Abstract
The majority of recent research data has underlined that diet influences the serum lipid profile, especially triglycerides (TGs), total cholesterol (TC), low-density lipoproteins (LDL), high-density lipoproteins (HDL), and very-low-density lipoproteins (VLDL), lipid peroxidation (LPO), and a number of other parameters such as apolipoproteins (Apo), lipoprotein a (LP(a)), C-reactive protein, systolic blood pressure (SBP), diastolic blood pressure (DBP), etc., having a direct impact on human health. In the above context, there is a scientific viewpoint about the association of Mediterranean diet with serum markers of lipids and human health. The Mediterranean dietary pattern is characterized by an abundant use of olive oil; a high consumption of plant-based foods (fruits, vegetables, legumes, grains, nuts, seeds, etc.); frequent but moderate wine consumption (mainly red) at meals; moderate intake of fish, seafood, fermented dairy products (yogurt, cheese, milk), poultry, and eggs; and reduced consumption of red meat, processed meat products, and also sweets.
Several studies, including the most recent meta-analyses, show that the traditional Mediterranean diet, defined as the dietary pattern of the individuals that live around the Mediterranean Sea in the 1960s, may be the most effective dietary pattern with protective effect on chronic diseases (cardiovascular, obesity, metabolic syndrome, etc.) attributed to the association of the above type of diet with serum markers of lipids. Taking this for granted, researchers indicated health benefits related to possible positive changes on serum markers of lipids, in people with a high adherence to the Mediterranean dietary pattern, while higher risk of chronic diseases correlated with the possible adverse effects of serum lipid markers in those with a low adherence to the above type of diet. In addition, it is necessary to explain more the relationship of Mediterranean diet adherence with serum markers of lipids and consequently the health outcomes with a view to laying a solid foundation for further research on this topic in the future.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Mediterranean diet adherence
- Health effect
- Serum markers of lipids
- Health outcomes
- Cardiovascular diseases
Introduction
Serum Lipid Profile
The major lipids present in the plasma are fatty acids, TGs, cholesterol, and phospholipids and other lipid-soluble substances, present in much smaller amounts (Burdge and Calder 2015). More specifically, serum lipid profile is a pattern of lipids in the blood, typically including the levels of TC, HDL-C, the calculated LDL-C, VLDL-C, and TGs. Along with the above lipid profile, it should be noted and a number of other parameters (total lipids, Apo, LP(a), etc.) for its most complete description and analysis (Orozco-Beltran et al. 2017).
Association of Serum Lipid Profile with Human Health
Numerous studies worldwide have clearly indicated that the abnormal levels of serum lipids are associated with a high risk of appearance of various chronic diseases. Dyslipidemia is a disorder characterized by abnormal amounts of blood lipids and lipoproteins and one of the top five major risk factors leading to cardiovascular disorders (Ding et al. 2016). A great example is that a part of incidents with cardiovascular diseases globally is related not only to high blood cholesterol levels but also to the form of lipoproteins, as oxidized and very-low-density lipoproteins are more atherogenic, independently whether cholesterol levels are increased (Vincent-Baudry et al. 2005).
Particularly, elevated LDL-C and TGs and decreased concentrations of HDL-C are associated with an increased risk of coronary heart disease and atherosclerosis (Yuan et al. 2007). Apart from cardiovascular diseases, diabetes (owing to abnormal blood sugar levels) and obesity (due to high blood cholesterol levels) are associated with aggravated lipid profile, concluding that an adverse lipid profile is related to the induction of a large part of disease states (Franz et al. 2003; Dallongeville et al. 2007).
Influence of Lipid Profile by Environmental Factors, Such as Nutritional Attitudes
Undoubtedly, a normal serum lipid profile implies the improved host health. The formation of serum markers of lipids in general population that is extremely associated with health is influenced not only by genetic background (Pires et al. 2016) but also by a plethora of environmental parameters related to the general lifestyle. In the last decades, various secondary factors such as lifestyle, social, economic, and mainly dietary factors have been investigated as possible parameters with a significant effect on specific biomarkers, especially glucose levels, serum markers of lipids, postprandial state, etc. They have also been correlated with obesity, cancer, diabetes, and cardiovascular disease (Puolakka et al. 2016). The above factors are of high significance in individuals with elevated serum lipids (Harada-Shiba et al. 2018).
Focusing on dietary factors, a vertical increase of various chronic diseases has occurred in recent years due to the high adherence to Western type of diet that is associated with a high risk of dyslipidemia, accompanied by a decrease of HDL-C and a raise in TC, LDL-C, and VLDL-C levels (Sadakane et al. 2008; Sialvera et al. 2012). Thus, care should be taken to avoid unhealthy eating habits, limiting the appearance of negative health outcomes associated with dyslipidemia which is an index of abnormal serum markers of lipids. A healthy diet adherence combined with a balanced lifestyle is a significant strategic treatment for non-normal blood lipids that are negatively associated with human health (Yoon 2014).
Particularly, research data clarifies the crucial role of a balanced diet based on the Mediterranean dietary pattern with a wide variety of dietary nutrients derived from the consumption of specific functional foods, including also a decreased intake of saturated fat, low cholesterol and simple sugar consumption, and a high intake of complex carbohydrates without reducing protein intake, in order to regulate the serum markers of lipids and thus prevent dyslipidemia or other pathological conditions. This protective effect may be associated with a decreased risk of atherosclerosis or other cardiovascular disease development (Kwiterovich Jr 2008).
Association of Dietary Nutrients (Fats, Carbohydrates, Proteins, Fibers, and Antioxidants) with Serum Lipid Profile
A large part of studies has been conducted in order to investigate the association of different dietary nutrients with lipid profile (Reiner et al. 2011). The mechanisms of nutrient effect on serum lipids are indicated below:
Fats
Although previous recommendations about the dietary treatment of hypercholesterolemia focused on the decrease of total dietary fats to less than 30% of daily calories, this strategy did not bring the expected results in improving the lipid profile. Also the replacing of fats with carbohydrates tends to reduce the HDL levels, inducing hypertriglyceridemia (Howard et al. 2006), and diets rich in fats raise the total intake of calories, increasing the risk of various diseases such as obesity and atherosclerosis (Fletcher et al. 2005; Mensink et al. 2003). Taking into account the above data, it is observed that the most important factor which in turn affects the lipid profile is the composition of fat intake with emphasis on mono-unsaturated fats as they are associated with positive changes on serum markers of lipids (Hu et al. 2001).
Saturated Fatty Acids
Saturated fats contained in red meat, butter, or dairy products (milk, yogurt, and cheese) are dietary nutrients with an active effect on the LDL-C levels, because they increase the amount of cholesterol in all lipoprotein fractions when they replace other dietary fatty acids or carbohydrates. A significant element is that the increase or decrease by 1% of caloric intake of saturated fats leads to increase or decrease respectively by 2% of LDL. The main fats in order for hypercholesterolemic activity are myristic (C14:0), palmitic (C16:0, and lauric (C12:0). It is also noted that a reduction of dietary fat intake has a beneficial effect on serum lipid profile, especially when accompanied by weight loss where required (Hu et al. 2001; Muller et al. 2003).
Polyunsaturated Fatty Acids
Omega-3 polyunsaturated fatty acids contained in fish and fish oils have a protective effect against coronary heart disease and sudden death. Their benefits have a wide range and relate to lipid metabolism, lipoproteins, arterial contractility, endothelial function, and mechanisms of atherogenic process. Furthermore, omega-3 fatty acids have antiseptic and anti-inflammatory action, with docosahexaenoic acid and eicosapentaenoic acid to reduce the blood triglyceride concentrations but no low-density lipoprotein cholesterol levels. In addition to omega-3s, omega-6s are also included in polyunsaturated fatty acids and contained mainly in vegetable oils. Replacing saturated fats by omega-6 fatty acids (especially by linoleic acid: C18:2) leads to decreased LDL levels and also reduced HDL concentrations which should normally be high at increased levels. In general, n-6 polyunsaturated and n-3 polyunsaturated fatty acids have beneficial effect on serum markers of lipids which in turn may be associated with a low risk of numerous chronic diseases (Sabate and Ratzin-Turner 2001).
