Abstract
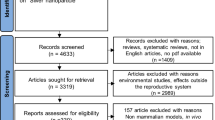
Nanotechnological tools have been greatly exploited in all possible fields. However, advancement of nanotechnology has raised concern about their adverse effects on human and environment. These deleterious effects cannot be ignored and need to be explored due to safety purpose. Several recent studies have demonstrated possible health hazard of nanoparticles on organism. Moreover, studies showed that toxicity of metallic nanomaterial could also lead to reproductive toxicity. Various deleterious effects have demonstrated decreased sperm motility, increased abnormal spermatozoa, altered sperm count, and altered sperm morphology. Morphological and ultrastructural changes also have been reported due to the accumulation of these nanomaterials in reproductive organs. Nonetheless, studies also suggest crossing of metallic nanoparticles through blood testes barrier and generation of oxidative stress which plays major role in reproductive toxicity. In the present study, we have incorporated updated information by gathering all available literature about various metallic nanomaterials and risk related to reproductive system.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Histopathological changes
- Reactive oxygen species
- Teratogenicity
- Fertility
- Iron oxide nanoparticles
- Gold nanoparticles
7.1 Introduction
Nanotechnology deals with the particles of size less than 100 nanometers (nm) at least in one dimension. Nanotechnology includes synthesis, exploitation, and handling of nanomaterials (NMs) (Hoyt and Mason 2008) due to their unique features. Nanoparticles are being employed in various fields such as medicine, cosmetics, and industrial purposes (Gaharwar et al. 2019).
However, the huge concern that has arisen is because of the extraordinary physiological properties of the nanomaterials which resulted in their increased used in different applications. Nanoparticles are highly reactive as they possess high surface area-to-volume ratio which ultimately results in adverse effects in organism (Oberdorster et al. 2005). There are several means through which nanoparticles may come in contact with human lives and ecosystems such as water, food products, commercial applications, and medicinal uses (Gaharwar et al. 2019). Medicinal and therapeutic uses of nanomaterials lead to their distribution in different organs through blood circulation. Apart from these, during production, recycling, and disposal, nanoparticles may get released into the environment (Roy et al. 2014).
In addition, nanomaterials have been reported to induce reproductive toxicity (Liu et al. 2007; Srám et al. 1999; Yokota et al. 2013). Reproduction and fertility are related to the species sustainability. Reproductive toxicity has drawn the public attention toward engineered nanoparticles and their adverse effects on animals (Hougaard et al. 2015). Metallic nanomaterial is known for the generation of oxidative stress and inflammation to which reproductive organs are sensitive (Azenabor et al. 2015; Das et al. 2016; Walczak-Jedrzejowska et al. 2013). Increased oxidative stress has been recognized as major source of damage in reproductive organs and resulted in infertility due to reduced spermatogenesis (Bisht et al. 2017; Han et al. 2016). Previous studies have shown that various metallic nanoparticles, such as silver nanoparticles (AgNPs) (Ema et al. 2016 & Opris et al. 2019), titanium dioxide nanoparticles (TiO2NPs) (Meena et al. 2014), and cerium oxide nanoparticles (CeNPs) (Qin et al. 2019) induce oxidative stress in male reproductive organs. CeO2 NPs treatment reduced synthesis of testosterone hormone and impaired maturation of sperm (Qin et al. 2019). CeO2 NPs were also reported to be found in the testicles and epididymis in rats after inhalation, but the reproductive outcomes associated with CeO2 NPs accumulation in the testis were not assessed (Geraets et al. 2012). Now, infertility has become a major issue among young individuals; however, possible reason behind this is unclear till date (Lan and Yang 2012). Moreover, exposure to engineered nanomaterial could pose threat as their release in the environment increased the availability. Nanomaterials have been reported to cross blood testes barriers too which raises the issue about their safety (Gaharwar et al. 2019; Shittu et al. 2018). Therefore, reproductive toxicity has raised concern among researchers to demonstrate the potential adverse effects of metallic nanomaterials (Campagnolo et al. 2012; El-Sayed et al. 2015; Hougaard et al. 2015; Kadar et al. 2013). However, little information is still available about them, especially in mammals (Ema et al. 2010), and mechanisms of toxicity in reproductive system is yet to be understood. In this study, we have incorporated probable toxicity of metallic nanoparticles along with their possible mechanism.
7.2 Manganese Nanoparticles (Mn NPs)
Manganese (Mn) is naturally present in many foods and is an essential trace element. It is important for the development and normal functioning of the brain (Elder et al. 2006) but affects its function when present in excess. Tissues rich in mitochondria like the liver, muscles, brain, etc. attract Mn. It also functions as a co-factor for metalloenzymes such as superoxide dismutase (SOD), glutamine synthase, and pyruvate carboxylase (Erikson and Aschner 2003). These enzymes require Mn for their function, but its excess quantity has been reported to inhibit their function. For example, in the central nervous system, glutamic acid is converted to glutamine by the enzyme glutamine synthetase, but in the presence of excess Mn, the enzyme is inhibited (Normandin and Hazell 2002).
Manganese oxide has attracted widespread research interest due to its distinct chemical, physical, catalytic, electrical, and magnetic properties that is different from its bulky counterpart (Wei et al. 2011; Song et al. 2013). Manganese oxide nanoparticles represent a prospective nanomaterial that has shown significant potential in the areas of ion exchange, molecular adsorption, biological and chemical sensing, energy storage, catalysis, magnetic data storage, magnetic resonance imaging, targeted drug delivery, and as an antimicrobial agent (Deng et al. 2013; Miyamoto et al. 2015; Kumara et al. 2014; El-Deab and Ohsaka 2006; Li et al. 2006; Frey et al. 2009; Estelrich et al. 2015; Haneefa et al. 2017). Despite the potential benefits of manganese nanoparticles (MNPs), its adverse effect on animal health is a cause for concern (Pardhiya et al. 2020; Singh et al. 2013a). Thus, understanding the toxicological characteristics of MNPs is crucial prior to its clinical translation. Discharge from factories that produce steel and non-steel alloy, colorants, battery, catalysts, and metal coatings contain high concentration of Mn. Airborne particles containing Mn is also an occupational and environmental problem. The Mn content of the NPs could reach the brain through the airways from breathing and may result in brain damage (Sárközi et al. 2009). Many studies have reported that MNPs have the potential to induce neurotoxicity that could cause neurological syndromes like Parkinson’s disease (Karmakar et al. 2014; Singh et al. 2013a; Máté et al. 2016). The gastrointestinal tract is another important portal of MNPs entry. MNPs have also been shown to cause serious pathological risks to hepatic, renal, spleen, blood, reproductive, and developmental systems (Singh et al. 2013a, b; Hussain et al. 2005; Pardhiya et al. 2020; Yousefalizadegan et al. 2019). MNPs have also been reported to induce toxicity to intestinal epithelial cells (Fredericks et al. 2020). In the last decade, many researchers have studied the reproductive toxicity of MNPs.
7.2.1 Effect of Mn NPs on Male Reproductive System
In another study, gonadotoxicity of MnO2 nanoparticles was examined upon oral administration via gastric tube in male Wistar rats (Zaitseva and Zemlyanova 2019). In this study, rats were divided into five groups, where the first group received 257.7 mg/kg, group 2 received 51.54 mg/kg, group 3 received 10.3 mg/kg, group 4 received 5.15 mg/kg, and group 5 was the control group that received distilled water. The nanosuspension of MnO2 was administered once a day, for 90 days. After the treatment period, rats were euthanized and their sperm were examined for any alterations. Sperm from rats of group 1 and 2 showed 2.18 and 1.7 times decrease in quantity, respectively, as compared to the control rats, while no significant alterations in sperm count was found for the rats in groups 3 and 4. They also found that sperm from rats of groups 1 and 2 showed a significant decrease in osmotic and acidic resistance (1.2–1.3 times) as compared to the control group. Changes in head, neck, and tail morphology in groups 1 and 2 were 1.7–10.3 times more frequent than those from control rats. Thus, only high doses of 51.54 mg/kg and 257.7 mg/kg MnO2 nanosuspension exerted significant changes in sperm parameters of rats.
Negahdary et al. (2015) administered Mn2O3 nanoparticles orally to rats at different doses (100, 200, and 400 ppm) for 14 days. He found a significant decrease of LH, FSH, and testosterone in the serum of 400 ppm administered rats. They also reported a significant decrease of spermatogonial cells, primary spermatocytes, and spermatid cells in the testis of the 400 ppm group of rats. The histopathological evaluation of the rat testis showed that the 400 ppm dosage of the nanoparticles led to an increase in cellular disruption, interstitial edema, and vacuole formation in the seminiferous tubules. They also observed increased interstitial space between the seminiferous tubules and decrease in the epithelium diameter.
To study the plausible reproductive toxicity of MnO2 micro- and nanoparticles, Yousefalizadegan et al. (2019) exposed adult male Wistar rats to the MnO2 particles via subcutaneous injection. They injected the micro- and nanoparticles at 100 mg/kg dose to rats once a week, for 4 weeks. After the experimental duration, they found that the weight of reproductive organs such as testis, epididymis, and prostrate did not alter significantly in the treated rats as compared to the control rats. There were also no significant alterations in the diameter of left testis. However, they reported that the sperm count decrease was highly significant in both the micro- and nano-MnO2 treated groups. The treated groups also showed 100% immobile sperm. The decrease in the number of spermatocytes and spermatogonia in treated groups was highly significant as compared to control group. Serum concentrations of testosterone, estradiol, and follicle-stimulating hormone did not alter significantly among the groups.
Zhang et al. (2020) examined the reproductive toxicity of Mn3O4 on 6- to 7-week-old Sprague-Dawley rats. They administered 10 mg/kg nanoparticles intravenously to the rats once every week for 0, 60, and 120 days. After the experimental duration, they found that the Mn content in the serum and testis increased significantly after 60 and 120 days of the NP administration. Serum testosterone levels decreased significantly in 60 and 120 days groups, whereas follicle-stimulating hormone decreased significantly only in 120 days exposure group as compared to the 0 day group. There was no significant alteration in the luteinizing hormone among the groups. Sperm count and percentage motility decreased significantly and percentage sperm abnormality significantly increased only in 120 days exposure group. They also found significant reduction of the antioxidant enzyme SOD and significant increase in the lipid peroxidation parameter, i.e., malondialdehyde (MDA) after 120 days exposure period. Histopathological assessment of testis from rats of 60 days exposure period revealed that the germinal layer in seminiferous tubules decreased and some Sertoli cells and spermatogenic cells were separated from basal membrane. The 120 days nanoparticle exposure revealed severe damage to the testis. They observed significant decrease in germinal layer with degeneration of seminiferous tubule such as germ cell degeneration, sloughing, atrophy, structural shrinkage, and increased interstitial space between the tubules.
