Abstract
Coagulopathy is the disruption of the harmonic balance between hemostasis and fibrinolysis. A frequently encountered cause of pediatric coagulopathy for the pediatric surgeon is trauma-induced coagulopathy. Historically, blood counts and conventional coagulation tests served as limited assessments of coagulation cascade abnormalities; however, viscoelastic monitoring allows for real-time assessment of the coagulation cascade with goal-directed hemostatic resuscitation. Transfusion of blood products (red blood cells, plasma, platelets) has inherent risk ranging from clinically benign to life threatening. This is especially relevant in pediatric transfusion medicine as certain age groups (neonates) are predisposed to laboratory abnormalities, such as thrombocytopenia. Historically, these abnormalities resulted in liberal transfusion thresholds and guidelines; however, more recent guidelines have moved toward restrictive transfusion strategies, balanced resuscitation, and even the use of whole blood transfusions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Trauma-induced coagulopathy
- Viscoelastic monitoring
- Restrictive transfusion strategies
- Balanced resuscitation
Coagulopathy is a well-described phenomenon of multifactorial etiology that is most common in traumatically injured or critically ill children and is strongly associated with increased morbidity and mortality. The early identification and management of coagulopathy is a critical component of successful resuscitation. More than a third of pediatric trauma patients admitted to the ICU have coagulopathy (INR ≥ 1.2). In adults and children, risk factors for acute traumatic coagulopathy include penetrating injury, traumatic brain injury, shock, and non-accidental trauma. Additionally, coagulopathy is associated with higher transfusion requirements, greater incidence of multiorgan dysfunction syndrome, longer ICU stay, longer hospital stay, increased duration of mechanical ventilation, and increased mortality.
Hemostasis and Fibrinolysis
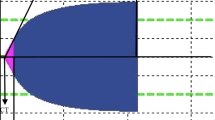
Coagulation is a dynamic, interwoven process that can be described in several phases: (1) endothelial injury with formation of the platelet plug, (2) propagation of the clotting process by the coagulation cascade, (3) termination of the process by antithrombotic mechanisms, and (4) removal of clot with fibrinolysis. After injury to the endothelium, platelets are exposed to subendothelial components leading to platelet activation, adhesion, and aggregation. Following activation, platelets undergo significant shape changes with platelet adhesion to the endothelium due to the binding of platelet surface receptor GPIb to von Willebrand factor (vWF). Platelet aggregation then proceeds with the interaction between platelet surface receptor GPIIb/IIIa, fibrinogen, and vWF. Abnormalities within these interactions are known to cause several congenital coagulopathies. Once the platelet plug has successfully formed, the coagulation cascade occurs to stabilize the clot (Fig. 12.1). Unique to the pediatric population, children exhibit age-dependent variation in coagulation factor profiles, termed developmental hemostasis, a limitation in applying the adult coagulopathy literature to children.
Coagulation cascade with impairments caused by acidemia. Boxed figures represent factors and complexes in which activity is significantly increased by acidemia. Dashed lines represent inhibition of reactions. Adapted and modified from (Choi PM, Vogel AM. Acute coagulopathy in pediatric trauma. Curr Opin Pediatr. 2014;26(3):343–9). PAI-1 plasminogen activator inhibitor-1, tPA tissue plasminogen activator
Evolutionary checks in the form of natural anticoagulation factors and fibrinolysis are essential to ensure clot formation does not propagate unwarranted, resulting in uncontrolled thrombosis. The key anticoagulation factors are antithrombin and activated protein C (APC). The primary role of antithrombin is to neutralize thrombin, eliminating its ability to cleave fibrinogen to fibrin. It additionally prevents the activation of factors V and VIII and inhibits the activation and aggregation of platelets. The second primary player, APC, acts by inactivating factors V and VIII. And finally, to complement the natural anticoagulants, physiologic clot formation is controlled with fibrinolysis, which ensures thrombus formation does not propagate outside of the traumatic site. The central enzyme for this process is plasmin, a protease generated from the inactive proenzyme plasminogen by tissue plasminogen activator (tPA). Plasminogen and tPA are incorporated into the fibrin clot during its formation. In perfect evolutionary balance, thrombin actually promotes the release of tPA from endothelial cells. In summary, hemostasis is a complex, interlinked process of clot formation, clot stabilization, inhibition of propagation, and dissolution with central players including platelets and endothelial cells utilizing key molecules such as tissue factor, thrombin, fibrin, and plasmin. Abnormalities in any of the essential steps in this complex process can lead to coagulopathy.
Coagulopathy
Normal coagulation is the balance of hemostatic and fibrinolytic processes, which permit control of bleeding and prevent intravascular thrombosis. Coagulopathy occurs when there is an imbalance between these processes, typically due to a combination of acidosis related to tissue injury or shock, hypothermia from exposure and fluid resuscitation, and hemodilution due to fluid or excessive component blood product administration. Pediatric surgeons commonly encounter coagulopathy when managing critically ill patients suffering from sepsis, trauma, receiving extracorporeal life support, and following complex, high blood loss procedures. Inadequate systemic perfusion in the setting of shock leads to metabolic acidosis, inciting coagulopathy by decreasing the efficacy of coagulation factors. One iatrogenic intervention that can worsen acidosis includes resuscitation with normal saline, which contributes to a non-anion gap metabolic acidosis. Additionally, hypothermia has a synergistic effect on acidosis with an increase in mortality with both compared to each alone. Hypothermia specifically results in platelet dysfunction and impaired enzymatic function with temperatures between 33 and 37 °C causing impairment of tissue factor activity, platelet aggregation, and platelet adhesion. For every 1° drop, clotting activity is decreased by approximately 5%. A final contributor to coagulopathy is resuscitation-associated coagulopathy, in which large-volume resuscitation with crystalloid, colloid, and packed RBC alone leads to dilution of clotting factors.
