Abstract
Drug hypersensitivity (DH) is a growing problem worldwide. Although the exact mechanism is not well understood, it is considered immune-mediated. Drug hypersensitivity reactions are primarily classified into immediate or delayed type reactions and their presentation range from mild skin reactions [e.g., maculopapular exanthema (MPE) and urticaria] to severe life-threatening systemic reactions, such as drug reactions with eosinophilia and systemic symptoms (DRESS), Stevens–Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP) and anaphylaxis. There are four postulated models to explain the interaction between drugs, human leukocyte antigens (HLA), and T cell receptors (TCR): (1) apten theory, (2) p–i concept, (3) altered peptide repertoire model, and the (4) altered T cell receptor (TCR) repertoire. Current pharmacogenomic studies have shown that pre-prescription screening of HLAs and drug-metabolizing enzymes variants may prevent severe cutaneous adverse reactions. The basic understanding of the mechanisms of DH would serve as a platform for future approaches to prevent and treat such diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Drug hypersensitivity
- Human leukocyte antigens (HLA)
- Severe cutaneous adverse drug reactions (SCARs)
- T-cell receptor (TCR)
- Drug reaction with eosinophilia and systemic symptoms (DRESS)
- Stevens–Johnson syndrome (SJS)
- Toxic epidermal necrolysis (TEN)
- Acute generalized exanthematous pustulosis (AGEP)
1 Introduction
Drug hypersensitivity reactions (DH) is a growing problem worldwide. These reactions are immune-mediated and are traditionally classified according to Gell and Coombs’s criteria (Fig. 1) (Johansson et al. 2001). Type I reactions are immunoglobulin-E (IgE) mediated and their clinical presentations include urticaria, angioedema, bronchospasm, gastrointestinal symptoms, giddiness, and anaphylactic shock. They typically occur within the first hour of drug administration; hence, they are also known as immediate reactions (Montanez et al. 2017). Such reactions are more likely to be caused by small antigens (e.g., drug haptens), proteins, and high-molecular-weight peptides. Type II reactions, on the other hand, are usually IgG- and IgM-mediated. Drugs acting as antigens interact with membrane-bound IgG or IgM and the subsequent clearance by macrophages result in further cell destruction. Red blood cells, platelets, and neutrophils may also be involved in type II reaction. The incidence of type II reaction is relatively rare as the drug exposure needs to be of significant duration and dose in order for drug-specific antibodies to be produced. Type III reactions are mediated by antigen–antibody complexes. Circulating immune complexes formed by the binding of IgG (occasionally IgM) to the drug are deposited in various tissues, such as the blood vessels, joints, and renal glomeruli. These immune complexes activate the complement cascade and induce local inflammation, causing fever, urticaria, vasculitis, arthralgia, and serum sickness (Wedi 2010). Similar to type II reaction, type III reactions are less common and usually occur with prolonged drug usage. Lastly, type IV reactions are CD 4+ and CD8+ T-cell-mediated and these reactions usually take several days or even weeks to manifest following drug exposure. Recent studies have highlighted significant association between class I and/or II HLA alleles and T cell-mediated SCARs and this serves as a platform for screening and prevention of such reactions (Pichler 2002). The clinical presentation of type IV reactions ranges from maculopapular exanthem (MPE) to life-threatening SCARs (severe cutaneous adverse drug reactions), including drug reaction with eosinophilia and systemic symptoms (DRESS), Stevens–Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN), and acute generalized exanthematous pustulosis (AGEP) (Valeyrie-Allanore et al. 2007).
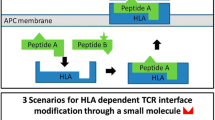
2 Models of Drug Antigen Presentation
There are four hypotheses that have been proposed to explain the interactions between drug, HLA, and T cells (Fig. 2): (1) the “hapten–prohapten” theory, (2) the “p–i concept,” (3) the “altered peptide repertoire” model, and (4) the “altered TCR repertoire” model (Valeyrie-Allanore et al. 2007; Watkins and Pichler 2013). In the hapten–prohapten theory, a drug or its metabolite interacts with endogenous peptide covalently to form an antigenic hapten complex. In this model, the recognition of the hapten complex by T cells results in T cell activation and downstream responses (Padovan et al. 1997). In the “p–i” model, the drug can directly bind to the self-peptide when the peptide is presented by the antigen-presenting cells (APC). For example, carbamazepine (CBZ) can directly interact with HLA-B*15:02 protein. Appropriate loading of endogenous peptides to HLA-B*15:02 is required for the stability of the HLA complex to present CBZ to T cells. Unlike the hapten model, this binding occurs without intracellular antigen presentation or drug metabolism (Wei et al. 2012). In the “altered peptide repertoire” model, binding of the drug (e.g., abacavir) to HLA protein results in a conformational change, thereby altering peptide specificity of HLA binding (Ostrov et al. 2012). Finally, in the “altered TCR repertoire” model, binding of the drug to the specific TCR results in a secondary structural alteration of the TCR, which results in the interaction with HLA-self-peptides (Watkins and Pichler 2013). For example, upon specific drug binding, the drug–TCR complex will trigger activation and expansion of cytotoxic T lymphocytes (CTL) (Naisbitt et al. 2003) with downstream production of cytotoxic proteins (Chung et al. 2008).
Models of the interaction of human leukocyte antigen (HLA), drug, and T-cell receptor (TCR). (1) The “hapten–prohapten” theory. Drugs/metabolites bind covalently with the endogenous peptides that are processed conventionally in antigen-presenting cells (APC) to form the drug–HLA–TCR complex. (2) The “p–i” model theory. Drugs directly bind to the HLA–peptide complex or TCR, this response is independent on process in APC. (3) The “altered peptide repertoire” theory. Drugs bind to a specific altered peptide repertoire but may not directly bind to HLA, and thus interact with TCR to promote the drug-specific T-cell activation. (4) The “altered TCR repertoire” model. Drugs bind to TCR directly cause conformational change of TCR. This modified drug–TCR structure has the potential to bind HLA–self-peptide complex
3 Genetic Factors in Drug Hypersensitivity
Most cases of drug hypersensitivity are unpredictable. However, recent publications have shown that in some reactions, genetic variants, particularly those involved in HLAs and drug-metabolizing enzymes may play a role. Screening for these at-risk variants is a potential preventive strategy. The genetic factors involved in both immediate and delayed type reactions are summarized below.
