Abstract
Multiple types of voltage-gated calcium (CaV) channels including CaV1.2, CaV1.3, CaV2.1, CaV2.2, CaV2.3, CaV3.1, and CaV3.2 operate in electrically excitable β cells under both physiological and pathophysiological conditions. Physiologically functioning β cell CaV channels mediate spatiotemporally distinct Ca2+ entries to trigger exquisite glucose-stimulated insulin secretion (GSIS) and to sustain β cell maturity, viability, and physiological expansion, thereby maintaining blood glucose homeostasis. In addition, these channels also interconnect with exocytotic proteins, InsP3 receptors, and PKC to form signalosomes for fine-tuning GSIS. Pathologically affected β cell CaV channels, resulting from their phenotypic switch, mutation, altered expression and dysregulation, impair GSIS, and compensatory β cell expansion, induce β cell dedifferentiation, and even drive β cell death due to insufficient or excessive Ca2+ influx. In fact, abnormal upregulation of β cell CaV channels couples diabetogenic serum components, like apolipoprotein CIII and IgGs in sera from patients with amyotrophic lateral sclerosis and type 2 diabetes, to Ca2+-dependent β cell demise. Consequently, these detrimental Ca2+-dependent events lead to insulin deficiency, hyperglycemia, and diabetes. The efficacy of curative treatments for diabetes critically relies on molecular target- and mechanism-based therapies. β Cell CaV channels per se, their regulation mechanisms and signaling pathways most likely serve as druggable targets for medical intervention of Ca2+-dependent β cell dysfunction, abnormal expansion, dedifferentiation, and death in association with diabetes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- β cell
- Calcium channel
- Cell death
- Cell dedifferentiation
- Cell expansion
- Cell maturity
- Cell viability
- Glucose-stimulated insulin secretion
Introduction
Nature has endowed the β cell with multiple types of voltage-gated calcium (CaV) channels including CaV1.2, CaV1.3, CaV2.1, CaV2.2, CaV2.3, CaV3.1, and CaV3.2 (Fig. 1). These CaV channels share some similar features but possess distinct characteristics in their intrinsic properties and functionalities (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). As in other types of electrically excitable cells, β cell CaV channels transit from closed pores to Ca2+-conduits upon membrane depolarization, resulting from ATP-sensitive potassium (KATP) channel closure by ATP produced in glucose metabolism. This glucose-stimulated conformational transition of CaV channels allows extracellular Ca2+ to rapidly enter the cytoplasm of β cells, initially generating electrical signals of the β cell and subsequently raising cytoplasmic-free Ca2+ concentration ([Ca2+]i) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). [Ca2+]i that serves as a versatile and ubiquitous second messenger and controls almost all known molecular and cellular events in the β cell, like glucose metabolism, insulin secretion, β cell endocytosis, differentiation, maturation, survival, growth, protein phosphorylation, gene expression, protein and organelle trafficking (Fig. 1) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Therefore, physiologically orchestrated β cell CaV channels mediate appropriate Ca2+ influx to ensure adequate β cell function, identity, and viability, thereby maintaining satisfactory insulin release and glucose homeostasis in the body (Fig. 1) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Pathological disturbances in β cell CaV channels, resulting from their mutation, altered expression, and dysregulation, impair insulin secretion and even drive β cell destruction due to insufficient or excessive Ca2+ influx (Fig. 1). Consequently, this brings about insulin deficiency, resultant hyperglycemia and diabetes (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Effective treatments for diabetes depend on molecular target- and mechanism-based therapies. β Cell CaV channels and their regulation mechanisms and signaling pathways most likely serve as druggable targets for medical intervention of Ca2+-dependent β cell dedifferentiation and death associated with diabetes. Therefore, β cell CaV channels, their regulation mechanisms and signaling pathways have intrigued numerous researchers and clinicians including us. A series of seminal findings have been gained from basic studies by combining the patch-clamp technique, fluorescence microscopy, biochemical methods, pharmacological approaches, cellular and molecular techniques, and clinical investigations in patients with diabetes (Ovalle et al., 2018; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014).
A scheme illustrating pancreatic β cell CaV channels in health and disease. The β cell is equipped with CaV1.2, CaV1.3, CaV2.1, CaV2.2, CaV2.3, CaV3.1, and CaV3.2 channels. It converts glucose into ATP via cytosolic glycolysis and mitochondrial citric acid cycle bringing about KATP channel closure and plasma membrane depolarization to open CaV channels. In physiological contexts, β cell CaV channels take center stage in GSIS and a part in β cell maturity, viability, and expansion by mediating spatiotemporally distinct Ca2+ entries, which trigger Ca2+-dependent protein-protein interactions and enzymatic responses and are involved in almost all known molecular and cellular events in the β cell. When suffering genetic mutations or undergoing phenotype switch, altered expression, and dysregulation under pathological conditions, β cell CaV channels become inadequate, hyperactivated, accumulated, or dislocated resulting in impaired GSIS, β cell dedifferentiation, poor expansion, and death due to insufficient, excessive, misspaced or ill-timed Ca2+ influx. Consequently, insulin deficiency, hyperglycemia, and diabetes occur. CAC citric acid cycle, CaV voltage-gated calcium, EV endocytotic vesicles, GLUT glucose transporter, IG insulin-containing granule, InsP3R InsP3 receptor, KATP ATP-sensitive, RyR ryanodine receptor, ψ depolarization
This chapter focuses on the physiological and pathological aspects of CaV channels in β cells.
β Cell CaV Channels Under Healthy Circumstances
The role of β cell CaV channels in the regulation of glucose-stimulated insulin secretion (GSIS) and the participation of CaV channels in the control of β cell maturity, viability, and expansion as well as signaling networks of β cell CaV channel subunits have thoroughly been characterized under healthy circumstances (Fig. 1) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014).
CaV Channel Regulation of Glucose-Stimulated Insulin Secretion
β Cell CaV channels serve as the pivot of a molecular network controlling GSIS where they exert insulinotropic action in a complex manner (Fig. 1) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). They not only directly steer insulin-secretory granule trafficking and trigger its exocytosis by mediating Ca2+ influx, but also indirectly regulate these two processes by facilitating the generation of glucose metabolism-derived signals. These allosteric actions are the most important for β cell CaV channel regulation of GSIS (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). In addition, the β cell CaV channel-mediated Ca2+ influx in response to glucose stimulation also acts as an indispensable player in guaranteeing β cell maturity, growth and viability and ultimately adequate β cell mass and function by controlling β cell transcriptome, proteome, signalome, and metabolome (Fig. 1). This is well accounted for by the findings from a series of studies showing that Ca2+ passing through β cell CaV channels takes an eminent part in β cell gene expression, protein phosphorylation, proliferation, differentiation, and metabolism (for details, see section “Involvement of CaV channels in β cell maturity, viability, and expansion”) (Benes et al., 1998; Berridge et al., 1998; Efrat et al., 1991; Jing et al., 2005; Namkung et al., 2001; Popiela & Moore, 1991; Sjoholm, 1995; Yu et al., 2020). Moreover, some of the β cell CaV channel subunits are also endowed with non-channel functionality that regulates GSIS (Berggren et al., 2004; Rajagopal et al., 2014). In fact, CaVβ3 subunits represent a good paradigm for the non-channel functionality of CaV channel subunits. CaVβ3 subunit-deficient β cells release significantly more insulin when subjected to glucose stimulation (Berggren et al., 2004; Rajagopal et al., 2014). This is attributed to the facts that the CaVβ3 subunit physically interacts with InsP3 receptors and serves as a brake for intracellular Ca2+ mobilization from endoplasmic reticulum stores and that this subunit acts as a protein kinase C (PKC) inhibitor, thereby reducing GSIS (see section “CaV channel-centered interaction networks in the β cell”) (Belkacemi et al., 2018; Berggren et al., 2004). Differential regulation of insulin-secretory granule trafficking and exocytosis in GSIS by distinct types of β cell CaV channels are discussed as follows.
In the process of GSIS, many steps such as glucose catabolism, insulin-secretory granule trafficking, docking and priming are involved in [Ca2+]i contributed from β cell CaV channel-mediated Ca2+ entry and importantly the final and key step, i.e., the fusion of insulin-secretory granule with the plasma membrane, is triggered by Ca2+ influx through CaV channels. This brings β cell CaV channels onto center stage in regulation of GSIS (Salinno et al., 2019; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Of particular importance is that distinct types of β cell CaV channels are likely to mediate spatiotemporally dissimilar Ca2+ influxes to differentially regulate insulin-secretory granule trafficking and exocytosis in GSIS (Barg et al., 2002; MacDonald et al., 2005; Rorsman & Braun, 2013; Rorsman & Renstrom, 2003; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). In general, all known types of β cell CaV channels including CaV1.2, CaV1.3, CaV2.1, CaV2.2, CaV2.3, CaV3.1, and CaV3.2 channels are engaged in the regulation of GSIS by mediating Ca2+ influx (Lang, 1999; Yang & Berggren, 2005a).
The current consensus is that the CaV1 channel takes a predominant role over other types of CaV channels in Ca2+ triggered insulin exocytosis, the most distal step of GSIS (Yang & Berggren, 2005a). Studies with CaV channel blockers reveal that Ca2+ influx through the CaV1 channel brings about 60–80% of GSIS from mouse, rat, and human islets whose β cells possess various types of CaV channels (Davalli et al., 1996; Ohta et al., 1993; Schulla et al., 2003). Similarly, CaV1 channel-mediated Ca2+ entry also acts as a major player in triggering insulin exocytosis in insulin-secreting cell lines (Satin, 2000; Sher et al., 2003; Yang & Berggren, 2005a). Extensive investigations elucidated the role of CaV1 channels in dynamic insulin secretion following glucose stimulation (Davalli et al., 1996; Ohta et al., 1993; Schulla et al., 2003; Wollheim & Sharp, 1981). In an early study, the CaV1 channel blocker verapamil was shown to selectively inhibit the second phase of GSIS (Wollheim et al., 1978). However, accumulated experimental results verified that CaV1 channels regulate both phases of insulin secretion, predominantly triggering insulin release during the first phase in the mouse islet (Davalli et al., 1996; Ohta et al., 1993; Schulla et al., 2003). Dynamic perifusion in combination with pharmacological manipulation showed that three CaV1 channel antagonists nifedipine, diltiazem, and verapamil significantly reduce both the first and second phase of GSIS from perifused rat islets (Ohta et al., 1993). The CaV1 channel agonist Bay K8644 prominently elevated GSIS at both phases in human perifused islets (Davalli et al., 1996). Furthermore, islets from CaV1.2 subunit knockout (CaV1.2−/−) mice drastically reduced their first phase insulin secretion when perifused with stimulatory glucose. Capacitance measurements verified that the CaV1.2−/− resulted in a selective impairment in the initial rapid component of insulin exocytosis (Schulla et al., 2003).
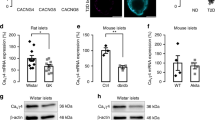
Two subtypes of CaV1 channels, CaV1.2 and CaV1.3 channels, operate in the β cell (Namkung et al., 2001; Schulla et al., 2003; Wiser et al., 1999; Yang et al., 1999). They indeed distinctly contribute to GSIS, but the distinctive contribution has not been thoroughly characterized in different species and still stands as a controversial issue. Rat β cells express a higher level of CaV1.3 subunit mRNA that is 2.5 times greater than that of CaV1.2 subunit mRNA (Iwashima et al., 1993). In CaV1.2−/− mice, β cell CaV currents were reduced by about 45% and their first phase insulin secretion decreased by about 80%, while the remaining CaV channel currents and insulin release were insensitive to CaV1 channel blockers (Schulla et al., 2003). Another study showed that mouse islet β cells displayed negative CaV1.3 subunit immunoreactivity (Barg et al., 2001). Comparison of the data obtained from CaV1.2−/− mice and those acquired from CaV1.2+/+ mice have given the impression that CaV1.2 channels alone mediate Ca2+ influx to couple glucose stimulation to insulin secretion in mouse islet β cells. However, other observations provide evidence that both CaV1.3 subunit mRNA and protein are present in islet β cells from some strains of mice (Namkung et al., 2001; Yang et al., 1999, 2015). CaV1.3−/− β cells compensatorily increase the expression of CaV1.2 subunit proteins (Namkung et al., 2001). Patch-clamp analysis witnessed that although both the total voltage-gated Ba2+ current density and L-type current density did not differ between CaV1.3−/− and CaV1.3+/+ mouse islet β cells, the biophysical properties of L-type Ca2+ currents in CaV1.3−/− mouse islet β cells were markedly altered. Genetic ablation of the CaV1.3 subunit only resulted in a shift of about 10 mV towards more positive potentials at the lower voltage range (Namkung et al., 2001). Mutant islets released less insulin than wild-type islets when bathed in a buffer containing 3 mM glucose, but displayed insulin secretion similar to that of wild-type islets when exposed to 6 mM or higher concentrations of glucose. These observations suggest that compensatory upregulation of CaV1.2 channels occurs in CaV1.3−/− mouse islet β cells to maintain insulin secretion capacity (Namkung et al., 2001). The findings reflect that CaV1.3 subunits appear to mediate Ca2+ entry into wild-type mouse β cells for basal insulin secretion and stimulus-secretion coupling at the lower range of glucose concentrations (Namkung et al., 2001). The distinct contribution of CaV1.2 and CaV1.3 subtypes to insulin exocytosis remains to be further investigated.