Trauma-Induced Coagulopathy
One of the most common forms of coagulopathy observed is trauma-induced coagulopathy (TIC), which carries a high risk of significant morbidity and mortality. TIC is an impairment of both hemostasis and fibrinolysis occurring immediately after initial injury due to hemorrhage and tissue damage. Tissue injury results in the exposure of collagen, inciting the coagulation cascade. Following initial tissue injury, hemorrhage shortly follows with associated hypoperfusion stimulating the endothelium to release thrombomodulin, which interacts with thrombin to activate protein C. APC inactivates factors V and VIII, ultimately leading to hypocoagulation, and consumes plasminogen activator inhibitor-1, leading to an increase in tPA and relative hyperfibrinolysis. Furthermore, fibrinogen levels decrease after initial traumatic injury with half of pediatric trauma patients having hypofibrinogenemia on laboratory assessment. Based on these laboratory findings, patients with TIC can meet criteria for disseminated intravascular coagulation, and some have suggested TIC represents an early stage of compensated DIC. However, TIC occurs in the absence of thrombocytopenia and only when tissue injury is superimposed with systemic hypoperfusion; therefore, the underlying pathologic mechanisms are likely distinct.
Disseminated Intravascular Coagulopathy
DIC is an acquired syndrome characterized by excessive systemic activation of coagulation causing simultaneous hemorrhage and microvascular thrombosis with consumptive coagulopathy ultimately leading to end organ damage. It is a secondary process caused by varying etiologies including systemic infection, malignancy, and trauma. Sepsis is the leading cause of DIC in both infants and children. With regard to malignancy, DIC is especially common in children with hematologic disorders and can serve as a major cause of morbidity and mortality. Again, traumatic injury can also be an inciting factor in DIC with damaged tissue releasing tissue enzymes and phospholipids into the system circulation triggering activation of the coagulation system. A particular high-risk pediatric trauma population is those patients with TBI as brain tissue is a potent procoagulant with severe brain injury increasing the risk of DIC. Finally, newborns, especially preterm, are particularly vulnerable to DIC due to an imbalance of coagulation factors, specifically antithrombin and protein C, with the main causes, including sepsis, respiratory distress syndrome, perinatal asphyxia, and neonatal enterocolitis.
Hematologic Assessment and Monitoring
Independent of the etiology behind coagulopathy the underlying mechanisms have a similar end result with an imbalance of hemostasis and fibrinolysis. Early recognition with clinical acumen and laboratory evaluation allows for timely interventions with appropriate product resuscitation. Historically, coagulopathy was detected with blood counts and conventional coagulation testing (CCT); however, techniques, such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM), allow for real-time goal-directed hemostatic resuscitation. Blood counts and CCT have limitations with identifying coagulopathy and have been shown to not adequately characterize the complex disequilibrium of TIC. Additionally, these tests require more time (approximately 30–50 min) to process before results are available.
Viscoelastic Monitoring
TEG and ROTEM are point-of-care measures of hemostasis that evaluate the global viscoelastic mechanical properties of whole blood and appear to be more accurate measures of TIC. With TEG, a sample of whole blood is pipetted into a cuvette and activated with a reagent. The activated blood sample is then placed into a thromboelastography machine and the cuvette begins to oscillate. The viscoelastic mechanical properties of the blood sample are transduced by a pin into a graphical tracing, (Fig. 12.2) and a computational algorithm generates individual data points. For ROTEM, the pin oscillates instead of the cuvette. A variant of the TEG called rTEG utilizes tissue factor to accelerate initial activation of the clotting cascade, allowing results within 5–15 min. The TEG tracing provides different variables, which represent clot initiation, clot strength, and fibrinolysis. The activated clotting time (R time) is time from initiation of clotting cascade to fibrin formation and represents the efficacy of clotting factors. The α-angle is the rate of clot formation with decreasing values corresponding to hypofibrinogenemia. The maximum amplitude (MA) corresponds to quantity and efficacy of platelet function, and the clot lysis at 30 min (LY30) represents fibrinolysis. In the evaluation of resuscitation, different abnormalities within the TEG tracing suggest different mechanisms of coagulopathy and direct appropriate blood product resuscitation in real time. Blood products and pharmacologic adjuncts may be administered based on viscoelastic monitoring interpretation.
Transfusion Complications
Transfusion of blood products is not a benign intervention with several well-known complications arising from transfusions. The immediate management of all serious transfusion complications includes cessation of transfusion with consultation to transfusion medicine or the institutional blood bank to assist with work-up and generating differential diagnoses.
