Abstract
Blood pressure (BP) is frequently elevated in subjects with diabetes mellitus. The superiority of out-of-office BP over office BP to predict hypertension-induced organ damage and the risk of major cardiovascular complications and mortality, emerging from studies conducted in mixed cohorts of diabetic and nondiabetic subjects, has been substantially confirmed in the specific context of diabetes. Consequently, self-measured home BP and 24-h BP monitoring are generally recommended in the management of diabetic subjects. This review will focus on some specific areas regarding out-of-office BP in diabetic subjects (masked hypertension, white-coat hypertension, 24-h BP and day-night BP changes, self-measured home BP, BP variability, therapeutic implications). Masked hypertension (MH) is defined as untreated subjects with normal office BP associated with abnormally elevated BP at home or during 24-h ambulatory BP monitoring, while white-coat hypertension (WCH) is defined as subjects with elevated office BP associated with normal out-of-office BP. A blunted fall in BP from day to night has been associated with increased progression of diabetic nephropathy, although it remains unclear whether the major trigger for nephropathy is the blunted day-night BP drop or the increased nighttime BP in itself. Similarly, the incidence of major macrovascular complications is more closely related to out-of-office than to office BP. The more appropriate out-of-office BP targets remain undefined. There is the suggestion that home BP should be kept below 125/75 mmHg, as resulting from some longitudinal studies, but there are no randomized controlled studies comparing different home BP targets in diabetics. Similar considerations hold for 24-h ambulatory BP monitoring. Long-term observational studies suggest that 24-h systolic BP levels <120/75 mmHg are associated with significant cardiovascular protection in diabetic subjects. Because of the continuous rise in the incidence of diabetes worldwide and the deleterious impact of hypertension in these subjects, further studies addressing the management of out-of-office BP in diabetes are urgently needed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Diabetes
- Hypertension
- Stroke
- Myocardial infarction
- Congestive heart failure
- Nephropathy
- Albuminuria
- Left ventricular hypertrophy
- Home blood pressure
- Ambulatory blood pressure monitoring
1 Introduction
Several studies have been conducted over the past 30 years to investigate whether the superiority of out-of-office blood pressure (BP) over office BP for improving cardiovascular risk stratification, initially obtained from mixed cohorts of diabetic and nondiabetic subjects [1,2,3,4], is suitably extendible to fully diabetic cohorts. Dealing with diabetes, these studies mostly focused on diabetic microvascular complications at the renal, retinal, and neural level, in addition to macrovascular complications and mortality.
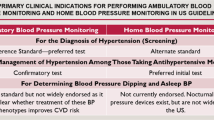
Extensive reviews and commentaries have been published on this issue [5,6,7]. Here, we will provide a clinically oriented overview of clinical studies, which investigated the impact of office versus out-of-office BP, either at home or during 24-h ambulatory BP monitoring, on target organ damage and major cardiovascular events in diabetic subjects. Table 5.1 summarizes the main areas of interest.
2 Masked Hypertension
Initially coined by Pickering in year 2002 [8], the term “masked hypertension” (MH) is defined as untreated subjects with normal BP during the clinical visit associated with abnormally elevated BP out of the clinical setting (i.e., self-measured at home or during 24-h ambulatory BP monitoring). Such definition has been subsequently extended to treated subjects apparently controlled by treatment, using the term “uncontrolled masked hypertension” [9].
The prevalence of MH is generally elevated in diabetic subjects. In the IDACO (International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes) study, the prevalence of MH, defined by 24-h ambulatory BP monitoring in untreated subjects, was 29%, versus 19% among nondiabetics [10]. When the analysis was restricted to treated subjects, the prevalence of MH was 42% among diabetics and 30% among nondiabetics [10]. In other studies conducted with 24-h ambulatory BP monitoring, the prevalence of MH among diabetics was 30% [11] and 47% [12]. In a study from Japan with MH detected using self-measured home BP in diabetic patients, the prevalence of MH was 41% (112 subjects over 270 with normal home BP) [13]. In a recent study, the prevalence of MH was 29% in offspring of patients with diabetes, versus only 3% in offspring of nondiabetic subjects [14].
Which are the predictors of MH? As shown in Table 5.2, several factors including diabetes have been associated with a higher probability of MH.
2.1 Masked Hypertension and Organ Damage
Diabetic subjects with MH generally present greater organ damage when compared with diabetic controls with normal out-of-office blood pressure. In studies from independent laboratories, diabetic subjects with MH showed an increased left ventricular mass at echocardiography [22, 23] and a reduction of active diastolic relaxation [23] when compared with diabetic normotensive controls. A meta-analysis of published studies showed a nonsignificant trend towards a higher left ventricular mass in diabetic subjects with MH [24]. Urinary albumin excretion rate (UAER) has been found increased in diabetic subjects with MH [22] and the progression from microalbuminuria to macroproteinuria was eightfold more frequent in diabetic subjects with MH [13].
Eguchi et al. found an excess risk of silent cerebral infarctions in diabetic subjects with MH [12]. In a study from Sweden, diabetic subjects with MH defined by a normal office BP associated with an isolated raise in nighttime BP (30 out of 100 subjects) showed an increased pulse wave velocity and central blood pressure, reflecting increased large artery stiffness [25].
2.2 Masked Hypertension and Outcome
MH is associated with a markedly increased risk of major cardiovascular events. In a meta-analysis from our group, the risk of major CV events was higher in subjects with MH than in the normotensive subjects regardless of whether MH was defined according to self-measured BP at home (hazard ratio [HR] 2.13; 95% confidence interval [CI], 1.35–3.35; P = 0.001) or 24-h ambulatory BP (HR 2.00; 95% CI: 1.54–2.60; P < 0.001) [26].
