Abstract
In 1946, the paediatric radiologist John P. Caffey was the first to describe the relation between the presence of multiple fractures of the long bones and subdural haematomas in six children in whom no previous trauma was known. Since then, radiology plays a pivotal role in the detection and description of fractures related to potential child abuse. It is not uncommon that radiologists are the first clinicians that raise the possibility of potential non-accidental injury. In this chapter the importance of radiological imaging protocols, such as those from the Royal College of Radiologists and the Society and College of Radiographers and the American College of Radiology, is highlighted. The different imaging techniques and their indications and limitations in living and deceased victims of potential child are also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radiology
- Conventional radiography
- Computed tomography
- Magnetic resonance imaging
- Linear slot scanning
- Bone densitometry
- Imaging protocol
3.1 Introduction
Even before Kempe published his now classic article on ‘the battered child syndrome’ in 1962, radiologists drew attention to fractures that could really only be explained by the impact of external mechanical force [1]. In 1946, Caffey was the first to describe the relation between the presence of multiple fractures of the long bones and subdural haematomas in six children in whom no previous trauma was known [2]. He thought it remarkable that in a number of children no new anomalies were found while hospitalized; however, some children showed new manifestations as soon as they returned home. Based on the fact that in children subdural haematomas are usually of traumatic origin, he suspected that this combination had a traumatic origin. In 1953, Silberman established that the combination of injuries as described by Caffey had to have a traumatic background [3]. In 1955, Woolley was the first to conclude that the found anomalies were the result of ‘intentionally’ inflicted physical injuries [4]. In 1957, 11 years after his original publication, Caffey concluded that physical abuse by either one or both parent(s) could be a possible explanation for this combination of injuries [5].
The importance of radiological examination when there are suspicions of inflicted injuries was not just demonstrated by the earlier-mentioned radiologists. Ellerstein performed routine radiological examinations in children suspected of being physically abused [6]. In 11.5% he found radiological indications for inflicted injuries. Approximately 20% of these children had fractures without any clinical manifestations.
Generally, fractures are the result of the more serious forms of physical abuse. Non-accidental fractures (inflicted fractures, fractures seen in child abuse) are similar to fractures sustained in an accident. Whether a fracture can be the result of non-accidental circumstances is determined by a combination of:
-
The type of fracture.
-
The age and level of development of the child.
-
The manner in which the fracture must have been sustained (according to established biomechanical data).
-
The statement of the child, the parents, or the caregivers, regarding the origin of the fracture.
Non-accidental circumstances are likely when the first three factors are contradicted by the fourth. The role of (paediatric) radiologists is of great importance and often conclusive in determining whether non-accidental circumstances are involved. In children below a certain age (see Sect. 3.2) who are suspected of being physically abused, it is indicated to do a skeletal survey. The purpose of the skeletal survey is:
-
To detect occult fractures.
-
To obtain additional information on clinically suspect abnormalities.
-
To date fractures.
-
To diagnose the underlying skeletal abnormalities that may provide an increased risk for fractures.
In the following paragraphs, the existing guidelines and quality criteria that apply to radiological imaging will be discussed.
3.2 Conventional Radiology
3.2.1 Guidelines
There currently are two major guidelines on imaging in case of suspected physical child abuse. The first is from the American College of Radiology (ACR) and the second is from the Royal College of Radiologists in collaboration with Society and College of Radiographers (RCR & SCoR). Both guidelines are discussed in detail and the minor differences are highlighted. In Europe, the European Society of Paediatric Radiology (ESPR) advises to adhere to the RCR & SCoR guideline.
3.2.1.1 American College of Radiology
According to the ACR, the use of specific imaging techniques in suspected physical child abuse will depend on the age of the child and the signs and symptoms presented [7]. For this purpose the ACR uses the following guidelines; for completeness, not just conventional radiology is mentioned:
-
1.
Suspected physical abuse. Child ≤24 months of age. Neurological or visceral injuries not clinically suspected. Initial imaging evaluation.
-
(a)
A full skeletal survey (Table 3.1).
-
(b)
Tc-99 m bone scan whole body; can be a complementary/adjunctive examination for detecting skeletal trauma. It should only be used when the radiographic skeletal survey is negative but clinical suspicion remains high and search for further evidence of skeletal trauma is warranted.
-
(c)
There is no strong evidence to recommend universal screening with neuroimaging. However, clinicians should have low threshold for performing head CT or MRI in young children with suspected child abuse.
-
(a)
-
2.
Suspected physical abuse. Child >24 months of age. Neurological or visceral injuries not clinically suspected. Initial imaging evaluation.
-
(a)
Initial imaging should focus on the areas of clinical concern. In children >2 years of age, skeletal survey is usually not done but may be performed based on clinical findings and the need to document the presence or absence of injuries.
-
(b)
There is no strong evidence to recommend universal screening with neuroimaging in the absence of clinical suspicion for AHT.
-
(a)
-
3.
Child with one or more of the following: neurologic signs or symptoms, apnoea, complex skull fracture, other fractures, or injuries highly suspicious for child abuse. Initial imaging evaluation.
-
(a)
A full skeletal survey in all children <2 years of age in whom there is suspicion of abuse (Table 3.1).
-
(b)
Tc-99 m bone scan whole body (see point 1).
-
(c)
MRI scan of the head should be performed if the clinical presentation warrants further assessment.
-
(d)
MRI of the cervical spine should be strongly considered at the time of MRI brain imaging.
-
(e)
MRI of the total spine should be reserved for cases where the distinction between abusive and accidental trauma is not clear.
-
(a)
-
4.
Child. Suspected physical abuse. Suspected thoracic or abdominopelvic injuries (e.g. abdominal skin bruises, distension, tenderness, or elevated liver or pancreatic enzymes). Initial imaging evaluation.
-
(a)
A full skeletal survey in all children <2 years of age in whom there is suspicion of abuse (Table 3.1).
-
(b)
Tc-99 m bone scan whole body (see point 1).
-
(c)
CT or MRI of the head should also be performed in children with neurologic symptoms or risk factors for intracranial injuries.
-
(d)
Contrast-enhanced CT of the abdomen is indicated in acute evaluation of the child with suspected abdominopelvic injuries. Routine CT scan screening for abdominal or chest injury is not recommended.
-
(a)
In other words: when child abuse is suspected, radiological examination is always advised in children <2 years old, and in children >2 years only when there are further serious external or internal injuries.
When the radiographs show any abnormalities, a view in a second plane should be made. A repeat skeletal survey should be performed approximately 2 weeks after the initial examination.
3.2.1.2 The Royal College of Radiologists and the Society and College of Radiographers
In September 2017, the RCR & SCoR formulated a British guideline, endorsed by the Royal College of Paediatrics and Child Health, for imaging when child abuse is suspected (Table 3.1) [8]. According to this guideline, a skeletal survey should be made in each child <2 years who is suspected of being subjected to child abuse. In view of the medical/legal implications of this examination, this skeletal survey should meet the highest technical standards and as such should be made by two trained radiographers. The examination should be performed under the supervision of a radiologist, who also safeguards the quality of the examination. The child is only allowed to leave the radiology department after the radiologist has approved the complete examination.
An important difference with the ACR protocol is the standard addition of oblique views of the ribs (Fig. 3.1a, b). Ingram et al. showed in a randomized control study that this increases the sensitivity of the detection of rib fractures by 17% (95% CI 2–36%) and the specificity by 7% (95% CI 2–13%) [9]. Hansen et al. described a series of 22 patients in which the oblique view changed the interpretation in 12 cases (p = 0.02) [10]. In these 12 cases, 19 rib fractures were found on the oblique views, and six fractures were excluded. All patients with rib fractures showed at least one fracture on the anterior-posterior and lateral views. A similar study by Marine et al found that in a group of 212 patients (106 patients with at least one rib fracture and 106 patients without rib fractures), when the four-view series were used as a gold standard, the sensitivity and specificity for any rib fracture on the two-view series was respectively 57% (range 47–70) and 99% (range 98–100) [11]. For posterior rib fractures this was almost identical at respectively 59% (range 53–67) and 99% (range 97–100). The reported confidence increased from 0.022 to 0.061 for the two-view series to 0.007 to 0.031 for the four-view series (p < 0.001).
The authors of this chapter have one comment with regard to the updated RCR & SCoR guideline and that relates to the use of AP radiographs of the whole limb. We feel that, based on our personal experiences, this should be discouraged as it can lead to insufficient radiographs in children who actually are too big for this approach. It is a well-known fact that in general skeletal surveys a substantial deviation from the protocols in use is seen, and adding an additional option to the process will certainly not lead to an improvement [12,13,14].
Although this book covers fractures and the imaging thereof, we feel that it is important to underline the importance of the complete workup of children, in whom child abuse is suspected. According to the guidelines all children under the age of 1 year and those children older than 1 year who have external evidence of head trauma and/or neurological symptoms should undergo neuroimaging. This should be done according to the flow chart shown in Fig. 3.2.
3.2.1.3 Examination on Indication
Besides the indications in the earlier-mentioned guidelines, there are also further situations in which imaging may be indicated. Among these situations we would like to highlight young children with burns and drug-endangered children. In the first group it is known that a significant proportion are non-accidental burns, according to a systematic review the incidence in all children (aged 0–17 years) ranged from 0.5% to 24.6%, in children under the age of 13 this was up to 25%, with pooled data showing an incidence of 9.7% [15]. Hicks and Stolfi studied a small group of children with burns who underwent a skeletal survey, and they found that 5 (14%) out of 36 children had a positive skeletal survey [16]. Fagen et al. studied a group of 112 children with burns, mean age 15 months (range 1 month to 110 months) [17]. They grouped the children into three categories; non-accidental, indeterminate, and accidental. The outcome of the skeletal surveys were positive for respectively 15/45 (33%), 2/36 (6%), and 0/29 (0%). Degraw et al. studied a group of 97 children, under the age of 24 months, with burns who were referred for subspecialty child abuse evaluation [18]. Of these 97 children 18 (18.6%) were found to have occult fractures on the skeletal survey. In the second group it is a well-known fact that in children who have parents with illicit drug use there is a higher risk for child abuse [19,20,21]. Howell et al. studied the yield of skeletal surveys in a group of 1252 children referred to their C.A.R.E. Team for drug endangerment. Of these children, 340 underwent a skeletal survey with 12 (4%) positive cases [19].
Studies have shown that physicians dealing with suspicions of child abuse are of the opinion that when one child of a family is abused, this is sufficient reason to subject the other children in the family to medical examination (Fig. 3.3a, b) [22]. In a retrospective analysis of 759 siblings of 400 index children, it appeared that in 37% of cases abuse was directed to all children and in 20% to one or several children in the family [23]. In a more recent study Lindberg et al. found that in a population of 134 siblings of index children referred to child advocacy teams, under 24 months of age, that in 16 (11.9%, 95% CI 7.5–18.5) at least one abusive fracture was diagnosed [24]. It is of interest to note that in none of these children associated findings were present on physical examination. Furthermore, they found that twins were at increased risk compared to nontwin contacts (odds ratio 20.1, 95% CI 5.8–69.9). The authors of this study concluded that ‘A skeletal survey should be obtained in the contacts of injured, abused children for contacts who are <24 months old, regardless of physical examination findings’. This is in keeping with the current protocol of the Royal College of Radiologists.