Febrile Non-hemolytic Transfusion Reaction
One of the most common of all transfusion reactions is febrile non-hemolytic transfusion reaction (FNHTR) with estimated prevalence of 0.1–1% and an increased prevalence in children relative to adults. The underlying mechanism for the reaction is generation and accumulation of cytokines, specifically IL-1, IL-6, IL-8, and TNFα, during the storage process. Increased duration of product storage and number of leukocytes in the product are associated with an increased risk of FHNTR. The classic clinical presentation of FNHTR is self-limited fever or chills within 1–6 h of transfusion and is diagnosed after excluding more severe reactions, such as acute hemolytic reaction. The treatment for FNHTR is supportive with stopping the transfusion and administration of antipyretics. Primary preventive measure for FNHTR is reducing the number of leukocytes in the blood product via leukoreduction. Interestingly, premedication with acetaminophen or diphenhydramine does not appear to be effective in reducing the incidence of FNHTR compared to placebo; therefore, it is currently not recommended as a preventive strategy.
Allergic Transfusion Reactions
A similarly benign but common transfusion reaction is an urticarial or allergic reaction to product transfusion, occurring with an estimated incidence of 1%. The underlying mechanism occurs when soluble products in the transfused blood product react with preformed recipient IgE antibodies and cause release of histamine from mast cells. Clinical diagnosis is based on identification of new-onset urticaria without progression to more severe symptoms. Urticarial reactions are one of the few transfusion reactions in which the transfusion can safely continue; however, it should be temporarily stopped and diphenhydramine administered prior to completion.
Anaphylactic transfusion reactions share the same underlying mechanism as urticarial reaction; however, it is significantly worse and potentially life threatening. Fortunately, the incidence of anaphylactic transfusions is very low, occurring only in approximately 1 in 50,000 RBC and plasma transfusions. One well-characterized mechanism for this reaction is IgG anti-IgA antibodies in IgA-deficient patients. While selective IgA-deficient patients are fairly common (1 in 300 patients), few patients actually develop IgG anti-IgA antibodies (1 in 1600), which drive the anaphylactic mechanism. Anaphylactic transfusion reactions occur within a few seconds to minutes following transfusion with hypotension, angioedema, wheezing, and respiratory distress. Correct diagnosis is based on clinical evaluation with identification of symptom presentation with relation to timing of transfusion. The differential includes other transfusion reactions, including transfusion-related lung injury (TRALI), transfusion-related circulatory overload (TACO), and sepsis. A differentiating clinical symptom is angioedema and wheezing, which are not observed with these other reactions. Treatment includes immediate cessation of transfusion, stabilization of the airway with possible intubation if necessary, intramuscular epinephrine (0.01 mg/kg), and fluid resuscitation. This algorithm should be well known as timely diagnosis and intervention will be life saving for the child.
Hemolytic Reactions
A similarly life-threatening transfusion reaction is the hemolytic transfusion reaction (HTR), characterized by immune-mediated hemolysis. HTR is further grouped into acute (within 24 h) or delayed (days to weeks) presentation based on timing of reaction with transfusion event. Acute HTR can be caused by any blood product but is typically secondary to ABO blood group incompatibility due to clerical error. Recipient IgG anti-A or anti-B antibodies result in destruction of the donor blood cells, resulting in intravascular thrombosis and possibly acute kidney injury, DIC, and hemodynamic collapse. Acute HTR is a medical emergency and initial steps include discontinuing the transfusion and providing hemodynamic support with crystalloid and inotropic medications. Importantly, the crystalloid of choice should be normal saline as lactated ringers contain calcium, which can further activate the clotting cascade. While an acute HTR can be life threatening, it is self-limited and dependent on volume of transfused product.
Delayed HTR commonly presents 1–2 weeks after transfusions and are due to a response to a foreign RBC antigen (Rh antigen) for which the patient was previously exposed. In contrast to the intravascular hemolysis characteristic of acute HTR, delayed HTR results in extravascular hemolysis and is therefore frequently clinically silent. The diagnosis is often made by the blood bank due to a new positive antiglobulin test or new positive antibody screen. In patients diagnosed with delayed HTR, no specific intervention is required besides monitoring of hemoglobin.
Transfusion-Related Acute Lung Injury
TRALI occurs at a rate of 0.04–0.1% for transfused blood components with the incidence increasing to approximately 5% in certain high-risk populations such as the critically ill. Risk factors for TRALI include positive fluid balance, smoking, increased IL-8 levels, high peak airway pressures during invasive mechanical ventilation, shock, chronic alcohol abuse, recent liver transplantation, emergency cardiac surgery, hematologic malignancy, and massive transfusion. Blood component-specific risk factors include high plasma volume components such as plasma, apheresis plasma concentrates, and whole blood; female donors; and increased volume of transfused anti-human neutrophil antigen antibody. The underlying pathogenesis of TRALI occurs via a two-hit mechanism. First, prior to the transfusion event, lung endothelial cells prime and sequester neutrophils secondary to a pre-existing injury. The need for this pre-existing injury is one reason the incidence of TRALI is increased in the critically ill population. Then, the primed recipient neutrophils are activated by blood components, releasing cytokines, reactive oxygen species, oxidases, and proteases that further damage the pulmonary endothelium causing an inflammatory pulmonary edema. A second model related to the two-hit model is the threshold model. In this model, the second step is so significant that a priming event is unnecessary. This model helps explain how a previously healthy individual can develop TRALI.
