Abstract
Cardiovascular diseases (CVDs) are among the leading causes of mortality in the United States and worldwide. Cholesterol at high levels in circulation has been established as a major risk factor for CVDs in humans. Statins have been widely used for lowering and controlling the endogenous levels of cholesterol to prevent or treat CVDs. Statins lower cholesterol by inhibiting 3-hydroxy-3-methyl-glutaryl-CoA reductase (HMG-CoA reductase), the rate-limiting enzyme in the biosynthetic pathway of endogenous cholesterol. Despite their efficacy for cardiovascular indications, statins may induce undesired side effects, including cause skeletal muscle damage (myotoxicity and myalgia). However, the mechanisms and treatment of statin-induced myotoxicity and myalgia are not well known. Phospholipase D (PLD) is a ubiquitous membrane phospholipid-hydrolyzing enzyme involved in mediating lipid signaling in mammalian cells, including skeletal muscle cells (myocytes). Therefore, we hypothesized that statins would mediate skeletal muscle myocyte damage through activation of the PLD-mediated lipid signaling, and inhibition of PLD activation would protect against the statin-induced myotoxicity. In order to test our hypothesis, we used the well-established C2C12 mouse skeletal muscle myoblast cell line and studied the PLD activation and cytotoxicity in vitro induced by two different widely prescribed statins (mevastatin and simvastatin). Our studies revealed that the statins caused dose- (10–100 μM) and time-dependent (4–24 h) activation of PLD (as determined by the [32]P-labeling of cells and thin-layer chromatography of phosphatidylbutanol formation) and cytotoxicity and mitochondrial dysfunction (as determined by the release of intracellular lactate dehydrogenase, suppression of MTT reduction, and alterations in cell morphology) in the C2C12 myoblast cells. Our results also showed that cholesterol replenishment protected against the statin-induced toxicity to the C2C12 cells. Furthermore, our results showed that the novel PLD-specific inhibitor, 5-fluoro-2-indolyl des-chlorohalopemide (FIPI) inhibited the statin-induced PLD activation and cytotoxicity in the C2C12 myoblast cells. For the first time, our study demonstrated the role of endogenous cellular cholesterol depletion and PLD-mediated lipid signaling in statin-induced skeletal muscle myocyte damage and emphasized the importance of PLD inhibition in attenuating the statin-induced myotoxicity and myalgia in CVD patients consuming statins to lower the elevated levels of endogenous cholesterol.
This work was submitted as honors dissertation by the author, Eric M. Tretter for partial fulfillment of the requirements for graduation “With Honors Research Distinction” in the College of Arts and Sciences of The Ohio State University in 2015 under the supervision of Dr. Narasimham L. Parinandi.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Cardiovascular Disease
In developed countries across the world, and particularly in the United States, cardiovascular disease (CVD), including the cerebrovascular diseases, remain the number one cause of death [1, 2]. CVD is the result of restricted blood vessels that lead to chest pain, stroke, heart attack, or other painful heart conditions [3,4,5,6,7]. A host of risk factors have been identified for CVD, including a diet high in fat and cholesterol, lack of exercise, use of tobacco, drugs, and alcohol, and a stressful environment [8,9,10,11,12,13,14,15]. High concentrations of circulating blood cholesterol can cause the deposition of this cholesterol in blood vessels and eventually lead to plaque formation in the blood vessel and ultimate obstruction of the circulation to vital organs, including the heart, brain, and kidney [16,17,18,19]. Prescription of drugs that lower endogenously synthesized cholesterol in order to lower the risk for cardiovascular disease have become increasingly common to modify CVD risk [20].
Cholesterol and Cardiovascular Diseases
Cholesterol is the major component of the cell membrane lipid backbone that regulates membrane fluidity, structure, and function [21, 22]. Cholesterol occurs in circulation in two different types: high-density lipoproteins (HDLs) and low-density lipoproteins (LDLs) [23, 24]. HDLs have been found to reduce the risk for heart disease when in high concentrations, and thus are often designated as “good cholesterol” [25]. In contrast, high concentrations of LDLs are associated with coronary artery disease, earning them the distinction of “bad cholesterol” [26]. Having high concentrations of LDL-cholesterol (LDL-C) is referred to as hypercholesterolemia, and can have genetic or dietary roots [26].
Familial hypercholesterolemia is an inherited condition caused by a defect in LDL-C receptor expression/function [27]. Dysfunction in LDL-C receptors results in insufficient uptake of LDL-C into cells, leading to increased circulating LDL-C in the bloodstream that can accumulate on the vessel walls. In addition, individuals with familial hypercholesterolemia typically demonstrate a loss of the normal feedback inhibition that stops the synthesis of cholesterol by inhibiting 3-hydroxy-3-methyl-glutaryl-CoA reductase (HMG-CoA reductase), a rate-limiting enzyme in cholesterol synthesis (Schema 1), when high concentrations are detected in the blood [28,29,30] (Schema 1). Dietary hypercholesterolemia results from a diet high in saturated fats and cholesterol, more than recommended daily allowance. The excessive amount of cholesterol consumed finds its way into the blood stream and can accumulate on vessel walls leading to plaque formation and atherosclerotic lesions in the blood vessel that would obstruct blood flow leading to the CVDs and cerebrovascular disorders.
Statins as the Endogenous Cholesterol-Lowering Drugs
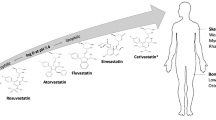
Current therapeutic intervention for hypercholesterolemia involves the use of HMG-CoA reductase-specific inhibitors, known as statins (Schema 2), to attenuate or suppress the synthesis of endogenous cholesterol [28,29,30]. Suppressing or inhibiting endogenous cholesterol synthesis lowers the levels of LDL-C in the blood circulation. Among the most common statins in clinical use are atorvastatin (Lipitor), pravastatin (Pravachol), simvastatin (Zocor), mevastatin (Compactin), and lovastatin (Altoprev) [31,32,33].
Although statins have dramatically altered the landscape for CVD risk, adverse effects have been identified, yet are not well understood. Myopathy is a disorder encompassing an array of ailments that impact the skeletal muscles, and is one of the most common and significant side effects of statin myotoxicity. Conditions developed can vary from the milder myalgia or myositis to the possibly life-threatening rhabdomyolysis [34,35,36,37,38,39,40]. Symptoms of statin-induced myopathy include muscle pain, weakness, and fatigue [35]. Studies have shown that statins use in certain individuals results in statin intolerance associated with myotoxicity [34,35,36,37,38,39,40,41,42]. The exact rate of incidence is still disputed. In observational studies, statin-associated muscle symptoms (SAMS) have been seen in between 10% and 30% of statin users [35]. In other randomized control studies, 9.4% of patients taking statins experienced myalgia compared to the 4.6% of placebo patients that experienced myalgia [35]. However, a recent study from Jordan found that overall incidence of myopathy in patients taking statins was 27.8%; specifically, incidence was 31.4% in males, 22.6% in females, and 34% among patients ≥60 years old [36]. According to a separate study of patients experiencing statin myopathy, 13% were hospitalized for treatment for rhabdomyolysis [37]. More importantly, though, all of the patients in the study who ceased using statins were able to successfully recover from statin-associated myopathy within an average of 2.3 months after stopping statin treatment, with over 50% reporting resolution of muscle symptoms within 1 month [37]. Statins have pleiotropic effects in the body, but the mechanism through which they cause myalgia or other adverse effects remains unclear. If understood, the safety and effectiveness of statins could increase. It seems there exist multiple mechanisms through which statins cause myotoxicity, one being the mitochondrial mechanism, which holds valid to some extent [43]. Previous studies have shown that statins can cause damage to skeletal myocyte mitochondria, which reduces the energy metabolism of the cell and can ultimately result in cell death [38, 39, 44]. Based on this previous work, we hypothesized that statins cause membrane lipid signaling perturbation and mitochondrial dysfunction through cholesterol depletion, which ultimately leads to statin-induced myalgia.
