Abstract
One of the most important and crucial aspects of leprosy control and elimination has been early diagnosis and treatment. Although we have been able to eradicate leprosy as a public health issue in many countries around the globe, its prevalence or new case diagnosis rate has not decreased significantly in the endemic countries over the last 15 years. The transmission of the disease and delayed detection of cases leading to deformities and even transmission are the major deterrents in our efforts to eradicate leprosy. Clinical criteria and slit skin smear (SSS) are the commonly used diagnostic modalities for leprosy. However, SSS is not practiced in most of the places due to increased risk of HIV/HBV/HCV and lack of expertise; hence, the diagnosis is based on clinical criteria only, which may miss some cases like polar lepromatous leprosy or pure neural leprosy. Extensive research has been carried out in the past to develop different serological and molecular assays for the diagnosis of leprosy. PGL-1 and LID-1 proteins are useful in serological testing; however, they have shown poor sensitivity in detection of paucibacillary and pure neuritic leprosy. The molecular-based approaches such as polymerase chain reaction (PCR) and real-time PCR are promising techniques for the diagnosis of leprosy because of higher sensitivity and specificity, but they are not feasible for use in the field settings due to requirement of equipment, setup, and expertise. We are still far from getting a rapid, easy point-of-care test for the diagnosis of leprosy as none of these diagnostic tests described are recommended by WHO for use in diagnosis of cases and contacts. Combination of both serological and molecular techniques will improve the leprosy diagnostics and will be helpful in diagnosis as well as monitoring the response to treatment as well.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Overview
Mycobacterium leprae (M. leprae) is the causative agent of leprosy, a chronic infectious disease with dermato-neurological and incapacitating symptoms. Despite various global initiatives to eradicate this disease, countries like India, Bangladesh, and Brazil still have high annual new case detection rates and it remains a public health issue. In this regard, WHO has designated the reduction of new cases as a priority in its global strategy, emphasising the importance of early detection, which seeks to minimise disease transmission in the population by early diagnosis of the suspicious case and contacts [1]. It is thought that a large number of people might have subclinical infection which self-heals with only minor symptoms. However, if untreated, leprosy may lead to a stage where it causes permanent nerve damage, including severe sensory and motor nerve loss, deformity, and blindness. It is already confirmed that sooner a leprosy patient is diagnosed and treated, the higher their chances of recovery. Identifying leprosy patients based on antigen-specific responses, ideally before the onset of symptoms, may seem to have a significant impact on clinical outcome [2].
Clinical criteria and slit skin smear (SSS) are the commonly used diagnostic modalities for leprosy. However, SSS is not being done in most of the places and in the field; hence, the diagnosis is based on clinical criteria only, which may miss some cases like polar lepromatous leprosy, histoid leprosy, and pure neural leprosy [3].
Early diagnosis and treatment have been the central tenets of leprosy control programmes. Early diagnosis is defined as diagnosis and start of treatment before onset of nerve impairment. Diagnosis of M. leprae at initial stages and early start of its treatment is essential not only for cure and prevention of deformities, but it may also prove useful in checking the transmission by earlier detection of multibacillary cases, but we need better diagnostic tests which could help in detecting leprosy cases that are missed by the clinical examination and slit skin smear examination.
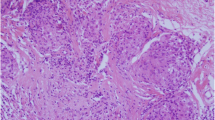
Diagnosis of Leprosy
The detection of leprosy depends on existence of at least one of the three cardinal signs which include presence of skin lesions (that can vary widely in colour, appearance, and form) and existence of thickened or swollen peripheral nerves accompanied with varying degree of sensory loss, muscle weakness, and presence of acid-fast bacilli in the skin [4].
Detection of AFB in scraping of the skin is one of the cardinal signs for diagnosis of leprosy, and slit skin smear (SSS) has been one of the standard and most commonly used techniques, which has been discontinued over the last few years. It needs to be reintroduced in the leprosy control programmes as it is not only helpful in early diagnosis of multibacillary cases of leprosy, but it also helps in assessing the response to treatment and stratification of cases as far as the risk of reactions and deformities is concerned.