TRALI is a clinical diagnosis based on acute onset hypoxemia within 6 h of a transfusion, bilateral infiltrates on chest radiography in the absence of circulatory overload, and pre-existing acute lung injury or acute respiratory distress. Hypoxemia is documented with oxygen saturation <90% on room air or PaO2/FiO2 less than 300 mmHg. The cornerstone of treatment is supplemental oxygenation, CPAP/BiPAP, or invasive mechanical ventilation, as needed. Hemodynamic support should be used with resuscitation and pharmacologic agents if necessary. There is no evidence supporting the use of corticosteroids for TRALI. The duration of mechanical ventilation typically lasts 3–10 days following transfusion event with most survivors returning to baseline pulmonary function. But in critically ill patients, mortality approaches 50%. Several preventive strategies have been used to mitigate the incidence of TRALI, include deferral of multiparous female donors, transfusion of pooled solvent/detergent-treated plasma product instead of FFP, and suspension of platelets in platelet additive solution.
Transfusion-Associated Circulatory Overload
TACO is defined as circulatory overload secondary to transfusion of products and is directly related to volume of transfusion. Specific risk factors associated with TACO include pre-existing cardiorenal disease, low body weight, extremes of age (<3, >60), and increasing units of product transfused. The incidence of TACO in perioperative patients is approximately 1%. While TACO can occur in children, it is more frequent in adults. The underlying pathophysiology includes pre-existing volume incompliance secondary to cardiorenal disease. Diagnosis should be considered in any patient with respiratory distress, hypoxia, and hypertension within 6–12 h of transfusion with severity ranging from mild dyspnea to acute respiratory decompensation. The initial evaluation is focused on differentiating TRALI and TACO. TACO is more likely in very young patients with underlying cardiac disease who received a large-volume transfusion over a short period of time. Treatment parallels the treatment for cardiogenic pulmonary edema with cessation of transfusion, mobilization of intravascular volume with diuresis, and supplemental oxygen. The treatment algorithm further highlights the importance of differentiating between TRALI and TACO as TRALI includes fluid resuscitation while TACO requires diuresis. The primary preventive strategy for TACO is avoiding unnecessary transfusions and transfusing small volumes of products slowly.
Infections
A final complication associated with transfusions is infections, both viral and bacterial. All blood products in the US are screened for HIV, Hepatitis B and C, and more viruses, significantly decreasing the risk of viral transmission following transfusion. However, a risk still exists during a window period following initial exposure of virus prior to a donor’s immunologic response and generation of detectable antibodies against the virus. Bacterial infections are much more common than viral infections. Organisms associated with transfusion-associated bacterial infection (TABI) are varied, including both gram-positive and gram-negative organisms associated with skin and gut flora. Sources of organisms include donor blood, donor skin, phlebotomist’s skin, and environmental contamination during production and packaging. Platelets are significantly more likely to be contaminated than other products due to their storage at room temperature. Clinical manifestations of TABI include fever, rigors, tachycardia, and hypotension with symptom onset at approximately 30 min after transfusion. The presenting symptoms are similar to many of the other transfusion reactions; therefore, initial management is similar with cessation of transfusion and resuscitation. When clinically concerned for TABI, initial labs should include blood cultures followed by empiric broad-spectrum antibiotics. Preventive strategies to decrease the risk of TABI include skin preparation with 2% chlorhexidine in 70% isopropyl alcohol, discarding the initial aliquot of donor blood, reduced storage time, and bactericidal treatments, such as ultraviolet light exposure after psoralen.
Transfusion Products
Red Blood Cells
The primary intent in RBC transfusion is to improve oxygen carrying capacity. In 2018, the Pediatric Critical Care Transfusion and Anemia eXpertise Initiative (TAXI) reviewed the literature regarding RBC transfusions in critically ill children and released clinical guidelines for critically ill children. The over-arching recommendations were that RBC transfusion should be based not only on hemoglobin concentration but also on patient-related data such as age, comorbidities, severity of illness, and laboratory assessment. RBC transfusion was warranted for critically ill children with hemoglobin <5 g/dL and not warranted for hemodynamically stable children with hemoglobin >7 g/dL. There is currently insufficient evidence to make recommendations regarding transfusion thresholds for critically ill children with hemoglobin from 5 to 7 g/dL. For critically ill children with life-threatening bleeding or hemorrhagic shock, a balanced ratio of RBC, FFP, and platelets of either 1:1:1 or 2:1:1 is recommended. The goal should be to address the original indication for transfusion, not necessarily to normalize hemoglobin.
The dosing of RBC transfusion is typically 10–15 mL/kg with an associated increase in hemoglobin concentration of 2–3 g/dL or the hematocrit by 6–9%. A transfusion rate of 2.5 mL/kg per hour helps in preventing TACO; therefore, 10 mL/kg can be safely transfused over 4 h. Patients at high risk for TACO, such as those with cardiac or renal comorbidities, can be transfused at a slower rate of 1 mL/kg/h. Importantly, certain fluids are incompatible with RBC transfusions, which include hypotonic solutions due to hemolysis and lactated Ringers due to the calcium reversing the anticoagulation added to stored RBC. RBC are typically stored at low temperatures ranging from 1 to 6 °C ;therefore, blood warmers are necessary in certain clinical scenarios to prevent hypothermia, including unstable infants, patients who require rapid transfusion of a large amount of blood (>15 mL/kg/h), patients who require exchange transfusions, or patients with cold agglutinin disease.