Sometimes the question arises whether or not to perform a skeletal survey in children aged over 24 months of age. A study by McNamara et al. showed that out of 325 skeletal surveys performed in children over 24 months of age (mean age 37.2 months, SD 16.5) 88 (27.1) were positive [25]. Of these, 88 showed known fractures only, in 1 case the authors state ‘fracture without enough information’ and in only 6 (2%) cases occult fractures were found. Of these 4 cases were physically abused, where in each case the diagnosis was already made, and in 2 cases a fall from a window caused the fractures. This study shows that in individual cases a skeletal survey over the age of 24 months can be obtained but the expected yield is low.
3.2.2 Adequacy of Examination
3.2.2.1 Number of Views
When child abuse is suspected, and the decision is made to continue with radiological examination, this should be conducted adequately. It should first be established that in young infants the so-called babygram (consisting of one anterior-posterior view and one lateral view) of the skeleton should be considered obsolete and an error of judgement (Fig. 3.4a, b). In diagnostic radiology, a babygram is inadequate when child abuse is suspected [26]. According to professional standards, this radiograph, preferably made on a mammograph, is only admissible in premature foetuses in which imaging is otherwise impossible.
It regularly happens that the radiological examinations performed do not meet the required standard. Offiah and Hall studied the quality of radiological examinations performed within the scope of child abuse that were submitted for re-evaluation to Great Ormond Street Children’s Hospital (London, UK) [13]. They used three exclusion criteria:
-
Examinations in which only a selection of the produced radiographs was submitted for re-evaluation.
-
Examinations of less than three radiographs (excluding babygrams).
-
Examinations of children ≥2 years.
In total they admitted the skeletal surveys of 50 consecutive children to their study. Per child an average of 10 [2,3,4,5,6,7,8,9,10,11,12,13] radiographs were made. Hereby it should be mentioned that a professionally executed skeletal survey comprises 18–19 radiographs. In total, Offiah and Hall found 37 different combinations, including five babygrams. None of the examinations met the required standard. In general, hands and feet radiographs were absent. A study of Kleinman et al. from the United States confirmed the findings of Offiah and Hall [12]. As part of their study they inquired, by means of a questionnaire, in 155 paediatric hospitals which radiological protocol was used when child abuse was suspected. Of the 155 hospitals, 69% returned the questionnaire. Of these responders, 90.7% were members of the Society for Pediatric Radiology (SPR). Here too, a large variety was seen in the number of radiographs made. Van Rijn et al. evaluated the Dutch practices with regard to the radiological examination used in suspected child abuse, and found that only 7% of the reviewed skeletal surveys complied with the ACR criteria [14].
Hulson et al. performed a web-based survey among members of the European Society of Paediatric Radiology and found a considerable difference in practice across Europe, this was however before the ESPR adopted the guidelines of the Royal Collage of Radiologists [27]. Swinson et al. studied the effects of the publication of the guidelines of the British Society of Paediatric Radiology (followed by the guidelines for The Royal Collage of Radiologists and the Royal College of Paediatrics and Child Health) and compared their findings with the earlier-mentioned article of Offiah and Hall [28]. Their study still showed a considerable deviation in imaging, but significantly less so than in the earlier study. The publication of guidelines and education of the physicians involved seem to have a positive effect on the quality of imaging in cases suspected of child abuse. The same finding was reported by Patel et al. who evaluated the quality of radiographs in the skeletal surveys and found an improvement in the content of skeletal surveys [29]. More recently, Wanner et al. conducted an intervention study among members of the ACR in 69 different referring hospitals [30]. During this study they showed that after a 21-month intervention period there was a significant improvement in the total number of compliant views per skeletal survey.
3.2.2.2 Technique
Not only is it essential that the examination is complete, the techniques used are also of great importance.
When film-screen combinations are still used, a film with a speed of maximal 200 and a resolution of at least 10 line pairs per millimetre should be employed. The use of a grid is undesirable. When digital radiology is used (CR/DR), the optimal parameters for imaging a child skeleton should be chosen. When the radiograph is made, the extremities should be fully extended. Up to the present, the influence of digital radiology on the detection of subtle anomalies has not been investigated yet.
In view of the social and medical/legal implications, in this examination quality is of the essence. For this reason it is advised to perform this examination during office hours, unless a medical indication necessitates acute execution of the examination. In all cases, the (paediatric) radiologist must see the radiographs immediately after they have been made. The patient is only allowed to leave the department after the radiologist has approved the examination and decided that no additional views were required.
The examination should be performed by at least two radiographers. From a judicial point of view, it is important that they can be traced via the initials on the radiographs. The radiology report needs to be complete and all abnormalities must be reported separately; furthermore, attention should be paid to dating the abnormalities (see Chap. 11). Finally, the report must systematically describe all findings in an orderly fashion and state whether the reported anomalies are suspect for inflicted injuries and whether it concurs with the provided clinical information.
When the complete skeletal survey confirms suspected non-accidental fractures, or when anomalies suspect for non-accidental fractures are found in routine radiographs of the child, this should be explicitly mentioned in the conclusion.
3.2.2.3 Technical Shortcomings in Making a Skeletal Survey
Even when the skeletal survey is made according to valid guidelines, there will be technical shortcomings that will complicate the evaluation or make it impossible to evaluate the radiological examination. In the retrospective study of Offiah and Hall it was shown that 35% of all images showed an artefact [13]. The most prevalent mistake was the presence of a hand to steady the child (32%). Other artefacts were e.g. the presence of drip-lines, buttons, and identification bracelets. In the study of van Rijn et al., artefacts were also frequently seen (17.5% of all radiographs); in these cases, the researchers frequently saw hands, drip-lines, diapers, and bracelets (Fig. 3.5a–h) [14].
(a) The hands of the radiographer are projected over the proximal femur metaphysis. (b) Although the gastric tube and trachea cannula cannot be removed, one should remove all other lines (situated outside the patent) as much as possible. (c) The diaper is clearly visible (asterisk) and can adversely influence the diagnosis. In spite of the presence of the diaper, a healing metaphyseal corner fracture with callus formation can be seen along the femoral shaft (open arrow). (d) Identification bracelet that nearly covers the distal metaphysis of the radius. (e) The position of the pulse oximeter makes it impossible to evaluate the phalanges of digits 3–5 of the foot. (f) Bandage used to stabilize the drip makes it impossible to evaluate the distal tibia and fibula. (g) Press studs of a baby suit projected over the left costal arch. (h) On the left side a radiograph of the dressed arm and on the right side the same arm after undressing, note the wrinkles of clothing that could cover or mimic a subtle fracture
It should be mentioned that when a child dies while hospitalized, it is not allowed to remove the drip-lines and tubes that have been inserted by physicians before autopsy (Fig. 3.6a, b). In this case, their presence on the skeletal survey is not considered to be a technical shortcoming.
3.2.2.4 Follow-Up Skeletal Survey
When a radiograph of a tender area found at physical examination does initially not show any anomalies, a follow-up radiograph after 2 weeks is indicated to show or exclude callus formation or a subperiosteal haemorrhage or an epiphyseal injury without dislocation (Fig. 3.7a, b). In the new RCR guideline, a limited follow-up skeletal survey is proposed (Table 3.1). In this follow-up skeletal survey, all abnormal or suspicious areas on the initial skeletal survey are visualized as well as a limited set of additional radiographs. Using this approach a significant reduction in radiation exposure is achieved.
(a) Initial chest radiograph shows an acute angle at the lateral aspect of the sixth rib on the left. On the right side a pleural thickening is seen. (b) Repeat radiograph after 14 days clearly shows callus formation on the lateral aspect of the third to sixth rib on the right and the fourth to seventh rib on the left
As early as 1996, Kleinman et al. described this positive effect in their study that comprised 23 children who had sustained fractures [31]. In 61% of children, additional information was found. The number of confirmed fractures went up from 70 to 89, an increase of 27% (p = 0.005). According to Kleinman et al., repeating the examination also assisted in the dating of a number of fractures. Unfortunately, they did not mention which data they had used in this case [32].
Zimmerman et al. described the results of follow-up examinations in 48 patients [33]. In 46% of cases, the follow-up examination provided additional information. In 11 children, 27 fractures were found that had not been diagnosed earlier. These were mainly rib fractures (51%) and metaphyseal corner fractures (11%). Furthermore, in 15 children ambiguous anomalies were confirmed. In one child, in whom ambiguous fractures of the three metatarsals were seen, no indications for fractures were seen at follow-up examination. Consequently, the suspicion of child abuse could be rejected.
Harper et al. found that in a series of 796 follow-up skeletal surveys a total of 174 (21.5%) had new findings [34]. This included at least one new fracture detected in 124 cases (15.6%) and 55 cases (6.9%) where the findings were reassuring compared to the initial skeletal survey. The follow-up skeletal survey frequently affected the perceived likelihood of physical abuse.
3.3 Bone Scintigraphy
Bone scintigraphy should not be used as an initial imaging technique in diagnosing child abuse (Fig. 3.8a–d). According to the guidelines of the ACR and RCR-SCoR, bone scintigraphy is only indicated when, after a full skeletal survey in which no anomalies are found, the presence of non-accidental fractures is still suspected [7]. It should be kept in mind that with the decreasing use of bone scintigraphy in children due to replacement by PET-CT or MRI, the experience in reading these studies also diminishes. This can result in less reliable outcomes of bone scintigraphy studies in daily practice.
(a) Three-month-old infant that had been presented at the emergency department with a swollen right knee. The radiograph shows a classic metaphyseal corner fracture (see inset); however, this had not been interpreted as such. (b) Bone scintigraphy, made the day after the radiograph, shows increased up-take around the right knee (open arrow). (c) Bone scintigraphy also shows increased up-take in the right proximal humerus (open arrow). This was not radiographed. (d) Five weeks after the initial examination, the patient presented again at the emergency department. However, this time she is in coma. A CT of the brain shows a subdural haemorrhage (open arrow) and bilateral diffuse ischaemic injuries
Drubach et al. proposed the use of 18F-NaF PET in the diagnosis of occult fractures [35]. In a study of 22 patients younger than 2 years, they showed that the conventional skeletal survey showed a total of 156 fractures versus 200 fractures with 18F-NaF PET. 18F-NaF PET had a higher sensitivity for rib fractures but a lower sensitivity for metaphyseal corner fractures. Since this publication, to the best of our knowledge, no other 18F-NaF PET studies in the field of suspected child abuse have been performed.