Slit skin smears and histopathology of the skin are useful diagnostic modalities, but they also have their limitation for diagnosis as well as large-scale implementation in the leprosy control programmes. There is an urgent need for diagnostics (tests) that are inexpensive, specific, user-friendly, fast, accurate, and simple to deliver to end users. Broad surveys to determine the prevalence of leprosy in a given region would also benefit from such studies. Over the last few years, there has been a lot of research on the genomic structure and immune-pathogenesis of leprosy, and this has led to discovery of some useful antigens and techniques which are helpful in the diagnosis of leprosy.
The diagnostic tests used in leprosy can be broadly classified as bacterial tests which identify the bacillus in the samples like the SSS or the molecular tests like PCR or RT-PCR and the immunological tests which pick up the tissue or the immune response to the bacilli like serological tests against various leprosy antigens (PGL-1, LID-1).
Serological Investigations
Different mycobacterial antigens have been studied for the serological assays, and the basic principle is to study the antibodies directed against the antigen by using techniques like ELISA, agglutination, and lateral flow tests. Immunochromatographic lateral flow assay, detecting IgM antibodies against PGL-I and IgG antibodies to LID-1, is being developed as a point-of-care test for diagnosis of leprosy. We will be discussing some of the antigens which have been studied and have shown promise to be used for the diagnosis of leprosy (Table 5.1).
Phenolic Glycolipid-1 (PGL-1)
Phenolic glycolipid-1 (PGL-1) is an immunodominant antigen which induces a strong humoral immune response, mainly immunoglobulin M (IgM) which is measured using ELISA [5]. Brennan and Barrow in 1980 discovered PGL-1, and it was used by Payne et al. for the first time in serological studies in 1982. Identification of anti-PGL-1 antibody through ELISA is directly proportional to bacillary load which helps in classifying the severity of disease and also the response to treatment. During the treatment, decreased titre in anti-PGL-1 antibody is followed by antigen elimination and can correlate with BI [6]. However, PGL-1 antigen can persist in tissues for a long duration of time, even in the absence of live bacilli [7]. Therefore, positive anti PGL-1 titre is not always indicative of progressive disease [8, 9]. Although its performance in PB and pure neural leprosy cases is limited, serum anti-PGL-1 antibody response is a relatively reliable and simple method which is helpful to confirm diagnosis of MB leprosy and has even been used for prediction of type 2 lepra reactions [10,11,12].
35kD Protein
The epitope on the 35kD antigen of M. leprae reacts directly with MLO3-A1 monoclonal antibody [13]. Recent studies revealed that MLO3 shares 82% of its DNA and 90% of its amino acids with M. avium also, another species of mycobacterium [14]. Another specific sequence for 35kD, MLO4, is also used for serological tests. Initially developed as a radioimmunoassay based on competitive inhibition between patient’s serum and I-125-labelled MLO4 [15], this assay eventually standardised as an ELISA using MLO4-labelled horse radish peroxidase [16, 17]. Despite the fact that this 35kD antigen shares certain genes with M. avium, M. kansasii, and M. paratuberculosis, the standardised serodiagnostic assay for leprosy diagnosis was found to be 97.5% precise and 90% sensitive [18]. Later, purified recombinant 35kD (r35kDa) protein was used and found 94.3% specific. The sensitivity for MB and PB cases was 83% and 17%, respectively. The presence of cross-reactive mycobacterial proteins of M. smegmatis in the cloned purified recombinant protein or the presence of subclinical infection in the exposed contacts could explain the low sensitivity of the r35kD antigen assay [19].
M. Leprae Recombinant Proteins and Development of LID-1 and NDO-LID Rapid Test
The sequencing of M. leprae genome provided the opportunity for generation of protein diagnostic candidates, and a new fusion protein was developed by the Infectious Disease Research Institute, Seattle, USA, i.e., leprosy IDRI protein-1 (LID 1), which has expression of ML0405 and ML2331 antigens that have shown good immunogenicity in the serological assays and were considered appropriate alternatives for rapid diagnosis [20]. LID 1 can also be used as a carrier protein for the NDO to yield NDO-LID. Anti-natural octyl disaccharide-leprosy IDRI diagnostic (NDO-LID) is a ready-to-use kit for testing in the field and gives results within 20 min of charging of samples. Using this NDO-LID rapid diagnosis, the sensitivity and accuracy in detecting MB cases were found to be 87% and 96.1% [21].