The IDACO study specifically investigated the prognostic impact of MH among diabetic subjects. Overall, 229 diabetic and 5486 nondiabetic subjects who underwent 24-h ambulatory BP monitoring were followed for a median of 11 years [10]. After adjustment for potential confounders, the excess risk of total cardiovascular events (Fig. 5.1) in untreated subjects with diabetes and MH tended to be higher than that in diabetic normotensive subjects (HR 1.96; 95% CI 0.97–3.97; P = 0.059), not dissimilar from subjects with stage 1 hypertension (HR, 1.07; 95% CI 0.58–1.98; P = 0.82) and definitely lower than in subjects with stage 2 hypertension (HR 0.53; CI 0.29–0.99; P = 0.048) [10]. The prognostic impact of MH tended to disappear in treated subjects: in this subgroup, the risk of cardiovascular events did not differ between those with MH and the normotensive group (HR 1.13; 95% CI 0.54–2.35; P = 0.75), as well as with the group with stage 1 hypertension (HR, 0.91; 95% CI 0.49–1.69; P = 0.76) and stage 2 hypertension (HR 0.65; 95% CI, 0.35–1.20; P = 0.17) [10].
Incidence of major cardiovascular events in diabetic subjects with normotension, masked hypertension, stage 1 hypertension, and stage 2 hypertension. From Franklin et al. [10], modified
In addition to 24-h ambulatory BP, self-measured home BP may be useful to identify diabetic subjects with MH and increased cardiovascular risk. In the HONEST (Home BP measurement with Olmesartan Naive patients to Establish Standard Target blood pressure) study, which included treated diabetic patients, the incidence of major cardiovascular events was 13.2/1.000 patients/year in the group with masked uncontrolled hypertension, versus 6.1/1.000 patients/year (HR 2.77) in the normotensive subgroup [27].
An interesting finding noted in the PAMELA (Pressioni Arteriose Monitorate E Loro Associazioni) study was the increased risk to develop diabetes in the long term among initially nondiabetic subjects with MH [28]. This finding may be accounted for by the unfavorable metabolic profile of these subjects even in a prediabetic phase [28].
The recent European Hypertension Guidelines provided some important recommendations on the management of subjects with MH [29] and there is no reason why these recommendations should not be extended to diabetic subjects [29]. First, “In masked hypertension, lifestyle changes are recommended to reduce cardiovascular risk, with regular follow-up, including periodic out-of-office BP monitoring” (I C recommendation) [29]. Second, “antihypertensive drug treatment should be considered in masked hypertension to normalize the out-of-office BP, based on the prognostic importance of out-of-office BP elevation” (IIa C recommendation) [29] Third, “antihypertensive drug up-titration should be considered in treated patients whose outof-office BP is not controlled (i.e. masked uncontrolled hypertension), because of the high CV risk of these patients” (IIa C recommendation) [29].
Taken together, these findings strongly suggest the usefulness of 24-h ambulatory BP monitoring in diabetic subjects with normal office BP, particularly in those who are still untreated, with the aim to identify the high-risk subgroup with MH. These subjects should be treated with the aim to normalize out-of-office blood pressure.
Notwithstanding the utility of regular self-measurements of BP at home in the long term, 24-hour ABPM remains strongly recommended at least in the initial diagnostic phase because self-measured BP at home may miss about 25% of subjects with MH [30]. Thus, 24-h ABP monitoring may be particularly recommended when one or more predictors for MH (Table 5.2) in addition to diabetes coexist in the same individual.
3 White-Coat Hypertension
White-coat hypertension (WCH) is defined by an elevated office BP combined with normal BP at home or during 24-h ambulatory BP monitoring [31]. Such definition relies on the belief that WCH is mostly accounted for by the alerting reaction and the transient rise in BP which commonly occur during the clinical visit [32]. WCH mostly applies to untreated subjects because drug treatment could induce a different drop in BP as captured by office and out-of-office BP measurement [1]. Subsequently, the term “white-coat uncontrolled hypertension” has been introduced to define, in treated subjects, a condition with elevated office BP and normal home or 24-hour ABP as opposed to a condition of “sustained uncontrolled hypertension” with elevation of both office and out-of-office BP [29].
The prognostic impact of WCH hypertension has been extensively debated [1, 29]. It is generally believed that such condition should be considered at intermediate cardiovascular risk between normotension (i.e., office plus out-of-office normotension) and sustained hypertension (i.e., elevation in both office and out-of-office BP) [1, 29].
In patients with type 2 diabetes, the prevalence of WCH was around 18% [33]. Some studies addressed the issue of target organ damage in diabetic patients with WCH, but results are limited by the generally low sample sizes of these studies. For example, WCH was not associated with diabetic nephropathy or left ventricular hypertrophy in some studies [34, 35], while other studies found a greater organ damage in diabetic patients with WCH, which included increased arterial stiffness [36], silent cerebral infarcts [37], and diabetic retinopathy and nephropathy [38].
Evidence from a long-term outcome study is limited. In a longitudinal study of 262 patients with type 2 diabetes followed for about 4 years, the incidence of major cardiovascular events was significantly lower among patients with WCH than in those with sustained hypertension [33]. Unfortunately, such study did not include clinically normotensive individuals [33]. As a consequence of such uncertainty, the medical literature hosted some hot debates over the past few years about whether clinically hypertensive patients with diabetes and WCH should receive drug treatment [39] or not [40].
