Abstract
Approximately 15% of pregnant women are known to have an anxiety disorder. In addition to causing distress to women, studies have highlighted the longstanding impact of untreated maternal anxiety on infant and child outcomes. Whilst many studies have demonstrated that cognitive behavioural approaches using exposure are effective for anxiety disorders, scant evidence exists of their use with pregnant women. Furthermore, women are sometimes denied treatment due to assumptions about the risks involved. This chapter reviews evidence and techniques for the use of exposure-based treatments in pregnancy, presenting case material on the treatment of obsessive-compulsive disorder and post-traumatic stress disorder.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Pregnancy can be a longed-for yet daunting process for women, even in the best of circumstances. It is accompanied by a range of significant physical, psychological and social changes, with birth marking both the endpoint of the phase of gestation and the beginning of a new and challenging phase of parenting a newborn. There can be varying degrees of medical complications to navigate through pregnancy, as well as the uncertainties of labour and birth for mother and child. Whilst many women manage well, it is not surprising that anxiety is a relatively common experience. During pregnancy, the prevalence of significant anxiety symptoms is high, increasing across the trimesters from 18.2% of women in the first trimester to 24.6% in the third trimester (Dennis et al., 2017). This may be anxiety specifically related to the pregnancy and birth (‘pregnancy-related anxiety’) or have another focus. Antenatal (occurring during pregnancy) anxiety disorders are very common, affecting approximately 15% of women (Dennis et al., 2017). For some women, aspects of being pregnant may precipitate an anxiety disorder, whilst those with a pre-existing problem may experience an exacerbation of symptoms (Biaggi et al., 2016; Fairbrother et al., 2016; Viswasam et al., 2019). In all cases, the context of pregnancy is crucial to understanding how to formulate and treat the problem.
Anxiety disorders encompass a broad range of problems including specific phobias, generalised anxiety disorder (GAD), panic disorder and social anxiety disorder. Other relevant anxiety presentations (recategorised since DSM-5) are obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD). Many have direct relevance to pregnancy, such as tokophobia (fear of childbirth), emetophobia (fear of vomiting), blood-injury phobia and PTSD caused by a previous traumatic birth (Nath et al., 2020). OCD can present with distressing intrusive thoughts of deliberately harming the unborn child or fears the baby will be harmed by contamination (Abramowitz et al., 2003). All anxiety-related disorders are by definition distressing and demanding, with functional impairment common to the diagnosis; and anxiety disorders during pregnancy are no exception (Martini et al., 2010). Therefore, timely treatment is important for all sufferers. Almost all women are in contact with health services at some point during their pregnancy, presenting a unique opportunity for screening and treatment of mental health problems.
Anxiety disorders during pregnancy have been associated with greater risk of emergency Caesarean and instrumental deliveries (Dekel et al., 2019) as well as obstetric complications and preterm delivery (Ding et al., 2014; Martini et al., 2010). Associations with greater pregnancy-related anxiety symptoms have also been reported (Martini et al., 2016).
Many women are motivated to seek treatment in order to help them manage through the pregnancy and to prevent any postpartum impact of their disorder on their child or their parenting. This is a reasonable concern, with associations between antenatal and postnatal anxiety disorders and impairments in parent-child interactions and quality of life shown by several studies (Challacombe et al., 2016; Murray et al., 2008; Petzoldt et al., 2016). Antenatal anxiety disorders have also been associated with postpartum depression, which may explain some of this impact (Coelho et al., 2011; Martini et al., 2010; Tietz et al., 2014).
There has been considerable research attention on the impact of antenatal anxiety, and women and professionals alike are often concerned about the impact of anxiety on the foetus. In large longitudinal studies, antenatal anxiety has been associated with long-ranging impacts on child development, including emotional and behavioural problems, leading some authors to suggest it might be a sensitive time for relevant aspects of foetal brain development (Capron et al., 2015; O’Connor et al., 2003). Potential mechanisms include HPA axis dysfunction (Van den Bergh et al., 2005) and anxiety-related changes in uterine blood flow (Teixeira et al. 1999). Consistently elevated stress, depression and anxiety have been associated with increased cortisol levels that may alter placental functioning to impact the foetus, although these associations are correlational (Buss et al., 2010; Kane et al., 2014; Sarkar et al., 2008). Much is yet to be understood about the complex interplay between maternal mood, mechanisms of transmission and infant outcomes. However, given the range of impacts of untreated antenatal anxiety, providers have many reasons to treat pregnant women to maximise the benefit to them and their offspring. The rest of the chapter will focus on the issues of delivery and content related to using exposure-based therapy with pregnant women with anxiety disorders.