IgA Antibody-Based Test
Salivary samples are used for the diagnosis of M. leprae using M. leprae-specific IgA antibodies in order to overcome the problem of invasive sampling. Different studies have used assays to measure salivary IgA/IgM antibodies against PGL-1 in patients and contacts and have found good correlation with serum IgM levels and recommend its use as a diagnostic tool for the contacts of leprosy patients [22]. Major problem with the serological assays in diagnosis of leprosy is their poor performance for detection of paucibacillary and pure neuritic leprosy.
Cytokines/Chemokines as Biomarker in Leprosy
During M. leprae infection, T cells get activated and secrete IFN-γ(interferon gamma) which is a pro-inflammatory marker against M. leprae and M. tuberculosis [23]. IFN-γ can be used as a marker for the diagnosis of M. leprae; however, we cannot differentiate between patients who have the disease and those who only have the infection or people who have been treated.
Moreover, immunopathogenicity induced by M. leprae infection activates host immune cells which secrete various effector and regulatory molecules. IL-1β, MIP-1, and MCP-1 can be used to differentiate pathogenic immunological responses existing in mycobacterial disease patients from those induced through asymptomatic M. leprae exposure.
Lastly, M. leprae protein such as ML-2478 in combination with interferon gamma release assay (IGRA) can be used as a novel method for anticipating the extent of M. leprae transmission in a given population and identifying people who are prone to contracting M. leprae infection and acquiring leprosy [24].
Gene-Based Assays
Molecular approaches like polymerase chain reaction (PCR) or real-time (RT)-PCR are routinely used for identification of specific M. leprae DNA sequence in clinical samples. These are highly sensitive assays which can be used for diagnosis of infection in doubtful/difficult cases, for assessing bacterial load, for detection of drug resistance, and for monitoring the response of treatment.
M. Leprae-Specific PCR
M. leprae-specific PCR could be carried out on routine basis in laboratory using DNA isolated from a wide range of biological specimens such as blood, skin smear, saliva, skin biopsy, oral or nasal swab, nerve section, and urine [25,26,27,28]. Detection range of M. leprae using PCR ranges between 10 and 30 fg which is equivalent to 2.8–8.3 bacilli [29]. Few M. leprae-specific PCR genes are RLEP, hsp85, 18 kDa, 36 kDa, 16S rRNA, and sodA (Table 5.2). Among these, the most sensitive and specific gene target-based PCR is M. leprae-specific repetitive element (RLEP) PCR [30]. The sensitivity of PCR is 100% in patients with a positive bacteriological index and lower in case of patients having low or negative bacteriological index.
Multiplex PCR (M-PCR)
M-PCR is a better alternative and sensitive type of PCR technique in which two or more set of primers are used simultaneously for amplification of different target genes present in the same reaction (Table 5.3). However, selection of primers should be done carefully on the basis of these three parameters:
-
(a)
The primers should have similar annealing temperature.
-
(b)
The primers should not be complementary to each other.
-
(c)
The size of the amplicon from each primer pair must be different so that they can be easily visualised as distinct bands by gel electrophoresis.
In M. leprae clinical diagnosis, M-PCR employs more than one specific gene to its DNA. This technique is used for the detection of paucibacillary forms or indeterminate leprosy by targeting pseudo genes of M. leprae such as ML1545, ML2180, and ML2179 with the positive detection range of 75.61% [31]. In case of PB patients, the positivity rate of M-PCR has been increased from 22.2% (conventional PCR) to 80.3% [32]. Different types of clinical samples can be used like blood, nasal swab, saliva, and SSS for the detection of PB and MB cases with the help of M-PCR using RLEP, 16S rRNA, and sodA targets [33] (Table 5.4).
After amplification of individual genes, products are electrophoresed using 2% agarose gel, whereas M-PCR-amplified gene products are electrophoresed using 4% agarose gel. The products are viewed using a gel documentation system. M-PCR using multiple gene targets improves the identification of M. leprae DNA with respect to sensitivity and specificity.