Electrophysiological and pharmacological studies substantiate that CaV2.1 channels participate in GSIS from rat islet β cells (Ligon et al., 1998). Partial high voltage-activated Ca2+ currents disappeared in rat islet β cells exposed to the CaV2.1 channel blocker ω-Aga IVA. This pharmacological blockade inhibited the DHP-resistant component of GSIS by about 30% (Ligon et al., 1998). The involvement of CaV2.1 channels in GSIS is also true in rat insulin-secreting RINm5F cells (Sher et al., 2003). Moreover, CaV2.1 channels play a prominent role in the regulation of GSIS from human islet β cells. Human β cells exposed to ω-Aga IVA showed about a 65% reduction in GSIS (Sher et al., 2003). However, the participation of CaV2.1 channels in the regulation of GSIS from mouse islet β cells remains to be examined. The regulation of GSIS by CaV2.2 channels is still controversial. A study observed that the CaV2.2 channel blocker ω-CTX GVIA did not appreciably alter GSIS in human islets (Davalli et al., 1996). On the contrary, another observation showed that this blocker significantly inhibited GSIS in these islets (Sher et al., 2003). In addition, ω-CTX GVIA produced inhibitory effects on second phase GSIS from rat islets but did not affect first phase GSIS and high K+-evoked insulin exocytosis. This inconsistency led to speculation that the ω-CTX GVIA-induced impairment of second phase GSIS occurred due to toxic effects rather than blockade of CaV2.2 channels (Komatsu et al., 1989). However, this speculation was made without considering the possibility that the β cell CaV2.2 channel-mediated Ca2+ influx does not directly trigger insulin exocytosis per se, but rather is engaged in signaling critical for second phase insulin secretion. Indeed, further work on the effect of ω-CTX GVIA on second phase insulin secretion verifies that ω-CTX GVIA significantly decreased the ATP/ADP ratio (Ohta et al., 1993). This suggests that Ca2+ entry through CaV2.2 channels participates in Ca2+-dependent glucose metabolism, thereby promoting later phase production of ATP, which is critical for second phase insulin secretion (Ainscow & Rutter, 2002; Rorsman & Renstrom, 2003). It appears that an increase in glucose concentration can only result in a limited initial increase in cytosolic ATP, which then brings about the sequential events, KATP channel closure, CaV1 channel opening and first phase insulin secretion. In addition, non-CaV1 channel-mediated Ca2+ influx induced by glucose stimulation is likely to promote mitochondrial metabolism resulting in later production of ATP, which activates the signaling pathway specific for second phase insulin secretion in a KATP channel-independent manner (Ainscow & Rutter, 2002; Rorsman & Renstrom, 2003). Of note, Ca2+-dependent regulation of mitochondrial metabolism is complex. As an example, the oxidative phosphorylation inhibitors carbonyl cyanide mchlorophenylhydrazone and sodium azide elevate [Ca2+]i, but reduce mitochondrial membrane potential and ATP production in pancreatic β cells (Rustenbeck et al., 1997). It is worthwhile to point out that CaV2.2 channel-mediated Ca2+ entry is likely to directly trigger insulin exocytosis in insulin-secreting RINm5F and INS-1 cells. Experimental evidence for this comes from an observation that shows that ω-CTX GVIA inhibits both CaV currents and insulin secretion in these insulin-secreting cell lines, the latter being stimulated not only by glucose but also by high K+ (Sher et al., 1992, 2003).
The use of the CaV2.3−/− mouse model and the CaV2.3 channel selective peptide blocker SNX-482 greatly advanced our understanding of the role of CaV2.3 channels in the regulation of GSIS (Jing et al., 2005; Newcomb et al., 1998; Pereverzev et al., 2002a; Yang & Berggren, 2005b). It is clear that Ca2+ entry through CaV2.3 channels regulates insulin secretion from both the pancreatic β cell line INS-1 and primary mouse β cells (Jing et al., 2005; Pereverzev et al., 2002a, b; Vajna et al., 2001; Yang & Berggren, 2005b). An initial study showed that CaV2.3−/− does not influence β cell mass and insulin content. Importantly, however, CaV2.3-deficient mice exhibited impaired insulin secretion, glucose intolerance and hyperglycemia. Unfortunately, this study did not examine dynamic insulin granule exocytosis and phasic insulin secretion from CaV2.3−/− β cells (Pereverzev et al., 2002a). Later, capacitance analysis showed that SNX-482 significantly reduces the late component of depolarization-induced exocytotic events without appreciable influence on the exocytotic response to the first depolarization in mouse pancreatic β cells (Schulla et al., 2003). Akin to the pharmacological manipulation with SNX-482, the genetic ablation of the CaV2.3 subunit gene gives rise to selective suppression of the late component without altering the early component of the depolarization-induced capacitance responses (Jing et al., 2005). This β cell capacitance analysis offers an indication that CaV2.3 channels are likely to selectively control second phase insulin secretion. The indication has been verified by performing a phasic insulin secretion assay. It revealed that either genetic deletion of the CaV2.3 subunit gene or pharmacological block of the CaV2.3 channel with SNX-482 resulted in significant impairment in second phase GSIS without affecting first phase insulin secretion. These findings demonstrate that CaV2.3 channels mediate a specific form of Ca2+ entry whereby they selectively regulate second phase GSIS (Jing et al., 2005; Schulla et al., 2003). Taken together, it is quite plausible to postulate that as distinct from the β cell CaV1 channels, which are physically associated with and functionally coupled to the exocytotic machinery, the CaV2.3 channel appears to be distant from exocytotic sites in the β cell. On the basis of this, the CaV2.3 channel-mediated Ca2+ influx is likely to specifically recruit insulin-containing granules from the reserve pool to the readily releasable pool/immediately releasable pool to govern second phase GSIS (Jing et al., 2005; Yang & Berggren, 2005b). Of particular interest is the finding showing that CaV2.3−/− islets displayed a 20% decrease in integral [Ca2+]i, a 30% decrease in [Ca2+]i oscillation frequency, and a 50% decrease in insulin secretion. This points out that both the amount of [Ca2+]i and the [Ca2+]i oscillation frequency serve to regulate insulin secretion, especially in the second phase. They do so by activating Ca2+-dependent adenylyl cyclase (AC) and phospholipase C resulting in the specific generation of cAMP and diacylglycerol (DAG), important insulinotropic signals, in second phase insulin secretion in pancreatic β cells (Jing et al., 2005; Yang & Berggren, 2005b).
CaV3 channels are likely to be engaged in stimulus-secretion coupling in the β cell. The CaV3 channel blocker NiCl2 reduced insulin secretion from INS-1 cells in a dose-dependent manner (Bhattacharjee et al., 1997). The nonselective CaV1 and CaV3 channel antagonist flunarizine inhibited both glucose- and K+-induced insulin secretion in perifused rat islets (Ohta et al., 1993). CaV3 channels appear to serve as key players in pacemaking in human islet β cells. This is most strikingly seen at membrane potentials around the threshold for action potential firing (−55 mV) and particularly important for insulin secretion induced by glucose at its threshold concentration. Blockade of CaV3 channels with NNC 55-0396 results in a slowdown of action potential firing and reduced insulin secretion in response to stimulation with 6 mM glucose (Braun et al., 2008). The exact role of the CaV3 channel in insulin secretion from human islet β cells remains for further research.
Involvement of CaV Channels in β Cell Maturity, Viability, and Expansion
Guaranteeing the adequate functional β cell mass under different metabolic conditions requires not only a reasonably high number of viable mature β cells, but also the sufficient capacity of β cell expansion including β cell proliferation, neogenesis, and hypertrophy (Bell & Polonsky, 2001; Mathis et al., 2001; Pipeleers et al., 2008; Rhodes, 2005; Wajchenberg, 2007). Naturally, β cells reach their full maturity through intrauterine differentiation and postnatal maturation (Liu & Hebrok, 2017; Salinno et al., 2019). Mature β cells are equipped with β cell-specific transcriptome, proteome, interactome, signalome and metabolome, and are characterized by exquisite glucose sensitivity and adequate insulin secretory capacity (Liu & Hebrok, 2017; Salinno et al., 2019). β Cells not only expand during intrauterine differentiation and postnatal maturation but also after postnatal development in some situations, e.g., pregnancy, where insulin demand increases (Liu & Hebrok, 2017; Salinno et al., 2019). Available evidence indicates that ion channels and in particular CaV channels are involved in β cell maturity, viability, and expansion by altering membrane potentials and mediating Ca2+ influx (Fig. 1). This is because β cell maturity, viability, and expansion rely on a number of Ca2+-dependent cellular and molecular events like protein phosphorylation, transcription, metabolism, cell cycle, proliferation, differentiation, and maturation (Fig. 1) (Berridge et al., 1998; Yang & Berggren, 2005a, 2006; Yang et al., 2014).
Genetic ablation of CaVα1 subunits significantly impairs the postnatal expansion of β cells (Jing et al., 2005; Namkung et al., 2001). The CaV1.3−/− mouse model shows that the CaV1.3 channel is indispensable for postnatal islet β cell expansion. Newborn CaV1.3−/− and CaV1.3+/+ mice possess an equivalent number of islets when normalized to body weight although the former weighs less than the latter. In adulthood, however, differences between adult mutant and wild-type mice become obvious, the number and the size of islets in adult mutant mice drastically decline due to impaired β cell proliferation rather than β cell death (Namkung et al., 2001). Interestingly, CaV2.3 subunit deletion markedly impedes islet cell differentiation and maturation. This is suggested by an immunocytochemical observation showing that the majority of the glucagon-positive cells are also insulin-positive in CaV2.3−/− mouse islets. Such a type of polyhormonal cells has been considered immature fetal β cells (Hrvatin et al., 2014). This immunocytochemical phenotype indicates that the CaV2.3 channel-mediated Ca2+ influx is likely to drive the expression of some genes critical for β cell differentiation and maturation. Furthermore, pharmacological manipulation of CaV channel opening and closure markedly influences β cell proliferation and viability (Popiela & Moore, 1991; Sjoholm, 1995). It has been demonstrated that depolarization and hyperpolarization of β cells with the selective KATP channel blocker glibenclamide and opener diazoxide, which result in subsequent CaV channel opening and closure, induce facilitation of DNA synthesis and an impediment in β cell proliferation, respectively (Sjoholm, 1995). Importantly, the CaV1 channel blockers D-600 and diltiazem can produce a similar effect, i.e., a striking inhibition of β cell proliferation, as glibenclamide (Popiela & Moore, 1991; Sjoholm, 1995).
CaV channel-dependent regulation of β cell maturity, viability, and expansion is based on Ca2+-dependent maintenance of normal transcriptome and proteome in the β cell. The expression of a range of genes in the β cell is associated with Ca2+ influx through CaV channels (Efrat et al., 1991; German et al., 1990; Lee & Laychock, 2000; Macfarlane et al., 2000). For example, the insulin gene, the most specific β cell gene, is regulated by glucose. This glucose-stimulated regulation depends on Ca2+ influx through β cell CaV channels. It is effectively abolished by the CaV channel blockers, such as D-600 and verapamil (Efrat et al., 1991; German et al., 1990). This is also true for the islet amyloid polypeptide amylin. This peptide is co-localized and co-secreted with insulin and regulates glucose metabolism as well as insulin resistance. The β cell elevates amylin gene transcription when exposed to stimulatory glucose. Such glucose-induced transcription can no longer occur in the presence of the CaV1 channel blocker verapamil (Macfarlane et al., 2000). Inositol 1,4,5-trisphosphate (InsP3) receptor gene expression is also under the influence of CaV channel-mediated Ca2+ influx. The CaV1 channel blocker nimodipine effectively ablates the expression of InsP3 receptor type II and III genes induced by protein kinase A (PKA) activation (Lee & Laychock, 2000).
All factors that are able to alter β cell CaV1 channel activity or density may affect β cell maturity, viability, and expansion. Thus far, a limited number of factors have been examined. In fact, β cells fail with regard to maturity, viability, and expansion in a significant proportion of patients with diabetes. Understanding the special involvement of CaV channels in these processes may lead to the development of new preventive measures and curative treatments for diabetes.
CaV Channel-Centered Interaction Networks in the β Cell
Cellular proteins interact with each other in concert to constitute a plethora of cellular signaling networks (Bennett et al., 1992; Bezprozvanny et al., 1995; Ji et al., 2002; Kang et al., 2002; Leveque et al., 1992; Mochida et al., 1996; Rettig et al., 1996; Sheng et al., 1994, 1996, 1997; Wiser et al., 1999; Yang et al., 1999). As a typical example, CaV channel subunits interact with many other proteins to create complex signaling networks in addition to forming Ca2+ conducting pores in the plasma membrane (Belkacemi et al., 2018; Yang & Berggren, 2005a, 2006; Yang et al., 2014). In a CaV channel subunit complex, CaV channels no longer sense and respond only to voltage depolarization, but are also modulated by their interacting partners (for additional information, please see chapter “Modulation of VGCCs by G-protein Coupled Receptors and Their Second Messengers” by Mark and colleagues). They signal not only by altering membrane potentials and conducting Ca2+, but also by physically acting on their interacting partners. Exceptionally, CaV channel subunits can even stay away from the CaV channel subunit complex to function as non-channel proteins and crosstalk with other signaling molecules (Belkacemi et al., 2018; Berggren et al., 2004; Hibino et al., 2003; Yang & Berggren, 2005a, 2006; Yang et al., 1999, 2014). This is well exemplified by the fact that a short splice variant of the CaVβ4 subunit enters the nucleus where it directly acts on the nuclear protein chromobox protein 2 and controls gene silencing (Hibino et al., 2003). Here we discuss some CaV channel-centered interaction networks in the β cell including CaV1 channel-exocytotic proteins, CaVβ3 subunit-InsP3 receptor, and CaVβ subunit-PKC signaling pathways.