Our group has also studied the toxic effects of MnO2 nanoparticle on the reproductive organ, liver, and kidney and their function on rats (Pardhiya et al. 2020). The adult male Wistar rats were administered with the NPs (30 mg/kg) every alternative day for 45 days. At the end of the experiment, morphometric analysis of the testes showed that its seminiferous tubule height decreased insignificantly and germinal epithelial height decreased significantly. Various alterations like formation of vacuoles, desquamation of epithelial cells, and loss of tubular morphology of seminiferous tubules was observed. Sperm count in the NP-treated rats decreased significantly and sperm damage increased significantly. Treated rats also showed different abnormal sperm head morphology like amorphous head, banana-shaped head, and bent head. The NP-treated rats also showed significant variations in liver function tests and histopathological observations of liver and kidney. Additionally, in the presence of a physical stressor, radiofrequency radiation (RFR), there was a synergistic response in sperm damage.
7.2.2 Effect of Mn NPs on Embryotoxicity and Teratogenicity
Effect of MnO2 NPs on embryotoxicity and teratogenicity was examined by the oral administration of the NPs dispersed in water to male and female Wistar rats (Zaitseva and Zemlyanova 2019). Male and female rats were made to mate during two estrous cycles. Nanosuspension of MnO2 was administered via gastric tube to female rats from the first day of pregnancy to the twenty-first day, once daily in two doses, 0.25 and 2.5 mg/kg, while the control group of rats received distilled water. During the experimental period, the female rats had normal motion activity, reaction to external irritants and feeding of forage was normal, visible mucous tunic was physiologically colored with no discharge, and they had normal body weight, appearance, and behavior as those of control group. The pregnant female rats were euthanized on the twenty-first day of pregnancy, and embryotoxicity and teratogenicity were examined. The embryotoxicity parameters like the number of implantation points, viable fetuses, and number of resorptions of the pregnant rats did not alter significantly from those of the control group. Teratogenic effects of the MnO2 nanoparticles were examined. Fetuses did not show any external congenital malformations, and no discrepancies in the body weight and cranio-caudal body dimensions were observed in the treated and control fetuses. No changes were observed in the morphology of fetus internal organs or skeletal system in the treated groups. Thus, nanodispersed MnO2 did not show any embryotoxic or teratogenic effects upon intragastric administration at 0.25 and 2.5 mg/kg doses.
7.2.3 In Vitro Toxicity of Mn NPs
Upon in vitro assessment of Mn3O4 NP on TM4 cells, reactive oxygen species (ROS) increased with the increasing concentration of the NPs from 0 to 20 μg/ml (Zhang et al. 2020). The authors also reported alterations in the integrity of mitochondrial membrane of TM4 cells when exposed to the nanoparticles, suggesting that Mn3O4 nanoparticles may induce collapse of the mitochondrial membrane potential. Furthermore, they reported increased apoptotic rate in TM4 cells with increase in the nanoparticle concentration.
7.2.4 Mechanism of Mn NPs Toxicity
In order to assess the mechanism of Mn3O4 NPs toxicity to the testis of rats, transcription profiling analysis of the testis from the control and treated rats was done (Zhang et al. 2020). Mn3O4 NPs treatment resulted in upregulation of few genes, which was further enhanced upon 120 days of treatment. Based on Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis, they reported that after 120 days of treatment, four pathways were activated based on the upregulated genes, i.e., PPAR (peroxisome proliferator-activated receptors) signalling pathway (genes Fabp1, Apoa2, Apoa3, and Pck1 upregulated), steroid hormone biosynthetic pathway (genes LOC100361547, Cyp2c12, Cyp2c6v1, and Ugt2b37 upregulated), xenobiotic metabolism by cytochrome P450 (genes Gsta4, LOC102550391, Ugt2b37 and Sult 2a2 upregulated), and drug metabolism by cytochrome P450 (genes Gsta4, LOC102550391, Ugt2b37 upregulated). The authors have proposed a mechanism for the toxicity induced by Mn3O4 NPs based on these findings (Fig. 7.1).
7.2.5 Effect of Mn NPs on Fertility
Effect of Mn3O4 NPs on the fertility of rats was studied (Zhang et al. 2020). The authors reported that the fertility rates, fetus numbers, and rate of live fetus did not differ significantly in the 60 day exposure group of rats as compared to the 0 day exposure. However, after 120 days of nanoparticle exposure, these parameters decreased significantly as compared to 0 day exposure.
7.3 Silver Nanoparticles (AgNPs)
For thousands of years, silver and its compounds have been used as antibacterial and therapeutic agents (Alexander 2009; Barillo and Marx 2014). Silverwares were used to store food, water, and wine to prevent spoilage by the ancient Romans and Greeks. Silver preparations were used to treat ulcer and for wound healing by Hippocrates. Silver nitrate was used for wound care and as an instrument disinfectant. Sims, in 1852, used fine wires of silver to suture the vesicovaginal fistulas caused by delivery and found that it decreased infection significantly. Silver preparations to treat wound infection and burn care were developed at the beginning of nineteenth century. Silver nanoparticles (AgNPs) thus have several medical applications like antimicrobial (Salomoni et al. 2015, 2017; Paredes et al. 2014; Rónavári et al. 2018; Kumar et al. 2017; Sun et al. 2005) and anticancer agents (Gurunathan et al. 2015, 2018; Al-Sheddi et al. 2018; Yuan et al. 2017; Zielinska et al. 2018; Fard et al. 2018; Ahmadian et al. 2018; Tavakoli et al. 2018; Kovács et al. 2016), dental applications (Oei et al. 2012), bone healing and wound repair promoter, enhancement of vaccine immunogenicity (Asgary et al. 2016), anti-diabetic effects (Saratale et al. 2017), and biosensors (Anderson et al. 2017). In spite of these applications, various in vivo studies suggest that AgNPs may be toxic in nature. AgNPs can be distributed in the body through various routes of exposure mainly through ingestion, inhalation, subcutaneous or intravenous injections, and skin contact (Xu et al. 2020). They are absorbed and distributed in systems like the dermis, spleen, digestive, respiratory, nervous, immune, urinary, and reproductive systems (Singh et al. 2017b; Lansdown 2006). Thus, its non-specific distribution may cause toxicities like dermal toxicity, hepatobiliary toxicity, respiratory toxicity, neurotoxicity, ocular toxicity, and reproductive toxicity. The potential of the toxicity depends on route of administration and NP properties like its size, shape, and concentration. AgNPs can cross biological barriers like blood-testis, placental barriers, epithelial barrier and deposit in the testis, epididymis, ovary and uterus. Thus, cells of the reproductive system such as germ cells and related cells like primary follicle, secondary follicle, germline stem cells, and Leydig and Sertoli cells (Ong et al. 2016; Zhang et al. 2015) may be at the risk of damage by these NPs. It may also cause changes in sexual behavior by altering the secretion of reproductive hormones. Studies have reported that the NPs cause reproductive toxicity by increasing inflammation, decreasing the function of mitochondria, downregulating gene expression, inducing the production of ROS, and disrupting DNA structure and apoptosis, and these toxicities depend on size of NPs, dose, and duration of exposure (Zhang et al. 2015; Fathi et al. 2019).
7.3.1 In Vitro Effect of AgNPs
Zhang et al. (2015) reported that 10 nm AgNPs were more toxic to male somatic Leydig (TM3 cells) and Sertoli (TM4) cells than 20 nm sized NPs. The cell proliferation decreased in a concentration-dependent manner from 0 to 100 μg/ml of NPs. The Sertoli cells treated with the NPs showed decreased expression of ZO-1 and Cx43 which encodes tight junction proteins involved in the formation of the blood-testis barrier. However, NP-treated Leydig cells showed decreased expression of StAR, 3β-Hsd, and 17β-Hsd which are involved in testosterone production. Testosterone in turn is needed for induction of spermatogenesis and normal functioning of Sertoli cells. Sertoli cells secrete cytokines that are involved in the proliferation and renewal of spermatogonial stem cells (SSCs). SSCs produce sperm throughout the male’s postnatal life. Thus, the study suggested that AgNPs can affect Leydig and Sertoli cell function, decrease SSCs function, and eventually decrease male fertility.
7.3.2 Effect of AgNPs on Male Reproductive System
Lafuente et al. (2016) investigated the effect of oral administration of polyvinylpyrrolidone-coated AgNPs (50, 100, and 200 mg/kg) per day for 90 days on the sperm of rats. They reported abnormality in sperm morphology in a dose-dependent manner. The various abnormalities in sperm morphology like banana-headed sperm, sperms with bent tail, headless, and neck abnormalities were significantly increased in 100 mg/kg treated rats. Higher doses of NPs showed a progressive but not significant adverse effect on the viability and motility of sperm. Shehata et al. (2021) also showed that 50 mg/kg AgNPs oral administration to rats for 90 days adversely affect sperm count, morphology, mobility, and viability, decrease the levels of reproductive hormones (luteinizing hormone, follicle-stimulating hormone, and testosterone), and induce oxidative stress and lipid peroxidation in testis. The NPs also resulted in DNA degeneration in the testis, and testicular histopathological alterations like thickened testicular capsule, congested blood vessels in capsules and edema of walls, layers of disorganized spermatogonial cells, detachment of germinal epithelium from the basement membrane of seminiferous tubules and mild interstitial edema, degeneration of spermatogonial cells with necrosis, and nuclear pyknosis were observed. The presence of multinucleated giant spermatid cells, defective spermatogenesis, and irregular contour of seminiferous tubules with wide interstitial spaces was also observed. Various other studies have reported the toxic effect of AgNPs on Leydig cells, reproductive hormones, sperm morphology, and mobility in rats (Baki et al. 2014; de Brito et al. 2020). Dziendzikowska et al. (2016) showed that AgNPs had an adverse effect on the hormonal regulation of male rat reproductive system. The NPs altered the sex steroid balance and expression of genes that are involved in steroid metabolism and steroidogenesis. AgNPs have also been reported to alter gene expression in the testis. Intraperitoneal treatment with 50 mg/kg/day AgNPs for 79 days showed alterations in the testicular nuclear transcription factors that are involved in biogenesis and function of mitochondria (Younus et al. 2020). AgNPs treatment resulted in a two-fold increase in the expression of uncoupling protein 2 (UCP2) gene as compared to control. While combined treatment of AgNPs with iron oxide NPs (Fe2O3 NPs) increased the expression of UCP 2 to more than five-folds as compared to control. They found a decreased expression of mitochondrial transcription factor A (mtTFA). Its decreased expression may indicate a reduced mitochondria biogenesis and decreased mitochondrial DNA replication and transcription which may lead to mitochondrial dysfunction. Wang et al. (2016a, b) showed alteration in reproductive parameters and gene expression in Balb/c mice exposed to 125 mg/kg AgNPs. The NPs showed accumulation in the testis and alteration in sperm count, histology, and apoptosis in the testis of treated rats. They showed that 383 genes were altered in mice testis significantly after the treatment. These genes were associated with oxidative stress, apoptosis, and other signalling pathways. Apoptosis-related gene (caspase 3, Myc, and Mdm2) expression was increased, thereby explaining high cellular apoptosis in the testis of 125 mg/kg AgNP-treated mice.