Monounsaturated Fatty Acids
Research data has shown that when monounsaturated acids, mainly oleic acid (C18:1) contained in olive oil, replace the dietary saturated fatty acids, there is a significant reduction of TC and LDL-C levels and blood triglyceride concentrations (Mensink et al. 2003). Also, oleic acid is the only monounsaturated fatty acid that is considered nutritionally significant. Common sources of oleic acid are olive and canola oil, as well as nuts. It has been proved that monounsaturated fats may reduce susceptibility of LDL to oxidation (Koutelidakis and Dimou 2016).
Furthermore, the action of monounsaturated fatty acids (cis-isomers) in HDL-C is influenced by the total fat intake, and the levels of HDL-C are raised when the high intake of monounsaturated fat (>15%) is accompanied by moderate total intake (≈30%). On the other hand, the high total fat intake (>35% of the total kcal) does not seem to influence or increase slightly HDL-C concentrations when it is combined with a high intake of monounsaturated fatty acids (>15%). In the case of trans-isomers (resulting from industrial hydrogenation of the unsaturated fatty acids with the aim of solidifying and containing them in milk, butter, and beef fat), their effects are completely different and coincide with the effects of saturated fats as they increase the levels of LDL and decrease the concentrations of HDL, taking them at a level of 3 and 6% of the total consumed, respectively (Rosa Cde et al. 2015).
Dietary Cholesterol
Dietary cholesterol increases the TC/HDL-C ratio and also the levels of LDL-C but to a lesser extent than saturated fats (especially an increase of 25 mg leads to an increase of 1 mg/dl). Almost whether the dietary cholesterol intake exceeds the limit of 500 mg per day, the response of serum levels decreases, referring to individuals with normal sensitivity to dietary cholesterol due to the compensatory mechanisms developed in endogenous production. Also extremely important is the synergistic effect of saturated fats and dietary cholesterol on the increase of LDL-C levels, inducing the appearance of chronic diseases, most notably atherosclerosis (De Caterina et al. 2006; Fletcher et al. 2005).
Carbohydrates
The role of carbohydrates in serum lipid profile varies depending on the type of nutrient it replaces. When carbohydrates are consumed in place of saturated fats, they generally reduce the LDL-C levels. However, when replacement is not gradual, hypertriglyceridemia can be observed owing to the increased composition of VLDL-C and reduced lipoprotein lipase activity (decreased chylomicron catabolism and VLDL-C). Moreover, the type of carbohydrates that will replace fat (simple, complex, or fiber) is of great importance for the outcome of the lipid profile, with particular preference to a high consumption of complex carbohydrates or fiber that is more efficient in improving it (Ma et al. 2006).
Proteins
Generally, the role of protein intake is relatively neutral in terms of lipoprotein levels. Some studies conclude that low-fat diets decrease the risk of cardiovascular diseases (coronary heart disease, etc.) as they improve dyslipidemia (abnormal blood lipid concentrations). Also, the above results are due to the low intake of animal fat and not to the reduction of protein itself (Rosa Cde et al. 2015).
Fibers
The water-soluble fibers seem to have an effect in fat absorption and in serum cholesterol levels owing to the absorption of fatty acids, cholesterol, and bile acids in the fibers, their inability to form micelles to be absorbed by the small intestine, and their excretion through the feces or their degradation by colon bacteria. Depending on these mechanisms, on the one hand, the resorption of bile acids and reduced cholesterol synthesis are required, and on the other hand the production of propionic acid by bacteria inhibits the cholesterol synthesis. Thus, a decrease of TC and LDL-C levels and especially an increase of plant water-soluble fibers by 5–10 mg per day can reduce the low-density cholesterol by 5%. Some of the most efficient soluble fibers are psyllium, pectins, guar gum, oatmeal and then oat bran, or soybean fiber, while the bran of corn, wheat, and rice do not have a significant effect on serum lipid profile (Rosa Cde et al. 2015).
Also, soluble dietary fibers including pectin from apples and citrus fruits, beta-glucans from oat and barley, and the fibers of flax and barley are well investigated as factors that decrease serum LDL-C. Cholesterol reduction is attributed to the binding of bile acids and inhibition of cholesterol synthesis. As fiber pass through the gastrointestinal system, it may create complexes which bind bile acids, transferring them from the intestines to the rest of the gastrointestinal tract. This process reduces the formation of bile acid micelles that are responsible for the absorption of cholesterol, preventing cholesterol absorption (Koutelidakis and Dimou 2016).
Research data has not proven until now the effect of these insoluble fibers on lipid profile. It should be noted that food consumed provide a mixture of soluble and insoluble fibers, and so the adequate consumption of fruits, vegetables, and whole grains can contribute to the improvement of hypercholesterolemia. Simultaneously, a high-fiber and low-fat meal is less energy dense with lower fat or added sugars, reducing the risk of chronic disease appearance (Anderson and Woodend 2003).
Furthermore, whole grain products may have a beneficial effect on serum markers of lipids. In particular, a meta-analysis showed an inverse association between TC, LDL-C (reduced), and HDL-C (increased), after consumption of glucans (oat, barley, and other functional foods). An additional meta-analysis proved that intake of 2–10 g per day of dietary soluble fiber from oats resulted in a small but important decrease of TC and LDL (Koutelidakis and Dimou 2016).
Antioxidants
A variety of antioxidants such as vitamins, minerals, carotenoids, and polyphenols have the ability to neutralize free radicals and reduce the LDL-C oxidation, improving the serum lipid profile and thus possibly acting as protective factors against mainly cardiovascular diseases. Nevertheless, further research should be conducted to draw safer conclusions about the effect of these dietary nutrients on the serum lipid profile (Dragsted et al. 2006; De Madeco Goncalves Fronta et al. 2010; Jenkins et al. 2011).
The Mediterranean Diet and Serum Markers of Lipids
Definition and Main Characteristics of the Mediterranean Diet
The Mediterranean diet is a dietary model that is consistent with the above dietary recommendations for the treatment of various abnormal lipid concentrations in the blood plasma. The above traditional dietary type refers to specific food consumption patterns typical of some Mediterranean regions in the early 1960s, such as Spain, southern Italy, Crete, and other parts of Greece (Elmaliklis et al. 2019). Generally, the traditional Mediterranean diet is characterized by a high consumption of olive oil, fruits, vegetables, cereals, potatoes, nuts, legumes, and lean fish; a moderate consumption of milk, dairy products, poultry, and red wine; and finally a low consumption of red meat (Lampropoulou et al. 2020). In this dietary model, the most basic foods are olive oil, which is the main component of this diet and is a rich source of unsaturated fats, and also cereals and nuts, which are typically Mediterranean foods with a high content of nutrients, antioxidants, phytochemicals, and polyunsaturated fats.
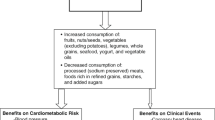
Τhis dietary pattern consists of:
-
Daily consumption of non-refined cereals and products (whole grain bread, pasta, brown rice, etc.), vegetables (2–3 servings/day), fruits (6 servings/day), olive oil (as the main added fat component), and dairy products (1–2 servings/day, of which yogurt and cheese intake is higher than milk consumption)
-
Weekly consumption of fish (4–5 servings/week), poultry (3–4 servings/week), and olives, pulses, and nuts (3 servings/week)
-
Monthly consumption of red meat and meat products (4–5 servings/month) (Dontas et al. 2007) (Fig. 1)
The traditional healthy Mediterranean diet pyramid (Roycor 2017)
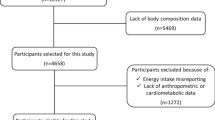
Interaction of the Mediterranean Diet Adherence with Various Biomarkers (Including Lipid Markers) and Consequently Health Outcomes
The above dietary pattern has been recognized as a possible protective factor against various diseases, mainly in the prevention of cardiovascular diseases (Trichopoulou et al. 2009). Until now research data has demonstrated a possible protective effect of various specific functional foods included to the Mediterranean diet against atherosclerotic process and thus cardiovascular disease development.
