Abstract
Leprosy is an important chronic, infectious disease affecting the peripheral nerves. As it is a treatable disease, it is of paramount importance to detect nerve impairment early in the disease as it can help in the prevention of disability. Electrophysiologic examination of the peripheral nerves is a noninvasive and sensitive method in the early detection of neuropathy. Nerve conduction study can detect the functional derangement of nerves prior to the clinical manifestations of symptoms and signs. Reduction of NCV and worsening of EMG indicate failure of medical treatment and are an indication for surgical intervention. Radiologic examination helps in evaluating the extent of bone involvement and the risks of a pathological fracture in a patient of leprosy. High-resolution ultrasonography is a noninvasive imaging technique that provides accurate morphologic information about peripheral nerves using the improvised spatial and contrast resolution. Vital information on nerve structure, morphology, vascularity, and real-time blood flow in the nerve contributes to the diagnosis and assessment of nerve damage in leprosy. MRI is a sensitive modality which helps in detecting early neuro-arthropathic changes and soft tissue changes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Leprosy is a chronic infectious granulomatous disease caused by Mycobacterium leprae which involves the skin and peripheral nerves [1]. Among peripheral nerve disorders, leprosy is a common treatable disease. Early detection of nerve impairment is very important in the management of leprosy as it can help in the prevention of disability. Very often, there may be a visible (Fig. 4.1) or palpable grossly thickened peripheral nerve with clinical examination itself which is sufficient to analyze the neurological defects. Early nerve involvement often necessitates electrophysiological and imaging studies. Bone and vascular changes are identified only by the imaging workup. This chapter highlights the utility of noninvasive investigations like electrophysiological studies and radiological investigations in the comprehensive management of leprosy.
Electrophysiological Studies
Electrophysiologic examination of the peripheral nerves is a sensitive method in early detection of neuropathy when compared with quantitative thermal sensory, vibrometry, dynamometry, monofilament testing, and voluntary muscle testing. These studies have become useful diagnostic tools in the assessment of nerve function in leprosy. They provide vital information to confirm or alter a clinical diagnosis and can prevent major diagnostic errors.
Nerve Conduction Study (NCS)
Direct involvement of the peripheral nerve is the most important outcome of leprosy. The varied manifestations of nerve damage in leprosy include silent neuropathy, loss of tactile sensations, dryness, muscle weakness, atrophy, or contracture.
NCS involves the recording, display, measurement, and interpretation of action potentials arising from the peripheral nerves. It can detect the functional derangement of nerves before the appearance of clinical signs and symptoms [2]. Detection and early treatment of nerve function impairment (NFI) can reduce disability and deformity. Trained technicians are able to perform these tests at a faster pace with the availability of modern, affordable, and portable electrophysiology machines [3].
Principles
NCS involves application of a depolarizing square wave electrical pulse to the skin over a peripheral nerve, producing (1) a propagated nerve action potential recorded at a distant point over the same nerve and (2) a compound muscle action potential (CMAP) arising from activation of muscle fibers in a target muscle supplied by the nerve [4].
The two methods to stimulate a nerve include skin surface stimulator or a needle placed close to a nerve or a nerve root. Motor studies are performed by electrical stimulation of a nerve and recording the CMAP from surface electrodes overlying a muscle supplied by that nerve [5].
Interpretation
The interpretation of electrophysiological functions of nerve trunks is carried out using distal latency (myelination), amplitude (number of axons), and velocity (myelination).
Latency is the time from stimulus artifact to the onset of the response. In motor nerve studies, this latency includes nerve conduction time and neuromuscular transmission time. Proximal latency starts at the proximal stimulation point and ends at the first deflection from baseline. Distal latency is measured from the distal stimulation point to the first deflection from the baseline.
Amplitude is dependent on the number of axons that conduct impulses from the stimulus point to the muscle, number of functioning motor endplates, and muscle volume. The amplitude is measured from the baseline to the negative peak.
Conduction velocity (CV) is calculated by dividing the length of the nerve segment between the two stimulation points by the difference between the proximal and distal latency [6].
In sensory conduction studies, sensory nerve action potential (SNAP) is obtained by electrically stimulating sensory fibers by using supramaximal stimulus and recording the nerve action potential at a point further along that nerve.