Delivering Therapy with Pregnant Women
Pregnant women demonstrate a strong preference for psychological therapy over medication, often due to fears of teratogenic effects (Arch, 2013). This preference explicitly includes a willingness to engage in exposure therapy. Recent reviews suggest that SSRI use (the most common pharmacological intervention for anxiety) can elevate the small absolute risk of adverse outcomes in infants (Fischer Fumeaux et al., 2019). Cognitive behavioural approaches (CBT), in particular those including exposure therapy, are well-developed for anxiety-related disorders, having demonstrated efficacy and effectiveness in the general population in many studies (Hans & Hiller, 2013; Olatunji et al., 2010). However, despite the high prevalence of anxiety-related problems in pregnancy, there are no large-scale trials investigating the delivery of such treatments at this time (Marchesi et al., 2016; Nillni et al., 2018). One factor behind this has been the historical exclusion of pregnant women in intervention research, due in part to fears of additional risks in treating this group. Similar fears that pregnant women may be at risk of harm from exposure-based treatments are sometimes raised in clinical settings, where clinicians may encounter resistance at a service level. Furthermore, some clinicians can be unwilling to do exposure therapy due to their own anxious beliefs (Meyer et al., 2014). Clinicians therefore need a good grasp of the issues involved.
How Safe Is Exposure Therapy During Pregnancy?
A key component of CBT interventions for anxiety is deliberate, planned and repeated exposure to what is feared, including objects, situations, memories, images and body sensations (Lohr et al., 2012). The main controversy around using exposure in pregnancy stems from the idea that as exposure entails an initial rise in anxiety when the person confronts their fears, this may be associated with a rise in cortisol that negatively impacts the baby. The arguments are summarised eloquently and in detail by Arch et al. (2012). (1) The evidence base highlights the biological impact of untreated maternal anxiety on children; women seeking treatment are by definition already anxious. (2) Pregnant women present with unique biological differences during this period: healthy pregnant women have an increased HPA axis reactivity, with cortisol levels which would be considered pathological in non-pregnant women (Mastorakos & Ilias, 2003). Additionally, pregnant women may have a diminished physiological response to acute stress on a variety of physiological indices (de Weerth & Buitelaar, 2005). Potentially, pregnant women who undergo exposure-based therapy may not have the same heightened physiological anxiety response commonly seen in non-pregnant peers. This could have an impact on efficacy rather than safety. (3) Perhaps most importantly, the stress response from undertaking exposure is temporary, lasting 60–90 minutes and often much less before habituation occurs. Exposure leads to overall reductions in anxiety between sessions (Craske et al., 2008).
Recent studies examining the physiology of exposure exercises have found that there is no strong evidence (in non-pregnant populations) of a lasting effect on cortisol, even in the context of high subjective distress (Kellner et al., 2020; Mayer et al., 2017). (4) The short-lived nature of any increase in anxiety seems consistent across disorders. Exposure to the trauma memory in PTSD can lead to a temporary increase in intrusions which resolves, and is not related to worse treatment outcome (Foa et al., 2002). Exposure in general is not highly distressing or the cause of lasting physiological impact. Whilst specific data are needed for pregnant women, it is highly likely that the potential benefits of exposure-based treatments outweigh any risks in pregnancy.
In one of the few treatment trials of exposure treatment of pregnant women, Lilliecreutz et al. (2010) designed a group treatment for pregnant women with blood and injection phobia and reported no adverse effects (Lilliecreutz et al., 2010). Blood-injury-injection phobias have a different physiological response involving a vasovagal/parasympathetic surge and therefore are unique amongst the anxiety disorders. In a recent review of the safety and effectiveness of non-pharmacological interventions for PTSD, Bass and colleagues collected safety data during pregnancy from available trials (Baas et al., 2020). A range of interventions were looked at including trauma-focused CBT, EMDR therapy, self-hypnosis and relaxation. No adverse effects on the mother or the unborn child were reported, suggesting that these treatments are safe. In their review of treatments for antenatal anxiety disorders, including three studies using CBT, no adverse effects of non-pharmacological treatments were reported (Marchesi et al., 2016). However, caution is warranted as the majority of the evidence available is from case studies. In summary, the existing evidence base, though limited in size and scope, has not highlighted any adverse effects from the use of exposure-based treatments in pregnancy.
How Effective Are Exposure-Based Treatments in Pregnancy?
The evidence suggests that CBT is effective in pregnancy, although detailed information on the use of exposure within these treatments is not available (Marchesi et al., 2016). The only trial to date is a non-randomised study examining a two-session group exposure intervention to reduce blood and injection phobias. Groups comprised four to six women, and trial took place at 25–30 weeks of pregnancy, with the second group a month later, and they were co-led by a therapist and midwife. Forty-six women acted as non-treated controls (Lilliecreutz et al., 2010). Eleven women preferred an individual intervention, the results of which have not been published. In this trial, women improved significantly on several measures including the Injection Phobia Scale–Anxiety, Anxiety subscale and measures of anxiety and depression.
A recent meta-analysis demonstrated that when exposure was a component in CBT-based treatment, there was a larger effect size on perinatal anxiety symptoms than when it was not (Maguire et al., 2018). However, the meta-analysis included only three studies. It should be noted that most of the CBT treatments consisted of a more cognitive approach and included relaxation strategies when treating pregnant women with an anxiety disorder, possibly due to the inclusion of guided self-help protocols in this study or due to concerns of treating pregnant women with exposure therapy.
Practical Considerations when Considering Exposure Therapy in Pregnancy
Timing of Treatment
Given the time-limited context, practical considerations are paramount in treating pregnant women. Considering the possibility of adverse impact on mother and child, it is imperative that women are offered treatment as soon as possible once they present with clinical anxiety. NICE guidelines recommend accelerating women into treatment within 4 weeks of referral (CG192).