3.3.1 Effectivity of Bone Scintigraphy Versus Conventional Radiology
There are several publications which looked at the additional value of bone scintigraphy compared to a skeletal survey [36,37,38,39,40,41,42].
On behalf of the Welsh Child Protection Review Group, Kemp et al. compared the effectivity of bone scintigraphy and conventional radiology in cases of suspected child abuse [43]. Based on mainly case reports/series they came to the following conclusions: fractures will be overlooked in conventional radiology as well as in bone scintigraphy, bone scintigraphy is very sensitive for the detection of rib and acute fractures, whereas these may be overlooked in conventional radiology. And, when using bone scintigraphy, skull fractures, metaphyseal and epiphyseal fractures may be overlooked.
In a systematic review, Blangis et al. evaluated studies which assessed the value of bone scintigraphy after an initial negative skeletal survey, in total seven studies (with a total of 783 children) were included [44]. Based on the included studies, the authors concluded that a bone scan after a negative skeletal survey increased the summary absolute detection rates with an estimate of 10 percentage points. In approximately half of the children in whom non-accidental skeletal injuries were suspected the initial skeletal survey was negative. The summary number needed to scan with bone scintigraphy to detect one additional child with skeletal injury was 3. It is important to state that there was no assessment of the added value of bone scintigraphy to, as the standards dictate, a follow-up skeletal survey. Also looking at the included studies most studies suffered from methodological issues, e.g. retrospective, unclear patient selection and risk of inclusion bias. As a result the authors state that ‘The quality of the reviewed evidence was low, pointing to the need for high-quality studies in this field’ [44]. So if this approach would be implemented it is to be suspected that the yield of bone scintigraphy would than be lower. Therefore, for now there is no indication to deviate from the ACR and SCR-SCoR guidelines and use bone scintigraphy, as a problem solving tool, only in exceptional cases.
3.4 Computed Tomography
Nowadays, CT is increasingly used in the primary evaluation of trauma victims. By now, studies in adults have shown that by using this technique relevant pathology will be found with a higher sensitivity and specificity, which leads to a significant improvement in the patient’s prognosis [45,46,47,48]. However, in suspected child abuse CT in general has no place in the primary detection of occult fractures. A substantial percentage of fractures seen within the scope of suspected child abuse, e.g. rib fractures or CMLs, have neither from a diagnostic or a therapeutic point of view any need for additional imaging. The exception to this rule are fractures of the vertebrae, where it is essential to establish fracture stability. In these cases, in order to make a proficient evaluation, CT is required since this technique provides information on the stability of all three pillars of the spinal column.
Having said this CT has shown to be valuable in several anatomic areas which are relevant to potential child abuse cases, this is especially the case for rib and skull fractures. In recent years there have been several publications on the use of CT of the chest in the diagnosis of rib fractures, although there remains a discussion whether or not this should be done [49,50,51,52]. Sanchez et al., in a retrospective study, looked at 16 children under the age of 12 months with a total of 105 rib fractures [50]. Of these fractures 84% were seen on the first skeletal survey and 16% only after follow-up imaging, of which 11 out of 18 rib fractures were only seen on CT. Shelmerdine et al. retrospectively looked at 25 paired post-mortem skeletal surveys and post-mortem CT scans in a study population aged 1 month to 7 years [52]. In their study they found a total of 136 rib fractures at autopsy, three times as many rib fractures were correctly identified on CT compared to the skeletal survey (sensitivity 44.9% [95% CI 31.7–58.9] vs 13.5% [8.1–21.5]; difference 31.4% [23.3–37.8; p < 0.001]). Radiologists also reported a higher confidence when reporting on CT compared to the skeletal survey. In light of the radiation exposure of the chest CT, with the potential detrimental long-term consequences, it is not yet advised to perform a chest CT instead of the four-view chest radiographs. More research into the validation of low-dose chest CT scans is needed before routine chest CT imaging can be recommended.
In neurotrauma, CT is widely used for the primary evaluation of the patient. Over the past few years, authors in the radiological and paediatric literature increasingly argue the case for a standard head CT in all children of ≤2 years old who are suspected of being physically abused (Fig. 3.9) [53]. As CT is used more frequently, the question arises if conventional radiography of the skull is still needed. Culotta et al. performed a retrospective study in 167 children (median age 5 months) who were evaluated for potential AHT [54]. They found no significant difference (p = 0.18) between conventional radiography and CT. Sharp et al. performed a retrospective study in 94 infants (aged 24 days–23 months) in whom there was a suspicion of child abuse and in whom both conventional radiographs and CT of the head were made [55]. They found that in none of the cases conventional radiographs added findings over the findings on CT. Martin et al. performed a retrospective study in which they compared conventional radiographs, CT without 3D reconstruction, and CT with 3D reconstruction [56]. They found that CT with 3D reconstruction had a 100% sensitivity, specificity, PPV, and NPV (Fig. 3.10a, b). Based on these results the authors concluded ‘Conventional radiographs (SRX) does not add further diagnostic information and can be omitted from the skeletal survey when CT with 3D reconstruction is going to be, or has been, performed’. Penell et al. evaluated data from 158 infants who underwent both skull radiography and CT [57]. In their study population, they found 46 skull fractures on 3D CT and 40 on skull radiographs. The interrater reliability was higher for 3D CT (κ = 0.95) compared to skull radiographs (=0.65). Even though 5 fractures were identified on skull radiographs only, whereas 11 fractures were identified on 3D CT only, the authors concluded that omitting the skull radiograph is justified when a 3D CT of the skull is obtained. In an older study, Orman et al. retrospectively reviewed 250 paediatric cases (mean 7.82 years, range 4 days–17.4 years) with linear skull fractures on consensus reading by two experienced paediatric neuroradiologists [58]. Three reviewers (a third year resident, a fellow in neuroradiology, and a paediatric neuroradiologist) first reviewed the 2D dataset and later a combined 2D/3D dataset. They found that the combination of 2D&3D had a superior sensitivity and specificity (83.9% and 97.1%) compared to 2D only.
Based on this literature omitting the conventional skull radiographs, if a sufficient CT including 3D reconstructions is available, can be considered in cases of suspected child abuse.
3.5 Linear Slot Scanning
A relatively unknown and new technique, marketed as Statscan® (Lodox Systems, [Pty] Ltd., Sandton, South Africa), is linear slot scanning [59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]. The Statscan® was initially developed to detect diamond smugglers working in the South African diamond mines [70, 74]. Since approximately 2000 it is also used in a trauma setting and in forensic facilities. This technique allows for full body imaging; for this a C-arm traverses the patient trolley along the Z-axis. As the C-arm can rotate up to a maximum angle of 100°, lateral and oblique radiographs are also possible (Fig. 3.11a, b). The system uses a collimated fan-beam and a linear bank of CCD cameras as a detector. The acquisition time of a scan is approximately 13 s [72]. Compared to a full skeletal survey (in adults) the dose has been reported to be 65.0% to 94.0% less [72, 75]. Currently it has a noticeable install basis in the Southern part of Africa and in medical examiners offices throughout the United States [76].
There have been a few small studies into the use of Statscan in the paediatric trauma population [67, 68, 73]. The largest reported series is on 23 children where the AP linear slot bodygram showed 26 of 27 fractures (96%) in the study cohort. There is however no evidence with respect to the detection of, e.g. posterior rib fractures and metaphyseal corner fractures. In adults, a retrospective study in 245 consecutive trauma cases showed an overall sensitivity of 73% and a specificity of 100% [59]. However, in 50% of cases additional radiographs were obtained to provide a more detailed or an additional view for pre-operative planning. Spies et al. performed a post-mortem animal study using piglets comparing conventional radiology, Lodox, and CT to assess the sensitivity of Lodox for fracture detection [77]. A total of 586 fractures were created by blunt force trauma in 10 piglets, of which CT correctly detected 427 (73%), X-ray 294 (50%), and Lodox 245 (42%). Looking at just the ribs CT was most sensitive (84%) and Lodox least sensitive (50%).
Based on the literature evidence it could be concluded that if no CT scanner is available or to costly to acquire, linear slot scanning can be used to diagnose major trauma findings. For the detection of subtle fractures, dedicated spot radiographs will remain essential.
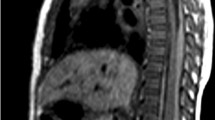
3.6 Magnetic Resonance Imaging
Up to the present, MRI is not widely used in the initial diagnosis of suspected child abuse. MRI is essential as a second stage imaging method in order to determine the prognosis in severe neurological trauma in intracranial as well as in spinal injuries (Fig. 3.12). In abdominal trauma, and more specifically in pancreatic injuries, MRI/MRCP may provide additional information on the intra-abdominal parenchymal organs (Fig. 3.13a, b).
With respect to fractures the use of MRI is limited. However, due to the relatively short scan times available in Short T1 Inverse Recovery (STIR), whole body imaging of children is possible. STIR is a sequence that yields a uniform fat suppression in the field of view leading to increased visualization of, e.g. bone marrow oedema. Clinical paediatric radiology has shown whole body STIR (WB-STIR) to be a sensitive technique for the detection of, e.g. bone metastases or foci of non-bacterial osteitis (Fig. 3.14a, b) [78,79,80,81,82,83,84,85,86]. Some authors suggest the use of WB-STIR for the detection of occult fractures in suspected child abuse (Fig. 3.15a–c) [33, 87, 88]. Besides a few case reports in which this technique has been described, two studies have been published in which WB-STIR and conventional skeletal surveys were compared [89, 90]. The first study comprised 16 children (average age 9 months; range: 1.5–37 months) that were suspected of being abused. The average time interval between WB-STIR and conventional skeletal survey was 1.9 days (range: 0–13 days). The sensitivity of WB-STIR for rib fractures was 75% (33/44), CML 67% (2/3), metaphyseal fractures 100% (1/1), diaphyseal fractures 100% (6/6), and parietal skull fractures 100% (1/1). In total, 11 rib fractures were overlooked. However, all children had sustained multiple fractures and at least one rib fracture was detected by WB-STIR. In three children, WB-STIR showed fractures that had not been visible on the conventional skeletal survey. In the second study, the authors evaluated the additional value of WB-STIR and bone scintigraphy in addition to the initial conventional skeletal survey [90]. In this study 107 children under the age of 3 years who were suspected victims of child abuse were included. In this study, the skeletal survey had the highest sensitivity and specificity (88.4% [95% CI 82.0–93.1%] and 99.7% [95% CI 99.5–99.8%]), followed by WB-STIR (69.9% [95% CI 61.7–77.2%] and 99.5% [95% CI 99.2–99.7%]) and bone scintigraphy (54.8% [95% CI 46.4–63.0%] and 99.7% [95% CI 99.5–99.9%]). The combination of the skeletal survey and WB-MRI had the highest sensitivity (95.9% [95% CI 91.3–98.5%]) and the combination of the skeletal survey and bone scintigraphy had the highest specificity (99.4% [95% CI 99.2–99.6%]). Based on their findings the authors concluded both WB-STIR and bone scintigraphy can be used in case of equivocal lesions. In many infants who are suspected to be a victim of child abuse MRI of the brain and spine will be obtained, and in these cases WB-MRI could be used as an ‘add-on’ to the standard brain and spine.