NCS and Leprosy
NCS can detect subclinical leprosy neuropathy, which is helpful for prevention of clinical neuropathies [7].Slowing of sensory velocity and motor nerve conduction velocity (NCV) is observed in patients without any clinical abnormality which represent the preclinical stage of damage. Ramadan et al. in their study found significant reduction in MNCV, prolongation of distal latency, and reduction of amplitude [8]. Amplitude has been found to be the most affected parameter, followed by velocity and latencies by Sunki K et al. in their study [9]. Early involvement of sensory nerves with marked amplitude changes in motor nerves has been reported in leprosy [10].
Electromyography (EMG)
Principles
Electromyography (EMG) studies the electrophysiological activity of resting and contracting skeletal muscle. Detection and recording of the electrical activity from a portion of a muscle by recording of motor unit potentials are accomplished by EMG. The usual method employed followed in the study of leprosy patients is needle EMG.
Muscles selected for the EMG studies should be superficial, easily identified, and should be located away from major vessels and nerve trunks. Abductor pollicis brevis is used for testing the function of the median nerve, abductor digiti minimi for testing the ulnar nerve, and extensor digitorum brevis for testing the lateral popliteal nerve [8]. EMG is performed separately for each muscle to be tested.
Interpretation
The abnormal EMG findings indicating neuropathy include fibrillation, fasciculation, giant motor unit potentials, and incomplete interference or reduced recruitment pattern. DeFaria CR et al. have documented that motor and sensory amplitude reduction was the earliest and the most frequent encountered abnormality among their patients [11].
EMG and Leprosy
Applications of EPS in leprosy [12].
-
1.
Early detection of subclinical neuropathy.
-
2.
Management of neuritis.
Based on EMG and NCV, several guidelines have been listed for indications of surgery in leprosy [13].
-
Recent neuritis: Reduction of NCV and worsening of EMG indicate failure of medical treatment and are an indication for surgical intervention.
Stable NCV/EMG with a clinical background of subclinical neuritis warrants continuation of pharmacotherapy.
-
Long-standing neuritis: Surgery is contraindicated in a patient of leprosy with clinically complete sensory-motor deficits, and EMG/NCV results are abnormal.
-
-
3.
Monitoring the Medical Treatment
-
NCV of a patient shows improvement with treatment.
-
Drug efficacy in leprosy reactions can be monitored using MNCV.
-
-
4.
Detection of Thalidomide-Induced Peripheral Neuropathy: Features of Thalidomide-Induced Neuropathy Include Reduction in SNAP Amplitude and Relative Conservation of NCV [14]
The limitation of EPS is that it does not always allow assessment of the exact location, cause, and extent of a nerve lesion and coexistent disease of surrounding tissues.
Radiologic Examination
Leprosy can involve the bones and soft tissue due to direct invasion or by indirect influence due to neuropathy. It can be detected by ordering suitable radiological interventions. Radiological investigations relevant in leprosy include the conventional radiography of the hands, feet, and face, high-resolution ultrasonography (HRUS), and magnetic resonance imaging (MRI). Objectives of the radiological assessment of leprosy in principle include the conventional radiography for the bone changes, HRUS for the structural nerve changes, and MRI for the soft tissue and neuro-arthropathic changes.
Radiography of the Hands, Feet, and Face
Preliminary radiographs are necessary in assessing the extent of bone involvement and the risks of a pathological fracture in a patient of leprosy. Their utility has been explored more frequently in recent times after the advent of higher-resolution imaging techniques. They are useful in the assessment of the structural changes which generally cannot be assessed by clinical examination.
Hands and Feet
The hands and feet are commonly affected by leprosy especially in lepromatous leprosy and type 1 lepra reaction. Radiological examination (antero-posterior (AP), lateral or oblique skiagrams) of both the hands and feet is necessary to look for the presence of the bone changes, heel infections, and suspected tarsal infections.
Nonspecific changes include bone erosions, absent phalanges (resorption of digits), osteomyelitis (atrophy or trauma), tarsal disintegration, and disuse osteoporotic changes.