7.3.3 Effect of AgNPs on Female Reproductive System
Studies have also reported the effect of AgNPs on female reproductive system. Intravenous administration of AgNPs at 2 and 4 mg/kg once a day, 10 times, showed the inhibition of oocyte maturation in mice (Lytvynenko et al. 2017). A 1 and 5 times administration of the doses resulted in an increased number of apoptotic cells, whereas 10 times administration increased apoptosis and necrosis of follicular cells surrounding oocytes.
7.3.4 Effect of AgNPs on Fertility and Development
AgNPs have been reported to show fetal developmental toxicity (Mozafari et al. 2020). 1 mg/kg AgNPs was orally administered to pregnant mice at gestation days (GD) 1–7, GD 8–14, and GD 1–14 (Mozafari et al. 2020). On GD 15 the uterus was excised. The NPs decreased the fetal body weight and crown-rump length significantly. Various disorders like exencephaly, scoliosis, small head, lordosis, short thorax, short trunk, and fused digits were found in the treated groups. The fetal midbrain showed fibrosis, necrosis, and apoptosis in groups GD 8–14 and GD 1–14. These results suggest adverse effect of AgNPs in the development of the fetus. A study on the fertility and development of Drosophila was done by Ong et al. (2016) at different AgNP concentrations (0–5 μg/ml). The NPs were fed to Drosophila, absorbed through ingestion, and accumulated in a dose-dependent manner. The treatment resulted in a decreased viability and delayed development in a dose-dependent manner. The germline stem cells and early germ cells were observed to be concentrated at the apical tip of testis, and a significant level of ROS was reported at this tip in the 5 μg/ml AgNP-treated group. They also showed that AgNP treatment promoted precocious differentiation of germline stem cells which might disrupt its maintenance, thereby resulting in a decreased sperm cell count. They also reported a delayed eclosion or hatching of Drosophila and a decreased number of male offsprings in the groups treated with higher concentrations of the NP. Further, they reported a decreased success in mating and number of second and third generations in NP-treated groups, suggesting the possible transfer of AgNPs accumulated in germline stem cells to offsprings which might have affected the development and fertility of the offsprings.
7.3.5 Reproductive Toxicity of AgNPs on Zebrafish
Chen et al. (2017) used zebrafish ovarian follicle as an in vitro model to assess the toxicity of AgNPs and Ag+ on the oocyte maturation. The follicular cells showed vacuolation, swollen mitochondria, and condensed nucleus in the treated follicular cells. The oocytes showed decreased cyclic adenosine monophosphate (cAMP) concentration resulting in resumption of meiosis. Caspases 3 and 9 were upregulated in AgNPs- and Ag+ treated groups, respectively, leading to apoptosis of ovarian follicle cells. Ma et al. (2018) exposed zebrafish to 0, 10, 33, and 100 μg/L AgNPs for 5 weeks and assessed their effect in the reproductive system. Exposure at 33 and 100 μg/L for 5 weeks was reported to decrease the fecundity in female zebrafish significantly. The number of apoptotic cells also increased in ovarian and testicular tissues. The NPs were biodistributed in both the ovary and testis, and increasing ROS levels were reported. The expression patterns of genes involved in mitochondria-mediated apoptotic pathway (bax, bcl2, caspases 3 and 9) were altered to some extent.
7.4 Gold Nanoparticles (AuNPs)
Gold nanoparticles (AuNPs) have optical and electrical properties owing to which it has gained increasing attention in optical, chemical, and biochemical fields. They have been functionalized with different molecules such as peptides, drugs, genes, and other targeting ligands to achieve an improved antiviral and antibacterial function (Burygin et al. 2009). They also have potential application in drug delivery where it could be used to deliver proteins, vaccines, drugs, or nucleotides to their target. They have been studied to overcome bacterial drug resistance by conjugating the antibiotics with AuNPs (Singh et al. 2017a). AuNPs are usually considered safe and thus have been used extensively in cosmetic materials, antimicrobial, and in medical filling material and as drug carriers (Selvaraj et al. 2010). However, studies have shown in vitro and in vivo cytotoxic effects of AuNPs (Jia et al. 2017). Studies in rodents showed toxicity in the liver, kidney, spleen, and sperm (Chen et al. 2013; Fraga et al. 2014; Wiwanitkit et al. 2009). Yahyaei et al. (2019) assessed the toxicity of AuNPs in male Wistar rats. They synthesized 50 nm AuNPs and decided the toxic and non-toxic dose based on in vitro study. They exposed the rats with both doses for 3 days after which they assessed histopathological alterations in the liver, kidney, and testis. They found that at non-toxic dose, there were no alterations in testis and mild alterations in some parts of the liver and kidney. At the toxic dose, they observed mild alterations in all the three organs. They concluded that the toxic response of AuNPs in vitro and in vivo are different and that mild changes even at the toxic dose may be due to shorter duration of exposure and/or the fact that AuNPs used were biologically synthesized from a fungal strain Fusarium oxysporum.
7.4.1 Effect of AuNPs on Male Reproductive System
Wiwanitkit et al. (2009) showed that upon 15 minutes of incubation of human semen with AuNPs, the motility of the sperm decreased (75% motility) as compared to control (95% motility). The NPs were found to penetrate the sperm head and tail regions. AuNPs (2.5–15 nm) also caused swelling and chromatin unpacking in mouse sperm DNA (Skuridin et al. 2010). Balb/c mice were exposed to AuNPs (10–30 nm) at 40 and 200 μg/kg/day for 7 and 35 days, respectively (Nazar et al. 2016). The results showed decreased motility, increased abnormal spermatozoa, and altered sperm morphology in the exposed groups especially in the 35 day exposure group. Other studies also suggest adverse effects of AuNPs on spermatozoa (Taylor et al. 2010, 2012). In contrast, the intramuscular administration of gold core silica shell NPs (70 nm) did not show the presence of NPs in the testis with no morphological alterations in the testis (Leclerc et al. 2015). AuNPs at 1 mg/kg dose for 10 days was reported to cause more alteration in the epididymis of adult rats (6 months old) than in the young rats (1 month old) upon intraperitoneal administration (Kalynovskyi et al. 2016). The mechanism of cellular toxicity was shown by Liu et al. (2020). They observed that the 5 nm AuNPs could enter Leydig cells (TM3 cell line) and induce formation of autophagosomes, thereby increasing ROS production and disrupting S phase of the cell cycle. This resulted in concentration-dependent toxicity of NPs in cells and DNA damage. The AuNPs also inhibited expression of androgen synthesizing enzyme, 17α-hydroxylase, due to which the testosterone production in the cells reduced significantly. Repeated administration of 0.17 and 0.5 mg/kg AuNPs intravenously to Balb/c mice caused retained accumulation of NPs in mice testis. The testosterone level in 0.5 mg/kg group was reduced significantly with a decreased expression of 17α-hydroxylase enzyme in testis. The AuNP treatment also significantly increased the rate of sperm malfunction in the epididymis, but the treatment did not affect mice fertility. AuNPs also alter the levels of reproductive hormones. Behnammorshedi and Nazem (2015) showed that intraperitoneal injection of 25 ppm, 50 ppm, and 100 ppm AuNPs for 10 days increased the levels of luteinizing and follicle-stimulating hormones and decreased the level of testosterone with increase in the NP dose. The testis histopathological analysis showed degeneration of seminiferous tubules at 100 ppm dose. Gupta et al. (2018) studied the biodistribution of AuNPs after the oral treatment of male rats with 20 μg/g for 90 days. They observed the NPs to be accumulated in Leydig cells, interstitial space in testis, and in germ cells. AuNPs were also detected in the cytoplasm of Sertoli cells, and AuNPs entrapped in lysosomes were observed near developing spermatids and cytoplasm of germ cells. The testis histopathology showed mild sloughing of germ cells from basement membrane of seminiferous tubules. A report suggested that laser-synthesized dextran-coated AuNPs are safe for biological use (Bailly et al. 2019). Upon intravenous administration of AuNPs (1 mg/kg) in mice, they accumulated preferentially in the liver and spleen without causing histopathological alterations or inflammation toxicity in the tissues. There was no acute or chronic toxicity in the liver, kidney, and spleen of the mice. However, in this study the dose of AuNPs taken was less, and it was a one-time exposure to the NPs.
7.4.2 Effect of AuNPs on Female Reproductive System
AuNPs have also been reported to cause adverse effects in female reproductive system. Biodistribution of PEGylated AuNPs in the ovary and uterus is size dependent (Poley et al. 2020). When 20 nm, 50 nm, 100 nm, and 200 nm sized PEGylate AuNPs were intravenously injected during estrus stage of female mice, accumulation of 100 nm and 200 nm NPs in ovary was ~two-fold and ~five-fold less, respectively, as compared to 10 nm and 20 nm sized NPs. Similarly, in the uterus, accumulation of 100 nm was ~3.5-fold less and 200 nm was ~12.5-fold less as compared to smaller sized NPs. Granulosa cells in the ovary are involved in steroid synthesis. AuNPs can traverse granulosa cell membrane and certain organelles like lipid droplets and mitochondria.
7.4.3 Mechanism of AuNPs Toxicity on Ovarian Follicle
AuNPs of smaller size can accumulate in granulosa cells of the ovary (Fig. 7.2) and affect hormone secretion. Figure 7.2 shows accumulation of AuNPs in theca and granule cells of follicle. Their accumulation may result in apoptosis of ovarian cell and acceleration of antrum formation. Major NPs are accumulated in the cumulus cell layer that surrounds the oocyte. No NPs enter the oocyte as they are trapped in the zona pellucida layer. AuNP toxicity was shown to induce imbalance in steroid hormone synthesis and ovum dysplasia when the 10 nm AuNPs were engulfed by granulosa cells (Stelzer and Hutz 2009).
The level of estradiol-17 beta was shown to significantly alter after 24 h. Oral administration of AuNPs (20 μg/g/day) for 28 days to zebrafish caused accumulation of the NPs in ovary, histopathological alteration of ovarian tissue, and DNA strand breaks of ovarian cells (Dayal et al. 2017). Mammalian oocytes show different toxicological response to different NPs (AuNPs, AgNPs, and Au and Ag alloy NPs) (Tiedemann et al. 2014). Tiedemann et al. (2014) showed that both AuNPs and AgNPs accumulate in cumulus layers and oocytes, but toxicity of NPs to oocytes increased with increase in the silver molar fraction.