3.1 Genetic Factor in Immediate-Type Drug Hypersensitivity
Immediate-type drug hypersensitivity reactions arising from the use of β-lactams, aspirin, and other NSAIDs have been shown to have pharmacogenetics association. HLA genes such as HLA-DR4, HLA-DR9, HLA-DR14.1, and HLA-DR17 have been linked to penicillin-induced immediate hypersensitivity reactions in Chinese (Yang et al. 2006), whereas HLA-DRA rs7192 and HLA-DRA rs8084 are associated with penicillin/amoxicillin-induced immediate hypersensitivity reactions in Spanish and Italians (Gueant et al. 2015). The association between DRB1*13:02 and HLA-DRB1*06:09 with aspirin-induced urticaria and angioedema has been reported (Kim et al. 2006). In addition, DRB1∗11 has been shown to be associated with aspirin/NSAIDs-induced urticaria/angioedema and hypotension/laryngeal edema (Quiralte et al. 1999). Interestingly, both aspirin/NSAID-induced chronic idiopathic urticaria and aspirin/NSAID-induced hypersensitivity reactions are associated with HLA-B44 and HLA-Cw5 (Pacor et al. 2006). Besides HLA genes, genetic variants of cytokines (such as TGFB1, TNF, and IL18) have also been shown to mediate β-lactams and aspirin-induced hypersensitivity (Kim et al. 2011a; Choi et al. 2009; Qiao et al. 2005; Yang et al. 2005). The genes belonging to arachidonic acid pathway (ALOX15, ALOX5, ALOX5AP, CYSLTR1, PTGDR, and TBXAS1) are also involved in NSAIDs-mediated hypersensitivity (Cornejo-Garcia et al. 2012; Oussalah et al. 2016).
3.2 Genetic Factor in Delayed-Type Drug Hypersensitivity
As shown in Fig. 3, following exposure to an offending drug, a drug–peptide complex is formed and this interacts with a specific HLA of an antigen-presenting cells. This is subsequently recognized by the TCR of T cells, resulting in the initiation of delayed-type drug hypersensitivity. Various HLA alleles have been reported in association with SJS/TEN. Such associations are drug and ethnicity-specific and are summarized in Table 1 (Yang et al. 2006; Gueant et al. 2015; Kim et al. 2006; Quiralte et al. 1999; Pacor et al. 2006; Romano et al. 1998; Mallal et al. 2002; Hung et al. 2005; Martin et al. 2005; Littera et al. 2006; Gatanaga et al. 2007; Locharernkul et al. 2008; Lonjou et al. 2008; Saag et al. 2008; Chantarangsu et al. 2009; Kazeem et al. 2009; Hung et al. 2010; Ikeda et al. 2010; Kaniwa et al. 2010; Kim et al. 2010; Kim et al. 2011b; McCormack et al. 2011; Ozeki et al. 2011; Somkrua et al. 2011; Chung and Hung 2012; Cheung et al. 2013; Tangamornsuksan et al. 2013; Zhang et al. 2013; Chung et al. 2014; Genin et al. 2014; Tassaneeyakul et al. 2016; Chang et al. 2017; Chen et al. 2017; Konvinse et al. 2019; Mockenhaupt et al. 2019; Tangamornsuksan and Lohitnavy 2019).
The pathogenic factors involved in drug hypersensitivity. Different drug-antigen presentation mechanisms and pathogenic factors influence the development of drug hypersensitivity. These include genetic polymorphisms in human leukocyte antigen (HLA), drug antigen presentation of specific HLA/drug/TCR complex and T cell-mediated immune responses such as cytotoxic protein secretion cause tissue destruction
3.2.1 Allopurinol
Allopurinol is a xanthine oxidase inhibitor that is frequently prescribed for the treatment of gout. Initial comparison between cases of allopurinol-induced SCARs and tolerant controls showed a strong association of HLA-B*58:01, with this HLA being present in all cases of allopurinol SCARs (Hung et al. 2005). This strong association was subsequently reproduced in different ethnicities, including Han Chinese, Thai populations (Lonjou et al. 2008; Somkrua et al. 2011) as well as in Korean, Japanese, and European populations, thereby validating HLA-B*58:01 as a useful predictive biomarker for allopurinol induced SCARs. It is therefore reasonable for allopurinol to be contraindicated in patients who are positive for HLA-B∗58:01 (Hung et al. 2005). However, in our follow-up study, only 84%, and not 100%, of Chinese patients with allopurinol hypersensitivity carried the HLA-B∗58:01 allele. The low positive predictive value and variable negative predictive value of HLA-B∗58:01 for allopurinol-induced SCARs suggest that other factors may contribute to the pathogenesis of allopurinol-induced SCARs (Ng et al. 2016).
3.2.2 Aromatic Anticonvulsants
Aromatic anticonvulsants such as CBZ, oxcarbazepine (OXC), phenytoin (PHT), and lamotrigine (LTG) are high-risk drugs for drug hypersensitivity reactions. We first reported a strong association between CBZ and HLA-B∗15:02 in patients who developed SJS/TEN in Taiwan in 2004 (Chung et al. 2004). Since then, other aromatic antiepileptic drugs, such as PHT (Locharernkul et al. 2008), OXC (Chen et al. 2017), and LTG (Shi et al. 2011), have also been shown to have a positive association with HLA-B*15:02 allele for SJS/TEN. This allele has been further validated in different populations from Thailand, Malaysia, Singapore, and India (Locharernkul et al. 2008; Tangamornsuksan et al. 2013). Based on these results, the genetic screening of HLA-B∗15:02 prior to the initiation of CBZ has been recommended in some Asian populations (Ferrell Jr. and McLeod 2008). On the other hand, HLA-A*31:01 allele has been identified as a risk factor for CBZ-induced DRESS, but not of CBZ-induced SJS/TEN in Europeans, Han Chinese, and Koreans (Kim et al. 2011b; Genin et al. 2014; Hung et al. 2006). HLA-A*31:01 was also shown to be associated with CBZ-induced cutaneous adverse drug reactions (ADR) across the spectrum, from MPR to DRESS, and SJS/TEN in the Japanese (McCormack et al. 2011; Ozeki et al. 2011). For CBZ-induced SJS/TEN in Europeans, a recent study from RegiSCAR group showed that HLA-B*57:01, instead of HLA-A*31:01, was a risk factor (Mockenhaupt et al. 2019). Lastly, HLA-B∗15:11 allele was shown to be associated with carbamazepine-induced SJS/TEN in Japanese and Korean populations as well (Kaniwa et al. 2010; Kim et al. 2011b).
3.2.3 Abacavir
Abacavir is used in the treatment of HIV infection and is also a high notoriety drug for drug hypersensitivity reactions. In 2002, two studies demonstrated that HLA-B*57:01 was a risk factor for abacavir-related hypersensitivity (Mallal et al. 2002; Hetherington et al. 2002). In addition, it has been shown that 44% of white study participants and 100% of black participants with the HLA-B*57:01 allele experienced abacavir-induced hypersensitivity (Saag et al. 2008). A further randomized trial confirmed that screening for HLA-B*57:01 as an effective measure for the prevention of abacavir induced hypersensitivity (Mallal et al. 2008).