CaV1 Channel-Exocytotic Protein Interaction Networks
The first evidence for interactions between CaV channels and exocytotic proteins results from observations of the pull-down of ω-CTX GVIA binding proteins by antibodies against syntaxin or synaptotagmin (Bennett et al., 1992; Leveque et al., 1992). Soon after that, CaV channels were found to physically associate with exocytotic proteins and thereby forming an exocytotic signalosome. This exocytotic signalosome in combination with their upstream and downstream molecules makes up a complex signaling network whereby CaV channels and exocytotic proteins interact with each other to efficiently and precisely orchestrate complex cellular and molecular processes (Bezprozvanny et al., 1995; Mochida et al., 1996; Rettig et al., 1996; Sheng et al., 1994, 1996, 1997). In distinct cell types, specific types of CaV subunits selectively interact with exocytotic proteins likely due to their subcellular localization. In neurons, CaV2.1 or CaV2.2 subunits are not only colocalized, but also physically associated with exocytotic proteins in active zones, but CaV1 subunits are not (Sheng et al., 1998). By contrast, a CaV1 subunit-exocytotic protein signaling network indeed operates in pancreatic β cells (Ji et al., 2002; Kang et al., 2002; Wiser et al., 1999; Yang et al., 1999). Both CaV1.2 and CaV1.3 subunits have similar interaction with the exocytotic machinery as the neuronal CaV2.1 and CaV2.2 subunits (Ji et al., 2002; Kang et al., 2002; Wiser et al., 1999; Yang et al., 1999).
The interaction of CaV1.3 subunits with syntaxin 1A in the pancreatic β cell has been experimentally verified (Yang et al., 1999). This interaction indeed has clear functional significance. Interrupting the formation of a syntaxin 1A/CaV1.3 subunit complex not only induces the rundown of β cell CaV1 channel activity but also impairs insulin exocytosis independently of this rundown. These findings corroborate that the interaction between the β cell CaV1 channel and syntaxin 1A is required for a proper β cell function (Yang et al., 1999). The β cell CaV1.2 subunit also interacts with exocytotic proteins (Wiser et al., 1999). Its II-III loop is physically associated with syntaxin 1A, SNAP-25 and synatotagmin. Among these interaction partners, syntaxin 1A dampens the amplitude of CaV1.2 subunit-mediated currents. This inhibitory effect is partially counteracted by synaptotagmin (Wiser et al., 1999). Disruption of this CaV1.2 subunit-exocytotic protein complex almost completely abolishes depolarization-evoked exocytosis (Kang et al., 2002; Wiser et al., 1999). β Cell CaV1 channels functionally interact with distinct domains within SNAP-25 (Ji et al., 2002). Interestingly, the long N-terminus (SNAP-25(1–197)) and the short C-terminus of this exocytotic protein (SNAP-25(198–206)) produce opposite effects on CaV1 channel activity, namely stimulation and inhibition, respectively. The stimulatory effect of SNAP-25(1–197) is weaker than the inhibitory effect of SNAP-25(198–206) (Ji et al., 2002).
In conclusion, the β cell CaV1 channel physically associates with the exocytotic machinery to constitute CaV1 channel-exocytotic protein interaction networks. Such networks serve to anchor β cell CaV1 channels and exocytotic machinery in close proximity to each other within the site of insulin exocytosis and to fine-tune β cell CaV1 channel function. This allows them to gain the most effective use of Ca2+ influx for insulin exocytosis and avoid adverse effects of unnecessary excessive Ca2+ influx.
CaVβ3 Subunit-InsP3 Receptor Signaling Pathway
Both the plasma membrane CaV channels and intracellular InsP3 receptors serve to create the exquisitely fine-tuned dynamics of [Ca2+]i, namely, the precise spatiotemporal arrangement of [Ca2+]i, by mediating Ca2+ influx from the extracellular space and Ca2+ mobilization from the intracellular store (Catterall, 2000; Taylor et al., 2004). The dynamics of [Ca2+]i act as a ubiquitous second messenger encoding a rich assortment of information to control Ca2+-dependent protein-protein interactions and enzymatic responses in the cell (Berridge et al., 2000, 2003).
Unexpectedly, the CaVβ3 subunit does not behave as a required building block of β cell CaV channels. Instead, it promiscuously crosstalks with the intracellular Ca2+ release machinery to establish a CaVβ3 subunit-intracellular Ca2+ store network (Berggren et al., 2004). This is strongly supported by the following findings: genetic ablation of CaVβ3 subunits (β3−/−) did not alter the activity and gating properties of CaV channels at both the single channel and whole-cell level in the β cell, but prominently enhanced InsP3-induced Ca2+ release and markedly increased the frequency of glucose-induced [Ca2+]i oscillations in islets. Intact CaVβ3−/− islets significantly increased their GSIS, whereas permeabilized CaVβ3−/− islets showed unaltered Ca2+-evoked insulin secretion in comparison to wild-type islets. Restoration of the CaVβ3 subunit effectively counteracted the enhancement of GSIS induced by the deletion of this subunit. Importantly, mutant mice displayed a better glucose tolerance and more efficient glucose homeostasis. Furthermore, ectopic expression of the CaVβ3 subunit in COS-7 cells, where there are no endogenous CaV channels, significantly dampened Ca2+ release from InsP3-sensitive stores. The endogenous CaVβ3 subunit in pancreatic β cells and ectopically expressed CaVβ3 subunit in COS-7 were mainly localized in intracellular compartments resembling ER where InsP3 receptors reside. In addition to the above findings, the large cytoplasmic region of the InsP3 receptor subunit carries numerous recognition sites for a range of small molecules and proteins like InsP3, Ca2+, nucleotides, protein kinases and phosphatases, calmodulin, apoptotic proteins, transient receptor potential channels, and G-protein βγ subunits. (Taylor et al., 2004). Such a molecular organization opens the possibility for InsP3 receptors to interact with CaVβ3 subunits. This prompted us to propose that physical and functional interactions of the CaVβ3 subunit with InsP3 receptors operate in the pancreatic β cell to act as a brake on InsP3 receptor-mediated Ca2+ mobilization from intracellular stores (Berggren et al., 2004).
Recently, the aforementioned proposal, by taking advantage of CaVβ3−/− mouse model and heterologous expression systems, was closely examined and substantiated (Belkacemi et al., 2018). Co-immunoprecipitation and immunoblot assay revealed that antibodies against CaVβ3 subunits or InsP3 receptor subtypes 1–3 effectively co-immunoprecipitated InsP3 receptor subtypes 1–3 or CaVβ3 subunits, but were unable to do so when the SH3-HOOK domain of CaVβ3 subunits was deleted. [Ca2+]i measurements showed that the presence of CaVβ3 subunits resulted in inhibition of Ca2+ mobilization from InsP3-sensitive stores, whereas the absence of CaVβ3 subunits gave rise to sensitization of InsP3-sensitive Ca2+ stores to low InsP3 levels. The inhibitory effect required the CaVβ3 SH3-HOOK domain binding to InsP3 receptors. Furthermore, radioligand binding assays revealed that InsP3 receptors reduced their sensitivity to InsP3 in the presence of CaVβ3 subunits. Overall, these findings demonstrate that the CaVβ3 subunit indeed physically and functionally interacts with InsP3 receptors and acts as a brake on InsP3 receptor-mediated Ca2+ mobilization from intracellular stores (Belkacemi et al., 2018). Releasing the brake by ablating the CaVβ3 subunit is beneficial for glucose homeostasis and skin wound healing, which is relevant for patients with diabetes (Belkacemi et al., 2018; Berggren et al., 2004). However, the physiological significance of the interaction between CaVβ3 subunits and InsP3 receptors remains enigmatic and interesting.
CaVβ Subunit-PKC Signaling Pathway
Interestingly, a promiscuous interaction of CaVβ2 or CaVβ3 subunits with PKCα has been found to limit insulin secretion (Rajagopal et al., 2014). Following injection of CaVβ2 or CaVβ3 siRNAs into the tail vein, mice showed elevated serum insulin levels and improved glucose homeostasis. The same did not hold true for mice subjected to tail vein injection of CaVβ1 or β4 siRNAs. A clear CaVβ2- or CaVβ3-immunoreactive band appeared in cytoplasmic fractions of islets isolated from control mice, but not from mice treated with CaVβ2 or CaVβ3 siRNAs. The treatment indeed effectively silenced CaVβ2 or CaVβ3 subunit expression. Enhanced GSIS occurred in islets and islet cells from mice treated with CaVβ2 or CaVβ3 siRNAs, but not in those from controls (Rajagopal et al., 2014). Furthermore, there was a clear translocation of PKCα, PKCβII, and PKCθ, to the plasma membrane of islet β cells obtained from CaVβ2- or β3 siRNA-treated mice. This reflects released Cavβ2 and β3 subunit inhibition on PKCα, PKCβII, and PKCθ. Moreover, mice treated with PKCα, but not with PKCβII or PKCθ siRNAs displayed a reduction in serum insulin levels and an elevation in blood glucose concentrations. This raises the possibility that PKCβII and PKCθ are not as important as PKCα in the regulation of GSIS. Taken together, these findings demonstrate that CaVβ2 or CaVβ3 subunits interact with PKCα inhibiting GSIS (Rajagopal et al., 2014).
β Cell CaV Channels in Pathology
Massive efforts have been made to understand β cell CaV channels in pathology (Yang & Berggren, 2005a, 2006; Yang et al., 2014). The resulting findings provide strong evidence that β cell CaV channels suffer deterioration in several aspects under unhealthy circumstances and especially in diabetes (Fig. 1). Here we discuss pathological alterations of β cell CaV channel phenotypes, associations of CaV channel gene mutation and polymorphism with abnormal insulin secretion and diabetes, engagement of CaV channels in β cell dedifferentiation and death as well as CaV channel-mediated coupling of diabetogenic serum components to Ca2+-dependent β cell demise.
Pathological Alterations of β Cell CaV Channel Phenotypes
A series of papers verify that the phenotypic switch of β cell CaV channels happens in a diabetic milieu although β cell CaV channelome is genetically inherited. In fact, T-type Ca2+ currents are not detectable in the normal mouse pancreatic β cell (Ashcroft & Rorsman, 1989; Satin, 2000; Schulla et al., 2003; Sher et al., 2003; Yang & Berggren, 2005a). However, such Ca2+ currents appear in NOD mouse pancreatic β cells (Wang et al., 1996). Importantly, the newly appeared T-type Ca2+ currents elevate basal [Ca2+]i and thereby driving the Ca2+-dependent apoptosis of NOD mouse β cells (Wang et al., 1996, 1999). This is undoubtedly involved in the development of type 1 diabetes (T1D) in the NOD mice, an animal model of human T1D characterized by leukocytic infiltration in islets and β cell death (Solomon & Sarvetnick, 2004; Yoshida & Kikutani, 2000). Experimental evidence shows that inflammatory cytokines, produced by the immune cells in the peri-islet and intra-islet infiltrate, induce abnormal expression of CaV3 channels, resultant excessive [Ca2+]i and consequent Ca2+-dependent apoptosis in β cells, but not in a glucagon-secreting α cell line (Wang et al., 1999). The above findings clearly pinpoint cytokines as the main culprit causing the phenotypic switch of β cell CaV channels and Ca2+-dependent β cell death, thereby playing an important role in the development of T1D. However, some deep-seated problems remain to be addressed. For example, what are the mechanistic details whereby cytokines selectively initiate the appearance of β cell CaV3 channels in the T1D situation? Do cytokines turn on de novo expression of β cell CaV3 channel genes or just activate functionally concealed CaV3 channels in β cells?
Association of CaV Channel Gene Mutations and Polymorphisms with Abnormal Insulin Secretion and Diabetes
Type 2 diabetes (T2D) is a complex polygenic trait that is phenotypically characterized by a progressive loss and/or impairment in functional β cell mass (American Diabetes Association, 2014; Mathis et al., 2001; Saltiel, 2001; van Belle et al., 2011). It is rational to deem genes critical for GSIS and/or β cell viability, as exemplified by CaV channel genes, as potential diabetes risk genes (American Diabetes Association, 2014; Ashcroft & Rorsman, 2004; Holmkvist et al., 2007; Mathis et al., 2001; Reinbothe et al., 2013; Saltiel, 2001; van Belle et al., 2011). Efforts have been put into research understanding the association of CaV channel gene mutation and polymorphism with abnormal insulin secretion and diabetes. Some interesting findings on the association of CaV channel gene mutations and polymorphisms with abnormal insulin secretion and diabetes are discussed below.
It has been clearly verified that CaV1.2 missense mutations are the cause of the monogenetic disorder Timothy syndrome. This inherited disease manifests with a wide clinical spectrum that involves the cardiac, endocrine, immune and central nervous systems (Splawski et al., 2004). This complex clinical spectrum stems from a single nucleotide G > A transition at position 1216 or substitution of glycine with arginine at residue 406 (G406R) in the CaV1.2 subunit gene. Such mutant CaV1.2 subunits almost completely lose voltage-dependent inactivation. The loss of voltage-dependent inactivation in CaV1.2 channels should enhance insulin secretion in patients with Timothy syndrome. In fact, 36% of the patients suffered from episodic hypoglycemia, reflecting that excessive insulin secretion occurs due to the exaggerated Ca2+ influx through the mutant CaV1.2 channels in the pancreatic β cell. Moreover, such episodic hypoglycemia caused by inadequate insulin secretion has led to the decease of some affected patients (Splawski et al., 2004).