(a) Two-month-old infant with severe inflicted traumatic brain injury. The diffusion-weighted views show areas of severe cytotoxic oedema (open arrow) resulting from hypoxia. (b) Cor STIR-weighted view of the chest shows increased signal intensity at the site of the seventh left rib (open arrow). This corresponds with a fresh fracture. (c) Oblique chest view, made 6 days after the MRI, shows callus formation at the site of the seventh left rib (open arrow). Furthermore, there are fractures visible at the costochondral junctions of ribs 7 and 8 (see inset)
A relatively new development in the field of MRI is the use of the so-called ‘black bone’ sequence [91,92,93]. In 2012, Eley et al. were the first to present this sequence which consists of a low flip angle gradient echo MRI sequence providing high image contrast between bone and other tissues while at the same time reducing the contrast between soft tissues. There are only a handful of studies which have evaluated the sensitivity and specificity of this sequence compared to cranial CT as a gold standard. Dremmen et al. showed in a study of 28 children that ‘black bone’ MRI had a lower sensitivity (66.7% versus 100%) and specificity (87.5% versus 100%) (Fig. 3.16a–c) [94]. In a more recent study by Kralik et al., ‘black bone’ MRI showed an 83% sensitivity (95%[CI] 36–99%) and a 100% specificity (95%[CI] 88–100%) [95]. To date the evidence is insufficient to advocate replacing CT by ‘black bone’ MRI for the diagnosis of skull fractures.
(a) Infant with a right parietal skull fracture (arrow) with overlying haematoma. (b) Corresponding black bone sequence shows the fracture as well (arrow). (c) The inverted image shows an imaging resembling a CT scan (courtesy of M.H.G. Dremmen MD. PhD., Sophia Children’s Hospital, Erasmus MC+, Rotterdam, the Netherlands)
3.7 Ultrasonography
In recent years, there have been some publications on the use of ultrasonography (US) in the diagnosis of fractures, due to non-accidental circumstances [96,97,98,99,100].
Marine et al. presented a descriptive retrospective study in 22 patients who had, based on the skeletal survey, a total of 39 CMLs [96]. In their population in 85% of cases the US exams were abnorma. The authors concluded that ‘while a negative US does not exclude CML, US may have a role in either confirming or evaluating radiographically equivocal CMLs’. A recent retrospective study in 63 children by Karmazyn et al. focused on the accuracy of US for CMLs [97]. In this study, both in a group of children in whom the diagnosis CML was in doubt and in a group of children with radiologically proven CMLs US of the lower extremity was performed. Based on their findings the authors concluded that ‘US has low sensitivity and high specificity in the diagnosis of CMLs in the lower extremities’ and that ‘US for CML may help substantiate the diagnosis’ (Fig. 3.17a, b).
There are two publications on the use of US in diagnosing rib fractures, the first is by Kelloff et al. who describe a case of a 9-week-old infant [99]. The attending physician noted crepitus of the chest on physical exam and when the chest radiographs, including the obliques, were negative US was used as a problem solver. The follow-up skeletal survey showed healing rib fractures of the left sixth and seventh posterolateral ribs and right seventh, eighth, and ninth anterolateral ribs. Smeets et al. reported on a 9-month-old girl that on a skeletal survey showed multiple healing rib fractures [100]. A soft tissue swelling was noted on the left lateral thoracic wall. US of this area revealed a subcutaneous haematoma overlying costochondral dislocations of all left lower ribs (Fig. 3.18a, b).
3.8 Bone Densitometry
In children presenting with fractures, the question of bone density in relation to bone fragility is often raised. In a publication from 1936 by Lachmann and Whelan, the authors stated that at least 20–40% of bone mass should be lost before it is visible on conventional radiography [101]. This is often mentioned in presentations and in court proceedings. However, the authors performed their experimental work on cadaveric bones and using film-screen combinations. The question is if this also applies to modern techniques and children. Recently, Rosendahl et al. performed a systematic review which addressed this question [102]. In their study, they couldn’t find any evidence to support the statement that before it is noticeable on conventional radiography that 20–40% bone mass should be lost. Therefore, in order to make a statement on bone mass bone densitometry is necessary. Within the world of bone densitometry historically the focus has been on middle aged women suffering from age-related osteoporosis, all techniques have been developed and initially validated for use in this specific population. However, once these techniques became more readily available it also found its way into the field of paediatrics.
The use of bone densitometry techniques in children is, without proper knowledge of its limitations, not without risks [103]. One of the obvious differences between adults and children is the propensity to grow for the latter group. As growth is a volumetric process techniques using a two-dimensional approach have the inherent problem of not only measuring a change in bone mass but also a change in size.
If bone densitometry is performed, the outcome of the study should not be reported as the T-score, as is customary in adults. In children the Z-Score should be adopted, this score not only adjusts for sex and racial background but also for age. One problem is that Z-score reference curves are in general only available for children aged 5 years and over, making it not useful for the age range in which children who are subject to physical child abuse tend to be [104, 105].
There are multiple techniques available to assess bone density, e.g. Dual-Energy X-ray Absorptiometry (DXA), Quantitative UltraSound (QUS), Digital Radiogrammetry (DXR), and Quantitative Computed Tomography (QCT) (Table 3.2) [106,107,108]. Of these, DXA is most widely in use and its use in children is recommended by the PDC. This technique measures bone mass as Bone Mineral Content (BMC, gram), Bone Mineral Density (BMD, gram/cm2), or the derivative Bone Mineral apparent Density (BMaD, gram/cm3) (Fig. 3.19).
With respect to reporting bone densitometry studies, the PDC states that terminology like ‘T-score’, ‘Osteopenia’, and ‘Osteoporosis’ based on densitometry studies only cannot be used in children. This as these terms are developed for studies in adult women. Therefore, in 2013 PDC revised the clinical criteria for the definition of osteoporosis in paediatrics. In this they defined osteoporosis as the finding of one or more vertebral compressions fractures (VCF) in the absence of local disease or high energy trauma, independently of densitometric results. Moreover, it was confirmed that, in the absence of VCF, only the combination of both a reduced bone mass for age and sex [BMC or BMD below 2 Z-score at the spine (L1–L4) and/or at the total body less head] and a significant history of fragility fractures (2 or more or 3 or more respectively by the age of 10 or below 19 years of age) is indicative of osteoporosis [109]. This statement is mainly supported by expert’s opinion as the quality of evidence unfortunately was rated low.
A second aspect of reporting bone densitometry studies is the question whether the measurements should be corrected for length, body mass, skeletal age, or pubertal stage. This is especially the case in children with an underlying disease affecting one or more of these parameters. However, for every potential correction a potential error is also introduced. It is therefore important that the clinician who requests a bone densitometric study realizes the advantages but also the drawbacks of bone densitometry.
Finally and perhaps most important is the relation of fracture risk based on the bone densitometry findings. Although in adults a lot of strong evidence with respect to the predictive value of bone densitometry has been published, this is not the case for paediatrics [110,111,112]. Given the lack of consensus and limited amount of evidence, it would be unwise to use the outcome of bone densitometry studies as foundation for legal reports.
3.9 Post-Mortem Imaging
When a child dies suddenly and unexplained or in case of suspected unnatural death, the use of imaging techniques is part of the standard procedures of the post-mortem examination. The examination is of importance in the death of each minor. Although in physical child abuse skeletal lesions rarely have a life-threatening character, during autopsy they often are one of the strongest radiological indicators of physical child abuse. In all cases of sudden unexpected death in infancy (SUDI) defined as ‘All cases in which there is death (or collapse leading to death) of a child, which would not have been reasonably expected to occur 24 h previously and in whom no pre-existing medical cause of death is apparent’, post-mortem skeletal imaging according to the RCR guideline is mandatory. This can be complemented by a CT scan and/or MRI, even if an autopsy will be performed. The radiological examination is a very valuable addition to the autopsy and may direct the investigation [113, 114]. In the Netherlands, an evidence based national guideline for post-mortem imaging in a clinical setting of SUDI has been published [115, 116]. Although this guideline was specifically developed for a clinical setting, it can of course also be applied to a forensic medical setting. Recently, the European Society of Paediatric Radiology and the International Society of Forensic Radiology and Imaging issue a joint statement on a PMCT protocol [117] (Fig. 3.20). As mentioned earlier in this chapter, the so-called babygram (one single overview or two views) of the skeleton in young infants was shown to be inadequate when child abuse is suspected [26]. This examination should be considered obsolete, also in post-mortem evaluation. It is of interest to note that a 2009 American survey study into the use of skeletal surveys in a forensic post-mortem setting yielded rather poor results [118]. Of the respondents 29% reported the routine use of a babygram, 73% only 1–5 views, and only 5% more than 16 views. There thus seems to be a large discrepancy between the clinical setting and the post-mortem forensic setting.
Graphic representation of the post-mortem CT protocol as proposed by the European Society of Paediatric Radiology and the International Society of Forensic Radiology and Imaging [117]
During a full autopsy of a child, conspicuous fractures such as skull fractures or fractures of the long bones will generally not be overlooked. However, there is a greater risk that the more subtle skeletal anomalies may be overlooked, such as a CML, since the ends of the long bones are not routinely inspected at autopsy. There is also a reasonable chance that rib fractures (especially when located on the posterior side) will be overlooked [119].
When the sudden and unexplained death occurred in non-accidental circumstances, e.g. physical child abuse, it is not rare to find signs of earlier injuries at post-mortem radiological examination [120]. In a retrospective study of McGraw et al. of 106 consecutive post-mortem skeletal surveys, 14 children showed signs of inflicted skeletal injuries [121]. Sperry and Pfalzgraf describe a 9-month-old child whose death was initially contributed to cot death [122]. However, post-mortem examination showed healing clavicle fractures and a healing fracture of the humerus on the left. Extensive investigation revealed that 4 weeks prior to death a non-qualified chiropractor had treated the child for a ‘shoulder dislocation’. It was very likely that this treatment was the cause of the fractures. Also, Ojima et al. describe the finding of fractures in a child who died suddenly and unexplained [123]. This child had undiagnosed osteogenesis imperfecta.