3.2.4 Other Drugs
Several other antibiotic-induced hypersensitivity reactions and pharmacogenomic associations have been reported. These include HLA-B*38 and sulfamethoxazole (Lonjou et al. 2008), HLA-B*13:01 and dapsone-induced hypersensitivity syndrome (Zhang et al. 2013), HLA-A*32:01 and vancomycin-induced DRESS (Konvinse et al. 2019) as well as HLA-A*2 and DRW52 in aminopenicillins-induced DRESS (Romano et al. 1998). Nevirapine-induced MPE or DRESS is associated with HLA-DRB1*01:01 in Western Australia (Shepherd et al. 2005), B*14:02 in Caucasians in Sardinians (Littera et al. 2006), HLA-B*35:05 in Thailand (Chantarangsu et al. 2009), and HLA-Cw8 in Japan (Gatanaga et al. 2007). Other associations include HLA-B*59:01 and methazolamide-induced SJS/TEN (Kim et al. 2010; Tangamornsuksan and Lohitnavy 2019), HLA-B*73:01 and oxicam-induced SJS/TEN (Lonjou et al. 2008).
4 Drug Metabolism in SCARs
In addition to pharmacogenetic associations , individual drug metabolism and clearance are also critical factors that influence susceptibility and prognosis of SCARs. Individuals with rapid drug clearance may be at a lower risk of developing SCARs. This is illustrated in genetic variants of CYP2C9*3 and PHT-related SCAR (Chung et al. 2014). CYP2C9*3 attenuates the clearance of PHT and patients with phenytoin-associated SCAR patients who carried the CYP2C9*3 showed a delayed clearance of plasma PHT, resulting in an increase of PHT toxicity and a higher likelihood of hypersensitivity reactions (Chung et al. 2014). Other examples include the strong association between CYP3A5*3 and antiepileptics-induced hypersensitivity reactions (Tanno et al. 2015) as well as CYP2B6, with nevirapine-induced SJS/TEN (Ciccacci et al. 2013).
Another example illustrating the role of drug metabolism and dosage is in allopurinol SCARS. High starting doses of allopurinol and renal impairment are known risk factors. Renal impairment or chronic kidney disease impacts the clearance of oxypurinol (the metabolite of allopurinol). This leads to elevated plasma concentrations and a higher risk of SCARs (Chung et al. 2015a). In addition, the coexistence of renal impairment and HLA-B*58:01 increase the risk of allopurinol-induced cutaneous adverse drug reactions (heterozygous HLA-B*58:01 and normal renal function: OR: 15.25, specificity: 82%; homozygous HLA-B*58:01 and severe renal impairment: OR: 1269.45, specificity: 100%) (Ng et al. 2016). These results suggests that allopurinol should be avoided in patients with coexisting HLA-B*58:01 and renal impairment.
5 Immune Mechanisms in DH
5.1 Immediate-Type: IgE-Mediated DH
Type I DH reactions are mainly mediated by mast cells and basophils activation via allergic (IgE-mediated) or nonallergic (non-IgE-mediated) mechanisms (Fig. 4). Type I DH response can be systemic or local in nature and generally arises due to the cross-linking of membrane-bound IgE antibodies on the basophil/mast cell with antigens. The cross-linkage of drug antigens to Ig-E bound high-affinity Fc receptor (FcεRI) located on mast cells/basophils results in degranulation and the release of mediators. These mediators include histamine, leukotrienes, and prostaglandins which are responsible for the clinical features of urticaria, angioedema, or anaphylaxis (Moon et al. 2014; Schnyder and Pichler 2009). In contrast, NSAIDs (except pyrazolones) are believed to cause anaphylaxis via an aberrant arachidonic acid metabolism pathway or selective T cell-mediated mechanism instead of the classical IgE-mediated pathway (Blanca-Lopez et al. 2016; Canto et al. 2009; Brockow et al. 2013). Other non-IgE mechanisms include those mediated by IgG antibodies, complement or via contact system activation. The clinical presentation of these alternative pathways is indistinguishable from IgE-mediated anaphylaxis (Munoz-Cano et al. 2016; Finkelman et al. 2016). The cross linkage of drugs with drug-specific IgG bound to FcγRIII stimulates the release of platelet activation factor (PAF) from basophils, macrophages, or neutrophils (Finkelman et al. 2016). This IgG immune-complex can trigger further complement activation. Another non-Ig E mechanism is via the contact system activation of complements. Upon activation, bradykinin formation is initiated and this may play a role in anaphylaxis (Finkelman et al. 2016). Reactions to radiocontrast media, dextran, and some NSAIDs are postulated to occur via these non-Ig E pathways (Wedi 2010; Dona et al. 2016; Laroche et al. 1999; Kishimoto et al. 2008). Finally, nonimmunologic mechanisms may be involved in anaphylaxis: Direct mast cell degranulation via MAS-related G protein-coupled receptor-X2 (MRGPRX2) has been shown. This pathway may mediate reactions that are caused by quinolones, vancomycin, and neuromuscular blocking drugs (Subramanian et al. 2016).
Multiple mechanisms and pathways involved in anaphylaxis. The pathways of anaphylaxis can be classified into immunological and nonimmunological depending on the underlying mechanism. Immunological anaphylaxis can be mediated by an IgE, IgG, and complement mechanism, whereas nonimmunological anaphylaxis involves contact system activation and direct stimulation
5.2 Delayed-Type: T Cells Mediated DH
Delayed reactions vary in severity. MPEs are generally benign, whereas SCARs such as DRESS, SJS/TEN, and AGEP are associated with significant morbidity and/or mortality. The mechanisms differ across diseases and are summarized below.
5.2.1 MPE (Type Iva)
In MPE, the activation of CD4+ T cells through drug presentation by antigen presenting cells leads to the release of inflammatory cytokines such as interferon-gamma (IFN-γ). IFN-γ further activates macrophages and amplifies the release of cytokines and chemokines that recruit additional monocytes (Pichler 2003).
