Abstract
Tumor necrosis factor-α (TNF-α) plays a central role in the immunopathogenesis of a wide variety of inflammatory conditions from diseases such as rheumatoid arthritis to inflammatory bowel diseases. Development of TNF-α inhibitors (TNFI) has revolutionized the ability to treat these conditions, resulting in substantial improvement in clinical outcomes. Since the introduction of infliximab and etanercept in 1998, indications for the use of TNFI have expanded, and these medications are predominately prescribed by rheumatologists, dermatologists, and gastroenterologists for moderate to severe inflammatory and autoimmune diseases. As a result of widespread use of these effective therapies, there have been safety concerns related to immunosuppression, the foremost of which is the increased incidence of infections caused by a broad range of pathogens. In this chapter, we review available data on the epidemiology of infectious complications in patients receiving TNFI for the treatment of inflammatory conditions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tumor necrosis factor-alpha
- Anti-tumor necrosis factor-alpha
- Anti-TNF-α infections
- Infection
- Tuberculosis
- Herpes zoster
Introduction
Tumor necrosis factor-α (TNF-α) plays a central role in the immunopathogenesis of a wide variety of inflammatory conditions from diseases such as rheumatoid arthritis (RA) to inflammatory bowel diseases (IBD). Development of TNF-α inhibitors (TNFI) has revolutionized the ability treat these conditions resulting in substantial improvement in outcomes [1,2,3]. Since the introduction of infliximab and etanercept in 1998, indications for the use of TNFI have expanded, and these medications are predominately prescribed by rheumatologists, dermatologists, and gastroenterologists for moderate to severe inflammatory and autoimmune diseases. Although these drugs have had a substantial impact in the treatment of many diseases, there are important safety concerns, the foremost of which is increased risk of infection caused by bacterial, mycobacterial, fungal, and viral pathogens [4]. Herein, we will review available data on the epidemiology of infectious complications in patients receiving TNFI for the treatment of inflammatory conditions.
Tumor Necrosis Factor-Alpha and the Innate Immune System
Tumor necrosis factor-α, primarily produced by macrophages and T-lymphocytes, is the principal endogenous regulator of inflammation and immune responses. First described in 1975 and named after its ability to cause tumor apoptosis in vitro, TNF-α is found constitutively in macrophages as a 233-amino acid transmembrane protein. Monomeric membrane-bound TNF-α aggregates into metabolically active homotrimers. When cleaved by the membrane-bound metalloprotease TNF-α converting enzyme (TACE), a soluble 157-amino acid TNF-α residue is released into circulation [5]. Only in the homotrimeric form is soluble TNF-α able to bind to its target receptors (Fig. 5.1). The activity of TNF-α is mediated by two types of receptors: tumor necrosis factor receptor 1 (TNFR1, also known as p55) and 2 (TNFR2, also known as p75). Although both receptors are structurally related, they are functionally distinct receptors mediating the activity of TNF-α in cells [6]. TNFR1 is found in a broad array of cells including macrophages, while TNFR2 is expressed predominantly in endothelial cells and lymphocytes [6]. Activation of TNFR1, which contains an intracellular death domain, results in induction of a signaling cascade with pleotropic effect that includes cell proliferation, apoptosis, and cytokine secretion [7]. TNFR2 does not contain a death domain and its stimulation can result in proliferation, migration, and production of cytokines such as interleukins -1 (IL-1) or -6 (IL-6), both important mediators of inflammation [7].
Overview of the TNF-α cascade in the presence of TNF-α inhibitors. Left half: Transmembrane TNF-α found on cell membranes of macrophages and other immune cells forms trimers and are released as biologically active homotrimeric soluble form via cleavage by TNF-α converting enzyme (TACE). Both soluble and transmembrane TNF-α homotrimers can bind to their ligand receptors (TNFR1 and TNFR2) found in a wide variety of cells throughout the body. The effect of which is a cascade of cell signaling that includes (1) cytokine and chemokine release; (2) maturation, proliferation, and migration of macrophages and other immune cells; (3) increased phagocytic activity of macrophages; and (4) formation and maintenance of granuloma. Right half: TNF-α inhibitors (TNFI) act by either binding transmembrane (A) and/or soluble (B) TNF-α. TNFI with IgG1 Fc region contains a CH1 domain that in the presence of complements can induce complement-dependent cytotoxicity (CDC) and antibody-dependent cell-mediated cytotoxicity (ADCC) leading to apoptosis of cells expressing transmembrane TNF-α (e.g. macrophages). (Illustration created by authors with BioRender.com)
The activation of the innate immune response by an infectious pathogen includes release of TNF-α by activated macrophages into the affected tissue. The subsequent activation of TNFR1 and TNFR2 by binding with the homotrimer TNF-α results in a torrent of inflammatory events that includes release of inflammatory cytokines IL-1β, IL-6, IL-8, and granulocyte-macrophage colony stimulating factor (GM-CSF); upregulation of adhesion molecules, including intracellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), and E selectin (also known as endothelial leukocyte adhesion molecule-1, or ELAM-1); and increased expression of chemokines (e.g. RANTES, MCP-1, MIP-2) [8,9,10,11,12,13]. The combined effect results in vasodilatation at the infection site, coordinated recruitment, and migration of leukocytes to the target site, and activation of efficient phagocytosis of the pathogens resulting in successful host defense [13, 14].
TNF-α is essential for mounting effective host defense against pathogens that require granuloma formation for control [13]. These pathogens, which include Mycobacterium species including M. tuberculosis (TB), M. avium, and fungal pathogens such as Histoplasma capsulatum, Aspergillus fumigatus, and Cryptococcus neoformans, are not easily eradicated by host defense mechanisms and require sequestration into granulomas [13, 15,16,17,18,19]. TNF-α coordinates the organized formation of granulomas initially with chemokine production, phagosome activation, and leukocyte recruitment and differentiation, and subsequent leukocyte aggregation into function granulomas that can control infectious pathogens [13, 14].
Tumor Necrosis Factor-Alpha Inhibitors (TNFI)
Currently there are five approved anti-TNF-α agents available for various clinical indications (Table 5.1). All are indicated for the treatment of RA, ankylosing spondylitis, and psoriatic arthritis [2, 3, 20]. Except for etanercept, inflammatory bowel diseases (namely, Crohn’s disease and ulcerative colitis) can be effectively treated with TNFI [21, 22]. Other TNFI indications include treatment of inflammation of the skin (plaque psoriasis and hidradenitis suppurativa) and the eye (uveitis) [23,24,25].