Pregnant women may have many demands on their time, often balancing midwife or obstetrician appointments and hospital scans, work and other caring responsibilities. CBT is typically offered in a course of 8–16 sessions depending on the problem; clinicians should consider the pregnant women’s gestation stage and the number of sessions that are available to feasibly complete psychoeducation and exposure tasks to meet the woman’s therapy goals. If women are referred later in pregnancy, careful assessment should be made of what can reasonably be achieved in the time before the birth, including the woman’s physical state, and resources available to allow her to commit to the sessions and between-session practice. Although no robust research evidence is available, consideration should be given to postponing formal treatment if the woman is referred after 32 weeks of pregnancy. Support may still be provided, or alternatively, focused treatment around birth-related anxiety.
There is some evidence that benefit can be gained from shorter treatment protocols. In the general population, research has emerged suggesting that briefer versions of CBT (perhaps as few as four sessions) offer similar effectiveness to longer versions (8–16 sessions). Improvements were reported in those who had four or five sessions of CBT for panic disorder (Craske et al., 1995), seven sessions of CBT for panic disorder with agoraphobia (Marchand et al., 2009) and one session of exposure for specific phobias (Ost, 1989). Given the effectiveness of a two-session intervention for blood-injury phobia described above (Lilliecreutz et al., 2010), further research is needed to explore the impact of briefer CBT interventions with exposure in pregnant women with anxiety disorders.
Time-Intensive Therapy
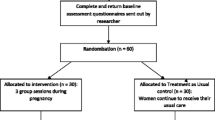
Considering the pressure to improve anxiety symptomatology as quickly as possible during pregnancy, clinicians may also want to consider offering accelerated or intensive exposure therapy programme. Time-intensive treatment involves the patient being offered the same number of sessions over a shorter time frame, rather than the typical weekly schedule. Outside of pregnancy this has been shown to be beneficial in the treatment of OCD (Storch et al., 2008), agoraphobia (Knuts et al., 2015) and panic disorder (Wootton & MacGregor, 2018). Additionally, findings reported that enhanced longer-term benefits were observed. CBT with exposure has been used to treat postnatal OCD over a 2-week period. Mothers reported this approach to be acceptable and reported reductions in OCD symptoms and benefits to parenting (Challacombe & Salkovskis, 2011). Given the time parameters, a similar approach could be tested with anxiety disorders in pregnancy (Challacombe et al., 2021).
Group Versus Individual Therapy
Clinicians may want to consider the pros and cons of group versus individual exposure therapy. Group therapy may be a cost-effective option, although preliminary findings suggest that individual CBT may be superior to group CBT for pregnant women with anxiety (Maguire et al., 2018). This mirrors the general literature which showed greater benefits in individual CBT versus group CBT in the treatment of panic and agoraphobia (Sharp et al., 2004) and social anxiety (Stangier et al., 2003). However, groups do offer additional benefits such as normalising patient concerns, peer support and the sharing of ideas which could be particularly useful for pregnant women, given the importance of peer support in general at this time (Huang et al., 2020).
Online Therapy
There has been an increased interest in online therapies which can increase access and may be useful for pregnant women given other limitations. Emerging evidence suggests that online programmes focusing on improving anxiety symptomatology in pregnant women offer some benefits (Loughnan et al., 2019). However, it may be more difficult to conduct exposure treatment in this format, due to limitations in modelling and other constraints. Further research, however, is needed to fully understand the benefits of remote (online) treatment for anxiety disorders.
Assessment
The context of pregnancy frames an understanding of the presentation and treatment of anxiety throughout a course of treatment. A standard assessment includes questions about the presenting symptoms and history of the disorder as well as comorbid problems. It is also important to ascertain a medical history alongside any pregnancy-related complications in order to consider any limitations to the tasks tackled in exposure therapy. For example, exposure may be significantly modified (or not used) in those with respiratory, cardiac and pulmonary conditions. If there is a query about an underlying physical diagnosis that may be related to presenting symptoms (e.g. heart palpitations), it is advisable for the woman to seek guidance from a medical practitioner before proceeding.
Pregnant women may abruptly cease taking psychotropic medication when they find out they are pregnant or feel intense guilt and anxiety about the decision to continue (Einarson et al., 2001). Medication status should therefore be carefully assessed, alongside the woman’s feelings about her decision to use (or not use) such agents. Feelings about becoming a parent should also be included in the assessment as they are highly relevant to current mood. Parenting characterised by high control and low warmth confers additional risk for anxiety and depression in pregnancy, over and above other times (Biaggi et al., 2016).
It is important to consider instruments which have been validated in the perinatal population, in particular those which are less reliant on the physical symptoms of anxiety (Meades & Ayers, 2011). Commonly used measures are the General Health Questionnaire, the State-Trait Anxiety Inventory (STAI) and the Depression Anxiety Stress Scale (DASS-21).
Note that pregnancy is a dynamic state and many of these factors will warrant reassessment at every treatment contact, for example, the medical status of the pregnancy and any change in circumstances. Table 11.1 provides a checklist of items to assess pregnant women presenting for the treatment of anxiety.