Lipid Signaling and Statin-Induced Myotoxicity or Myalgia
The phospholipid bilayer forms a barrier between the cell and the external environment. Membrane phospholipids, protein channels, and cholesterol compose much of the membrane bilayer of living cells across species, including in humans [45,46,47]. An essential function of the bilayer is to interact with the environment and relay information to the cell wherein the membrane lipid signaling accomplishes these goals [48]. Phospholipases are the house-keeping enzymes that hydrolyze membrane phospholipids to support turnover/maintenance of the membrane, leading to the formation of a host of bioactive lipid molecules, each with an associated membrane lipid signal as interpreted by the cell. Four major phospholipases exist, including the phospholipase A1, A2, C, and D, and each catalyzes a specific hydrolysis of the membrane phospholipid within the cell [49,50,51,52,53,54]. Specifically, phospholipase D (PLD) hydrolyzes the membrane phospholipid (phosphatidylcholine, PC) releasing phosphatidic acid (PA), a potent bioactive cell signaling mediator [53, 55]. The cell can further convert the PLD-generated PA to potent bioactive lipid signal mediators such as lysophosphatidic acid (LPA) or diacylglycerol (DAG) upon the actions of phospholipase A1 (PLA1) or PLA2, which can cause myotoxicity (Schema 3) [56,57,58,59,60,61]. It has been demonstrated that lowering of cell membrane cholesterol in the vascular endothelial cells leads to the activation of PLD and generation of PA [62]. Therefore, here it is hypothesized that statins cause cholesterol depletion in the membranes of the skeletal muscle cells through the inhibition of HMG-CoA reductase, leading to the activation of PLD that generates the bioactive lipid signal mediator (PA), resulting in mitochondrial damage and myotoxicity as a mechanistic basis of the statin-induced myalgia or myotoxicity. In order to test our hypothesis, in the current study, we chose the well-established skeletal muscle cell model, C2C12 myoblast cells. Our studies revealed that the two widely used statins (HMG-CoA reductase inhibitors), mevastatin and simvastatin, caused PLD activation and generation of the bioactive lipid signal mediator (PA), leading to the mitochondrial dysfunction and cytotoxicity in the C2C12 myoblast cells through cholesterol depletion [63].
Mechanism of the phospholipase D (PLD)-mediated hydrolysis of the membrane phospholipids (e.g., phosphatidylcholine, PC) in mammalian cells. PLD hydrolyzes PC at the head group and forms the bioactive lipid signal mediator, phosphatidic acid (PA). PA can further be converted to potent bioactive lipid signal mediators such as the lysophosphatidic acid (LPA) by the action of phospholipases A1/A2 (PLA1 or PLA2) and diacylglycerol (DAG) by the action of lipid phosphate phosphatase. Both LPA and DAG are potent lipid mediators of cell signaling. PA can also directly modulate cellular proteins and cause functional alterations in the cells. One salient feature of PLD is that enzyme is capable of using stereospecifically a primary alcohol instead of water such as ethanol, 1-butanol, and 1-propanol during the hydrolysis of the membrane phospholipid to convert the PLD-generated PA into the corresponding phosphatidylalcohols (e.g., phosphatidylethanol [PEt], phosphatidylbutanol [PBt], and phosphatidylpropanol [PProp]). Hence, the phosphatidylalcohols serve as the indices of PLD activity in cells in situ
Materials and Methods
Materials
Mouse skeletal muscle myoblast cells (C2C12s) (passage 2) were obtained from Cell Applications Inc. (San Diego, CA). Phosphate-buffered saline (PBS) was purchased from Biofluids Inc (Rockville, Maryland). Minimal Essential Medium (MEM), FBS, trypsin, nonessential amino acids, penicillin/streptomycin, Dulbecco Modified Eagle Medium (DMEM) tissue culture reagents, phosphate-free modified medium, 3-[4,5-dimethylthiazol-2-yl]-2, 5-diphenyl tetrazolium bromide reduction kit (MTT assay kit), lactate dehydrogenase cytotoxicity assay kit (LDH release assay kit), and analytical reagents of the highest purity were all obtained from Sigma Chemical Co (St Louis, Missouri). Phosphatidylbutanol (PBt), was acquired from Avanti Polar Lipids (Alabaster, Alabama). [32P]orthophosphate (carrier-free) was purchased from New England Nuclear (Wilmington, Delaware). Anti-rabbit AlexaFluor 488-conjugated antibody and the Amplex Red cholesterol determination kit were purchased from Molecular Probes Invitrogen Co (Carlsbad, California). 5-Fluoro-2-indolyl des-chlorohalopemide hydrochloride hydrate (FIPI) was prepared as described in earlier publications [59, 60]. All other reagents were acquired from the Sigma Chemical Company (St. Louis, MO).
In Vitro Cell Culture
The C2C12 myoblast cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% FBS and antibiotics up to 90–100% confluence in sterile 35-mm or 60-mm dishes and in 96-well plates under a sterile and humidified atmosphere of 95% air–5% CO2 at 37 °C. C2C12s were used up to passage 20 for experiments.
Assay of Phospholipase D (PLD) Activation
PLD activity in the C2C12 myoblast cells was determined according to our previously published procedure [59, 60]. C2C12 myoblast cells cultured in 35-mm dishes were labeled with [32P]orthophosphate (5 mCi/ml) in DMEM phosphate-free medium containing 2% (vol/vol) fetal bovine serum for 14 h. Following the experimental treatments for the chosen periods of time, [32P]-labeled phosphatidylbutanol ([32P]PBt), formed from the PLD activation and transphosphatidylation reaction in cellular lipid extracts as an index of PLD activity in intact cells, was separated by thin-layer chromatography (TLC). Radioactivity associated with the [32P]PBt was quantified by liquid scintillation counting and data were expressed as DPM normalized to the total [32P] in the lipid extract of the cells in the dish.
Lactate Dehydrogenase (LDH) Release Assay of Cytotoxicity
The C2C12 myoblast cells were grown up to 90–100% confluence in sterile 15.5-mm dishes (24-well culture plate) and treated with DMEM alone or DMEM containing the chosen concentrations of statins and/or FIPI at designated time points. At the end of the incubation period, the supernatant was removed, and the level of lactate dehydrogenase (LDH) activity was measured spectrophotometrically according to the manufacturer’s protocol (Sigma Chemical Co., St. Louis, MO).
MTT Cell Proliferation Assay
The C2C12 myoblast cells were grown up to 90–100% confluence in sterile 15.5-mm dishes (24-well culture plate) and treated with DMEM alone or DMEM containing the chosen concentrations of statins and/or FIPI at designated time points. At the end of the incubation period, the supernatant was removed, and the extent of MTT reduction was measured spectrophotometrically according to the manufacturer’s protocols (Cayman Chemical Co., Ann Arbor, MI).
Cellular Morphology
Morphological changes in the C2C12 myoblast cells grown in the sterile 35-mm dishes up to 90–100% confluence, following their exposure to the chosen concentrations of statins and/or FIPI for different time periods, were examined under light microscope as an index of cytotoxicity. Images of cell morphology were digitally captured using the Zeiss Axioskop 200 with Zen 2011 software at 20× magnification.
Cholesterol Determination
The C2C12 myoblast cells were grown up to 90–100% confluence in sterile 60-mm dishes, and treated with DMEM alone or DMEM containing the chosen concentrations of statins and/or FIPI for the chosen periods of time. Cells were then liberated from dish, reconstituted in PBS, and protein was determined following the protein determination by the BCA assay. Cholesterol contents in the samples was normalized to the total cellular protein (1 mg) according to our previously published method [64].
Phospholipase D1 (PLD1) Phosphorylation Visualization by Confocal Immunofluorescence Microscopy
The C2C12 myoblast cells were grown on sterile glass cover slips (~90% confluence) and treated with DMEM alone or DMEM containing chosen concentrations of statins for 12 h. Cover slips were then rinsed three times with PBS, and fixed with 3.7% formaldehyde in PBS for 10 min. at room temperature. The cells were permeabilized in 0.25% Triton X-100 prepared in PBS containing 0.01% Tween-20 (PBS-T) for 5 min. The cells were again washed three times with PBS-T, and treated with PBS-T containing 1% BSA blocking buffer for 30 min. at room temperature. Cover slips were then incubated overnight at room temperature with the primary antibody [phospho-PLD1 (1:150 dilution)] in 1% BSA solution. After rinsing three times with PBS-T, the cells were labeled with secondary AlexaFluor 488 (1:100 dilution) in 1% BSA in PBS-T for 1 h. Finally, the cells were washed three times with PBS-T, mounted, and examined under Zeiss LSM 710 Confocal/Multiphoton Microscope powered by Argon-2 laser with 500–550 BP filter. The images were captured digitally, and the average fluorescent intensity of triplicate samples was determined using ImageJ.
Preparation of Solutions Containing Pharmacological Agents for Treatment of Cells
All water-soluble pharmacological agent solutions were freshly formulated in DMEM for treatment of cells. The stock solutions of lipophilic pharmacological agents, including all statins and FIPI, were freshly assembled in DMSO and then diluted in DMEM for treatment of cells. The final DMSO concentration in the cell treatment medium did not exceed 0.1% (vol/vol) and did not appear to have any influence on experimental outcomes.
Statistical Analysis
All experiments were completed in triplicate. Results were reported as mean ± standard deviation (SD). Statistical analysis of data was accomplished by one-way analysis of variance (ANOVA) by use of the SigmaStat (Jandel Scientific, San Rafael, California). The statistical significance level was taken as p ≤ 0.05.