More recently, an important contribution on this topic came from a longitudinal analysis of the IDACO (International Database on Ambulatory Blood Pressure Monitoring) study, in which 653 untreated subjects with WCH and 653 normotensive controls were followed for a median of 10.8 years [41]. Notably, the subjects with WCH were divided into “low” and “high” cardiovascular risk on the basis of established risk factors (diabetes, male sex, smoking, obesity, dyslipidemia). Of course, the prevalence of diabetes was 0% in the subgroup at “low” risk versus 19%–23% in the subgroup at “high” risk [41]. During follow-up, the incidence of new cardiovascular events was significantly higher in the WCH group than in the age-matched normotensive group (HR 2.06, 95% CI 1.10–3.84, P = 0.023) [41]. However, the higher risk in WCH was restricted to the high-risk subjects aged 60 years or more (HR 2.19, 95% CI 1.09–4.37) not to the low-risk subgroup (HR 0.88, 95% CI 0.51–1.53, P = 0.66). The P-value for interaction between the two groups was statistically significant (P = 0.04) [41].
Taken together, all these findings suggest that WCH may not be an innocent phenotype in patients with diabetes, differently from other clinical lower-risk phenotypes.
4 24-Hour Day-Night BP Changes
The superiority of ambulatory BP over office BP for cardiovascular risk stratification in mixed populations of diabetic and nondiabetic subjects is well established [2, 29, 42]. In 1994, we provided the first longitudinal evidence that WCH and a non-dipping pattern were independent predictors of major cardiovascular events after adjustment for several potential confounders including diabetes [3].
Over the subsequent years, a growing number of studies investigated the prognostic impact of 24-hour ambulatory BP in cohorts of diabetic subjects.
4.1 Relationship with Organ Damage
A blunted fall in BP from day to night has been associated with increased urinary albumin excretion in patients with diabetes [43,44,45,46], but it was not clear whether the major determinant of albuminuria was the blunted day-night BP drop or the increased nighttime BP in itself. In a study, a blunted decline in BP from day to night antedated the progressive worsening of renal function in diabetic subjects [47]. The percent decline in glomerular filtration rate (GFR) over a follow-up period of 3.6 years was 21.8% among diabetics, versus 6.6% among nondiabetics (P < 0.001), and it was greater in non-dippers (−15.9%) than in dippers (+1.3%) [47]. Notably, a mean 24-h systolic BP >136 mmHg was an additional independent predictor of GFR decline even after adjustment for non-dipping (P = 0.04) [47].
Ambulatory BP also showed a closer association with echocardiographic left ventricular mass [48,49,50] and carotid atherosclerosis [48] when compared with office BP in diabetic patients. Some authors have also found that a blunted day-night BP fall is associated with diabetic neuropathy independently from pain-related sleep disorders and obstructive sleep apnea [51].
Subjects with diabetes are more prone to develop cognitive decline and dementia and hypertension is believed to increase the likelihood of neurological deficits. However, both low and high 24-h BP values are associated with impaired global cognitive functioning, consistent with a U-curve phenomenon [52].
4.2 Relationship with Outcome
Knudsen et al. first noted that diabetic subjects with a history of macrovascular events had an increased BP at night [53]. The first longitudinal evidence that ambulatory BP predicts outcome in diabetic subjects dates back to year 2000, when Sturrock et al. published a small study of 75 diabetic subjects followed for 4 years [54]. In that study, a non-dipping pattern was associated with an increased risk of mortality [54]. In 2004, a larger study from Japan conducted in initially hospitalized diabetic subjects followed up for about 7 years found that the mean 24-h pulse pressure and mean nighttime systolic BP were independent predictors of major cardiovascular events, independent of the day-night BP changes [55]. These findings have been subsequently confirmed from longitudinal studies conducted in Italy [56] and Japan [57]. In 2009, a longitudinal study of 1178 diabetic patients found that a blunted day-night rhythm of heart rate, in addition to the ambulatory arterial stiffness index (a measure of the dynamic relationship between systolic and diastolic BP reflecting arterial stiffness), were independent predictors of mortality [58].
An important longitudinal study in this area, the Rio de Janeiro type 2 Diabetes Cohort Study (RIO-T2D), was published in 2013 by Salles et al. [59]. In brief, 565 subjects with type 2 diabetes were followed for 5.75 years and 24-h ambulatory BP monitoring was performed at baseline and during follow-up [59]. After controlling other cardiovascular risk factors, 24-h systolic BP and 24-h pulse pressure were stronger predictors of major cardiovascular events than office BP. Notably, achieved BP was more potent than baseline BP on risk stratification [59]. The multivariate spline analysis showed that the risk of events in these subjects increased when 24-h ambulatory BP levels exceeded 120/75 mmHg, which corresponds to 130/80 mmHg for daytime BP and 110/65 mmHg for nighttime BP [59]. Although not being a randomized trial between more intensive and less intensive ambulatory BP targets, the study by Salles generates the hypothesis that lower ambulatory BP goals may be beneficial in the management of patients with diabetes.
4.3 Impact on Chronotherapy
In a prospective, randomized study in 448 hypertensive patients with type 2 diabetes followed for 5.4 years, Hermida et al. found that administration of at least one antihypertensive drug at bedtime was associated with a significant reduction of a composite outcome of major cardiovascular events (Fig. 5.2) as compared with administration of all antihypertensive drugs in the morning [60]. Whereas daytime BP at follow-up did not differ between the two groups (127/71 mmHg in both), asleep BP was lower in the group with at least one antihypertensive drug at bedtime (115/60 vs 122/64 mmHg) [60]. In a commentary, Friedman and Banrji noted that these results partly disagree with the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, which did not find a different incidence of major cardiovascular events between the groups randomized to a more intensive (<120 mmHg) or less intensive systolic BP goals (<140 mmHg) [61]. In a subsequent study conducted in a smaller diabetic cohort, bedtime administration of antihypertensive drugs was associated with lower nighttime and 24-h BP, increased natriuresis, and lower levels of C-reactive protein, the latter suggesting a reduction in low-grade inflammation [62].