Investigation of human CaV1.3 subunit gene variation in 918 Japanese type 2 diabetics and 336 control subjects identified an ATG repeat expansion of this gene in type 2 diabetics (Yamada et al., 2001). However, this mutation appears at low frequency and is not closely associated with the development of common T2D. Nevertheless, it may give rise to a subgroup of this polygenic disease (Yamada et al., 2001; Yang & Berggren, 2005a, 2006). Furthermore, the association of the single nucleotide polymorphisms (SNPs) rs312480, rs312486 and rs9841978 in the CaV1.3 subunit gene in humans with impaired insulin secretion and T2D has been characterized in 8987 non-diabetic Finnish and Swedish people and 2830 Finnish and Swedish patients with T2D. The obtained data show that the SNP rs312480 is associated with decreased mRNA expression of the CaV1.3 subunit gene and impaired GSIS and that the SNPs rs312486 and rs9841978 are linked to T2D (Reinbothe et al., 2013). Moreover, the SNP rs673391 in the human CaV2.3 subunit has also been identified by the Botnia Study Group in collaboration with others (Holmkvist et al., 2007). It is closely associated with T2D and impaired insulin secretion and in particular reduced second-phase insulin secretion (Holmkvist et al., 2007).
The association of CaV2.1 subunit gene mutation-caused spinocerebellar ataxia type 6 with T2D has been found in a Japanese family (Takiyama et al., 1998; Yang & Berggren, 2005a, 2006). In this five-generation family, thirteen members are diagnosed with CaV2.1 subunit mutation and suffer from spinocerebellar ataxia type 6. Three out of the five patients examined also have overt T2D. This CaV2.1 subunit mutant carries abnormal CAG repeat expansion encoding a polyglutamine tract (Takiyama et al., 1998; Yang & Berggren, 2005a, 2006). Characterization of biophysical properties and surface expression of this mutant shows contradictory results from two groups (Piedras-Renteria et al., 2001; Toru et al., 2000; Yang & Berggren, 2005a, 2006). One group reveals that the polyglutamine-containing CaV2.1 subunit expressed in HEK 293 cells displayed a negative shift of voltage-dependent inactivation resulting in reduced Ca2+ influx (Toru et al., 2000; Yang & Berggren, 2005a, 2006). In contrast, the other witnesses that the mutant CaV2.1 subunit does not alter its biophysical properties, but instead is expressed more abundantly in the plasma membrane in HEK 293 cells, giving rise to higher CaV channel current density as compared to the wild-type CaV2.1 subunit (Piedras-Renteria et al., 2001; Yang & Berggren, 2005a, 2006). It remains to be seen how the mutant CaV2.1 channel behaves in the β cell to induce T2D concurrent with spinocerebellar ataxia type 6 (Takiyama et al., 1998; Yang & Berggren, 2005a, 2006).
Interestingly, a genomewide linkage analysis has found a novel neonatal diabetes locus mapped to chromosome 10p12.1-p13 in a large consanguineous family with autosomal recessively inherited neonatal diabetes (Sellick et al., 2003; Yang & Berggren, 2005a, 2006). This region contains the CaVβ2 subunit gene, which is predominantly expressed in the β cell (Berggren et al., 2004). All affected individuals in this family phenotypically manifested low or even undetectable levels of circulating insulin indicating inadequate β cell mass and impaired insulin synthesis and secretion (Sellick et al., 2003; Yang & Berggren, 2005a, 2006). These findings indicate that the CaVβ2 subunit gene should be considered as one of the potential susceptibility genes for neonatal diabetes (Sellick et al., 2003; Yang & Berggren, 2005a, 2006).
Engagement of CaV Channels in β Cell Dedifferentiation and Death
Correctly-localized and properly-functioning CaV channels with an appropriate density serve as central players in the creation and orchestration of dynamics, homeostasis, and remodeling of [Ca2+]i in the β cell (Yang & Berggren, 2005a, 2006; Yang et al., 2014). This is critical for β cell maturity, viability, and expansion, as discussed earlier. Conversely, in pathological contexts, β cell CaV channels undergo hypoactivation or hyperactivation, become abnormally scarce or abundant, or are out of position (Fig. 1). These pathological disturbances make β cell CaV channels mediate either deleteriously high or harmfully low Ca2+ influx, resulting in exaggerated and minimized [Ca2+]i, respectively, or have them conduct Ca2+ into wrong subcellular locations. This leads to activating detrimental signaling pathways driving β cell dedifferentiation or immaturity and β cell death (Fig. 1) (Yang & Berggren, 2005a, 2006; Yang et al., 2014).
CaV Channels in β Cell Dedifferentiation
Strong evidence has accumulated to support that abnormal CaV channels can contribute to β cell dedifferentiation (Fig. 1). In islets of GK rats, a non-obese, T2D model, pathological hyperactivation of β cell CaV3 and CaV1 channels appear coincidentally with lower levels of insulin and exocytotic proteins, including vesicle-associated membrane protein-2 (VAMP-2), synaptotagmin III, cysteine string protein (CSP), the mammalian homolog of the unc-18 gene (Munc-18), α-soluble N-ethylmaleimide-sensitive attachment protein (α-SNAP), N-ethylmaleimide-sensitive factor (NSF) and synaptosomal-associated protein of 25 kDa (SNAP-25) (Kato et al., 1996; Rose et al., 2007; Salinno et al., 2019; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014; Zhang et al., 2002). Furthermore, GK rats suffer impairment of GSIS, which has thus far been considered the most important and most specific parameter representing the metabolic and functional maturity of the β cell (Kato et al., 1996; Rose et al., 2007; Salinno et al., 2019; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). It is most likely that pathological Ca2+ influx through hyperactivated β cell CaV3 and CaV1 channels drives β cell dedifferentiation by decreasing expression of exocytotic proteins, resulting in impaired GSIS of GK islets. There is also a possibility that such a GK rat β cell dedifferentiation occurs due to hyperactivated CaV channels being redistributed apart from exocytotic sites to instead serve as a Ca2+-dependent β cell dedifferentiation signal (Yang & Berggren, 2005a, 2006; Yang et al., 2014).
A recent study demonstrates that enhanced expression of β cell CaV3.1 channels drive the dedifferentiation of these cells, as evidenced by impaired GSIS and aberrant glucose homeostasis (Yu et al., 2020). Detailed analysis shows that de novo expression of a recombinant adenovirus encoding enhanced green fluorescent protein-CaV3.1 subunit (Ad-EGFP-CaV3.1) in the β cell increases typical T-type Ca2+ currents and basal [Ca2+]i. Islets transduced with Ad-EGFP-CaV3.1 secrete less insulin under both basal and first phases in response to glucose stimulation and display the inability to normalize hyperglycemia in diabetic rats. Furthermore, Ad-EGFP-CaV3.1-transduced β cells exhibit decreased phosphorylated FoxO1 in their cytoplasm, increased FoxO1 nuclear retention and reduced syntaxin 1A, SNAP-25 and synaptotagmin III. Importantly, these disturbances are reduced by inhibiting CaV3.1 channels or the Ca2+-dependent phosphatase calcineurin. These findings corroborate that enhanced expression of β cell CaV3.1 channels induces β cell dedifferentiation via a signaling pathway consisting of initial excessive Ca2+ influx, subsequent activation of calcineurin, consequent dephosphorylation, and nuclear retention of FoxO1 and eventual FoxO1-mediated downregulation of β cell exocytotic proteins. This Ca2+-dependent β cell dedifferentiation is strong enough to interfere with glucose homeostasis and hence being a pathogenic mechanism in diabetes (Yu et al., 2020).
CaV Channels and β Cell Death
A set of molecules responsible for cell survival can no longer function and another set of molecules being in charge of cell demise becomes activated when [Ca2+]i goes below or over a physiological range or becomes spatiotemporally impaired owing to the pathological conductivity, abnormal density or dislocation of β cell CaV channels. Such pathologically-disturbed [Ca2+]i drives β cells to death (Fig. 1) (Chang et al., 2004; Juntti-Berggren et al., 1993, 2004; Wang et al., 1999).
Pathologically exaggerated [Ca2+]i mediated by hyperactivated β cell CaV channels can drive apoptotic and necrotic β cell death by activating various Ca2+-sensitive enzymes, e.g., calcineurin, endonucleases, transglutaminase, and calpains (Chang et al., 2004; Efanova et al., 1998; Huo et al., 2003; Juntti-Berggren et al., 1993, 2004; Wang et al., 1999; Zaitsev et al., 2001). The serine- and threonine-specific protein phosphatase (PP) calcineurin is conserved in all eukaryotes and undergo activation in a Ca2+- and calmodulin-dependent manner. It acts as a key player in cell death signaling. Activated calcineurin catalyzes dephosphorylation of the Bcl-2 family member Bad to play its pro-apoptotic role (Orrenius et al., 2003). It has been shown that calcineurin orchestrates β cell CaV1 channel-mediated Ca2+ influx and the cytokine signal transduction cascade in the process of β cell death. Treatment with interleukin 1β induces pancreatic β cell apoptosis. This apoptotic event is largely counteracted by either the CaV1 channel inhibitor D-600 or the calcineurin inhibitor deltamethrin (Zaitsev et al., 2001). Furthermore, hyperactivated CaV channels can activate calpain by overloading insulin-secreting MIN6N8 cells with Ca2+ and subsequently calpain initiates activation of calcineurin. Upon activation, calcineurin directly dephosphorylates Bad bringing about apoptosis of the insulin-secreting cells (Chang et al., 2004).
Ca2+-dependent endonucleases induce programmed cell death i.e., apoptosis by catalyzing the cleavage of chromosomal DNA into oligonucleosomal size fragments, a biochemical hallmark of apoptosis (Orrenius et al., 2003). This happens in pancreatic β cells where these DNA cutting enzymes become activated to evoke Ca2+-dependent β cell apoptosis as pathologically excessive Ca2+ ions enter β cells subsequent to CaV channel activation (Efanova et al., 1998; Yang & Berggren, 2006). This is well exemplified by the fact that high glucose exposure induces typical Ca2+-dependent apoptosis which is mimicked by the KATP channel blocker tolbutamide, abolished by either the KATP channel opener diazoxide or the CaV1 channel blocker D-600, and prevented by the endonuclease inhibitor aurintricarboxylic acid (Efanova et al., 1998; Yang & Berggren, 2006).
Transglutaminases are widely distributed in various organs, tissues, and body fluids to catalyze Ca2+-dependent post-translational modification of proteins. Transglutaminase 2, also known as tissue transglutaminase, is ubiquitously expressed in mammalian cells including β cells where it extensively cross-links various cytoskeletal proteins and nucleosomal histones as the distal steps of apoptosis (Ballestar et al., 1996; Esposito & Caputo, 2005; Yang & Berggren, 2006). Transglutaminase 2 is activated by Ca2+ and inhibited by GTP. The activated enzyme extensively cross-links various cytoskeletal proteins, such as microtubule protein tau, β-tubulin, actin, myosin, spectrin, thymosin β, troponin T, and vimentin. This Ca2+-dependent cross-linking of cytoskeletal proteins brings the apoptotic process into its final steps (Esposito & Caputo, 2005). The activated transglutaminase 2 also regulates post-translational modification of nuclear proteins, like core histones. The resultant histone cross-linking is speculated to mediate the chromatin condensation in apoptosis (Ballestar et al., 1996). Importantly, activated transglutaminase 2 also induces apoptotic cell death in a Ca2+-dependent fashion (Orrenius et al., 2003). Experimental data show that insulin-secreting HIT-T15 cells subjected to depletion of GTP with mycophenolic acid display increased transglutaminase 2 activity and in turn undergo apoptosis. Of particular interest is that β cell apoptosis induced by activated transglutaminase 2 is effectively counteracted by reducing extracellular Ca2+ concentrations (Huo et al., 2003). Most likely transglutaminase 2 acts as a potential decoder of excessive Ca2+ entry through hyperactivated CaV channels in β cell apoptosis.
Calpains are Ca2+-activated neutral cysteine proteases. Among them, the two best characterized isoforms are μ- and m-calpain, which are so named because they are activated in vitro by concentrations of Ca2+ in μM and mM ranges, respectively. The activated μ- and m-calpains proteolyze a number of cytoskeletal, membrane-associated, and regulatory proteins involved in a range of cellular processes including necrosis and apoptosis (Goll et al., 2003; Liu et al., 2004). An interesting study shows that apoptotic signaling cascade proceeds in a sequence of cytokine, PKC, CaV channels, calpain, calcineurin, Bad, cytochrome c, and caspases in insulin-secreting MIN6N8 cells (Chang et al., 2004). Co-treatment with interferon-γ and TNF-α significantly enhances high CaV channel activity, prominently increases [Ca2+]i and consequently induces apoptotic death of these insulin-secreting cells. The effects are effectively abolished by the PKC inhibitor chelerythrine. It is likely that PKC phosphorylation results in the enhanced activity of high CaV channels through which excessive Ca2+ influx occurs triggering Ca2+-dependent apoptosis. In fact, the excessive Ca2+ influx first activates the Ca2+-activated protease calpain. Then, the activated calpain induces activation of calcineurin, which catalyzes the dephosphorylation of Bad at S112. Subsequently, Bad dephosphorylation leads to the release of cytochrome c from the mitochondria to the cytoplasm. Eventually, caspases 9, 3, and 7 are cleaved and activated resulting in apoptosis (Chang et al., 2004).