Treatment
Pregnancy is an opportunity for women to address psychological problems before becoming a parent, and therapy presents the potential for benefitting both mother and child. This point can be used to increase incentive to help women approach exposure tasks within CBT. Still, it is important to provide a clear rationale for exposure tasks since it will involve deliberately provoking discomfort. Modifications to the nature and intensity of exposure (relative to its use with non-pregnant patients) are likely, and less may be needed to trigger anxiety. For example, Arch (2012) lists a number of possible exercises to induce panic-like sensations in pregnancy such as holding one’s breath (fears of suffocation) or staring at a light and then looking away (fears of derealisation).
Two case studies are presented in this section to illustrate particular considerations when treating these disorders in pregnant women. Common elements include gaining a shared understanding of how the anxiety problem interacts with the woman’s specific pregnancy, introducing exposure adapted to this context and the use of modelling during exposure to enhance engagement. Where possible, once the person has a good understanding of the model and has begun to use exposure, partners or family members should be invited to a session in order to support the person to continue practice at home.
OCD in Pregnancy
OCD can take a number of different forms, any of which may coincide with pregnancy, with an overall estimated prevalence of approximately 2% at this time, slightly higher than the general population prevalence (Russell et al., 2013). For many women, obsessions and compulsions centre around the wellbeing of the unborn baby. Distressing intrusive thoughts or images of deliberately or accidentally harming the baby or that something is wrong may dominate. This can lead to extensive avoidance, checking and excessive reassurance seeking from the internet, family and health professionals. OCD is associated with inflated responsibility (Salkovskis et al., 2000), and the combination of responsibility and uncertainty inherent in pregnancy can be difficult for many women with OCD. Pregnant women are bombarded with information about possible threats to their baby, and treating OCD in this context needs to take this into account.
Case Example
Chanelle, a 30-year-old married occupational therapist, was referred for treatment by her midwife when she was 16 weeks’ pregnant with her first child. She had no formal history of OCD but reported experiencing mild anxiety from obsessive-compulsive thoughts as a child and described herself as a perfectionist. She had conceived after two early miscarriages following 3 years of trying to become pregnant. Her anxiety began at the start of her pregnancy, and she was becoming increasingly distressed by her fears that she might eat contaminated food or come into contact with something that could terminate the pregnancy or harm her unborn baby. Her diet was becoming increasingly restrictive and she was finding it difficult to attend work due to her fears. She was excessively cleaning herself and her house to avoid contamination. In order to limit contact with others, she had also stopped doing many of the things she enjoyed, such as Yoga, and was spending several hours a day researching ingredients of household products to determine whether they were safe to use during pregnancy. Finally, Chanelle’s relationship with her husband was becoming increasingly strained. Her scores on measures of anxiety, depression and OCD were in the severe range.
Following an initial assessment, Chanelle was encouraged to set treatment goals for the next few weeks and remainder of the pregnancy, and for after childbirth (see Table 11.2). She initially found this difficult and was asked to consider what would be reasonable for a pregnant woman at the same stage to be eating and doing. Setting goals for beyond the pregnancy helped Chanelle consider herself as a parent and start to think more broadly about the impact of her intense focus on physical safety on herself, her baby and her husband.
A formulation of Chanelle’s symptoms was developed using the cognitive behavioural model of OCD (Salkovskis, 1999). This helped her see that the key fear driving her behaviours was the idea that unless she did everything possible to prevent harm coming to her baby, something could go wrong and this would have been her fault. Chanelle felt that she could not cope with this outcome. Normalising the motivation was important: this idea is understandable and desirable for parents, and the difficult circumstances of conception were relevant to her fear. However, the rigidity with which she was applying this was causing the problem, leading her to do far in excess of what was required. Chanelle’s compulsions of avoidance, checking, reassurance seeking and cleaning were therefore all aimed at helping her feel she had done everything she could. At the same time, doing these things maintained the belief that the precautions were necessary and responsible.
Although Chanelle knew that her behaviour was excessive, she also held a belief that to change things would lead to intolerable feelings of guilt if anything went wrong; and she therefore felt stuck. Chanelle would have been reluctant to make any changes if she did not have a clear understanding of why and how this could help. It was necessary to present a new but credible perspective to inform exposure and behavioural change and create a therapeutic atmosphere where Chanelle could choose to do things differently.
Chanelle was asked to consider her problem as one of excessive anxiety rather than danger, and she and her therapist created the table in Table 11.3. Chanelle was not at any more risk than other pregnant women based on her medical history. Yet ironically, everything she was doing to stay ‘safe’ was in fact increasing her anxiety which was causing a number of immediate problems.
Following completion of this table together, the therapist wanted to move Chanelle to the action stage. The following dialogue took place:
- Therapist (T)::
-
So, what explanation do you think is the best fit with your experiences?
- Chanelle (C)::
-
I see that perhaps I have been doing my best to solve the wrong problem, that it’s anxiety.
- T::
-
That’s right. It makes sense as everything in the pregnancy is new, and it’s so precious to you. You’ve understandably been taking a ‘better safe than sorry’ approach.
- C::
-
Yes, that’s exactly what I’ve been doing.