Specific changes due to direct infiltration by M. leprae can present with bone cysts or pseudocysts and sequestrate, honeycomb appearance, enlarged nutrient foramina, subarticular erosions, concentric cortical erosions (pencilling or sucked candy appearance), and osteoporosis with lepromatous arthritis [15, 16]. Patients of lepra reactions may show terminal tuft dissolution (juxta-articular decalcification), destruction/erosion of epiphyseal bone, sclerosis, subperiosteal bone erosion, and osteoperiostitis [17].
Face
Atrophy of anterior nasal spine and maxillary alveolar process are the features to look for on radiologic evaluation [18]. Paranasal sinuses are an important reservoir of M. leprae in MB leprosy. CT scan of paranasal sinus studies can reveal localized or diffuse thickening of mucosa and opacity of the sinus [19]. Ethmoid sinuses are most frequently affected, followed by maxillary sinus, while frontal and sphenoid sinuses are least affected. The findings of the study by Kiris A et al. suggest that persistent infection is common among lepromatous leprosy patients, despite previous treatment [20]. Hence, paranasal sinus CT examination is a useful method of evaluating patient response to treatment and follow-up.
High-Resolution Ultrasonography (HRUS)
Principles
HRUS is a noninvasive, cost-effective imaging technique that enables real-time examination of soft tissues in static and dynamic states. It gives significant information on nerve structure, morphology, and vascularity in the nerve, and this adds a new dimension in diagnosing leprosy particularly pure neuritic type and assessment of nerve damage which can prevent disabilities.
Clinical examination of nerves in leprosy is subjective and can be inaccurate. Hence, HRUS can delineate peripheral nerves in the upper and lower with accurate morphologic information using the improvised spatial and contrast resolution. It also helps in the evaluation of both entrapment and peripheral neuropathy.
HRUS with a broadband frequency ranging from 10 to 14 MHz, color Doppler (CD) with broadband frequency of 6–18 MHz, and linear array transducer are utilized for the imaging of peripheral nerves. Settings of color Doppler ultrasound examination are set to detect signals from low flow velocity vessels in the nerves. After B-mode imaging of the nerve, a color box is put over a small part of the nerve in its longitudinal axis. Sequential increase in color gain till color bleed (noise) appears in the color box is performed, and the color gain is kept just lower to this to avoid the noise. The frequency of pulse repetition is set to pick up very low blood flow with avoidance of noise in the image and arterial pulsations. No significant arterial pulsations are detected in normal nerves. The detection of blood flow signals in the perineural plexus or intrafascicular vessels during imaging is taken as a sign of nerve hypervascularity.
Parameters Assessed
-
1.
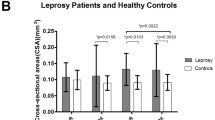
Cross-sectional area (CSA): It is determined from the area within the inner margin of the hyperechoic rim. This helps in assessing peripheral nerve enlargement (Fig. 4.2) [21].
-
2.
Echogenicity: The echo density of the nerves assessed on imaging can be graded as follows: mild, some hypoechogenicity; moderate, obvious hypoechogenicity; and severe, absence of any fascicular pattern. Nerves were classified as abnormal if they showed hypoechoic or hyperechoic areas or focal thickening with loss of the normal fascicular pattern.
-
3.
Size of fascicles: Enlarged fascicles have been reported in patients with leprosy [22].
-
4.
Thickness of the epineurium: HRUS has shown that the epineurium of the ulnar nerve is often strikingly thickened in leprosy patients when involved [23].
-
5.
Vascularization of a peripheral nerve: Increased neural vascularity (Fig. 4.3) with interfascicular edema reflects immune-mediated inflammation in leprosy reactions.
Interpretation
-
(a)
Objective measurement of nerve damage by demonstrating the nerve thickening, altered echotexture, and abnormal vascularity.
-
(b)
Detection of more extensive changes than those diagnosed clinically in nerves with clinical features of impairment of function.
-
(c)
Calculation of the cross-sectional areas of peripheral nerves. HRUS measurement of increased nerve size is a sensitive indicator of the presence of neuropathy in leprosy [24].
-
(d)
Study of the structural changes in nerves that cannot be biopsied especially the mixed nerves due to risk of muscle palsy.
-
(e)
HRUS can examine the nerve for a longer length when compared with MRI which can evaluate only a defined segment [25].
Since ultrasonography is an operator-dependent imaging modality, it requires a high level of expertise. It also requires higher-resolution ultrasound machines with color Doppler settings to assess the nerve diameter and vascularity changes.