In general, there are two ways for CaV channels to be engaged in β cell apoptosis (Fig. 1). On one hand, CaV channels undergo upregulation of their conductivity and/or density in the β cell. The upregulated CaV channels mediate excessive Ca2+ influx into the β cell resulting in abnormally exaggerated [Ca2+]i which in turn initiates apoptotic cascades in the β cell. This is exemplified by the case of calpain-mediated β cell apoptosis triggered by hyperactivated CaV channel-mediated Ca2+ entry (Fig. 1) (Chang et al., 2004). On the other hand, physiological Ca2+ influx through β cell CaV channels can serve as a permissive condition for initiation of apoptosis under some conditions. This is well illustrated by the fact that interleukin 1β cannot induce β cell apoptosis without Ca2+ influx through CaV1 channels that are not directly affected by this cytokine (Zaitsev et al., 2001).
The loss of β cells occurs in both T1D and T2D. The former is characterized by the absolute loss of pancreatic β cells, whereas the latter is defined by not only the progressive loss of β cell function but also increased β cell apoptosis (Mathis et al., 2001). As illustrated above, hyperactivation of β cell CaV channels plays an important role in β cell apoptosis (Fig. 1) (Chang et al., 2004; Juntti-Berggren et al., 1993, 2004; Wang et al., 1999). These findings pinpoint β cell CaV channels as potential therapeutic targets for the prevention of β cell loss during the development of diabetes. In fact, it has been demonstrated that systemic application of the CaV1 channel blocker verapmil ameliorates and even prevents low-dose streptozotocin-induced progressive diabetes in mice through reduction of β cell apoptosis and promotion of β cell survival and function (Xu et al., 2012).
CaV Channel-Mediated Coupling of Diabetogenic Serum Components to Ca2+-Dependent β Cell Demise
T1D sera contain diabetogenic components that hyperactivate β cell CaV1 channels to provoke Ca2+-dependent β cell death (Fig. 1) (Juntti-Berggren et al., 1993, 2004; Shi et al., 2014). In fact, diabetogenic components are also present in sera from patients with neurodegenerative disorders like amyotrophic lateral sclerosis (ALS) (Shi et al., 2019).
Originally, T1D serum has been verified to hyperactivate β cell CaV1 channels driving pathological Ca2+ influx into β cells and consequent Ca2+-dependent β cell apoptosis (Juntti-Berggren et al., 1993). In cell-attached single-channel recordings, unitary CaV1 currents display more frequent openings in β cells exposed to T1D serum. Consistent with single CaV1 channel analysis, whole-cell patch-clamp recordings reveal that CaV1 currents are massively increased in T1D serum-treated β cells. As a direct consequence of the hyperactivation of β cell CaV1 channels, excessive Ca2+ ions enter β cells resulting in pathologically exaggerated [Ca2+]i in these cells. The Ca2+ overload eventually causes β cell apoptosis as verified by the appearance of typical apoptotic DNA “ladder”. Interestingly, the T1D serum-induced β cell apoptosis disappears upon pharmacological ablation of CaV1 channels. This demonstrates that hyperactivated CaV1 channels serve to convey apoptotic cues from T1D serum to the intrinsic apoptotic machinery in β cells (Juntti-Berggren et al., 1993).
More recently, the subtypes of CaV1 channels hyperactivated by T1D serum and the biophysical mechanisms responsible for T1D serum-induced hyperactivation of β cell CaV1 channels have been clarified by using CaV1.2 and CaV1.3 knockout mice in combination with patch-clamp recordings and single-cell RT-PCR analysis (Yang et al., 2015). Interestingly, a subgroup of islet β cells from CaV1.2 knockout mice express functional CaV1.3 channels. Importantly, T1D sera increase whole-cell CaV currents in islet β cells from CaV1.2- or CaV1.3-deficient mice. They boost the open probability and number of functional unitary CaV1 channels in CaV1.2- and CaV1.3-deficient β cells. It is clear that T1D sera hyperactivate both CaV1.2 and CaV1.3 channels by increasing their conductivity and number (Yang et al., 2015). These findings pinpoint CaV1.2 and CaV1.3 channels as potential targets for anti-diabetes therapy.
To nail down the actual factor(s), i.e. molecular component(s), responsible for T1D serum-induced hyperactivation of β cell CaV1 channels, high-performance liquid chromatography of T1D sera has been carried out. The obtained data show that T1D sera contain significantly higher levels of apolipoprotein CIII (ApoCIII). Interestingly, patch-clamp recordings show that this apolipoprotein is capable of mimicking T1D serum to hyperactivate β cell CaV channels. Like T1D sera, ApoCIII markedly increases whole-cell CaV channel currents and [Ca2+]i in the β cell and prominently provokes β cell apoptosis. Neutralization of ApoCIII with anti-ApoCIII antibodies effectively abolishes both T1D serum- and ApoCIII-induced elevation in [Ca2+]i and apoptosis (Juntti-Berggren et al., 2004). The findings provide promising evidence that ApoCIII is likely to act as the actual factor in T1D sera to hyperactivate β cell CaV channels.
Unfortunately, the above findings cannot reveal which CaV channel type(s) are targeted by ApoCIII and whether CaV channel conductivity, density, or both are influenced by ApoCIII treatment? These two issues have been addressed by combining patch-clamp techniques and pharmacological manipulation (Shi et al., 2014). Cell-attached single-channel recordings reveal that ApoCIII increases both the open probability and density of unitary CaV1 currents. Whole-cell patch-clamp analysis visualizes that ApoCIII enhances whole-cell Ca2+ currents and the enhancement can no longer occur in the presence of the CaV1 channel blocker nimodipine. The findings corroborate that ApoCIII selectively targets β cell CaV1 channels and increases their conductivity and density (Shi et al., 2014).
The key issue of what the signaling mechanisms are whereby ApoCIII hyperactivates β cell CaV channels has drawn great attention. The findings obtained in other cell types suggest that plasma membrane-standing scavenger receptor class B type I (SR-BI) can directly sense extracellular ApoCIII and subsequently signals downstream to the SR-BI interaction partner β1 integrin that activates PKA, PKC, and Src kinase to phosphorylate their substrates like CaV1 channels. Indeed, SR-BI physically associates with ApoCIII in a CHO heterologous expression system and also interacts with β1 integrin in microglial cells (Bamberger et al., 2003; Xu et al., 1997). ApoCIII activates PKC through indirect interaction with β1 integrin in monocytic cells (Kawakami et al., 2006). Furthermore, β1 integrin activation leads to increased CaV1 channel activity in neurons, ventricular myocytes, and vascular smooth muscle cells through stimulation of PKA, PKC, and Src kinase (Gui et al., 2006; Rueckschloss & Isenberg, 2004; Waitkus-Edwards et al., 2002; Wu et al., 2001). In fact, all these components are expressed in β cells (Bosco et al., 2000; Kantengwa et al., 1997; Mukai et al., 2011; Nikolova et al., 2006; Yang & Berggren, 2006). Hyperactivation of CaV1 channels by ApoCIII is hardly influenced by individual inhibition of PKA, PKC, or Src, but significantly abolished by a cocktail of PKA, PKC, and Src or by coinhibition of PKA and Src. Moreover, knockdown of β1 integrin or SR-BI effectively prevents ApoCIII from hyperactivating β cell CaV channels. These findings demonstrate that ApoCIII hyperactivates β cell CaV1 channels through SR-BI/β1 integrin-dependent coactivation of PKA and Src (Shi et al., 2014).
Moreover, additional factors in T1D sera may signal upstream of β cell CaV channels to drive β cell apoptosis as suggested by a study performed in neuroblastoma cells (Pittenger et al., 1997). This study shows that Fas-specific antibodies in T1D sera induce neuroblastoma cell apoptosis similar to T1D-induced β cell apoptosis. This indicates that Fas-specific antibodies in T1D sera may act as another candidate factor involved in the hyperactivation of β cell CaV channels and Ca2+-dependent β cell death (Pittenger et al., 1997). As a matter of fact, N1E-115 murine neuroblastoma cells show a gradual increase in [Ca2+]i followed by Fas-mediated apoptosis characterized by the appearance of condensed chromatin, shrunken cytoplasm, and DNA fragmentation when exposed to T1D sera (Pittenger et al., 1997). Given that β cell apoptosis happens following activation of the Fas signaling pathway or exposure to T1D sera, it is intriguing to clarify if Fas-specific antibodies in T1D sera drive β cell apoptosis through hyperactivation of β cell CaV1 channels (Maedler et al., 2001).
Possible involvement of inhibitory G proteins in T1D serum-induced hyperactivation of β cell CaV channels is suggested by studies with serum from the TID animal model, Bio Bred/Worchester diabetic (BBW) rat. BBW rat serum-induced hyperactivation of neuronal CaV channels is very similar to human T1D-induced hyperactivation of β cell CaV channels. Nondiabetic rat dorsal root ganglion neurons display a drastic increase in CaV channel activity following treatment with the BBW rat serum. This occurs most likely due to impaired regulation of the inhibitory G protein-CaV channel complex (Ristic et al., 1998). Interestingly, both high voltage-activated and low voltage-activated Ca2+ channels in dorsal root ganglion neurons from the BBW rats undergo an enhancement due to a decrease in opiate-mediated inhibition of PTX-sensitive, G protein-coupled CaV channels (Hall et al., 1995, 1996, 2001). The β cell also accommodates inhibitory G proteins that down-regulate β cell CaV channel activity (Ammala et al., 1992; Robertson et al., 1991). There is a high likelihood that human T1D serum-induced hyperactivation of β cell CaV channels involves inhibitory G proteins.
T1D serum has been found to promote the expression of CaV3 channels in a particular type of neurons with triangular soma in cerebellar granule cell cultures (Chandra et al., 2001). This is interesting because T1D serum does not affect the CaV3 channel in RINm5F cells, an insulin-secreting cell line (Juntti-Berggren et al., 1993; Shi et al., 2014). Maybe this is due to differences in signaling pathways upstream of CaV3 channels between nonproliferating primary cells like cerebellar granule neurons and islet β cells and the highly proliferative RINm5F cell line. As a matter of fact, current available data on islet β cells cannot fully rule out the possibility that TID sera also attack β cell CaV3 channels to provoke Ca2+-dependent β cell death.
Indeed, a T-lymphocyte-mediated autoimmune attack is crucial for β cell death in T1D (Mathis et al., 2001). In addition, the above-discussed findings add another layer of complexity to the mechanism of β cell death in T1D and suggest that factors such as ApoCIII and Fas-specific antibodies in T1D sera can attack β cell-cell CaV channels and initiate cell death (Juntti-Berggren et al., 2004; Pittenger et al., 1997; Shi et al., 2014). The complete repertoire of diabetogenic factors in T1D sera and their involvement in β cell CaV channels are of therapeutic interest and need further investigation.
In addition to T1D sera, sera from patients with amyotrophic lateral sclerosis (ALS) and T2D (ALS-T2D) also express diabetogenic factors (Shi et al., 2019). About 60% ALS-T2D patients have positive sera that exaggerate [Ca2+]i responses induced by K+ depolarization in mouse islet cells. The component responsible for the effect has been identified as pathogenic immunoglobulin Gs (IgGs). These pathogenic IgGs not only immunocapture CaVα2δ1 subunits in the β cell plasma membrane, but also hyperactivate β cell CaV1 channels. The hyperactivated CaV1 channels conduct excessive Ca2+ entry leading to pathologically exaggerated increases in [Ca2+]i that activate multiple Ca2+-dependent events detrimental to β cell function and viability. These detrimental events include impaired mitochondrial function, disturbed [Ca2+]i dynamics, reduced GSIS, and nonviable β cells. The findings verify that cytotoxic ALS-T2D-IgG autoantibodies appear in sera from ALS-T2D patients, behaving as a causal link between two closely-associated disorders ALS and T2D by immunoattacking CaVα2δ1 subunits. Interestingly, this study suggests that in a fraction of patients T2D is likely to result from immune destruction of β cells by cytotoxic ALS-T2D-IgG autoantibodies reflecting altered humoral immunity. This may suggest a new pharmacological treatment strategy for patients suffering from a combination of ALS and T2D.
Conclusions
Over decades, persistent attempts and continuous efforts to understand pancreatic β cell CaV channels in health and disease have led to significant progress (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Electrically excitable β cells accommodate at least seven CaVα1 subunits including CaV1.2, CaV1.3, CaV2.1, CaV2.2, CaV2.3, CaV3.1, and CaV3.2. These pore-forming subunits and certain CaV auxiliary subunits are noncovalently assembled into different types of CaV channels that conduct L-, P/Q-, N-, R-, and T-type CaV currents, respectively (Braun et al., 2008; Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). As reflected by the name of these channels, they undergo conformational transitions from an impermeable state to a highly permeable pore upon membrane depolarization initiated by the glucose-induced closure of KATP channels, mediating rapid Ca2+ entry into β cells (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Such a Ca2+ entry not only generates electrical signals in the β cell plasma membrane but also the versatile intracellular messenger [Ca2+]i (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). This makes CaV channels different from other ion channels in promoting Ca2+-dependent molecular and cellular events besides producing electrical signals (Catterall, 2000).
