Abstract
Severe gut motility disorders are characterized by ineffective propulsion of intestinal contents. As a result, patients often develop extremely uncomfortable symptoms, ranging from nausea and vomiting along with alterations of bowel habits, up to radiologically confirmed subobstructive episodes. Chronic intestinal pseudo-obstruction (CIPO) is a typical clinical phenotype of severe gut dysmotility due to morphological and functional alterations of the intrinsic (enteric) innervation and extrinsic nerve supply (hence neuropathy), interstitial cells of Cajal (ICCs) (mesenchymopathy), and smooth muscle cells (myopathy). In this chapter, we highlight some molecular mechanisms of CIPO and review the clinical phenotypes and the genetics of the different types of CIPO. Specifically, we will detail the role of some of the most representative genetic mutations involving RAD21, LIG3, and ACTG2 to provide a better understanding of CIPO and related underlying neuropathic or myopathic histopathological abnormalities. This knowledge may unveil targeted strategies to better manage patients with such severe disease.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Chronic intestinal pseudo-obstruction
- Enteric neurons
- Enteric neuropathy
- Neurogenetics
- Severe gut dysfunction
2.1 Introduction
Severe gut dysmotility is a clinical condition characterized by a major impairment of intestinal propulsion due to changes of various key cells, such as enteric neurons and/or glial cells, interstitial cells of Cajal (ICCs), and smooth muscle cells of GI tract [6]. In very few cases, the functional impairment of digestive neuro-ICC-muscular integrated systems is so pronounced to hinder oral feeding leading to severe symptoms, which markedly compromise patients’ quality of life. CIPO is a clinical phenotype of severe gut dysmotility usually with poor prognosis.
Patients with CIPO typically manifest with recurrent intestinal subocclusive episodes and clinical /radiological findings mimicking mechanical obstruction [5, 24]. In addition to the acute subobstructive phases, during the intercrisis period, patients complain of a variety of symptoms (e.g., chronic nausea, vomiting, abdominal distension, and constipation/diarrhea) requiring nutritional support to avoid weight loss and malnutrition [7]. Treatment options for CIPO are essentially aimed at preventing malnutrition (by providing adequate caloric intake), restore motility (via prokinetic/enterokinetic pharmacological agents), and control symptoms, for example, abdominal pain, nausea/vomiting, and diarrhea (often ascribable to bacterial overgrowth). Taken together, these options might allow for stabilization of the clinical picture at best, but certainly do not target the mechanisms underlying CIPO. The lack of established animal models, which could provide a basis for a better understanding of the molecular pathways contributing to neuro-ICC-myopathy underlying CIPO, is hindering preventative approaches and effective treatments. Highlighting molecular mechanisms of CIPO can be a strategy to decipher its clinical complexity, simplify the wide heterogeneity inherent to this condition, and ultimately pave the way to new treatment options. Herein, we review the clinical phenotypes and the genetics of the different types of CIPO with the goal of providing answers for a better understanding of severe dysmotility and related histopathological abnormalities with a special emphasis on neuro-myopathy.
2.2 Genetics of CIPO
In recent years, we and other groups have provided evidence for a genetic basis of the enteric neuronal and/or smooth muscle degeneration and loss observed in specific forms of CIPO. The discovery of novel genes mutated in different patients represents the first step in identifying the downstream molecular impairment in CIPO. The genes so far identified in CIPO patients are summarized in Table 2.1. An in-depth study of these gene variants in vitro and in vivo is required to understand the role of the different genes identified in the ENS and muscular alterations that can lead to a severe enteric dysmotility, such as CIPO. In the next paragraphs, we will highlight the role of genetic mutations involving RAD21, LIG3, and ACTG2.