7.4.4 Toxicity of AuNPs to Placental Barriers and Embryonic Development
Transplacental crossing of AuNPs have been reported in experimental animals (Semmler-Behnke et al. 2007; Hougaard et al. 2015). A study showed that intravenously administered AuNPs could enter placental cells via endocytosis (Rattanapinyopituk et al. 2013). However, permeability of NPs also depends on its coating. Rather than crossing the placental barrier, PEGylated AuNPs were found to be aggregated in the syncytiotrophoblast cell layer in human placenta (Myllynen et al. 2008). Fetal exposure to NPs also depends upon the stage of gestational maturation. Yang et al. (2012) showed that three types of AuNP coatings, viz., ferritin, PEG, and citrate, were administered from GD 5.5 to GD 15.5 to the pregnant CD1 mice. Before GD 11.5, all the coating types of AuNPs were detected in the fetal tissue. Thereafter their levels declined in the tissue. This may be due to the maturation of the placental barrier. Overall, out of the three coatings, PEG- and ferritin-coated AuNPs were found to be accumulated to a higher degree than the citrate-coated NPs. AuNPs have generational impact as well where it can disrupt embryonic development. Exposure to AuNPs altered the expression of 19 genes in the human fetal lung fibrolasts (Ng et al. 2011). AuNPs show comparatively lower toxicity than AgNPs (Asharani et al. 2011; Bar-Ilan et al. 2009). Exposure to AuNPs and AgNPs at 3, 10, 50, and 100 nm sizes caused 3% and 100% mortality, respectively, to zebrafish embryo post 120 h fertilization (Bar-Ilan et al. 2009). While AuNPs induced a minimal toxic effect, AgNPs produced a variety of embryonic morphological malformations. Parallel sized AgNPs and AuNPs showed very different toxicity profiles, with AgNPs showing size-dependent toxicity while AuNPs were inert in all the sizes. AgNPs showed concentration-dependent mortality, whereas AuNPs did not increase mortality at higher doses. As both the NPs were accumulated in the embryo, the reason for AgNP toxicity may have been caused by the NP itself or Ag+ formed due to in vivo NP destabilization. On the other hand, Browning et al. (2009) showed that the bioaccumulation of AuNPs in zebrafish embryo increased with increasing concentration but the effect of the NPs in embryo development was not proportional to its concentration. Furthermore, AuNPs synthesized using polyvinyl alcohol as the capping agent did not show any embryonic toxicity (Asharani et al. 2011). The extent of toxicity of AuNPs has been related to its morphology. Spherical AuNPs have been reported to be more toxic to zebrafish embryos than the rod- or polyhedron-shaped AuNPs (Wang et al. 2016a, b).
7.4.5 Mechanism of AuNPs Toxicity
AuNPs enter cells through endocytosis and accumulate. These NPs are phagocytosed by lysosomes which result in accumulation of AuNPs in lysosomes. This increases the lysosomal pH and makes it alkaline, impairing its degradation capacity. This process can induce autophagy. Previous studies have shown that AuNPs induce autophagy in germ cells. There was an upregulation of LC3, a autophagy involved protein and downregulation of P62 indicating the impediment of autophagosome degradation (Ma et al. 2011).
7.5 Titanium Nanoparticles (TiNPs)
TiNPs have tremendous application such as white pigment in paint, in ceramics, in sunscreens, as food additive and packaging material, in cosmetic creams, and in surgical implants. Due to its radical generating property, TiO2 NPs are being used as an antimicrobial agent in paints (Kaiser et al. 2013). They are also used in environmental decontamination of water, air, and soil (Choi et al. 2006; Tran and Webster, 2009; Besov et al. 2010; Shi et al. 2013), anti-fogging materials, as well as in sanitization and disinfectant products in hospitals (Krystek et al. 2014). It has also been studied for therapy in dermatologic diseases such as acne vulgaris, condyloma acuminata, hyperpigmented skin lesions, and atopic dermatitis (Wiesenthal et al. 2011). However, toxicological reports of TiNPs in in vitro and in vivo models have raised concerns on human impact of TiNPs. Several studies suggest its adverse effects on the brain, liver, bone marrow, RBC, sperm, testis, ovary, and embryo development (Bakare et al. 2016; Jia et al. 2017; Morgan et al. 2017; Ma et al. 2010; Li et al. 2009; Ze et al. 2014; Hu et al. 2010; Solaiman et al. 2020; Ali et al. 2019).
7.5.1 Effect of TiNPs on Male Reproductive System
The effect of different concentrations of TiO2 NPs (1, 20, and 100 μg) on buffalo spermatozoa was observed (Pawar and Kaul 2014). The NPs were internalized by the sperm head and cytoplasm. They found that after 6 h of exposure, there was a significant decrease in cell viability and membrane integrity of sperm. At higher doses, a significant increase in sperm capacitation was observed. There was a dose-dependent increase in the DNA fragmentation of sperm. In vivo study of the effect of intraperitoneally administered anatase TiO2 NPs (2.5 and 5 mg/kg) for 3 days in mice showed accumulation of nanomaterial in mice scrotum (Smith et al. 2015). This led to testicular histopathology and affected the sperm maturation and function in the epididymis after 4–8 days (but not 10 days to 5 weeks) postinjection. In the treated rats, there were several sperm abnormalities like flagellar abnormality, inability of sperm acrosome to react, excess residual cytoplasm, reduced motility, and increased ROS levels. Another study was done by Bakare et al. (2016) in mice at 9.38, 18.75, 37.5, 75, and 160 mg/kg body weight of animal administered intraperitoneally for 5 consecutive days. They found increase in number of abnormal sperm. The testes showed histopathological alterations such as vacuolation, necrosis, and congestion of interstitial edema. Gao et al. (2013) also reported lesions in the testis and sperm, decrease in sperm count and motility, imbalance of sex hormones, and alteration of 254 genes (153 genes upregulated and 101 downregulated) in the testicular tissue of mice after 90-day intragastric administration of TiNPs.
7.5.2 Biphasic Effect of TiNPs on the Sperm and Testis
A study showed a decrease in sperm motility after intravenous administration of TiNP (10 and 50 mg/kg) to male C57BL/6 J mice (Miura et al. 2019). They showed the adverse effect of short-term exposure of TiNPs to mice. They also administered the NPs orally at 20 or 100 mg/kg to mice. However, in both cases (intravenous and oral administration), they did not find significant reduction in sperm count in the testis and cauda, and thus they hypothesized that the NPs targeted mature spermatozoa. In an in vitro study, they found that TiNP reduced sperm motility, incorporation of [3H]-thymidine, and ATP levels. Since long-term exposure studies of TiNPs indicate testicular impairment, they concluded that the effect of TiNPs on the sperm and testis is biphasic, i.e., short-term exposure to TiNPs affects mature sperm by attacking the blood-epididymis barrier and long-term exposure affects the testis by attacking the blood-testis barrier (Fig. 7.3).
Morgan et al. (2017) showed the long-term oral exposure effect of TiNPs on rats. They exposed rats with 100 mg/kg TiNPs for 8 weeks daily. The results showed apoptosis in rat testis with edema, sloughing of germ cells, and pyknosis of spermatogonial layer. NPs also decreased the testosterone level significantly, decreased viability, and increased the morphological abnormalities of sperm like presence of deformed and detached heads and curved and coiled tails. The TiNPs significantly increased lipid peroxidation and decreased antioxidant glutathione in testis. This provide insights into oxidative stress induction by TiNPs. The expression of testin gene increased 27.47-folds as compared to untreated rats. Concentration of testin, secreted by the Sertoli cells, is inversely correlated with the cell junctions in the testis. Thus, increase in the gene expression of the testis may be due to disruption of the testicular cell junction. Moreover, 90 days oral treatment to adult rats with 10 mg/kg TiNPs showed adverse effect on rat reproductive system (Solaiman et al. 2020). Low level of testosterone, sperm count, and Johnson score significantly increased lipid peroxidation and lactate dehydrogenase level, and degenerative alterations in seminiferous tubules of testis were observed in TiNPs-exposed rats.
7.5.3 Effect of TiNPs on Female Reproductive System
TiNPs have also been found to cause adverse effect in female rats (Ali et al. 2019). Immature female Wistar rats were intraperitoneally injected with 50, 100, and 150 mg/kg of TiNPs for 5 days. They found a significant increase in the levels of estrogen and progesterone in 150 mg/kg group. The NPs caused histopathological alterations in the ovary such as loss of Graafian follicles, reduction of granulosa and theca layer thickness and destruction of follicle walls. Higher doses of 100 and 150 mg/kg decreased the number of corpus luteum, growing follicles, and Graafian follicles significantly. Other studies also suggest the adverse effect of TiNPs on reproductive parameters of female rodents (Gao et al. 2012; Tassinari et al. 2014). TiNPs have also been studied for their toxicity to developing embryo. For assessing the toxicity of TiNPs in embryo, the embryos of 8.5 days were isolated from female mice and cultured and incubated with TiO2 NPs (5–10, 60, and 90 nm) at 0, 50, 100, and 200 μg/ml for 16, 24, and 48 h (Jia et al. 2017). They observed a dose- and time-dependent toxicity of the NPs on the growth and development of embryos. They found that the increasing toxicity like decrease in VXY diameter of embryo, crown-rump length, head length, and number of body sections of embryo and malformation rate was associated with larger particle size. In order to assess the potential toxic effect of TiNPs in pregnant women, Lee et al. (2019) exposed rats orally to 0, 100, 300, and 100 mg/kg from GD (gestation day) 6–19. They found the accumulation of NPs in maternal liver, brain, and placenta. But the NPs did not induce marked toxicities in the maternal rats and did not affect the embryo development. In another experiment on gestational exposure of pregnant mice to TiNPs, the mice were orally exposed to 0, 1, and 10 mg/kg/day TiNPs from GD 1–13 (Zhang et al. 2018). They found no difference in the number of implanted and resorbed embryos and placental weight in the treated groups. However, placental to body weight was reduced in 1 mg/kg dose group at GD13. In the 10 mg/kg dose group, the proportion of spongiotrophoblast was higher than the untreated group, yet the placental labyrinth was significantly lower. The intricate fetal vessel formation was impaired, and the number of uterine natural killer cells was reduced in TiNP-treated rats. The treatment inhibited the proliferation, induced apoptosis in the placenta by nuclear pyknosis with activation of caspase 3, upregulation of Bax, and downregulation of Bcl-2 proteins on GD13. In the TiNP-treated placenta, the expression levels of Exc1, Ascl2, Hand1, Hand2, Eomes, and Fra1 mRNA decreased. Thus, exposure of pregnant mice to TiNPs significantly impaired the growth and development of placenta.
7.6 Cadmium Nanoparticles (Cd NPs)
Nanomaterials containing cadmium have various applications including in electronic, optical, and biological applications (Nirmal et al. 1996; Bowers et al. 2005; Agarwal et al. 2005). Thus, its environmental and human health impacts has become a cause of concern. Toxicity of cadmium selenide NPs (CdSe NPs) is linked to the release of Cd2+ which generates ROS and can produce oxidative stress (Kirchner et al. 2005; Haque et al. 2013). Cd NPs have been reported to induce neurotoxicity, hepatotoxicity, and pulmonary and reproductive toxicities (Horvath et al. 2011; Gao et al. 2018; De La Cruz et al. 2019; Blum et al. 2012; Bajaj et al. 2013). Cadmium sulfide (CdS) nanodots are more toxic than nanorods in terms of accumulation in organs, DNA damage, viability and abnormality of spermatozoa, oxidative stress, and liver and kidney damage (Liu et al. 2014). CdS nanodots have been reported to be more toxic than microsized CdS (Li et al. 2009).