In Silico Molecular Techniques
In silico molecular techniques for drug resistance are used for the patients who are not responding to MDT. Resistance to anti-leprosy medicines like dapsone, rifampicin, and fluoroquinolones has been detected using molecular-based techniques to find mutation in drug resistance-determining regions (DRDR). Rifampicin resistance is associated with mutation in rpoB gene sequencing coding β-subunit of RNA polymerase, dapsone resistance is associated with mutation within the folP1 sequence coding the dihydropteroate synthase (DDS), and ofloxacin resistance is associated with mutation within the gyrA sequence coding the subunit A of DNA gyrase [34]. To perform PCR for drug resistance, skin biopsy or SSS from the patient is preserved in 70% ethanol and sent to the laboratory to check mutation by gene sequencing in respective DRDR.
Loop-Mediated Isothermal Amplification (LAMP) Assay
It is a DNA amplification method that has been used to develop assays for various diseases like tuberculosis, nontuberculous mycobacteria, and COVID-19. Notomi et al. first devised this novel isothermal amplification method to amplify a limited amount of DNA copies into a million copies within an hour [35]. It utilises a set of four (or six) different primers which bind to six (or eight) different regions on the target gene making it highly specific. The end result or a positive test can be assessed easily by observing a change in turbidity or colour of the reaction with the naked eye or by using a turbidimeter or colorimeter or even a smartphone-based application for reading the colour or turbidity. It is an ideal assay for resource-constrained facilities due to minimal hardware requirements. The results can be read within an hour from the sample and the visualisation of the results is by seeing the change in colour of the analyte. Different primers have been used for the diagnosis of leprosy, a recent study by Jiang et.al developed a LAMP assay targeting the M. leprae RLEP gene and were of the opinion that the high sensitivity and rapidity of the LAMP assay, together with its ability to readily identify the M. leprae subspecies through naked eye evaluation, make it an attractive tool for routine diagnostics [36].
According to a recent meta-analysis of all leprosy diagnostic tests, agglutination tests had the highest sensitivity of the three serological tests studied (ELISA, agglutination test, and lateral flow), and all had comparable specificity. Among molecular analysis, qPCR had better sensitivity but lower specificity than traditional PCR. The PCR method was significantly more reliable than ELISA. However, the authors concluded that the findings among studies differed greatly, so they cannot suggest these tests for detection of leprosy patients due to heterogeneity in variation, thresholds, antigens targeted, and concerns about study aspect [37].
Conclusion
Early detection and management of M. leprae is the need of the hour if we want to check the transmission of leprosy and fulfil our dream of a leprosy-free world. We need more robust tests that can be used in the field to screen and diagnose leprosy patients and their contacts and maybe which can help us to classify the patients into paucibacillary and multibacillary so that adequate treatment can be given to those diagnosed with leprosy. A combination of serological and molecular testing may prove to be useful and better and help to eradicate leprosy from society in order to have a leprosy-free world.
References
WHO. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO
Kumar B, Dogra S. Leprosy: a disease with diagnostic and management challenges! Indian J Dermatol Venereol Leprol. 2009;75:111–5.
Martinez AN, Talhari C, Moraes MO, Talhari S. PCR-based techniques for leprosy diagnosis: from the laboratory to the clinic. PLoS Negl Trop Dis [Internet]. 2014;8(4):e2655. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983108/.
Leprosy WEC on, Organization WH. WHO expert committee on leprosy: eighth report. World Health Organization; 2012. https://apps.who.int/iris/handle/10665/75151.
Brennan PJ, Barrow WW. Evidence for species-specific lipid antigens in mycobacterium leprae. Int J Lepr Mycobact Dis Off Organ Int Lepr Assoc. 1980;48:382–7.
Chin-a-Lien RA, Faber WR, van Rens MM, Leiker DL, Naafs B, Klatser PR. Follow-up of multibacillary leprosy patients using a phenolic glycolipid-I-based ELISA. Do increasing ELISA-values after discontinuation of treatment indicate relapse? Lepr Rev. 1992;63:21–7.