2.2.1 RAD21
We identified the homozygous causative variant in a large consanguineous family segregating an autosomal-recessive form of CIPO. The affected family members also presented other clinical features including megaduodenum, long-segment Barrett’s esophagus (up to 18 cm from the squamocolumnar junction or “Z-line”), and cardiac abnormalities of variable severity (OMIM 611376; Mungan syndrome). We performed whole-exome sequencing analysis on the genomic DNA from two affected individuals and found the novel homozygous change c.1864 G>A in RAD21 (NM_006265.2) producing the damaging missense variant p.Ala622Thr [3]. Any derangement to RAD21 molecular structure and function can result in significant changes to many tissues, including the gut neuro-muscular layer. In fact, RAD21 is part of the cohesin complex, involved in pairing and unpairing of sister chromatids during cell replication and division, and also regulates gene expression directly and independently of cell division [13]. The RAD21 subunit of the cohesin complex plays important structural and functional roles, as it serves as physical link between the SMC1/SMC3 (Structural Maintenance of Chromosome 1 and 3) heterodimer and the STAG subunit. RAD21 integrity regulates the association or disassociation of functional cohesin with chromatin and also plays a key role in double-strand breaks DNA repair [1]. Cohesin binds to many sites throughout the genome, in combination with the CCCTC-binding factor (CTCF) insulator protein, which is known to mediate chromatin loop formation. Cohesin colocalizes with CTCF along chromosome arms, cooperating with this protein in the regulation of gene expression and chromatin structure [23]. RAD21 is associated with other transcriptional regulators, such as estrogen receptor-α [8], and the RNA-polymerase-binding complex Mediator [14] in a cell-type-specific manner. In combination with other factors, cohesin selectively binds genes with paused RNA polymerase II and can regulate transcription by determining the amount of elongating RNA polymerase II on genes [18]. Cohesin-mediated chromatin organization plays an important role in the formation/stabilization of chromosome architecture and gene transcription and repression. RAD21 interacts with CTCF and other cohesin-associated proteins to maintain and stabilize multidimensional organizations of topologically associating domains and chromatin loops [12]. In addition, human RAD21 is linked to the apoptotic pathways and RAD21 cleavage can be induced by a broad spectrum of apoptotic stimuli at residue p.Asp279, which is different from the mitotic cleavage sites required for chromosomal segregation [4, 22].
In our study, in vitro and in vivo data (zebrafish model) showed that the mutant RAD21 p.Ala622Thr protein did not activate one of its well-known target genes, that is, RUNX1, which exerts a crucial role for RAD21 function [3]. Moreover, using the zebrafish as a model, we recapitulated the CIPO phenotype observed in patients with the homozygous RAD21 causative variant, in terms of severe impairment of motility and marked reduction of neurons (hence a histopathology pattern reminiscent of an “oligo-neuronal hypoganglionosis”). After injecting a morpholino (mo) specific for the functional ablation of rad21, zebrafish embryos were allowed to develop to 5 days post-fertilization (dpf), when the digestive system has already developed. Control and mo-treated embryos were fed fluorescent beads through microgavage, a technique that allows to determine the rate of intestinal motility as a function of time. After 8 hours post microgavage of fluorescent beads, the GI tract of embryos was divided into four zones based on anatomical landmarks and the presence of fluorescent bead was scored in each segment. Compared to controls, rad21 morphants showed delayed food transit along the gut and a significant depletion of enteric neurons as shown by staining the enteric neurons with antibodies against the neuronal marker HuC/D. The marked reduction of HuC/D-immunolabeled enteric neurons was highly suggestive of a neuropathic impairment responsible for the observed motility impairment (no evidence of any smooth muscle damage in the zebrafish embryos) [3]. Furthermore, Rad21 immunoreactivity was