7.6.1 Effect of Cd NPs on Male Reproductive System
CdS NPs were investigated for its effect in male Wistar rats, where the NPs were intraperitoneally injected at 2.5 mg/rat/day for 30 days (Bajaj et al. 2013). The results showed a reduction in sperm count and motility, fertility index, decrease in testis weight, decrease in testis protein and glycogen, increased cholesterol, and decreased testosterone level. Antioxidants like the enzyme SOD and glutathione significantly decreased and lipid peroxidation significantly increased in the testis. Histopathological observation showed degradation in testicular tissue. Single dose of intraperitoneal administration of dextrin-coated CdS NPs at 100 μg/kg to rats showed quick distribution in the body, with maximum concentration after 72 h in all the analyzed tissues (De La Cruz et al. 2019). Upon continuous administration for 90 days, testis degeneration and chronic lung inflammation were observed.
7.6.2 Effect of Cd NPs on Fertility, Embryo, and Post-natal Development
Blum et al. (2012) performed a study to assess the ability of cadmium oxide (CdO) NPs to reach the placenta and affect the fetus and/or neonate upon exposure of pregnant CD1 mice to CdO NPs. The pregnant mice were exposed every other day to 100 μg (exposure 1) or daily to 230 μg (exposure 2) of CdO NPs/m3 for 2.5 h from 4.5 to 16.5 days post coitus. The concentration of Cd increased in the uterus, placenta, and other maternal organs but was undetectable in the fetus at 17.5 days post coitus. A decrease in pregnancy incident (i.e., no implantation evidence) by 23%, delay in maternal weight gain, decrease in length of fetus, and delayed neonatal weight gain was observed in exposure 2 group. Inhalation of CdO NPs thus has an adverse effect on reproductive fecundity and fetal and postnatal growth. Yan et al. (2016) investigated the effect of cadmium telluride quantum dots (CdTe-QDs) on gonads of Bombyx mori. They injected the organism through dorsal vein with 0.32 nmol of CdTe-QDs. The QDs induced early germ cell death or malformations via mechanisms related to autophagy and apoptosis through lysosomal and mitochondrial pathways. Quantitative analysis of development of germ cells and histological observation of gonads showed that reproductive toxicity was characterized by male sensitivity. The quantity and quality of sperm deteriorated due to QD exposure in early stages of male, which was the main reason that the eggs remained unfertilized. Chan and Shiao (2008) investigated the effect CdSe QD on post-implantation embryonic mice development. They incubated mouse blastocytes in CdSe QDs at 250 and 500 nmol/L for 24 h. They found dose-dependent apoptosis in blastocytes. The QDs induced inhibition of cell proliferation especially in the inner cell mass and inhibition of post-implantation embryo development. Very few blastocysts could reach later stages of development. The QDs also inhibited pre-implantation development of morulas to blastocysts. Furthermore, 500 nmol/L dose group resulted in the resorption of blastocysts and decrease in weight of fetus. Hsieh et al. (2009) investigated the effect of CdSe QDs on mice oocyte maturation, fertilization, and pre- and post-implantation development. The QDS significantly reduced oocyte maturation rate, fertilization, and embryo development (in vitro). 500 nM QDs in vitro treatment resulted in resorption of post-implantation embryo and decreased the fetal and placental weights. Chu et al. (2010) investigated the transfer of CdTe and CdS QDs from pregnant mice to their fetuses. They showed that the QDs could cross the placental barrier and transfer from mice to fetus. Smaller QDs were easily transferred than the larger ones and the number of QDs transferred increased with increase in dosage. Capping the QDs with silica or polyethylene glycol could reduce the transfer of QDs but did not prevent. These results limit the QDs utility in pregnant women. CdTe QDs may retard hatching of zebrafish and increase the oxidative stress in zebrafish embryos (Tian et al. 2019). Cd NPs can be modified to decrease or delay its toxic effects. For example, carbon-coated Cd NPs reduce toxicity by mitigating the release of Cd2+ (Balmuri et al. 2017).
7.7 Conclusion
Nanotechnology is a rapidly expanding field in terms of application and adverse impact on both animals and environment. Its positive impacts are undoubtedly important for the medicinal and industrial sector. However, increasing health hazards due to NM application cannot be overlooked. Therefore, toxicological impacts of NMs need to be explored thoroughly. Safer and sustainable application of nanotechnology cannot be approached without its complete nanotoxicological assessment. Knowledge acquired from the nanotoxicological assessments will allow production of safer and sustainable NMs.
This study discusses that metallic NMs may induce reproductive toxicity. NMs reach the systemic circulation through blood and may get accumulated in reproductive organs (testes) as they are able to cross the blood testes barrier. Bioaccumulation of these metallic NMs lead to the generation of oxidative stress in reproductive organs and cause hazardous effects such as reduced sperm count, sperm mobility and adversely affects hormonal regulation and morphological and ultrastructural changes. Nonetheless, more elaborated studies on reproductive toxicity are needed to demonstrate safer nanotechnological exploitation to benefit mankind. Therefore, by addressing the toxicological concerns of NMs, nanotechnology will be able to be utilized at its most.
References
Agarwal R, Barrelet CJ, Lieber CM. Lasing in single cadmium sulfide nanowire optical cavities. Nano Lett. 2005;5(5):917–20.
Ahmadian E, Dizaj SM, Rahimpour E, Hasanzadeh A, Eftekhari A, Halajzadeh J, Ahmadian H. Effect of silver nanoparticles in the induction of apoptosis on human hepatocellular carcinoma (HepG2) cell line. Mater Sci Eng C. 2018;93:465–71.
Alexander JW. History of the medical use of silver. Surg Infect. 2009;10(3):289–92.
Al-Sheddi ES, Farshori NN, Al-Oqail MM, Al-Massarani SM, Saquib Q, Wahab R, et al. Anticancer potential of green synthesized silver nanoparticles using extract of Nepeta deflersiana against human cervical cancer cells (HeLA). Bioinorg Chem Appl. 2018;2018:9390784.
Ali N, Amiri BA, Melika G. The effect of titanium dioxide nanoparticles injection in neonatal period on ovaries in mature rats. GSC Biol. Pharm. Sci. 2019;6(1).
Anderson K, Poulter B, Dudgeon J, Li SE, Ma X. A highly sensitive nonenzymatic glucose biosensor based on the regulatory effect of glucose on electrochemical behaviors of colloidal silver nanoparticles on MoS2. Sensors. 2017;17(8):1807.
Asgary V, Shoari A, Baghbani-Arani F, Shandiz SAS, Khosravy MS, Janani A, et al. Green synthesis and evaluation of silver nanoparticles as adjuvant in rabies veterinary vaccine. Int J Nanomed. 2016;11:3597.
Asharani PV, Lianwu YI, Gong Z, Valiyaveettil S. Comparison of the toxicity of silver, gold and platinum nanoparticles in developing zebrafish embryos. Nanotoxicology. 2011;5(1):43–54.
Azenabor A, Ekun AO, Akinloye O. Impact of inflammation on male reproductive tract. J Reprod Infertil. 2015;16:123.
Bailly AL, Correard F, Popov A, Tselikov G, Chaspoul F, Appay R, et al. In vivo evaluation of safety, biodistribution and pharmacokinetics of laser-synthesized gold nanoparticles. Sci Rep. 2019;9(1):1–12.
Bajaj VK, Goyal A, Sharma G, Sharma KB, Gupta RS. Synthesis of CdS nanoparticle and reveal its effect on reproductive system of male albino rats. BioNanoScience. 2013;3(1):58–66.
Bakare AA, Udoakang AJ, Anifowoshe AT, Fadoju OM, Ogunsuyi OI, Alabi OA, Alimba CG, Oyeyemi IT. Genotoxicity of titanium dioxide nanoparticles using the mouse bone marrow micronucleus and sperm morphology assays. J Pollut Eff. Control. 2016;7:1–7.
Baki ME, Miresmaili SM, Pourentezari M, Amraii E, Yousefi V, Spenani HR, et al. Effects of silver nano-particles on sperm parameters, number of Leydig cells and sex hormones in rats. Iran J Reprod Med. 2014;12(2):139.
Bar-Ilan O, Albrecht RM, Fako VE, Furgeson DY. Toxicity assessments of multisized gold and silver nanoparticles in zebrafish embryos. Small. 2009;5(16):1897–910.
Barillo DJ, Marx DE. Silver in medicine: a brief history BC 335 to present. Burns. 2014;40:S3–8.
Behnammorshedi M, Nazem H. The effect of gold nanoparticle on luteinizing hormone, follicle stimulating hormone, testosterone and testis in male rat. Biomed Res. 2015;26(2):348–52.
Besov AS, Krivova NA, Vorontsov AV, Zaeva OB, Kozlov DV, Vorozhtsov AB, Parmon VN, Sakovich GV, Komarov VF, Smirniotis PG, Eisenreich N. Air detoxification with nanosize TiO2 aerosol tested on mice. J Hazard Mater. 2010;173(1–3):40–6.
Bisht S, Faiq M, Tolahunase M, Dada R. Oxidative stress and male infertility. Nat Rev Urol. 2017;14:470–85.
Blum JL, Xiong JQ, Hoffman C, Zelikoff JT. Cadmium associated with inhaled cadmium oxide nanoparticles impacts fetal and neonatal development and growth. Toxicol Sci. 2012;126(2):478–86.
Balmuri SR, Selvaraj U, Kumar VV, Anthony SP, Tsatsakis AM, Golokhvast KS, Raman T. Effect of surfactant in mitigating cadmium oxide nanoparticle toxicity: implications for mitigating cadmium toxicity in environment. Environ Res. 2017;152:141–9.
Bowers MJ, McBride JR, Rosenthal SJ. White-light emission from magic-sized cadmium selenide nanocrystals. J Am Chem Soc. 2005;127(44):15378–9.
Browning LM, Lee KJ, Huang T, Nallathamby PD, Lowman JE, Xu XH. Random walk of single gold nanoparticles in zebrafish embryos leading to stochastic toxic effects on embryonic developments. Nanoscale. 2009;1(1):138–52.
Burygin GL, Khlebtsov BN, Shantrokha AN, Dykman LA, Bogatyrev VA, Khlebtsov NG. On the enhanced antibacterial activity of antibiotics mixed with gold nanoparticles. Nanoscale Res Lett. 2009;4(8):794–801.
Campagnolo L, Massimiani M, Magrini A, Camaioni A, Pietroiusti A. Physico-chemical properties mediating reproductive and developmental toxicity of engineered nanomaterials. Curr Med Chem. 2012;19(26):4488–94.
Chan WH, Shiao NH. Cytotoxic effect of CdSe quantum dots on mouse embryonic development. Acta Pharmacol Sin. 2008;29(2):259–66.
Chen H, Dorrigan A, Saad S, Hare DJ, Cortie MB, Valenzuela SM. In vivo study of spherical gold nanoparticles: inflammatory effects and distribution in mice. PLoS One. 2013;8(2):e58208.
Chen SX, Yang XZ, Deng Y, Huang J, Li Y, Sun Q, et al. Silver nanoparticles induce oocyte maturation in zebrafish (Danio rerio). Chemosphere. 2017;170:51–60.