When it is decided that post-mortem examination with radiological techniques will take place, this should always happen prior to autopsy. It is important to recognize that imaging deceased children, due to rigor mortis or the legal inability to remove foreign objects, can present with difficulties and that the resulting quality can be lower compared to imaging a living child [124]. Preferably the images are evaluated by an experienced paediatric radiologist before the pathologist starts the autopsy. This enables the pathologist to take the radiological findings into consideration. Sometimes the pathologist will find fractures at autopsy that were not visible on the radiographs. When this is the case, the bone may be removed in its totality and be subjected to specimen radiography [125]. Specimen radiography should preferably be performed on a high-resolution system; in general a mammography system is the technique of choice (Fig. 3.21a–d).
(a) Chest radiographs shows multiple rib fractures with callus formation, among others on the lateral aspect of the fourth left rib (inset). (b) CT of the chest clearly shows the rib fracture of the fourth left rib. (c) 3D reconstruction of the chest in a bone window showing the rib fracture of the fourth left rib. (d) Specimen radiograph clearly shows the rib fracture of the fourth left rib (arrow) but also a healing fracture of the neck of the fourth right rib (inset)
An important development in clinical and forensic pathology is the use of post-mortem CT (Fig. 3.22a–c) and MRI (Figs. 3.23a, b and 3.24a, b) [126,127,128]. The use of these, clinically widely used, techniques is evident; also, for laymen it produces (when reconstructions are used) an image they can understand, and that is suitable for presentation in court cases. Furthermore, it provides calibrated three-dimensional measurements and long-term storage of images. However, post-mortem imaging also has its disadvantages. Firstly, obviously there is no blood circulation, which makes it difficult to use contrast media. A possible solution to this problem has been developed by the ‘Virtopsy project’ in Bern, where after perfusion with paraffin oil and with the use of a heart-lung machine it was still possible to produce an angiography [126]. A second, even more important problem is the interpretation of the CT and MRI images. Where radiologists are experienced in evaluating the images of living patients and pathologists are experienced in the performing and interpreting autopsies, there is little or no overlapping knowledge. This may lead to problems in interpretation; for example when air is seen in the portal system (Fig. 3.25). In living patients this is a rare finding, but in post-mortem CTs of critically ill patients, this is regularly found. Shiotani et al. described portal air in 33% of 190 post-mortem CTs [129].
(a) Found demised neonate, PMCT shows gasless lungs as a sign that the neonate died in utero. (b) 3D reconstruction shows a normally developed skeleton. (c) Based on the length assessment of the left femur the gestational age was calculated to be 37 weeks (SD 2.1 weeks) [151]
(a) Deceased neonate, found in a refuse container. Post-mortem T2-weighted MRI shows oedema around the blood vessels in the neck (open arrow). Also, the neonatal anatomy is clearly visible. (* = thymus; L = liver; S = stomach; arrow = right atrium; arrow point = umbilical cord) (b) Autopsy (seen from above) shows a haematoma around the blood vessels on the right side of the neck (open arrow), possibly the result of strangulation
To date most forensic PMCT studies have focused on the adult population [130,131,132]. Most paediatric post-mortem studies have focused on a very young population, including foetuses, making use of PMMRI which makes it difficult to incorporate their findings in a forensic setting [133].In children there only have been a few studies published on the use of PMCT in a forensic setting [134,135,136,137]. These three studies have shown somewhat conflicting results with respect to the sensitivity and specificity related to the cause of death. In a series of 18 children under the age of 2 years, in whom a cause of death was found at autopsy, Proisy et al. found that this was in accordance with PMCT in 15 cases (83%) [135]. Krentz et al. reported on a series of 26 children aged 0–12 years; in this series consisting of a mix of cases useful findings were more frequently detected by autopsy compared to PMCT (192 out of a total of 244 findings) [134]. Sieswerda et al. reported on a series of 98 children where CT and autopsy identified the same cause of death in 66/98 cases [136]. They found an important influence of the case mix with respect to the concordance between PMCT and autopsy, 59–67% concordance in unnatural deaths compared to 0% agreement to natural deaths. More recently, Shelmerdine et al. performed a retrospective study in 136 cases, 74 (54.4%) boys and 62 (45.6%) girls with a mean age of 2 years and 1 month (range: 2 days–14.7 years) [137]. In 77 cases, autopsy revealed a definitive cause of death; of these cases in 55 (71.4%) PMCT had a similar cause of death. For the whole population PMCT identified 40.4% (55/136) of the main pathologic findings. In this mixed study, containing unexplained deaths as well as forensic cases, there were depending on body area varying diagnostic accuracy rates. There were high diagnostic accuracy rates for neurologic findings (75.6%) and musculoskeletal findings (98.4%), whereas there were significantly lower rates for thoracic (64.7%), abdominal (53.8%), and cardiovascular (31.3%) findings. Overall it can be concluded that in all studies PMCT excelled in the detection of skeletal pathology and autopsy excelled in soft tissue findings. Despite the differences between these studies, it can be concluded that PMCT and autopsy should be considered to be complementary modalities.
Although post-mortem radiology is still in full development, and its values and limitations will have to be proven in the future, it seems obvious that after its successful introduction into the clinic it will now also find its place in pathology.
3.10 Radiation Dose in Imaging Suspected Child Abuse
Over the past decades, there are growing concerns about the small but potential adverse effects of ionizing radiation used in medical imaging [138,139,140,141]. There are two types of adverse effects related to the use of ionizing radiation, deterministic and stochastic. Deterministic effects are characterized by a dose-related increase in risk and associated severity of outcome. They only occur above a threshold dose and examples include radiation-induced dermatitis and cataract. Stochastic effects, on the other hand, are caused by a radiation-induced mutation or other permanent change in cells which otherwise remain viable. Examples of stochastic effects include cancer and hereditary effects. The probability of stochastic effects increases with dose without a threshold, which means that even a small X-ray dose has the potential to cause a base change in DNA, and that the severity of the outcome is not related to the dose. These small but not negligible health risks of the use of ionizing radiation is of particular concern in children as their tissues are more radiosensitive than adults and they have more years ahead in which cancerous changes might occur.
The term usually used to describe the effect of ionizing radiation is ‘effective dose’, which reflects a rough estimate of the whole body dose based on summed dose values to important critical organs and tissues within the exposed body area multiplied by ICRP103 weighting factors (wT). It allows for comparison of risks among various radiological imaging techniques and is measured in units of milliSievert (mSv). There are different ways to express radiation dose such as background equivalent radiation time (BERT), critical organ dose (COD), surface absorbed dose (SAD), dose area product (DAP), diagnostic acceptable reference level (DARLing), and effective dose (ED) [142]. In explaining effective dose to parents/caretakers the easiest is to use the background equivalent radiation time (BERT), in which the exposure is compared to the annual natural background radiation exposure such as natural radioactive substances in the air, soil, and environment to which the population is exposed on a daily basis. Depending on where you live the annual background radiation exposure differs slightly, but on average this is 2.4 mSv per year [143]. There are numerous sources that expose us to radiation, in Table 3.3 some of these sources and the radiological exams used in evaluating child abuse cases are presented, Fig. 3.26 shows a break-down of the sources of natural back. The U.S. Nuclear Regulatory Commission (NRC) has an online calculator, focused on America, to calculate your personal annual radiation exposure, this might be useful in educating parents about the perceived risk of radiation [144].
Break-down of the sources of natural background radiation [152]. The first four causes are external radiation, the following two are caused by inhalation, and the last four are the result of ingestion of radio isotopes
Berger et al. investigated the effective dose of the skeletal survey based on the recommendations of the American Academy of Pediatrics and consisting of 15 different radiographs [139]. The radiographic examinations were acquired using an X-ray system with a digital flat panel detector and manually set technique factors optimized to provide a high-quality diagnostic image at the lowest possible radiation dose. Based on Monte Carlo simulations, the total effective dose of the 15 radiographs was estimated to be 0.2 mSv for both female and male infants. Similar results were found in a recent study published in 2019 by Rao et al. [141]. They investigated the effective dose of a skeletal survey compliant with the national guideline and based on the most recent ACR and RCR/SCoR guidelines. This skeletal survey included at least 14 different radiographs (19 in the absence of a paediatric radiologist), whereas the follow-up survey included fewer radiographs. The mean effective dose was 0.20 mSv (95% CI 0.18–0.22) for the initial skeletal survey and 0.10 mSv (95% CI 0.08–0.11) for the follow-up survey. They also looked at the mean effective dose of CT head, which delivered a mean effective dose of 2.49 mSv (95% CI 2.37–2.60). In a minority of patients in their study cohort a bone scintigraphy was performed, with a mean effective dose of 2.27 mSv (95% CI 2.11–2.43). Finally, in a recent newborn phantom study by Hampel et al. effective doses of approximately 0.06–0.09 mSv were found for a skeletal survey according to the RCR/SCoR guidelines [8]. Therefore, from these studies it can be concluded that (optimized) skeletal surveys deliver a relatively low effective dose of ionizing radiation, and that the benefits of early detection of physical abuse certainly outweigh the potential risks of the use of ionizing radiation. This seems to be true for the use of CT head (estimated dose 1.6 mSv [145]) in case of suspected abusive head trauma, although for non-acute head injury presentations MRI is preferred to keep the radiation dose to the child as low as reasonably achievable. In a large meta-analysis published in 2020, the authors concluded ‘no evidence of an increased risk of all cancers was observed after X-ray exposure’ [146]. For CT this isn’t so clear cut, based on pooled results from studies on CT exposure during childhood, the life risk for leukaemia and brain tumours seems higher. However, these published studies all suffer from different levels of methodological limitations and given the fact that long-term data is needed the scans were made with significantly higher radiation exposures as are used in modern day scanners. For the true impact of the life risk of cancer after diagnostic paediatric CT, we will have to wait for the results of the ongoing European EPI-CT study [147].