- T::
-
And what’s the problem with that?
- C::
-
It seems like it doesn’t keep you particularly safe and it definitely makes you very sorry!
- T::
-
So would you be willing to try making a few changes?
Chanelle had a clear understanding of the benefits of therapy and felt ready to try testing things out. The next several sessions were spent doing exposure-based experiments based on her treatment goals, which formed the foundations of an exposure hierarchy. For example, Chanelle brought some fruit to eat during one therapy session. The therapist ate some of the fruit without washing it and even after placing it on the floor for a little while. When it was Chanelle’s turn to try this exposure, she insisted on washing her fruit as this was consistent with normal precautions, but she agreed not to wash her own hands before eating it – a difficult step for her. Although her anxiety level (SUDS) increased to 90% just before the task, she was surprised to find that her level of distress was temporary and that she was able to manage these feelings better than she had anticipated. Chanelle discussed the need to challenge self-critical and guilty thoughts if they came up and to remind herself of the benefit to her baby of working on her anxiety in pregnancy. Regular tasks were set as homework and discussed in sessions each week, along with check-ins on questionnaire measures and issues around pregnancy.
Other elements of treatment were bringing Chanelle’s husband into a session to help him better understand her behaviour and to develop alternatives to reassurance. Chanelle suggested he could praise her and help her delay reassurance seeking, should she feel the need to ask. During this session, Chanelle and her husband set up new tasks that would benefit her therapy and their relationship such as going out for a meal. A relapse prevention plan was developed including anticipating how to deal with obsessions about the baby’s health in the postpartum period. Follow-up sessions were arranged for the postpartum period.
PTSD in Pregnancy
The prevalence rate of post-traumatic stress disorder (PTSD) ranges from 0.6% to 16% during pregnancy (Viswasam et al., 2019). Pregnant women often experience similar traumatic events to those experienced by the non-pregnant population, but providers should be aware that there are particularly high rates of concurrent partner abuse (James et al., 2013) and that PTSD treatment is not appropriate if threatening conditions continue to exist. Pregnant women may also experience PTSD-related anxiety during a subsequent pregnancy if they previously experienced previous birth complications or a traumatic delivery (Yildiz et al., 2017). Care should be taken when deciding whether to treat historic sexual trauma, and a careful assessment should be made of the woman’s resources to engage in treatment. Liaison with midwives and obstetric colleagues may be necessary to help the woman with potentially triggering situations such as intimate exams and aspects of the birth.
Case Example
India experienced a traumatic birth 2 years before her current pregnancy. This experience involved a prolonged labour during which she thought her baby would not survive. Although the newborn was treated in the neonatal intensive care unit and ultimately healthy, India experienced flashbacks and significant anxiety in the postpartum period. These eventually resolved on their own yet re-emerged when she became pregnant for a second time. During her initial consultation with her midwife at 12 weeks’ gestation, she became very panicky, experienced a recurrence of her flashbacks and was referred for assessment and therapy. As India had a busy job, she decided to undergo intensive therapy, in which treatment was delivered in a series of longer sessions over 2 weeks (Ehlers et al., 2014). She took leave from her work for this time period to focus on the therapy.
Treatment followed the protocol for trauma-focused cognitive behavioural therapy developed by Ehlers and Clark (Ehlers & Clark, 2000). This involves imaginal exposure to the memory of the traumatic experience to help process these memories, stimulus discrimination techniques to help gain control over flashbacks triggered by sensory similarities to the trauma, behavioural activation to address depression and anhedonia and cognitive therapy to challenge dysfunctional beliefs and appraisals. As this chapter focuses on exposure therapy, we will focus on this element here.
Initial assessment established that India was in a stable and supportive home situation and wished to work on her PTSD in order to feel better in pregnancy and have a more positive birth experience. The possibility of an increase in traumatic memories after initial sessions was raised, and India discussed strategies with her therapist to deal with this should it arise. After initial goal setting and psychoeducation about the nature of traumatic memories, India was asked to ‘relive’ her experience (with pre-established start and endpoints), using the first person present voice, with eyes closed and focusing the sensory qualities of the memory to increase ‘nowness’. The therapist was careful to identify ‘hotspots’, moments of the trauma that were particularly difficult and associated with high emotion in reliving them (see Table 11.4). It was these moments that India was re-experiencing in flashbacks (Crawley et al., 2018). India went through reliving twice, with a reduction in intensity and distress between the two exposures, suggesting some initial habituation of fear in response to the memory was occurring. Two key moments were identified for updating.
To update hotspot one, India was asked to look at a recent picture of Jenson (her firstborn son) in which he was playing, very much alive and well. She was then asked to relive and expose herself to her trauma narrative again, pausing at the key moment to insert the updated information of what she knew now, and to visualise Jenson as he is in the present. In the initial reliving which began to piece the memory together, India had recalled that the nurse had later returned to talk to her, something she had previously forgotten. This information allowed her to update her appraisal made at the time, that the nurse was callous and she was alone at the worst moment, something that is predictive of perinatal PTSD (Ford & Ayers, 2011). During the imaginal exposure, India was able to insert the updated information. She listened to recordings of the updated narrative at home, and experienced significant reductions in distress, along with reductions in the frequency and intensity of her flashbacks (Grey et al., 2002).