Results
Statins induce PLD activation in C2C12 myoblast cells
Statins are HMG-CoA reductase inhibitors and lower endogenous levels of cholesterol by inhibiting cellular cholesterol synthesis [65, 66]. We have previously shown that the cholesterol-depleting agent such as the methyl-β-cyclodextrin (MβCD) lowers cholesterol levels and causes activation of PLD in the vascular endothelial cells [62, 64]. Taking these as the premise, here we hypothesized that statin-induced decrease of cellular cholesterol would lead to activation of PLD in C2C12 myoblast cells. To test our hypothesis, we treated C2C12 cells with two selected statins, mevastatin and simvastatin, for different periods of time (4–24 h) and assayed the activation of PLD. We determined the activity of PLD by analyzing the intracellular formation of phosphatidylbutanol as the transphosphatidylation reaction product of PLD, which is an established and widely used assay of cellular PLD activity [67]. Both mevastatin and simvastatin (10 μM) caused significant time-dependent activation of PLD in the C2C12 myoblast cells (Fig. 1a, b). Although the PLD activity peaked at 12 h for mevastatin-treated cells, simvastatin caused a significant linear increase of the PLD activity from 4 h up to 24 h compared to the untreated control cells (Fig. 1a, b). At 12 h, mevastatin caused a 4.5-fold increase of PLD activation in the C2C12 cells compared to control untreated and mevastatin-treated cells at 4 h. PLD activity remained significantly elevated at 24 h compared to control, although not to the level observed at 12 h. On the other hand, simvastatin caused a significant and approximately sevenfold increase in PLD activity at 24 h as compared to the same in the control untreated and simvastatin-treated cells at 4 h (Fig. 1b). One noteworthy response of the control untreated cells was that the basal PLD activity (formation of PA without statin treatment) also linearly increased with time (Fig. 1a, b). These results revealed that both mevastatin and simvastatin caused a significant activation of PLD in the C2C12 myoblast cells and simvastatin apparently was more potent than mevastatin in inducing the activation of PLD and generating the bioactive lipid signal mediator (PA) in cells.
(a) Mevastatin induces PLD activation in C2C12 cells. C2C12 myoblast cells (2 × 105 cells) were pre-labeled for 12 h with carrier free [32P] orthophosphate in complete medium, following which cells were treated with mevastatin (10 μM) for different time periods (4–24 h) in 95% air–5% CO2 under humidified sterile environment at 37 °C. Under identical conditions, appropriate controls were established without the statin treatment. At the end of the experiment for the designated time, lipids were extracted under acidic conditions with 2:1 chloroform-methanol (vol/vol) and separated by thin-layer chromatography (TLC) as described in the section “Materials and Methods”. Phosphatidylbutanol (PBt) as the product of PLD activity generated by the transphosphatidylation reaction was identified by iodination on the TLC plate with authentic PBt standard as described in the section “Materials and Methods”. The PBt spots on the TLC plates wereFig. 1 (continued) scrapped and [32P] radioactivity was determined on a liquid scintillation counter and normalized to the total lipid phosphorus [32P] of the cells and expressed as DPM/cells in the dish. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. (b) Simvastatin induces PLD activation in C2C12 cells. C2C12 myoblast cells (2 × 105 cells) were pre-labeled for 12 h with carrier free [32P] orthophosphate in complete medium, following which cells were treated with simvastatin (10 μM) for different time periods (4–24 h) under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Under identical conditions, appropriate controls were established without the statin treatment. At the end of the experiment for the designated time, lipids were extracted under acidic conditions with 2:1 chloroform-methanol (vol/vol) and separated by thin-layer chromatography (TLC) as described in the section “Materials and Methods”. Phosphatidylbutanol (PBt) as the product of PLD activity generated by the transphosphatidylation reaction was identified by iodination on the TLC plate with authentic PBt standard as described in the section “Materials and Methods”. The PBt spots on the TLC plates were scrapped and [32P] radioactivity was determined on a liquid scintillation counter and normalized to the total lipid phosphorus [32P] of the cells and expressed as DPM/cells in the dish. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05
FIPI, the PLD-specific inhibitor attenuates statin-induced PLD activation in C2C12 cells
In previous studies, we have demonstrated efficacy of FIPI, the only available PLD-specific pharmacological inhibitor, in PLD inhibition in cell culture models [59, 60]. Here, we used FIPI (i) to investigate its inhibitory action on the statin-induced PLD activation and (ii) to confirm that statins indeed activate PLD in the C2C12 myoblast cells. By virtue of its PLD-specific inhibitory action, FIPI (0.1–1 μM, 12 h of pretreatment) significantly and drastically inhibited the basal PLD activity in the control untreated C2C12 myoblast cells at 24 h (Fig. 2a, b). At 1 μM concentration, FIPI caused ~85–92% decrease of basal PLD activation in the control untreated cells (Fig. 2a, b). Furthermore, FIPI, in a dose-dependent manner (0.1–1 μM), significantly and robustly attenuated the statin-induced PLD activation in cells treated with both mevastatin (10 μM) and simvastatin (10 μM) for 24 h as compared with the cells treated with statins alone (Fig. 2a, b). FIPI (1 μM) significantly attenuated the statin-induced PLD activation by ~90–95% in cells treated with both mevastatin (10 μM) and simvastatin (10 μM) for 24 h as compared to the same in the C2C12 myoblast cells treated with statins alone (Fig. 2a, b). These results clearly revealed that (i) FIPI was a potent inhibitor of the statin-induced PLD activation at doses ranging between 0.1–1 μM and the 1 μM dose was the most efficacious in causing effective inhibition of the statin-induced PLD activation and (ii) indeed, statins, induced the activation of PLD in the C2C12 myoblast cells.
(a) FIPI, the PLD-specific inhibitor, attenuates mevastatin-induced PLD activation in C2C12 cells. C2C12 myoblast cells (2 × 105 cells) were pre-labeled for 12 h with carrier free [32P] orthophosphate in complete medium, following which cells were first treated with the PLD-specific pharmacological inhibitor, FIPI (0.1–1 μM) for 12 h and then treated with mevastatin (10 μM) for 24 h in absence and presence of FIPI under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Under identical conditions, appropriate controls were established without FIPI and the statin treatment and with FIPI treatments alone. At the end of the experiment for the designated time, lipids were extracted under acidic conditions with 2:1 chloroform-methanol (vol/vol) and separated by thin-layer chromatography (TLC) as described in the section “Materials and Methods”. Phosphatidylbutanol (PBt) as the product of PLD activity generated by the transphosphatidylation reaction was identified by iodination on the TLC plate with authentic PBt standardFig. 2 (continued) as described in the section “Materials and Methods”. The PBt spots on the TLC plates were scrapped and [32P] radioactivity was determined on a liquid scintillation counter and normalized to the total lipid phosphorus [32P] of the cells and expressed as DPM/cells in the dish. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05. (b) FIPI, the PLD-specific inhibitor, attenuates simvastatin-induced PLD activation in C2C12 cells. C2C12 myoblast cells (2 × 105 cells) were pre-labeled for 12 h with carrier free [32P] orthophosphate in complete medium, following which cells were first treated with the PLD-specific pharmacological inhibitor, FIPI (0.1–1 μM) for 12 h and then treated with simvastatin (10 μM) for 24 h in absence and presence of FIPI under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Under identical conditions, appropriate controls were established without FIPI and the statin treatment and with FIPI treatments alone. At the end of the experiment for the designated time, lipids were extracted under acidic conditions with 2:1 chloroform-methanol (vol/vol) and separated by thin-layer chromatography (TLC) as described in the section “Materials and Methods”. Phosphatidylbutanol (PBt) as the product of PLD activity generated by the transphosphatidylation reaction was identified by iodination on the TLC plate with authentic PBt standard as described in the section “Materials and Methods”. The PBt spots on the TLC plates were scrapped and [32P] radioactivity was determined on a liquid scintillation counter and normalized to the total lipid phosphorus [32P] of the cells and expressed as DPM/cells in the dish. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05
Statins induce cytotoxicity in C2C12 cells
It is becoming increasingly evident that the lipid-lowering and cholesterol-depleting drugs such as the lipophilic statins cause cytotoxicity to mammalian cells including the normal and malignant cells [68,69,70,71]. Also, our earlier studies revealed that cyclodextrin-induced cellular cholesterol depletion causes cytotoxicity in the vascular endothelial cells in culture [62, 64]. Based on these findings, we investigated whether statins (simvastatin and mevastatin) induce cytotoxicity in C2C12 cells as determined by lactate dehydrogenase (LDH) release. Our results revealed that both simvastatin and mevastatin (10–100 μM) significantly induced LDH release from cells in a dose-dependent fashion at 24 h of exposure as compared to control untreated cells (Fig. 3a, b). Both statins at 10 μM dose caused robust and significant increase in the LDH release from cells (twofold increase by simvastatin; 3.7-fold increase by mevastatin) and further increase in release of the intracellular LDH was not markedly enhanced by increasing the dose of statins at 24 h of treatment of the C2C12 cells (Fig. 3a, b). Therefore, our current results revealed that statins (simvastatin and mevastatin) induced cytotoxicity in the C2C12 cells even at 10 μM dose as demonstrated by the release of intracellular LDH, the standard mammalian cytotoxicity assay. Furthermore, mevastatin was more potent than simvastatin at 10 μM dose in causing cytotoxicity in the C2C12 myoblast cells (Fig. 3a, b).