Particularly, specific functional foods of the Mediterranean diet such as olive oil, honey, fruits (citrus fruits, pomegranate, grapes, berries), vegetables (tomatoes, cauliflower, broccoli, crumbled vegetables), wild greens (fennel, radish), and herbs (oregano, mint, salvia, sage, verbena, mountain tea) may have a positive effect on cardiovascular disease prevention, owing to the bioactive compounds of the above types of foods, as phytochemicals and polyphenols, such as oleuropein, resveratrol, sulforaphane, anthocyanins, quercetin, tannins, etc. Possible mechanisms of their action encompass improving serum lipid profile, endothelial factors, thrombotic factors, etc. Recent scientific data indicated that the Mediterranean diet adherence may be a significant health-promoting dietary approach for people of all ages (Koutelidakis and Dimou 2016).
In human subjects, a great part of studies indicated that a higher compliance with the Mediterranean diet was related to a higher physical activity, a lower body mass index and psychological stress or psychological disorders (anxiety and depression), fewer subclinical atherosclerosis markers, improved metabolic biomarkers, and better blood pressure regulation and serum lipid profile. Understanding all the above information about individuals adhering to the Mediterranean diet, people’s Mediterranean dietary habits in combination with a healthy lifestyle is of high importance to regulating serum markers of lipids, having thus positive health outcomes, and reducing pathological conditions associated with an abnormal lipid profile (Farajian and Zampelas 2015).
The main purpose of this chapter was to extend reliable scientific evidence about the association of Mediterranean diet adherence with the serum markers of lipids for its in-depth analysis and understanding.
Summary of Research Findings About the Effect of the Mediterranean Diet on Serum Lipid Profile and Health
Lyon Diet Heart Study
Researchers from the Lyon Diet Heart Study examining 605 patients aged 55–80 years with a history of myocardial infarction indicated the benefits of the Mediterranean diet extended to the secondary prevention of cardiovascular disease owing to improved serum lipid profile influenced by the above dietary type. In particular, volunteers with a high Mediterranean diet adherence had 50–70% lower risk of recurrent heart disease relative to those with a low adherence to this diet. According to the above findings, the potential significance of the Mediterranean dietary model compared with other recommended diets was attributed to the positive effect of the above diet on basic parameters of serum lipids, especially a decrease of TC, LDL-C, and TGs and conversely an increase of HDL-C, reducing thus the risk of cardiovascular or other severe chronic diseases (De Lorgeril et al. 1999).
HALE Study
The HALE study which was conducted on a sample of 2339 people (1507 men and 832 women) aged 70–90 years found that participants who did not follow a low-risk lifestyle, characterized by Mediterranean dietary habits, moderate alcohol consumption, increased physical activity, and abstinence from smoking, were at a greater risk of coronary heart disease and generally cardiovascular diseases. This higher risk was attributed to the adverse lipid profile of these individuals owing to their unbalanced eating habits, while the lower risk of the above diseases was associated with an improved serum lipid profile related to Mediterranean diet adherence and healthful lifestyle (Knoops et al. 2004).
ATTICA Study
In the same year, another research demonstrated a significant association of Mediterranean diet with serum lipid profile. Particularly in ATTICA study of 2282 individuals, 1128 men and 1154 women (aged >18 years old) from Greece, researchers observed that volunteers who adopted the Mediterranean diet and received statin had on average 9% lower TC, 19% lower LDL-C concentrations, and 32% lower oxidized LDL-C levels relative to those who were untreated and followed a Westernized diet, concluding on the one hand a beneficial lipid profile in volunteers with a high Mediterranean diet adherence and on the other hand an unhealthy serum lipid profile in those with a low Mediterranean dietary adherence who consumed foods found in Western dietary pattern (Panagiotakos et al. 2004).
The above results were in accordance with the findings of another research in 3042 healthy participants (1514 men and 1528 women) without clinical evidence of cardiovascular disease selected from the Attica area of Greece. The objective of this study was to investigate the effect of the Mediterranean diet on the total antioxidant capacity. According to the results, volunteers who were more adherent to the Mediterranean diet had on average 11% higher total antioxidant capacity levels relative to participants with a lower adherence to the above dietary pattern. Also, the total antioxidant capacity was positively related to the consumption of olive oil and fruit and vegetables, whereas it was inversely correlated with the intake of red meat. An additional finding was that participants with the highest Mediterranean diet adherence had on average 19% lower oxidized LDL-C levels compared with those with the lowest. Therefore, greater adherence to the Mediterranean diet is associated with elevated total antioxidant capacity levels and a low oxidized LDL-C concentration, which may explain the beneficial role of this diet on the cardiovascular system (Pitsavos et al. 2005).
Medi-RIVAGE Study
A similar type of research, especially the Medi-RIVAGE study in 212 volunteers of moderate risk for cardiovascular diseases, comparing a 3-month dietary intervention with the Mediterranean diet and low-fat diet concluded that serum lipid profile, body mass index, and glucose levels were decreased in both cases, but the cardiovascular risk reduction forecast reached 15% for the Mediterranean diet versus 9% for the low-fat diet. Through the above results after a 3-month Mediterranean diet intervention, there were significant changes on the serum lipid profile, decreasing possibly the risk of cardiovascular diseases (Vincent-Baudry et al. 2005).
Randomized Controlled Trials
In a further 3-month dietary intervention study, 772 individuals divided into 3 groups followed the Mediterranean diet (either with a high intake of olive oil or nuts) and a similar type of low-fat diet. The two types of diets based on Mediterranean dietary patterns were associated with a statistically significant improvement in serum lipid profile and glucose levels compared to the third group, in which it is worth noting that such intensive nutritional training had not been done. Therefore, a balanced diet based on Mediterranean dietary pattern and supplemented with olive oil or nuts may lead to a reduction in cardiovascular disease appearance owing to the positive effect of the above diet on significant parameters of serum lipids (Estruch et al. 2006).
372 subjects at a high cardiovascular risk (210 women and 162 men, aged 55–80 years) who were recruited into a large, multicenter, randomized, controlled, parallel-group clinical trial directed at testing the efficacy of the traditional Mediterranean diet on the primary prevention of coronary heart disease were assigned to a low-fat diet or 1 of the 2 traditional Mediterranean types of diets (traditional Mediterranean diet + virgin olive oil or traditional Mediterranean diet + nuts). After the 3-month intervention, there were significant changes, especially decreased oxidized LDL-C concentrations in the traditional Mediterranean diet + virgin olive oil group, while there were no changes on serum lipid profile in the low-fat diet group. Therefore, significant reductions in cellular lipid levels and LDL-C levels were observed in individuals at a high cardiovascular risk who improved their diet toward a traditional Mediterranean dietary pattern (Fito et al. 2007).
A randomized parallel controlled-feeding trial was conducted in 60 non-diabetics with mild abdominal obesity. After a two-week run-in with a diet high in saturated fatty acids, subjects were allocated a monounsaturated fat-rich diet, a Mediterranean diet, or a high saturated fat diet, for 8 weeks. The adherence to monounsaturated fat diet and the Mediterranean diet did not influence fasting insulin levels, but the high monounsaturated fat diet decreased TC and LDL-C relative to the high saturated fat diet and alongside the Mediterranean diet increased HDL-C levels, conversely reducing the TC/HDL-C ratio compared with the high monounsaturated fat diet. Consequently, replacing a high saturated fat diet with a high monounsaturated fat diet or a Mediterranean diet improved serum markers of lipids, with the Mediterranean diet being the most effective (Bos et al. 2010).
Taking into account the previous research that has identified several metabolites related to the Mediterranean dietary pattern, knowledge about longitudinal changes in metabolic biomarkers after a Mediterranean diet intervention is quite limited. A subsample of 48 firefighters cluster-randomized trial at Indianapolis fire stations was randomly selected for the metabolomics study at 12 months of follow-up, where Group 1 (n = 24) continued for further 6 months in a self-sustained Mediterranean diet intervention and Group 2 (n = 24), the control group at that time, began with an active Mediterranean diet intervention for 6 months. At the two times points, a total of 225 metabolites were examined. The Mediterranean diet intervention was associated with significant changes in biomarkers related to lipid metabolism, including decreased LDL-C, ApoB/ApoA1 ratio, remnant cholesterol, and VLDL-C and conversely greater HDL-C and better lipoprotein composition. In general, this intervention induces modest changes in adherence to the Mediterranean diet and consequently in metabolic biomarkers (Sotos-Prieto et al. 2020).