Other elements of India’s treatment included a site visit to the hospital where the birth took place in order to focus on differences between then and now and tackling of avoidance of engaging with professionals in her current pregnancy. India’s scores on measures of PTSD, anxiety and depression substantially improved after the 2-week treatment period.
Conclusions
Exposure-based treatments have been used successfully with pregnant women and the available evidence indicates that they are safe. This is important as there are clear impacts on mother and child from untreated anxiety problems. CBT demands that exposure exercises are tailored to the individual and the specific circumstances of the pregnant woman should be explored in detail in order to set up and conduct successful treatment. Ideally, some sessions should take place in the postpartum period in order to support woman into this period. We have discussed important points for clinicians to consider with regard to the use of exposure-based CBT for pregnant women. We have also outlined an appropriate assessment strategy. Finally, we have detailed the use of exposure therapy in two perinatal patients with clinical anxiety.
References
Abramowitz, J. S., Schwartz, S. A., Moore, K. M., & Luenzmann, K. R. (2003). Obsessive-compulsive symptoms in pregnancy and the puerperium: A review of the literature. Journal of Anxiety Disorders, 17, 461–478.
Arch, J. J. (2013). Cognitive behavioral therapy and pharmacotherapy for anxiety: Treatment preferences and credibility among pregnant and non-pregnant women. Behaviour Research and Therapy. https://doi.org/10.1016/j.brat.2013.11.003
Arch, J. J., Dimidjian, S., & Chessick, C. (2012). Are exposure-based cognitive behavioral therapies safe during pregnancy? Archives of Women’s Mental Health, 15, 445–457. https://doi.org/10.1007/s00737-012-0308-9
Baas, M. A. M., van Pampus, M. G., Braam, L., Stramrood, C. A. I., & de Jongh, A. (2020). The effects of PTSD treatment during pregnancy: systematic review and case study European journal of psychotraumatology, 11, 1762310. https://doi.org/10.1080/20008198.2020.1762310
Biaggi, A., Conroy, S., Pawlby, S., & Pariante, C. M. (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders, 191, 62–77. https://doi.org/10.1016/j.jad.2015.11.014
Buss, C., Davis, E. P., Muftuler, L. T., Head, K., & Sandman, C. A. (2010). High pregnancy anxiety during mid-gestation is associated with decreased gray matter density in 6-9-year-old children. Psychoneuroendocrinology, 35. https://doi.org/10.1016/j.psyneuen.2009.07.010
Capron, L. E., et al. (2015). Associations of maternal and paternal antenatal mood with offspring anxiety disorder at age 18 years. Journal of Affective Disorders, 187, 20–26. https://doi.org/10.1016/j.jad.2015.08.012
Challacombe, F. L., & Salkovskis, P. M. (2011). Intensive cognitive-behavioural treatment for women with postnatal obsessive-compulsive disorder: A consecutive case series. Behaviour Research and Therapy, 49, 422–426. https://doi.org/10.1016/j.brat.2011.03.006
Challacombe, F. L., Salkovskis, P. M., Woolgar, M., Wilkinson, E. L., Read, J., & Acheson, R. (2016). Parenting and mother-infant interactions in the context of maternal postpartum obsessive-compulsive disorder: Effects of obsessional symptoms and mood. Infant Behavior and Development, 44, 11–20. https://doi.org/10.1016/j.infbeh.2016.04.003
Challacombe, F. L., Potts, L., Carter, B., Lawrence, V., Husbands, A., Howard, L. M. (2021).Optimising psychological treatment for Anxiety DisordErs in Pregnancy (ADEPT): study protocol for a feasibility trialof time-intensive CBT versus weekly CBT. Pilot Feasibility Stud. 7(1):101. PMID: 33931111; PMCID: PMC8085465. https://doi.org/10.1186/s40814-021-00838-8
Coelho, H. F., Murray, L., Royal-Lawson, M., & Cooper, P. J. (2011). Antenatal anxiety disorder as a predictor of postnatal depression: A longitudinal study. Journal of Affective Disorders, 129, 348–353. https://doi.org/10.1016/j.jad.2010.08.002
Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., & Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46, 5–27. https://doi.org/10.1016/j.brat.2007.10.003
Craske, M. G., Maidenberg, E., & Bystritsky, A. (1995). Brief cognitive-behavioral versus nondirective therapy for panic disorder. Journal of Behavior Therapy and Experimental Psychiatry, 26, 113–120. https://doi.org/10.1016/0005-7916(95)00003-I
Crawley, R., Wilkie, S., Gamble, J., Creedy, D. K., Fenwick, J., Cockburn, N., & Ayers, S. (2018). Characteristics of memories for traumatic and nontraumatic birth Applied Cognitive Psychology. No Pagination Specified. https://doi.org/10.1002/acp.3438.