Etanercept and Infliximab were the earliest developed TNFI for clinical use and both were approved in 1998. Etanercept is a soluble fusion protein consisting of two human TNF-α receptor-2 (TNFR2) bound to the constant (Fc) region of a human IgG1 that acts as a decoy and binds both soluble forms of TNF-α and TNF-β, the latter is a related cytokine that utilizes the same receptors as TNF-α [26]. In contrast, infliximab is a chimeric monoclonal antibody consisting of a mouse anti-TNF-α variable (Fab′) region coupled with a human IgG Fc region. Adalimumab and Golimumab are both fully human IgG monoclonal anti-TNF-α antibodies with both humanized Fab′ and Fc regions [26]. As IgG1 monoclonal antibodies, infliximab, adalimumab, and golimumab can inhibit both soluble and membrane-bound forms of TNF-α but do not neutralize TNF-β [27]. As the Fc region of IgG1 contains a CH2 domain that is responsible for the activation of C1 (first component of the classical pathway of complement activation), both the full chain IgG monoclonal antibodies (infliximab, adalimumab, and golimumab) and etanercept in the presence of complements can induce both complement-dependent cytotoxicity (CDC) and antibody-dependent cell-mediated cytotoxicity (ADCC) with subsequent lysis of membrane-bound TNF-α expressing cells [26,27,28]. Lacking a CH1 domain that serves as the platform for C3 activation (the most vital step in the complement cascade), etanercept induces significantly less CDC on membrane-bound TNF-α-expressing cells [27, 28].
Certolizumab is a PEGylated Fab′ fragment of a humanized monoclonal anti-TNF-α antibody. The attachment of the Fab′ fragment to a 40-kDa polyethylene glycol moiety markedly increases the half-life of certolizumab compared to other TNFIs [29]. Like the full-chain anti-TNF-α monoclonal antibodies, certolizumab inhibits both soluble and membrane-bound TNF-α and lacks activity against TNF-β [29]. But in contrast to other inhibitors, certolizumab does not contain the crystallizable IgG Fc fragment and does not cause complement fixation, thus it does not induce CDC and ADCC in vitro [27,28,29].
Risk of Infection
Data evaluating infection risk are derived from a variety of sources, including clinical trials, meta-analyses, observational studies, and registries [30,31,32,33,34] (Table 5.2). In general, there is increased risk of infection with TNFI use, especially for tuberculosis, bacterial infections, and fungal infections. Several studies report a higher infection risk with infliximab when compared to adalimumab or etanercept [32, 35, 36]. However, there are several important limitations. Clinical trials may be limited by small sample sizes, inclusion of healthier patients, and insufficient statistical power to detect uncommon infection events. In observational studies, due to lack of randomization, confounding factors can impact results. Patients with autoimmune diseases enrolled in trials may be receiving corticosteroids or other medications that increase risk of infection, making attribution of infection risk to a particular TNFI challenging. Another important limitation in identifying TNFI infection risk in populations is related to underlying diseases that may impact infection risk. For example, patients with RA have an increased risk of infection compared with non-RA controls [37].
Mycobacterial Infections
Effective host immune response against Mycobacterium tuberculosis involves TNF-α-mediated formation of organized granulomas for control and prevention of dissemination. Studies including meta-analyses of randomized controlled trials, retrospective and prospective cohorts, and post-marketing registries have consistently shown increased risk for active tuberculosis (TB) in people on TNFI [30, 33, 38,39,40,41]. Patients with latent tuberculosis infection (LTBI) receiving TNFI therapy for RA, ankylosing spondylitis, or psoriatic arthritis have an estimated fourfold increased risk of TB reactivation as compared to controls [4, 30, 39, 41]. In a recent publication, Cao and colleagues reviewed 23 placebo-controlled clinical trials and similar increased odds of active tuberculosis were seen in patients with Crohn’s disease receiving TNFI [38]. All TB reactivation cases occurred in the TNFI arm and none in the placebo controls, with an odds ratio (OR) of 4.85 with a 95% confidence interval (CI) between 1.02 and 22.99 [38].
The risk of active TB may be different among TNFI [39, 40]. A systematic review in patients with RA treated with TNFI showed higher risk of tuberculosis with the use of adalimumab and infliximab compared to etanercept, with OR of 3.88 and 2.78, respectively [39]. The French RATIO registry reported a significantly higher odds ratio with adalimumab (OR 17.08) and infliximab (OR 13.29) when compared to etanercept [40]. Tuberculosis reactivation occurred five times higher during the first year of initiating TNFI therapy [40]. Latent TB infection screening and treatment for patients who will be receiving TNFI therapy can reduce risk of reactivation by 65% [39].
Nontuberculous mycobacteria (NTM) can cause a variety of human diseases particularly of the lungs in people with underlying lung conditions. Few data exist on the risk of NTM in patients on TNFI. The U.S. Food and Drug Administration (FDA) MedWatch database report in 2009 found 105 cases of NTM related to TNFI use. The majority were women (65%), had rheumatoid arthritis (70%), and most were receiving infliximab (70%) [42]. Half of the NTM infections were due to Mycobacterium avium, and though 56% were lung infections, extrapulmonary infections were not uncommon [42].
Mycobacterial infection rates in patients who used TNFI were evaluated using the Kaiser Permanente database [43]. TNFI-associated rates of NTM were 49 per 100,000 person years, greater than in unexposed RA patients (19.2 per 100,000 person years) or the general population (4.1 per 100,000 person years). NTM rates were lower for users of etanercept, when compared with infliximab or adalimumab [43].
Bacterial and Other Serious Infections
Many studies have reported data on TNFI use and serious (hospitalized) infections, which include a variety of organisms, but most frequently refer to bacterial infections [4, 30,31,32]. However, fewer details have been captured on specific bacteria causing an infection or infectious syndrome. Typically, pneumonia, skin, and soft tissue and urinary tract infections are the most common serious infections observed in adults, similar to the pre-biologic era [37]. In children, skin/soft tissue and respiratory infections are common [44].