Choi H, Stathatos E, Dionysiou DD. Sol–gel preparation of mesoporous photocatalytic TiO2 films and TiO2/Al2O3 composite membranes for environmental applications. Applied Catalysis B: Environmental. 2006;63(1–2):60–7.
Chu M, Wu Q, Yang H, Yuan R, Hou S, Yang Y, et al. Transfer of quantum dots from pregnant mice to pups across the placental barrier. Small. 2010;6(5):670–8.
Das J, Choi YJ, Song H, Kim JH. Potential toxicity of engineered nanoparticles in mammalian germ cells and developing embryos: treatment strategies and anticipated applications of nanoparticles in gene delivery. Hum Reprod. 2016;22:588–619.
Dayal N, Singh D, Patil P, Thakur M, Vanage G, Joshi DS. Effect of bioaccumulation of gold nanoparticles on ovarian morphology of female zebrafish (Danio rerio). World J Pathol. 2017;6(1).
de Brito JLM, Lima VND, Ansa DO, Moya SE, Morais PC, Azevedo RBD, Lucci CM. Acute reproductive toxicology after intratesticular injection of silver nanoparticles (AgNPs) in Wistar rats. Nanotoxicology. 2020;14(7):893–907.
De La Cruz GG, Gomez-Cansino R, Rodriguez-Fragoso P, Jaimeschavez P, Barbosa-Rayo AL, Reyes-Esparza J, Rodriguez-Fragoso L. Disposition and biocompatibility of dextrin-coated cadmium sulphide nanoparticles after a single dose and multiple doses in rats. Indian J Pharm Sci. 2019;81(5):876–84.
Deng QF, Ren TZ, Yuan ZY. Mesoporous manganese oxide nanoparticles for the catalytic total oxidation of toluene. React Kinet Mech Catal. 2013;108(2):507–18.
Dziendzikowska K, Krawczyńska A, Oczkowski M, Królikowski T, Brzóska K, Lankoff A, Gromadzka-Ostrowska J. Progressive effects of silver nanoparticles on hormonal regulation of reproduction in male rats. Toxicol Appl Pharmacol. 2016;313:35–46.
El-Deab MS, Ohsaka T. Manganese oxide nanoparticles electrodeposited on platinum are superior to platinum for oxygen reduction. Angew Chem Int Ed. 2006;45(36):5963–6.
Elder A, Gelein R, Silva V, Feikert T, Opanashuk L, Carter J, Oberdörster G. Translocation of inhaled ultrafine manganese oxide particles to the central nervous system. Environ Health Perspect. 2006;114(8):1172–8.
El-Sayed YS, Shimizu R, Onoda A, Takeda K, Umezawa M. Carbon black nanoparticle exposure during middle and late fetal development induces immune activation in male offspring mice. Toxicology. 2015;327:53–61.
Ema M, Kobayashi N, Naya M, Hanai S, Nakanishi J. Reproductive and developmental toxicity studies of manufactured nanomaterials. Reprod Toxicol. 2010;30(3):343–52.
Ema M, Hougaard KS, Kishimoto A, Honda K. Reproductive and developmental toxicity of carbon-based nanomaterials: a literature review. Nanotoxicology. 2016;10:391–412.
Erikson KM, Aschner M. Manganese neurotoxicity and glutamate-GABA interaction. Neurochem Int. 2003;43(4–5):475–80.
Estelrich J, Sánchez-Martín MJ, Busquets MA. Nanoparticles in magnetic resonance imaging: from simple to dual contrast agents. Int J Nanomedicine. 2015;10:1727.
Fard NN, Noorbazargan H, Mirzaie A, Hedayati C, M., Moghimiyan, Z., & Rahimi, A. Biogenic synthesis of AgNPs using Artemisia oliveriana extract and their biological activities for an effective treatment of lung cancer. Artif Cells Nanomed Biotechnol. 2018;46(sup3):S1047–58.
Fathi N, Hoseinipanah SM, Alizadeh Z, Assari MJ, Moghimbeigi A, Mortazavi M, et al. The effect of silver nanoparticles on the reproductive system of adult male rats: a morphological, histological and DNA integrity study. Adv Clin Exp Med. 2019;28(3):299–305.
Fraga S, Brandão A, Soares ME, Morais T, Duarte JA, Pereira L, et al. Short-and long-term distribution and toxicity of gold nanoparticles in the rat after a single-dose intravenous administration. Nanomedicine. 2014;10(8):1757–66.
Fredericks J, Senapati S, Wannemuehler MJ. Cytotoxic effects of manganese oxide nanoparticles in combination with microbial components on intestinal epithelial cells. F1000Research. 2020;9(975):975.
Frey NA, Peng S, Cheng K, Sun S. Magnetic nanoparticles: synthesis, functionalization, and applications in bioimaging and magnetic energy storage. Chem Soc Rev. 2009;38(9):2532–42.
Gaharwar US, Meena R, Rajamani P. Biodistribution, clearance and morphological alterations of intravenously administered iron oxide nanoparticles in male wistar rats. Int J Nanomedicine. 2019;14:9677–9692. https://doi.org/10.2147/IJN.S223142.
Gao G, Ze Y, Li B, Zhao X, Zhang T, Sheng L, Hu R, Gui S, Sang X, Sun Q, Cheng J. Ovarian dysfunction and gene-expressed characteristics of female mice caused by long-term exposure to titanium dioxide nanoparticles. J Hazard Mater. 2012;243:19–27.
Gao G, Ze Y, Zhao X, Sang X, Zheng L, Ze X, Gui S, Sheng L, Sun Q, Hong J, Yu X. Titanium dioxide nanoparticle-induced testicular damage, spermatogenesis suppression, and gene expression alterations in male mice. J Hazard Mater. 2013;258:133–43.
Gao M, Yang Y, Lv M, Song W, Song Z. Oxidative stress and DNA damage in zebrafish liver due to hydroxyapatite nanoparticles-loaded cadmium. Chemosphere. 2018;202:498–505.
Geraets L, Oomen AG, Schroeter JD, Coleman VA, Cassee FR. Tissue distribution of inhaled micro-and nano-sized cerium oxide particles in rats: results from a 28-day exposure study. Toxicol Sci. 2012;127(2):463–73.
Gupta H, Singh D, Vanage G, Joshi DS, Thakur M. Evaluation of histopathological and ultrastructural changes in the testicular cells of Wistar rats post chronic exposure to gold nanoparticles. 2018;17:9–15.
Gurunathan S, Park JH, Han JW, Kim JH. Comparative assessment of the apoptotic potential of silver nanoparticles synthesized by Bacillus tequilensis and Calocybe indica in MDA-MB-231 human breast cancer cells: targeting p53 for anticancer therapy. Int J Nanomedicine. 2015;10:4203.
Gurunathan S, Qasim M, Park C, Yoo H, Kim JH, Hong K. Cytotoxic potential and molecular pathway analysis of silver nanoparticles in human colon cancer cells HCT116. Int J Mol Sci. 2018;19(8):2269.
Han JW, Jeong JK, Gurunathan S, Choi YJ, Das J, Kwon DN, Cho SG, Park C, Seo HG, Park JK, et al. Maleand female-derived somatic and germ cell-specific toxicity of silver nanoparticles in mouse. Nanotoxicology. 2016;10:361–73.
Haneefa M, Jayandran M, Balasubramanian M. Evaluation of antimicrobial activity of green-synthesized manganese oxide nanoparticles and comparative studies with curcuminaniline functionalized nanoform. Asian J Pharm Clin Res. 2017;10(3):347–52.
Haque MM, Im HY, Seo JE, Hasan M, Woo K, Kwon OS. Acute toxicity and tissue distribution of CdSe/CdS-MPA quantum dots after repeated intraperitoneal injection to mice. J Appl Toxicol. 2013;33(9):940–50.
Horvath E, Oszlánczi G, Máté Z, Szabó A, Kozma G, Sápi A, et al. Nervous system effects of dissolved and nanoparticulate cadmium in rats in subacute exposure. J Appl Toxicol. 2011;31(5):471–6.
Hougaard KS, Campagnolo L, Chavatte-Palmer P, Tarrade A, Rousseau-Ralliard D, Valentino S, Park MV, de Jong WH, Wolterink G, Piersma AH, Ross BL, Hutchison GR, Hansen JS, Vogel U, Jackson P, Slama R, Pietroiusti A, Cassee FR. A perspective on the developmental toxicity of inhaled nanoparticles. Reprod Toxicol. 2015;56:118–40.
Hoyt VW, Mason E. Nanotechnology: emerging health issues. J Chem Health Saf. 2008;15:10–5.
Hsieh MS, Shiao NH, Chan WH. Cytotoxic effects of CdSe quantum dots on maturation of mouse oocytes, fertilization, and fetal development. Int J Mol Sci. 2009;10(5):2122–35.
Hu R, Gong X, Duan Y, Li N, Che Y, Cui Y, Zhou M, Liu C, Wang H, Hong F. Neurotoxicological effects and the impairment of spatial recognition memory in mice caused by exposure to TiO2 nanoparticles. Biomaterials. 2010;31(31):8043–50.
Hussain SM, Hess KL, Gearhart JM, Geiss KT, Schlager JJ. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol In Vitro. 2005;19(7):975–83.
Jia YP, Ma BY, Wei XW, Qian ZY. The in vitro and in vivo toxicity of gold nanoparticles. Chin Chem Lett. 2017;28(4):691–702.
Kadar E, Dyson O, Handy RD, Al-Subiai SN. Are reproduction impairments of free spawning marine invertebrates exposed to zero-valent nano-iron associated with dissolution of nanoparticles? Nanotoxicology. 2013;7(2):135–43.
Kaiser JP, Zuin S, Wick P. Is nanotechnology revolutionizing the paint and lacquer industry? A critical opinion. Science of the Total Environment. 2013;442:282–9.
Kalynovskyi VY, Pustovalov AS, Grodzyuk GY, Andriushyna NS, Dzerzhynsky ME. Effect of gold and silver nanoparticles on the morpho-functional state of the epididymis and prostate gland in rats. Regul Mech Biosyst. 2016;7(2):106–11.
Karmakar A, Zhang Q, Zhang Y. Neurotoxicity of nanoscale materials. J Food Drug Anal. 2014;22(1):147–60.
Kirchner C, Liedl T, Kudera S, Pellegrino T, Muñoz Javier A, Gaub HE, et al. Cytotoxicity of colloidal CdSe and CdSe/ZnS nanoparticles. Nano Lett. 2005;5(2):331–8.
Kovács D, Igaz N, Keskeny C, Bélteky P, Tóth T, Gáspár R, et al. Silver nanoparticles defeat p53-positive and p53-negative osteosarcoma cells by triggering mitochondrial stress and apoptosis. Sci Rep. 2016;6(1):1–13.
Krystek P, Tentschert J, Nia Y, Trouiller B, Noël L, Goetz ME, … & De Jong WH. Method development and inter-laboratory comparison about the determination of titanium from titanium dioxide nanoparticles in tissues by inductively coupled plasma mass spectrometry. Anal Bioanal Chem. 2014;406(16), 3853–3861.