Incidence of major cardiovascular events in hypertensive subjects randomized to receive all antihypertensive drugs at awakening, or at least one drug at bedtime. From Hermida et al. [60], modified
Taken together, these data suggest the potential usefulness of bedtime administration of antihypertensive drugs in diabetic patients, particularly in those with elevated nighttime BP values. A caveat to consider is that the sleep disturbances possibly caused by cuff inflations during nocturnal BP monitoring could trigger a monitoring-related raise in nighttime BP, which might invalidate its prognostic impact [63]. Further, randomized studies are urgently needed to provide a definite answer to this question.
5 Self-Measured Home Blood Pressure
Several longitudinal studies conducted in mixed cohorts of diabetic and nondiabetic subjects clearly demonstrated that BP self-measured by patients at home (home BP) is superior to office BP for the prediction of major cardiovascular events and mortality [64,65,66,67,68].
Some cross-sectional and longitudinal studies investigated the applicability of these findings to diabetic subjects. Cross-sectional studies found an association of home BP with diabetic nephropathy, retinopathy, and history of major cardiovascular complications [69, 70]. In a longitudinal study, the progression of diabetic nephropathy from normo-albuminuria to micro- and macroproteinuria was more frequent among subjects with home BP in the range of 120–129 mmHg than among those with home BP <120 mmHg (OR 2.72, P = 0.035) even after adjustment for other potential determinants of proteinuria. Of note, the risk of coronary events did not increase (i.e., there was no “J-curve”) among the subjects with home BP <120 mmHg [71].
In the Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) trial, 979 patients with impaired fasting glucose (IFG) or type 2 diabetes were followed for a median of 5.45 years. At entry, home systolic BP was a significant predictor of major cardiovascular events in the total population of subjects with IFG or diabetes (HR 1.68, 95% CI 1.26–2.26, P = 0.0005] [72]. Home BP recorded during follow-up was a significant predictor of cardiovascular events even after adjustment for clinic BP, which did not achieve significance in the multivariate analysis. Since only 26 events occurred in the diabetic subgroup, this study could not assess the prognostic impact of home BP in these subjects. Notably, home BP values <125/75 mmHg were associated with a 47% (systolic BP) and 55% (diastolic BP) lower risk of cardiovascular events when compared with subjects with higher home BP [72].
The Japan Morning Surge Home Blood Pressure (J-HOP) study provided important data on the prognostic value of home BP in diabetic subjects [73]. In that study, 1057 subjects with diabetes and 3251 without diabetes were followed for a median of 4.0 years. After adjustment for confounders, home systolic BP ≥135 mmHg was associated with increased risk of cardiovascular events both in the diabetic (HR 2.45, P = 0.017) and nondiabetic (HR 1.79, P = 0.024) cohorts. Conversely, home systolic BP ≥125 mmHg predicted an increased risk of cardiovascular events only in the diabetic cohort (HR 4.35, P = 0.045), not in the other cohort [73]. Again, although it was not a randomized study between different treatment goals, the J-HOP study generates the hypothesis that home systolic BP should be kept below 125 mmHg for an optimal protection from major cardiovascular events.
As discussed above, home BP may be useful to identify diabetic subjects with white-coat or masked hypertension, as shown in the HONEST study [27]. An interesting point to be kept present when interpreting the data is represented by the seasonal variations in home BP. A study from Japan conducted in patients with type 2 diabetes showed that home BP is considerably lower in August (about 126/70 mmHg) than in January (about 140/77 mmHg) [74].
Diabetic patients should be instructed to share the results of home BP measurements with their doctors. A study specifically conducted in 566 subjects with diabetes clearly showed that the patient-clinician communication of results of home BP monitoring is an independent factor associated with a better BP control [75].
6 Blood Pressure Variability
BP variability is a complex phenomenon which results from the interaction between extrinsic (physical activity, psychological stress, temperature, etc.) and intrinsic (neural and humoral mechanisms) factors [7]. BP variability can be detected beat-by-beat using intra-arterial BP recoding, or over longer time windows using 24-h noninvasive BP monitoring (BP variability during the day, night, or over 24 h) or home BP measurements (day-to-day and seasonal variability). When using 24-h ambulatory BP monitoring, BP variability can be estimated through the standard deviation of daytime, nighttime, or 24-h BP, the latter being more properly an expression of the day-night dipping pattern (see above). Unfortunately, the standard deviation of daytime and nighttime BP may not be sensitive enough to short or very short changes in BP that may occur during day or night.
BP variability during the day, night, and over 24 h tends to be increased in hypertensive subjects with diabetes as compared with subjects without diabetes [76, 77]. In subjects at risk of diabetes due to overweight or obesity, a visit-to-visit variability of systolic BP of at least 10 mmHg predicted an increased likelihood to develop diabetes over time [78]. A study in diabetic subjects showed that day-to-day home BP variability is more closely associated with daytime variability than with nighttime variability from 24-h ambulatory BP monitoring [79].
Several factors including increased arterial stiffness, autonomic dysfunction, and elevated adrenergic activity could explain the increased BP variability in subjects with diabetes [76, 80, 81]. An elevated variability of systolic BP during the night and 24-hour BP has also been linked with coronary artery disease [82].