Magnetic Resonance Imaging
Principles
MRI is an operator-independent imaging modality. MRI can distinctly delineate a nerve from surrounding soft tissues, precisely visualize nerve fascicles, and clearly localize the site of the pathology. In leprosy, peripheral nerve involvement ranges from nerve thickening with preserved fascicular architecture to disruption of fascicular architecture and formation of micro-abscesses. Large abscesses are formed by coalescence of micro-abscesses which extend into the surrounding soft tissue [25].
Interpretation
MRI findings in leprosy are nonspecific and may show diffuse edema and swelling of the involved nerve. Findings of nodules or nerve sheath granulomas are suggestive of leprosy. Nerve abscesses appear hypointense on T1-weighted images and hyperintense on T2-wighted images and show peripheral enhancement on postcontrast study [26].
MRI is a sensitive modality in ascertaining early neuro-arthropathic changes such as degradation and interruption of the subcutaneous fat and effusion and synovitis of the metatarsophalangeal joints in leprosy patients [27]. MRI is more accurate in detecting soft tissue changes, such as subcutaneous fat infiltration, cellulitis, and abscess [28].
Conclusion
Electrophysiological and radiological investigations are the noninvasive tools that aid in the clinical findings of leprosy. They are useful objective tools in assessing the structural and functional impairments which may alter the course of treatment in leprosy. It could be stated that electrophysiological studies help in demonstrating and detecting the integrity of nerve function in leprosy. They are useful not only in assessing nerve function at the time of diagnosis but also during the follow-up of leprosy patients as a supplement to clinical tests for nerve function assessment. Radiological assessment is recommended in cases of leprosy that clinically predicts early bone changes. HRUS is a noninvasive, cost-effective tool that gives significant information on nerve structure, morphology, vascularity, and real-time blood flow in the nerve, and this information adds a new dimension to the diagnosis of leprosy and assessment of nerve damage which can prevent disabilities. Routine use of HRUS improves the diagnosis of leprosy and assesses extent and severity of nerve involvement. MRI, though not commonly used, is a sensitive tool in assessing the soft tissue changes and early neuroarthropathy. The electrophysiological and radiological studies will help the clinicians to understand the gravity of the damage caused by leprosy and timely institution of therapeutic and preventive interventions. Objective of leprosy treatment is the prevention of permanent loss of function, deformities, and disabilities.
References
Jopling WH, Mcdougall AC. The disease. In: Hand book of leprosy. 5th ed. New Delhi: CBS Publishers and Distributors; 1996. p. 10–53.
Ooi WW, Srinivasan J. Leprosy and the peripheral nerve system: basic and clinical aspects. Muscle Nerve. 2004;30:393–409.
Vasanthy B, Chandrathil VP, Haris AA, George J. Nerve conduction study for early detection of leprosy. Int J Med Health Res. 2018;4:4–8.
Indu Krishnan MU, Sobhanakumari K, Jose P, Amitha NP, Irimpan KJ. High resolution ultrasound, nerve conduction study, and other non-invasive investigations in leprosy. J Skin Sex Transm Dis. 2021;3(2):136–42. https://doi.org/10.25259/JSSTD_1_2021.
Mallik A, Weir AL. Nerve conduction studies: essentials and pitfalls in practice. J Neurol Neurosurg Psychiatry. 2005;76:ii23–31.
Vashisht D, Das AL, Vaishampayan SS, Vashisht S, Joshi R. Nerve conduction studies in early tuberculoid leprosy. Indian Dermatol Online J. 2014;5(Suppl S2):71–5.
Marahatta S, Bhattarai S, Paudel BH. Electrophysiological profiles of leprosy neuropathy. Lepr Rev. 2017;88:373–80.
Ramadan W, Mourad B, Fadel W, Ghoraba E. Clinical, electrophysiological, and immunopathological study of peripheral nerves in Hansen's disease. Lepr Rev. 2001;72(1):35–49.
Sunki K, Koneti BB, Sreerangapuri N, Mounika Y, Pinjala P, Prasad JV. Nerve conduction study: can it diagnose leprosy early? Int J Res Dermatol. 2020;6:161–6.