5.2.2 DRESS Syndrome (Type IVb)
DRESS is characterized by peripheral blood eosinophil activation (Rive et al. 2013) and high serum levels of cytokines and chemokines, such as interleukin-4 (IL-4), interleukin-5 (IL-5), interleukin-13 (IL-13), and thymus and activation-regulated chemokine (TARC)/CC chemokine ligand 17 (Choquet-Kastylevsky et al. 1998; Teraki and Fukuda 2017). This profile suggests a Th2-type immune response as the dominant pathway. As the disease progresses from acute to subacute and resolution phases, there is a corresponding transition from an initial Treg expansion to Th17 cell expansion (Hashizume et al. 2016; Fujiyama et al. 2014; Olteanu et al. 2019). In addition, it has recently been shown that type 2 innate lymphoid cells were increased both in the skin and serum of patients with DRESS. These were associated with high levels of serum ST-2, IL-5 and TSLP as well as increased expression of IL-33/ST-2 expression in type 2 innate lymphoid cells. These markers may mediate the skin inflammation in DRESS and serum ST2 may be a biomarker for liver involvement in DRESS (Tsai et al. 2019). The CXCL3/CXCR10 axis has also been found to be associated with the development of long-term sequelae and HHV-6 reactivation in DRESS (Yang et al. 2020; Chen et al. 2015). More recently, the JAK-STAT (Janus kinase-signal transducer and activator of transcription) pathway has been recently shown to be a possible disease pathway in DRESS. In a patient with severe DRESS, the use of tofacitinib (JAK1 and JAK3 inhibitor) brought about control of disease (Kim et al. 2020). The mechanisms in DRESS are summarized in Fig. 5.
The pathomechanisms in DRESS. Th2 and ST2 membrane-bound ILC2 are activated by TARC/CCL17 and IL-33 which is released from dendritic cells and monocytes. Subsequently, activated T cells produce various cytokine including IL-4, IL-5 and IL-13 as chemoattractant to cause recruitment of eosinophils. In addition, CD8 T cells may observed in skin lesion
5.2.3 SJS/TEN (Type IVc)
The central hypothesis to explain SJS/TEN is the activation of CTLs/nature killer (NK) cells and the release of cytotoxic proteins. Three cytotoxic proteins, granulysin, perforin/granzyme B, and Fas–FasL, are thought to be the major mediators responsible for the extensive skin necrosis in SJS/TEN (Fig. 6).
The pathomechanisms involved in SJS/TEN. CTLs are activated through the antigen (drug) presentation by the antigen presenting cell (APC) and subsequently carry out the cellular immune reactions directed at keratinocytes. Upon activation, CTLs release various cytotoxic proteins, including granulysin, perforin/granzyme B, Fas/Fas ligand, and other cytokines/chemokines resulting in disseminated keratinocyte death in skin lesions. These toxic signals in turn regulate trafficking, proliferation, and activation of T cells and other immune cells to amplify the reaction
5.2.3.1 Granulysin
Granulysin belongs to the saposin-like protein (SAPLIP) family. It is expressed on activated CTL and NK cells and is involved in cell cytotoxicity. The transcription and expression of granulysin is much higher compared to perforin, granzyme B, and soluble Fas ligand (sFasL) in blister fluids, suggesting it is the most important mediator for necrolysis. This is further supported in mice studies, whereby SJS/TEN-like lesions were replicated following granulysin injections (Chung et al. 2008). Serum granulysin is elevated during the early stage of SJS/TEN, suggesting its role as an early diagnostic marker of SJS/TEN (Abe et al. 2009). Moreover, granulysin is a chemoattractant and is involved in the recruitment of antigen-presenting cells (APCs) thereby amplifying the specific immune response. Pro-inflammatory cytokines released from these inflammatory cells include Regulated upon Activation, Normal T-cell Expressed, and Secreted (RANTES), chemokine (C–C motif) ligand (CCL)5, monocyte chemotactic protein (MCP)-1, MCP-3, macrophage inflammatory protein-1a, CCL3, interleukin (IL)-10, IL-1, IL-6, and interferon (IFN)-α (Deng et al. 2005).
5.2.3.2 Perforin/Granzyme B Pathway
Perforin and granzyme B are stored within the cytotoxic granules of activated CTL and NK cells (Bots and Medema 2006). When activated, perforin would punch a pore on the membrane of keratinocytes, promoting the entry of granzyme B which induces apoptosis via caspase pathways (Pinkoski et al. 2001; Nassif et al. 2002). Prior studies have shown that blister lymphocytes were cytotoxic in nature and these cytotoxic effects were abrogated by blocking the perforin/granzyme pathway and not with anti-Fas monoclonal antibody (Nassif et al. 2002).
5.2.3.3 NK Cells
NK cells are found in the blister fluid of SJS/TEN patients (Chung et al. 2008) suggesting that NK cells are important immune effectors for epidermal detachment in SJS/TEN. The cytotoxicity of NK cells is regulated by activation and inhibitory signals through the surface NK receptors (Lanier 2005). It has been reported that the activation receptor CD94/NKG2C is found in NK cells and the expression of its soluble ligand HLA-E is increased in the keratinocytes of SJS/TEN patients (Morel et al. 2010).
5.2.3.4 Fas–FasL Interaction
It is first reported that the activated Fas–Fas ligand (FasL) binding may play a role in the apoptosis of keratinocytes in SJS/TEN (Viard et al. 1998). In TEN patients, FasL was reported to be found on both the keratinocyte surface and also in high levels within the circulation (Viard et al. 1998). However, the exact role of Fas–FasL remains controversial as a later study was unable to demonstrate the expression of membrane-bound FasL on keratinocytes in either patients with TEN or healthy controls even though elevated levels of sFasL in SJS/TEN were detected (Abe et al. 2003).
5.2.3.5 Annexin A1–FPR1 Interaction
Annexin A1 was identified in the supernatants of specific drug-stimulated PBMCs of SJS/TEN patients by mass spectrometric analysis (Saito et al. 2014). In a fraction of keratinocytes in the SJS/TEN, cell death was shown to be mediated through programmed cell necrosis or necroptosis. This process is initiated by annexin-1 binding to FPR1 (the receptor for annexin A1) which is expressed on keratinocytes (Saito et al. 2014). Also, high levels of RIP3 expression in the epidermis of patients with SJS/TEN were also found (Saito et al. 2014; Kim et al. 2015). RIP3-mediated phosphorylation and activation of MLKL (a key downstream component of RIP3) was detected in the necrotic keratinocytes, supporting the hypothesis of necroptosis as one of the cell death mechanisms in SJS/TEN (Kim et al. 2015).
5.2.3.6 Cytokines/Chemokines Involved in the Cell Immunity of SJS/TEN
Several studies have shown increased expression of certain cytokines/chemokines in the blister fluid, plasma, blister cells, or peripheral mononuclear cells of patients with SCARs. TNF-α, which induces cell apoptosis, activation, differentiation and inflammation, is increased in lesional skin of TEN patients (Chavez-Galan et al. 2009; Paquet et al. 1994). Increased serum levels of TNF-α and IFN-γ as well as inducible FasL expression have been demonstrated in TEN (Viard-Leveugle et al. 2013). Interleukin-15 (IL-15) is a cytokine which is able to induce the proliferation of natural killer cells as well as other leukocytes. In SJS/TEN, the levels of IL-15 and granulysin showed positive correlation with disease severity. Furthermore, IL-15 was associated with mortality of SJS/TEN and shown to enhance cytotoxicity of cultured natural killer cells and blister cells from patients with TEN (Su et al. 2017). In addition to TNF-α, IFN-γ, and IL-15, other cytokines such as IL-5, IL-6, IL-10, IL-12, IL-13, IL-18, CCR3, CXCR3, CXCR4, and CCR10 may be responsible for the trafficking, proliferation, regulation or activation of T cells and other leukocytes involved in SJS/TEN (Paquet et al. 2000; Correia et al. 2002; Nassif et al. 2004; Tapia et al. 2004; Caproni et al. 2006).