Comparative Study
The Seven Countries Study of 12,763 middle-aged men selected from 16 cohorts around the world underlined the protective effect of the Mediterranean dietary pattern against atherosclerosis that can be partially attributed to the decrease of blood pressure levels. A great part of the scientific community has recently associated the Mediterranean diet with improvements in blood lipid profile, reduced oxidation of lipids, and decreased risk of thrombosis (i.e., fibrinogen levels), all changes meaning improvement in endothelial function (Kromhout et al. 2018).
BioCycle Study
In the BioCycle Study (a prospective cohort study of menstrual cycle function) conducted between 2005 and 2007, 259 healthy premenopausal women, aged 18–44 years from western New York, were followed for 1 (n = 9) or 2 (n = 250) menstrual cycles, investigating in those whether Mediterranean diet adherence was associated with lower lipid peroxidation levels. Adherence to the Mediterranean dietary pattern has been correlated with a reduction in LPO levels and higher ascorbic acid concentrations, decreasing the risk of cardiovascular diseases and total mortality.
Crossover Design Studies
In a crossover design after a 4-week run-in period with a healthy diet, eligible candidates were randomized into three diet sequences, with a common background diet enriched with virgin olive oil, walnuts, or almonds, lasting 4 weeks each. As regards the results, there were significant changes in serum lipid profile and oxidation and inflammation markers. In 18 volunteers who completed the study, low-density lipoprotein cholesterol was decreased from baseline by 7.3%, 10.8%, and 13.4% after the virgin olive oil, walnut, and almond diets, respectively, and corresponding reduction results were observed about the TC and LDL-C/HDL-C ratio. However, there were no changes in other lipid fractions, oxidation analytes, or inflammation biomarkers. All the above findings in of hypercholesterolemic patients showed that the consumption of virgin olive oil, walnuts, or almonds that are basic components of the Mediterranean diet was extremely significant to improve specific parameters of serum lipids (Damasceno et al. 2011).
A randomized, controlled, crossover design compared the effect of a Mediterranean diet with three to four daily servings of dairy (MedDairy) and a low-fat (LF) control diet on significant biomarkers (including serum markers of lipids) associated with cardiovascular diseases. Forty-one volunteers aged ≥45 years and at risk of cardiovascular disease were randomly allocated to their first dietary intervention, either the MedDairy or low-fat diet, following each intervention for 8 weeks, with an 8-week washout period separated interventions. According to the main observations of this research, compared with the low-fat intervention, the MedDairy intervention resulted in a significantly lower morning SBP, lower morning DBP and clinic SBP, significantly greater HDL-C levels, lower TG concentrations, and also lower ratio of TC to HDL-C. Nevertheless there were no statistically significant effects on CRP, plasma glucose, and serum insulin. In general, the conclusion following a Mediterranean diet with additional dairy foods led to significant positive changes in various markers of cardiovascular diseases, mainly serum lipids (Wade et al. 2018).
Cross-Sectional Study
A cross-sectional analysis was conducted on the data from 1290 volunteers of the Aragon Workers Health Study cohort, examining the effect of a Mediterranean dietary pattern, high in vegetables, fruits, fish, white meat, nuts, and olive oil, and a Western diet, high in red meat and fast and refined food. Compared with the participants in the lowest quintile of Western-type adherence, those in the highest quintile had 4.6 mg/dl lower HDL-C, lower ApoA1 concentrations, and a higher risk of having reduced HDL-C. On the contrary volunteers with a high Mediterranean diet adherence had 3.3 mg/dl higher HDL-C levels and 0.43 times lower ratio of TGs to HDL. Thus, it was obvious that the Mediterranean diet adherence is positively associated with plasma lipids, while the adherence to Western dietary pattern was related to abnormal serum markers of lipids (Penalvo et al. 2015).
PREDIMED Sub-study
A sub-study of the PREDIMED (Prevention with Mediterranean Diet) trial in 1139 volunteers with a high cardiovascular risk also aimed to analyze the relationship of polyphenol intake from a Mediterranean diet, measured by polyphenol extraction, with circulating inflammatory biomarkers and cardiovascular risk factors in elderly people. The main findings of the present research indicated that participants in the highest tertile of changes in urinary polyphenol excretion were associated with lower plasma inflammatory biomarkers such as IL6, TNF-a and other parameters compared with those in the lowest tertile. In addition, systolic and diastolic blood pressure decreased, and conversely plasma HDL-C increased in parallel with increasing urinary polyphenol excretion. Therefore, high polyphenol intake from the Mediterranean dietary pattern was correlated not only with decreased inflammatory biomarkers but also improved markers of serum lipid profile (Medina-Remon et al. 2017).
Retrospective Observational Study
A retrospective observational study was performed in 31 children with dyslipidemia (aged 3–14 years) to investigate a possible association between nutritional habits or a general lifestyle based on Mediterranean dietary pattern and serum lipid levels (TC, LCL-C, HDL-C, TGs, ApoA1, ApoB, and LP(a)). From this research, although there was no statistically significant correlation between children’s serum lipid levels and Mediterranean diet compliance, breakfast consumption, and consumption of fruits, vegetables, fresh juices, desserts, and sodas, some parameters of serum lipids differed significantly. More specifically, children with increased physical activity had lower triglyceride levels relative to those with lower physical activity. Also, children who consumed only one meal per day had increased levels of TC, LDL-C, ApoB, and LP(a), compared with those who consumed more than three meals per day. Another significant association was that children who were breastfed less than 6 months had significantly increased LDL-C levels relative to children who were breastfed more than 6 months. Therefore, there is a correlation of general healthy dietary habits with specific parameters of lipid profile (Lampropoulou et al. 2020) (Table 1).
Functional Foods of the Mediterranean Diet with a Beneficial Effect on Serum Markers of Lipids
In the context of the Mediterranean diet, specific functional foods proved to have physiological health benefits, decreasing the risk of various chronic diseases apart from their basic nutritional functions. Most constituents of some typically Mediterranean foods with functional value are associated with long-term mitigation of certain diseases, while there are also some perceived to increase short-term well-being. Furthermore, nutraceutical of these types of foods is an additional term that has been lately used to define foods that can be used as means to promote health and protect against diseases (Johnston 2009).
Studies in human or non-human subjects indicate the importance of specific conventional or processed functional food intake within a Mediterranean dietary pattern, for the prevention of cardiovascular diseases; this effect is measured by specific biomarkers mainly serum lipids levels, as the abundance of bioactive compounds seems to have a positive effect on new or more functional goals of the human body, with a huge benefit for its health. Oleic acid, dietary fibers such as pectins, beta-glucans, and inulin; phytosterols; monounsaturated and polyunsaturated fatty acids; antioxidant vitamins and minerals; antioxidants; phytochemicals; and bioactive peptides are characterized as the basic functional components with protective effects against various pathological conditions of the host. The compliance with a diet based on Mediterranean dietary pattern characterized by a high consumption of several functional food categories or types, especially fruits and vegetables (wild greens, soy, pomegranate, olive oil, cranberries, garlic tomatoes, grapes, etc.), whole grains, nuts, fishes, red wine, herb drinks, and fortified foods (enriched with vitamins and minerals), may be significantly associated with the improvement of serum markers of lipids related to the human health status. Some of the typically functional foods from the Mediterranean diet with beneficial effects on serum lipid profile are listed in Table 2 (Koutelidakis and Dimou 2016).
Further Analyze the Significance of Specific Mediterranean Foods with Functional Value in Regulating the Serum Lipid Profile
Olive Oil
It is widely known that olive oil is a main fat component of the Mediterranean diet and contains an abundance of bioactive compounds, mainly oleic acid and polyphenols, with significant health benefits related to its positive effect on serum markers of lipids. In a randomized controlled trial, a basic finding was that a balanced diet based on Mediterranean dietary pattern with 30 grams (g) olive oil per day led to a statistically significant reduction in levels of SBP, TC, TGs, LDL-C, and VLDL-C. The above results indicated that olive oil may have a beneficial effect on specific parameters of lipid profile, reducing the risk of various chronic diseases (Atefi et al. 2018).