Fresh Frozen Plasma
The primary reason for transfusion of FFP is to correct deficiencies of clotting factors. However, the pediatric literature suggests FFP is commonly over-transfused without any significant implementation or adoption of the restrictive strategies observed for RBC transfusions. Approximately half of neonates receive prophylactic FFP secondary to abnormal coagulation values without evidence of active bleeding. Coagulation times in the neonate, especially the premature neonate, are expected to be longer than adults, but this is not associated with an increased risk of bleeding or an indication for FFP transfusion. Similarly in the pediatric ICU, significant bleeding is the reason for only about a fifth of FFP transfusions, and transfusion significantly improves PT/INR only in patients with an INR > 2.5. And in more than half of FFP transfusions given to children on ECMO for bleeding prophylaxis, there is no significant change in laboratory values pre- and post-transfusion. There is limited research currently identifying the risk associated with FFP transfusions; however, it appears to be associated with increased dose-dependent risk of allergic reactions, fever, TRALI, TACO, hemolysis, and venous thrombosis. With limited high-quality research available, current guidelines recommend transfusion of FFP for active coagulopathic bleeding and preceding surgery or invasive procedures in the setting of PT/PTT >5× normal or abnormal viscoelastic monitoring. In contrast, FFP should not be given in non-bleeding children to prophylactically prevent bleeding except for invasive procedures with risk of significant coagulopathic bleeding and children with significant abnormal age-adjusted coagulation profiles. Furthermore, it should not be given prior to surgery or invasive procedure with only minor prolongation of PT/PTT (<1.5× normal) or solely as volume replacement.
A typical dose of FFP is 10–20 mL/kg transfused at a rate of 10–20 mL/kg/h with an expected increase in factor levels by 15–25%. Prior to transfusion, FFP should be thawed to approximately 35 °C and transfused as soon as possible. However, it can be administered up to 24 h after thawing if stored at 4 °C.
Platelets
The fundamental purpose of platelet transfusion is to provide platelets for coagulation and assist with clotting. Similar to the FFP, more than half of platelet transfusions administered to critically ill children are given as prophylaxis in non-bleeding scenarios. Neonates have a high prevalence of thrombocytopenia leading to increased rates of platelet transfusions relative to other age groups. However, similar to abnormal coagulation tests, the abnormality does not correlate with an increased risk of bleeding. Current literature emphasizes the hazardous effects of platelet transfusions in children; however, there are several circumstances when it is indicated, including <25,000/μL with no associated bleeding; <50,000/μL with bleeding, coagulopathy, or preceding surgery; or <100,000/μL with major bleeding or major surgery.
Apheresis (rather than pooled) platelets are recommended for children <16 years old to reduce donor exposure. Dosing is dependent on weight with children <15 kg administered 10–20 mL/kg and children >15 kg administered approximately 300 mL with each transfusion. The recommended rate of administration is 10–20 mL/kg/h. A single platelet transfusion is expected to raise the platelet count by 30–60,000/μL.
Hemostatic Resuscitation
Hemostatic resuscitation in trauma-induced coagulopathy is a cornerstone of damage control resuscitation and aims to provide balanced resuscitation with blood products resembling the basic components of whole blood. Additional tenets include permissive hypotension and damage control surgery. Historically, trauma patients have been aggressively resuscitated with crystalloid solutions to maintain normal blood pressure, which ultimately led to poor outcomes from resuscitation-associated coagulopathy. In contrast, hemostatic resuscitation uses balanced ratios of blood products to maintain circulating volume, correct ongoing coagulopathy, and prevent hypothermia and acidosis. Current research regarding hemostatic resuscitation has focused on the use of viscoelastic monitoring, massive transfusion protocols, balanced blood product ratios, and the use of whole blood.
Conventional Coagulation Tests Vs. Viscoelastic Monitoring
CCT was the primary laboratory assessment of the coagulation cascade for management of TIC for the past 50 years. One primary limitation of CCT is delayed availability of results with tests requiring approximately 30–60 min to finalize. In an acutely hemorrhaging patient with multiple injuries and worsening coagulopathy, the time during initial assessment is invaluable in correctly identifying the abnormalities of the coagulation cascade and providing appropriate resuscitation. In contrast, viscoelastic monitoring allows for a real-time, in-depth view of the coagulation cascade and can allow for timely hemostatic resuscitation. Viscoelastic monitoring includes TEG, r-TEG, and ROTEM with results available as quickly as 5–15 min (Fig. 12.3).
TEG abnormalities with associated changes in the tracing: (a) Normal R time and α-angle with low MA and high LY30, reflecting primary hyperfibrinolysis prior to the clot reaching its maximum strength. Based on this interpretation, the patient would benefit from tranexamic acid (TXA) administration. (b) Normal R time and α-angle with a high LY30; however, the MA is normal with close overlap between the two tracings, representing secondary hyperfibrinolysis. In this scenario, fibrinolysis does not occur until maximum clot strength has occurred; this patient would also benefit from TXA. (c) A patient with thrombocytopenia with normal values except for MA, suggesting the need for platelet transfusion. (d) A patient with prolonged R time with noticeably decreased α-angle and MA with normal LY30. In this scenario, the patient has enzymatic (R time) and platelet (MA) hypocoagulability with poor fibrin deposition (α-angle). Therefore, the patient would benefit from transfusion of FFP, cryoprecitate, and platelets. (e) A patient with hypercoagulability due to a shortened R time (enzymatic hypercoagulability) and increased α-angle (excessive fibrin deposition)
The R time (normal 5–10 min) represents the initiation of clot formation; therefore, a prolonged time represents a deficiency in clotting factors and the resuscitation should include FFP to replenish the depleted factors. The α-angle (normal 53–72°) represents clot stabilization and the efficacy of conversion of fibrinogen to fibrin. A depressed α-angle suggests the patient requires cryoprecipitate to restore normal levels of fibrinogen. The maximum amplitude (MA) corresponds to the quantity and quality of platelet function; therefore, a decreased MA (normal 50–70 mm) suggests the patient requires platelet resuscitation. And finally, an increased clot lysis at 30 min (LY30, normal 0–3%) represents over-active fibrinolysis, so the patient may be treated with an anti-fibrinolytic agent, such as tranexamic acid.