Kumar SD, Singaravelu G, Ajithkumar S, Murugan K, Nicoletti M, Benelli G. Mangrove-mediated green synthesis of silver nanoparticles with high HIV-1 reverse transcriptase inhibitory potential. J Clust Sci. 2017;28(1):359–67.
Kumara BP, Karikkatb S, Krishna SH, Udayashankarab TH, Shivaprasada KH, Nagabhushanac BM. Synthesis, characterization of nano MnO2 and its adsorption characteristics over an azo dye. J Mater Sci. 2014;2(1):27–31.
Lafuente D, Garcia T, Blanco J, Sánchez DJ, Sirvent JJ, Domingo JL, Gómez M. Effects of oral exposure to silver nanoparticles on the sperm of rats. Reprod Toxicol. 2016;60:133–9.
Lan Z, Yang WX. Nanoparticles and spermatogenesis: how do nanoparticles affect spermatogenesis and penetrate the blood–testis barrier. Nanomedicine. 2012;7:579–96.
Lansdown AB. Silver in health care: antimicrobial effects and safety in use. Biofunct Text Skin. 2006;33:17–34.
Leclerc L, Klein JP, Forest V, Boudard D, Martini M, Pourchez J, et al. Testicular biodistribution of silica-gold nanoparticles after intramuscular injection in mice. Biomed Microdevices. 2015;17(4):1–11.
Lee J, Jeong JS, Kim SY, Park MK, Choi SD, Kim UJ, Park K, Jeong EJ, Nam SY, Yu WJ. Titanium dioxide nanoparticles oral exposure to pregnant rats and its distribution. Part Fibre Toxicol. 2019;16(1):1–12.
Li WN, Yuan J, Shen XF, Gomez-Mower S, Xu LP, Sithambaram S, et al. hydrothermal synthesis of structure-and shape-controlled manganese oxide octahedral molecular sieve nanomaterials. Adv Funct Mater. 2006;16(9):1247–53.
Li KG, Chen JT, Bai SS, Wen X, Song SY, Yu Q, et al. Intracellular oxidative stress and cadmium ions release induce cytotoxicity of unmodified cadmium sulfide quantum dots. Toxicol In Vitro. 2009;23(6):1007–13.
Liu S, Krewski D, Shi Y, Chen Y, Burnett RT. Association between maternal exposure to ambient air pollutants during pregnancy and fetal growth restriction. J Expo Sci Environ Epidemiol. 2007;17(5):426–32.
Liu L, Sun M, Li Q, Zhang H, Alvarez PJ, Liu H, Chen W. Genotoxicity and cytotoxicity of cadmium sulfide nanomaterials to mice: comparison between nanorods and nanodots. Environ Eng Sci. 2014;31(7):373–80.
Liu Y, Li X, Xiao S, Liu X, Chen X, Xia Q, et al. The effects of gold nanoparticles on Leydig cells and male reproductive function in mice. Int J Nanomed. 2020;15:9499.
Lytvynenko A, Rieznichenko L, Sribna V, Stupchuk M, Grushka N, Shepel A, et al. Functional status of reproductive system under treatment of silver nanoparticles in female mice. Int J Reprod Contracept Obstet Gynecol. 2017;6(5):1713–20.
Ma L, Liu J, Li N, Wang J, Duan Y, Yan J, Liu H, Wang H, Hong F. Oxidative stress in the brain of mice caused by translocated nanoparticulate TiO2 delivered to the abdominal cavity. Biomaterials. 2010;31(1):99–105.
Ma X, Wu Y, Jin S, Tian Y, Zhang X, Zhao Y, et al. Gold nanoparticles induce autophagosome accumulation through size-dependent nanoparticle uptake and lysosome impairment. ACS Nano. 2011;5(11):8629–39.
Ma YB, Lu CJ, Junaid M, Jia PP, Yang L, Zhang JH, Pei DS. Potential adverse outcome pathway (AOP) of silver nanoparticles mediated reproductive toxicity in zebrafish. Chemosphere. 2018;207:320–8.
Máté Z, Horváth E, Kozma G, Simon T, Kónya Z, Paulik E, et al. Size-dependent toxicity differences of intratracheally instilled manganese oxide nanoparticles: conclusions of a subacute animal experiment. Biol Trace Elem Res. 2016;171(1):156–66.
Meena R, Kajal K, Paulraj R. Cytotoxic and genotoxic effects of titanium dioxide nanoparticles in testicular cells of male wistar rat. Appl Biochem Biotechnol. 2014;75(2):825–40.
Miura N, Ohtani K, Hasegawa T, Yoshioka H, Hwang GW. Biphasic adverse effect of titanium nanoparticles on testicular function in mice. Sci Rep. 2019;9(1):1–8.
Miyamoto Y, Kuroda Y, Uematsu T, Oshikawa H, Shibata N, Ikuhara Y, et al. Synthesis of ultrasmall Li–Mn spinel oxides exhibiting unusual ion exchange, electrochemical and catalytic properties. Sci Rep. 2015;5(1):1–13.
Morgan AM, Ibrahim MA, Noshy PA. Reproductive toxicity provoked by titanium dioxide nanoparticles and the ameliorative role of Tiron in adult male rats. Biochemical and biophysical research communications. 2017;486(2):595–600.
Mozafari M, Khoradmehr A, Danafar A, Miresmaeili M, Kalantar SM. Toxic effects of maternal exposure to silver nanoparticles on mice fetal development during pregnancy. Birth Defects Res. 2020;112(1):81–92.
Myllynen PK, Loughran MJ, Howard CV, Sormunen R, Walsh AA, Vähäkangas KH. Kinetics of gold nanoparticles in the human placenta. Reprod Toxicol. 2008;26(2):130–7.
Nazar M, Talebi AR, Sharifabad MH, Abbasi A, Khoradmehr A, Danafar AH. Acute and chronic effects of gold nanoparticles on sperm parameters and chromatin structure in mice. Int J Reprod BioMed. 2016;14(10):637.
Negahdary M, Arefian Z, Dastjerdi HA, Ajdary M. Toxic effects of Mn2O3 nanoparticles on rat testis and sex hormone. J Nat Sci Biol Med. 2015;6(2):335.
Ng CT, Dheen ST, Yip WCG, Ong CN, Bay BH, Yung LYL. The induction of epigenetic regulation of PROS1 gene in lung fibroblasts by gold nanoparticles and implications for potential lung injury. Biomaterials. 2011;32(30):7609–15.
Nirmal M, Dabbousi BO, Bawendi MG, Macklin JJ, Trautman JK, Harris TD, Brus LE. Fluorescence intermittency in single cadmium selenide nanocrystals. Nature. 1996;383(6603):802–4.
Normandin L, Hazell AS. Manganese neurotoxicity: an update of pathophysiologic mechanisms. Metab Brain Dis. 2002;17(4):375–87.
Oberdorster G, Oberdorster E, Oberdorster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspect. 2005;113:823–39.
Oei JD, Zhao WW, Chu L, DeSilva MN, Ghimire A, Rawls HR, Whang K. Antimicrobial acrylic materials with in situ generated silver nanoparticles. J Biomed Mater Res B Appl Biomater. 2012;100(2):409–15.
Ong C, Lee QY, Cai Y, Liu X, Ding J, Yung LYL, et al. Silver nanoparticles disrupt germline stem cell maintenance in the Drosophila testis. Sci Rep. 2016;6(1):1–10.
Opris R, Toma V, Olteanu D, Baldea I, Baciu AM, Lucaci FI, Berghian-Sevastre A, Tatomir C, Moldovan B, Clichici S, et al. Effects of silver nanoparticles functionalized with Cornus mas L. extract on architecture and apoptosis in rat testicle. Nanomedicine. 2019;14:275–99.
Pardhiya S, Gaharwar US, Gautam R, Priyadarshini E, Nirala JP, Rajamani P. Cumulative effects of manganese nanoparticle and radiofrequency radiation in male Wistar rats. Drug Chem Toxicol. 2020:1–13.
Paredes D, Ortiz C, Torres R. Synthesis, characterization, and evaluation of antibacterial effect of Ag nanoparticles against Escherichia coli O157: H7 and methicillin-resistant Staphylococcus aureus (MRSA). Int J Nanomedicine. 2014;9:1717.
Pawar K, Kaul G. Toxicity of titanium oxide nanoparticles causes functionality and DNA damage in buffalo (Bubalus bubalis) sperm in vitro. Toxicol Ind Health. 2014;30(6):520–33.
Poley M, Shammai Y, Kaduri M, Koren L, Adir O, Shklover J, et al. Chemotherapeutic nanoparticles accumulate in the female reproductive system during ovulation affecting fertility and anticancer activity. bioRxiv. 2020.
Qin F, Shen T, Li J, Qian J, Zhang J, Zhou G, Tong J. SF-1 mediates reproductive toxicity induced by Cerium oxide nanoparticles in male mice. J Nanobiotechnol. 2019;17(1):41.
Rattanapinyopituk K, Shimada A, Morita T, Sakurai M, Asano A, Hasegawa T, et al. Demonstration of the clathrin-and caveolin-mediated endocytosis at the maternal–fetal barrier in mouse placenta after intravenous administration of gold nanoparticles. J Vet Med Sci. 2013:13-0512.
Rónavári A, Igaz N, Gopisetty MK, Szerencsés B, Kovács D, Papp C, et al. Biosynthesized silver and gold nanoparticles are potent antimycotics against opportunistic pathogenic yeasts and dermatophytes. Int J Nanomed. 2018;13:695.
Roy R, Kumar S, Tripathi A, Das M, Dwivedi PD. Interactive threats of nanoparticles to the biological system. Immunol Lett. 2014;158(1–2):79–87.
Salomoni R, Léo P, Rodrigues MFA. Antibacterial activity of silver nanoparticles (AgNPs) in Staphylococcus aureus and cytotoxicity effect in mammalian cells. SubStance. 2015;17:18.
Salomoni R, Léo P, Montemor AF, Rinaldi BG, Rodrigues MFA. Antibacterial effect of silver nanoparticles in Pseudomonas aeruginosa. Nanotechnol Sci Appl. 2017;10:115.
Saratale GD, Saratale RG, Benelli G, Kumar G, Pugazhendhi A, Kim DS, Shin HS. Anti-diabetic potential of silver nanoparticles synthesized with Argyreia nervosa leaf extract high synergistic antibacterial activity with standard antibiotics against foodborne bacteria. J Clust Sci. 2017;28(3):1709–27.
Sárközi L, Horváth E, Kónya Z, Kiricsi I, Szalay B, Vezér T, Papp A. Subacute intratracheal exposure of rats to manganese nanoparticles: behavioral, electrophysiological, and general toxicological effects. Inhal Toxicol. 2009;21:83–91.
Selvaraj V, Grace AN, Alagar M, Hamerton I. Antimicrobial and anticancer efficacy of antineoplastic agent capped gold nanoparticles. J Biomed Nanotechnol. 2010;6(2):129–37.