Fruits and Vegetables
A main characteristic of the Mediterranean dietary pattern is the high consumption of fruits and vegetables. In the last years, there is an increased interest from the scientific community to investigate the positive interaction of these foods with a significant potential to decrease several chronic diseases, mainly cardiovascular diseases. Until now, the possible mechanism of the above correlation is that fruits and vegetables may protect LDL-C from oxidation (Aburto et al. 2013). Also the high content of them in vitamins, minerals and micronutrients, beta-glucans, fibers (psyllium) that act together synergistically leads to inhibition of cholesterol synthesis and reduced LDL-C levels. Also in a randomized placebo-controlled double-blind clinical trial with a sample of 151 patients on hemodialysis, a main observation was the role of vitamin C supplementation contained in fruits with a view to reducing the CRP concentrations (Biniaz et al. 2014) and decreasing the LDL-C levels (Aguirre and May 2008).
Carotenoids (lycopene and beta-carotene) that are contained in carrots, tomatoes, and dark-green vegetables decrease oxidative stress in vivo. Moreover, healthy adults’ intake of two cups per day of tomato juice for 2 weeks led to a reduction in plasma levels of CRP and TNF. In an additional group of patients with grade-1 hypertension, a high intake of tomato extract for approximately 1 month reduced systolic and diastolic blood in plasma and LDL-C concentrations. Also bioactive compounds, mainly polyphenols (tannins, lignins, and flavonoids), found generally in fruits and vegetables may have a beneficial effect on various biomarkers, including the serum lipid profile (Puglisi et al. 2008; Koutelidakis 2015).
Pomegranate
A typical example of food rich in polyphenols is pomegranate, a traditional Greek functional food belonging to the Mediterranean diet. The high content of pomegranate polyphenols may be related to the reduction in blood pressure and triglyceride concentrations and conversely an increase of high-density lipoprotein cholesterol (Shema-Didi et al. 2014). Another fruit rich in bioactive compounds with beneficial effects on serum lipid profile is cranberry. Particularly research data has proven that cranberry intake (either whole fruit or its juice) may be significantly associated with a decrease of LDL-C levels and conversely an increase of HDL-C concentrations, preventing cardiovascular diseases (Zikria et al. 2010).
Raisins
The scientific community elaborates on the significance of Mediterranean raisins, focusing especially on indigenous Greek varieties (e.g., Zante currants), widely known in food industry due to their high functional value attributed to their rich content in bioactive compounds (Papadaki et al. 2021). Particularly the above variety of raisins is a significant source of dietary fibers and polyphenols that may decrease cardiovascular disease risk by influencing lipoprotein and inflammation. The above functional food is included to the traditional Mediterranean diet, and its consumption based on study findings is related to reduced SBP, TC, and LDL-C levels and decreased TNF-a. Thus, research data indicates that simple lifestyle modifications such as adding raisins to a balanced diet may have beneficial effect on serum markers of lipids, lowering the risk of appearance of various chronic diseases (atherosclerosis, coronary heart disease, etc.) (Puglisi et al. 2008).
Wild Greens
Wild greens (fennel, radish) are among typical Mediterranean foods that belong to the category of vegetable with a high functional value. These foods may have a protective effect against atherosclerotic process and thus cardiovascular disease development. This protective effect is due to the bioactive compounds of these foods, including phytochemicals and polyphenols such as sulforaphane, pectin, quercetin, etc. Possible mechanisms of their action include improving endothelial factors, thrombotic factors, and serum lipid profile (Lampropoulou et al. 2020).
Aromatic Plants and Essential Oils
The abundance of aromatic plants, such as oregano, mint, rosemary, sage, garlic, onion, etc., found in Mediterranean diet has been investigated in recent years for their possible health benefits owing to the bioactive components (oleuropein, resveratrol, quercetin, sulforaphane, anthocyanins, tannins, etc.,) of those functional foods. The possible effect of aromatic plants may be the result of either their polyphenolic extract or their essential oils. Essential oils and their constituents have been demonstrated to have a high antioxidant activity, protecting against LDL-C oxidation. Furthermore essential oils of several food components in the Mediterranean diet, of plant origin, are rich in phenolic compounds, lowering the concentrations of total cholesterol and triglycerides (Koutelidakis and Dimou 2016).
Fish and Fish Oil
One of the main foods that are included to the Mediterranean diet is fish, which is a major food source of long-chain n-3 polyunsaturated fatty acids (including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)) that contribute to lowering blood pressure and decreasing also plasma triglyceride and low-density lipoprotein cholesterol levels (Mozaffarian 2008). Apart from fish, the intake of fish oil supplements inhibits hepatic triglyceride secretion and contributes to clearance of triglyceride in plasma, having thus a positive effect on serum markers of lipids (Ueeda et al. 2008).
Nuts and Walnuts
Apart from fish that was previously analyzed as a source of polyunsaturated fatty acids, there are other functional foods found in the Mediterranean diet with a high content of the above dietary nutrient. Particularly nuts (almonds, etc.) are traditional Mediterranean foods rich in polyunsaturated fats, having a possible beneficial effect on serum markers of lipids. Research data showed that an almond-based diet led to a reduction in TC and LDL-C while preserving HDL-C concentrations (Spiller et al. 1998). Also recent epidemiological studies provide an evidence of favorable effect of nut consumption on serum lipid profile, as the primary mechanism by which nuts prevent from various diseases (cardiovascular diseases, etc.) is through improvement of lipid and apolipoprotein profile (Altamimi et al. 2020).
Undoubtedly frequent consumption of nuts was correlated with improved serum lipid profile and lowered risk of cardiovascular diseases. In order to explore more the above association, researchers investigated the role of walnut intake on serum lipids and blood pressure. The main finding of this research was that the long-term consumption of walnuts inhibited the serum levels of TC and also decreased the LDL-C/HDL-C ratio due to the higher reduction of LDL-C than HDL-C, induced by this food (Sabate et al. 1993).
Mushrooms
Mushrooms have functional value and are included to the Mediterranean diet. Several studies in human and non-human subjects indicated that dietary intake of specific mushroom species contributed to the decrease of serum lipid levels. Particularly diets containing shiitake mushroom decrease serum lipids and serum lipophilic antioxidant capacity in rats (Yu et al. 2016). Also a research showed the lipid-lowering effects of oyster mushroom (Pleurotus ostreatus) in humans, as the treatment with oyster mushroom soup led to a significant decrease of oxidized LDL-C levels and a significant tendency in lowering TC concentrations (Schneider et al. 2011).
Dairy Products
Although a great part of researchers have supported the correlation of full-fat dairy product consumption with an increased risk of cardiovascular diseases, there is a scientific viewpoint that the intake of low-fat dairy products, which belong to “light category” (functional foods for specified nutritional uses), in parallel with a balanced diet based on Mediterranean dietary pattern, is proposed to consumers with a high risk of cardiovascular diseases, with a view to managing their body weight and improving their serum markers of lipids. More specifically, in a clinical study, an adolescent who consumed 2 liters of skim milk per day for 3 weeks appeared to have a reduction in levels of plasma cholesterol and LDL-C, relative to those who consumed full-cream milk or yogurt (Rossouw et al. 1981).
Another research showed that daily consumption of 200 ml of a functional yogurt may have a beneficial effect on serum markers of lipids associated with cardiovascular diseases (Agerbaek et al. 1995). As an extension of the above information, in general the daily consumption of dairy products (yogurt, fermented milk, etc.) with a high content of probiotics and other beneficial bioactive compounds in permitted quantities defined according to the Mediterranean diet may lead to an improved lipid profile with a positive impact on human health (Koutelidakis 2015).
Herb Drinks (Green Tea, Et Cetera)
In the nutritional recommendations based on the Mediterranean dietary pattern, it is proposed to replace soft drinks with other functional drinks such as herb drinks. In this category there is a wide variety of teas; mainly green tea is rich in catechins (especially epigallocatechin) that are extremely effective as lipid-lowering factors by inhibiting significant steps in the intestinal absorption of dietary fat, cholesterol, and other lipids. According to recent research findings, the biological role of tea on serum lipid profile is a main result of its antioxidant effect (attenuation of low-density lipoprotein oxidation) and of its possible effect on the expression of specific genes with the ability to regulate various metabolic pathways associated with various chronic diseases (Koutelidakis 2015).
Another research examined the effect of green tea on postprandial levels of plasma total antioxidant capacity (TAC), serum lipids, CRP, and glucose in patients with cardiovascular disease. The most significant observation was the increase in TAC at 1.5 and 3 h after breakfast with tea and the decrease in serum uric acid at 1.5 h after breakfast with tea. Thus, frequent consumption of tea may have a beneficial effect on specific markers of lipids associated with human health (Koutelidakis et al. 2014).