Massive Transfusion Protocols
Using a balanced ratio of blood products, massive transfusion protocols improve mortality and risk of coagulopathic complications in the adults. However, definitive evidence in pediatrics is lacking. Massive transfusion in children has been defined as 35–40 mL/kg in 4–24 h. Although in the past decade several pediatric trauma centers have successfully implemented MTP and reported their outcomes, current evidence is insufficient to support a significant improvement in overall mortality. Prospective multi-center trials are needed to answer this important question.
The adult trauma literature supports the use of balanced 1:1:1 resuscitation of RBC, FFP, and platelets in massively transfused coagulopathic patients. The theoretical benefit of balanced resuscitation is simultaneous correction of acute blood loss and stabilization of coagulation. The current pediatric transfusion literature, on the other hand, suffers from a relatively small sample size of children who require massive transfusion and the preponderance of retrospective studies. Future controlled trials will need to be conducted to fully address the research question. Until then it seems reasonable, based on the overwhelming evidence in favor of balanced resuscitation in adults, for pediatric surgeons to resuscitate critically ill pediatric patients based on a balanced protocol.
Whole Blood
Historically, the initial use of whole blood transfusions to correct acute hemorrhage and coagulopathy was in the military with soldiers themselves serving as mobile blood banks. Over the past 100 years, trauma resuscitation moved toward component separation and crystalloid resuscitation. However, a robust body of research in support of balanced resuscitation strategies has allowed the foundation of resuscitation to return full circle to whole blood. The primary limitation of whole blood use in the previous military setting was concerns for the potential of hemolysis, the efficacy of cold-stored platelets, the need for ABO compatibility, and the lack of platelet-sparing whole blood leukoreduction filter. However, recent translational research has shown the safety and efficacy of using cold-stored low-titer anti-A and anti-B group-O whole blood to address several of these limitations. The use of low-titer group-O whole blood serves several advantages over traditional component resuscitation, including higher hematocrit levels, increased platelet counts, increased factor concentrations, and less additive solution for an equivalent blood volume. Additionally, since low-titer group-O whole blood is stored in colder temperatures (1–6 °C) relative to component platelets (20–24 °C), the shelf-life increases by more than a week. The primary limitations regarding universal use of low-titer group-O whole blood is limited availability with fewer qualified donors, labor-intensive stocking and re-processing for blood banks, and theoretical concerns regarding the transfusion of group-O whole blood to non-group-O recipients. In the pediatric trauma literature, single-center studies have shown the safety and benefits of using group-O whole blood transfusions. While these early studies show promising results for the use of low-titer group-O whole blood in the pediatric trauma population, larger prospective trials are required to continue to support its universal use.
Pharmacologic Adjuncts
Prothrombin Complex Concentrates and Recombinant Factor VII
Prothrombin complex concentrate (PCC) is rich with factors II, VII, IX, and X. In the clinical setting, PCC has primarily been evaluated for reversal of Vitamin K antagonists. In pediatrics, there is weak evidence regarding indications with current guidelines recommending PCC for acquired coagulopathic conditions from Vitamin K antagonists in patients undergoing invasive surgery. Another factor-based therapy that has emerged in the specific management of TIC is recombinant factor VII. Its use in trauma was spawned by the knowledge that the principle trigger of clot formation in trauma was the interaction between injury-exposed TF binding to activated factor VII. While it has shown promise in decreasing blood product requirements in adult trauma populations, it has only been reported in case reports in children.
Tranexamic Acid
Tranexamic acid (TXA)is an anti-fibrinolytic agent used in a broad range of applications, including surgery and trauma. Several randomized controlled trials in pediatric patients undergoing cardiac surgery, spinal fusion, and craniosynostosis repair have identified TXA as safe and effective in reducing both blood loss and transfusion requirements. While the pediatric literature has shown promising results for its perioperative use, there is very limited research involving positive outcomes in the pediatric trauma population. However, studies in adults have calculated risk/benefit for trauma patients, suggesting those with acute life-threatening hemorrhage and hyperfibrinolysis who present within 3 h of injury benefit significantly from TXA (Fig. 12.3a), but that patients with delayed presentation and absence of fibrinolysis (LY30 0%) are at higher risk of thromboembolic complications and long-term organ failure if administered TXA. This significant difference in outcomes based on timing of injury and administration of TXA further supports the essential role of viscoelastic monitoring in hemostatic resuscitation. With these findings in mind, it is important to remember that TXA serves as only as a clot stabilizer, by blocking the conversion of plasminogen to plasmin, and there appears to be little significant increase in thromboembolic complications when administered for appropriate indications. Therefore, the primary indications for administration in the pediatric population include prophylaxis or treatment of trauma or surgery with major bleeding and prophylaxis or treatment for mild or moderate bleeding when there is a desire to avoid RBC transfusions or pre-existing anemia, coagulopathy, or hypofibrinogenemia. Current recommendations for dosing of TXA are a loading dose of 10–30 mg/kg followed by a maintenance infusion of 5–10 mg/kg/h.