5.2.4 AGEP (Type IVd)
The activation , proliferation, and migration of drug-specific CD4+ and CD8+ T cells play an important role in the development of AGEP (Choi et al. 2010; Belhadjali et al. 2008). Drug-specific T cells produces chemotactic chemokine (C–X–C motif) ligand 8 (CXCL8)/IL-8 which contributes to the recruitment of neutrophils in AGEP (Schaerli et al. 2004). In AGEP, high levels of circulating Th17 cells and the elevated serum IL-17 and IL-22 may stimulate keratinocytes to produce IL-8 (Kabashima et al. 2011). This increase in the levels of IL-17 and IL-22 as well as granulocyte–macrophage colony-stimulating factor (GM-CSF) works synergistically with CXCL8/IL-8 –induced neutrophilic activity and prevents apoptosis of neutrophils (Kabashima et al. 2011). Mutations in IL-36 receptor antagonist gene (IL36RN) contribute to recruitment of neutrophils via production of pro-inflammatory cytokines, such as IL-1, IL-6, and IL-8 (Navarini et al. 2013). In AGEP, dysregulation of IL-36 signaling pathway is postulated to drive the neutrophilic process; IL-36 production derived from blood monocytes and keratinocytes triggers the release of IL-8 from peripheral blood mononuclear cells (Meier-Schiesser et al. 2019). The immune mechanisms for AGEP are summarized in Fig. 7.
The summarized mechanism in AGEP development. Drug-specific CD4 and CD8 T cells play an important role in the development of AGEP. T cells and keratinocytes release various chemokines and cytokines such as CXCL8/IL-8, IL-17, IL-22, GM-CSF, and IL-36 which recruits and activates neutrophils. Cellular damage is mediated through neutrophils and their mediators
6 T Cell Receptor (TCR) Repertoire in Drug Hypersensitivity
In allopurinol-induced SCAR , preferential TCR-V-β usage and clonal expansion of specific CDR3 (third complementarity-determining region) were found in the blister cells of allopurinol induced SCAR (Chung et al. 2015b). These data suggest that, in addition to HLA-B*58:01, clonotype-specific T cells expressing granulysin upon oxypurinol induction are involved in the pathogenesis of allopurinol-induced SCAR.
In CBZ-induced SJS/TEN , CBZ-specific T cells are restricted by HLA-B*15:02 and only a few heavy chain residues allow for CBZ presentation. A restricted TCR clonotype has been identified, and is responsible for the recognition of carbamazepine within the context of HLA-B*15:02 (Wei et al. 2012). Recently, the role of TCR repertoire was further validated in the demonstration of public αβTCR of CTL being involved in immune synapses mediating SCARs (Pan et al. 2019). Furthermore, adoptive transfer of T cells expressing this public αβTCR to HLA-B*15:02 transgenic mice receiving CBZ resulted in multiorgan injuries similar to SCARs (Pan et al. 2019). These findings suggest potential clinical applications of TCR in therapeutics (Pan et al. 2019). In addition, expanded clones and a less diverse TCR repertoire have been found to be associated with clinical severity of disease in patients with SJS/TEN by systematic sequence analysis for TCRβ (Xiong et al. 2019).
In the “altered TCR repertoire” model, drugs (such as sulfamethoxazole) alter the conformation of a specific TCR, thereby facilitating the binding of HLA–self-peptide complex (Watkins and Pichler 2013). In this model, the causative drug directly interacts with this specific TCR, but not with the peptides or HLA molecules.
In contrast, in the “altered peptide repertoire ” model, binding of the drug (e.g., Abacavir) to HLA protein results in a conformational change, thereby altering peptide specificity of HLA binding (Ostrov et al. 2012; Illing et al. 2012). This was demonstrated in the abacavir model, whereby the binding of abacavir to the F-pocket of HLA-B*57:01, altered the shape and chemistry of the antigen-binding cleft. The binding of self-peptides to these antigen-binding clefts result in “polyclonal” T cell activation and autoimmune-like systemic reaction manifestations. An abacavir-stimulated patch test–positive skin in a patient 14 years after abacavir-induced DH was also shown to have “polyclonal” memory T-cell responses, adding further support for the altered peptide model (Redwood et al. 2019).
7 Conclusion
The mechanism of drug hypersensitivity is complex and not entirely understood. In this chapter, we summarize the genetic factors and different immune mechanism that are involved in drug specific allergic and nonallergic responses. Although the optimal therapeutic strategies for drug hypersensitivity remain unclear, an understanding of these mechanisms would pave the way for novel therapeutic approaches.
Abbreviations
- ADR:
-
Adverse drug reactions
- APC:
-
Antigen-presenting cells
- CBZ:
-
Carbamazepine
- CCL:
-
Chemokine (C–C motif) ligand
- CTL:
-
Cytotoxic T lymphocytes
- CXCL8 :
-
Chemotactic chemokine (C–X–C motif) ligand 8
- CYP2C:
-
Cytochrome P450 2C
- DH:
-
Drug hypersensitivity
- DRESS:
-
Drug reaction with eosinophilia and systemic symptoms
- FADD:
-
Fas-associated death domain
- GM-CSF:
-
Granulocyte–macrophage colony-stimulating factor
- HLA:
-
Human leukocyte antigen
- IFN:
-
Interferon
- IL:
-
Interleukin
- LTG:
-
Lamotrigine
- MCP:
-
Monocyte chemotactic protein
- MPE:
-
Mild maculopapular exanthema
- NK:
-
Nature killer
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- OXC:
-
Oxcarbazepine
- OXP:
-
Oxypurinol
- PHT:
-
Phenytoin
- RANTES:
-
Regulated upon activation, normal T-cell expressed, and secreted
- SAPLIP:
-
Saposin-like protein
- SCAR:
-
Severe cutaneous adverse reactions
- sFASL:
-
Soluble Fas ligand
- SJS:
-
Stevens–Johnson syndrome
- TCR:
-
T-cell receptors
- TEN:
-
Toxic epidermal necrolysis
- TNF-α:
-
Tumor necrosis factor-α
References
Abe R, et al. Toxic epidermal necrolysis and Stevens–Johnson syndrome are induced by soluble Fas ligand. Am J Pathol. 2003;162(5):1515–20.