References
Kempe CH, Silverman FN, Steele BF, Droegenmueller W, Silver HK (1962) The battered-child syndrome. JAMA 181:17–24
Caffey J (1946) Multiple fractures in the long bones of infants suffering from chronic subdural hematoma. Am J Roentgenol Radium Therapy, Nucl Med 56:163–173
Silverman FN (1953) The roentgen manifestations of unrecognized skeletal trauma in infants. Am J Roentgenol Radium Therapy Nucl Med 69:413–427
Woolley PV Jr, Evans WA Jr (1955) Significance of skeletal lesions in infants resembling those of traumatic origin. J Am Med Assoc 158:539–543
Caffey J (1957) Some traumatic lesions in growing bones other than fractures and dislocations: clinical and radiological features: the Mackenzie Davidson memorial lecture. Br J Radiol 30:225–238
Ellerstein NS, Norris KJ (1984) Value of radiologic skeletal survey in assessment of abused children. Pediatrics 74:1075–1078
Wootton-Gorges SL, Soares BP, Alazraki AL, Anupindi SA, Blount JP, Booth TN, Dempsey ME, Falcone RA Jr, Hayes LL, Kulkarni AV, Partap S, Rigsby CK, Ryan ME, Safdar NM, Trout AT, Widmann RF, Karmazyn BK, Palasis S (2017) ACR appropriateness criteria - suspected physical abuse-child. J Am Coll Radiol 14:S338–s349
The Royal College of Radiologists (RCR) and the Society and College of Radiographers (SCoR) (2017) The radiological investigation of suspected physical abuse in children. https://www.rcr.ac.uk/publication/radiological-investigation-suspected-physical-abuse-children. Accessed 5 July 2021
Ingram JD, Connell J, Hay TC, Strain JD, Mackenzie T (2000) Oblique radiographs of the chest in nonaccidental trauma. Emerg Radiol 7:42–46
Hansen KK, Prince JS, Nixon GW (2008) Oblique chest views as a routine part of skeletal surveys performed for possible physical abuse–is this practice worthwhile? Child Abuse Negl 32:155–159
Marine MB, Corea D, Steenburg SD, Wanner M, Eckert GJ, Jennings SG, Karmazyn B (2014) Is the new ACR-SPR practice guideline for addition of oblique views of the ribs to the skeletal survey for child abuse justified? AJR Am J Roentgenol 202:868–871
Kleinman PL, Kleinman PK, Savageau JA (2004) Suspected infant abuse: radiographic skeletal survey practices in pediatric health care facilities. Radiology 233:477–485
Offiah AC, Hall CM (2003) Observational study of skeletal surveys in suspected non-accidental injury. Clin Radiol 58:702–705
van Rijn RR, Kieviet N, Hoekstra R, Nijs HGT, Bilo RAC (2009) Radiology in suspected non accidental injury: theory and practice in the Netherlands. Eur J Radiol 71:147–151
Loos MHJ, Almekinders CAM, Heymans MW, de Vries A, Bakx R (2020) Incidence and characteristics of non-accidental burns in children: a systematic review. Burns 46(6):1243
Hicks RA, Stolfi A (2007) Skeletal surveys in children with burns caused by child abuse. Pediatr Emerg Care 23:308–313
Fagen KE, Shalaby-Rana E, Jackson AM (2015) Frequency of skeletal injuries in children with inflicted burns. Pediatr Radiol 45:396–401
Degraw M, Hicks RA, Lindberg D (2010) Incidence of fractures among children with burns with concern regarding abuse. Pediatrics 125:e295–e299
Howell S, Bailey L, Coffman J (2019) Evaluation of drug-endangered children: the yield of toxicology and skeletal survey screening. Child Abuse Negl 96:104081
Wells K (2009) Substance abuse and child maltreatment. Pediatr Clin N Am 56:345–362
Kelleher K, Chaffin M, Hollenberg J, Fischer E (1994) Alcohol and drug disorders among physically abusive and neglectful parents in a community-based sample. Am J Public Health 84:1586–1590
Campbell KA, Bogen DL, Berger RP (2006) The other children: a survey of child abuse physicians on the medical evaluation of children living with a physically abused child. Arch Pediatr Adolesc Med 160:1241–1246
Hamilton-Giachritsis CE, Browne KD (2005) A retrospective study of risk to siblings in abusing families. J Fam Psychol 19:619–624
Lindberg DM, Shapiro RA, Laskey AL, Pallin DJ, Blood EA, Berger RP (2012) Prevalence of abusive injuries in siblings and household contacts of physically abused children. Pediatrics 130:193–201
McNamara CR, Panigrahy A, Sheetz M, Berger RP (2021) The likelihood of an occult fracture in skeletal surveys obtained in children more than 2 years old with concerns of physical abuse. Pediatr Emerg Care 38(2):e488–e492
Alexander R, Kleinman PK (2000) Diagnostic imaging of child abuse – portable guides to investigating child abuse. US Department of Justice, Washington
Hulson OS, van Rijn RR, Offiah AC (2014) European survey of imaging in non-accidental injury demonstrates a need for a consensus protocol. Pediatr Radiol 44:1557–1563
Swinson S, Tapp M, Brindley R, Chapman S, Offiah A, Johnson K (2008) An audit of skeletal surveys for suspected non-accidental injury following publication of the British Society of Paediatric Radiology guidelines. Clin Radiol 63:651–656
Patel H, Swinson S, Johnson K (2017) Improving national standards of child protection skeletal surveys: the value of college guidance. Clin Radiol 72:202–206
Wanner MR, Marine MB, Hibbard RA, Ouyang F, Jennings SG, Shea L, Karmazyn B (2019) Compliance with skeletal surveys for child abuse in general hospitals: a Statewide quality improvement process. AJR Am J Roentgenol 2019:1–6
Kleinman PK, Nimkin K, Spevak MR, Rayder SM, Madansky DL, Shelton YA, Patterson MM (1996) Follow-up skeletal surveys in suspected child abuse. AJR Am J Roentgenol 167:893–896
Prosser I, Maguire S, Harrison SK, Mann M, Sibert JR, Kemp AM (2005) How old is this fracture? Radiologic dating of fractures in children: a systematic review. AJR Am J Roentgenol 184:1282–1286
Zimmerman S, Makoroff K, Care M, Thomas A, Shapiro R (2005) Utility of follow-up skeletal surveys in suspected child physical abuse evaluations. Child Abuse Negl 29:1075–1083
Harper NS, Eddleman S, Lindberg DM (2013) The utility of follow-up skeletal surveys in child abuse. Pediatrics 131:e672–e678
Drubach LA, Sapp MV, Laffin S, Kleinman PK (2008) Fluorine-18 NaF PET imaging of child abuse. Pediatr Radiol 38:776–779
Blangis F, Poullaouec C, Launay E, Vabres N, Sadones F, Eugène T, Cohen JF, Chalumeau M, Gras-Le Guen C (2020) Bone scintigraphy after a negative radiological skeletal survey improves the detection rate of inflicted skeletal injury in children. Front Pediatr 8:498
Haase GM, Ortiz VN, Sfanakis GN (1980) The value of radionuclide bone scanning in the early recognition of deliberate child abuse. J Trauma 20:873–875
Sty JR, Starshak RJ (1983) The role of bone scintigraphy in the evaluation of suspected child abuse. Radiology 146:369–375
Jaudes PK (1984) Comparison of radiography and radionuclide bone scanning in the detection of child abuse. Pediatrics 73:166–168
Mandelstam SA, Cook D, Fitzgerald M, Ditchfield MR (2003) Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child 88:387–390
Bainbridge JK, Huey BM, Harrison SK (2015) Should bone scintigraphy be used as a routine adjunct to skeletal survey in the imaging of non-accidental injury? A 10 year review of reports in a single centre. Clin Radiol 70:e83–e89
Barlucea A, Silva F, Laguna R, Montalvan C (2010) Child abuse patterns: retrospective evaluation of clinical, radiographic and scintigraphic data in a Hispanic population. J Nucl Med 51:1655
Kemp AM, Butler A, Morris S, Mann M, Kemp KW, Rolfe K, Sibert JR, Maguire S (2006) Which radiological investigations should be performed to identify fractures in suspected child abuse? Clin Radiol 61:723–736
Blangis F, Taylor M, Adamsbaum C, Devillers A, Gras-Le Guen C, Launay E, Bossuyt PM, Cohen JF, Chalumeau M (2020) Add-on bone scintigraphy after negative radiological skeletal survey for the diagnosis of skeletal injury in children suspected of physical abuse: a systematic review and meta-analysis. Arch Dis Child 106(4):361–366
Scaglione M, Pinto A, Pedrosa I, Sparano A, Romano L (2008) Multi-detector row computed tomography and blunt chest trauma. Eur J Radiol 65:377–388
Sangster GP, Gonzalez-Beicos A, Carbo AI, Heldmann MG, Ibrahim H, Carrascosa P, Nazar M, D’Agostino HB (2007) Blunt traumatic injuries of the lung parenchyma, pleura, thoracic wall, and intrathoracic airways: multidetector computer tomography imaging findings. Emerg Radiol 14:297–310
Provenzale J (2007) CT and MR imaging of acute cranial trauma. Emerg Radiol 14:1–12
Geijer M, El-Khoury GY (2006) MDCT in the evaluation of skeletal trauma: principles, protocols, and clinical applications. Emerg Radiol 13:7–18
Ringl H, Lazar M, Topker M, Woitek R, Prosch H, Asenbaum U, Balassy C, Toth D, Weber M, Hajdu S, Soza G, Wimmer A, Mang T (2015) The ribs unfolded – a CT visualization algorithm for fast detection of rib fractures: effect on sensitivity and specificity in trauma patients. Eur Radiol 25:1865–1874
Sanchez TR, Grasparil AD, Chaudhari R, Coulter KP, Wootton-Gorges SL (2018) Characteristics of rib fractures in child abuse-the role of low-dose chest computed tomography. Pediatr Emerg Care 34:81–83
Sanchez TR, Lee JS, Coulter KP, Seibert JA, Stein-Wexler R (2015) CT of the chest in suspected child abuse using submillisievert radiation dose. Pediatr Radiol 45:1072–1076
Shelmerdine SC, Langan D, Hutchinson JC, Hickson M, Pawley K, Suich J, Palm L, Sebire NJ, Wade A, Arthurs OJ (2018) Chest radiographs versus CT for the detection of rib fractures in children (DRIFT): a diagnostic accuracy observational study. Lancet Child Adolesc Health 2:802–811
Stoodley N (2006) Controversies in non-accidental head injury in infants. Br J Radiol 79:550–553
Culotta PA, Crowe JE, Tran QA, Jones JY, Mehollin-Ray AR, Tran HB, Donaruma-Kwoh M, Dodge CT, Camp EA, Cruz AT (2017) Performance of computed tomography of the head to evaluate for skull fractures in infants with suspected non-accidental trauma. Pediatr Radiol 47:74–81