The prognostic impact of blunted day-night BP variability has been discussed above. Coming to the day-to-day BP variability, there is large evidence that such variability is associated with a greater organ damage and a higher risk of major cardiovascular events [7]. Increased home BP variability predicted a higher risk of development and progression of diabetic nephropathy [83, 84]. In subjects with type 1 diabetes, the year-to-year BP variability was linked with a higher risk of subsequent diabetic nephropathy, but not retinopathy [85]. In a study from Japan conducted in subjects with type 2 diabetes, the standard deviation and the coefficient of variation of home BP measured in the morning were significantly associated with the risk of progression from micro- to macroalbuminuria over 2 years even after adjustment for important confounders including sex, duration of diabetes, obesity, glycosylated hemoglobin, serum creatinine, and antihypertensive treatment [86]. These data have been confirmed in a large study from the United States [87]. In another longitudinal study, day-to-day variability was associated with greater arterial stiffness, reflected by pulse wave velocity and urinary albumin excretion, in a large cohort of subjects with type 2 diabetes [88].
The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) study, conducted in 8811 subjects with diabetes and no previous cardiovascular events, strongly supported the prognostic value of visit-to-visit BP variability [89]. In this study, the association between systolic BP variability and macrovascular and microvascular events was continuous even after adjustment for mean systolic BP and other confounding factors. The HRs in the upper tenth versus the lowest tenth were 1.54 (0.99–2.39) for macrovascular events and 1.84 (1.19–2.84) for microvascular events [89].
7 Blood Pressure Targets
The 2018 ESC/ESH Guidelines [29] and the 2019 ESC Guidelines on diabetes, prediabetes, and cardiovascular diseases [90] recommended that in subjects with diabetes:
-
(a)
Antihypertensive treatment is needed when office BP is ≥140/90 mmHg (I A recommendation).
-
(b)
Systolic BP should be targeted to 130 mmHg and <130 mmHg if tolerated, but not <120 mmHg (I A recommendation).
-
(c)
In people aged ≥65 years, systolic BP should be targeted to 130–139 mmHg (I A recommendation).
-
(d)
Diastolic BP should be targeted to <80 mmHg, but not <70 mmHg (I C recommendation) [29, 90].
Conversely, the 2017 Guidelines issued by the American College of Cardiology, the American Heart Association, and other scientific societies recommend starting antihypertensive drug treatment when office BP is 130/80 mmHg or higher, with the aim to reduce it to <130/80 mmHg [91].
The Standards of Medical Care in Diabetes-2019 issued by the American Diabetes Association suggest that BP should be targeted <130/80 mmHg in diabetic hypertensive subjects at high cardiovascular risk (history of cardiovascular disease, or 10-year atherosclerotic cardiovascular disease risk >15%) and to <140/90 mmHg in those at lower risk (no history of cardiovascular disease, or 10-year atherosclerotic cardiovascular disease risk <15%) [92].
While office BP targets in subjects with diabetes appear to be well established, out-of-office BP targets remain undefined. Home BP should be kept below 125/75 mmHg according to the HOMED-BP study [72]. Also the J-HOP study [73] and the HONEST study [27] suggested that home systolic BP <125 mmHg is an appropriate target. Thus, a home BP target <125/75 mmHg sounds like a reasonable proposal.
As for ambulatory BP monitoring, the RIO-T2D study concluded that achieved 24-h systolic BP values <120/75 mmHg are associated with significant cardiovascular protection [59].
Despite the reported association between a blunted day-night BP decline and organ damage (see above), uncertainty remains whether the higher nocturnal BP in itself or the blunted day-night BP drop is the main determinant of outcome [47, 55]. Similar caveats may apply to long-term (i.e., visit-to-visit) BP variability, although the ADVANCE study provided clear evidence that the relation between visit-to-visit systolic BP variability and outcome is continuous and independent from the mean BP [89].
8 Conclusions
The above data strongly suggest that, owing to the continuous rise in the incidence of diabetes worldwide, the deleterious impact of elevated BP in these subjects, and the superiority of out-of-office versus office BP for cardiovascular risk stratification in diabetic subjects, further studies with home BP and 24-h ambulatory BP in diabetes are urgently needed. In the meantime, the use of both techniques of out-of-office BP measurements should be encouraged in the clinical practice. This review provides some out-of-office BP goals based on available outcome-based studies.
References
Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure: evidence and limits. Circ Res. 2015;116:1034–45.
Verdecchia P. Prognostic value of ambulatory blood pressure : current evidence and clinical implications. Hypertension. 2000;35:844–51.
Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24(6):793–801.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Bursztyn M, Ben-Dov IZ. Diabetes mellitus and 24-hour ambulatory blood pressure monitoring. Hypertension. 2009;53:110–1.
Parati G, Bilo G. Should 24-h ambulatory blood pressure monitoring be done in every patient with diabetes? Diabetes Care. 2009;32(Suppl 2):S298–304.
Parati G, Ochoa JE, Salvi P, Lombardi C, Bilo G. Prognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetes. Diabetes Care. 2013;36(Suppl 2):S312–24.
Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40(6):795–6.
Franklin SS, O’Brien E, Staessen JA. Masked hypertension: understanding its complexity. Eur Heart J. 2017;38:1112–8.
Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, et al. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61(5):964–71.
Leitao CB, Canani LH, Kramer CK, Moehlecke M, Pinto LC, Ricardo ED, et al. Blood pressure means rather than nocturnal dipping pattern are related to complications in Type 2 diabetic patients. Diabet Med. 2008;25(3):308–13.
Eguchi K, Ishikawa J, Hoshide S, Pickering TG, Shimada K, Kario K. Masked hypertension in diabetes mellitus: a potential risk. J Clin Hypertens (Greenwich). 2007;9(8):601–7.
Ushigome E, Oyabu C, Tanaka T, Hasegawa G, Ohnishi M, Tsunoda S, et al. Impact of masked hypertension on diabetic nephropathy in patients with type II diabetes: a KAMOGAWA-HBP study. J Am Soc Hypertens. 2018;12(5):364–71.