Summary
In conclusion, trauma-induced coagulopathy is the most frequently encountered cause of coagulopathy for the pediatric surgeon and carries a high risk of associated morbidity and mortality. New viscoelastic monitoring allows physicians to more accurately and speedily diagnose and correct coagulation deficits. While the current pediatric literature is limited, clinical guidelines primarily support restrictive, balanced resuscitation strategies for coagulopathy.
Editor’s Comments
PT/PTT are not very useful as a screening for coagulopathy and, unless there is a clinical concern for a risk of a bleeding diathesis, are should probably no longer be considered routine prior to most elective pediatric surgical operations. This is especially true in infants under 1 year of age, whose coagulation parameters are often prolonged but routinely disregarded. Detailed family and personal histories of significant bleeding episodes are more reliable. Patients with traumatic brain injury should also be assumed to have a bleeding diathesis, regardless of what the lab tests suggest.
For a long time, the only assessments of a patient’s coagulation status available to the clinician included PT/PTT and platelet count. A bleeding time was available but rarely a practical option for children. We now have much better tests. Thromboelastography (TEG) and rotational thromboelastometry (ROTEM) provide more practical information regarding a patient’s coagulation status with a quicker turnaround time. These should become more widely available in the OR and in the trauma bay.
Preventing coagulopathy during trauma resuscitation or major operations is at least partly the surgeon’s responsibility. This includes proactive measures to avoid hypothermia, using careful technique so as to avoid major hemorrhage, and, when a patient requires a massive transfusion, insisting that they receive either whole blood, when available, or packed red blood cells, FFP, and platelets in a 1:1:1 ratio. Vitamin K administration is nearly risk free and should be considered in neonates, patients who have undergone major liver resection, and those with familial or acquired cholestasis. For a while, activated factor VII was fashionable and used extensively in patients with major bleeding but, although safe and effective when used properly, its overuse can lead to thrombotic complications. Finally, the clot stabilizer TXA is increasingly shown to be effective in decreasing the risk of significant hemorrhage after major trauma and surgery in adults but, for reasons that are not entirely clear, it is not used as much as it probably should be in children or adolescents during operations expected to result in major blood loss (spinal fusion, liver resection, some tumor resections), especially given how safe it appears to be.
Venous thromboembolism (VTE) and pulmonary embolism (PE) are fortunately exceedingly rare in children and not nearly as prevalent in adolescents as they are in adults. Nevertheless, they remain a significant cause of death and life-long debility in pediatric surgical patients. Surgeons have traditionally taken the lead in enacting measures to prevent these potentially devastating complications. This usually means, for patients 12 years or older who are at average risk, using sequential compression devices during operations that last more than an hour or so and after surgery making the patient walk early and often. But for patents at highest risk (obesity, malignancy, IBD) we should not be afraid to give enoxaparin, even if we have become less comfortable or experienced in its use. Probably the most important factor in preventing VTE is obtaining a detailed family history prior to any major elective operation—it is surprisingly common (and awfully embarrassing) how often the patient with a thrombotic complication will divulge, when asked, that their mother/father/brother/aunt “had the same thing happen to them.” Any patient with a family history of a clot-based disease or complication should be referred to a hematologist ahead of time for testing and probably should be administered prophylactic enoxaparin regardless. The factor V Leiden mutation is especially prevalent (~5% of Caucasians) and should be specifically screened for. Finally, surgeons should be vigilant for the subtle signs of thrombosis in their postoperative patients. Traditional signs like fever, calf tenderness, and chest pain are dubious and non-specific. More important signs include asymmetrical leg swelling, swelling in an extremity with a PICC in place, vague but intense postprandial abdominal pain (suggesting mesenteric vein thrombosis), and subtle signs of hypoxia (tachypnea, anxiety) or pleuritic chest pain, which can suggest PE. Although expensive and undeniably overused, US or CT should be obtained whenever there is concern for thrombosis. And because they appreciate that the implications of a thromboembolic event cannot be overstated, experienced surgeons know not to make smug remarks when these tests come back negative.
Further Reading
Butler EK, Mills BM, Arbabi S, Bulger EM, Vavilala MS, Groner JI, et al. Association of blood component ratios with 24-hour mortality in injured children receiving massive transfusion. Crit Care Med. 2019;47(7):975–83.
Chidester SJ, Williams N, Wang W, Groner JI. A pediatric massive transfusion protocol. J Trauma Acute Care Surg. 2012;73(5):1273–7.
Choi PM, Vogel AM. Acute coagulopathy in pediatric trauma. Curr Opin Pediatr. 2014;26(3):343–9.
Cohen MJ, Call M, Nelson M, Calfee CS, Esmon CT, Brohi K, et al. Critical role of activated protein C in early coagulopathy and later organ failure, infection and death in trauma patients. Ann Surg. 2012;255(2):379–85.
Cotton BA, Faz G, Hatch QM, et al. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. J Trauma. 2011;71(2):407–17.
Cunningham ME, Rosenfeld EH, Zhu H, Naik-Mathuria BJ, Russell RT, Vogel AM. A high ratio of plasma: RBC improves survival in massively transfused injured children. J Surg Res. 2019;233:213–20.
Curley A, Stanworth SJ, Willoughby K, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380(3):242–51.