Sharp SR, Patel SM, Brown RE, Landes C (2018) Head imaging in suspected non accidental injury in the paediatric population. In the advent of volumetric CT imaging, has the skull X-ray become redundant? Clin Radiol 73:449–453
Martin A, Paddock M, Johns CS, Smith J, Raghavan A, Connolly DJA, Offiah AC (2020) Avoiding skull radiographs in infants with suspected inflicted injury who also undergo head CT: “a no-brainer?”. Eur Radiol 30:1480–1487
Pennell C, Aundhia M, Malik A, Poletto E, Grewal H, Atkinson N (2021) Utility of skull radiographs in infants undergoing 3D head CT during evaluation for physical abuse. J Pediatr Surg 56(6):1180
Orman G, Wagner MW, Seeburg D, Zamora CA, Oshmyansky A, Tekes A, Poretti A, Jallo GI, Huisman TA, Bosemani T (2015) Pediatric skull fracture diagnosis: should 3D CT reconstructions be added as routine imaging? J Neurosurg Pediatr 16:426–431
Deyle S, Brehmer T, Evangelopoulos DS, Krause F, Benneker LM, Zimmermann H, Exadaktylos AK (2010) Review of Lodox Statscan in the detection of peripheral skeletal fractures in multiple injury patients. Injury 41:818–822
Deyle S, Wagner A, Benneker LM, Jeger V, Eggli S, Bonel HM, Zimmermann H, Exadaktylos AK (2009) Could full-body digital X-ray (LODOX-Statscan) screening in trauma challenge conventional radiography? J Trauma 66:418–422
Evangelopoulos DS, von Tobel M, Cholewa D, Wolf R, Exadaktylos AK, Zachariou Z (2010) Impact of Lodox Statscan on radiation dose and screening time in paediatric trauma patients. Eur J Pediatr Surg 20:382–386
Flach PM, Ross SG, Ampanozi G, Ebert L, Germerott T, Hatch GM, Thali MJ, Patak MA (2012) “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol 81:2518–2526
Fu CY, Wang YC, Hsieh CH, Chen RJ (2011) Lodox/Statscan provides benefits in evaluation of gunshot injuries. Am J Emerg Med 29:823–827
Fu CY, Wu SC, Chen RJ (2008) Lodox/Statscan provides rapid identification of bullets in multiple gunshot wounds. Am J Emerg Med 26:965.e965–965.e967
Huang HC, Fu CY, Hsieh CH, Wang YC, Wu SC, Chen RJ, Huang JC (2012) Lodox/Statscan facilitates the early detection of commonly overlooked extracranial injuries in patients with traumatic brain injury. Eur J Trauma Emerg Surg 38:319–326
Knobel GJ, Flash G, Bowie GF (2006) Lodox Statscan proves to be invaluable in forensic medicine. S Afr Med J 96:593–594, 596
Pitcher RD, van As AB, Sanders V, Douglas TS, Wieselthaler N, Vlok A, Paverd S, Kilborn T, Rode H, Potgieter H, Beningfield SJ (2008) A pilot study evaluating the “STATSCAN” digital X-ray machine in paediatric polytrauma. Emerg Radiol 15:35–42
Pitcher RD, Wilde JC, Douglas TS, van As AB (2009) The use of the Statscan digital X-ray unit in paediatric polytrauma. Pediatr Radiol 39:433–437
Whiley SP, Alves H, Grace S (2013) Full-body X-ray imaging to facilitate triage: a potential aid in high-volume emergency departments. Emerg Med Int 2013:437078
Whiley SP, Mantokoudis G, Ott D, Zimmerman H, Exadaktylos AK (2012) A review of full-body radiography in nontraumatic emergency medicine. Emerg Med Int 2012:108129
Yang L, Ye LG, Ding JB, Zheng ZJ, Zhang M (2016) Use of a full-body digital X-ray imaging system in acute medical emergencies: a systematic review. Emerg Med J 33:144–151
Beningfield S, Potgieter H, Nicol A, van As S, Bowie G, Hering E, Latti E (2003) Report on a new type of trauma full-body digital X-ray machine. Emerg Radiol 10:23–29
Douglas TS, Sanders V, Pitcher R, van As AB (2008) Early detection of fractures with low-dose digital X-ray images in a pediatric trauma unit. J Trauma 65:E4–E7
Solomons I (2015) Scanners to combat diamond theft at Debswana mines. Mining Weekly. https://www.miningweekly.com/article/hi-tech-scanners-to-expose-diamond-theft-2015-01-23
Mantokoudis G, Hegner S, Dubach P, Bonel HM, Senn P, Caversaccio MD, Exadaktylos AK (2013) How reliable and safe is full-body low-dose radiography (LODOX Statscan) in detecting foreign bodies ingested by adults? Emerg Med J 30:559–564
du Plessis M, Date-Chong M, Liebenberg L (2020) Lodox®: the invaluable radiographic solution in the forensic setting. Int J Legal Med 134:655–662
Spies AJ, Steyn M, Bussy E, Brits D (2020) Forensic imaging: the sensitivities of various imaging modalities in detecting skeletal trauma in simulated cases of child abuse using a pig model. J Forensic Legal Med 76:102034
Hargaden G, O'Connell M, Kavanagh E, Powell T, Ward R, Eustace S (2003) Current concepts in wholebody imaging using turbo short tau inversion recovery MR imaging. AJR Am J Roentgenol 180:247–252
Kellenberger CJ, Epelman M, Miller SF, Babyn PS (2004) Fast STIR whole-body MR imaging in children. Radiographics 24:1317–1330
Kumar J, Seith A, Kumar A, Sharma R, Bakhshi S, Kumar R, Agarwala S (2008) Whole-body MR imaging with the use of parallel imaging for detection of skeletal metastases in pediatric patients with small-cell neoplasms: comparison with skeletal scintigraphy and FDG PET/CT. Pediatr Radiol 38:953–962
Schooler GR, Davis JT, Daldrup-Link HE, Frush DP (2018) Current utilization and procedural practices in pediatric whole-body MRI. Pediatr Radiol 48:1101–1107
Merlini L, Carpentier M, Ferrey S, Anooshiravani M, Poletti PA, Hanquinet S (2017) Whole-body MRI in children: would a 3D STIR sequence alone be sufficient for investigating common paediatric conditions? A comparative study. Eur J Radiol 88:155–162
Albano D, Patti C, Lagalla R, Midiri M, Galia M (2017) Whole-body MRI, FDG-PET/CT, and bone marrow biopsy, for the assessment of bone marrow involvement in patients with newly diagnosed lymphoma. J Magn Reson Imaging 45:1082–1089
Arnoldi AP, Schlett CL, Douis H, Geyer LL, Voit AM, Bleisteiner F, Jansson AF, Weckbach S (2017) Whole-body MRI in patients with non-bacterial osteitis: radiological findings and correlation with clinical data. Eur Radiol 27:2391–2399
Leclair N, Thormer G, Sorge I, Ritter L, Schuster V, Hirsch FW (2016) Whole-body diffusion-weighted imaging in chronic recurrent multifocal osteomyelitis in children. PLoS One 11:e0147523
Smets AM, Deurloo EE, Slager TJE, Stoker J, Bipat S (2018) Whole-body magnetic resonance imaging for detection of skeletal metastases in children and young people with primary solid tumors – systematic review. Pediatr Radiol 48:241–252
Elterman T, Beer M, Girschick HJ (2007) Magnetic resonance imaging in child abuse. J Child Neurol 22:170–175
Stranzinger E, Kellenberger CJ, Braunschweig S, Hopper R, Huisman TAGM (2007) Whole-body STIR MR imaging in suspected child abuse: an alternative to skeletal survey radiography? Eur J Radiol Extra 63:43–47
Evangelista P, Barron C, Goldberg A, Jenny C, Tung G (2006) MRI STIR for the evaluation of nonaccidental trauma in children
Proisy M, Vivier PH, Morel B, Bruneau B, Sembely-Taveau C, Vacheresse S, Devillers A, Lecloirec J, Bodet-Milin C, Dubois M, Hamonic S, Bajeux E, Ganivet A, Adamsbaum C, Treguier C (2021) Whole-body MR imaging in suspected physical child abuse: comparison with skeletal survey and bone scintigraphy findings from the PEDIMA prospective multicentre study. Eur Radiol 31(11):8069
Eley KA, McIntyre AG, Watt-Smith SR, Golding SJ (2012) “Black bone” MRI: a partial flip angle technique for radiation reduction in craniofacial imaging. Br J Radiol 85:272–278
Eley KA, Watt-Smith SR, Golding SJ (2012) “Black bone” MRI: a potential alternative to CT when imaging the head and neck: report of eight clinical cases and review of the Oxford experience. Br J Radiol 85:1457–1464
Low XZ, Lim MC, Nga V, Sundar G, Tan AP (2021) Clinical application of “black bone” imaging in paediatric craniofacial disorders. Br J Radiol 94:20200061
Dremmen MHG, Wagner MW, Bosemani T, Tekes A, Agostino D, Day E, Soares BP, Huisman T (2017) Does the addition of a “black bone” sequence to a fast multisequence trauma MR protocol allow MRI to replace CT after traumatic brain injury in children? AJNR Am J Neuroradiol 38:2187–2192
Kralik SF, Supakul N, Wu IC, Delso G, Radhakrishnan R, Ho CY, Eley KA (2019) Black bone MRI with 3D reconstruction for the detection of skull fractures in children with suspected abusive head trauma. Neuroradiology 61:81–87
Marine MB, Hibbard RA, Jennings SG, Karmazyn B (2019) Ultrasound findings in classic metaphyseal lesions: emphasis on the metaphyseal bone collar and zone of provisional calcification. Pediatr Radiol 49:913–921
Karmazyn B, Marine MB, Wanner MR, Delaney LR, Cooper ML, Shold AJ, Jennings SG, Hibbard RA (2020) Accuracy of ultrasound in the diagnosis of classic metaphyseal lesions using radiographs as the gold standard. Pediatr Radiol 50:1123
Markowitz RI, Hubbard AM, Harty MP, Bellah RD, Kessler A, Meyer JS (1993) Sonography of the knee in normal and abused infants. Pediatr Radiol 23:264–267
Kelloff J, Hulett R, Spivey M (2009) Acute rib fracture diagnosis in an infant by US: a matter of child protection. Pediatr Radiol 39:70–72
Smeets AJ, Robben SG, Meradji M (1990) Sonographically detected costo-chondral dislocation in an abused child. A new sonographic sign to the radiological spectrum of child abuse. Pediatr Radiol 20:566–567
Lachmann E, Whelan M (1936) The roentgen diagnosis of osteoporosis and its limitations. Radiology 26:165–177
Rosendahl K, Lundestad A, Bjørlykke JA, Lein RK, Angenete O, Augdal TA, Müller LO, Jaramillo D (2020) Revisiting the radiographic assessment of osteoporosis-osteopenia in children 0–2 years of age. A systematic review. PLoS One 15:e0241635
van Rijn RR, Van Kuijk C (2009) Of small bones and big mistakes; bone densitometry in children revisited. Eur J Radiol 71:432–439
Kalkwarf HJ, Zemel BS, Yolton K, Heubi JE (2013) Bone mineral content and density of the lumbar spine of infants and toddlers: influence of age, sex, race, growth, and human milk feeding. J Bone Miner Res 28:206–212
Manousaki D, Rauch F, Chabot G, Dubois J, Fiscaletti M, Alos N (2016) Pediatric data for dual X-ray absorptiometric measures of normal lumbar bone mineral density in children under 5 years of age using the lunar prodigy densitometer. J Musculoskelet Neuronal Interact 16:247–255