Red Wine
According to the dietary recommendation based on the Mediterranean dietary pattern, there is a permitted daily amount of red wine consumption (especially 100 ml per day for women and 200 ml per day for men). A prospective randomized trial was performed from 2009 to 2011 in 108 patients with carotid atherosclerosis in order to investigate whether a daily glass of red wine associated with lifestyle changes improves the serum lipid profile of the above volunteers. After this dietary intervention, there was a significant reduction in low-density lipoprotein cholesterol levels and also a decrease of LDL-C/HDL-C ratio. Additional significant reductions were obvious in the concentrations of total cholesterol and triglycerides (Droste et al. 2013).
Application to Prognosis, Other Diseases, or Conditions
Applications to Prognosis
In this chapter the major blood plasma lipids (TC, TGs, VLDL-C, LDL-C, HDL-C, etc.) (Burdge and Calder 2015) have been reviewed which together show remarkable correlations with various chronic diseases. In particular dyslipidemias are disorders characterized by abnormal amounts of serum lipids (decrease of HDL-C, possible increase of TC, VLDL, and LDL levels) which are considered to be one of the most significant modifiable risk factors for cardiovascular diseases (Rizvi and Nagra 2014). Diagnosis, management, and treatment of dyslipidemias are of high importance with a view to preventing atherosclerosis and decreasing the incidence of cardiovascular diseases (coronary artery disease, etc.), a leading cause of mortality in adulthood. It is possible that serum lipid biomarkers may be used clinically in investigating prognosis in patients (Lampropoulou et al. 2020).
Applications to Other Diseases or Conditions
In this chapter we review an analytical platform for rapidly determining serum lipid status. Application of this methodology suggests that there is an aggravated serum lipid profile in patients with cardiovascular diseases (Rizvi and Nagra 2014). Several socioeconomic factors have been related to disorders of lipid levels in adults, such as increased screen time, reduced physical activity, lower socioeconomic status, shorter sleep duration, and unbalanced diet. The primary treatment of dyslipidemia in adults includes healthy lifestyle, increased physical activity, and balanced diet based on Mediterranean dietary pattern. More specifically Mediterranean dietary habits, such as low consumption of sugar-sweetened beverages, saturated fat, and high-calorie products and conversely an increased intake of complex carbohydrates and functional foods (fruits, vegetables, whole grains, olive oil, flaxseed, nuts, fishes, fortified foods enriched with phytosterols, vitamins, minerals, and antioxidants) improve serum lipid levels, reducing the risk not only of cardiovascular diseases (Koutelidakis and Dimou 2016) but also of obesity, metabolic diseases, and diabetes (Lampropoulou et al. 2020) which in turn are associated with abnormal blood plasma lipid biomarkers (Franz et al. 2003; Dallongeville et al. 2007).
Mini-dictionary of Terms
-
Apolipoproteins: Proteins that bind lipids to form lipoproteins, whose main function is to transport lipids.
-
Blood lipids: Lipids in the blood, either free or bound to other molecules.
-
Cholesterol: The main representative of sterols, free or esterified with a fatty acid, and alongside it is a basic component of cell membranes and a precursor molecule of many steroids in the body.
-
Chylomicrons: Ultra-low-density lipoproteins that transport food lipids from the small intestine to the tissues.
-
HDL: High-density lipoprotein that transports cholesterol from the tissues to the liver.
-
Intermediate-density lipoproteins VLDL: Intermediated products of VLDL metabolism.
-
LDL: Low-density lipoprotein that transports cholesterol from the liver to tissues.
-
Lipids: Heterogeneous group of molecules that share the common property of hydrophobicity as they are insoluble in water, but soluble in fat solvents, having a great significance in the human organism (storage of energy, constituents of cell membrane, constituents of neural tissue, as an insulator and protective coating, and as vitamins).
-
Lipoproteins: Spherical complexes of lipids and proteins that transport a great part of lipids and fat-soluble vitamins to and from tissues and also contain the core of hydrophobic lipids surrounded hydrophilic lipids and proteins.
-
Phospholipids: A class of lipids whose molecule has a hydrophilic “head” containing a phosphate group and two hydrophobic “tails” derived from fatty acids, joined by a glycerol molecule.
-
TGs: Glycerol esters with fatty acids and present in the blood to enable the bidirectional transference of adipose fat and blood glucose from the liver.
-
VLDL: Very-low-density lipoprotein for transport of endogenously synthesized fat to tissues.
Key Facts
Key Facts of Dyslipidemia
-
Dyslipidemia is one of the top five major risk factors leading to cardiovascular disorders.
-
It is a disorder characterized by abnormal amounts of serum lipids.
-
The main characteristics of dyslipidemia are high TC, TGs, and LDL-C and conversely low HLD-C.
-
The prevalence of the above disorder in early age shows a large increase in recent years worldwide and increases further when various factors coexist, such as obesity, low physical activity, unbalanced diet, unhealthy lifestyle, etc.
-
The rates of dyslipidemia and mortality from diseases associated with this disorder may be reduced through a high degree of adherence to the Mediterranean diet, as compliance with the recommendations of this dietary pattern can improve serum lipid profile, decreasing TC, TGs, and LDL-C and increasing HDL-C.
Summary Points
-
Various biomarkers especially serum lipid profile (TC, LDL-C, VLDL-C, HDL-C, TGs, Apo, LPO, etc.) are influenced not only by genetic background of individuals but also environmental factors, mainly their nutritional habits.
-
There is a large part of clinical and epidemiological studies about the effect of fiber, unsaturated fatty acids, and other nutritional habits based on Mediterranean dietary pattern on reduced levels of TC, LDL-C or VLDL-C, LPO, TGs, interleukins, TNF, or other inflammatory markers and conversely an increased HDL-C and ApoA1.
-
A high Mediterranean diet adherence may have a positive effect on serum markers of lipids and health benefits, while low compliance with the above dietary model is possibly associated with negative health outcomes, owing to its negative changes on the lipid profile.
-
Further research is needed to confirm the possible effect of specific foods, especially fruits and vegetables (almonds, wild greens, tomatoes, pomegranate), whole grains (psyllium, oat), nuts, flaxseed, olive oil, beverages (tea and aromatic plant extracts, red wine), and fortified foods (with phytochemicals, polyphenols, vitamins, minerals, etc.) included to the Mediterranean diet adherence on serum markers of lipids.
-
In the context of Mediterranean diet, the consumption of conventional functional foods, super foods, and processed novel functional foods from the industry, rich in bioactive compounds, is of high importance to design nutritional policies and promote healthy nutritional habits, improving the serum lipid profile.
Abbreviations
- Apo (A1):
-
Apolipoprotein A1
- Apo (B):
-
Apolipoprotein B
- C12:0:
-
Lauric acid
- C14:0:
-
Myristic acid
- C16:0:
-
Palmitic acid
- CRP:
-
C-reactive protein
- DBP:
-
Diastolic blood pressure
- DHA:
-
Docosahexaenoic acid
- EPA:
-
Eicosapentaenoic acid
- HDL:
-
High-density lipoprotein
- IDL:
-
Intermediate-density lipoprotein
- LDL:
-
Low-density lipoprotein
- LF:
-
Low fat
- LP(a):
-
Lipoprotein (a)
- LPO:
-
Lipid peroxidation
- SBP:
-
Systolic blood pressure
- SDLDL:
-
Small dense low-density lipoprotein
- TAC:
-
Total antioxidant capacity
- TC:
-
Total cholesterol
- TGs:
-
Triglycerides
- VLDL:
-
Very-low-density lipoprotein
References
Aburto JN, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. https://doi.org/10.1136/bmj.f1378.
Agerbaek M, Gerdes LU, Richelsen B. Hypocholesterolaemic effect of a new fermented milk product in healthy middle-aged men. Eur J Clin Nutr. 1995;49:346–52.
Aguirre R, May JM. Inflammation in the vascular bed: importance of vitamin C. Pharmacol Ther. 2008;119:96–103. https://doi.org/10.1016/j.pharmthera.2008.05.002.
Altamimi M, Zidan S, Badrasawi M. Effect of three nuts consumption on serum lipid profile in hyperlipidemic individuals: a systematic review. Nutr Metab Insights. 2020;13:1178638820926521. https://doi.org/10.1177/1178638820926521.