Meeker HC, Schuller-Levis G, Fusco F, Giardina-Becket MA, Sersen E, Levis WR. Sequential monitoring of leprosy patients with serum antibody levels to phenolic glycolipid-I, a synthetic analog of phenolic glycolipid-I, and mycobacterial lipoarabinomannan. Int J Lepr Mycobact Dis Off Organ Int Lepr Assoc. 1990;58:503–11.
Cunanan A, Chan GP, Douglas JT. Risk of development of leprosy among Culion contacts. Int J Lepr Mycobact Dis. 1998;66:S78A.
Fujiwara T, Hunter SW, Cho SN, Aspinall GO, Brennan PJ. Chemical synthesis and serology of disaccharides and trisaccharides of phenolic glycolipid antigens from the leprosy bacillus and preparation of a disaccharide protein conjugate for serodiagnosis of leprosy. Infect Immun. 1984;43(1):245–52.
Fine PE, Ponnighaus JM, Burgess P, Clarkson JA, Draper CC. Seroepidemiological studies of leprosy in northern Malawi based on an enzyme-linked immunosorbent assay using synthetic glycoconjugate antigen. Int J Lepr Mycobact Dis Off Organ Int Lepr Assoc. 1988;56(2):243–54.
Contin LA, Alves CJM, Fogagnolo L, Nassif PW, Barreto JA, Lauris JRP, et al. Use of the ML-flow test as a tool in classifying and treating leprosy. An Bras Dermatol. 2011;86(1):91–5.
Cardona-Castro N, Beltrán-Alzate JC, Manrique-Hernández R. Survey to identify mycobacterium leprae-infected household contacts of patients from prevalent regions of leprosy in Colombia. Mem Inst Oswaldo Cruz. 2008;103:332–6.
Mohagheghpour N, Munn MW, Gelber RH, Engleman EG. Identification of an immunostimulating protein from mycobacterium leprae. Infect Immun. 1990;58:703–10.
Triccas JA, Winter N, Roche PW, Gilpin A, Kendrick KE, Britton WJ. Molecular and immunological analyses of the Mycobacterium avium homolog of the immunodominant mycobacterium leprae 35-kilodalton protein. Infect Immun. 1998;66:2684–90.
Sinha S, Sengupta U, Ramu G, Ivanyi J. A serological test for leprosy based on competitive inhibition of monoclonal antibody binding to the MY2a determinant of mycobacterium leprae. Trans R Soc Trop Med Hyg. 1983;77:869–71.
Mwatha J, Moreno C, Sengupta U, Sinha S, Ivanyi J. A comparative evaluation of serological assays for lepromatous leprosy. Lepr Rev. 1988;59:195–9.
Sinha S, Sengupta U, Ramu G, Ivanyi J. Serological survey of leprosy and control subjects by a monoclonal antibody-based immunoassay. Int J Lepr Mycobact Dis Off Organ Int Lepr Assoc. 1985;53:33–8.
Triccas JA, Roche PW, Britton WJ. Specific serological diagnosis of leprosy with a recombinant mycobacterium leprae protein purified from a rapidly growing mycobacterial host. J Clin Microbiol. 1998;36(8):2363–5.
Roche PW, Failbus SS, Britton WJ, Cole R. Rapid method for diagnosis of leprosy by measurements of antibodies to the M. leprae 35-kDa protein: comparison with PGL-I antibodies detected by ELISA and “dipstick” methods. Int J Lepr Mycobact Dis Off Organ Int Lepr Assoc. 1999;67:279–86.
Duthie MS, Ireton GC, Kanaujia GV, Goto W, Liang H, Bhatia A, et al. Selection of antigens and development of prototype tests for point-of-care leprosy diagnosis. Clin Vaccine Immunol. 2008;15:1590–7.
Douglas JT, Cellona RV, Fajardo TT Jr, Abalos RM, Balagon MV, Klatser PR. Prospective study of serological conversion as a risk factor for development of leprosy among household contacts. ClinDiagn Lab Immunol. 2004;11:897–900.
Cabral PB, Júnior JE, De Macedo AC, Alves AR, Gonçalves TB, TCB C, et al. Anti-PGL1 salivary IgA/IgM, serum IgG/IgM, and nasal mycobacterium leprae DNA in individuals with household contact with leprosy. Int J Infect Dis. 2013;17(11):e1005–10.