de Weerth, C., & Buitelaar, J. K. (2005). Physiological stress reactivity in human pregnancy – A review. Neuroscience and Biobehavioral Reviews, 29, 295–312. https://doi.org/10.1016/j.neubiorev.2004.10.005
Dekel, S., Ein-Dor, T., Berman, Z., Barsoumian, I. S., Agarwal, S., & Pitman, R. K. (2019). Delivery mode is associated with maternal mental health following childbirth. Archives of Women’s Mental Health, 22, 817–824. https://doi.org/10.1007/s00737-019-00968-2
Dennis, C.-L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. The British Journal of Psychiatry. https://doi.org/10.1192/bjp.bp.116.187179
Ding, X.-X., et al. (2014). Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. Journal of Affective Disorders, 159, 103–110. https://doi.org/10.1016/j.jad.2014.02.027
Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. https://doi.org/10.1016/s0005-7967(99)00123-0
Ehlers, A., et al. (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. The American Journal of Psychiatry, 171, 294–304. https://doi.org/10.1176/appi.ajp.2013.13040552
Einarson, A., Selby, P., & Koren, G. (2001). Abrupt discontinuation of psychotropic drugs during pregnancy: Fear of teratogenic risk and impact of counselling. Journal of Psychiatry & Neuroscience, 26, 44–48.
Fairbrother, N., Janssen, P., Antony, M. M., Tucker, E., & Young, A. H. (2016). Perinatal anxiety disorder prevalence and incidence. Journal of Affective Disorders, 200, 148–155. https://doi.org/10.1016/j.jad.2015.12.082
Fischer Fumeaux, C. J., et al. (2019). Risk-benefit balance assessment of SSRI antidepressant use during pregnancy and lactation based on best available evidence – An update expert opinion on drug safety, 18, 949–963. https://doi.org/10.1080/14740338.2019.1658740
Foa, E. B., Zoellner, L. A., Feeny, N. C., Hembree, E. A., & Alvarez-Conrad, J. (2002). Does imaginal exposure exacerbate PTSD symptoms? Journal of Consulting and Clinical Psychology, 70, 1022–1028. https://doi.org/10.1037/0022-006X.70.4.1022
Ford, E., & Ayers, S. (2011). Support during birth interacts with prior trauma and birth intervention to predict postnatal post-traumatic stress symptoms. Psychology & Health, 26, 1553–1570. https://doi.org/10.1080/08870446.2010.533770
Grey, N., Young, K., & Holmes, E. (2002). Cognitive restructuring within reliving: A treatment for peritraumatic emotional “hotspots” in posttraumatic stress disorder. Behavioural and Cognitive Psychotherapy, 30, 37–56. https://doi.org/10.1017/S1352465802001054
Hans, E., & Hiller, W. (2013). A meta-analysis of nonrandomized effectiveness studies on outpatient cognitive behavioral therapy for adult anxiety disorders. Clinical Psychology Review, 33, 954–964. https://doi.org/10.1016/j.cpr.2013.07.003
Huang, R., Yan, C., Tian, Y., Lei, B., Yang, D., Liu, D., & Lei, J. (2020). Effectiveness of peer support intervention on perinatal depression: A systematic review and meta-analysis. Journal of Affective Disorders, 276, 788–796. https://doi.org/10.1016/j.jad.2020.06.048
James, L., Brody, D., & Hamilton, Z. (2013). Risk factors for domestic violence during pregnancy: A meta-analytic review. Violence and Victims, 28(3) 359–380. PMID: 23862304 https://doi.org/10.1891/0886-6708.VV-D-12-00034
Kane, H. S., Schetter, C. D., Glynn, L. M., Hobel, C. J., & Sandman, C. A. (2014). Pregnancy anxiety and prenatal cortisol trajectories. [references]. Biological Psychology, 100(2014), 13–19. https://doi.org/10.1016/j.biopsycho.2014.04.003
Kellner, M., Yassouridis, A., Adel, F., Muhtz, C., Jelinek, L., & Wiedemann, K. (2020). Cortisol, DHEA and DHEA-S during exposure therapy in patients with obsessive-compulsive disorder – Secretion patterns and prediction of treatment response. Psychiatry Research, 291, 113288. https://doi.org/10.1016/j.psychres.2020.113288
Knuts, I. J. E., Esquivel, G., Overbeek, T., Schruers, K. R. (2015). Intensive behavioral therapy for agoraphobia. J. Affect. Disord. 174, 19–22. https://doi.org/10.1016/j.jad.2014.11.029
Lilliecreutz, C., Josefsson, A., & Sydsjo, G. (2010). An open trial with cognitive behavioral therapy for blood- and injection phobia in pregnant women – A group intervention program. Archives of Women’s Mental Health, 13, 259–265. https://doi.org/10.1007/s00737-009-0126-x
Lohr, J. M., Lilienfeld, S. O., & Rosen, G. M. (2012). Anxiety and its treatment: Promoting science-based practice. Journal of Anxiety Disorders, 26, 719–727. https://doi.org/10.1016/j.janxdis.2012.06.007
Loughnan, S. A., Joubert, A. E., Grierson, A., Andrews, G., & Newby, J. M. (2019). Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: A systematic review and meta-analysis. Archives of Women’s Mental Health, 22, 737–750. https://doi.org/10.1007/s00737-019-00961-9