Anderson GH, Woodend D. Effect of glycemic carbohydrates on short-term satiety and food intake. Nutr Rev. 2003;61:17–26. https://doi.org/10.1301/nr.2003.may.S17-S26.
Atefi M, Pisbdad GR, Fagbib S. Canola oil and olive oil impact on lipid profile and blood pressure in women with type 2 diabetes: a randomized, controlled trial. Progress Nutr. 2018;20:102–9. https://doi.org/10.23751/pn.v20il-S.5854.
Biniaz V, Shermeh MS, Edabi A, et al. Effect of vitamin C supplementation on C-reactive protein levels in patients undergoing hemodialysis: a randomized double blind, placebo-controlled study. Nephrourol Monthly. 2014;6:e13351. https://doi.org/10.5812/numonthly.13351.
Bos MB, de Vries JHM, Feskens EJM, et al. Effect of high monounsaturated fatty acids diet and a Mediterranean diet on serum lipids and insulin sensitivity in adults with mild abdominal obesity. Nutr Metab Cardiovasc Dis. 2010;20:591–8. https://doi.org/10.1016/j.numecd.2009.05.008.
Burdge GC, Calder PC. Introduction to fatty acids and lipids. In: Calder PC, et al., editors. Intravenous lipid emulsions. World Rev Nutr Diet, vol. 112. Basel: Karger; 2015. p. 111–6. https://doi.org/10.1159/000365423.
Dallongeville J, Gruson E, Dallinga-Thie G, et al. Effect of weight loss on the postprandial response to high -fat and high-carbohydrate meals in obese women. Eur J Clin Nutr. 2007;61:711–8. https://doi.org/10.1038/sj.ejcn.1602603.
Damasceno NRT, Perez-Heras A, Serra M, et al. Crossover study of diets enriched with virgin olive oil, walnuts or almonds. Effects on lipids and other cardiovascular risk markers. Nutr Metab Cardiovasc Dis. 2011;21:14–20. https://doi.org/10.1016/j.numecd.2010.12.006.
De Caterina R, Zampolli A, Del Turco S. Nutritional mechanisms that influence cardiovascular disease. Am J Clin Nutr. 2006;83:421–6. https://doi.org/10.1093/ajcn/83.2.421S.
De Lorgeril M, Salen P, Martin JL, et al. Mediterranean diet, traditional risk factors and the rate of cardiovascular complications after myocardial infarction. Final report of the Lyon Heart Study. Circulation. 1999;99:779–85. https://doi.org/10.1161/01.CIR.99.6.779.
De Madeco Goncalves Fronta K, Matias ACG, Areas JAG. Influence of food components on lipid metabolism: scenarios and perspectives on the control and prevention of dyslipidemias. Food Sci Technol. 2010;30. https://doi.org/10.1590/S0101-20612010000500002.
Ding W, Cheng H, Yan Y, et al. 10-year trends in serum lipid levels and dyslipidemia among children and adolescents from several schools in Beijing, China. J Epidemiol. 2016;26:637–45. https://doi.org/10.2188/jea.JE20140252.
Dontas AS, Zerefos NS, Panagiotakos DB, et al. Mediterranean diet and prevention of coronary heart disease in the elderly. Clin Interv Aging. 2007;2:109–15. https://doi.org/10.2147/ciia.2007.2.1.109.
Dragsted LO, Krath B, Ravn-Haren G, et al. Biological effect of fruits and vegetables. Proc Nutr Soc. 2006;65:61–7. https://doi.org/10.1079/pns2005480.
Droste DW, Iliescu C, Vaillant M, et al. A daily glass of red wine associated with lifestyle changes independently improves blood lipids in patients with carotid arteriosclerosis: results from a randomized controlled trial. Nutr J. 2013;12:art147.
Elmaliklis IN, Liveri A, Ntelis B, et al. Increased functional foods’ consumption and Mediterranean diet adherence may have a protective effect in the appearance of gastrointestinal diseases: a case-control study. Medicines. 2019;6:50. https://doi.org/10.3390/medicines6020050.
Estruch R, Martinez-Gonzalez MA, Corella D, et al. Effects of Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11. https://doi.org/10.7326/0003-4819-145-1-200607040-00004.
Farajian P, Zampelas A. Chapter 7 – Mediterranean diet in children and adolescents. In: Watson VPR, editor. The Mediterranean diet: an evidence-based approach. 1st ed. Elsevier; 2015. p. 69–80. https://doi.org/10.1016/B978-0-12-407849-9.00007-5.
Fito M, Guxens M, Corella D, et al. Effect of a traditional Mediterranean diet on lipoprotein oxidation. A randomized controlled trial. Arch Intern Med. 2007;167:1195–203. https://doi.org/10.1001/archinte.167.11.1195.
Fletcher B, Berra K, Ades P, et al. AHA scientific statement: managing abnormal blood lipids. Circulation. 2005;112:3184–209. https://doi.org/10.1161/CIRCULATIONAHA.105.169180.
Franz MJ, Bantle JP, Beebe CA, et al. ADA: evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003;26:51–61. https://doi.org/10.2337/diacare.26.2007.s51.
Harada-Shiba M, Arai H, Ishigaki Y, et al. Working group by Japan atherosclerosis society for making guidance of familial hypercholesterolemia. Guidelines for diagnosis and treatment of familial hypercholesterolemia. J Atheroscler Thromb. 2018;25:751–70. https://doi.org/10.5551/jat.CR003.
Howard BV, Van Horn L, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: the women’s health initiative randomized controlled dietary modification trial. JAMA. 2006;295:655–66. https://doi.org/10.1001/jama.295.6.655.
Hu FB, Manson JE, Willet WC. Types of fat and risk of coronary heart disease: a critical review. J Am Coll Nutr. 2001;20:5–19. https://doi.org/10.1080/07315724.2001.10719008.
Jenkins DJA, Srichaikul K, Mirrahimi A, et al. Functional foods to increase the efficacy of diet in lowering serum cholesterol. Can J Cardiol. 2011;27:397–400. https://doi.org/10.1016/j.cjca.2011.03.008.
Johnston C. Functional foods as modifiers of cardiovascular disease. Am J Lifestyle Med. 2009;3:39–43. https://doi.org/10.1177/1559827609332320.
Knoops KT, de Grout LC, Kromhout D, et al. Mediterranean diet, lifestyle factors and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–9. https://doi.org/10.1001/jama.292.12.1433.
Koutelidakis AE. In: Ziti, editor. Functional foods: their role on health promotion. Thessaloniki, Greece; 2015.
Koutelidakis A, Dimou C. The effects of functional food and bioactive compounds on biomarkers of cardiovascular diseases. In: Martirosyan D, editor. Functional foods text book, 1st edn. 2016. p 89–117.
Koutelidakis AE, Rallidis L, Koniari K, et al. Effect of green tea on postprandial antioxidant capacity, serum lipids, C-reactive protein and glucose levels in patients with coronary artery disease. Eur J Nutr. 2014;53:479–86. https://doi.org/10.1007/s00394-013-0548-0.
Kromhout D, Menotti A, Alberti-Fidanza A, et al. Comparative ecologic relationships of saturated fat, sucrose, food groups, and a Mediterranean food pattern score to 50-year coronary heart disease mortality rates among 16 cohorts of the Seven countries study. Eur J Clin Nutr. 2018;72:1103–10. https://doi.org/10.1038/s41430-018-0183-1.
Kwiterovich PO Jr. Recognition and management of dyslipidemia in children and adolescents. J Clin Endocrinol Metab. 2008;93:4200–9. https://doi.org/10.1210/jc.2008-1270.
Lampropoulou M, Chaini M, Rigopoulos N, et al. Association between serum lipid levels in Greek children with dyslipidemia and Mediterranean diet adherence, dietary habits, lifestyle and family socioeconomics factors. Nutrients. 2020;12:1600. https://doi.org/10.3390/nu12061600.
Ma Y, Li Y, Chiriboga DE, et al. Association between carbohydrate intake and serum lipids. J Am Coll Nutr. 2006;25:155–63. https://doi.org/10.1080/07315724.2006.10719527.