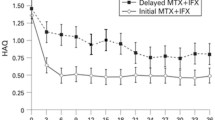
In general, when comparing patients on TNFI to those receiving conventional disease modifying anti-rheumatic drugs (DMARDs), there is an increased risk of serious infection, with adjusted rate ratios ranging from 1.5 to 5.0, and infections per 100 person-years ranging from 2 to 15 [32, 33, 45,46,47]. It is important to note that timing of risk assessment is important, as studies focused on the first year of TNFI therapy show adjusted increased rate ratios, where a decline in absolute and relative risk of infection is typically seen after 1 year [32, 46,47,48].
A 2011 network meta-analysis of RCTs and extension studies found that TNFIs increased serious infection risk [30]. Certolizumab pegol was the only individual TNFI agent that significantly increased the risk of serious infection compared to control (OR 3.51; 95% CI 1.59–7.79). Another recent meta-analysis of 106 RCTs of targeted therapies (mostly TNFI) in RA patients demonstrated an increased risk of serious infections (OR 1.31, 95% CI 1.09–1.58) in patients who received standard dose TNFIs compared with traditional DMARDS. The risk was more pronounced (OR 1.9, 95% CI 1.50–2.39) in patients receiving high doses [31].
Studies in other populations have shown a variability in risk estimates. A meta-analysis evaluating patients with psoriatic arthritis reported a crude OR for infection of 1.18 (95% CI: 1.05–1.33) in patients exposed to TNFI (versus controls) [49]. In a meta-analysis among patients with ankylosing spondylitis, the risk of serious infection related to TNFI was low and was not significantly increased compared to untreated controls [50]. Two meta-analyses in patients with inflammatory bowel disease concluded that the risk of serious infection with TNFI was not increased [51, 52].
Many randomized controlled trials and observational studies fail to detail the precise nature of infectious syndromes or the causative agents. However, some series have reported either site-specific infections or data on specific pathogens. Risk for septic arthritis in RA with use of TNFI was evaluated in the British Society for Rheumatology Biologics Register. The adjusted hazard ratio for septic arthritis was 2.3 (95% CI: 1.2–4.4) for TNFI compared with traditional DMARDs. Staphylococcus aureus was the most common cause of septic arthritis [53].
Several studies have evaluated TNFI use and risk of listeriosis, one of which described a fourfold increased risk of severe listeriosis with TNFI in comparison with the general population [54,55,56]. There is a risk for legionellosis and TNFI, with one study finding the incidence rate of legionellosis in patients in TNFI to be 46.7 per 100,000 person-years and greater than the general population [57].
Viral Infections
Hepatitis B
TNF-α stimulates hepatitis B (HBV)-specific T-cell responses, inhibits HBV replication, and mediates HBV clearance in infected hepatocytes [58, 59]. Hepatitis B reactivation is the result of the loss of HBV immune control and is defined as an increase in HBV DNA level of either: (1) ≥2 log (100-fold) compared to baseline, (2) ≥2 log (1000) IU/mL in a previously undetectable level, or (3) ≥4 log (10,000) IU/mL if baseline not available [60]. HBV reactivation is a well-known complication in patients receiving TNFI [61,62,63,64,65]. In a retrospective Taiwanese study, HBV reactivation occurred in 5 (28%) of 18 hepatitis B surface antigen (HBsAg)-positive patients and 1 (25%) in 4 patients with occult HBV infection during the first year of TNFI therapy [62]. In addition, HBV reactivation occurs in previously inactive HBsAg carriers occurs following TNFI therapy [61]. A prospective Japanese cohort of 50 anti-HBc-positive RA patients on TNFI therapy followed up to 32 months, HBV reactivation was seen in 2 of 5 (40%) of HBsAg-positive patients and only 1 of 45 (2%) HBsAg [65]. In patients with previously resolved HBV infection, TNFI therapy was found to be safe, with no HBV seroconversion or reactivation observed [66]. Prophylactic antiviral therapy is effective in preventing reactivation [62, 67].
Guidelines consider use of TNFI as a moderate risk category with regards to HBV reactivation. Patients who are to start TNFI should at least have a baseline HBV serology that includes HBV surface antigen (HBsAg) and total HBV core antibody (anti-HBc) [67]. In HBV-endemic areas, HBV DNA should also be checked at baseline to detect occult HBV infections. In patients with either positive HBsAg or HBV DNA, preemptive anti-HBV antivirals with high barrier to resistance, such as tenofovir or entecavir, should be considered until 6–12 months after the last TNFI dose. Serial monitoring of HBV while on TNFI therapy every 6–12 months even for those with resolved HBV infections (anti-HBc positive but negative for HBsAg and HBV DNA) is recommended.
Hepatitis C
Evidence supports a TNF-α role in mediating inflammatory responses to hepatitis C (HCV) such as enabling apoptosis of infected cells, but it does not appear to play a pivotal role in the control of HCV replication [68]. In addition, TNF-α polymorphism has no significant effect to HCV susceptibility or viral clearance [68]. Data on the safety of TNFI use in patients with chronic HCV is limited and mostly derived from small cohorts and aggregates of case reports and case series. In a small cohort of 29 patients with both active RA and mild chronic HCV, use of etanercept was observed to be safe, with no increased risk of hepatic flare related to HCV replication [69]. A literature review found 216 patients with HCV who received TNFI (either etanercept, infliximab, or adalimumab) with mean observation time of 1.2 years and found only three patients needing TNFI withdrawal due to suspected HCV reactivation [70]. The limited data available supports that TNFI use in HCV patients is at least safe in the short-term [69, 70]. With the availability of safe and effective direct acting antivirals (DAAs) for HCV, treatment should be considered for patients planning to receive or receiving TNFI.
Herpes Zoster
Numerous studies have evaluated risk of herpes zoster with TNFI use, but evidence of risk of herpes zoster and TNFI therapy have been conflicting. A large U.S. multicenter cohort study [71] involving more than 33,000 patients with RA and other inflammatory diseases showed no increased risk of HZ when treated with TNFI. However, European registries [35, 72,73,74] and an Asian case-control study [75] showed an approximate twofold increase risk. Moreover, patients on TNFI had almost a ten times higher rate of hospitalization related to zoster when compared to the general population (32 vs. 3.4 cases per 100,000 patient-years) in a Spanish registry [74]. An international prospective registry study of patients with psoriasis showed that TNFI was not significantly associated with an increased risk of HZ, although the adjusted hazard ratio was 2.73 (95% CI 0.98–7.58) [76]. A British registry study found that zoster was highest among patients on infliximab (hazard risk [HR] of 2.2; 95% confidence interval [CI] 1.4–3.4) and lowest with adalimumab use (HR 1.5; 95% CI 1.1–2.0) [35].