In physiological contexts, β cell CaV channels take center stage in GSIS and are engaged in the control of β cell maturity, viability, and expansion, thereby acting as a multifaceted player in β cell signaling (Fig. 1) (Yang & Berggren, 2005a, b, 2006; Yang et al., 2014). Impressively, β cell CaV channels interplay with other non-channel proteins to create complex signaling networks in addition to promoting Ca2+ influx over the plasma membrane (Belkacemi et al., 2018; Berggren et al., 2004; Ji et al., 2002; Rajagopal et al., 2014; Wiser et al., 1999; Yang & Berggren, 2005a, 2006; Yang et al., 1999, 2014). This renders β cell CaV channels versatile, efficient, and even specific in β cell signaling. β Cell CaV1 subunits and exocytotic proteins specifically interact at the site of exocytosis to drive insulin release, thus preventing detrimental actions of unnecessary excessive Ca2+ influx (Ji et al., 2002; Wiser et al., 1999; Yang & Berggren, 2005a, 2006; Yang et al., 1999). Of interest is that promiscuous CaVβ subunits are networking with InsP3 receptors and PKC to limit GSIS (Belkacemi et al., 2018; Berggren et al., 2004; Rajagopal et al., 2014; Yang & Berggren, 2005a, 2006; Yang et al., 2014). It seems difficult to reconcile the evolutionary conservation of CaVβ subunits and their negative action on GSIS, but it becomes understandable why these signaling networks are conserved in β cells if adding pathological roles of insulin hypersecretion into the context. They likely function as protective mechanisms against insulin hypersecretion and its obesogenic and even carcinogenic effects (Erion & Corkey, 2017; Gallagher & LeRoith, 2020). Surprisingly, CaVβ3 subunits do not appear as a required building block for β cell CaV channels, but instead an interaction partner of InsP3 receptors to serve as a brake on Ca2+ mobilization from InsP3-sensitive stores (Belkacemi et al., 2018; Berggren et al., 2004; Yang & Berggren, 2005a, 2006; Yang et al., 1999, 2014).
β Cell CaV channels suffering from inherited defects or acquired impairments conduct pathological Ca2+ influx, being insufficient, excessive, or spatiotemporally disorganized, causing β cell dysfunction, dedifferentiation, destruction, aberrant expansion, and eventual diabetes (Fig. 1) (Yang & Berggren, 2005a, 2006; Yang et al., 2014). They undergo either hyperactivation or hypoactivation under diabetic conditions (Yang & Berggren, 2005a, 2006; Yang et al., 2014). Excessively-expressed CaVβ3 subunits drive diabetic phenotypes in obese mice, whereas CaVβ3 gene silencing reverses these phenotypes (Lee et al., 2018). CaV3 channels show no functional operation in healthy mouse β cells, but become active in NOD mouse β cells (Yang & Berggren, 2005a, 2006; Yang et al., 2014). CaV channel gene mutation and polymorphism are closely associated with abnormal insulin secretion and diabetes (Holmkvist et al., 2007; Splawski et al., 2004). For example, the CaV1.2G406R mutant in patients with Timothy syndrome displays little voltage-dependent inactivation and mediates exaggerated Ca2+ influx that enhances insulin secretion resulting in lethal hypoglycemia (Splawski et al., 2004). The close association of the SNPs rs312480, rs312486, and rs9841978 in the CaV1.3 subunit gene with impaired insulin secretion and T2D is verified in Finnish and Swedish patients (Holmkvist et al., 2007). Interestingly, CaV3.1 channels overexpressed in β cells activate detrimental signaling pathways driving β cell dedifferentiation or maturity loss through FoxO1-mediated downregulation of β cell exocytotic proteins (Yu et al., 2020). In worst-case scenarios, β cell CaV channels mediate exaggerated Ca2+ entry resulting in excessive [Ca2+]i and consequent Ca2+-dependent β cell death by activating various Ca2+-sensitive enzymes, e.g., calcineurin, endonucleases, transglutaminase and calpains (Chang et al., 2004; Efanova et al., 1998; Huo et al., 2003; Juntti-Berggren et al., 1993, 2004; Wang et al., 1999; Zaitsev et al., 2001). In general, β cell CaV channels serve to couple diabetogenic factors, such as ApoCIII, CaVα1δ2-specific, and Fas-specific antibodies in sera from patients with T1D or ALS-T1D to Ca2+-dependent β cell demise (Juntti-Berggren et al., 1993, 2004; Shi et al., 2014, 2019; Yang et al., 2014, 2015; Yang & Berggren, 2005a, 2006). More specifically, CaV1 channels increase their density and activity in the β cell plasma membrane in response to ApoCIII through SR-BI/β1 integrin-dependent coactivation of PKA and Src kinase (Shi et al., 2014). Cytotoxic IgG autoantibodies in sera from ALS-T2D patients immunocapture CaVα2δ1 subunits and hyperactivate β cell CaV channels leading to impairments in [Ca2+]i dynamics, mitochondrial function, insulin secretion, and survival of β cells, thereby serving as a causal link between ALS and T2D (Shi et al., 2019).
The current knowledge on β cell CaV channels have been gained mostly from studies with rodent β cells, but seldom from those with human ones (Yang & Berggren, 2005a, 2006; Yang et al., 2014). Caution should be exercised in generalizing such knowledge to human β cells. Human β cell CaV channelome, physiology, pathology, regulation mechanisms, and therapeutic potentials should be subjected to further high-priority research. The findings from studies with rodent β cells support that β cell CaV1 and CaV3 channels and their associated interplayers ApoCIII, InsP3 receptors, PKC and calcineurin most likely serve as druggable targets for clinical intervention of Ca2+-dependent β cell dedifferentiation and death associated with diabetes (Belkacemi et al., 2018; Berggren et al., 2004; Juntti-Berggren et al., 2004; Rajagopal et al., 2014; Shi et al., 2014, 2019; Yang & Berggren, 2005a, 2006; Yang et al., 2014; Yu et al., 2020). Of particular interest are clinical trials of CaV3 channel blockers for diabetes treatment. Thus far, the visualization of the ultra-high resolution structure of CaV channels has indeed been turned into reality with the development of advanced technologies, like x-ray crystallography, cryo-electron microscopy, stimulated emission depletion microscopy, and single-molecule microscopy. However, vivid super-ultra high-resolution imaging of instantaneous switch in CaV channel conformation and dynamic redistribution of CaV channels in the plasma membrane is still infeasible. This has created a wide range of physiological enigmas and medical dilemmas and prevented in-depth understanding of β cell CaV channels in health and disease. To resolve these issues, one has to develop and apply super-ultra high spatiotemporal resolution technologies.
Abbreviations
- [Ca2+]i:
-
cytoplasmic-free Ca2+ concentration
- ALS:
-
amyotrophic lateral sclerosis
- ApoCIII:
-
apolipoprotein CIII
- BBW:
-
Bio Bred/Worchester diabetic
- CaV:
-
voltage-gated calcium
- GSIS:
-
glucose-stimulated insulin secretion
- PKA:
-
protein kinase A
- PKC:
-
protein kinase C
- SR-BI:
-
scavenger receptor class B type I
- T1D:
-
type 1 diabetes
- T2D:
-
type 2 diabetes
References
Ainscow, E. K., & Rutter, G. A. (2002). Glucose-stimulated oscillations in free cytosolic ATP concentration imaged in single islet β-cells: Evidence for a Ca2+-dependent mechanism. Diabetes, 51, S162–S170.
American Diabetes Association. (2014). Diagnosis and classification of diabetes mellitus. Diabetes Care, 37, S81–S90.
Ammala, C., Berggren, P. O., Bokvist, K., & Rorsman, P. (1992). Inhibition of L-type calcium channels by internal GTPγS in mouse pancreatic β cells. Pflügers Archiv, 420, 72–77.
Ashcroft, F. M., & Rorsman, P. (1989). Electrophysiology of the pancreatic β-cell. Progress in Biophysics and Molecular Biology, 54, 87–143.
Ashcroft, F., & Rorsman, P. (2004). Type 2 diabetes mellitus: Not quite exciting enough? Human Molecular Genetics, 13, R21–R31.
Ballestar, E., Abad, C., & Franco, L. (1996). Core histones are glutaminyl substrates for tissue transglutaminase. The Journal of Biological Chemistry, 271, 18817–18824.
Bamberger, M. E., Harris, M. E., McDonald, D. R., Husemann, J., & Landreth, G. E. (2003). A cell surface receptor complex for fibrillar beta-amyloid mediates microglial activation. The Journal of Neuroscience, 23, 2665–2674.
Barg, S., Ma, X., Eliasson, L., Galvanovskis, J., Gopel, S. O., Obermuller, S., Platzer, J., Renstrom, E., Trus, M., Atlas, D., et al. (2001). Fast exocytosis with few Ca2+ channels in insulin-secreting mouse pancreatic β cells. Biophysical Journal, 81, 3308–3323.
Barg, S., Eliasson, L., Renstrom, E., & Rorsman, P. (2002). A subset of 50 secretory granules in close contact with L-type Ca2+ channels accounts for first-phase insulin secretion in mouse β-cells. Diabetes, 51, S74–S82.
Belkacemi, A., Hui, X., Wardas, B., Laschke, M. W., Wissenbach, U., Menger, M. D., Lipp, P., Beck, A., & Flockerzi, V. (2018). IP3 receptor-dependent cytoplasmic Ca2+ signals are tightly controlled by CaVbeta3. Cell Reports, 22, 1339–1349.
Bell, G. I., & Polonsky, K. S. (2001). Diabetes mellitus and genetically programmed defects in β-cell function. Nature, 414, 788–791.
Benes, C., Roisin, M. P., Van Tan, H., Creuzet, C., Miyazaki, J., & Fagard, R. (1998). Rapid activation and nuclear translocation of mitogen-activated protein kinases in response to physiological concentration of glucose in the MIN6 pancreatic β cell line. The Journal of Biological Chemistry, 273, 15507–15513.
Bennett, M. K., Calakos, N., & Scheller, R. H. (1992). Syntaxin: A synaptic protein implicated in docking of synaptic vesicles at presynaptic active zones. Science, 257, 255–259.
Berggren, P. O., Yang, S. N., Murakami, M., Efanov, A. M., Uhles, S., Kohler, M., Moede, T., Fernstrom, A., Appelskog, I. B., Aspinwall, C. A., et al. (2004). Removal of Ca2+ channel β3 subunit enhances Ca2+ oscillation frequency and insulin exocytosis. Cell, 119, 273–284.
Berridge, M. J., Bootman, M. D., & Lipp, P. (1998). Calcium-a life and death signal. Nature, 395, 645–648.
Berridge, M. J., Lipp, P., & Bootman, M. D. (2000). The versatility and universality of calcium signalling. Nature Reviews. Molecular Cell Biology, 1, 11–21.
Berridge, M. J., Bootman, M. D., & Roderick, H. L. (2003). Calcium signalling: Dynamics, homeostasis and remodelling. Nature Reviews. Molecular Cell Biology, 4, 517–529.
Bezprozvanny, I., Scheller, R. H., & Tsien, R. W. (1995). Functional impact of syntaxin on gating of N-type and Q-type calcium channels. Nature, 378, 623–626.
Bhattacharjee, A., Whitehurst, R. M., Jr., Zhang, M., Wang, L., & Li, M. (1997). T-type calcium channels facilitate insulin secretion by enhancing general excitability in the insulin-secreting β-cell line, INS-1. Endocrinology, 138, 3735–3740.
Bosco, D., Meda, P., Halban, P. A., & Rouiller, D. G. (2000). Importance of cell-matrix interactions in rat islet β-cell secretion in vitro: Role of α6β1 integrin. Diabetes, 49, 233–243.
Braun, M., Ramracheya, R., Bengtsson, M., Zhang, Q., Karanauskaite, J., Partridge, C., Johnson, P. R., & Rorsman, P. (2008). Voltage-gated ion channels in human pancreatic β-cells: Electrophysiological characterization and role in insulin secretion. Diabetes, 57, 1618–1628.
Catterall, W. A. (2000). Structure and regulation of voltage-gated Ca2+ channels. Annual Review of Cell and Developmental Biology, 16, 521–555.
Chandra, J., Yang, S. N., Kohler, M., Zaitsev, S., Juntti-Berggren, L., Berggren, P. O., Zhivotovsky, B., & Orrenius, S. (2001). Effects of serum from patients with type 1 diabetes on primary cerebellar granule cells. Diabetes, 50, S77–S81.
Chang, I., Cho, N., Kim, S., Kim, J. Y., Kim, E., Woo, J. E., Nam, J. H., Kim, S. J., & Lee, M. S. (2004). Role of calcium in pancreatic islet cell death by IFN-γ/TNF-α. Journal of Immunology, 172, 7008–7014.
Davalli, A. M., Biancardi, E., Pollo, A., Socci, C., Pontiroli, A. E., Pozza, G., Clementi, F., Sher, E., & Carbone, E. (1996). Dihydropyridine-sensitive and -insensitive voltage-operated calcium channels participate in the control of glucose-induced insulin release from human pancreatic β cells. The Journal of Endocrinology, 150, 195–203.
Efanova, I. B., Zaitsev, S. V., Zhivotovsky, B., Kohler, M., Efendic, S., Orrenius, S., & Berggren, P. O. (1998). Glucose and tolbutamide induce apoptosis in pancreatic β-cells. A process dependent on intracellular Ca2+ concentration. The Journal of Biological Chemistry, 273, 33501–33507.
Efrat, S., Surana, M., & Fleischer, N. (1991). Glucose induces insulin gene transcription in a murine pancreatic β-cell line. The Journal of Biological Chemistry, 266, 11141–11143.