Medina-Remon A, Casas R, Tressera-Rimbau A, et al. Polyphenol intake from a Mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a sub-study of the PREDIMED trial. Bri J Clin Pharmacol. 2017;83:114–28. https://doi.org/10.1111/bcp.12986.
Mensink R, Zock P, Kester A, et al. Effects of dietary fat acids and carbohydrates on the ratio of total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146–55. https://doi.org/10.1093/ajcn/77.5.1146.
Mozaffarian D. Fish and n-3 fatty acids for the prevention of fatal coronary heart disease and sudden cardial health. Am J Clin Nutr. 2008;87:1991–6. https://doi.org/10.1093/ajcn/87.6.1991S.
Muller H, Lindsman A, Brantsaeter A, et al. The serum LDL/HDL cholesterol ratio is influenced more favorably by exchanging saturated fat in the diet of women. J Nutr. 2003;133:78–83. https://doi.org/10.1093/jn/133.1.78.
Orozco-Beltran D, Gil-Guillen V, Redon J, et al. Lipid profile, cardiovascular disease and mortality in a Mediterranean high-risk population: the ESCARVAL-RISK study. PLoS One. 2017;12:e0186196. https://doi.org/10.1371/journal.pone.0186196.
Panagiotakos DB, Pitsavos C, Christhood C. Status and management of blood lipids in Greek adults and their relation to socio-demographic, lifestyle and dietary factors: the Attica study blood lipids distribution in Greece. Atherosclerosis. 2004;173:353–61. https://doi.org/10.1016/j.atherosclerosis.2003.12.031.
Papadaki A, Kachrimanidou V, Lappa IK, et al. Mediterranean raisins / currants as traditional superfoods: processing, health benefits, food applications and future trends within the bio-economy era. Appl Sci. 2021;11:1605. https://doi.org/10.3390/app11041605.
Penalvo JL, Oliva B, Sotos-Prieto M, et al. Greater adherence to a Mediterranean dietary pattern is associated with improved plasma lipid profile: the Aragon Health Workers study cohort. Rev Esp Cardiol. 2015;68:290–7. https://doi.org/10.1016/j.rec.2014.09.019.
Pires A, Sena C, Seic R. Dyslipidemia and cardiovascular changes in children. Curr Opin Cardiol. 2016;31:95–100. https://doi.org/10.1097/HCO.0000000000000249.
Pitsavos C, Panagiotakos DB, Tzima N, et al. Adherence to the Mediterranean diet is associated with total antioxidant capacity in healthy adults: the Attica study. Am J Clin Nutr. 2005;82:694–9. https://doi.org/10.1093/acjn.82.3.694.
Puglisi MJ, Vaishnav U, Shrestha S, et al. Raisins and additional walking have distinct effects on plasma lipids and inflammatory cytokines. Lipids Health Dis. 2008;7:14. https://doi.org/10.1186/1476-511X-7-14.
Puolakka E, Pahkala K, Laitinen T, et al. Childhood socioeconomic status in predicting metabolic syndrome and glycose abnormalities in adulthood: the cardiovascular risk in young Finns study. Diabetes Care. 2016;39:2311–7. https://doi.org/10.2337/dc16-1565.
Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2011;32:1769–818. https://doi.org/10.1093/eurheartj/ehr158.
Rizvi NB, Nagra SA. Introduction: Lipid profile. In: Minerals and lipids profiles in cardiovascular disorders in south Asia. 1st ed. Berlin/Heidelberg: Springer; 2014. p. 9–11. https://doi.org/10.1007/978-3-642-34249-3_2.
Rosa Cde O, Dos Santos CA, Leite JI, et al. Impact of nutrients and food components on dyslipidemias: what is the evidence? Adv Nutr. 2015;6:703–11. https://doi.org/10.3945/an.115.009480.
Rossouw JE, Burger EM, Der Vyver PV, et al. The effect of skim milk, yoghurt, and full cream milk on human serum lipids. Am J Clin Nutr. 1981;34:351–6. https://doi.org/10.1093/ajcn/34.3.351.
Roycor A. The Mediterranean diet pyramid. 2017. Available online: http://www.mediterraneandiet.com/oldways-diets-pyramids/the-mediterranean-diet-pyramid/. Accessed 31 Mar 2021.
Sabate J, Ratzin-Turner R. Vegetarian nutrition. 1st ed. Boca Raton: CRC Press; 2001.
Sabate J, Fraser GE, Burke K, et al. Effects of walnuts on serum lipid levels and blood pressure in normal men. N Engl J Med. 1993;328:603–7. https://doi.org/10.1056/NEJM199303043280902.
Sadakane A, Tsutsumi A, Gotoh T, et al. Dietary patterns and levels of blood pressure and serum lipids in a Japanese population. J Epidemiol. 2008;18:58–67. https://doi.org/10.2188/jea.18.58.
Schneider I, Kressel G, Meyer A, et al. Lipid lowering effects of oyster mushroom (Pleurotus ostreatus) in humans. J Function Foods. 2011;3:17–24. https://doi.org/10.1016/j.jff.2010.11.004.
Shema-Didi L, Kristal B, Sela S, et al. Does pomegranate intake attenuate cardiovascular risk factors in hemodialysis patients? Nutr J. 2014;13:18. https://doi.org/10.1186/1475-2891-13-18.
Sialvera TE, Pounis GD, Koutelidakis AE, et al. Phytosterols supplementation decreases plasma small and dense LDL levels in metabolic syndrome patients on westernized type diet. Nutr Metab Cardiovasc Dis. 2012;22:843–8. https://doi.org/10.1016/j.numecd.2010.12.004.
Sotos-Prieto M, Ruiz-Canela M, Song Y, et al. The effects of a Mediterranean diet intervention on targeted plasma metabolic biomarkers among US firefighters: a pilot cluster-randomized trial. Nutrients. 2020;12:3610. https://doi.org/10.3390/nu12123610.
Spiller GA, Jenkins DA, Bosello O, et al. Nuts and plasma lipids: an almond-based diet lowers LDL-C while preserving HDL-C. J Am Coll Nutr. 1998;17:285–90. https://doi.org/10.1080/07315724.1998.10718761.
Trichopoulou A, Bamia C, Trichopoulos D. Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study. BMJ. 2009;338:b2337. https://doi.org/10.1136/bmj.b2337.
Ueeda M, Doumei T, Takaya Y, et al. Serum N-3 polyunsaturated fatty acid levels correlate with the extent of coronary plaques and calcifications in patients with acute myocardial infarction. Circ J. 2008;72:1836–43. https://doi.org/10.1253/circj.CJ-08-0249.
Vincent-Baudry S, Defoort C, Gerber M, et al. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or low fat diet. Am J Clin Nutr. 2005;82:964–71. https://doi.org/10.1093/ajcn/82.5.964.
Wade AT, Davis CR, Dyer KA, et al. A Mediterranean diet supplemented with dairy foods improves markers of cardiovascular risk: results from the MedDairy randomized controlled trial. Am J Clin Nutr. 2018;108:1166–82. https://doi.org/10.1093/ajcn/nqy207.
Yoon JM. Dyslipidemia in children and adolescents: when and how to diagnose and treat? Pediatr Gastroenterol Hepatol Nutr. 2014;17:85–92. https://doi.org/10.5223/pghn.2014.17.2.85.
Yu S, Wu X, Ferguson M, et al. Diets containing shiitake mushroom reduce serum lipids and serum lipophilic antioxidant capacity in rats. J Nutr. 2016;146:2491. https://doi.org/10.3945/jn.116.239806.
Yuan G, Al-Shali KZ, Hegele RA, et al. Hypertriglyceridemia: its etiology, effects and treatment. CMAJ. 2007;176:1113–20. https://doi.org/10.1503/cmaj.060963.
Zikria M, Goldman R, Ansell J. Cranberry juice and warfarin: when bad publicity trumps science. Am J Med. 2010;123:384–92. https://doi.org/10.1016/j.amjmed.2009.08.019.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this entry
Cite this entry
Elmaliklis, IN., Koutelidakis, A. (2022). Mediterranean Diet Adherence and Serum Markers of Lipids. In: Patel, V.B., Preedy, V.R. (eds) Biomarkers in Nutrition . Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Cham. https://doi.org/10.1007/978-3-031-07389-2_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-07389-2_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07388-5
Online ISBN: 978-3-031-07389-2
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences