Abstract
Vitreoretinal lymphoma (VRL) is the most common type of intraocular lymphoma. It is a high-grade B-cell lymphoma, and is often associated with central nervous system lymphoma (CNSL). The hallmark of VRL is the presence of lymphoma cells in the vitreous and retinal and sub-retinal infiltrates. Systemic chemotherapy and radiation therapy have been used for years to treat VRL. In the recent two decades, intra-vitreal chemotherapy as monotherapy or combined with systemic chemotherapy has become a common method for treating VRL. Methotrexate is the most common drug used for intra-vitreal chemotherapy with a very good response, rare intraocular recurrence of the disease (when following the treatment protocol) and acceptable side effects. When CNSL is associated with VRL, systemic chemotherapy is used for the brain disease. Intra-vitreal injections of rituximab have also been used with encouraging results and almost no adverse effects. Limited experience with intra-vitreal injections of other drugs also was found to be effective for the cure of VRL. Other drugs have been experimentally tested in animal models and may be used in the future.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Vitreoretinal lymphoma (VRL), although a rare disease, is the most common type of intraocular lymphoma, and may involve the vitreous, retina, sub-retinal space, retinal pigment epithelium, and the optic nerve. These are high-grade, mostly B-cell malignancies that are associated with a poor prognosis, if the patient also develops central nervous system lymphoma (CNSL) [1]. T-cell VRLs are much less common [2]. Three other groups of intraocular lymphomas involve various parts of the uvea and are usually low-grade B-cell lymphomas [1].
VRL is often associated with CNSL, and is considered by specialists as a subgroup of CNSL [3, 4]. It has been reported that 56–90% of VRL patients ultimately develop CNSL, while 11–25% of patients with CNSL develop VRL [3, 5,6,7,8]. VRL is commonly diagnosed in patients over 50 years of age, although younger patients are also diagnosed. There is no clear sex predilection [3, 4], although in several studies more women were affected than men [9,10,11].
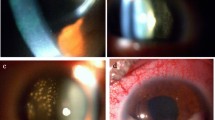
The hallmark of VRL is the presence of cells in the vitreous, mainly in clumps, which is often misdiagnosed as a non-responsive uveitis, along with retinal and sub-retinal infiltrates [12]. These findings may reduce the visual acuity, although often the visual acuity is unexpectedly good.
When VRL is suspected clinically, a diagnostic vitrectomy or vitreous tap is performed. The vitreous samples can be analyzed for the presence of malignant cells by cytopathology with possible immunohistochemical staining or flow cytometry to identify the cell type and monoclonality. Other diagnostic methods are the measurement of the levels of interleukins (IL-10 and IL-6) and the ratio between them, which was found to be a very sensitive test, also in aqueous humor samples from the anterior chamber (AC) of the eye; PCR for detection of immunoglobulin heavy chain (IgH) or T-cell receptor (TCR) gene rearrangement which indicates clonality of malignant cells; and a search for an L265P mutation in the myeloid differentiation primary response gene 88 (MYD88) in diffuse large B-cell lymphoma [3, 8, 13,14,15,16,17].
Since intraocular lymphoma was first recognized in 1951 [18, 19], initially as ocular reticulum cell sarcoma, its treatment has evolved from enucleation [19] through radiation therapy, with or without whole-brain radiotherapy, systemic chemotherapy, intrathecal chemotherapy, intra-vitreal chemotherapy, and biological therapy.
The treatment of VRL aims to eradicate the intraocular disease. For years it has been debated whether treatment of VRL may prevent the development of CNSL, or whether patients with VRL without evidence of CNSL should be treated systemically to prevent CNSL [3]. So far, there have been no randomized clinical trials that can lead to a consensus recommendation that will solve this debate. In their report, the International CNSL Collaborative Group recommended on systemic treatment if the disease involves the CNS and local ocular treatment if the disease involves only the eye, with close follow-up and ongoing collaboration between neuro-oncologists and ophthalmologists [3].