Mahfouz RA, Gouda M, Alawady W. Determinants and impact of masked hypertension in offspring of patients with diabetes: relation with coronary flow and cardiac function. Blood Press. 2019;28(1):57–63.
Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, determinants, and clinical significance of masked hypertension in a population-based sample of African Americans: the Jackson heart study. Am J Hypertens. 2015;28(7):900–8.
Trudel X, Brisson C, Milot A. Job strain and masked hypertension. Psychosom Med. 2010;72(8):786–93.
Seki M, Inoue R, Ohkubo T, Kikuya M, Hara A, Metoki H, et al. Association of environmental tobacco smoke exposure with elevated home blood pressure in Japanese women: the Ohasama study. J Hypertens. 2010;28(9):1814–20.
Hanninen MR, Niiranen TJ, Puukka PJ, Jula AM. Metabolic risk factors and masked hypertension in the general population: the Finn-Home study. J Hum Hypertens. 2014;28(7):421–6.
Bangash F, Agarwal R. Masked hypertension and white-coat hypertension in chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol. 2009;4(3):656–64.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Sleep-time blood pressure and the prognostic value of isolated-office and masked hypertension. Am J Hypertens. 2012;25(3):297–305.
Tabara Y, Okada Y, Uetani E, Nagai T, Igase M, Kido T, et al. Postprandial hypotension as a risk marker for asymptomatic lacunar infarction. J Hypertens. 2014;32(5):1084–90; discussion 90.
Leitao CB, Canani LH, Kramer CK, Boza JC, Pinotti AF, Gross JL. Masked hypertension, urinary albumin excretion rate, and echocardiographic parameters in putatively normotensive type 2 diabetic patients. Diabetes Care. 2007;30(5):1255–60.
Marchesi C, Maresca AM, Solbiati F, Franzetti I, Laurita E, Nicolini E, et al. Masked hypertension in type 2 diabetes mellitus. Relationship with left-ventricular structure and function. Am J Hypertens. 2007;20(10):1079–84.
Pierdomenico SD, Cuccurullo F. Ambulatory blood pressure monitoring in type 2 diabetes and metabolic syndrome: a review. Blood Press Monit. 2010;15(1):1–7.
Wijkman M, Lanne T, Engvall J, Lindstrom T, Ostgren CJ, Nystrom FH. Masked nocturnal hypertension–a novel marker of risk in type 2 diabetes. Diabetologia. 2009;52(7):1258–64.
Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23(9):941–8.
Kushiro T, Kario K, Saito I, Teramukai S, Sato Y, Okuda Y, et al. Increased cardiovascular risk of treated white coat and masked hypertension in patients with diabetes and chronic kidney disease: the HONEST Study. Hypertens Res. 2017;40(1):87–95.
Mancia G, Bombelli M, Facchetti R, Madotto F, Quarti-Trevano F, Grassi G, et al. Increased long-term risk of new-onset diabetes mellitus in white-coat and masked hypertension. J Hypertens. 2009;27(8):1672–8.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Zhang L, Li Y, Wei FF, Thijs L, Kang YY, Wang S, et al. Strategies for classifying patients based on office, home, and ambulatory blood pressure measurement. Hypertension. 2015;65(6):1258–65.
Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988;259(2):225–8.
Mancia G, Bertinieri G, Grassi G, Parati G, Pomidossi G, Ferrari A, et al. Effects of blood-pressure measurement by the doctor on patient’s blood pressure and heart rate. Lancet. 1983;2(8352):695–8.
Eguchi K, Hoshide S, Ishikawa J, Ishikawa S, Pickering TG, Gerin W, et al. Cardiovascular prognosis of sustained and white-coat hypertension in patients with type 2 diabetes mellitus. Blood Press Monit. 2008;13(1):15–20.
Nielsen FS, Gaede P, Vedel P, Pedersen O, Parving HH. White coat hypertension in NIDDM patients with and without incipient and overt diabetic nephropathy. Diabetes Care. 1997;20(5):859–63.
Ng CM, Yiu SF, Choi KL, Choi CH, Ng YW, Tiu SC. Prevalence and significance of white-coat hypertension and masked hypertension in type 2 diabetics. Hong Kong Med J. 2008;14(6):437–43.
Ribeiro L, Gama G, Santos A, Asmar R, Martins L, Polonia J. Arterial distensibility in subjects with white-coat hypertension with and without diabetes or dyslipidaemia: comparison with normotensives and sustained hypertensives. Blood Press Monit. 2000;5(1):11–7.
Eguchi K, Kario K, Shimada K. Greater impact of coexistence of hypertension and diabetes on silent cerebral infarcts. Stroke. 2003;34(10):2471–4.
Kramer CK, Leitao CB, Canani LH, Gross JL. Impact of white-coat hypertension on microvascular complications in type 2 diabetes. Diabetes Care. 2008;31(12):2233–7.
Mancia G, Sega R, Bombelli M, Quarti-Trevano F, Facchetti R, Grassi G. Should white-coat hypertension in diabetes be treated? Pro. Diabetes Care. 2009;32(Suppl 2):S305–9.
Bursztyn M, Ben-Dov IZ. White-coat hypertension should not be treated in subjects with diabetes. Diabetes Care. 2009;32(suppl_2):S310–3.
Franklin SS, Thijs L, Asayama K, Li Y, Hansen TW, Boggia J, et al. The cardiovascular risk of white-coat hypertension. J Am Coll Cardiol. 2016;68(19):2033–43.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32(7):1359–66.