Abe R, et al. Granulysin as a marker for early diagnosis of the Stevens–Johnson syndrome. Ann Intern Med. 2009;151(7):514–5.
Belhadjali H, et al. Mercury-induced acute generalized exanthematous pustulosis misdiagnosed as a drug-related case. Contact Dermat. 2008;59(1):52–4.
Blanca-Lopez N, et al. Immediate hypersensitivity reactions to ibuprofen and other arylpropionic acid derivatives. Allergy. 2016;71(7):1048–56.
Bots M, Medema JP. Granzymes at a glance. J Cell Sci. 2006;119(Pt 24):5011–4.
Brockow K, et al. Skin test concentrations for systemically administered drugs—an ENDA/EAACI Drug Allergy Interest Group position paper. Allergy. 2013;68(6):702–12.
Canto MG, et al. Selective immediate hypersensitivity reactions to NSAIDs. Curr Opin Allergy Clin Immunol. 2009;9(4):293–7.
Caproni M, et al. Expression of cytokines and chemokine receptors in the cutaneous lesions of erythema multiforme and Stevens–Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 2006;155(4):722–8.
Chang CC, et al. Association of HLA-B*15:13 and HLA-B*15:02 with phenytoin-induced severe cutaneous adverse reactions in a Malay population. Pharmacogenom J. 2017;17(2):170–3.
Chantarangsu S, et al. HLA-B*3505 allele is a strong predictor for nevirapine-induced skin adverse drug reactions in HIV-infected Thai patients. Pharmacogenet Genom. 2009;19(2):139–46.
Chavez-Galan L, et al. Cell death mechanisms induced by cytotoxic lymphocytes. Cell Mol Immunol. 2009;6(1):15–25.
Chen YC, et al. Human herpes virus reactivations and dynamic cytokine profiles in patients with cutaneous adverse drug reactions—a prospective comparative study. Allergy. 2015;70(5):568–75.
Chen CB, et al. Risk and association of HLA with oxcarbazepine-induced cutaneous adverse reactions in Asians. Neurology. 2017;88(1):78–86.
Cheung YK, et al. HLA-B alleles associated with severe cutaneous reactions to antiepileptic drugs in Han Chinese. Epilepsia. 2013;54(7):1307–14.
Choi JH, et al. Association of TNF-alpha promoter polymorphisms with aspirin-induced urticaria. J Clin Pharm Ther. 2009;34(2):231–8.
Choi MJ, et al. Clinicopathologic manifestations of 36 korean patients with acute generalized exanthematous pustulosis: a case series and review of the literature. Ann Dermatol. 2010;22(2):163–9.
Choquet-Kastylevsky G, et al. Increased levels of interleukin 5 are associated with the generation of eosinophilia in drug-induced hypersensitivity syndrome. Br J Dermatol. 1998;139(6):1026–32.
Chung WH, Hung SI. Recent advances in the genetics and immunology of Stevens–Johnson syndrome and toxic epidermal necrosis. J Dermatol Sci. 2012;66(3):190–6.
Chung WH, et al. Medical genetics: a marker for Stevens–Johnson syndrome. Nature. 2004;428(6982):486.
Chung WH, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens–Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008;14(12):1343–50.
Chung WH, et al. Genetic variants associated with phenytoin-related severe cutaneous adverse reactions. JAMA. 2014;312(5):525–34.
Chung WH, et al. Insights into the poor prognosis of allopurinol-induced severe cutaneous adverse reactions: the impact of renal insufficiency, high plasma levels of oxypurinol and granulysin. Ann Rheum Dis. 2015a;74(12):2157–64.
Chung WH, et al. Oxypurinol-specific T cells possess preferential TCR clonotypes and express granulysin in allopurinol-induced severe cutaneous adverse reactions. J Investig Dermatol. 2015b;135(9):2237–48.
Ciccacci C, et al. Association between CYP2B6 polymorphisms and nevirapine-induced SJS/TEN: a pharmacogenetics study. Eur J Clin Pharmacol. 2013;69(11):1909–16.
Cornejo-Garcia JA, et al. Genetic variants of the arachidonic acid pathway in non-steroidal anti-inflammatory drug-induced acute urticaria. Clin Exp Allergy. 2012;42(12):1772–81.
Correia O, et al. Increased interleukin 10, tumor necrosis factor alpha, and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol. 2002;47(1):58–62.
Deng A, et al. Granulysin, a cytolytic molecule, is also a chemoattractant and proinflammatory activator. J Immunol. 2005;174(9):5243–8.
Dona I, et al. Hypersensitivity reactions to non-steroidal anti-inflammatory drugs. Curr Pharm Des. 2016;22(45):6784–802.
Ferrell PB Jr, McLeod HL. Carbamazepine, HLA-B*1502 and risk of Stevens–Johnson syndrome and toxic epidermal necrolysis: US FDA recommendations. Pharmacogenomics. 2008;9(10):1543–6.
Finkelman FD, Khodoun MV, Strait R. Human IgE-independent systemic anaphylaxis. J Allergy Clin Immunol. 2016;137(6):1674–80.
Fujiyama T, et al. Increased frequencies of Th17 cells in drug eruptions. J Dermatol Sci. 2014;73(1):85–8.
Gatanaga H, et al. HLA-Cw8 primarily associated with hypersensitivity to nevirapine. AIDS. 2007;21(2):264–5.
Genin E, et al. HLA-A*31:01 and different types of carbamazepine-induced severe cutaneous adverse reactions: an international study and meta-analysis. Pharmacogenom J. 2014;14(3):281–8.
Gueant JL, et al. HLA-DRA variants predict penicillin allergy in genome-wide fine-mapping genotyping. J Allergy Clin Immunol. 2015;135(1):253–9.
Hashizume H, Fujiyama T, Tokura Y. Reciprocal contribution of Th17 and regulatory T cells in severe drug allergy. J Dermatol Sci. 2016;81(2):131–4.
Hetherington S, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet. 2002;359(9312):1121–2.
Hung SI, et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc Natl Acad Sci USA. 2005;102(11):4134–9.
Hung SI, et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet Genom. 2006;16(4):297–306.
Hung SI, et al. Common risk allele in aromatic antiepileptic-drug induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Han Chinese. Pharmacogenomics. 2010;11(3):349–56.
Ikeda H, et al. HLA class I markers in Japanese patients with carbamazepine-induced cutaneous adverse reactions. Epilepsia. 2010;51(2):297–300.
Illing PT, et al. Immune self-reactivity triggered by drug-modified HLA-peptide repertoire. Nature. 2012;486(7404):554–8.
Johansson SG, et al. A revised nomenclature for allergy. An EAACI position statement f–rom the EAACI nomenclature task force. Allergy. 2001;56(9):813–24.
Kabashima R, et al. Increased circulating Th17 frequencies and serum IL-22 levels in patients with acute generalized exanthematous pustulosis. J Eur Acad Dermatol Venereol. 2011;25(4):485–8.