Davies P, Robertson S, Hegde S, Greenwood R, Massey E, Davis P. Calculating the required transfusion volume in children. Transfusion. 2007;47(2):212–6.
de Oliveira Manoel AL, de Oliveira Manoel AL, Neto AC, et al. Traumatic brain injury associated coagulopathy. Neurocrit Care. 2015;22(1):34–44.
Dirkmann D, Hanke AA, Görlinger K, Peters J. Hypothermia and acidosis synergistically impair coagulation in human whole blood. Anesth Analg. 2008;106(6):1627–32.
Faraoni D, Goobie SM. The efficacy of antifibrinolytic drugs in children undergoing noncardiac surgery: a systematic review of the literature. Anesth Analg. 2014;118(3):628–36.
Goobie SM, Faraoni D. Tranexamic acid and perioperative bleeding in children: what do we still need to know? Curr Opin Anaesthesiol. 2019;32(3):343–52.
Hauser CJ, Boffard K, Dutton R, et al. Results of the CONTROL trial: efficacy and safety of recombinant activated factor VII in the management of refractory traumatic hemorrhage. J Trauma. 2010;69(3):489–500.
Hwu RS, Spinella PC, Keller MS, Baker D, Wallendorf M, Leonard JC. The effect of massive transfusion protocol implementation on pediatric trauma care. Transfusion. 2016;56(11):2712–9.
Karam O, Russell RT, Stricker P, Vogel AM, et al. Recommendations on RBC transfusion in critically ill children with nonlife-threatening bleeding or hemorrhagic shock from the pediatric critical care transfusion and anemia expertise initiative. Pediatr Crit Care Med. 2018;19(9S Suppl 1):S127–S32.
Leeper CM, Yazer MH, Cladis FP, Saladino R, Triulzi DJ, Gaines BA. Use of uncrossmatched cold-stored whole blood in injured children with hemorrhagic shock. JAMA Pediatr. 2018;172(5):491–2.
Leeper CM, Yazer MH, Triulzi DJ, Neal MD, Gaines BA. Whole blood is superior to component transfusion for injured children: a propensity matched analysis. Ann Surg. 2020;272(4):590–4.
Neff LP, Cannon JW, Morrison JJ, Edwards MJ, Spinella PC, Borgman MA. Clearly defining pediatric massive transfusion: cutting through the fog and friction with combat data. J Trauma Acute Care Surg. 2015;78(1):22–9.
Nellis ME, Saini A, Spinella PC, et al. Pediatric plasma and platelet transfusions on extracorporeal membrane oxygenation: a subgroup analysis of two large international point-prevalence studies and the role of local guidelines. Pediatr Crit Care Med. 2020;21(3):267–75.
New HV, Berryman J, Bolton-Maggs PHB, et al. Guidelines on transfusion for fetuses, neonates and older children. Br J Haematol. 2016;175(5):784–828.
Ning S, Solh Z, Arnold DM, Morin PA. Premedication for the prevention of nonhemolytic transfusion reactions: a systematic review and meta-analysis. Transfusion (Philadelphia, Pa). 2019;59(12):3609–16.
Noland DK, Apelt N, Greenwell C, Tweed J, Notrica DM, Garcia NM, et al. Massive transfusion in pediatric trauma: an ATOMAC perspective. J Pediatr Surg. 2019;54(2):345–9.
Oakley FD, Woods M, Arnold S, Young PP. Transfusion reactions in pediatric compared with adult patients: a look at rate, reaction type, and associated products. Transfusion. 2015;55(3):563–70.
Puetz JMD, Witmer CMD, Huang Y-SVMS, Raffini LMD. Widespread use of fresh frozen plasma in us children’s hospitals despite limited evidence demonstrating a beneficial effect. J Pediatr. 2012;160(2):210–5.e1.
Rosenfeld E, Lau P, Zhang W, Russell RT, Shah SR, Naik-Mathuria B, et al. Defining massive transfusion in civilian pediatric trauma. J Pediatr Surg. 2019;54(5):975–9.
Sandler SG, Eder AF, Goldman M, Winters JL. The entity of immunoglobulin A-related anaphylactic transfusion reactions is not evidence based: the entity of IgA-related anaphylactic transfusion reactions is not evidence based. Transfusion (Philadelphia, Pa). 2015;55(1):199–204.
Sehdev M, Grigorian A, Kuza C, Dolich M, Borazjani B, Lekawa M, et al. Comparing unbalanced and balanced ratios of blood products in massive transfusion to pediatric trauma patients: effects on mortality and outcomes. Eur J Trauma Emerg Surg. 2022;48(1):179–86.
Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. The Lancet (British Edition). 2010;376(9734):23–32.
Vlaar AP, Binnekade JM, Prins D, et al. Risk factors and outcome of transfusion-related acute lung injury in the critically ill: a nested case-control study. Crit Care Med. 2010;38(3):771–8.
Vogel AM, Radwan ZA, Cox CS Jr, Cotton BA. Admission rapid thrombelastography delivers real-time “actionable” data in pediatric trauma. J Pediatr Surg. 2013;48(6):1371–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mehl, S.C., Vogel, A.M. (2022). Coagulation and Transfusion Medicine. In: Mattei, P. (eds) Fundamentals of Pediatric Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-07524-7_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-07524-7_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07523-0
Online ISBN: 978-3-031-07524-7
eBook Packages: MedicineMedicine (R0)