Fogari R, Zoppi A, Malamani GD, Lazzari P, Albonico B, Corradi L. Urinary albumin excretion and nocturnal blood pressure in hypertensive patients with type II diabetes mellitus. Am J Hypertens. 1994;7(9 Pt 1):808–13.
Pinkney JH, Denver AE, Mohamed-Ali V, Foster C, Yudkin JS. Insulin resistance in non-insulin-dependent diabetes mellitus is associated with microalbuminuria independently of ambulatory blood pressure. J Diabetes Complications. 1995;9(4):230–3.
Equiluz-Bruck S, Schnack C, Kopp HP, Schernthaner G. Nondipping of nocturnal blood pressure is related to urinary albumin excretion rate in patients with type 2 diabetes mellitus. Am J Hypertens. 1996;9(11):1139–43.
Mitchell TH, Nolan B, Henry M, Cronin C, Baker H, Greely G. Microalbuminuria in patients with non-insulin-dependent diabetes mellitus relates to nocturnal systolic blood pressure. Am J Med. 1997;102(6):531–5.
Davidson MB, Hix JK, Vidt DG, Brotman DJ. Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch Intern Med. 2006;166(8):846–52.
Li S, Wang X, Zhao L, Chen M, Long J, Cheng W, et al. The characteristics of 24-hour ambulatory blood pressure monitoring and its relationship with cardiovascular target organ damage in Chinese Han patients with concomitant type 2 diabetes and hypertension. Blood Press Monit. 2019;24(4):167–73.
Devereux RB, Roman MJ, Paranicas M, O'Grady MJ, Lee ET, Welty TK, et al. Impact of diabetes on cardiac structure and function: the strong heart study. Circulation. 2000;101(19):2271–6.
Palmieri V, Bella JN, Arnett DK, Liu JE, Oberman A, Schuck MY, et al. Effect of type 2 diabetes mellitus on left ventricular geometry and systolic function in hypertensive subjects: Hypertension Genetic Epidemiology Network (HyperGEN) study. Circulation. 2001;103(1):102–7.
D'Amato C, Morganti R, Di Gennaro F, Greco C, Marfia GA, Spallone V. A novel association between nondipping and painful diabetic polyneuropathy. Diabetes Care. 2014;37(9):2640–2.
Spauwen PJ, van Boxtel MP, Verhey FR, Kohler S, Sep SJ, Koster A, et al. Both low and high 24-hour diastolic blood pressure are associated with worse cognitive performance in type 2 diabetes: the Maastricht study. Diabetes Care. 2015;38(8):1473–80.
Knudsen ST, Poulsen PL, Hansen KW, Ebbehoj E, Bek T, Mogensen CE. Pulse pressure and diurnal blood pressure variation: association with micro- and macrovascular complications in type 2 diabetes. Am J Hypertens. 2002;15(3):244–50.
Sturrock ND, George E, Pound N, Stevenson J, Peck GM, Sowter H. Non-dipping circadian blood pressure and renal impairment are associated with increased mortality in diabetes mellitus. Diabet Med. 2000;17(5):360–4.
Nakano S, Ito T, Furuya K, Tsuda S, Konishi K, Nishizawa M, et al. Ambulatory blood pressure level rather than dipper/nondipper status predicts vascular events in type 2 diabetic subjects. Hypertens Res. 2004;27(9):647–56.
Mannucci E, Lambertucci L, Monami M, Fedeli A, Chiasserini V, Marchionni N, et al. Pulse pressure and mortality in hypertensive type 2 diabetic patients. A cohort study. Diabetes Metab Res Rev. 2006;22(3):172–5.
Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz JE, et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens. 2008;21(4):443–50.
Palmas W, Pickering TG, Teresi J, Schwartz JE, Moran A, Weinstock RS, et al. Ambulatory blood pressure monitoring and all-cause mortality in elderly people with diabetes mellitus. Hypertension. 2009;53(2):120–7.
Salles GF, Leite NC, Pereira BB, Nascimento EM, Cardoso CR. Prognostic impact of clinic and ambulatory blood pressure components in high-risk type 2 diabetic patients: the Rio de Janeiro Type 2 Diabetes Cohort Study. J Hypertens. 2013;31(11):2176–86.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Sleep-time blood pressure as a therapeutic target for cardiovascular risk reduction in type 2 diabetes. Am J Hypertens. 2012;25(3):325–34.
Friedman EA, Banerji MA. Chronobiology impacts response to antihypertensive drug regimen in type 2 diabetes. Diabetes Care. 2011;34(6):1438–9.
Rossen NB, Knudsen ST, Fleischer J, Hvas AM, Ebbehoj E, Poulsen PL, et al. Targeting nocturnal hypertension in type 2 diabetes mellitus. Hypertension. 2014;64(5):1080–7.
Verdecchia P, Angeli F, Borgioni C, Gattobigio R, Reboldi G. Ambulatory blood pressure and cardiovascular outcome in relation to perceived sleep deprivation. Hypertension. 2007;49(4):777–83.
Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291(11):1342–9.
Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, et al. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST study. J Am Coll Cardiol. 2016;67(13):1519–27.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16(7):971–5.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111(14):1777–83.
Yasui D, Asayama K, Ohkubo T, Kikuya M, Kanno A, Hara A, et al. Stroke risk in treated hypertension based on home blood pressure: the Ohasama study. Am J Hypertens. 2010;23(5):508–14.
Kamoi K, Miyakoshi M, Soda S, Kaneko S, Nakagawa O. Usefulness of home blood pressure measurement in the morning in type 2 diabetic patients. Diabetes Care. 2002;25(12):2218–23.
Kamoi K, Tanaka M, Ikarashi T, Miyakoshi M. Effect of the 2004 Mid-Niigata Prefecture earthquake on home blood pressure measurement in the morning in type 2 diabetic patients. Clin Exp Hypertens. 2006;28(8):719–29.