Kaniwa N, et al. HLA-B*1511 is a risk factor for carbamazepine-induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Japanese patients. Epilepsia. 2010;51(12):2461–5.
Kazeem GR, et al. High-resolution HLA genotyping and severe cutaneous adverse reactions in lamotrigine-treated patients. Pharmacogenet Genom. 2009;19(9):661–5.
Kim SH, et al. Genetic mechanism of aspirin-induced urticaria/angioedema. Curr Opin Allergy Clin Immunol. 2006;6(4):266–70.
Kim SH, et al. HLA-B*5901 is strongly associated with methazolamide-induced Stevens–Johnson syndrome/toxic epidermal necrolysis. Pharmacogenomics. 2010;11(6):879–84.
Kim SH, Lee KW, Song WJ, et al. Carbamazepine-induced msevere cutaneous reactions and HLA genotypes in Korea. Epilepsy Res. 2011;97:190–7.
Kim SH, et al. A functional promoter polymorphism of the human IL18 gene is associated with aspirin-induced urticaria. Br J Dermatol. 2011a;165(5):976–84.
Kim SH, et al. Carbamazepine-induced severe cutaneous adverse reactions and HLA genotypes in Koreans. Epilepsy Res. 2011b;97(1–2):190–7.
Kim SK, et al. Upregulated RIP3 expression potentiates MLKL phosphorylation-mediated programmed necrosis in toxic epidermal necrolysis. J Investig Dermatol. 2015;135(8):2021–30.
Kim D, et al. Targeted therapy guided by single-cell transcriptomic analysis in drug-induced hypersensitivity syndrome: a case report. Nat Med. 2020;26(2):236–43.
Kishimoto TK, et al. Contaminated heparin associated with adverse clinical events and activation of the contact system. N Engl J Med. 2008;358(23):2457–67.
Konvinse KC, et al. HLA-A*32:01 is strongly associated with vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Allergy Clin Immunol. 2019;144(1):183–92.
Lanier LL. NK cell recognition. Annu Rev Immunol. 2005;23:225–74.
Laroche D, et al. Anaphylactoid and anaphylactic reactions to iodinated contrast material. Allergy. 1999;54(Suppl 58):13–6.
Littera R, et al. HLA-dependent hypersensitivity to nevirapine in Sardinian HIV patients. AIDS. 2006;20(12):1621–6.
Locharernkul C, et al. Carbamazepine and phenytoin induced Stevens–Johnson syndrome is associated with HLA-B*1502 allele in Thai population. Epilepsia. 2008;49(12):2087–91.
Lonjou C, et al. A European study of HLA-B in Stevens–Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharmacogenet Genom. 2008;18(2):99–107.
Mallal S, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet. 2002;359(9308):727–32.
Mallal S, et al. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med. 2008;358(6):568–79.
Martin AM, et al. Predisposition to nevirapine hypersensitivity associated with HLA-DRB1*0101 and abrogated by low CD4 T-cell counts. AIDS. 2005;19(1):97–9.
McCormack M, et al. HLA-A*3101 and carbamazepine-induced hypersensitivity reactions in Europeans. N Engl J Med. 2011;364(12):1134–43.
Meier-Schiesser B, et al. Culprit drugs induce specific IL-36 overexpression in acute generalized exanthematous pustulosis. J Investig Dermatol. 2019;139(4):848–58.
Mockenhaupt M, et al. HLA-B*57:01 confers genetic susceptibility to carbamazepine-induced SJS/TEN in Europeans. Allergy. 2019;74(11):2227–30.
Montanez MI, et al. Epidemiology, mechanisms, and diagnosis of drug-induced anaphylaxis. Front Immunol. 2017;8:614.
Moon TC, Befus AD, Kulka M. Mast cell mediators: their differential release and the secretory pathways involved. Front Immunol. 2014;5:569.
Morel E, et al. CD94/NKG2C is a killer effector molecule in patients with Stevens–Johnson syndrome and toxic epidermal necrolysis. J Allergy Clin Immunol. 2010;125(3):703–10.
Munoz-Cano R, et al. Mechanisms of anaphylaxis beyond IgE. J Investig Allergol Clin Immunol. 2016;26(2):73–82.
Naisbitt DJ, et al. Hypersensitivity reactions to carbamazepine: characterization of the specificity, phenotype, and cytokine profile of drug-specific T cell clones. Mol Pharmacol. 2003;63(3):732–41.
Nassif A, et al. Drug specific cytotoxic T-cells in the skin lesions of a patient with toxic epidermal necrolysis. J Investig Dermatol. 2002;118(4):728–33.
Nassif A, et al. Evaluation of the potential role of cytokines in toxic epidermal necrolysis. J Investig Dermatol. 2004;123(5):850–5.
Navarini AA, et al. Rare variations in IL36RN in severe adverse drug reactions manifesting as acute generalized exanthematous pustulosis. J Investig Dermatol. 2013;133(7):1904–7.
Ng CY, et al. Impact of the HLA-B(*)58:01 allele and renal impairment on allopurinol-induced cutaneous adverse reactions. J Investig Dermatol. 2016;136(7):1373–81.
Olteanu C, et al. The 10th international congress on cutaneous adverse drug reactions, Shimane, Japan, 2018: focus on new discoveries. Drug Saf. 2019;42(6):797–801.
Ostrov DA, et al. Drug hypersensitivity caused by alteration of the MHC-presented self-peptide repertoire. Proc Natl Acad Sci USA. 2012;109(25):9959–64.
Oussalah A, et al. Genetic variants associated with drugs-induced immediate hypersensitivity reactions: a PRISMA-compliant systematic review. Allergy. 2016;71(4):443–62.
Ozeki T, et al. Genome-wide association study identifies HLA-A*3101 allele as a genetic risk factor for carbamazepine-induced cutaneous adverse drug reactions in Japanese population. Hum Mol Genet. 2011;20(5):1034–41.
Pacor ML, et al. Relationship between human leucocyte antigen class I and class II and chronic idiopathic urticaria associated with aspirin and/or NSAIDs hypersensitivity. Mediat Inflamm. 2006;2006(5):62489.
Padovan E, et al. Penicilloyl peptides are recognized as T cell antigenic determinants in penicillin allergy. Eur J Immunol. 1997;27(6):1303–7.
Pan RY, et al. Identification of drug-specific public TCR driving severe cutaneous adverse reactions. Nat Commun. 2019;10(1):3569.
Paquet P, et al. Macrophages and tumor necrosis factor alpha in toxic epidermal necrolysis. Arch Dermatol. 1994;130(5):605–8.
Paquet P, et al. Immunoregulatory effector cells in drug-induced toxic epidermal necrolysis. Am J Dermatopathol. 2000;22(5):413–7.