Herpes zoster is a vaccine preventable disease. Shingrix, an adjuvanted recombinant zoster vaccine, significantly reduced risk of shingles by 94–97% compared to placebo in immunocompetent adults 50 years or older [77]. In a pooled post hoc analysis of participants with autoimmune diseases from two phase 3 trials showed overall vaccine efficacy of Shingrix at 90.5% (95% CI: 73.5–97.5%) [78]. This vaccine given in two doses 2–6 months apart is currently recommended for adults age 50 including those who are on low dose immunosuppression or anticipating being on immunosuppressive therapy [79, 80]. Although no head-to-head studies present, Shingrix is preferred over the live attenuated HZ vaccine, Zostavax, due to the latter lower efficacy rates especially in the older at-risk groups [77, 81, 82]. Zostavax is no longer available in the United States.
Fungal Infections
Tumor necrosis factor-α plays an important role in the control of infection due to fungi; however, fungal infections complicating TNFI use are relatively uncommon. Most reports detail impact on histoplasmosis, coccidioidomycosis, aspergillosis, and Pneumocystis jirovecii pneumonia (PCP) [34, 83,84,85,86,87,88]. The precise risk of TNFI use and fungal infection is difficult to acertain, as the concomitant use of other immunosuppressive therapies, especially corticosteroids, renders risk interpretation problematic. A recent meta-analysis reported the risks of opportunistic infections in RA patients from clinical trial data of biologic use, mostly TNFI [34]. Biologic use did not significantly increase the risk for all fungal (superficial or invasive) infections (odds ratio 1.31, 95% CI 0.46–3.72), invasive fungal infections (odds ratio 2.58; 95% confidence interval 0.68–11.91), or PCP (odds ratio 1.77, 95% confidence interval 0.42–7.47). A large US cohort study evaluated new users of TNFI and investigated the incidence of nonviral opportunistic infections among patients with RA, ankylosing spondylitis, psoriatic arthritis, psoriasis, and IBD [89]. Among 33,324 new users of TNFI, 80 nonviral OIs were identified. Of these, 32 (40%) were caused by fungi, with a crude incidence rate of 112 cases per 100,000 person-years. The most common fungal infections were pneumocystosis (16 cases) and histoplasmosis (9 cases).
The estimated incidence of aspergillosis is approximately seven cases per 100,000 persons treated with TNFI [85, 88]. A case series was published by Tsiodras and colleagues, who reviewed publications up to June 1, 2007 to determine the association of fungal infections with TNF-α blockade [90]. Sixty-four cases of aspergillosis, mostly invasive pulmonary disease, were identified. The most common TNFI used was infliximab in 48 cases (75%), followed by etanercept in 14 (22%), and adalimumab in three cases (3%) [90].
The incidence of coccidioidomycosis in patients receiving TNFI is estimated to range up to 5.58 per 100,000 persons treated with infliximab and 0.88 per 100,000 persons treated with etanercept [91]. Bergstrom and colleagues described 13 cases among patients receiving TNFI from in areas endemic for coccidioidomycosis [92]. The interval between TNFI and infection ranged from 1 to 96 weeks (mean, 27 weeks), and two cases were likely due to reactivation. All patients had pneumonia on presentation, with 4 (30.7%) having disseminated disease. The risk of infliximab in development of symptomatic coccidioidomycosis when compared to other agents was greater (RR 5.23, 95% CI 1.54–17.71; p < 0.01).
Taroumian and colleagues described 44 patients with rheumatologic disease treated with nonbiologic DMARDS and/or biologic therapies in Tucson, Arizona [93]. Twenty-nine patients had pulmonary coccidioidomycosis, nine patients had disseminated disease, and six had asymptomatic coccidioidomycosis based on positive serology. With continuation or resuming biologic therapy after treatment, no patients had subsequent dissemination or complications of coccidioidomycosis.
Histoplasmosis is one of the most common fungal infections in patients receiving TNFI [84, 85]. Wallis and colleagues collected data from cases reported to FDA Adverse Event Reporting System (AERS) from January 1998 through September 2002 and identified 40 cases of histoplasmosis. The estimated rate of histoplasmosis per 100,000 patients treated was 18.78 in patients treated with infliximab and 2.65 in patients treated with etanercept [85]. Vergidis and colleagues described 98 patients diagnosed with histoplasmosis while receiving TNF-α inhibitors from January 2000 to June 2011. Seventy-four (76%) patients presented with disseminated histoplasmosis; pulmonary involvement was present in 78 (80%) patients. The median time to diagnosis after TNFI initiation was 15.5 months (range of 1–88 months) [84]. Rheumatoid arthritis was the most common underlying disease, and infliximab (67.3%) was most used. TNFI therapy was initially discontinued in 96.9% of patients but resumed in 33% of patients at a median of 12 months. The recurrence rate at follow-up was 3.2%.
Olson and colleagues found that 15 of 26 patients with RA who developed disseminated histoplasmosis from 1998 to 2009 were on TNFI and had a median time on TNFI to histoplasmosis diagnosis of 15 months (range, 2–132 months) [94]. Most patients were treated with at least 6 months of antifungal therapy. In this study, TNFI were discontinued at the time of infection in 14 patients and was restarted successfully in 4/15 with recurrence of disease in only one patient [94].
Pneumocystis Pneumonia
Pneumocystis jirovecii pneumonia (PCP) complicating patients receiving TNFI is uncommon, with variability in incidence rates depending on the population studied and diagnostic method used. Observational studies have reported incidence rates of up to 8.8 cases per 1000 patient-years [95,96,97]. Takeuchi and colleagues examined the incidence of adverse events in Japanese patients with RA for their first 6 months on infliximab as post-marketing surveillance [95]. The diagnosis of suspected PCP was made in 22 (0.4%) patients, with many cases diagnosed by PCR for P jirovecii DNA from bronchoalveolar lavage fluid.
The National Institutes of Health conducted a population-based study to determine if the incidence of PCP in patients with RA had changed significantly from 1996 to 2007 using data from the Nationwide Inpatient Sample and the California Office of Statewide Health Planning and Development [97]. They found no significant change in the number of patients with RA and PCP diagnoses over this period.