Radiation therapy in doses ranged between 30 and 50 Gy was the gold standard for the treatment of intraocular lymphoma in many institutions. However, because of high recurrence rate and ocular complications, radiation is less often considered nowadays for therapy of VRL [7]. Systemic chemotherapy, mainly with high-dose methotrexate (MTX), sometimes combined with rituximab, which is used for treating CNSL, has also been used for treating VRL. However, the limited penetration of systemic drugs into the vitreous is well known, leading to incomplete response [7]. Direct intra-vitreal injection of drugs, including among others, chemotherapeutic and biological drugs, has become routine in the treatment of various infectious, inflammatory, neovascular, and malignant intraocular disease. Intra-vitreal chemotherapy has become the most common method of treating VRL. In this chapter we review the current status of intraocular chemotherapy for VRL.
2 Intra-vitreal Chemotherapy
Intra-vitreal chemotherapy can be given as primary therapy for VRL, or as adjuvant therapy to other treatment methods, although in recent years the primary intra-vitreal treatment has become the gold standard.
A range of drugs has been used intra-vitreally for treating intraocular malignancies. Already in 1964 Ericson and associates [20] had performed trials of intra-vitreal injections of thiotepa, nitrogen mustard, cyclophosphamide, and methotrexate into rabbits’ eyes, finding no significant intraocular toxicity except in those treated with nitrogen mustard. They even treated several patients with retinoblastoma with intra-vitreal injections of thiotepa. Unfortunately, since then, until the recent two to three decades, there were no further investigations of direct intra-vitreal chemotherapy in treating intraocular malignancies.
In the following paragraphs we will describe the main drugs which are currently used in intra-vitreal injections for treating VRL.
2.1 Intra-vitreal Methotrexate
MTX is currently the most commonly used drug for VRL. It is an anti-metabolite that acts by competitive inhibition of the enzyme dihydrofolate reductase, resulting in reduced thymine synthesis, an essential nuclear base in DNA [21].
Fishburne and associates at the Oregon Health & Science University (OHSU, Portland, Oregon, USA) [21] were the first to report in 1997 on the treatment of VRL in seven eyes of four patients with intra-vitreal injections of 400 μg of MTX, injecting 6–11 injections per eye, in conjunction with systemic chemotherapy delivered by hyper-osmotic blood brain-barrier disruption (BBBD). All patients had complete remission without serious ocular toxic effects.
de Smet and associates [22, 23] from the National Eye Institute at the NIH reported two successful cases of treating recurrent VRL with combined intra-vitreal chemotherapy, one case with intra-vitreal MTX and thiotepa and one case with intra-vitreal MTX and dexamethasone, with a full remission.
de Smet and colleagues tested the pharmacokinetics of a single dose of intraocular injection of MTX in a blind eye of a patient with recurrent VRL by injecting 400 μg. This resulted in concentrations that were lymphocytotoxic for 5 days [22]. Velez and associates [24] investigated the pharmacokinetics and toxicity of several intra-vitreal injections of 400 μg MTX in rabbits’ eyes, together with single injections of fluorouracil and dexamethasone. They found that MTX vitreous levels remain therapeutic (>0.5 μM) in the rabbit eye for 48–72 h without evidence of toxicity.
In 2002 the OHSU group together with the Hadassah Medical Center group, reported a larger series of 26 eyes of 16 human immunodeficiency virus (HIV)-negative patients with VRL from the two centers, treated by intra-vitreal injections of 400 μg MTX in 0.1 mL [25]. Their protocol included three phases: two injections per week for a month as an induction phase; weekly injections for a month in one center and 2 months in the other center as a consolidation phase; and subsequently a maintenance phase of monthly injections to complete a year of treatment. All eyes achieved remission after a maximum of 12 MTX injections (mean of 8.5 injections). Three patients of one center had relapse in the eye, and were treated again using the same intra-vitreal injections protocol with complete remission. Six of the 16 patients died in follow-up as a result of progressive PCNSL, but without clinical ocular involvement.