Erion, K. A., & Corkey, B. E. (2017). Hyperinsulinemia: A cause of obesity? Current Obesity Reports, 6, 178–186.
Esposito, C., & Caputo, I. (2005). Mammalian transglutaminases. Identification of substrates as a key to physiological function and physiopathological relevance. The FEBS Journal, 272, 615–631.
Gallagher, E. J., & LeRoith, D. (2020). Hyperinsulinaemia in cancer. Nature Reviews. Cancer, 20, 629–644.
German, M. S., Moss, L. G., & Rutter, W. J. (1990). Regulation of insulin gene expression by glucose and calcium in transfected primary islet cultures. The Journal of Biological Chemistry, 265, 22063–22066.
Goll, D. E., Thompson, V. F., Li, H., Wei, W., & Cong, J. (2003). The calpain system. Physiological Reviews, 83, 731–801.
Gui, P., Wu, X., Ling, S., Stotz, S. C., Winkfein, R. J., Wilson, E., Davis, G. E., Braun, A. P., Zamponi, G. W., & Davis, M. J. (2006). Integrin receptor activation triggers converging regulation of Cav1.2 calcium channels by c-Src and protein kinase A pathways. The Journal of Biological Chemistry, 281, 14015–14025.
Hall, K. E., Sima, A. A., & Wiley, J. W. (1995). Voltage-dependent calcium currents are enhanced in dorsal root ganglion neurones from the Bio Bred/Worchester diabetic rat. The Journal of Physiology, 486, 313–322.
Hall, K. E., Sima, A. A., & Wiley, J. W. (1996). Opiate-mediated inhibition of calcium signaling is decreased in dorsal root ganglion neurons from the diabetic BB/W rat. The Journal of Clinical Investigation, 97, 1165–1172.
Hall, K. E., Liu, J., Sima, A. A., & Wiley, J. W. (2001). Impaired inhibitory G-protein function contributes to increased calcium currents in rats with diabetic neuropathy. Journal of Neurophysiology, 86, 760–770.
Hibino, H., Pironkova, R., Onwumere, O., Rousset, M., Charnet, P., Hudspeth, A. J., & Lesage, F. (2003). Direct interaction with a nuclear protein and regulation of gene silencing by a variant of the Ca2+-channel β4 subunit. Proceedings of the National Academy of Sciences of the United States of America, 100, 307–312.
Holmkvist, J., Tojjar, D., Almgren, P., Lyssenko, V., Lindgren, C. M., Isomaa, B., Tuomi, T., Berglund, G., Renstrom, E., & Groop, L. (2007). Polymorphisms in the gene encoding the voltage-dependent Ca2+ channel CaV2.3 (CACNA1E) are associated with type 2 diabetes and impaired insulin secretion. Diabetologia, 50, 2467–2475.
Hrvatin, S., O’Donnell, C. W., Deng, F., Millman, J. R., Pagliuca, F. W., DiIorio, P., Rezania, A., Gifford, D. K., & Melton, D. A. (2014). Differentiated human stem cells resemble fetal, not adult, beta cells. Proceedings of the National Academy of Sciences of the United States of America, 111, 3038–3043.
Huo, J., Metz, S. A., & Li, G. (2003). Role of tissue transglutaminase in GTP depletion-induced apoptosis of insulin-secreting (HIT-T15) cells. Biochemical Pharmacology, 66, 213–223.
Iwashima, Y., Pugh, W., Depaoli, A. M., Takeda, J., Seino, S., Bell, G. I., & Polonsky, K. S. (1993). Expression of calcium channel mRNAs in rat pancreatic islets and downregulation after glucose infusion. Diabetes, 42, 948–955.
Ji, J., Yang, S. N., Huang, X., Li, X., Sheu, L., Diamant, N., Berggren, P. O., & Gaisano, H. Y. (2002). Modulation of L-type Ca2+ channels by distinct domains within SNAP-25. Diabetes, 51, 1425–1436.
Jing, X., Li, D. Q., Olofsson, C. S., Salehi, A., Surve, V. V., Caballero, J., Ivarsson, R., Lundquist, I., Pereverzev, A., Schneider, T., et al. (2005). CaV2.3 calcium channels control second-phase insulin release. The Journal of Clinical Investigation, 115, 146–154.
Juntti-Berggren, L., Larsson, O., Rorsman, P., Ammala, C., Bokvist, K., Wahlander, K., Nicotera, P., Dypbukt, J., Orrenius, S., Hallberg, A., et al. (1993). Increased activity of L-Type Ca2+ channels exposed to serum from patients with type I diabetes. Science, 261, 86–90.
Juntti-Berggren, L., Refai, E., Appelskog, I., Andersson, M., Imreh, G., Dekki, N., Uhles, S., Yu, L., Griffiths, W. J., Zaitsev, S., et al. (2004). Apolipoprotein CIII promotes Ca2+-dependent β cell death in type 1 diabetes. Proceedings of the National Academy of Sciences of the United States of America, 101, 10090–10094.
Kang, Y., Huang, X., Pasyk, E. A., Ji, J., Holz, G. G., Wheeler, M. B., Tsushima, R. G., & Gaisano, H. Y. (2002). Syntaxin-3 and syntaxin-1A inhibit L-type calcium channel activity, insulin biosynthesis and exocytosis in β-cell lines. Diabetologia, 45, 231–241.
Kantengwa, S., Baetens, D., Sadoul, K., Buck, C. A., Halban, P. A., & Rouiller, D. G. (1997). Identification and characterization of α3β1 integrin on primary and transformed rat islet cells. Experimental Cell Research, 237, 394–402.
Kato, S., Ishida, H., Tsuura, Y., Tsuji, K., Nishimura, M., Horie, M., Taminato, T., Ikehara, S., Odaka, H., Ikeda, H., et al. (1996). Alterations in basal and glucose-stimulated voltage-dependent Ca2+ channel activities in pancreatic β cells of non-insulin-dependent diabetes mellitus GK rats. The Journal of Clinical Investigation, 97, 2417–2425.
Kawakami, A., Aikawa, M., Libby, P., Alcaide, P., Luscinskas, F. W., & Sacks, F. M. (2006). Apolipoprotein CIII in apolipoprotein B lipoproteins enhances the adhesion of human monocytic cells to endothelial cells. Circulation, 113, 691–700.
Komatsu, M., Yokokawa, N., Takeda, T., Nagasawa, Y., Aizawa, T., & Yamada, T. (1989). Pharmacological characterization of the voltage-dependent calcium channel of pancreatic β-cell. Endocrinology, 125, 2008–2014.
Lang, J. (1999). Molecular mechanisms and regulation of insulin exocytosis as a paradigm of endocrine secretion. European Journal of Biochemistry, 259, 3–17.
Lee, B., & Laychock, S. G. (2000). Regulation of inositol trisphosphate receptor isoform expression in glucose-desensitized rat pancreatic islets: Role of cyclic adenosine 3′,5′-monophosphate and calcium. Endocrinology, 141, 1394–1402.
Lee, K., Kim, J., Kohler, M., Yu, J., Shi, Y., Yang, S. N., Ryu, S. H., & Berggren, P. O. (2018). Blocking Ca2+ channel β3 subunit reverses diabetes. Cell Reports, 24, 922–934.
Leveque, C., Hoshino, T., David, P., Shoji-Kasai, Y., Leys, K., Omori, A., Lang, B., El Far, O., Sato, K., & Martin-Moutot, N. (1992). The synaptic vesicle protein synaptotagmin associates with calcium channels and is a putative Lambert-Eaton myasthenic syndrome antigen. Proceedings of the National Academy of Sciences of the United States of America, 89, 3625–3629.
Ligon, B., Boyd, A. E., & Dunlap, K. (1998). Class A calcium channel variants in pancreatic islets and their role in insulin secretion. The Journal of Biological Chemistry, 273, 13905–13911.
Liu, J. S., & Hebrok, M. (2017). All mixed up: Defining roles for β-cell subtypes in mature islets. Genes & Development, 31, 228–240.
Liu, X., Van Vleet, T., & Schnellmann, R. G. (2004). The role of calpain in oncotic cell death. Annual Review of Pharmacology and Toxicology, 44, 349–370.
MacDonald, P. E., Joseph, J. W., & Rorsman, P. (2005). Glucose-sensing mechanisms in pancreatic β-cells. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 360, 2211–2225.
Macfarlane, W. M., Campbell, S. C., Elrick, L. J., Oates, V., Bermano, G., Lindley, K. J., Aynsley-Green, A., Dunne, M. J., James, R. F., & Docherty, K. (2000). Glucose regulates islet amyloid polypeptide gene transcription in a PDX1- and calcium-dependent manner. The Journal of Biological Chemistry, 275, 15330–15335.
Maedler, K., Spinas, G. A., Lehmann, R., Sergeev, P., Weber, M., Fontana, A., Kaiser, N., & Donath, M. Y. (2001). Glucose induces β-cell apoptosis via upregulation of the Fas receptor in human islets. Diabetes, 50, 1683–1690.
Mathis, D., Vence, L., & Benoist, C. (2001). β-Cell death during progression to diabetes. Nature, 414, 792–798.
Mochida, S., Sheng, Z. H., Baker, C., Kobayashi, H., & Catterall, W. A. (1996). Inhibition of neurotransmission by peptides containing the synaptic protein interaction site of N-type Ca2+ channels. Neuron, 17, 781–788.
Mukai, E., Fujimoto, S., Sato, H., Oneyama, C., Kominato, R., Sato, Y., Sasaki, M., Nishi, Y., Okada, M., & Inagaki, N. (2011). Exendin-4 suppresses Src activation and reactive oxygen species production in diabetic Goto-Kakizaki rat islets in an Epac-dependent manner. Diabetes, 60, 218–226.
Namkung, Y., Skrypnyk, N., Jeong, M. J., Lee, T., Lee, M. S., Kim, H. L., Chin, H., Suh, P. G., Kim, S. S., & Shin, H. S. (2001). Requirement for the L-type Ca2+ channel α1D subunit in postnatal pancreatic β cell generation. The Journal of Clinical Investigation, 108, 1015–1022.
Newcomb, R., Szoke, B., Palma, A., Wang, G., Chen, X., Hopkins, W., Cong, R., Miller, J., Urge, L., Tarczy-Hornoch, K., et al. (1998). Selective peptide antagonist of the class E calcium channel from the venom of the tarantula Hysterocrates gigas. Biochemistry, 37, 15353–15362.
Nikolova, G., Jabs, N., Konstantinova, I., Domogatskaya, A., Tryggvason, K., Sorokin, L., Fassler, R., Gu, G., Gerber, H. P., Ferrara, N., et al. (2006). The vascular basement membrane: A niche for insulin gene expression and β cell proliferation. Developmental Cell, 10, 397–405.
Ohta, M., Nelson, J., Nelson, D., Meglasson, M. D., & Erecinska, M. (1993). Effect of Ca++ channel blockers on energy level and stimulated insulin secretion in isolated rat islets of Langerhans. The Journal of Pharmacology and Experimental Therapeutics, 264, 35–40.
Orrenius, S., Zhivotovsky, B., & Nicotera, P. (2003). Regulation of cell death: The calcium-apoptosis link. Nature Reviews. Molecular Cell Biology, 4, 552–565.
Ovalle, F., Grimes, T., Xu, G., Patel, A. J., Grayson, T. B., Thielen, L. A., Li, P., & Shalev, A. (2018). Verapamil and beta cell function in adults with recent-onset type 1 diabetes. Nature Medicine, 24, 1108–1112.
Pereverzev, A., Mikhna, M., Vajna, R., Gissel, C., Henry, M., Weiergraber, M., Hescheler, J., Smyth, N., & Schneider, T. (2002a). Disturbances in glucose-tolerance, insulin-release, and stress-induced hyperglycemia upon disruption of the CaV2.3 (α1E) subunit of voltage-gated Ca2+ channels. Molecular Endocrinology, 16, 884–895.
Pereverzev, A., Vajna, R., Pfitzer, G., Hescheler, J., Klockner, U., & Schneider, T. (2002b). Reduction of insulin secretion in the insulinoma cell line INS-1 by overexpression of a CaV2.3 (α1E) calcium channel antisense cassette. European Journal of Endocrinology, 146, 881–889.
Piedras-Renteria, E. S., Watase, K., Harata, N., Zhuchenko, O., Zoghbi, H. Y., Lee, C. C., & Tsien, R. W. (2001). Increased expression of α1A Ca2+ channel currents arising from expanded trinucleotide repeats in spinocerebellar ataxia type 6. The Journal of Neuroscience, 21, 9185–9193.
Pipeleers, D., Chintinne, M., Denys, B., Martens, G., Keymeulen, B., & Gorus, F. (2008). Restoring a functional β-cell mass in diabetes. Diabetes, Obesity & Metabolism, 10(Suppl 4), 54–62.
Pittenger, G. L., Liu, D., & Vinik, A. I. (1997). The apoptotic death of neuroblastoma cells caused by serum from patients with insulin-dependent diabetes and neuropathy may be Fas-mediated. Journal of Neuroimmunology, 76, 153–160.
Popiela, H., & Moore, W. (1991). Tolbutamide stimulates proliferation of pancreatic beta cells in culture. Pancreas, 6, 464–469.
Rajagopal, S., Fields, B. L., & Kamatchi, G. L. (2014). Contribution of protein kinase Calpha in the stimulation of insulin by the down-regulation of Cavbeta subunits. Endocrine, 47, 463–471.