detected in about 43% of HuC/D-immunoreactive myenteric neurons/field of both adult and young mouse small intestine. A subset of ChAT-immunolabeled myenteric neurons was also immunoreactive for Rad21. Rad21 silencing confirmed specificity of the immunolabeled neurons [2]. Following this first evaluation of the normal Rad21 localization in the mouse ENS, and based on the evidence that rad21−/− mice were embryonic lethal [27], we designed and developed a conditional knock-in (KI) mouse with the p.Ala626Thr missense variant (equivalent to the p.Ala622Thr in humans) in order to generate a model reminiscent of the clinical phenotype and histopathological changes in the originally described affected family members. The design of the construct allowed us to selectively drive the p.Ala626Thr variant into the mouse ENS in response to Cre-driven recombination of the floxed alleles by crossing with mice carrying the expression of Cre under the Wnt1 promoter. Compared to wild-type animals, preliminary data on the homozygous mice revealed that there was about 30% reduction of HuC/D myenteric neurons/ganglion in the Rad21KI mice [15], a finding indicative of the CIPO phenotype observed in patients. Also, subsets of HuC/D-IR myenteric neurons of wild-type mouse colon displayed either ChAT-immunoreactivity (43.71 ± 3.45) or nNOS-immunoreactivity (30.84 ± 5.40). However, in the Rad21KI mice, the HuC/D/ChAT-immunoreactive neurons/ganglions were 45.13 ± 4.27, whereas the HuC/D/nNOS-immunoreactive neurons/ganglions were 14.13 ± 1.40 (Bianco, unpublished data). These preliminary data point to an overall reduction of the myenteric neurons with a selective depletion of inhibitory motor neurons in Rad21KI mice, suggesting a role of this gene alteration in gut motility dysfunction. Further studies are currently ongoing to determine the full spectrum of abnormalities caused by the RAD21 mutation.
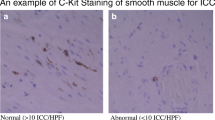
2.2.2 LIG3
We recently characterized another mutant gene underlying CIPO and neurological manifestations (reminiscent of mitochondrial neurogastrointestinal encephalomyopathy, MNGIE) in seven patients from three unrelated families (Bonora 2021 in press). In addition to CIPO, the most prominent and consistent clinical signs were neurological abnormalities, including leukoencephalopathy, epilepsy, migraine, stroke-like episodes, and neurogenic bladder. DNA from these patients was subjected to whole-exome sequencing. Compound heterozygous variants were identified in the gene LIG3 in all patients. All variants were predicted to have a damaging effect on the protein. The LIG3 gene encodes the unique mitochondrial DNA (mtDNA) ligase that binds POLG and plays a pivotal role in mtDNA repair and replication. The study of the consequences of LIG3 mutations was conducted in primary skin fibroblasts derived from patients and in transiently transfected cells expressing the different mutant versus wild-type proteins. All assays showed a severely reduced quantity of LIG3 protein in the mutant cells. In concordance, we demonstrated the lack of ligase activity in the mitochondrial extracts derived from patients’ cells compared to control fibroblasts. The LIG3 gene defects altered the mitochondrial network (Fig. 2.1a), affected mtDNA maintenance, leading to mtDNA depletion without the accumulation of multiple deletions observed in other mitochondrial disorders (e.g., MNGIE) and induced a severe imbalance in cell metabolism, with impaired ATP production and increased mitochondrial reactive oxygen species generation. The resultant mitochondrial dysfunction was key in the causative effects leading to the clinical phenotype observed in these patients. In the gut, the histopathological analysis and neuronal HuC/D immunoreactivity evaluation demonstrated a significant loss of the number of myenteric neurons in the colon (Fig. 2.1b). Likewise, in Rad21, the disruption of lig3 in the zebrafish model reproduced leukoencephalopathy in the brain and impaired gut transit, with an alteration of mitochondrial markers in the mutant models. Biallelic heterozygous loss-of-function variants in the LIG3 gene result therefore in a novel mitochondrial disease characterized by predominant gut dysmotility, encephalopathy, and neuronal abnormalities.