(a) Simvastatin induces lactate dehydrogenase (LDH) release from C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing Fig. 3 (continued) different concentrations of simvastatin (10–100 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of release of LDH was determined on a plate reader (visible) by the commercially available LDH spectrophotometric assay kit (Sigma Chemical Co., St. Louis, MO) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. (b) Mevastatin induces lactate dehydrogenase (LDH) release from C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing different concentrations of mevastatin (10–100 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of release of LDH was determined on a plate reader (visible) by the commercially available LDH spectrophotometric assay kit (Sigma Chemical Co., St. Louis, MO) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05
Statins decrease cholesterol in C2C12 cells
As statins are established to lower or decrease the cellular levels of cholesterol [70], here we investigated whether statins would decrease/lower the cholesterol levels in the C2C12 myoblast cells. All the three tested statins (simvastatin, mevastatin, and lovastatin) at 10 μM dose caused significant decrease of intracellular cholesterol (25%, 21%, and 46%, respectively) as compared to that in the control untreated cells at 24 h of treatment (Fig. 4a). Among all the chosen statins, lovastatin was the most effective statin in decreasing the intracellular cholesterol levels in the C2C12 myoblast cells. Therefore, these results revealed that statins caused significant decrease of the intracellular levels of cholesterol in the C2C12 myoblast cells.
(a) Statins induce decrease of cholesterol in C2C12 cells. C2C12 myoblast cells were cultured in complete medium up to ~90–100% confluence in 60-mm sterile culture dishes and treated with different statins at 10 μM concentration for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls were established simultaneously under identical condition without statin treatments. At the end of the treatment, the cholesterol content in the cells was then determined spectrofluorometrically on a plate reader (fluorescence) with the commercially available cholesterol determination kit according to the manufacturer’s recommendation (Molecular Probes – Invitrogen Detection Technologies, Grand Island, NY) as described in the section “Materials and Methods”. The cellular levels of cholesterol were normalized to protein and expressed as μg/mg protein. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. (b) Cholesterol replenishment protects against mevastatin-induced lactate dehydrogenase (LDH) release from C2C12 Cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing different concentrations of water-soluble cholesterol alone (1–2%) or mevastatin (10 μM) alone or water-soluble cholesterol (1–2%) + mevastatin (10 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the water-soluble cholesterol and statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of release of LDH was determined on a plate reader (visible) by the commercially available LDH spectrophotometric assay kit (Sigma Chemical Co., St. Louis, MO) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05. #Significantly different from the untreated control cells at p ≤ 0.05. (c) Cholesterol replenishment protects against simvastatin-induced lactate dehydrogenase (LDH) release from C2C12 Cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing different concentrations of water-soluble cholesterol alone (1–2%) or simvastatin (10 μM) alone or water-soluble cholesterol (1–2%) + simvastatin (10 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the water-soluble cholesterol and statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of release of LDH was determined on a plate reader (visible) by the commercially available LDH spectrophotometric assay kit (Sigma Chemical Co., St. Louis, MO) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05
Cholesterol replenishment protects against statin-induced cytotoxicity in C2C12 cells
Our earlier studies demonstrated that cholesterol replenishment offered protection against the cyclodextrin-induced cytotoxicity mediated through the intracellular cholesterol depletion in the vascular endothelial cells [64]. In the current study, we showed that statins cause both cytotoxicity (LDH release) and cholesterol depletion. Therefore, we investigated whether cholesterol replenishment would offer protection against the statin-induced cytotoxicity (LDH release) in the C2C12 myoblast cells. Our results revealed that both mevastatin (10 μM) and simvastatin (10 μM) caused significant cytotoxicity as revealed by the intracellular LDH release assay at 24 h of treatment with statins as compared to the control untreated cells (Fig. 4b, c). Furthermore, treatment of cells with the water-soluble (methylcyclodextrin-conjugated) cholesterol (1%) offered significant protection of the statin-induced cytotoxicity (attenuation of release of intracellular LDH) (Fig. 4b, c). However, cholesterol at 2% dose was not effective in lowering the mevastatin-induced release of intracellular LDH and failed to protect against the mevastatin-induced cytotoxicity in the C2C12 cells as opposed to the protective action offered by cholesterol at 1% dose (Fig. 4b). On the other hand, cholesterol at 2% dose, although effective in significantly protecting against the simvastatin-induced cytotoxicity in the C2C12 cells, its protective action was less effective than that was offered by cholesterol at 1% dose (Fig. 4c). Overall, these results revealed that (i) cholesterol replenishment offered protection against the statin-induced cytotoxicity in the C2C12 cells as revealed by the intracellular LDH assay and (ii) lower dose of cholesterol (1%) was more effective in significantly protecting against the statin-induced cytotoxicity.
FIPI, the PLD-specific inhibitor attenuates statin-induced cytotoxicity in C2C12 cells
We have earlier reported that the PLD-specific pharmacological inhibitor, FIPI protected against the oxidant- and drug-induced cytotoxicity mediated by the PLD-depended bioactive lipid signaling in the vascular endothelial cells [59, 60]. Therefore, here we investigated to show whether FIPI would offer protection against the statin-induced cytotoxicity (intracellular LDH release) in the C2C12 myoblast cells to demonstrate the role of PLD therein, since in the current study, it was revealed that statins caused significant activation of PLD which was significantly attenuated by FIPI in the C2C12 myoblast cells (Figs. 1 and 2). FIPI (1 μM, pretreatment for 12 h) offered significant protection against simvastatin (10 μM)- and mevastatin (10 μM)-induced cytotoxicity at 24 h as demonstrated by the release of intracellular LDH (Fig. 5). Overall, the current study demonstrated that (i) the PLD-specific pharmacological inhibitor, FIPI offered significant protection of the statin-induced cytotoxicity and (ii) the PLD-mediated bioactive lipid signaling also was involved in the statin-induced cytotoxicity in the C2C12 myoblast cells.
FIPI, the PLD-specific inhibitor, attenuates statin-induced lactate dehydrogenase (LDH) release from C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then pretreated for 12 h with FIPI, and then treated with simvastatin (10 μM) and mevastatin (10 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without and with FIPI and statins alone were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of release of LDH was determined on a plate reader (visible) by the commercially available LDH spectrophotometric assay kit (Sigma Chemical Co., St. Louis, MO) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05
Statins induce mitochondrial dysfunction in C2C12 cells
It is rapidly emerging that statins cause mitochondrial dysfunction and damage in different organs/cells, including the skeletal muscle, especially during the statin-induced myopathy [34, 72]. Although MTT reduction by the mitochondria is used as a valid indicator of cell proliferation and cytotoxicity, the assay is also utilized to ascertain the mitochondrial function [73]. Therefore, we utilized MTT reduction by the cellular mitochondria in the C2C12 cells to demonstrate the statin-induced mitochondrial dysfunction, since MTT is reduced by a mitochondria-specific dehydrogenase [73]. Both statins, simvastatin and mevastatin, caused significant dose-dependent decrease of MTT reduction in the C2C12 cells at 24 h of treatment as compared to the control untreated cells (Fig. 6a, b). Simvastatin (10 μM) and mevastatin (10 μM) significantly decreased MTT reduction, by 51% and 60%, respectively, by the C2C12 myoblast cells treated for 24 h as compared to the same in the control untreated cells (Fig. 6a, b). Therefore, these studies demonstrated that both mevastatin and simvastatin induced the mitochondrial dysfunction as revealed by the decrease in the MTT reduction by the C2C12 cells.
(a) Simvastatin induces decrease of MTT reduction by C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing different concentrations of simvastatin (10–100 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of MTT reduction by the cells was determined on a plate reader (visible) by the commerciallyFig. 6 (continued) available MTT reduction spectrophotometric assay kit (Cayman Chemical Co., Ann Arbor, MI) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. (b) Mevastatin induces decrease of MTT reduction by C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium and then treated with complete medium or medium containing different concentrations of mevastatin (10–100 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without the statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of MTT reduction by the cells was determined on a plate reader (visible) by the commercially available MTT reduction spectrophotometric assay kit (Cayman Chemical Co., Ann Arbor, MI) according to the manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05
FIPI, the PLD-specific inhibitor attenuates statin-induced mitochondrial dysfunction by C2C12 cells
In the earlier experiments of the current study, we had shown that (i) statins induced PLD activation; (ii) FIPI, the PLD-specific pharmacological inhibitor, attenuated the statin-induced PLD activation; and (iii) FIPI offered protection against the statin-induced cytotoxicity (intracellular LDH release) in the C2C12 myoblasts. Hence, here we investigated whether FIPI would attenuate the statin-induced mitochondrial dysfunction as assayed by the decrease of MTT reduction by the C2C12 cells to establish a link between the statin-induced PLD activation and bioactive lipid signal mediator (PA) generation and mitochondrial dysfunction. FIPI (1 μM, 12 h of pretreatment) significantly and markedly attenuated the simvastatin (10 μM)- and mevastatin (10 μM)-induced decrease of MTT reduction by the C2C12 cells (Fig. 7a). Furthermore, the protective action of FIPI against the simvastatin-induced decrease of MTT reduction by the C2C12 cells was more pronounced than that induced by mevastatin (Fig. 7a). Overall, these studies demonstrated that FIPI significantly attenuated the statin-induced mitochondrial dysfunction in the C2C12 myoblast cells as demonstrated by the mitochondria-specific MTT reduction assay, suggesting the role of PLD-generated bioactive lipid signal mediators therein.