Semmler-Behnke M, Fertsch S, Schmid G, Wenk A, Kreyling WG. Uptake of 1.4 nm versus 18 nm gold nanoparticles in secondary target organs is size dependent in control and pregnant rats after intratracheal or intravenous application. In: Proceedings of the EuroNanoForum; 2007. p. 19–21.
Shehata AM, Salem FM, El-Saied EM, Abd El-Rahman SS, Mahmoud MY, Noshy PA. Zinc nanoparticles ameliorate the reproductive toxicity induced by silver nanoparticles in male rats. Int J Nanomedicine. 2021;16:2555.
Shi H, Magaye R, Castranova V, Zhao J. Titanium dioxide nanoparticles: a review of current toxicological data. Particle and fibre toxicology. 2013;(1):1–33.
Shittu OK, Aaron SY, Oladuntoye MD, Lawal B. Diminazene aceturate modified nanocomposite for improved efficacy in acute trypanosome infection. J Acute Dis. 2018;7:36.
Singh SP, Kumari M, Kumari SI, Rahman MF, Mahboob M, Grover P. Toxicity assessment of manganese oxide micro and nanoparticles in Wistar rats after 28 days of repeated oral exposure. J Appl Toxicol. 2013a;33(10):1165–79.
Singh SP, Kumari M, Kumari SI, Rahman MF, Kamal SK, Mahboob M, Grover P. Genotoxicity of nano-and micron-sized manganese oxide in rats after acute oral treatment. Mutat Res Genet Toxicol Environ Mutagen. 2013b;754(1–2):39–50.
Singh R, Patil S, Singh N, Gupta S. Dual functionality nanobioconjugates targeting intracellular bacteria in cancer cells with enhanced antimicrobial activity. Sci Rep. 2017a;7(1):1–10.
Singh SP, Bhargava CS, Dubey V, Mishra A, Singh Y. Silver nanoparticles: biomedical applications, toxicity, and safety issues. Int J Res Pharm Pharm Sci. 2017b;4(2):01–10.
Skuridin SG, Dubinskaya VA, Rudoy VM, Dement’eva OV, Zakhidov ST, Marshak TL, et al. Effect of gold nanoparticles on DNA package in model systems. In: Doklady. Biochemistry and biophysics, vol. 432, no. 1. Dordrecht: Springer Nature BV. p. 141; 2010.
Smith MA, Michael R, Aravindan RG, Dash S, Shah SI, Galileo DS, Martin-DeLeon PA. Anatase titanium dioxide nanoparticles in mice: evidence for induced structural and functional sperm defects after short-, but not long-, term exposure. Asian J Androl. 2015;17(2):261.
Solaiman AA, Ramadan H, Eid AA. Histologic study of the possible protective effect of resveratrol versus resveratrol-loaded niosomes against titanium dioxide nanoparticles-induced toxicity on adult rat seminiferous tubules. Egypt. J. Histol. 2020;43(4):1143–61.
Song MK, Zhang Y, Cairns EJ. A long-life, high-rate lithium/sulfur cell: a multifaceted approach to enhancing cell performance. Nano Lett. 2013;13(12):5891–9.
Srám RJ, Binková B, Rössner P, Rubes J, Topinka J, Dejmek J. Adverse reproductive outcomes from exposure to environmental mutagens. Mutat Res. 1999;428(1–2):203–15.
Stelzer R, Hutz RJ. Gold nanoparticles enter rat ovarian granulosa cells and subcellular organelles, and alter in-vitro estrogen accumulation. J Reprod Dev. 2009:0909170201.
Sun RWY, Chen R, Chung NPY, Ho CM, Lin CLS, Che CM. Silver nanoparticles fabricated in Hepes buffer exhibit cytoprotective activities toward HIV-1 infected cells. Chem Commun. 2005;40:5059–61.
Tassinari R, Cubadda F, Moracci G, Aureli F, D’Amato M, Valeri M, De Berardis B, Raggi A, Mantovani A, Passeri D, Rossi M. Oral, short-term exposure to titanium dioxide nanoparticles in Sprague-Dawley rat: focus on reproductive and endocrine systems and spleen. Nanotoxicology. 2014;8(6):654–62.
Tavakoli F, Jahanban-Esfahlan R, Seidi K, Jabbari M, Behzadi R, Pilehvar-Soltanahmadi Y, Zarghami N. Effects of nano-encapsulated curcumin-chrysin on telomerase, MMPs and TIMPs gene expression in mouse B16F10 melanoma tumour model. Artif Cells Nanomed Biotechnol. 2018;46(sup2):75–86.
Taylor U, Petersen S, Barchanski A, Mittag A, Barcikowski S, Rath D. Influence of gold nanoparticles on vitality parameters of bovine spermatozoa. In: Reproduction in domestic animals, vol. 45. Malden: Wiley-Blackwell Publishing, Inc; 2010. p. 60.
Taylor UAWE, Barchanski A, Garrels W, Klein S, Kues W, Barcikowski S, Rath D. Toxicity of gold nanoparticles on somatic and reproductive cells. In: Nano-biotechnology for biomedical and diagnostic Research. Dordrecht: Springer; 2012. p. 125–33.
Tian J, Hu J, Liu G, Yin H, Chen M, Miao P, et al. Altered Gene expression of ABC transporters, nuclear receptors and oxidative stress signaling in zebrafish embryos exposed to CdTe quantum dots. Environ Pollut. 2019;244:588–99.
Tiedemann D, Taylor U, Rehbock C, Jakobi J, Klein S, Kues WA, et al. Reprotoxicity of gold, silver, and gold–silver alloy nanoparticles on mammalian gametes. Analyst. 2014;139(5):931–42.
Tran N, Webster TJ. Nanotechnology for bone materials. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 2009;1(3):336–51.
Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J. The role of oxidative stress and antioxidants in male fertility. Cent Eur J Urol. 2013;66:60.
Wang E, Huang Y, Du Q, Sun Y. Silver nanoparticles (AgNPs) induced changes of reproductive parameters and gene expression was involved in apoptosis in the murine male testis. Fertil Steril. 2016a;106(3):e283–4.
Wang Z, Xie D, Liu H, Bao Z, Wang Y. Toxicity assessment of precise engineered gold nanoparticles with different shapes in zebrafish embryos. RSC Adv. 2016b;6(39):33009–13.
Wei W, Cui X, Chen W, Ivey DG. Manganese oxide-based materials as electrochemical supercapacitor electrodes. Chem Soc Rev. 2011;40(3):1697–721.
Wiesenthal A, Hunter L, Wang S, Wickliffe J, Wilkerson M. Nanoparticles: small and mighty. Int J Dermatol. 2011;50(3):247–54.
Wiwanitkit V, Sereemaspun A, Rojanathanes R. Effect of gold nanoparticles on spermatozoa: the first world report. Fertil Steril. 2009;91(1):e7–8.
Xu L, Wang YY, Huang J, Chen CY, Wang ZX, Xie H. Silver nanoparticles: synthesis, medical applications and biosafety. Theranostics. 2020;10(20):8996.
Yahyaei B, Nouri M, Bakherad S, Hassani M, Pourali P. Effects of biologically produced gold nanoparticles: toxicity assessment in different rat organs after intraperitoneal injection. AMB Express. 2019;9(1):1–12.
Yan SQ, Xing R, Zhou YF, Li KL, Su YY, Qiu JF, et al. Reproductive toxicity and gender differences induced by cadmium telluride quantum dots in an invertebrate model organism. Sci Rep. 2016;6(1):1–16.
Yang H, Sun C, Fan Z, Tian X, Yan L, Du L, et al. Effects of gestational age and surface modification on materno-fetal transfer of nanoparticles in murine pregnancy. Sci Rep. 2012;2(1):1–8.
Yokota S, Moriya N, Iwata M, Umezawa M, Oshio S, Takeda K. Exposure to diesel exhaust during fetal period affects behavior and neurotransmitters in male offspring mice. J Toxicol Sci. 2013;38(1):13–23.
Younus AI, Yousef MI, Abdel-Nabi KM, Younus MI, Abdulrahman JM. Reproductive toxicity of iron oxide nanoparticles, silver nanoparticles and their mixture in male rats: effects on testicular gene expression. World J Adv Res Rev. 2020;7(2):075–81.
Yousefalizadegan N, Mousavi Z, Rastegar T, Razavi Y, Najafizadeh P. Reproductive toxicity of manganese dioxide in forms of micro-and nanoparticles in male rats. Int J Reprod BioMed. 2019;17(5):361.
Yuan YG, Peng QL, Gurunathan S. Silver nanoparticles enhance the apoptotic potential of gemcitabine in human ovarian cancer cells: combination therapy for effective cancer treatment. Int J Nanomedicine. 2017;12:6487.
Zaitseva NV, Zemlyanova MA. Toxicologic characteristics of nanodisperse manganese oxide: physical-chemical properties, biological accumulation, and morphological-functional properties at various exposure types. In: Heavy metal toxicity in public health. IntechOpen; 2019.
Ze Y, Sheng L, Zhao X, Hong J, Ze X, Yu X, Pan X, Lin A, Zhao Y, Zhang C, Zhou Q. TiO2 nanoparticles induced hippocampal neuroinflammation in mice. PloS one. 2014;9(3):e92230.
Zhang XF, Choi YJ, Han JW, Kim E, Park JH, Gurunathan S, Kim JH. Differential nanoreprotoxicity of silver nanoparticles in male somatic cells and spermatogonial stem cells. Int J Nanomedicine. 2015;10:1335.
Zhang L, Xie X, Zhou Y, Yu D, Deng Y, Ouyang J, Yang B, Luo D, Zhang D, Kuang H. Gestational exposure to titanium dioxide nanoparticles impairs the placentation through dysregulation of vascularization, proliferation and apoptosis in mice. Int J Nanomedicine. 2018;13:777.
Zhang X, Yue Z, Zhang H, Liu L, Zhou X. Repeated administrations of Mn3O4 nanoparticles cause testis damage and fertility decrease through PPAR-signaling pathway. Nanotoxicology. 2020;14(3):326–40.
Zielinska E, Zauszkiewicz-Pawlak A, Wojcik M, Inkielewicz-Stepniak I. Silver nanoparticles of different sizes induce a mixed type of programmed cell death in human pancreatic ductal adenocarcinoma. Oncotarget. 2018;9(4):4675.
Acknowledgement
The author (USG) thankfully acknowledges the Indian Council of Medical Research (ICMR) New Delhi for providing Research Associate Fellowship (Sanction No. 45/02/2018-NAN/BMS).
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gaharwar, U.S., Pardhiya, S., Rajamani, P. (2022). A Perspective on Reproductive Toxicity of Metallic Nanomaterials. In: Roychoudhury, S., Kesari, K.K. (eds) Oxidative Stress and Toxicity in Reproductive Biology and Medicine. Advances in Experimental Medicine and Biology, vol 1391. Springer, Cham. https://doi.org/10.1007/978-3-031-12966-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-12966-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12965-0
Online ISBN: 978-3-031-12966-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)