Wallis RS, Pai M, Menzies D, Doherty TM, Walzl G, Perkins MD, et al. Biomarkers and diagnostics for tuberculosis: progress, needs, and translation into practice. Lancet Lond Engl. 2010;375(9729):1920–37.
Geluk A, Bobosha K, van der Ploeg-van Schip JJ, Spencer JS, Banu S, Martins MB, et al. New biomarkers with relevance to leprosy diagnosis applicable in areas hyperendemic for leprosy. J Immunol Baltim Md. 2012;188:4782–91.
Santos AR, De Miranda AB, Sarno EN, Suffys PN, Degrave WM. Use of PCR-mediated amplification of mycobacterium leprae DNA in different types of clinical samples for the diagnosis of leprosy. J Med Microbiol. 1993;39:298–304.
de Wit MY, Douglas JT, McFadden J, Klatser PR. Polymerase chain reaction for detection of mycobacterium leprae in nasal swab specimens. J Clin Microbiol. 1993;31:502–6.
Caleffi KR, Hirata RDC, Hirata MH, Caleffi ER, Siqueira VLD, Cardoso RF. Use of the polymerase chain reaction to detect mycobacterium leprae in urine. Braz J Med Biol Res. 2012;45:153–7.
da Rosa FB, de Souza VC, de Almeida TAP, do Nascimento VA, Vásquez FG, da GS CM, et al. Detection of mycobacterium leprae in saliva and the evaluation of oral sensitivity in patients with leprosy. Mem Inst Oswaldo Cruz. 2013;108:572–7.
Bang PD, Suzuki K, Phuong LT, Chu TM, Ishii N, Khang TH. Evaluation of polymerase chain reaction-based detection of mycobacterium leprae for the diagnosis of leprosy. J Dermatol. 2009;36:269–76.
Turankar RP, Pandey S, Lavania M, Singh I, Nigam A, Darlong J, et al. Comparative evaluation of PCR amplification of RLEP, 16S rRNA, rpoT and sod a gene targets for detection of M. leprae DNA from clinical and environmental samples. Int J Mycobacteriol. 2015;4:54–9.
Chaitanya VS, Cuello L, Das M, Sudharsan A, Ganesan P, Kanmani K, et al. Analysis of a novel multiplex polymerase chain reaction assay as a sensitive tool for the diagnosis of indeterminate and tuberculoid forms of leprosy. Int J Mycobacteriol. 2017;6:1–8.
Banerjee S, Sarkar K, Gupta S, Mahapatra PS, Gupta S, Guha S, et al. Multiplex PCR technique could be an alternative approach for early detection of leprosy among close contacts–a pilot study from India. BMC Infect Dis. 2010;10:252.
Pathak VK, Singh I, Turankar RP, Lavania M, Ahuja M, Singh V, et al. Utility of multiplex PCR for early diagnosis and household contact surveillance for leprosy. Diagn Microbiol Infect Dis. 2019;95:114855.
Cambau E, Perani E, Guillemin I, Jamet P, Ji B. Multidrug-resistance to dapsone, rifampicin, and ofloxacin in mycobacterium leprae. Lancet Lond Engl. 1997;349(9045):103–4.
Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, Hase T. Loop-mediated isothermal amplification of DNA. Nucleic Acids. 2000;28:E63.
Jiang H, Tsang L, Wang H, Liu C. Loop-mediated isothermal amplification (LAMP) assay targeting RLEP for detection of mycobacterium leprae in leprosy patients. Int J Infect Dis. 2021;107:145–52.
Gurung P, Gomes CM, Vernal S, Leeflang MMG. Diagnostic accuracy of tests for leprosy: a systematic review and meta-analysis. Clin Microbiol Infect. 2019;25(11):1315–27.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Narang, T., Shilpa (2022). Serological and Molecular Investigations in Leprosy. In: Pradhan, S., Kumar, P. (eds) Clinical Cases in Leprosy. Clinical Cases in Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-031-08220-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-08220-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08219-1
Online ISBN: 978-3-031-08220-7
eBook Packages: MedicineMedicine (R0)