Reinbothe, T. M., Alkayyali, S., Ahlqvist, E., Tuomi, T., Isomaa, B., Lyssenko, V., & Renstrom, E. (2013). The human L-type calcium channel CaV1.3 regulates insulin release and polymorphisms in CACNA1D associate with type 2 diabetes. Diabetologia, 56, 340–349.
Rettig, J., Sheng, Z. H., Kim, D. K., Hodson, C. D., Snutch, T. P., & Catterall, W. A. (1996). Isoform-specific interaction of the α1A subunits of brain Ca2+ channels with the presynaptic proteins syntaxin and SNAP-25. Proceedings of the National Academy of Sciences of the United States of America, 93, 7363–7368.
Rhodes, C. J. (2005). Type 2 diabetes-a matter of β-cell life and death? Science, 307, 380–384.
Ristic, H., Srinivasan, S., Hall, K. E., Sima, A. A., & Wiley, J. W. (1998). Serum from diabetic BB/W rats enhances calcium currents in primary sensory neurons. Journal of Neurophysiology, 80, 1236–1244.
Robertson, R. P., Seaquist, E. R., & Walseth, T. F. (1991). G proteins and modulation of insulin secretion. Diabetes, 40, 1–6.
Rorsman, P., & Braun, M. (2013). Regulation of insulin secretion in human pancreatic islets. Annual Review of Physiology, 75, 155–179.
Rorsman, P., & Renstrom, E. (2003). Insulin granule dynamics in pancreatic beta cells. Diabetologia, 46, 1029–1045.
Rose, T., Efendic, S., & Rupnik, M. (2007). Ca2+-secretion coupling is impaired in diabetic Goto Kakizaki rats. The Journal of General Physiology, 129, 493–508.
Rueckschloss, U., & Isenberg, G. (2004). Contraction augments L-type Ca2+ currents in adherent guinea-pig cardiomyocytes. The Journal of Physiology, 560, 403–411.
Rustenbeck, I., Herrmann, C., & Grimmsmann, T. (1997). Energetic requirement of insulin secretion distal to calcium influx. Diabetes, 46, 1305–1311.
Salinno, C., Cota, P., Bastidas-Ponce, A., Tarquis-Medina, M., Lickert, H., & Bakhti, M. (2019). β-Cell maturation and identity in health and disease. The International Journal of Molecular Sciences, 20, 5417.
Saltiel, A. R. (2001). New perspectives into the molecular pathogenesis and treatment of type 2 diabetes. Cell, 104, 517–529.
Satin, L. S. (2000). Localized calcium influx in pancreatic β-cells: Its significance for Ca2+-dependent insulin secretion from the islets of Langerhans. Endocrine, 13, 251–262.
Schulla, V., Renstrom, E., Feil, R., Feil, S., Franklin, I., Gjinovci, A., Jing, X. J., Laux, D., Lundquist, I., Magnuson, M. A., et al. (2003). Impaired insulin secretion and glucose tolerance in β cell-selective CaV1.2 Ca2+ channel null mice. The EMBO Journal, 22, 3844–3854.
Sellick, G. S., Garrett, C., & Houlston, R. S. (2003). A novel gene for neonatal diabetes maps to chromosome 10p12.1-p13. Diabetes, 52, 2636–2638.
Sheng, Z. H., Rettig, J., Takahashi, M., & Catterall, W. A. (1994). Identification of a syntaxin-binding site on N-type calcium channels. Neuron, 13, 1303–1313.
Sheng, Z. H., Rettig, J., Cook, T., & Catterall, W. A. (1996). Calcium-dependent interaction of N-type calcium channels with the synaptic core complex. Nature, 379, 451–454.
Sheng, Z. H., Yokoyama, C. T., & Catterall, W. A. (1997). Interaction of the synprint site of N-type Ca2+ channels with the C2B domain of synaptotagmin I. Proceedings of the National Academy of Sciences of the United States of America, 94, 5405–5410.
Sheng, Z. H., Westenbroek, R. E., & Catterall, W. A. (1998). Physical link and functional coupling of presynaptic calcium channels and the synaptic vesicle docking/fusion machinery. Journal of Bioenergetics and Biomembranes, 30, 335–345.
Sher, E., Biancardi, E., Pollo, A., Carbone, E., Li, G., Wollheim, C. B., & Clementi, F. (1992). ω-Conotoxin-sensitive, voltage-operated Ca2+ channels in insulin-secreting cells. European Journal of Pharmacology, 216, 407–414.
Sher, E., Giovannini, F., Codignola, A., Passafaro, M., Giorgi-Rossi, P., Volsen, S., Craig, P., Davalli, A., & Carrera, P. (2003). Voltage-operated calcium channel heterogeneity in pancreatic β cells: Physiopathological implications. Journal of Bioenergetics and Biomembranes, 35, 687–696.
Shi, Y., Yang, G., Yu, J., Yu, L., Westenbroek, R., Catterall, W. A., Juntti-Berggren, L., Berggren, P. O., & Yang, S. N. (2014). Apolipoprotein CIII hyperactivates β cell CaV1 channels through SR-BI/β1 integrin-dependent coactivation of PKA and Src. Cellular and Molecular Life Sciences, 71, 1289–1303.
Shi, Y., Park, K. S., Kim, S. H., Yu, J., Zhao, K., Yu, L., Oh, K. W., Lee, K., Kim, J., Chaggar, K., et al. (2019). IgGs from patients with amyotrophic lateral sclerosis and diabetes target CaVα2δ1 subunits impairing islet cell function and survival. Proceedings of the National Academy of Sciences of the United States of America, 116(52), 26816–26822.
Sjoholm, A. (1995). Regulation of insulinoma cell proliferation and insulin accumulation by peptides and second messengers. Upsala Journal of Medical Sciences, 100, 201–216.
Solomon, M., & Sarvetnick, N. (2004). The pathogenesis of diabetes in the NOD mouse. Advances in Immunology, 84, 239–264.
Splawski, I., Timothy, K. W., Sharpe, L. M., Decher, N., Kumar, P., Bloise, R., Napolitano, C., Schwartz, P. J., Joseph, R. M., Condouris, K., et al. (2004). CaV1.2 calcium channel dysfunction causes a multisystem disorder including arrhythmia and autism. Cell, 119, 19–31.
Takiyama, Y., Sakoe, K., Namekawa, M., Soutome, M., Esumi, E., Ogawa, T., Ishikawa, K., Mizusawa, H., Nakano, I., & Nishizawa, M. (1998). A Japanese family with spinocerebellar ataxia type 6 which includes three individuals homozygous for an expanded CAG repeat in the SCA6/CACNL1A4 gene. Journal of the Neurological Sciences, 158, 141–147.
Taylor, C. W., da Fonseca, P. C., & Morris, E. P. (2004). IP3 receptors: The search for structure. Trends in Biochemical Sciences, 29, 210–219.
Toru, S., Murakoshi, T., Ishikawa, K., Saegusa, H., Fujigasaki, H., Uchihara, T., Nagayama, S., Osanai, M., Mizusawa, H., & Tanabe, T. (2000). Spinocerebellar ataxia type 6 mutation alters P-type calcium channel function. The Journal of Biological Chemistry, 275, 10893–10898.
Vajna, R., Klockner, U., Pereverzev, A., Weiergraber, M., Chen, X., Miljanich, G., Klugbauer, N., Hescheler, J., Perez-Reyes, E., & Schneider, T. (2001). Functional coupling between ‘R-type’ Ca2+ channels and insulin secretion in the insulinoma cell line INS-1. European Journal of Biochemistry, 268, 1066–1075.
van Belle, T. L., Coppieters, K. T., & von Herrath, M. G. (2011). Type 1 diabetes: Etiology, immunology, and therapeutic strategies. Physiological Reviews, 91, 79–118.
Waitkus-Edwards, K. R., Martinez-Lemus, L. A., Wu, X., Trzeciakowski, J. P., Davis, M. J., Davis, G. E., & Meininger, G. A. (2002). α4β1 Integrin activation of L-type calcium channels in vascular smooth muscle causes arteriole vasoconstriction. Circulation Research, 90, 473–480.
Wajchenberg, B. L. (2007). β-Cell failure in diabetes and preservation by clinical treatment. Endocrine Reviews, 28, 187–218.
Wang, L., Bhattacharjee, A., Fu, J., & Li, M. (1996). Abnormally expressed low-voltage-activated calcium channels in β-cells from NOD mice and a related clonal cell line. Diabetes, 45, 1678–1683.
Wang, L., Bhattacharjee, A., Zuo, Z., Hu, F., Honkanen, R. E., Berggren, P. O., & Li, M. (1999). A low voltage-activated Ca2+ current mediates cytokine-induced pancreatic β-cell death. Endocrinology, 140, 1200–1204.
Wiser, O., Trus, M., Hernandez, A., Renstrom, E., Barg, S., Rorsman, P., & Atlas, D. (1999). The voltage sensitive LC-type Ca2+ channel is functionally coupled to the exocytotic machinery. Proceedings of the National Academy of Sciences of the United States of America, 96, 248–253.
Wollheim, C. B., & Sharp, G. W. (1981). Regulation of insulin release by calcium. Physiological Reviews, 61, 914–973.
Wollheim, C. B., Kikuchi, M., Renold, A. E., & Sharp, G. W. (1978). The roles of intracellular and extracellular Ca++ in glucose-stimulated biphasic insulin release by rat islets. The Journal of Clinical Investigation, 62, 451–458.
Wu, X., Davis, G. E., Meininger, G. A., Wilson, E., & Davis, M. J. (2001). Regulation of the L-type calcium channel by α5β1 integrin requires signaling between focal adhesion proteins. The Journal of Biological Chemistry, 276, 30285–30292.
Xu, S., Laccotripe, M., Huang, X., Rigotti, A., Zannis, V. I., & Krieger, M. (1997). Apolipoproteins of HDL can directly mediate binding to the scavenger receptor SR-BI, an HDL receptor that mediates selective lipid uptake. Journal of Lipid Research, 38, 1289–1298.
Xu, G., Chen, J., Jing, G., & Shalev, A. (2012). Preventing β-cell loss and diabetes with calcium channel blockers. Diabetes, 61, 848–856.
Yamada, Y., Kuroe, A., Li, Q., Someya, Y., Kubota, A., Ihara, Y., Tsuura, Y., & Seino, Y. (2001). Genomic variation in pancreatic ion channel genes in Japanese type 2 diabetic patients. Diabetes/Metabolism Research and Reviews, 17, 213–216.
Yang, S. N., & Berggren, P. O. (2005a). β-Cell CaV channel regulation in physiology and pathophysiology. American Journal of Physiology. Endocrinology and Metabolism, 288, E16–E28.
Yang, S. N., & Berggren, P. O. (2005b). CaV2.3 channel and PKCλ: New players in insulin secretion. The Journal of Clinical Investigation, 115, 16–20.
Yang, S. N., & Berggren, P. O. (2006). The role of voltage-gated calcium channels in pancreatic β-cell physiology and pathophysiology. Endocrine Reviews, 27, 621–676.
Yang, S. N., Larsson, O., Branstrom, R., Bertorello, A. M., Leibiger, B., Leibiger, I. B., Moede, T., Kohler, M., Meister, B., & Berggren, P. O. (1999). Syntaxin 1 interacts with the LD subtype of voltage-gated Ca2+ channels in pancreatic β cells. Proceedings of the National Academy of Sciences of the United States of America, 96, 10164–10169.
Yang, S. N., Shi, Y., Yang, G., Li, Y., Yu, J., & Berggren, P. O. (2014). Ionic mechanisms in pancreatic β cell signaling. Cellular and Molecular Life Sciences, 71, 4149–4177.
Yang, G., Shi, Y., Yu, J., Li, Y., Yu, L., Welling, A., Hofmann, F., Striessnig, J., Juntti-Berggren, L., Berggren, P. O., et al. (2015). CaV1.2 and CaV1.3 channel hyperactivation in mouse islet β cells exposed to type 1 diabetic serum. Cellular and Molecular Life Sciences, 72, 1197–1207.
Yoshida, K., & Kikutani, H. (2000). Genetic and immunological basis of autoimmune diabetes in the NOD mouse. Reviews in Immunogenetics, 2, 140–146.
Yu, J., Shi, Y., Zhao, K., Yang, G., Yu, L., Li, Y., Andersson, E. M., Ammala, C., Yang, S. N., & Berggren, P. O. (2020). Enhanced expression of β cell CaV3.1 channels impairs insulin release and glucose homeostasis. Proceedings of the National Academy of Sciences of the United States of America, 117, 448–453.
Zaitsev, S. V., Appelskog, I. B., Kapelioukh, I. L., Yang, S. N., Kohler, M., Efendic, S., & Berggren, P. O. (2001). Imidazoline compounds protect against interleukin 1β-induced β-cell apoptosis. Diabetes, 50, S70–S76.
Zhang, W., Khan, A., Ostenson, C. G., Berggren, P. O., Efendic, S., & Meister, B. (2002). Down-regulated expression of exocytotic proteins in pancreatic islets of diabetic GK rats. Biochemical and Biophysical Research Communications, 291, 1038–1044.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yang, SN., Shi, Y., Zhao, K., Yang, G., Yu, J., Berggren, PO. (2022). Pancreatic β Cell CaV Channels in Health and Disease. In: Zamponi, G.W., Weiss, N. (eds) Voltage-Gated Calcium Channels . Springer, Cham. https://doi.org/10.1007/978-3-031-08881-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-031-08881-0_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08880-3
Online ISBN: 978-3-031-08881-0
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)