Thodberg HH, van Rijn RR, Tanaka T, Martin DD, Kreiborg S (2010) A paediatric bone index derived by automated radiogrammetry. Osteoporos Int 21:1391–1400
Di Iorgi N, Maruca K, Patti G, Mora S (2018) Update on bone density measurements and their interpretation in children and adolescents. Best Pract Res Clin Endocrinol Metab 32:477–498
Adams JE (2016) Bone densitometry in children. Semin Musculoskelet Radiol 20:254–268
Gordon CM, Leonard MB, Zemel BS (2014) 2013 Pediatric position development conference: executive summary and reflections. J Clin Densitom 17:219–224
Martins A, Monjardino T, Nogueira L, Canhao H, Lucas R (2017) Do bone mineral content and density determine fracture in children? A possible threshold for physical activity. Pediatr Res 82:396–404
Wasserman H, Gordon CM (2017) Bone mineralization and fracture risk assessment in the pediatric population. J Clin Densitom 20:389–396
Clark EM, Ness AR, Bishop NJ, Tobias JH (2006) Association between bone mass and fractures in children: a prospective cohort study. J Bone Miner Res 21:1489–1495
Cohen MC, Whitby E (2007) The use of magnetic resonance in the hospital and coronial pediatric postmortem examination. Forensic Sci Med Pathol 3:289–296
Dedouit F, Guilbeau-Frugier C, Capuani C, Sévely A, Joffre F, Rougé D, Rousseau H, Telmon N (2008) Child abuse: practical application of autopsy, radiological, and microscopic studies. J Forensic Sci 53:1424–1429
Sonnemans LJP, Vester MEM, Kolsteren EEM, Erwich J, Nikkels PGJ, Kint PAM, van Rijn RR, Klein WM (2018) Dutch guideline for clinical foetal-neonatal and paediatric post-mortem radiology, including a review of literature. Eur J Pediatr 177:791–803
Klein WM, Duijst WLJM, Erwich JJHM, Hofman PAM, Kint PAM, Kroll JJF, Nikkels PGJ, Renken NS, Van Rijn RR, Rosier Y, Scheeren CIE, Stomp SJ, van der Valk P (2018) Klinische postmortem radiologie. https://richtlijnendatabase.nl/richtlijn/klinische_postmortem_radiologie
Shelmerdine SC, Gerrard CY, Rao P, Lynch M, Kroll JJF, Martin D, Miller E, Filograna L, Martinez RM, Ukpo O, Daly B, Hyodoh H, Johnson K, Watt A, Taranath A, Brown SD, Perry DH, Thorup Boel LW, Borowska-Solonynko A, van Rijn RR, Klein WM, Whitby A, Arthurs OJ (2019) Joint European Society of Paediatric Radiology (ESPR) and International Society for Forensic Radiology and Imaging (ISFRI) guidelines: paediatric post-mortem computed tomography (CT) imaging protocol. Pediatr Radiol 49:694–701
Laskey AL, Haberkorn KL, Applegate KE, Catellier MJ (2009) Postmortem skeletal survey practice in pediatric forensic autopsies: a national survey. J Forensic Sci 54:189–191
Norman MG, Smialek JE, Newman DE, Horembala EJ (1984) The postmortem examination on the abused child. Pathological, radiographic, and legal aspects. Perspect Pediatr Pathol 8:313–343
Kleinman PK, Marks SC Jr, Richmond JM, Blackbourne BD (1995) Inflicted skeletal injury: a postmortem radiologic-histopathologic study in 31 infants. AJR AmJ Roentgenol 165:647–650
McGraw EP, Pless JE, Pennington DJ, White SJ (2002) Postmortem radiography after unexpected death in neonates, infants, and children: should imaging be routine? AJR Am J Roentgenol 178:1517–1521
Sperry K, Pfalzgraf R (1990) Inadvertent clavicular fractures caused by “chiropractic” manipulations in an infant: an unusual form of pseudoabuse. J Forensic Sci 35:1211–1216
Ojima K, Matsumoto H, Hayase T, Fukui Y (1994) An autopsy case of osteogenesis imperfecta initially suspected as child abuse. Forensic Sci Int 65:97–104
Hughes-Roberts Y, Arthurs OJ, Moss H, Set PA (2012) Post-mortem skeletal surveys in suspected non-accidental injury. Clin Radiol 67:868–876
Lorand MA, Fitzpatrick JJ, Soter DK (1996) Radiographic atlas of child abuse: a case studies approach. Igaku-Shoin Medical Pub, New York
Grabherr S, Gygax E, Sollberger B, Ross S, Oesterhelweg L, Bolliger S, Christe A, Djonov V, Thali MJ, Dirnhofer R (2008) Two-step postmortem angiography with a modified heart-lung machine: preliminary results. AJR Am J Roentgenol 190:345–351
Stawicki SP, Gracias VH, Schrag SP, Martin ND, Dean AJ, Hoey BA (2008) The dead continue to teach the living: examining the role of computed tomography and magnetic resonance imaging in the setting of postmortem examinations. J Surg Educ 65:200–205
Griffiths PD, Paley MN, Whitby EH (2005) Post-mortem MRI as an adjunct to fetal or neonatal autopsy. Lancet 365:1271–1273
Shiotani S, Kohno M, Ohashi N, Yamazaki K, Nakayama H, Watanabe K (2004) Postmortem computed tomographic (PMCT) demonstration of the relation between gastrointestinal (GI) distension and hepatic portal venous gas (HPVG). Radiat Med 22:25–29
Grabherr S, Egger C, Vilarino R, Campana L, Jotterand M, Dedouit F (2017) Modern post-mortem imaging: an update on recent developments. Forensic Sci Res 2:52–64
Ampanozi G, Thali YA, Schweitzer W, Hatch GM, Ebert LC, Thali MJ, Ruder TD (2017) Accuracy of non-contrast PMCT for determining cause of death. Forensic Sci Med Pathol 13:284–292
Grabherr S, Heinemann A, Vogel H, Rutty G, Morgan B, Wozniak K, Dedouit F, Fischer F, Lochner S, Wittig H, Guglielmi G, Eplinius F, Michaud K, Palmiere C, Chevallier C, Mangin P, Grimm JM (2018) Postmortem CT angiography compared with autopsy: a forensic multicenter study. Radiology 288:270–276
Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O, Gunny RS, Offiah AC, Owens CM, Saunders DE, Scott RJ, Jones R, Norman W, Addison S, Bainbridge A, Cady EB, Vita ED, Robertson NJ, Taylor AM (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 382:223–233
Krentz BV, Alamo L, Grimm J, Dedouit F, Bruguier C, Chevallier C, Egger C, Da Silva LF, Grabherr S (2016) Performance of post-mortem CT compared to autopsy in children. Int J Legal Med 130:1089–1099
Proisy M, Marchand AJ, Loget P, Bouvet R, Roussey M, Pele F, Rozel C, Treguier C, Darnault P, Bruneau B (2013) Whole-body post-mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 23:1711–1719
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, de Bakker H, van Rijn RR (2014) Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 128(6):957
Shelmerdine SC, Davendralingam N, Palm L, Minden T, Cary N, Sebire NJ, Arthurs OJ (2019) Diagnostic accuracy of postmortem CT of children: a retrospective single-center study. AJR Am J Roentgenol 212:1335. https://doi.org/10.2214/AJR.18.20534
Bajaj M, Offiah AC (2015) Imaging in suspected child abuse: necessity or radiation hazard? Arch Dis Child 100:1163
Berger RP, Panigrahy A, Gottschalk S, Sheetz M (2016) Effective radiation dose in a skeletal survey performed for suspected child abuse. J Pediatr 171:310–312
Hampel J, Pascoal A (2018) Comparison and optimization of imaging techniques in suspected physical abuse paediatric radiography. Br J Radiol 91:20170650
Rao R, Browne D, Lunt B, Perry D, Reed P, Kelly P (2019) Radiation doses in diagnostic imaging for suspected physical abuse. Arch Dis Child 104:863–868
Nickoloff EL, Lu ZF, Dutta AK, So JC (2008) Radiation dose descriptors: BERT, COD, DAP, and other strange creatures. Radiographics 28:1439–1450
United Nations Scientific Committee on the Effects of Atomic Radiation (2010) Sources and effects of ionizing radiation. https://www.unscear.org/docs/publications/2010/UNSCEAR_2010_Report.pdf. Accessed 5 July 2021
U.S. Nuclear Regulatory Commission (NRC) Personal annual radiation dose calculator. https://www.nrc.gov/about-nrc/radiation/around-us/calculator.html. Accessed 5 July 2021
Sheppard JP, Nguyen T, Alkhalid Y, Beckett JS, Salamon N, Yang I (2018) Risk of brain tumor induction from pediatric head CT procedures: a systematic literature review. Brain Tumor Res Treat 6:1–7
Abalo KD, Rage E, Leuraud K, Richardson DB, Le Pointe HD, Laurier D, Bernier MO (2021) Early life ionizing radiation exposure and cancer risks: systematic review and meta-analysis. Pediatr Radiol 51:45–56
Bernier MO, Baysson H, Pearce MS, Moissonnier M, Cardis E, Hauptmann M, Struelens L, Dabin J, Johansen C, Journy N, Laurier D, Blettner M, Le Cornet L, Pokora R, Gradowska P, Meulepas JM, Kjaerheim K, Istad T, Olerud H, Sovik A, Bosch de Basea M, Thierry-Chef I, Kaijser M, Nordenskjöld A, Berrington de Gonzalez A, Harbron RW, Kesminiene A (2019) Cohort profile: the EPI-CT study: a European pooled epidemiological study to quantify the risk of radiation-induced cancer from paediatric CT. Int J Epidemiol 48:379–381
Center for Disease Control and Prevention (CDD) Radiation from Air Travel. https://www.cdc.gov/nceh/radiation/air_travel.html. Accessed 5 July 2021
Public Health England (2011) Ionising radiation: dose comparisons. https://www.gov.uk/government/publications/ionising-radiation-dose-comparisons/ionising-radiation-dose-comparisons. Accessed 5 July 2021
U.S. Nuclear Regulatory Commission (NRC) Doses in Our Daily Lives. https://www.nrc.gov/about-nrc/radiation/around-us/doses-daily-lives.html. Accessed 5 July 2021
Scheuer JL, Musgrave JH, Evans SP (1980) The estimation of late fetal and perinatal age from limb bone length by linear and logarithmic regression. Ann Hum Biol 7:257–265
Rijksinstituut voor Volksgezondheid en Milieu Natural radiation in figures [Natuurlijke straling in cijfers]. https://www.rivm.nl/straling-en-radioactiviteit/straling-van-natuurlijke-oorsprong/natuurlijke-straling-in-cijfers. Accessed 5 July 2021
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
van Rijn, R.R., Nievelstein, R.A.J., Robben, S.G.F. (2023). Radiology in Suspected Child Abuse. In: Bilo, R.A., Robben, S.G.F., van Rijn, R.R. (eds) Forensic Aspects of Paediatric Fractures. Springer, Cham. https://doi.org/10.1007/978-3-031-12041-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-12041-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12040-4
Online ISBN: 978-3-031-12041-1
eBook Packages: MedicineMedicine (R0)