(a) FIPI, the PLD-specific inhibitor, attenuates statin-induced decrease of MTT reduction by C2C12 cells. C2C12 myoblast cells were cultured up to ~90–100% confluence in 15.5-mm sterile dishes (24-well cell culture plate) in complete medium, pre-treated with the PLD-specific pharmacological inhibitor (FIPI, 1 μM) for 12 h, and then treated with complete medium alone or medium containing FIPI alone or medium containing simvastatin (10 μM) and mevastatin (10 μM) for 24 h under a humidified sterile atmosphere of 95% air–5% CO2 at 37 °C. Appropriate controls without FIPI treatment and the statin treatments were established simultaneously under identical conditions. At the end of the treatment, the supernatant was removed, and the extent of MTT reduction by the cells was determined on a plate reader (visible) by the commercially available MTT reduction spectrophotometric assay kit (Cayman Chemical Co., Ann Arbor, MI) according to theFig. 7 (continued) manufacturer’s recommendations as described in the section “Materials and Methods”. Each histogram is an average of results obtained from three independent experiments under identical conditions with ± S.D. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05. (b) FIPI, the PLD-specific inhibitor, attenuates statin-induced morphological alterations in C2C12 cells. C2C12 myoblast cells were cultured in sterile 35-mm dishes up to ~90–100% confluence in complete medium under a humidified atmosphere of 95% air–5% CO2 at 37 °C, and then pre-treated with the PLD-specific pharmacological inhibitor, FIPI (1 μM) alone for 12 h, following which the cells were treated with medium alone or medium containing simvastatin (10 μM), mevastatin (10 μM), and lovastatin (10 μM), or FIPI (1 μM) + statin (10 μM) for 24 h. Appropriate controls were established with cells treated with medium alone or FIPI alone under identical conditions. At the end of the experiment, the images of cellular morphology were digitally captured using the Zeiss Axioskop 200 with Zen 2011 software at 20× magnification. Each photomicrograph is a typical representative of at least three independent observations from three different experiments conducted under identical conditions
FIPI, the PLD-specific inhibitor attenuates statin-induced morphological alterations in C2C12 Cells
Our results so far revealed that statins (mevastatin and simvastatin) induced cytotoxicity and mitochondrial dysfunction that was mediated by the PLD-generated bioactive lipid signaling and cholesterol depletion in the C2C12 myoblast cells. Cell morphology alterations serve as an index of cytotoxicity induced by toxic stresses [73, 74]. Here, we sought to test whether statins would induce morphological alterations in the C2C12 myoblast cells, which might be protected by the PLD-specific pharmacological inhibitor, FIPI. Simvastatin, mevastatin, and lovastatin at 10 μM dose caused severe cell morphological alteration at 24 h of treatment characterized by the light microscopic examinations, including elongated myoblast cells turning into round and circular cells (Fig. 7b). This indicated the drastic changes in the morphological nature of the cells upon the statin treatment. However, FIPI pre-treatment (1 μM for 12 h) offered almost complete protection of the statin-induced morphological alterations in the C2C12 myoblast cells (Fig. 7b). These results further confirmed that the statin-induced cell morphological alterations (cytotoxicity) was (i) protected by the PLD-specific pharmacological inhibitor, FIPI and (ii) PLD-generated bioactive lipid signaling through PA formation played a role in the statin-induced cell morphology alterations in the C2C12 cells.
Statins induce threonine phosphorylation of PLD1 in C2C12 cells
Our earlier reports revealed that oxidant stress and heavy metal toxicity cause the protein kinase-mediated serine-threonine phosphorylation of PLD isoenzymes upstream of PLD activation [60, 67]. Since the protein kinase-mediated serine-threonine phosphorylation regulates the activity of PLD isoenzymes, in this study, we investigated whether statins would induce threonine phosphorylation of PLD1 isoenzyme in the C2C12 myoblast cells as examined by the confocal immunofluorescence microscopy with the aid of PLD-phosphothreonine-specific antibody immunostaining. Both mevastatin and simvastatin at 10 μM dose induced intense phosphorylation of PLD1 isoenzyme in intact C2C12 myoblast cells at 12 h of treatment of cells with the statins (upstream of maximal PLD activation at 24 h) as compared to the same in the control untreated cells (Fig. 8a, b). This study demonstrated that statins induce serine phosphorylation of PLD1 isoenzyme upstream of the activation of the enzyme.
(a) Statins induce threonine phosphorylation of PLD1 in C2C12 cells. C2C12s were cultured on sterile glass cover slips (90% confluence) in complete medium under a humidified atmosphere of 95% air–5% CO2 at 37 °C and then treated with complete medium alone or medium containing chosen concentrations of statins for 12 h. As described in the section “Materials and Methods”, the cells on the cover slips were treated overnight at room temperature with the primary antibody [phosphothreonine-PLD1 (1:150 dilution)] in 1% BSA solution. Following that, the cells were labeled with the secondary AlexaFluor 488 (1:100 dilution) for 1 h and then the cells wereFig. 8 (continued) examined under the Zeiss LSM 710 Confocal/Multiphoton Microscope powered by Argon-2 laser with 500–550 BP filter. The images were captured digitally. Each confocal fluorescence micrograph is a typical representative of three independent observations from three different experiments conducted under identical conditions. The bright green fluorescence in situ depicts the threonine phosphorylation of PLD1 isoform. (b) Quantitative Analysis of Phospho-PLD1 by Confocal Fluorescence Microscopy. C2C12s were cultured on sterile glass cover slips (90% confluence) in complete medium under a humidified atmosphere of 95% air–5% CO2 at 37 °C and then treated with complete medium alone or medium containing chosen concentrations of statins for 12 h. As described in the section “Materials and Methods”, the cells on the cover slips were treated overnight at room temperature with the primary antibody [phosphothreonine-PLD1 (1:150 dilution)] in 1% BSA solution. Following that, the cells were labeled with the secondary AlexaFluor 488 (1:100 dilution) for 1 h and then the cells were examined under the Zeiss LSM 710 Confocal/Multiphoton Microscope powered by Argon-2 laser with 500–550 BP filter. The images were captured digitally. Each histogram is an average intensity of fluorescence of three independent confocal fluorescence micrographs of untreated control cells and treatments in triplicates with ± standard deviations. *Significantly different from the untreated control cells at p ≤ 0.05. **Significantly different from the statin-treated cells at p ≤ 0.05
Discussion
High cholesterol levels (hypercholesterolemia) in circulation have been considered as a risk factor for human vascular disorders, cardiovascular diseases (CVDs), cerebrovascular diseases, and chronic heart diseases (CHD). Therefore, aggressive therapy with cholesterol-lowering drugs to lower the endogenously synthesized cholesterol is common clinical practice [28,29,30,31,32,33]. Among the most successful and widely prescribed cholesterol-lowering drugs are the statins that target the HMG-CoA reductase as a rate-limiting enzyme in the cholesterol biosynthetic pathway [28,29,30] (Schema 1). However, it is becoming increasingly evident that statins are associated with adverse effects such as statin myalgia or statin myotoxicity [41, 42]. Mitochondrial dysfunction, apoptosis, and coenzyme-Q10 (CoQ10) depletion have been identified as potential cellular mediators of statin-induced dysfunction, but the precise mechanism remains unknown [34, 43, 44, 70]. In the current study, we hypothesized that statins would cause cholesterol depletion in the membranes of the skeletal muscle cells through the inhibition of HMG-CoA reductase (Schema 1), leading to the activation of PLD that could generate the bioactive lipid signal mediator (PA) (Schema 3), which in turn induces mitochondrial damage and myotoxicity as a mechanistic basis of the statin-induced myalgia or myotoxicity. To test our hypothesis, we utilized the well-established skeletal muscle cell model, the C2C12 myoblast cells. The current study demonstrated that the two widely used statins, mevastatin and simvastatin, induced PLD activation and formation of the bioactive lipid signal mediator (PA) causing mitochondrial dysfunction and cytotoxicity in a skeletal muscle cell model (C2C12 myoblast cells) through the decrease of endogenous cholesterol (Schema 4).
Proposed mechanism of statin-induced PLD activation leading to cytotoxicity through depletion of endogenous cholesterol in C2C12 myoblast cells. In addition to loss of cellular cholesterol, the PLD-generated lipid signal mediator, phosphatidic acid (PA) apparently is responsible for causing the statin-induced myotoxicity in the cells. Also, mitochondrial dysfunction, as observed by the loss of MTT reduction appears to be a critical player in statin-induced cytotoxicity in the C2C12 myoblast cells. Statin-induced PLD activation appears to be mediated by the upstream threonine phosphorylation of PLDs that may be regulated by the statin-mediated loss of membrane cholesterol and subsequent activation of the serine-threonine protein kinases. Both cholesterol replenishment and the pharmacological inhibition of PLD by the PLD-specific inhibitor, FIPI, offer protection against the statin-induced cytotoxicity in C2C12 myoblast cells. Overall, the results of the present study suggest that the statin-induced myotoxicity is mediated by the upstream cholesterol loss and the associated PLD activation leading to generation of the bioactive lipid signal mediator (PA) and also the mitochondrial dysfunction
By virtue of their ability to selectively inhibit the rate-limiting enzyme in the cholesterol biosynthetic pathway in the mammalian cells, statins drastically decrease or deplete the endogenous levels of cholesterol. On the other hand, cholesterol is an important lipidic component of the cell membranes that regulates the membrane structure and function [21, 22]. Our earlier studies demonstrated that the widely used experimental cholesterol-depleting agent, methyl-β-cyclodextrin (MβCD) causes cytotoxicity to vascular endothelial cells through cellular cholesterol depletion, which can be reversed with cholesterol replenishment, indicating that cellular cholesterol plays a crucial role in maintaining the viability of the mammalian cells [62, 64]. We propose that statin-induced cytotoxicity in C2C12 myoblast cells observed in the current study was caused by a similar depletion of cellular cholesterol in the skeletal muscle cell model. This was also confirmed by replenishing the cells with the water-soluble cholesterol which rescued the cells from statin-induced cytotoxicity. Together, these data suggest that statin-mediated cellular cholesterol depletion promotes statin-induced myotoxicity and myalgia.
Phospholipase D (PLD) is ubiquitously present in mammalian cells and belongs to the family of phospholipases that drive membrane phospholipid hydrolysis (Schema 3) [56,57,58,59,60,61]. Although PLD is a house-keeping enzyme involved in the metabolism of membrane phospholipids, the enzyme is known to be activated by a variety of agonists, including hormones, reactive oxygen species, heavy metals, toxins, and metabolic stresses [56,57,58,59,60,61]. PLD exists in cells as two isoforms, PLD1 and PLD2 [56,57,58,59,60,61]. Protein kinases such as mitogen-activated protein kinases (MAPKs), protein tyrosine kinases, protein kinase C, G-protein coupled receptors, and receptor-mediated kinases phosphorylate the PLD isoforms at the corresponding amino acid residues (serine or threonine or tyrosine), leading to their translocation and activation [56,57,58,59,60,61]. Upon activation, PLD hydrolyzes cell membrane phospholipids (e.g., phosphatidylcholine) to form PA, a highly potent bioactive signal lipid linked to cellular cytoskeletal alterations and cytotoxicity [59, 60]. Our earlier studies demonstrated that cholesterol depletion mediated by MβCD in the vascular endothelial cells activates PLD, causing cytotoxicity through the generation of the lipid signal mediator, PA [62]. Along these lines, in the current study, it was demonstrated for the first time that statins induced the activation of PLD in the C2C12 cells which was attenuated by the PLD-specific inhibitor, FIPI. Furthermore, the current study also showed that the PLD-specific inhibitor, FIPI effectively protected against the statin-induced cytotoxicity. The results of the current study also revealed that statins induced the upstream threonine phosphorylation of PLD1 isoenzyme in the C2C12 cells that could have been mediated by the MAPKs or PKC, leading to the translocation and activation of the enzyme as previously observed in other cellular models. Thus, a connection between statin-induced PLD activation and statin cytotoxicity in the C2C12 muscle cell model offers a PLD-dependent mechanism of statin myotoxicity and myalgia, suggesting a role of the PLD-generated bioactive lipids such as PA, LPA, and DAG therein.
In the current study, it was shown that statins caused the mitochondrial dysfunction as determined by the MTT reduction ability in the C2C12 cells [73]. The statin-induced mitochondrial dysfunction (decrease in MTT reduction catalyzed by the mitochondrial dehydrogenase) and cytotoxic cell morphology alterations were attenuated by the PLD-specific inhibitor. This suggested a reasonable connection or association with the PLD activation and subsequent generation of the bioactive signal lipid mediators (PA, LPA, and DAG) and the mitochondrial dysfunction and cytotoxicity in the C2C12 myoblast cells. However, other mitochondria-driven mechanisms of the statin-induced myotoxicity such as apoptosis, CoQ10 loss, decline of ATP production, and reactive oxygen species generation are not ruled out in mediating the statin-induced cytotoxicity in the C2C12 cells.
Overall, the current study demonstrated that the cholesterol-lowering HMG-CoA inhibitor drugs, statins, caused the cellular cholesterol depletion leading to the activation of PLD, which in turn caused the mitochondrial dysfunction and cytotoxicity in the skeletal muscle cell model, C2C12 cells (Schema 4). Thus, it is highly reasonable to ascertain that PLD activation and formation of the PLD-generated bioactive lipids could act as potential players in the statin-induced myalgia and myotoxicity. Therefore, PLD could be a pharmacological target for combating the statin myotoxicity.
Abbreviations
- ATP:
-
Adenosine 5-phosphate
- BCA:
-
Bicinchoninic acid
- BSA:
-
Bovine serum albumin
- CHD:
-
Chronic heart disease
- CoQ10:
-
Coenzyme Q10
- CVD:
-
Cardiovascular disease
- DAG:
-
Diacylglycerol
- DMEM:
-
Dulbecco’s modified Eagle medium
- DMSO:
-
Dimethylsulfoxide
- EDTA:
-
Ethylenediaminetetraacetic acid
- FBS:
-
Fetal bovine serum
- FIPI:
-
5-fluoro-2-indolyl des-chlorohalopemide hydrochloride hydrate
- HDL:
-
High-density lipoprotein
- HMG-CoA reductase:
-
3-hydroxy-3-methyl-glutaryl-CoA reductase
- LDH:
-
Lactate dehydrogenase
- LDL-C:
-
Low-density lipoprotein-cholesterol
- LPA:
-
Lysophosphatidic acid
- MAPK:
-
Mitogen-activated protein kinase
- MβCD:
-
Methyl-β-cyclodextrin
- MEM:
-
Minimal essential medium
- MTT:
-
3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide
- PA:
-
Phosphatidic acid
- PBS:
-
Phosphate-buffered saline
- PBS-T:
-
Phosphate-buffered saline-Tween-20
- PBt:
-
Phosphatidylbutanol
- PKC:
-
Protein kinase C
- PLA2:
-
Phospholipase A2
- PLD:
-
Phospholipase D
- ROS:
-
Reactive oxygen species
- TLC:
-
Thin-layer chromatography
References
Stock EO, Redberg R. Cardiovascular disease in women. Curr Probl Cardiol. 2012;37(11):450–526. https://doi.org/10.1016/j.cpcardiol.2012.07.001.
Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37(4):1053–9. https://doi.org/10.1161/01.hyp.37.4.1053.
Essop MR, Peters F. Contemporary issues in rheumatic fever and chronic rheumatic heart disease. Circulation. 2014;130(24):2181–8. https://doi.org/10.1161/CIRCULATIONAHA.114.009857.
Granger DN, Vowinkel T, Petnehazy T. Modulation of the inflammatory response in cardiovascular disease. Hypertension. 2004;43(5):924–31. https://doi.org/10.1161/01.HYP.0000123070.31763.55.
Chen K, Keaney JF Jr. Evolving concepts of oxidative stress and reactive oxygen species in cardiovascular disease. Curr Atheroscler Rep. 2012;14(5):476–83. https://doi.org/10.1007/s11883-012-0266-8.
Varghese MJ. Familial hypercholesterolemia: a review. Ann Pediatr Cardiol. 2014;7(2):107–17. https://doi.org/10.4103/0974-2069.132478.
Xiong J, Miller VM, Li Y, Jayachandran M. Microvesicles at the crossroads between infection and cardiovascular diseases. J Cardiovasc Pharmacol. 2012;59(2):124–32. https://doi.org/10.1097/FJC.0b013e31820c6254.
Nasr VG, Kussman BD. Advances in the care of adults with congenital heart disease. Semin Cardiothorac Vasc Anesth. 2015;19(3):175–86. https://doi.org/10.1177/1089253214563989.
Singh S, Schwarz K, Horowitz J, Frenneaux M. Cardiac energetic impairment in heart disease and the potential role of metabolic modulators: a review for clinicians. Circ Cardiovasc Genet. 2014;7(5):720–8. https://doi.org/10.1161/CIRCGENETICS.114.000221.
Lamarche B, Couture P. It is time to revisit current dietary recommendations for saturated fat. Appl Physiol Nutr Metab. 2014;39(12):1409–11. https://doi.org/10.1139/apnm-2014-0141.
Gielen S, Laughlin MH, O’Conner C, Duncker DJ. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog Cardiovasc Dis. 2015;57(4):347–55. https://doi.org/10.1016/j.pcad.2014.10.001.
Buttar HS, Li T, Ravi N. Prevention of cardiovascular diseases: role of exercise, dietary interventions, obesity and smoking cessation. Exp Clin Cardiol. 2005;10(4):229–49.
Salabei JK, Conklin DJ. Cardiovascular autophagy: crossroads of pathology, pharmacology and toxicology. Cardiovasc Toxicol. 2013;13(3):220–9. https://doi.org/10.1007/s12012-013-9200-8.
Katsiki N, Tziomalos K, Mikhailidis DP. Alcohol and the cardiovascular system: a double-edged sword. Curr Pharm Des. 2014;20(40):6276–88. https://doi.org/10.2174/1381612820666140620125741.
Hartley L, Mavrodaris A, Flowers N, Ernst E, Rees K. Transcendental meditation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;12:CD010359. https://doi.org/10.1002/14651858.CD010359.pub2.
Badimon L, Vilahur G. LDL-cholesterol versus HDL-cholesterol in the atherosclerotic plaque: inflammatory resolution versus thrombotic chaos. Ann N Y Acad Sci. 2012;1254:18–32. https://doi.org/10.1111/j.1749-6632.2012.06480.x.
Cozma A, Orăşan O, Sâmpelean D, Fodor A, Vlad C, Negrean V, Rednic N, Zdrenghea D. Endothelial dysfunction in metabolic syndrome. Rom J Intern Med. 2009;47(2):133–40.
Sander GE, Giles TD. Hypertension and lipids: lipid factors in the hypertension syndrome. Curr Hypertens Rep. 2002;4(6):458–63. https://doi.org/10.1007/s11906-002-0026-1.
Madden JA. Role of the vascular endothelium and plaque in acute ischemic stroke. Neurology. 2012;79(13 Suppl 1):S58–62. https://doi.org/10.1212/WNL.0b013e3182695836.
Ewang-Emukowhate M, Wierzbicki AS. Lipid-lowering agents. J Cardiovasc Pharmacol Ther. 2013;18(5):401–11. https://doi.org/10.1177/1074248413492906.
Cortes VA, Busso D, Maiz A, Arteaga A, Nervi F, Rigotti A. Physiological and pathological implications of cholesterol. Front Biosci (Landmark Ed). 2014;19(3):416–28. https://doi.org/10.2741/4216.
Owen DM, Gaus K. Imaging lipid domains in cell membranes: the advent of super-resolution fluorescence microscopy. Front Plant Sci. 2013;4:503. https://doi.org/10.3389/fpls.2013.00503.
Najam O, Ray KK. Familial hypercholesterolemia: a review of the natural history, diagnosis, and management. Cardiol Ther. 2015;4(1):25–38. https://doi.org/10.1007/s40119-015-0037-z.
Scanu AM, Wisdom C. Serum lipoproteins structure and function. Annu Rev Biochem. 1972;41:703–30. https://doi.org/10.1146/annurev.bi.41.070172.003415.
Rached FH, Chapman MJ, Kontush A. HDL particle subpopulations: focus on biological function. Biofactors. 2015;41(2):67–77. https://doi.org/10.1002/biof.1202.
Elshourbagy NA, Meyers HV, Abdel-Meguid SS. Cholesterol: the good, the bad, and the ugly – therapeutic targets for the treatment of dyslipidemia. Med Princ Pract. 2014;23(2):99–111. https://doi.org/10.1159/000356856.
Santos RD, Maranhao RC. What is new in familial hypercholesterolemia? Curr Opin Lipidol. 2014;25(3):183–8. https://doi.org/10.1097/MOL.0000000000000073.
Trapani L, Segatto M, Incerpi S, Pallottini V. 3-Hydroxy-3-methylglutaryl coenzyme A reductase regulation by antioxidant compounds: new therapeutic tools for hypercholesterolemia? Curr Mol Med. 2011;11(9):790–7. https://doi.org/10.2174/156652411798062403.
McPherson PA. From fungus to pharmaceuticals--the chemistry of statins. Mini Rev Med Chem. 2012;12(12):1250–60. https://doi.org/10.2174/138955712802762103.
Salakhutdinov NF, Rogoza LN, Tolstikov GA. Hypercholesterolemia: chemical aspect of approach. Curr Med Chem. 2011;18(26):4076–105. https://doi.org/10.2174/092986711796957248.
Malinowski JM. Atorvastatin: a hydroxymethylglutaryl-coenzyme A reductase inhibitor. Am J Health Syst Pharm. 1998;55(21):2253–303. https://doi.org/10.1093/ajhp/55.21.2253.
Moghadasian MH, Mancini GB, Frohlich JJ. Pharmacotherapy of hypercholesterolaemia: statins in clinical practice. Expert Opin Pharmacother. 2000;1(4):683–95. https://doi.org/10.1517/14656566.1.4.683.
Opie LH. Present status of statin therapy. Trends Cardiovasc Med. 2015;25(3):216–25. https://doi.org/10.1016/j.tcm.2014.10.002.
Stroes ES, Thompson PD, Corsini A, Vladutiu GD, Raal FJ, Ray KK, Roden M, Stein E, Tokgözoğlu L, Nordestgaard BG, Bruckert E, De Backer G, Krauss RM, Laufs U, Santos RD, Hegele RA, Hovingh GK, Leiter LA, Mach F, März W, European Atherosclerosis Society Consensus Panel, et al. Statin-associated muscle symptoms: impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur Heart J. 2015;36(17):1012–22. https://doi.org/10.1093/eurheartj/ehv043.
Vinci P, Panizon E, Tosoni LM, Cerrato C, Pellicori F, Mearelli F, Biasinutto C, Fiotti N, Di Girolamo FG, Biolo G. Statin-associated myopathy: emphasis on mechanisms and targeted therapy. Int J Mol Sci. 2021;22(21):11687. https://doi.org/10.3390/ijms222111687.
Abed W, Abujbara M, Batieha A, Ajlouni K. Statin induced myopathy among patients attending the National Center for Diabetes, Endocrinology, & Genetics. Ann Med Surg. 2022;74(2012):103304. https://doi.org/10.1016/j.amsu.2022.103304.
Hansen KE, Hildebrand JP, Ferguson EE, Stein JH. Outcomes in 45 patients with statin-associated myopathy. Arch Intern Med. 2005;165(22):2671–6. https://doi.org/10.1001/archinte.165.22.2671.
Ward NC, Watts GF, Eckel RH. Statin toxicity. Circ Res. 2019;124(2):328–50. https://doi.org/10.1161/CIRCRESAHA.118.312782.
Turner RM, Pirmohamed M. Statin-related myotoxicity: a comprehensive review of pharmacokinetic, pharmacogenomic and muscle components. J Clin Med. 2019;9(1):22. https://doi.org/10.3390/jcm9010022.
Sathasivam S, Lecky B. Statin induced myopathy. BMJ. 2008;337:a2286. https://doi.org/10.1136/bmj.a2286.
Ganga HV, Slim HB, Thompson PD. A systematic review of statin-induced muscle problems in clinical trials. Am Heart J. 2014;168(1):6–15. https://doi.org/10.1016/j.ahj.2014.03.019.
Ahmad Z. Statin intolerance. Am J Cardiol. 2014;113(10):1765–71. https://doi.org/10.1016/j.amjcard.2014.02.033.
Sirvent P, Mercier J, Lacampagne A. New insights into mechanisms of statin-associated myotoxicity. Curr Opin Pharmacol. 2008;8(3):333–8. https://doi.org/10.1016/j.coph.2007.12.010.
Dirks AJ, Jones KM. Statin-induced apoptosis and skeletal myopathy. Am J Physiol Cell Physiol. 2006;291(6):C1208–12. https://doi.org/10.1152/ajpcell.00226.2006.
Korn ED. Current concepts of membrane structure and function. Fed Proc. 1969;28(1):6–11.
Siekevitz P. Biological membranes: the dynamics of their organization. Annu Rev Physiol. 1972;34:117–40. https://doi.org/10.1146/annurev.ph.34.030172.001001.
Suetsugu S, Kurisu S, Takenawa T. Dynamic shaping of cellular membranes by phospholipids and membrane-deforming proteins. Physiol Rev. 2014;94(4):1219–48. https://doi.org/10.1152/physrev.00040.2013.
Slone EA, Fleming SD. Membrane lipid interactions in intestinal ischemia/reperfusion-induced injury. Clin Immunol. 2014;153(1):228–40. https://doi.org/10.1016/j.clim.2014.04.018.
Richmond GS, Smith TK. Phospholipases A1. Int J Mol Sci. 2011;12(1):588–612. https://doi.org/10.3390/ijms12010588.
Tani K, Kogure T, Inoue H. The intracellular phospholipase A1 protein family. Biomol Concepts. 2012;3(5):471–8. https://doi.org/10.1515/bmc-2012-0014.
Ghosh M, Tucker DE, Burchett SA, Leslie CC. Properties of the Group IV phospholipase A2 family. Prog Lipid Res. 2006;45(6):487–510. https://doi.org/10.1016/j.plipres.2006.05.003.
Krizaj I. Roles of secreted phospholipases A2 in the mammalian immune system. Protein Pept Lett. 2014;21(12):1201–8.
Zhang Y, Frohman MA. Cellular and physiological roles for phospholipase D1 in cancer. J Biol Chem. 2014;289(33):22567–74. https://doi.org/10.1074/jbc.R114.576876.
Follo MY, Manzoli L, Poli A, McCubrey JA, Cocco L. PLC and PI3K/Akt/mTOR signalling in disease and cancer. Adv Biol Regul. 2015;57:10–6. https://doi.org/10.1016/j.jbior.2014.10.004.
Gomez-Cambronero J. Phospholipase D in cell signaling: from a myriad of cell functions to cancer growth and metastasis. J Biol Chem. 2014;289(33):22557–66. https://doi.org/10.1074/jbc.R114.574152.
Parinandi NL, Scribner WM, Vepa S, Shi S, Natarajan V. Phospholipase D activation in endothelial cells is redox sensitive. Antioxid Redox Signal. 1999;1(2):193–210. https://doi.org/10.1089/ars.1999.1.2-193.
Parinandi NL, Roy S, Shi S, Cummings RJ, Morris AJ, Garcia JG, Natarajan V. Role of Src kinase in diperoxovanadate-mediated activation of phospholipase D in endothelial cells. Arch Biochem Biophys. 2001;396(2):231–43. https://doi.org/10.1006/abbi.2001.2609.
Cummings R, Parinandi N, Wang L, Usatyuk P, Natarajan V. Phospholipase D/phosphatidic acid signal transduction: role and physiological significance in lung. Mol Cell Biochem. 2002;234–235(1–2):99–109.
Patel RB, Kotha SR, Sherwani SI, Sliman SM, Gurney TO, Loar B, Butler SO, Morris AJ, Marsh CB, Parinandi NL. Pulmonary fibrosis inducer, bleomycin, causes redox-sensitive activation of phospholipase D and cytotoxicity through formation of bioactive lipid signal mediator, phosphatidic acid, in lung microvascular endothelial cells. Int J Toxicol. 2011;30(1):69–90. https://doi.org/10.1177/1091581810388850.
Secor JD, Kotha SR, Gurney TO, Patel RB, Kefauver NR, Gupta N, Morris AJ, Haley BE, Parinandi NL. Novel lipid-soluble thiol-redox antioxidant and heavy metal chelator, N,N′-bis(2-mercaptoethyl)isophthalamide (NBMI) and phospholipase D-specific inhibitor, 5-fluoro-2-indolyl des-chlorohalopemide (FIPI) attenuate mercury-induced lipid signaling leading to protection against cytotoxicity in aortic endothelial cells. Int J Toxicol. 2011;30(6):619–38. https://doi.org/10.1177/1091581811422413.
Varadharaj S, Steinhour E, Hunter MG, Watkins T, Baran CP, Magalang U, Kuppusamy P, Zweier JL, Marsh CB, Natarajan V, Parinandi NL. Vitamin C-induced activation of phospholipase D in lung microvascular endothelial cells: regulation by MAP kinases. Cell Signal. 2006;18(9):1396–407. https://doi.org/10.1016/j.cellsig.2005.10.019.
Kline MA, O’Connor Butler ES, Hinzey A, Sliman S, Kotha SR, Marsh CB, Uppu RM, Parinandi NL. A simple method for effective and safe removal of membrane cholesterol from lipid rafts in vascular endothelial cells: implications in oxidant-mediated lipid signaling. Methods Mol Biol. 2010;610:201–11. https://doi.org/10.1007/978-1-60327-029-8_12.
Tretter EM. Statins, the cholesterol-lowering drugs cause myotoxicity through phospholipase D-mediated lipid signaling in skeletal C2C12 myoblast cells. Honors Research Dissertation for Graduation “With Honors Research Distinction,” The Ohio State University. The Ohio State University Knowledge Bank. 2015. http://hdl.handle.net/1811/86177
Hinzey AH, Kline MA, Kotha SR, Sliman SM, Butler ES, Shelton AB, Gurney TR, Parinandi NL. Choice of cyclodextrin for cellular cholesterol depletion for vascular endothelial cell lipid raft studies: cell membrane alterations, cytoskeletal reorganization and cytotoxicity. Indian J Biochem Biophys. 2012;49(5):329–41.
Okuyama H, Langsjoen PH, Hamazaki T, Ogushi Y, Hama R, Kobayashi T, Uchino H. Statins stimulate atherosclerosis and heart failure: pharmacological mechanisms. Expert Rev Clin Pharmacol. 2015;8(2):189–99. https://doi.org/10.1586/17512433.2015.1011125.
Bockorny B, Dasanu CA. HMG-CoA reductase inhibitors as adjuvant treatment for hematologic malignancies: what is the current evidence? Ann Hematol. 2015;94(1):1–12. https://doi.org/10.1007/s00277-014-2236-4.
Natarajan V, Scribner WM, Morris AJ, Roy S, Vepa S, Yang J, Wadgaonkar R, Reddy SP, Garcia JG, Parinandi NL. Role of p38 MAP kinase in diperoxovanadate-induced phospholipase D activation in endothelial cells. Am J Physiol Lung Cell Mol Physiol. 2001;281(2):L435–49. https://doi.org/10.1152/ajplung.2001.281.2.L435.
Costa RA, Fernandes MP, de Souza-Pinto NC, Vercesi AE. Protective effects of l-carnitine and piracetam against mitochondrial permeability transition and PC3 cell necrosis induced by simvastatin. Eur J Pharmacol. 2013;701(1–3):82–6. https://doi.org/10.1016/j.ejphar.2013.01.001.
Abdoli N, Heidari R, Azarmi Y, Eghbal MA. Mechanisms of the statins cytotoxicity in freshly isolated rat hepatocytes. J Biochem Mol Toxicol. 2013;27(6):287–94. https://doi.org/10.1002/jbt.21485.
Kotamraju S, Williams CL, Kalyanaraman B. Statin-induced breast cancer cell death: role of inducible nitric oxide and arginase-dependent pathways. Cancer Res. 2007;67(15):7386–94. https://doi.org/10.1158/0008-5472.CAN-07-0993.
Kanugula AK, Gollavilli PN, Vasamsetti SB, Karnewar S, Gopoju R, Ummanni R, Kotamraju S. Statin-induced inhibition of breast cancer proliferation and invasion involves attenuation of iron transport: intermediacy of nitric oxide and antioxidant defence mechanisms. FEBS J. 2014;281(16):3719–38. https://doi.org/10.1111/febs.12893.
Abdoli N, Azarmi Y, Eghbal MA. Protective effects of N-acetylcysteine against the statins cytotoxicity in freshly isolated rat hepatocytes. Adv Pharm Bull. 2014;4(3):249–54. https://doi.org/10.5681/apb.2014.036.
Sliman SM, Eubank TD, Kotha SR, Kuppusamy ML, Sherwani SI, Butler ES, Kuppusamy P, Roy S, Marsh CB, Stern DM, Parinandi NL. Hyperglycemic oxoaldehyde, glyoxal, causes barrier dysfunction, cytoskeletal alterations, and inhibition of angiogenesis in vascular endothelial cells: aminoguanidine protection. Mol Cell Biochem. 2010;333(1–2):9–26. https://doi.org/10.1007/s11010-009-0199-x.
Patel RB, Kotha SR, Sauers LA, Malireddy S, Gurney TO, Gupta NN, Elton TS, Magalang UJ, Marsh CB, Haley BE, Parinandi NL. Thiol-redox antioxidants protect against lung vascular endothelial cytoskeletal alterations caused by pulmonary fibrosis inducer, bleomycin: comparison between classical thiol-protectant, N-acetyl-L-cysteine, and novel thiol antioxidant, N,N′-bis-2-mercaptoethyl isophthalamide. Toxicol Mech Methods. 2012;22(5):383–96. https://doi.org/10.3109/15376516.2012.673089.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tretter, E.M. et al. (2022). Role of Bioactive Lipid, Phosphatidic Acid, in Hypercholesterolemia Drug-Induced Myotoxicity: Statin-Induced Phospholipase D (PLD) Lipid Signaling in Skeletal Muscle Cells. In: Parinandi, N.L., Hund, T.J. (eds) Cardiovascular Signaling in Health and Disease. Springer, Cham. https://doi.org/10.1007/978-3-031-08309-9_14
Download citation
DOI: https://doi.org/10.1007/978-3-031-08309-9_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08308-2
Online ISBN: 978-3-031-08309-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)