Abstract
Successful surgical treatment of ulnar neuropathy at the elbow requires a careful patient-based approach to address all sites of compression and associated pathology. Inadequate decompression and recalcitrant symptoms are commonly associated with inadequate release and/or unrecognized associated pathology. Ulnar nerve decompression can be successfully performed using an in situ or extensile approach with anterior transposition. The surgical technique should be tailored to the patient, severity of disease, and associated pathology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ulnar neuropathy
- Cubital tunnel syndrome
- Ulnar nerve decompression
- In situ release
- Anterior transposition
1 Description
Ulnar neuropathy in the cubital tunnel can be successfully treated through surgical decompression. Anterior transposition can decrease traction during peak elbow flexion and provide stability in cases of ulnar nerve subluxation. Anterior transposition can be performed using subcutaneous, submuscular, and intramuscular techniques.
2 Key Principles
Cubital tunnel syndrome (CuTS) involves compression of the ulnar nerve at the level of the elbow. The ulnar nerve is a branch of the lateral cord of the brachial plexus, carrying C8-T1 fibers. The ulnar nerve descends the medial brachium to the elbow, penetrates the medial intermuscular septum (IMS), and courses deep to a fascial arcade of Struthers. The nerve courses posteriorly around the medial epicondyle of the distal humerus and enters the cubital retinaculum (Osborne’s ligament). The nerve finally exits the cubital tunnel and enters the forearm between the humeral and ulnar heads of the flexor carpi ulnaris (FCU) muscle. As it does so, it passes beneath a final fascial arcade (of Osborne), which is found deep to the fascia of the FCU. Release of any/all of these offending compressive structures is key to successful surgical decompression (see Fig. 46.1).
3 Expectations
In situ decompression of the ulnar nerve can be performed through an open or endoscopic approach. In these cases, the nerve is decompressed starting at the cubital retinaculum, through the leading fascial edge of FCU and between the heads of FCU. In situ ulnar nerve release involves a balance of wide release through a smaller exposure while avoiding subsequent iatrogenic nerve instability. When a wider release is performed, the far proximal and distal sites of compression can be more definitively addressed. A larger resection of the intermuscular septum, definitive visualization and decompression of the ligament of Struthers, extensile intramuscular decompression of the ulnar nerve as it traverses the FCU, and the ability to address concomitant pathology are all benefits of a more extensile open approach. A wider release is required to prevent tethering and subsequent “Z deformity” when performing an anterior transposition.
4 Indications
Symptomatic ulnar neuropathy commonly involves painful paraesthesias with predominant night time and positional exacerbations. The onset is typically idiopathic with no identifiable cause. Less commonly, the condition can be posttraumatic. Symptoms can occur with normal anatomy or in the presence of posttraumatic or congenital bony deformity. Nerve conduction studies (NCS) are commonly abnormal, showing increased latency, decreased amplitudes, with signs of denervation and axonal injury in more severe cases.
5 Contraindications
Contraindications to in situ release include symptomatic ulnar nerve instability and in some cases severe motor changes.
6 Special Considerations
Alternate and often compounding sites of compression (second crush phenomenon) should be considered in the diagnosis of CuTS. Clinical evidence of ulnar nerve subluxation warrants transposition techniques. Snapping triceps symptoms or other concomitant local pathology should guide additional procedures (e.g. debridement of snapping portion of the medial triceps band). Severe motor atrophy should prompt consideration of techniques to augment axonal regeneration (e.g. anterior interosseous nerve into motor branch of the ulnar nerve, end to side “supercharge” procedure) and/or address additional sites of compression.
7 Special Instructions, Positioning, and Anesthesia
Supine positioning on a gurney using a hand table with a high brachial sterile tourniquet is preferred. Regional anesthesia is preferred. The medial elbow is brought into view by abducting the flexed and externally rotated elbow to 90 degrees at the patient’s side over a bump of towels. The surgeon sits in the axilla, while an assistant stabilizes the arm and retracts opposite him or her (see Fig. 46.2).
8 Tips, Pearls, and Lessons Learned
Optimal visualization through an adequate surgical exposure facilitates definitive neural decompression. Anterior subcutaneous transposition is tolerated well and can be performed efficiently with minimal change to post-operative recovery.
9 Difficulties Encountered
Meticulous hemostasis prevents complicating hematoma formation. Wide decompression of the proximal course of the ulnar nerve through generous resection of the intermuscular septum minimizes proximal tethering of the nerve following anterior transposition. Meticulous care is required to prevent inadvertent traction injury to the nerve intra-operatively.
10 Key Procedural Steps
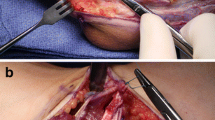
The medial epicondyle is a prominent landmark for any incision to expose the ulnar nerve. The incision is drawn just posterior to this, extending approximately 6 cm proximal, along the course of the palpable intermuscular septum, and 6 cm distal to the medial epicondyle. The distal extent angles gently posteriorly, toward the subcutaneous border of the ulna (see Fig. 46.3). The incision generally forms a straight line when the elbow is in an extended position. Care is taken during the approach to protect any encountered branches of the medial antebrachial cutaneous nerve (MABC). These are most commonly located crossing distal to the epicondyle. The ulnar nerve is best found proximal to the cubital tunnel as it lies deep and posterior to the IMS. Care is taken during this step to develop a definitive decompression plane that facilitates safe and efficient exposure of the nerve. Once the correct plane is identified, it is developed first superficially and then circumferentially to decompress the ulnar nerve in its entirety. Retraction of the superficial overlying tissue can facilitate visualization and decompression of the high IMS and any proximal fascial arcade (of Struthers). Superficial decompression of the ulnar nerve through Osborne’s ligament, around the prominence of the medial epicondyle, can be facilitated by slight elbow extension. Once exposure has descended to between the heads of FCU, care must be taken to decompress the superficial and deep fascial layers. It is at this level that motor branches of the ulnar nerve are encountered and must be dissected free to allow mobilization of the nerve anteriorly when transposition is performed. Once superficial dissection to the desired plane is completed, circumferential decompression is facilitated by gentle retraction of the nerve. This is best accomplished through non-mechanical pliable manipulation techniques, such as the use of a looped non-weighted Penrose drain. Circumferential decompression should allow un-tensioned anterior transposition of the ulnar nerve without any sharp angle (Z deformity) turns (see Fig. 46.4).
11 Bailout, Rescue, and Salvage Procedures
Any clinical evidence of pre-existing or iatrogenic instability resulting from decompression of the ulnar nerve should prompt consideration of anterior transposition. Stable anterior transposition can be performed successfully through various subcutaneous, intramuscular, and submuscular techniques. The type of technique chosen should reflect a patient specific surgical plan and depends heavily on response to prior surgery and concomitant pathology. In the setting of revision surgery, augments to prevent scaring around the nerve can be considered.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wilson, D.J., Cohen, M.S. (2022). Ulnar Nerve Decompression. In: Dines, J.S., van Riet, R., Camp, C.L., Mihata, T. (eds) Tips and Techniques in Elbow Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-08080-7_46
Download citation
DOI: https://doi.org/10.1007/978-3-031-08080-7_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08079-1
Online ISBN: 978-3-031-08080-7
eBook Packages: MedicineMedicine (R0)