Conclusion
Tumor necrosis factor-α inhibitors have become an important class of drugs and will continue to be used widely in the treatment of autoimmune and inflammatory diseases. Although uncommon, increased risk of infection caused by bacterial, mycobacterial, fungal, and viral pathogens have the potential for increased morbidity and mortality. Risk of infection is often difficult to characterize, as it may differ with underlying patient comorbidities, concomitant medications, and the specific TNFI agent. Use of TNFI will warrant clinician vigilance and continued infection surveillance.
Potential Conflicts of Interest
JVC: Research grants from Gilead Sciences, Inc.
JWB: Consultation for Eli Lilly and Viela Bio.
References
Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359(9317):1541–9.
Aaltonen KJ, Virkki LM, Malmivaara A, Konttinen YT, Nordström DC, Blom M. Systematic review and meta-analysis of the efficacy and safety of existing TNF blocking agents in treatment of rheumatoid arthritis. PLoS One. 2012;7(1):e30275.
Corbett M, Soares M, Jhuti G, Rice S, Spackman E, Sideris E, et al. Tumour necrosis factor-α inhibitors for ankylosing spondylitis and non-radiographic axial spondyloarthritis: a systematic review and economic evaluation. Health Technol Assess (Rockv). 2016;20(9):333.
Baddley JW, Cantini F, Goletti D, Gómez-Reino JJ, Mylonakis E, San-Juan R, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [I]: anti-tumor necrosis factor-α agents). Clin Microbiol Infect. 2018;24:S10–20.
Black RA, Rauch CT, Kozlosky CJ, Peschon JJ, Slack JL, Wolfson MF, et al. A metalloproteinase disintegrin that releases tumour-necrosis factor-∅ from cells. Nature. 1997;385(6618):729–33.
Walczak H. TNF and ubiquitin at the crossroads of gene activation, cell death, inflammation, and cancer. Immunol Rev. 2011;244(1):9–28.
Billmeier U, Dieterich W, Neurath MF, Atreya R. Molecular mechanism of action of anti-tumor necrosis factor antibodies in inflammatory bowel diseases. World J Gastroenterol. 2016;22(42):9300–13.
Kaushansky K, Broudy VC, Harlan JM, Adamson JW. Tumor necrosis factor-γ and tumor necrosis factor-β (lymphotoxin) stimulate the production of granulocyte-macrophage colony-stimulating factor, macrophage colony-stimulating factor, and IL-1 in vivo. J Immunol. 1988;141(10):3410–5.
Shalaby MR, Aggarwal BB, Rinderknecht E, Svedersky LP, Finkle BS, Palladino MA. Activation of human polymorphonuclear neutrophil functions by interferon-gamma and tumor necrosis factors. J Immunol. 1985;135(3):2069–73. http://www.ncbi.nlm.nih.gov/pubmed/3926894.
Sumagin R, Sarelius IH. TNF-α activation of arterioles and venules alters distribution and levels of ICAM-1 and affects leukocyte-endothelial cell interactions. Am J Physiol Heart Circ Physiol. 2006;291(5):H2116.
Murao K, Ohyama T, Imachi H, Ishida T, Cao WM, Namihira H, et al. TNF-α stimulation of MCP-1 expression is mediated by the Akt/PKB signal transduction pathway in vascular endothelial cells. Biochem Biophys Res Commun. 2000;276(2):791–6.
Victor FC, Gottlieb AB. TNF-alpha and apoptosis: implications for the pathogenesis and treatment of psoriasis. J Drugs Dermatol. 2002;1:264–75.
Roach DR, Bean AGD, Demangel C, France MP, Briscoe H, Britton WJ. TNF regulates chemokine induction essential for cell recruitment, granuloma formation, and clearance of mycobacterial infection. J Immunol. 2002;168(9):4620–7.
Marino MW, Dunn A, Grail D, Inglese M, Noguchi Y, Richards E, et al. Characterization of tumor necrosis factor-deficient mice. Proc Natl Acad Sci U S A. 1997;94(15):8093–8.
Flynn JAL, Goldstein MM, Chan J, Triebold KJ, Pfeffer K, Lowenstein CJ, et al. Tumor necrosis factor-α is required in the protective immune response against mycobacterium tuberculosis in mice. Immunity. 1995;2(6):561–72.
Resende M, Cardoso MS, Fróis-Martins R, Borges M, Jordan MB, Castro AG, et al. TNF-mediated compensatory immunity to Mycobacterium avium in the absence of macrophage activation by IFN-γ. J Immunol. 2019;203(9):2451–8.
Zhou P, Miller G, Seder RA. Factors involved in regulating primary and secondary immunity to infection with Histoplasma capsulatum: TNF-alpha plays a critical role in maintaining secondary immunity in the absence of IFN-gamma. J Immunol. 1998;160(3):1359–68. http://www.ncbi.nlm.nih.gov/pubmed/9570555.
Mehrad B, Strieter RM, Standiford TJ. Role of TNF-alpha in pulmonary host defense in murine invasive aspergillosis. J Immunol. 1999;162(3):1633–40.
Huffnagle GB, Toews GB, Burdick MD, Boyd MB, McAllister KS, McDonald RA, et al. Afferent phase production of TNF-α is required for the development of protective T cell immunity to Cryptococcus neoformans. J Immunol. 1996;157(10):4529–36.
Lemos LLP, de Oliveira Costa J, Almeida AM, Junior HO, Barbosa MM, Kakehasi AM, et al. Treatment of psoriatic arthritis with anti-TNF agents: a systematic review and meta-analysis of efficacy, effectiveness and safety. Rheumatol Int. 2014;34:1345–60.
Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):644–59.
Oussalah A, Danese S, Peyrin-Biroulet L. Efficacy of TNF antagonists beyond one year in adult and pediatric inflammatory bowel diseases: a systematic review. Curr Drug Targets. 2010;11(2):156–75.
Yamauchi PS, Bissonnette R, Teixeira HD, Valdecantos WC. Systematic review of efficacy of anti-tumor necrosis factor (TNF) therapy in patients with psoriasis previously treated with a different anti-TNF agent. J Am Acad Dermatol. 2016;75(3):612–18.e6. https://doi.org/10.1016/j.jaad.2016.02.1221.
Kimball AB, Okun MM, Williams DA, Gottlieb AB, Papp KA, Zouboulis CC, et al. Two phase 3 trials of adalimumab for hidradenitis suppurativa. N Engl J Med. 2016;375(5):422–34.
Sheppard J, Joshi A, Betts KA, Hudgens S, Tari S, Chen N, et al. Effect of adalimumab on visual functioning in patients with noninfectious intermediate uveitis, posterior uveitis, and panuveitis in the VISUAL-1 and VISUAL-2 trials. JAMA Ophthalmol. 2017;135(6):511–8.
Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117(2):244–79.
Ueda N, Tsukamoto H, Mitoma H, Ayano M, Tanaka A, Ohta SI, et al. The cytotoxic effects of certolizumab pegol and golimumab mediated by transmembrane tumor necrosis factorα. Inflamm Bowel Dis. 2013;19(6):1224–31.
Horiuchi T, Mitoma H, Harashima SI, Tsukamoto H, Shimoda T. Transmembrane TNF-α: structure, function and interaction with anti-TNF agents. Rheumatology. 2010;49(7):1215–28.
Nesbitt A, Fossati G, Bergin M, Stephens P, Stephens S, Foulkes R, et al. Mechanism of action of certolizumab pegol (CDP870): in vitro comparison with other anti-tumor necrosis factor α agents. Inflamm Bowel Dis. 2007;13(11):1323–32.
Singh JA, Wells GA, Christensen R, Tanjong Ghogomu E, Maxwell LJ, Macdonald JK, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2011(2):CD008794.
Singh JA, Cameron C, Noorbaloochi S, Cullis T, Tucker M, Christensen R, et al. Risk of serious infection in biological treatment of patients with rheumatoid arthritis: a systematic review and meta-analysis. Lancet. 2015;386(9990):258–65.
Grijalva CG, Chen L, Delzell E, Baddley JW, Beukelman T, Winthrop KL, et al. Initiation of tumor necrosis factor-αantagonists and the risk of hospitalization for infection in patients with autoimmune diseases. JAMA. 2011;306(21):2331–9.
Minozzi S, Bonovas S, Lytras T, Pecoraro V, González-Lorenzo M, Bastiampillai AJ, et al. Risk of infections using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and meta-analysis. Expert Opin Drug Saf. 2016;15:11–34. [cited 2020 Oct 10]. https://www.tandfonline.com/doi/abs/10.1080/14740338.2016.1240783.
Kourbeti IS, Ziakas PD, Mylonakis E. Biologic therapies in rheumatoid arthritis and the risk of opportunistic infections: a meta-analysis. Clin Infect Dis. 2014;58(12):1649–57.
Galloway JB, Mercer LK, Moseley A, Dixon WG, Ustianowski AP, Helbert M, et al. Risk of skin and soft tissue infections (including shingles) in patients exposed to anti-tumour necrosis factor therapy: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2013;72(2):229–34.
Van Dartel SAA, Fransen J, Kievit W, Flendrie M, Den Broeder AA, Visser H, et al. Difference in the risk of serious infections in patients with rheumatoid arthritis treated with adalimumab, infliximab and etanercept: results from the Dutch Rheumatoid Arthritis Monitoring (DREAM) registry. Ann Rheum Dis. 2013;72(6):895–900.
Doran MF, Crowson CS, Pond GR, O’Fallon WM, Gabriel SE. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum. 2002;46(9):2287–93.
Cao BL, Qasem A, Sharp RC, Abdelli LS, Naser SA. Systematic review and meta-analysis on the association of tuberculosis in Crohn’s disease patients treated with tumor necrosis factor-α inhibitors (anti-TNFα). World J Gastroenterol. 2018;24(25):2764–75.
Ai JW, Zhang S, Ruan QL, Yu YQ, Zhang BY, Liu QH, et al. The risk of tuberculosis in patients with rheumatoid arthritis treated with tumor necrosis factor-α antagonist: a metaanalysis of both randomized controlled trials and registry/cohort studies. J Rheumatol. 2015;42(12):2229–37. [cited 2020 Oct 6]. https://pubmed.ncbi.nlm.nih.gov/26472414/.
Tubach F, Salmon D, Ravaud P, Allanore Y, Goupille P, Bréban M, et al. Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective French research axed on tolerance of biotherapies registry. Arthritis Rheum. 2009;60(7):1884–94. [cited 2020 Oct 10]. http://doi.wiley.com/10.1002/art.24632.
Zhang Z, Fan W, Yang G, Xu Z, Wang J, Cheng Q, et al. Risk of tuberculosis in patients treated with TNF-α antagonists: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2017;7(3):e012567.
Winthrop KL, Chang E, Yamashita S, Iademarco MF, LoBue PA. Nontuberculous mycobacteria infections and anti-tumor necrosis factor-α therapy. Emerg Infect Dis. 2009;15(10):1556–61.
Winthrop KL, Baxter R, Liu L, Varley CD, Curtis JR, Baddley JW, et al. Mycobacterial diseases and antitumour necrosis factor therapy in USA. Ann Rheum Dis. 2013;72(1):37–42.
Toussi SS, Pan N, Walters HM, Walsh TJ. Infections in children and adolescents with juvenile idiopathic arthritis and inflammatory bowel disease treated with tumor necrosis factor-inhibitors: systematic review of the literature. Clin Infect Dis. 2013;57(9):1318–30.
Osterman MT, Sandborn WJ, Colombel JF, Peyrin-Biroulet L, Robinson AM, Zhou Q, et al. Crohn’s disease activity and concomitant immunosuppressants affect the risk of serious and opportunistic infections in patients treated with adalimumab. Am J Gastroenterol. 2016;111(12):1806–15.
Strangfeld A, Eveslage M, Schneider M, Bergerhausen HJ, Klopsch T, Zink A, et al. Treatment benefit or survival of the fittest: what drives the time-dependent decrease in serious infection rates under TNF inhibition and what does this imply for the individual patient? Ann Rheum Dis. 2011;301(7):737–44.
Askling J, Fored CM, Brandt L, Baecklund E, Bertilsson L, Feltelius N, et al. Time-dependent increase in risk of hospitalisation with infection among Swedish RA patients treated with TNF antagonists. Ann Rheum Dis. 2007;66(10):1339–44.
Galloway JB, Hyrich KL, Mercer LK, Dixon WG, Fu B, Ustianowski AP, et al. Anti-TNF therapy is associated with an increased risk of serious infections in patients with rheumatoid arthritis especially in the first 6 months of treatment: updated results from the British Society for Rheumatology Biologics Register with special emph. Rheumatology. 2011;50(1):124–31.
Dommasch ED, Abuabara K, Shin DB, Nguyen J, Troxel AB, Gelfand JM. The risk of infection and malignancy with tumor necrosis factor antagonists in adults with psoriatic disease: a systematic review and meta-analysis of randomized controlled trials. J Am Acad Dermatol. 2011;64(6):1035–50.
Fouque-Aubert A, Jette-Paulin L, Combescure C, Basch A, Tebib J, Gossec L. Serious infections in patients with ankylosing spondylitis with and without TNF blockers: a systematic review and meta-analysis of randomised placebo-controlled trials. Ann Rheum Dis. 2010;69(10):1756–61.
Bonovas S, Fiorino G, Allocca M, Lytras T, Nikolopoulos GK, Peyrin-Biroulet L, et al. Biologic therapies and risk of infection and malignancy in patients with inflammatory bowel disease: a systematic review and network meta-analysis. Clin Gastroenterol Hepatol. 2016;14(10):1385–97.
Zhang D, Xiong B, Li X, Xu T, Yu M. Meta-analysis: serious adverse events in Crohn’s disease patients treated with TNF-alpha inhibitors. Hepato-Gastroenterology. 2013;60(126):1333–42.
Galloway JB, Hyrich KL, Mercer LK, Dixon WG, Ustianowski AP, Helbert M, et al. Risk of septic arthritis in patients with rheumatoid arthritis and the effect of anti-TNF therapy: results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2011;70(10):1810–4.
Slifman NR, Gershon SK, Lee JH, Edwards ET, Braun MM. Listeria monocytogenes infection as a complication of treatment with tumor necrosis factor α-neutralizing agents. Arthritis Rheum. 2003;48(2):319–24.
Bodro M, Paterson DL. Listeriosis in patients receiving biologic therapies. Eur J Clin Microbiol Infect Dis. 2013;32(9):1225–30.
Peña-Sagredo JL, Hernández MV, Fernandez-Llanio N, Giménez-Ubeda E, Muñoz-Fernandez S, Ortiz A, et al. Listeria monocytogenes infection in patients with rheumatic diseases on TNF-alpha antagonist therapy: the Spanish Study Group experience. Clin Exp Rheumatol. 2008;26(5):854–9.
Lanternier F, Tubach F, Ravaud P, Salmon D, Dellamonica P, Bretagne S, et al. Incidence and risk factors of legionella pneumophila pneumonia during anti-tumor necrosis factor therapy: a prospective French study. Chest. 2013;144(3):990–8.
Kasahara S, Ando K, Saito K, Sekikawa K, Ito H, Ishikawa T, et al. Lack of tumor necrosis factor alpha induces impaired proliferation of hepatitis B virus-specific cytotoxic T lymphocytes. J Virol. 2003;77(4):2469–76.
Chyuan IT, Hsu PN. Tumor necrosis factor: the key to hepatitis B viral clearance. Cell Mol Immunol. 2018;15(8):731–3.
Terrault NA, Lok ASF, Mcmahon BJ, Chang K-M, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance American Association for the Study of Liver Diseases. Hepatology. 2018;67(4):1560–99.
Chung SJ, Kim JK, Park MC, Park YB, Lee SK. Reactivation of hepatitis B viral infection in inactive HBsAg carriers following anti-tumor necrosis factor-α therapy. J Rheumatol. 2009;36(11):2416–20.
Lan JL, Chen YM, Hsieh TY, Chen YH, Hsieh CW, Chen DY, et al. Kinetics of viral loads and risk of hepatitis B virus reactivation in hepatitis B core antibody-positive rheumatoid arthritis patients undergoing anti-tumour necrosis factor alpha therapy. Ann Rheum Dis. 2011;70(10):1719–25.
Pauly MP, Tucker LY, Szpakowski JL, Ready JB, Baer D, Hwang J, et al. Incidence of hepatitis B virus reactivation and hepatotoxicity in patients receiving long-term treatment with tumor necrosis factor antagonists. Clin Gastroenterol Hepatol. 2018;16(12):1964–73.
Lee YH, Bae SC, Song GG. Hepatitis B virus (HBV) reactivation in rheumatic patients with hepatitis core antigen (HBV occult carriers) undergoing anti-tumour necrosis factor therapy. Clin Exp Rheumatol. 2013;31(1):118–21.
Tamori A, Koike T, Goto H, Wakitani S, Tada M, Morikawa H, et al. Prospective study of reactivation of hepatitis B virus in patients with rheumatoid arthritis who received immunosuppressive therapy: evaluation of both HBsAg-positive and HBsAg-negative cohorts. J Gastroenterol. 2011;46(4):556–64.
Barone M, Notarnicola A, Lopalco G, Viggiani MT, Sebastiani F, Covelli M, et al. Safety of long-term biologic therapy in rheumatologic patients with a previously resolved hepatitis B viral infection. Hepatology. 2015;62(1):40–6.
Myint A, Tong MJ, Beaven SW. Reactivation of hepatitis B virus: a review of clinical guidelines. Clin Liver Dis. 2020;15(4):162–7.
Lopetuso LR, Mocci G, Marzo M, D’aversa F, Rapaccini GL, Guidi L, et al. Harmful effects and potential benefits of anti-tumor necrosis factor (TNF)-α on the liver. Int J Mol Sci. 2018;19(8):2199.
Iannone F, La Montagna G, Bagnato G, Gremese E, Giardina A, Lapadula G. Safety of etanercept and methotrexate in patients with rheumatoid arthritis and hepatitis C virus infection: a multicenter randomized clinical trial. J Rheumatol. 2014;41(2):286–92.
Pompili M, Biolato M, Miele L, Grieco A. Tumor necrosis factor-α inhibitors and chronic hepatitis C: a comprehensive literature review. World J Gastroenterol. 2013;19(44):7867–73.
Winthrop KL, Baddley JW, Chen L, Liu L, Grijalva CG, Delzell E, et al. Association between the initiation of anti-tumor necrosis factor therapy and the risk of herpes zoster. JAMA. 2013;309(9):887–95.
Strangfeld A, Listing J, Herzer P, Liebhaber A, Rockwitz K, Richter C, et al. Risk of herpes zoster in patients with rheumatoid arthritis treated with anti-TNF-α agents. JAMA. 2009;301(7):737–44.