Ushigome E, Hamaguchi M, Matsumoto S, Oyabu C, Omoto A, Tanaka T, et al. Optimal home SBP targets for preventing the progression of diabetic nephropathy in patients with type 2 diabetes mellitus. J Hypertens. 2015;33(9):1853–9; discussion 9.
Noguchi Y, Asayama K, Staessen JA, Inaba M, Ohkubo T, Hosaka M, et al. Predictive power of home blood pressure and clinic blood pressure in hypertensive patients with impaired glucose metabolism and diabetes. J Hypertens. 2013;31(8):1593–602.
Eguchi K, Hoshide S, Kario K. Target home morning SBP be below 125 mmHg in type 2 diabetes patients. J Hypertens. 2018;36(6):1284–90.
Ushigome E, Kitagawa N, Kitae A, Kimura T, Iwai K, Oyabu C, et al. Seasonal variation in home blood pressure and its relationship with room temperature in patients with type 2 diabetes. Diab Vasc Dis Res. 2020;17(1):1479164119883986.
Naik AD, Kallen MA, Walder A, Street RL Jr. Improving hypertension control in diabetes mellitus: the effects of collaborative and proactive health communication. Circulation. 2008;117(11):1361–8.
Ozawa M, Tamura K, Iwatsubo K, Matsushita K, Sakai M, Tsurumi-Ikeya Y, et al. Ambulatory blood pressure variability is increased in diabetic hypertensives. Clin Exp Hypertens. 2008;30(3):213–24.
Zhou TL, Kroon AA, Reesink KD, Schram MT, Koster A, Schaper NC, et al. Blood pressure variability in individuals with and without (pre)diabetes: The Maastricht Study. J Hypertens. 2018;36(2):259–67.
Joshipura KJ, Munoz-Torres FJ, Campos M, Rivera-Diaz AD, Zevallos JC. Association between within-visit systolic blood pressure variability and development of pre-diabetes and diabetes among overweight/obese individuals. J Hum Hypertens. 2017;32(1):26–33.
Iuchi H, Sakamoto M, Matsutani D, Suzuki H, Kayama Y, Takeda N, et al. Association between day-by-day and ambulatory blood pressure variability in type 2 diabetes patients. Blood Press Monit. 2017;22(6):351–4.
Frattola A, Parati G, Gamba P, Paleari F, Mauri G, Di Rienzo M, et al. Time and frequency domain estimates of spontaneous baroreflex sensitivity provide early detection of autonomic dysfunction in diabetes mellitus. Diabetologia. 1997;40(12):1470–5.
Ruiz J, Monbaron D, Parati G, Perret S, Haesler E, Danzeisen C, et al. Diabetic neuropathy is a more important determinant of baroreflex sensitivity than carotid elasticity in type 2 diabetes. Hypertension. 2005;46(1):162–7.
Tamura K, Tsurumi Y, Sakai M, Tanaka Y, Okano Y, Yamauchi J, et al. A possible relationship of nocturnal blood pressure variability with coronary artery disease in diabetic nephropathy. Clin Exp Hypertens. 2007;29(1):31–42.
Tamura K, Azushima K, Umemura S. Day-by-day home-measured blood pressure variability: another important factor in hypertension with diabetic nephropathy? Hypertens Res. 2011;34(12):1249–50.
Ushigome E, Fukui M, Hamaguchi M, Senmaru T, Sakabe K, Tanaka M, et al. The coefficient variation of home blood pressure is a novel factor associated with macroalbuminuria in type 2 diabetes mellitus. Hypertens Res. 2011;34(12):1271–5.
Kilpatrick ES, Rigby AS, Atkin SL. The role of blood pressure variability in the development of nephropathy in type 1 diabetes. Diabetes Care. 2010;33(11):2442–7.
Ushigome E, Matsumoto S, Oyabu C, Kitagawa N, Tanaka T, Hasegawa G, et al. Prognostic significance of day-by-day variability of home blood pressure on progression to macroalbuminuria in patients with diabetes. J Hypertens. 2018;36(5):1068–75.
Sohn MW, Epstein N, Huang ES, Huo Z, Emanuele N, Stukenborg G, et al. Visit-to-visit systolic blood pressure variability and microvascular complications among patients with diabetes. J Diabetes Complications. 2017;31(1):195–201.
Okada H, Fukui M, Tanaka M, Inada S, Mineoka Y, Nakanishi N, et al. Visit-to-visit variability in systolic blood pressure is correlated with diabetic nephropathy and atherosclerosis in patients with type 2 diabetes. Atherosclerosis. 2012;220(1):155–9.
Hata J, Arima H, Rothwell PM, Woodward M, Zoungas S, Anderson C, et al. Effects of visit-to-visit variability in systolic blood pressure on macrovascular and microvascular complications in patients with type 2 diabetes mellitus: the ADVANCE trial. Circulation. 2013;128(12):1325–34.
Wheeler DC, Valensi P, Sousa-Uva M, Seferović PM, Sattar N, Roffi M, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115.
American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S103–23.
Acknowledgment
This study was supported in part by the nonprofit Fondazione Umbra Cuore e Ipertensione-ONLUS, Perugia, Italy.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Verdecchia, P., Reboldi, G., Angeli, F. (2023). Office/Out-of-Office Blood Pressure Measurements. In: Berbari, A.E., Mancia, G. (eds) Blood Pressure Disorders in Diabetes Mellitus. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-031-13009-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-13009-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-13008-3
Online ISBN: 978-3-031-13009-0
eBook Packages: MedicineMedicine (R0)