Mitochondrial defects in vitro and ex vivo in presence of LIG3 mutations underlie a severe reduction in ENS neurons. (a) Representative images of 3D z stacks and relative Imaris software reconstruction of the mitochondrial network using MitoTracker green staining. Quantification of mitochondrial network volume represented as the mean isosurface volume per cell (n = 5 pictures/group). A significant decrease in the mitochondrial isosurface volume and green intensity was observed in a patient with biallelic LIG3 mutations (P ≤ 0.001). Scale bars: 5 μm and 25 μm. (b) Histological features of gut (colon) biopsies. HuC/D immunofluorescence (green) in gut tissue biopsies (colon) of controls and patient carrying LIG3 mutations; nuclear staining was obtained with DAPI (blue). Arrows point to labelled myenteric neurons. Myenteric neurons are significantly reduced in the LIG3 mutated patient (right panel, P = 0.0005; Student’s t-test). Scale bar: 50 μm
2.3 Smooth Muscle Actin–Related Diseases: Visceral Myopathy Driven by ACTG2 Mutations
Visceral myopathy (MIM# 155310) causes gut dysmotility due to smooth muscle dysfunction with phenotypes ranging from functional intestinal dysmotility along with massively distended bladder requiring catheterization, a condition also referred to as megacystis-microcolon intestinal hypoperistalsis syndrome (MMIHS), to cases characterized by predominant involvement of the GI tract with typical CIPO features. Causative variants in several genes have been identified in these phenotypes, but the majority of molecularly diagnosed cases are caused by heterozygous variants in ACTG2, resulting in dominant alleles running in families or arising de novo in the affected subjects [17, 25]. In vitro studies of the identified variants have shown an impairment of ACTG2 polymerization and a reduction of smooth muscle cell contractility [10, 11]. In a recent study, the molecular diagnostic rate of visceral myopathy was 64% (34/53), of which 97% (33/34) could be attributed to ACTG2 variants. In particular, missense changes in five conserved arginine residues contributed for 49% (26/53) of disease in the cohort. The ACTG2-negative cases had a more favorable clinical outcome and more restricted disease. In the ACTG2-positive group, the poor outcome (i.e., total parenteral nutrition dependence, need for transplantation, and death) was always due to one of the arginine missense alleles. The analysis of the effect of the specific residues suggests a severity degree of the missense changes, with p.Arg178>p.Arg257>p.Arg40, along with other less frequent variant alleles at p.Arg63 and p.Arg211. Four novel missense variants were also reported, including one that is apparently transmitted according to a recessive mode of inheritance [19], indicating that the overall genetic architecture of visceral myopathy is still to be fully characterized.
Additional genes have been found to play a role in visceral myopathy pathogenesis. ACTA2, encoding for a smooth muscle actin gene, is mutated in the multisystemic smooth muscle dysfunction syndrome (MIM #613834). The clinical features include bladder hypotonicity and abnormal intestinal peristalsis as well as a significant involvement of vascular and ciliary smooth muscle, leading to vascular aneurysms and mydriasis [20]. Autosomal-recessive forms of MMIHS are caused by biallelic loss-of-function variants in genes encoding for proteins involved in actin–myosin interactions, such as MYH11 (myosin heavy chain; [9]), MYLK (myosin-light chain kinase; [10, 11]), LMOD1 (leiomodin 1, an actin-binding protein expressed primarily in vascular and visceral smooth muscles [10, 11]), and MYL9 (regulatory myosin-light chain; [21]).
Several studies have highlighted the alterations in smooth muscle structural proteins and pathways related to smooth muscle function, providing mechanistic insights in the disease etiology. As an example, loss of LMOD1 in vitro and in vivo results in a reduction of filamentous actin, with elongated cytoskeletal dense bodies and impaired intestinal smooth muscle contractility [10, 11].
2.4 Conclusion and Future Perspectives
In this chapter, we have highlighted a possible strategy based on accurate clinical phenotyping followed by histopathology and in-depth molecular (genetic) analysis, which can be used to reconstruct a model to better understand neuro-ICC-muscular changes underlying severe gut dysmotility such as CIPO. Next-generation sequencing (NGS) has now made possible the analysis of multiple genomic regions simultaneously, shortening the time and cost of gene tests. Thus, several studies have unveiled the presence of many independent genes for severe gut dysmotility by adopting this technique (Fig. 2.2). The discovery of additional genes is crucial to identify altered pathways and is paramount for a better understanding of the disease and development of novel therapeutic targets. Moreover, identifying novel genetic factors is crucial to predict who is at risk of developing the disease, allowing for early detection. Regardless of the rates of clinical manifestations within each genetic group, patients with severe gut dysmotility represent difficult medical challenges, with a tremendous impact of the disease on the quality of life, severe clinical complications, and costly medical care, with minimally effective treatments.