Serac G, Tubach F, Mariette X, Salmon-Céron D, Ravaud P, Lioté F, et al. Risk of herpes zoster in patients receiving anti-TNF-α in the prospective French RATIO registry. J Invest Dermatol. 2012;132(3):726–9.
García-Doval I, Pérez-Zafrilla B, Descalzo MÁ, Roselló R, Hernández MV, Gómez-Reino JJ, et al. Incidence and risk of hospitalisation due to shingles and chickenpox in patients with rheumatic diseases treated with TNF antagonists. Ann Rheum Dis. 2010;69(10):1751–5.
Liao TL, Chen YM, Liu HJ, Chen DY. Risk and severity of herpes zoster in patients with rheumatoid arthritis receiving different immunosuppressive medications: a case-control study in Asia. BMJ Open. 2017;7(1):e014032.
Shalom G, Naldi L, Lebwohl M, Nikkels A, de Jong EMGJ, Fakharzadeh S, et al. Biological treatment for psoriasis and the risk of herpes zoster: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Dermatolog Treat. 2019;30(6):534–9.
Lal H, Cunningham AL, Godeaux O, Chlibek R, Diez-Domingo J, Hwang S-J, et al. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med. 2015;372(22):2087–96.
Dagnew AF, Rausch D, Hervé C, Zahaf T, Levin MJ, Schuind A. Efficacy and serious adverse events profile of the adjuvanted recombinant zoster vaccine in adults with pre-existing potential immune-mediated diseases: a pooled post hoc analysis on two parallel randomized trials. Rheumatology. 2021;60:1226–33.
Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, et al. Recommendations of the Advisory Committee on Immunization Practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103–8. [cited 2021 May 10]. http://www.cdc.gov/mmwr/volumes/67/wr/mm6703a5.htm?s_cid=mm6703a5_w.
Furer V, Rondaan C, Heijstek MW, Agmon-Levin N, Van Assen S, Bijl M, et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis. 2020;79(1):39–52.
Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352(22):2271–84.
Schmader KE, Levin MJ, Gnann JW, McNeil SA, Vesikari T, Betts RF, et al. Efficacy, safety, and tolerability of herpes zoster vaccine in persons aged 50-59 years. Clin Infect Dis. 2012;54(7):922–8.
Filler SG, Yeaman MR, Sheppard DC. Tumor necrosis factor inhibition and invasive fungal infections. Clin Infect Dis. 2005;41(Suppl 3):S208–12.
Vergidis P, Avery RK, Wheat LJ, Dotson JL, Assi MA, Antoun SA, et al. Histoplasmosis complicating tumor necrosis factor-α blocker therapy: a retrospective analysis of 98 cases. Clin Infect Dis. 2015;61(3):409–17.
Wallis RS, Broder MS, Wong JY, Hanson ME, Beenhouwer DO. Granulomatous infectious diseases associated with tumor necrosis factor antagonists. Clin Infect Dis. 2004;38(9):1261–5.
Kaur N, Mahl TC. Pneumocystis jiroveci (carinii) pneumonia after infliximab therapy: a review of 84 cases. Dig Dis Sci. 2007;52(6):1481–4.
Harigai M, Koike R, Miyasaka N. Pneumocystis pneumonia associated with infliximab in Japan. N Engl J Med. 2007;357(18):1874–6.
Warris A, Bjørneklett A, Gaustad P. Invasive pulmonary aspergillosis associated with infliximab therapy. N Engl J Med. 2001;344(14):1099–100.
Baddley JW, Winthrop KL, Chen L, Liu L, Grijalva CG, Delzell E, et al. Non-viral opportunistic infections in new users of tumour necrosis factor inhibitor therapy: results of the SAfety assessment of biologic ThERapy (SABER) study. Ann Rheum Dis. 2014;73(11):1942–8.
Tsiodras S, Samonis G, Boumpas DT, Kontoyiannis DP. Fungal infections complicating tumor necrosis factor α blockade therapy. Mayo Clin Proc. 2008;83(2):181–94.
Wallis RS, Broder M, Wong J, Lee A, Hoq L. Reactivation of latent granulomatous infections by infliximab. Clin Infect Dis. 2005;41(Suppl 3):S194–8.
Bergstrom L, Yocum DE, Ampel NM, Villanueva I, Lisse J, Gluck O, et al. Increased risk of coccidioidomycosis in patients treated with tumor necrosis factor α antagonists. Arthritis Rheum. 2004;50(6):1956–66.
Taroumian S, Knowles SL, Lisse JR, Yanes J, Ampel NM, Vaz A, et al. Management of coccidioidomycosis in patients receiving biologic response modifiers or disease-modifying antirheumatic drugs. Arthritis Care Res. 2012;64(12):1903–9.
Olson TC, Bongartz T, Crowson CS, Roberts GD, Orenstein R, Matteson EL. Histoplasmosis infection in patients with rheumatoid arthritis, 1998-2009. BMC Infect Dis. 2011;11:145.
Takeuchi T, Tatsuki Y, Nogami Y, Ishiguro N, Tanaka Y, Yamanaka H, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis. 2008;67(2):189–94.
Dixon WG, Watson K, Lunt M, Hyrich KL, Silman AJ, Symmons DPM. Rates of serious infection, including site-specific and bacterial intracellular infection, in rheumatoid arthritis patients receiving anti-tumor necrosis factor therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2006;54(8):2368–76.
Louie GH, Wang Z, Ward MM. Trends in hospitalizations for Pneumocystis jiroveci pneumonia among patients with rheumatoid arthritis in the US: 1996-2007. Arthritis Care Res. 2010;62(12):3826–7.
Ferri C, Ferraccioli G, Ferrari D, Galeazzi M, Lapadula G, Montecucco C, et al. Safety of anti-tumor necrosis factor-α therapy in patients with rheumatoid arthritis and chronic hepatitis C virus infection. J Rheumatol. 2008;35(10):1944–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chua, J.V., Baddley, J.W. (2022). Anti-tumor Necrosis Factor-Alpha Agents. In: Cervera, C., Aguado, J.M. (eds) Infectious Complications in Biologic and Targeted Therapies. Springer, Cham. https://doi.org/10.1007/978-3-031-11363-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-11363-5_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-11362-8
Online ISBN: 978-3-031-11363-5
eBook Packages: MedicineMedicine (R0)