Pichler WJ. Pharmacological interaction of drugs with antigen-specific immune receptors: the p–i concept. Curr Opin Allergy Clin Immunol. 2002;2(4):301–5.
Pichler WJ. Delayed drug hypersensitivity reactions. Ann Intern Med. 2003;139(8):683–93.
Pinkoski MJ, et al. Granzyme B-mediated apoptosis proceeds predominantly through a Bcl-2-inhibitable mitochondrial pathway. J Biol Chem. 2001;276(15):12060–7.
Qiao HL, Yang J, Zhang YW. Relationships between specific serum IgE, cytokines and polymorphisms in the IL-4, IL-4Ralpha in patients with penicillins allergy. Allergy. 2005;60(8):1053–9.
Quiralte J, et al. Association of HLA-DR11 with the anaphylactoid reaction caused by nonsteroidal anti-inflammatory drugs. J Allergy Clin Immunol. 1999;103(4):685–9.
Redwood AJ, et al. Single-cell transcriptomics reveal polyclonal memory T-cell responses in skin with positive abacavir patch test results. J Allergy Clin Immunol. 2019;144(5):1413–6.
Rive CM, Bourke J, Phillips EJ. Testing for drug hypersensitivity syndromes. Clin Biochem Rev. 2013;34(1):15–38.
Romano A, et al. Delayed hypersensitivity to aminopenicillins is related to major histocompatibility complex genes. Ann Allergy Asthma Immunol. 1998;80(5):433–7.
Saag M, et al. High sensitivity of human leukocyte antigen-b*5701 as a marker for immunologically confirmed abacavir hypersensitivity in white and black patients. Clin Infect Dis. 2008;46(7):1111–8.
Saito N, et al. An annexin A1-FPR1 interaction contributes to necroptosis of keratinocytes in severe cutaneous adverse drug reactions. Sci Transl Med. 2014;6(245):245ra95.
Schaerli P, et al. Characterization of human T cells that regulate neutrophilic skin inflammation. J Immunol. 2004;173(3):2151–8.
Schnyder B, Pichler WJ. Mechanisms of drug-induced allergy. Mayo Clin Proc. 2009;84(3):268–72.
Shepherd FA, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353(2):123–32.
Shi YW, et al. Hla-B alleles and lamotrigine-induced cutaneous adverse drug reactions in the Han Chinese population. Basic Clin Pharmacol Toxicol. 2011;109(1):42–6.
Somkrua R, et al. Association of HLA-B*5801 allele and allopurinol-induced Stevens–Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. BMC Med Genet. 2011;12:118.
Su SC, et al. Interleukin-15 is associated with severity and mortality in Stevens–Johnson syndrome/toxic epidermal necrolysis. J Investig Dermatol. 2017;137(5):1065–73.
Subramanian H, Gupta K, Ali H. Roles of Mas-related G protein-coupled receptor X2 on mast cell-mediated host defense, pseudoallergic drug reactions, and chronic inflammatory diseases. J Allergy Clin Immunol. 2016;138(3):700–10.
Tangamornsuksan W, Lohitnavy M. Association between HLA-B*5901 and methazolamide-induced Stevens–Johnson syndrome/toxic epidermal necrolysis: a systematic review and meta-analysis. Pharmacogenom J. 2019;19(3):286–94.
Tangamornsuksan W, et al. Relationship between the HLA-B*1502 allele and carbamazepine-induced Stevens–Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatol. 2013;149(9):1025–32.
Tanno LK, et al. The absence of CYP3A5*3 is a protective factor to anticonvulsants hypersensitivity reactions: a case-control study in Brazilian subjects. PLoS One. 2015;10(8):e0136141.
Tapia B, et al. Involvement of CCL27–CCR10 interactions in drug-induced cutaneous reactions. J Allergy Clin Immunol. 2004;114(2):335–40.
Tassaneeyakul W, et al. Associations between HLA class I and cytochrome P450 2C9 genetic polymorphisms and phenytoin-related severe cutaneous adverse reactions in a Thai population. Pharmacogenet Genom. 2016;26(5):225–34.
Teraki Y, Fukuda T. Skin-homing IL-13-producing T cells expand in the circulation of patients with drug rash with eosinophilia and systemic symptoms. Dermatology. 2017;233(2–3):242–9.
Tsai YG, et al. Increased type 2 innate lymphoid cells in patients with drug reaction with eosinophilia and systemic symptoms syndrome. J Investig Dermatol. 2019;139(8):1722–31.
Valeyrie-Allanore L, Sassolas B, Roujeau JC. Drug-induced skin, nail and hair disorders. Drug Saf. 2007;30(11):1011–30.
Viard I, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science. 1998;282(5388):490–3.
Viard-Leveugle I, et al. TNF-alpha and IFN-gamma are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Investig Dermatol. 2013;133(2):489–98.
Watkins S, Pichler WJ. Sulfamethoxazole induces a switch mechanism in T cell receptors containing TCRVβ20-1, altering pHLA recognition. PLoS One. 2013;8(10):e76211.
Wedi B. Definitions and mechanisms of drug hypersensitivity. Expert Rev Clin Pharmacol. 2010;3(4):539–51.
Wei CY, et al. Direct interaction between HLA-B and carbamazepine activates T cells in patients with Stevens–Johnson syndrome. J Allergy Clin Immunol. 2012;129(6):1562–9.
Xiong H, et al. Comprehensive assessment of T cell receptor beta repertoire in Stevens–Johnson syndrome/toxic epidermal necrolysis patients using high-throughput sequencing. Mol Immunol. 2019;106:170–7.
Yang J, Qiao HL, Dong ZM. Polymorphisms of IL-13 and IL-4-IL-13-SNPs in patients with penicillin allergies. Eur J Clin Pharmacol. 2005;61(11):803–9.
Yang J, et al. HLA-DRB genotype and specific IgE responses in patients with allergies to penicillins. Chin Med J. 2006;119(6):458–66.
Yang CW, et al. The interferon-gamma-induced protein 10/CXCR3 axis is associated with human herpesvirus-6 reactivation and the development of sequelae in drug reaction with eosinophilia and systemic symptoms. Br J Dermatol. 2020;183(5):909–19.
Zhang FR, et al. HLA-B*13:01 and the dapsone hypersensitivity syndrome. N Engl J Med. 2013;369(17):1620–8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chang, CJ., Chen, CB., Chung, WH. (2022). Mechanisms of Drug Hypersensitivity. In: Lee, H.Y., Creamer, D. (eds) Drug Eruptions. Updates in Clinical Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-031-09388-3_2
Download citation
DOI: https://doi.org/10.1007/978-3-031-09388-3_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-09387-6
Online ISBN: 978-3-031-09388-3
eBook Packages: MedicineMedicine (R0)