STRING analysis of the proteins involved in severe gut dysmotility. The proteins mutated in severe gut dysmotility disorders (red boxes) cluster into two different groups: the myopathic (i.e., ACTG2-related) and/or mitochondrial-related neuro-myopathic forms vs. prevalent enteric neuropathies (i.e., RAD21 related)
Nonetheless, the future is full of exciting promises relying upon the differentiation of human-induced pluripotent stem cells (PSCs) directed to the formation of organoids, physiological three-dimensional human organ cultures [16]. A recent study applied a tissue-engineering approach with embryonic and PSC to generate a human intestinal tissue containing functional ENS. The normal intestinal ENS development was recapitulated in vitro by combining human-PSC-derived neural crest cells and developing human intestinal organoids (HIOs), with migration into the mesenchyme, differentiation into neurons and glial cells, and generation of neuronal activity exhibiting rhythmic waves of calcium transients. The ENS-containing HIOs in vivo formed neuroglial structures in a close fashion to a myenteric and submucosal plexus, contained functional interstitial cells of Cajal, and regulated waves of propagating contraction. Equivalent approach was applied to repopulate with a functional ENS a PHOX2B mutated Hirschsprung disease mouse model [26]. We see this as the dawn of a new era highlighting pluripotent stem cells as possible treatment options for patients with CIPO and broadly with severe gut dysmotility.
References
Bauerschmidt C (2010) Cohesin promotes the repair of ionizing radiation-induced DNA double-strand breaks in replicated chromatin. Nucleic Acids Res 38(2):477–487. https://doi.org/10.1093/nar/gkp976
Bianco F (2018) SJ. Expression of RAD21 immunoreactivity in myenteric neurons of the human and mouse small intestine. Neurogastroenterol Motil 30(9):e13429. https://doi.org/10.1111/nmo
Bonora E (2015) Mutations in RAD21 disrupt regulation of APOB in patients with chronic intestinal pseudo-obstruction. Gastroenterology 148(4):771–782.e11. https://doi.org/10.1053/j.gastro.2014.12.034
Chen F (2002) Caspase proteolysis of the cohesin component RAD21 promotes apoptosis. J Biol Chem 277(19):16775–16781. https://doi.org/10.1074/jbc.M201322200
Cogliandro RF (2011) Patient-reported outcomes and gut dysmotility in functional gastrointestinal disorders. Neurogastroenterol Motil 23:1084–1091. https://doi.org/10.1111/j.1365-2982.2011.01783
De Giorgio R (2004) Advances in our understanding of the pathology of chronic intestinal pseudo-obstruction. Gut 53(11):1549–1552. https://doi.org/10.1136/gut.2004.043968
Di Nardo G (2017) Chronic intestinal pseudo-obstruction in children and adults: diagnosis and therapeutic options. Neurogastroenterol Motil 29:e12945. https://doi.org/10.1111/nmo.12945
Faure AJ (2012) Cohesin regulates tissue-specific expression by stabilizing highly occupied cis-regulatory modules. Genome Res 22(11):2163–2175. https://doi.org/10.1101/gr.136507.111
Gauthier J (2015) A homozygous loss-of-function variant in MYH11 in a case with megacystis-microcolon-intestinal hypoperistalsis syndrome. Eur J Hum Genet 23:1266–1268. https://doi.org/10.1038/ejhg.2014.256
Halim D (2017a) Loss of LMOD1 impairs smooth muscle cytocontractility and causes megacystis microcolon intestinal hypoperistalsis syndrome in humans and mice. Proc Natl Acad Sci U S A 114(13). https://doi.org/10.1073/pnas.1620507114