Samant G, Shetty VP, Uplekar MW, Antia NH. Clinical and electrophysiological evaluation of nerve function impairment, following cessation of multidrug therapy in leprosy. Lepr Rev. 1999;70:10–20.
DeFaria CR, Silva IM. Electromyographic diagnosis of leprosy. Arq Neuropsiquiatr. 1990;48(4):403–13.
Gupta P, Mainra A, Dhanta A. Nerve conduction studies in leprosy a review. IOSR J Dent Med Sci. 2018;17:27–32.
Carayon A, Rigal J. Value of electrophysiological investigation for therapeutic indications in leprous neuritis. Med Trop(Mars). 1972;32:9–21.
Sheskin J, Magora A, Sagher F. Motor conduction velocity studies in patients with leprosy reaction treated with thalidomide and other drugs. Int J Lepr. 1969;37:359–64.
Thappa DM, Sharma VK, Kaur S, Suri S. Radiological changes in hands and feet in disabled leprosy patients: a clinicoradiological correlation. Indian J Lepr. 1992;64:58–66.
Ankad BS, Hombal A, Rao S, Naidu VM. Radiological changes in the hands and feet of leprosy patients with deformities. J Clin Diagn Res. 2011;5:703–7.
Mohammad W, Malhotra SK, Garg PK. Clinicoradiological correlation of bone changes in leprosy patients presenting with disabilities/deformities. Indian J Lepr. 2016;88:83–95.
Christensen VM, Bakke SN, Melson RS, Waaler E. Changes in the anterior nasal spine of the alveolar process of the maxillary bone in leprosy. Int J Lepr. 1952;20:335–40.
Srinivasan S, Nehru VI, Bapuraj JR, Sharma VK, Mann SB. CT findings in involvement of the paranasal sinuses by lepromatous leprosy. Br J Radiol. 1999;72:271–3.
Kiris A, Karlidag T, Kocakoc E, Bozgeyik Z, Sarsilmaz M. Paranasal sinus computed tomography findings in patients treated for lepromatous leprosy. J Laryngol Otol. 2007;121(1):15–8.
Jain S, Visser LH, Praveen TL, Rao PN, Surekha T, Ellanti R, et al. High-resolution sonography: a new technique to detect nerve damage in leprosy. PLoS Negl Trop Dis. 2009;3:e498.
Beekman R, Visser LH, Verhagen WI. Ultrasonography in ulnar neuropathy at the elbow: a critical review. Muscle Nerve. 2011;43(5):627–35.
Visser LH, Jain S, Lokesh B, Suneetha S, Subbanna J. Morphological changes of the epineurium in leprosy: a new finding detected by high-resolution sonography. Muscle Nerve. 2012;46(1):38–41.
Elias J, Nogueira-Barbosa MH, Feltrin LT, Furini RB, Foss NT, Marques W, et al. Role of ulnar nerve sonography in leprosy neuropathy with electrophysiologic correlation. J Ultrasound Med. 2009;28:1201–9.
Martinoli C, Derchi LE, Bertolotto M, Gandolfo N, Bianchi S, Fiallo P, et al. US and MR imaging of peripheral nerves in leprosy. Skelet Radiol. 2000;29:142–50.
Hari S, Subramanian S, Sharma R. Magnetic resonance imaging of ulnar nerve abscess in leprosy: a case report. Lepr Rev. 2007;78:155–9.
Luyckx G, Vanhoenacker FM, Parizel PM. Exotic pathology of the hand and foot. A pictorial review. JBR–BTR. 2008;91:160–5.
Maas M, Slim EJ, Heoksma AF, van der Kleij AJ, Akkerman EM, den Heeten GJ, et al. MR imaging of neuropathic feet in leprosy patients with suspected osteomyelitis. Int J Lepr Other Mycobact Dis. 2002;70(103):97.
Acknowledgments
Dr. Swetalina Pradhan for USG image.
Dr. Ashwini Babu for the clinical and ultrasonographic images.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pinto, M., Manjunath Shenoy, M. (2022). Electrophysiological and Radiological Investigations. In: Pradhan, S., Kumar, P. (eds) Clinical Cases in Leprosy. Clinical Cases in Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-031-08220-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-08220-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08219-1
Online ISBN: 978-3-031-08220-7
eBook Packages: MedicineMedicine (R0)