MR. incidence of deep vein thrombosis among non-ICU patients hospitalized for COVID-19 despite pharmacological thromboprophylaxis. J Thromb Haemost. 2020;18(9):2358–63. https://doi.org/10.1111/jth.14992.
Artifoni M, Danic G, Gautier G, Gicquel P, Boutoille D, Raffi F, Néel A, Lecomte R. Systematic assessment of venous thromboembolism in COVID-19 patients receiving thromboprophylaxis: incidence and role of D-dimer as predictive factors. J Thromb Thrombolysis. 2020;50(1):211–6. https://doi.org/10.1007/s11239-020-02146-z.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ. Jonigk D pulmonary vascular Endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120. Epub 2020 May 21
Kaplan D, Casper TC, Elliott CG, Men S, Pendleton RC, Kraiss LW, Weyrich AS, Grissom CK, Zimmerman GA, Rondina MT. VTE incidence and risk factors in patients with severe sepsis and septic shock. Chest. 2015;148(5):1224–30. https://doi.org/10.1378/chest.15-0287.
Geerts W, Cook D, Selby R, Etchells E. Venous thromboembolism and its prevention in critical care. J Crit Care. 2002;17(2):95–104. https://doi.org/10.1053/jcrc.2002.33941.
Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70–8.
White D, MacDonald S, Bull T, Hayman M, de Monteverde-Robb R, Sapsford D, Lavinio A, Varley J, Johnston A, Besser M. Thomas W heparin resistance in COVID-19 patients in the intensive care unit. J Thromb Thrombolysis. 2020;50(2):287.
Marongiu F, Grandone E, Barcellona D. Pulmonary thrombosis in 2019-nCoV pneumonia? J ThrombHaemost. 2020;18:1511–3.
Marongiu F, Mameli A, Grandone E, Barcellona D. Pulmonary thrombosis: a clinical pathological entity distinct from pulmonary embolism? Semin Thromb Hemost. 2019;45(8):778–83. https://doi.org/10.1055/s-0039-1696942.
Porfidia A, Pola R. Venous thromboembolism and heparin use in COVID-19 patients: juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines. J Thromb Thrombolysis. 2020;50:68–71.
Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18(5):1023–6. https://doi.org/10.1111/jth.14810.
Zhai Z, Li C, Chen Y, Gerotziafas G, Zhang Z, Wan J, Liu P, Elalamy I, Wang C. Prevention treatment of VTE associated with COVID-19 infection consensus statement group. Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: a consensus statement before guidelines. Thromb Haemost. 2020;120(6):937–48. https://doi.org/10.1055/s-0040-1710019.
Lemos ACB, do Espírito Santo DA, Salvetti MC, Gilio RN, Agra LB, Pazin-Filho A, Miranda CH. Therapeutic versus prophylactic anticoagulation for severe COVID-19: A randomized phase II clinical trial (HESACOVID). Thromb Res. 2020;196:359. Epub 2020 Sep 21
Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N Engl J Med. 2021;385(9):777.
Akima S, McLintock C, Hunt BJ. ISTH interim guidance to recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18(8):2057.
Moores LK, Tritschler T, Brosnahan S, Carrier M, Collen JF, Doerschug K, Holley AB, Jimenez D, Le Gal G, Rali P. Wells P prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report. Chest. 2020;158(3):1143.
Cuker A, Tseng EK, Nieuwlaat R, et al. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19. Blood Adv. 2021;5:872.
Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020;324(8):799.
Bellosta R, Luzzani L, Natalini G, Pegorer MA, Attisani L, Cossu LG, Ferrandina C, Fossati A, Conti E, Bush RL. Piffaretti G acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020;72:1864.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Racca, F., Zanza, C., Longhitano, Y. (2022). Coagulation Abnormalities in Patients with COVID-19. In: Chiumello, D. (eds) Practical Trends in Anesthesia and Intensive Care 2020-2021. Springer, Cham. https://doi.org/10.1007/978-3-031-14612-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-14612-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-14611-4
Online ISBN: 978-3-031-14612-1
eBook Packages: MedicineMedicine (R0)