Halim D (2017b) Loss-of-function variants in MYLK cause recessive megacystis microcolon intestinal hypoperistalsis syndrome. Am J Hum Genet 101:123–129. https://doi.org/10.1016/j.ajhg.2017.05.011
Hansen AS (2017) CTCF and cohesin regulate chromatin loop stability with distinct dynamics. elife 6:e25776. https://doi.org/10.7554/eLife.25776
Horsfield JA (2012) Diverse developmental disorders from the one ring: distinct molecular pathways underlie the cohesinopathies. Front Genet 3:171. https://doi.org/10.3389/fgene.2012.00171
Kagey MH (2010) Mediator and cohesin connect gene expression and chromatin architecture. Nature 467:430–435. https://doi.org/10.1038/nature09380
Lattanzio G (2020) Modeling enteric neuropathy: the rad21 knock-in mouse. Eur J Histochem J Funct Cytol. ISSN 1121-760X volume 64/ supplement 3
Lehmann R (2019) Human organoids: a new dimension in cell biology. Mol Biol Cell 30:1129–1137. https://doi.org/10.1091/mbc.E19-03-0135
Lehtonen HJ (2012) Segregation of a missense variant in enteric smooth muscle actin γ-2 with autosomal dominant familial visceral myopathy. Gastroenterology 143(6):1482–1491.e3. https://doi.org/10.1053/j.gastro.2012.08.045
Mannini L (2015) Mutant cohesin affects RNA polymerase II regulation in Cornelia de Lange syndrome. Sci Rep 19(5):16803. https://doi.org/10.1038/srep16803
Matera I (2020) Novel ACTG2 variants disclose allelic heterogeneity and bi-allelic inheritance in pediatric chronic intestinal pseudo-obstruction. Clin Genet 99(3):430–436. https://doi.org/10.1111/cge.13895
Milewicz DM (2010) De novo ACTA2 mutation causes a novel syndrome of multisystemic smooth muscle dysfunction. Am J Med Genet 152A:2437–2443. https://doi.org/10.1002/ajmg.a.33657
Moreno CA (2018) Homozygous deletion in MYL9 expands the molecular basis of megacystis-microcolon-intestinal hypoperistalsis syndrome. Eur J Hum Genet 26(5):669–675. https://doi.org/10.1038/s41431-017-0055-5
Panigrahi AK (2012) A cohesin-RAD21 interactome. Biochem J 442(3):661–670. https://doi.org/10.1042/BJ20111745
Parelho V (2008) Cohesins functionally associate with CTCF on mammalian chromosome. Cell 132(3):422–433. https://doi.org/10.1016/j.cell.2008.01.011
Stanghellini V (2007) Chronic intestinal pseudo-obstruction: manifestations, natural history and management. Neurogastroenterol Motil 19(6):440–452. https://doi.org/10.1111/j.1365-2982.2007.00902
Wangler MF (2014) A heterozygous de novo and inherited mutations in the smooth muscle actin (ACTG2) gene underlie megacystis-microcolon-intestinal hypoperistalsis syndrome. PLoS Genet 10(3):e1004258
Workman MJ (2017) Human pluripotent-stem-cell-derived intestinal tissues with a functional enteric nervous system. Nat Med 23(1):49–59. https://doi.org/10.1038/nm.4233
Xu H (2010) Rad21-cohesin haploinsufficiency impedes DNA repair and enhances gastrointestinal radiosensitivity in mice. PLoS One 5(8):e12112. https://doi.org/10.1371/journal.pone.0012112
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Bianco, F. et al. (2022). Clinical and Pathological Features of Severe Gut Dysmotility. In: Spencer, N.J., Costa, M., Brierley, S.M. (eds) The Enteric Nervous System II. Advances in Experimental Medicine and Biology, vol 1383. Springer, Cham. https://doi.org/10.1007/978-3-031-05843-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-031-05843-1_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-05842-4
Online ISBN: 978-3-031-05843-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)