Frenkel and associates at the Hadassah Medical Center reported a large series of 44 eyes of 26 patients from a single center, who were treated by the same induction-consolidation-maintenance regimen of intra-vitreal MTX injections [9]. This group of patients also included several patients with T-cell lymphoma. (This group included half of the patients reported by Smith et al. [25]). Clinical remission was reached in all eyes after an average of 6.4 injections with 95% of the eyes needing 13 injections or less to be cleared of lymphoma cells. None of the patients had a relapse. All patients in these reports who had CNSL were also treated for the brain disease by systemic chemotherapy. Sou and colleagues [26] reported similar results in one Japanese center.
Some of the patients had decreased visual acuity during the early stages of the treatment, but most of them preserved their vision or had visual improvement. The most common side effects of the intra-vitreal injections are conjunctival hyperemia and transient keratopathy, ranging from diffuse punctate keratopathy to severe epitheliopathy, which usually subside during the maintenance phase [9, 25, 27]. Other complications are acceleration of existing cataract, which could also be due to diagnostic vitrectomy, neovascular glaucoma, which could have occurred because of the VRL itself, and intraocular inflammation that can be successfully treated by corticosteroids [9, 25, 28]. Patients who were treated by BBBD for CNSL may develop maculopathy without significant effect on their visual acuity [25]. None of the patients who were treated by intra-vitreal injections of MTX but were not treated by BBBD developed maculopathy [29].
There have been some differences in the protocols used in various institutions for intra-vitreal MTX monotherapy for treating VRL. Most treating ophthalmologists inject 400 μg in 0.1 mL, as in the first studies. Only a few inject less than 400 μg, and some, like us, reduced the injection volume to 0.05 mL. However, the number of injections varies widely, and some will inject “according to the clinical behavior of the lymphoma” [30], usually with higher relapse rate.
Combined treatment of intra-vitreal injections with systemic chemotherapy, mostly high-dose MTX, has been used in treating VRL [30,31,32,33]. However, there is no evidence that the systemic MTX improves or shortens the time of treatment, or increases the time to relapse and progression of the VRL. In addition, there is no proof that systemic chemotherapy prevents the development of CNSL in VRL patients without CNSL [8, 11]. In our experience and that of others, intra-vitreal MTX injections should be used for treating VRL and systemic chemotherapy for treating CNSL. We recommend avoiding systemic chemotherapy in the treatment of VRL patients when the CNS is not involved. Other combinational treatments for VRL are the use of intra-vitreal MTX and rituximab, sometimes with the addition of systemic chemotherapy or even radiotherapy [34,35,36,37].
2.2 Intra-vitreal Rituximab
Rituximab is a humanized monoclonal antibody that targets CD20-postive B-cells in all stages, from a pre-B-cell through a mature B-cell. Thus, CD20 also presents on lymphomatous B-cells in VRL and CNSL. Rituximab was approved in 1997 by the FDA to be used in B-cell lymphomas of various types. Since the vast majority of VRL and CNSL are B-cell in origin, it makes rituximab an ideal drug for intra-vitreal therapy. Obviously, rituximab is not an appropriate drug when the VRL is of T-cell type. The option of using intra-vitreal injections of rituximab for treating VRL was raised in order to overcome MTX-related side effects, to reduce the initially required frequency of intra-vitreal injections of MTX, and to reduce resistance to MTX therapy.
Some animal studies on intra-vitreal injections of rituximab were performed, and showed its effect on VRL. In all these studies the researchers injected 1 mg/0.1 mL rituximab. Kim and associates [38], investigating the pharmacokinetics of intra-vitreal injections of rituximab into rabbit eyes, found a half-life of 4.7 days in both the aqueous and vitreous. Pulido and colleagues [39] found that rituximab penetrated all retinal layers in rabbit eyes, and Kitzmann and associates [40] showed no toxicity to the rabbit eyes. Mineo and colleagues [41] showed eradication of lymphoma in more than half of the animals and significant inhibition of tumor progression in the rest.
The first reported use of intra-vitreal injection of rituximab for treating VRL was in 2007 by Kitzmann and colleagues [40], who published their experience in treating five eyes of three patients. They used 3–4 injections of 1 mg/0.1 mL rituximab with a good response, no toxicity and no evidence of recurrence after a short median follow-up of 3.6 months. Ohguro and associates [42] treated two patients who had VRL relapse after intra-vitreal MTX by 4 weekly injections of 1 mg/0.1 mL rituximab with complete remission and no recurrence after 2 months.
Hoshida and associates [43] reported their experience in treating 20 eyes of 13 patients who had discontinued previous intra-vitreal MTX treatment because of severe corneal epitheliopathy. They used 4 weekly injections of 1 mg/mL rituximab as one-course protocol, and additional injections were administered when VRL recurred in 11 of the eyes. All patients completed 1 year follow-up. Twelve eyes showed transient intraocular pressure elevation. No other significant side effects developed.
In 2014 Larkin and associates [44] presented what is still the largest series of intra-vitreal rituximab-based treatment for treating VRL, including 48 eyes of 34 patients in clinics in five countries. The eyes were treated with a median of 3.5 injections; the most common interval was monthly. About two-third of the eyes were also injected with MTX, usually on the same day with rituximab. Others were treated with more extensive cytotoxic therapies. Complete remission was achieved in 65% of the eyes and 23% showed partial remission. Among eyes that were treated only by intraocular chemotherapy, 53% experienced complete remission and 11 partial remission. After a median follow-up of 18 months, VRL recurred in 23% of the eyes. The main complication in this series was cataract in 19% of eyes.
The use of intra-vitreal rituximab for VRL was also reported in other small series and case reports. It was used mainly as a secondary treatment [45,46,47] or in combination with other drugs, mainly MTX [34,35,36,37]. There is still no significant series of eyes with VRL treated by rituximab alone as primary treatment. Such a study should be considered.
2.3 Other Drugs for Intra-vitreal Chemotherapy
The experience with using drugs other than MTX and rituximab for the treatment of VRL is very limited.
Intra-vitreal injections of melphalan have been often used in recent years for treating retinoblastoma. Melphalan is a phenylalanine derivative of nitrogen mustard and an alkylating agent. Shields and associates [48] reported in 2017 their experience in treating three eyes of two patients with VRL by intra-vitreal injections of 10 μg/0.1 mL melphalan. One of the patients with bilateral VRL showed clinical remission within 3 weeks after a single injection. Recurrence in one of the eyes was treated by additional 6 bimonthly injections with a good response and no recurrence after 19 months of follow-up. The other patient with bilateral VRL was treated by intra-vitreal melphalan in one eye and MTX in the other eye. The VRL in the eye treated with melphalan was cured by one injection. No toxicity was observed. This group expanded their use of melphalan and reported on 12 more patients with encouraging results [49]. Damato and associates [50] reported their good experience in treating one patient with VRL by intra-vitreal melphalan.
Thiotepa is an organophosphorus alkylating agent, which results in crosslinking of the double-stranded DNA helix and interferes with DNA replication. Ericson and associates reported their results of using intra-vitreal thiotepa injections for treating intraocular malignancies in rabbits’ eyes already in 1964 [20], finding no significant toxicity. de Smet and associates [22, 23] combined thiotepa (2 mg/0.1 mL) with MTX injections in treating a patient with VRL. However, the thiotepa injection was associated with elevated intraocular pressure and loss of vision. In light of the good results with intra-vitreal MTX alone, thiotepa is no longer being used.
Corticosteroids have lymphotoxic effect; however, the response is usually partial. Thus, corticosteroids are not used as a single agent for treating lymphoma. de Smet used a combination of MTX and dexamethasone in treating one patient with VRL resulting in full remission. Castellino and associates reported the use of intra-vitreal corticosteroids injections with other systemic and intra-vitreal drugs [47]. However, intra-vitreal injections of corticosteroids did not become part of the standard practice in treating VRL.
2.4 Investigational Drugs for Intra-vitreal Injections
During the recent two decades researchers reported their experience using various experimental drugs for intra-vitreal or intra-cameral injections in animal models of VRL. However, none of them have matured for clinical use.
Gregory and associates [51] studied the use of membrane FasL vesicles, the membrane-only form of Fas ligand, to activate innate immunity and terminate the immune privilege of the eye. By a single injection of membrane FasL vesicles into the anterior chamber of mice, they eliminated the lymphoma cells that were previously injected into this site.
Li and associates [52] used recombinant immunotoxin HA22 targeting human B-cell lymphoma in a mouse model of intraocular lymphoma. A single intra-vitreal injection of immunotoxin HA22 resulted in complete regression of the lymphoma, demonstrating B-cell-specific immunotoxin therapy.
Ublituximab is a glycoengineered anti-human-CD20 monoclonal antibody that was developed for treating multiple sclerosis. In 2013 Ben-Abdelwahed and associates [53] reported their results in treating the murine model of VRL by a single intra-vitreal injection of ublituximab with marked effect against the lymphoma B-cells expressing CD20.
Some other monoclonal antibodies such as daclizumab, efalizumab, and alemtuzumab showed positive results in animal models, and have the potential to be a useful adjuvant therapy for intraocular lymphoma [54]. However, as with previous experimental drugs, no further reports are available on their use in treating VRL.
3 Summary
Since intraocular lymphoma was first recognized about 70 years ago, its treatment has gradually evolved. Enucleation was often performed in the early years, when the disease was diagnosed late. When VRL was more frequently diagnosed, and its common association with CNSL was recognized, other methods of treatments have been used, including radiation therapy, systemic chemotherapy using various drugs, or in combination. Because of the limited penetration of drugs administered systemically into the eye and their systemic toxicity, and the local side effects of radiation to the eye, direct intra-vitreal chemotherapy has gained popularity and became a common method of treating VRL in the last two decades.
Intra-vitreal injections of MTX as monotherapy was found to be very effective in inducing intraocular tumor remission with acceptable side effects and rare occurrence of relapse. Additional systemic chemotherapy probably does not add to the cure rate of the VRL, and should be used only when CNS lymphoma is associated with the VRL.
In recent years the use of intra-vitreal injections of rituximab has been carried out in several centers, with or without combining MTX, with encouraging results and no significant adverse effects. However, its use varies markedly among experts and the results are still inferior to MTX. Intra-vitreal injection of melphalan was also proved to be an effective drug, but at this time has been employed only in one ocular oncology center.
Because of the rarity of VRL, international collaboration is needed for defining the role of intra-vitreal chemotherapy in eradicating this disease. The present drugs which are used clinically are effective, and probably a consensus on protocols of using them is needed. It seems that in the future the treatment of VRL will continue to evolve, new drugs will be introduced and new methods of intraocular delivery will be developed.
References
Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Exp Ophthalomol. 2008;36:564–78.
Chaput F, Amer R, Baglivo E, Touitou V, Kozyreff A, Bron D, Bodaghi B, Lettoang P, Bergstrom C, Grossniklaus HE, Chan CC, Pe’er J, Caspers LE. Intraocular T-cell lymphoma; clinical presentation diagnosis, treatment and outcome. Ocul Immunol Inflamm. 2017;25:644–53.
Chan CC, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, Cassoux N, Touitou V, Smith JR, Batchelor TT, Pulido JS. Primary vitreoretinal lymphoma: a report from an international primary central nervous system lymphoma collaborative group symposium. Oncologist. 2011;16:1589–99.
Kvopka M, Lake SR, Smith JR. Intraocular chemotherapy for vitreoretinal lymphoma: a review. Clin Exp Ophthalmol. 2020;48:240–8.
Hochberg FH, Miller DC. Primary central nervous system lymphoma. J Neurosurg. 1988;68:835–53.
Farall AL, Smith JR. Eye involvement in primary central nervous system lymphoma. Surv Ophthalmol. 2020;65:548–61.
Pe’er J, Hochberg FH, Foster CS. Clinical review: treatment of vitreoretinal lymphoma. Ocul Immunol Inflamm. 2009;17:290–306.
Grimm SA, Pulido JS, Jahnke K, et al. Primary intraocular lymphoma: an international primary central nervous system lymphoma collaborative group report. Ann Oncol. 2007;18:1851–5.
Frenkel S, Hendler K, Siegal T, Shalom E, Pe’er J. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol. 2008;92:383–8.
Kimura K, Usui Y, Goto H, for Japanese Intraocular Lymphoma Study Group. Clinical features and diagnostic significance of the intraocular fluid of 217 patients with intraocular lymphoma. Jpn J Ophthalmol. 2012;56:383–9.
Riemens A, Bromberg J, Touitou V, et al. Treatment strategies in primary vitreoretinal lymphoma. A 17-center European colaborative study. JAMA Ophthalmol. 2015;133:191–7.
Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol. 2004;242:901–13.
Fend F, Ferreri AJ, Coupland SE. How we diagnose and treat vitreoretinal lymphoma. Br J Haematol. 2016;173:680–92.
Chan CC, Sen HN. Current concepts in diagnosing and managing primary vitreoretinal (intraocular) lymphoma. Discov Med. 2013;15:93–100.
Reichstein D. Primary vitreoretinal lymphoma: an update on pathogenesis, diagnosis and treatment. Curr Opin Ophthalmol. 2016;27:177–84.
Frenkel S, Pe’er J, Kaufman R, Maly B, Habot-Wilner Z. The importance of cytokines analysis in the diagnosis of vitreoretinal lymphoma. Acta Ophthalmol. 2020;98:e668–78.
Carbonell D, Mahajan S, Chee SP, et al. Consensus recommendations for the diagnosis of vitreoretinal lymphoma. Ocul Immunol Inflamm. 2021;29(3):507–20.
Cooper EL, Riker JL. Malignant lymphoma of the uveal tract. Am J Ophthalmol. 1951;34:1153–8.
Vogel MH, Font RL, Zimmerman LE, Levine RA. Reticulum cell sarcoma of the retina and uvea. Report of six cases and review of the literature. Am J Ophthalmol. 1968;66:2005–15.
Ericson L, Karlberg B, Rosengren BH. Trials of intravitreal injections of chemotherapeutic agents in rabbits. Acta Ophthalmol. 1964;42:721–6.
Canellos GP, Lister TA, Skarin AT. Chemotherapy of the non-Hodgkin’s lymphomas. Cancer. 1978;42(2 Suppl):932–40.
de Smet MD, Vancs VS, Kohler D, Solomon D, Chan CC. Intravitreal chemotherapy for the treatment of recurrent intraocular lymphoma. Br J Ophthalmol. 1999;83:448–51.
de Smet MD. Management of non-Hodgkin’s intraocular lymphoma with intravitreal methotrexate. Bull Soc Belg Ophthalmol. 2001;279:91–5.
Velez G, Yuan P, Sung BC, Tansey G, Reed GF, Chan CC, Nussenblatt RB, Robinson MR. Pharmacokinetics and toxicity of intravitreal chemotherapy for primary intraocular lymphoma. Arch Ophthalmol. 2001;119:1518–24.
Smith JR, Rosenbaum JT, Wilson DJ, Doolittle ND, Siegal T, Neuwelt EA, Pe’er J. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002;109:1709–16.
Sou R, Ohguro N, Maeda T, Sainshin Y, Tano Y. Treatment of primary intraocular lymphoma with intravitreal methotrexate. Jpn J Ophthalmol. 2008;52:167–74.
Jeong Y, Ryu JS, Park UC, Oh JY. Corneal epithelial toxicity after intravitreal methotrexate injection for vitreoretinal lymphoma: clinical and in-vitro studies. J Clin Med. 2020;18:2672.
Goldberg S, Frenkel S, Blumenthal EZ, Solomon A, Pe’er J. Intraocular lymphoma. Ophthalmology. 2007;114:1236–7.
Vicuna-Kojchen J, Frenkel S, Siegal T, Shalom E, Chowers I, Pe’er J. Maculopathy in patients with CNS lymphoma treated with chemotherapy in conjunction with blood brain barrier disruption. Br J Ophthalmol. 2008;92:231–5.
Klimova A, Heissigerawa J, Rihova E, Brichova M, Pytlik R, Spicka I, Mrazova K, Karolova J, Svozilkova P. Combined treatment of primary vitreoretinal lymphoma significantly prolongs the time to first relapse. Br J Ophthalmol. 2018;102:1579–85.
Akiyama H, Takase H, Kubo F, Miki T, Yamamoto M, Tomita M, Mochizuki M, Miura O, Arai A. High-dose methotrexate following intravitreal methotrexate administration in preventing central nervous system involvement of primary intraocular lymphoma. Cancer Sci. 2016;107:1458–64.
Ma WL, Hou HA, Hsu YJ, Chen YK, Tang JL, Tsay W, Yeh PT, Yang CM, Lin CP, Tien HF. Clinical outcome of primary intraocular lymphoma patients treated with front-line systemic high-dose methotrexate and intravitreal methotrexate injection. Ann Hematol. 2016;95:593–601.
Kaburaki T, Taoka K, Matsuda J, Yamashita H, Matsuda I, Tsuji H, Tanaka R, Nakazaki K, Nakamura F, Kamiya K, Kurokawa M, Ohtomo K, Aihara M. Combined intravitreal methotrexate and immunochemotherapy followed by reduced-dose whole-brain radiotherapy for newly diagnosed B-cell primary intraocular lymphoma. Br J Haematol. 2017;179:246–55.
Abu Samra K, Oray M, Ebrahimiadib N, Lee S, Anesi S, Foster CS. Intraocular lymphoma: descriptive data of 26 patients including clinico-pathologic features, vitreous finding, and treatment outcome. Ocul Immunol Inflamm. 2018;26:347–52.
Pulido JS, Johnston PB, Nowakowski GS, Castellino A, Raja H. The diagnosis and treatment of primary vitreoretinal lymphoma: a review. Int J Retina Vitreous. 2018;4:18.
Castellino A, Pulido JS, Johnston PB, Ristow KM, Bennani NN, Inwards DJ, Macon WR, Michallef IN, King RL, Salomao DR, Witzig TE, Habermann TM, Nowakowski GS. Role of systemic high-dose methotrexate and combined approaches in the management of vitreoretinal lymphoma: a single center experience 1990-2018. Am J Hematol. 2019;94:291–8.
Giuffre C, Cicinelli MV, Marchese A, Modorati GM, Brambati M, Ferreri AJM, Calimeri T, Ponzoni M, Bandello F, Miserocchi E. Clinical experience in a large cohort of patients with vitreoretinal lymphoma in a single center. Ocul Immunol Inflamm. 2020;26:1–7.
Kim H, Csaky KG, Chan CC, et al. The pharmacokinetics of rituximab following an intravitreal injection. Exp Eye Res. 2006;82:760–6.
Pulido JS, Bakri SJ, Valyi-Nagy T, Shukla D. Rituximab penetrates full-thickness retina in contrast to tissue plasminogen activator control. Retina. 2007;27:1071–3.
Kitzmann AS, Pulido JS, Mohney BG, Baratz KH, Grube T, Marler RJ, Donaldson MJ, O’Neill BP, Johnston PB, Johnson KM, Dixon LE, Salomao DR, Cameron JD. Intraocular use of rituximab. Eye. 2007;21:1524–7.
Mineo JF, Scheffer A, Karkoutly C, Nouvel L, Kerdraon O, Trauet J, Bordron A, Dessaint JP, Labalette M, Berthou C, Labalette P. Using human CD20-transfected murine lymphomatous B cells to evaluate the efficacy of intravitreal and intracerebral rituximab injections in mice. Invest Ophthalmol Vis Sci. 2008;49:4738–45.
Ohguro N, Hashida N, Tano Y. Effect of intravitreous rituximab injections in patients with recurrent ocular lesions associated with central nervous system lymphoma. Arch Ophthalmol. 2008;126:1002–3.
Hashida N, Ohguro N, Nishida K. Efficacy and complications of intravitreal rituximab injection for treating primary vitreoretinal lymphoma. Transl Vis Sci Technol. 2012;98:99–103.
Larkin KL, Saboo US, Comer GM, et al. Use of intravitreal rituximab for treatment of vitreoretinal lymphoma. Br J Ophthalmol. 2014;98:99–103.
Echegaray JJ, Llop S, Sepulveda M, Velez-Rosario R, Perez N, Oliver AL. Intravitreal rituximab for the treatment of secondary intraocular relapse of a large B-cell lymphoma. Am J Ophthalmol Case Rep. 2018;9:77–9.
Fernandez-Canabate E, Fernandez-Canabate S. Intravitreal rituximab for the treatment of intraocular relapse of non-Hodgkin’s lymphoma. Farm Hosp. 2018;42:20–1.
Cicinelli MV, Marchese A, Miserocchi E, Giuffre C, Berchicci L, Querques G, Bandello F, Modaroti GM. Retinal and choroidal changes of vitreoretinal lymphoma from active remission phase after intravitreal rituximab. Ocul Immunol Inflamm. 2020;28:637–46.
Shields CL, Sioufi K, Masheyeki A, Shields JA. Intravitreal Melphalan for treatment of primary vitreoretinal lymphoma: a new indication for an old drug. JAMA Ophthalmol. 2017;135:815–8.
Dalvin LA, Lim LAS, Ancona-Lezama D, Mozloumi M, Chang M, Mashayekhi A, Shields CL. Tumor control and visual acuity outcomes in vitreoretinal lymphoma with and without sub–retinal pigment epithelium infiltration. Ophthalmol Retina. 2019;3:998–1005.
Damato B, Bever GJ, Kim DJ, Afshar AR, Rubenstein JL. An audit of retinal lymphoma treatment at the University of California San Francisco. Eye. 2020;34:515–22.
Gregory MS, Koh S, Huang E, Saff RR, Marshak-Rothstein A, Mukai S, Ksander BR. A novel treatment for ocular tumors using membrane FasL vesicles to activate innate immunity and terminate immune privilege. Invest Ophthalmol Vis Sci. 2005;46:2495–502.
Li Z, Mahesh SP, Shen DF, Liu B, Siu WO, Hwang FS, Wang QC, Chan CC, Pastan I, Nussenblatt RB. Eradication of tumor colonization and invasion by a B cell-specific immunotoxin in a murine model for human primary intraocular lymphoma. Cancer Res. 2006;66:10586–93.
Ben-Abdelwahed R, Donnou S, Ouakrim H, et al. Preclinical study of Ublituximab, a glycoengineered anti-human CD20 antibody, in morine models of primary cerebral and intraocular B-cell lymphomas. Invest Ophthalmol Vis Sci. 2013;54:3657–65.
Rodrigues EB, Farah ME, Maia M, et al. Therapeutic monoclonal antibodies in ophthalmology. Prog Retin Eye Res. 2009;28:117–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pe’er, J., Frenkel, S. (2022). Intra-vitreal Chemotherapy for Vitreoretinal Lymphoma. In: Chawla, B.V., Aronow, M.E. (eds) Global Perspectives in Ocular Oncology. Springer, Cham. https://doi.org/10.1007/978-3-031-08250-4_16
Download citation
DOI: https://doi.org/10.1007/978-3-031-08250-4_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08249-8
Online ISBN: 978-3-031-08250-4
eBook Packages: MedicineMedicine (R0)