Maguire, P. N., Clark, G. I., & Wootton, B. M. (2018). The efficacy of cognitive behavior therapy for the treatment of perinatal anxiety symptoms: A preliminary meta-analysis. Journal of Anxiety Disorders, 60, 26–34. https://doi.org/10.1016/j.janxdis.2018.10.002
Marchand, A., Roberge, P., Primiano, S., & Germain, V. (2009). A randomized, controlled clinical trial of standard, group and brief cognitive-behavioral therapy for panic disorder with agoraphobia: A two-year follow-up. Journal of Anxiety Disorders, 23, 1139–1147. https://doi.org/10.1016/j.janxdis.2009.07.019
Marchesi, C., Ossola, P., Amerio, A., Daniel, B. D., Tonna, M., & De Panfilis, C. (2016). Clinical management of perinatal anxiety disorders: A systematic review. Journal of Affective Disorders, 190, 543–550. https://doi.org/10.1016/j.jad.2015.11.004
Martini, J., Asselmann, E., Einsle, F., Strehle, J., & Wittchen, H. U. (2016). A prospective-longitudinal study on the association of anxiety disorders prior to pregnancy and pregnancy- and child-related fears. Journal of Anxiety Disorders, 40, 58–66. https://doi.org/10.1016/j.janxdis.2016.04.007
Martini, J., Knappe, S., Beesdo-Baum, K., Lieb, R., & Wittchen, H.-U. (2010). Anxiety disorders before birth and self-perceived distress during pregnancy: Associations with maternal depression and obstetric, neonatal and early childhood outcomes. Early Human Development, 86, 305–310. https://doi.org/10.1016/j.earlhumdev.2010.04.004
Mastorakos, G., & Ilias, I. (2003). Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartum. Annals of the New York Academy of Sciences, 997, 136–149. https://doi.org/10.1196/annals.1290.016
Mayer, S. E., Snodgrass, M., Liberzon, I., Briggs, H., Curtis, G. C., & Abelson, J. L. (2017). The psychology of HPA axis activation: Examining subjective emotional distress and control in a phobic fear exposure model. Psychoneuroendocrinology, 82, 189–198. https://doi.org/10.1016/j.psyneuen.2017.02.001
Meades, R., & Ayers, S. (2011). Anxiety measures validated in perinatal populations: A systematic review. Journal of Affective Disorders, 133, 1–15. https://doi.org/10.1016/j.jad.2010.10.009
Meyer, J. M., Farrell, N. R., Kemp, J. J., Blakey, S. M., & Deacon, B. J. (2014). Why do clinicians exclude anxious clients from exposure therapy? Behaviour Research and Therapy, 54, 49–53. https://doi.org/10.1016/j.brat.2014.01.004
Murray, L., de Rosnay, M., Pearson, J., Bergeron, C., Schofield, E., Royal-Lawson, M., & Cooper, P. J. (2008). Intergenerational transmission of social anxiety: The role of social referencing processes in infancy. Child Development, 79, 1049–1064. https://doi.org/10.1111/j.1467-8624.2008.01175.x
Nath, S., Busuulwa, P., Ryan, E. G., Challacombe, F. L., & Howard, L. M. (2020). The characteristics and prevalence of phobias in pregnancy. Midwifery, 82, 102590. https://doi.org/10.1016/j.midw.2019.102590
Nillni, Y. I., Mehralizade, A., Mayer, L., & Milanovic, S. (2018). Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: A systematic review. Clinical Psychology Review, 66, 136–148. https://doi.org/10.1016/j.cpr.2018.06.004
O’Connor, T. G., Heron, J., Golding, J., & Glover, V. (2003). Maternal antenatal anxiety and behavioural/emotional problems in children: A test of a programming hypothesis. Journal of Child Psychology and Psychiatry, 44, 1025–1036.
Olatunji, B. O., Cisler, J. M., & Deacon, B. J. (2010). Efficacy of cognitive behavioral therapy for anxiety disorders: A review of meta-analytic findings. The Psychiatric Clinics of North America, 33, 557–577. https://doi.org/10.1016/j.psc.2010.04.002
Ost, L. G. (1989). One-session treatment for specific phobias. Behaviour Research and Therapy, 27, 1–7. https://doi.org/10.1016/0005-7967(89)90113-7
Petzoldt, J., Wittchen, H., Einsle, F., & Martini, J. (2016). Maternal anxiety versus depressive disorders: Specific relations to infants’ crying, feeding and sleeping problems. Child: Care, Health and Development, 42, 231–245. https://doi.org/10.1111/cch.12292
Russell, E. J., Fawcett, J. M., & Mazmanian, D. (2013). Risk of obsessive-compulsive disorder in pregnant and postpartum women: A meta-analysis. Journal of Clinical Psychiatry, 74, 377–385.
Salkovskis, P. M. (1999). Understanding and treating obsessive-compulsive disorder. Behaviour Research and Therapy, 37, S29–S52.
Salkovskis, P. M., et al. (2000). Responsibility attitudes and interpretations are characteristic of obsessive compulsive disorder. Behaviour Research and Therapy, 38, 347–372.
Sarkar, P., Bergman, K., O’Connor, T. G., & Glover, V. (2008). Maternal antenatal anxiety and amniotic fluid cortisol and testosterone: Possible implications for foetal programming. Journal of Neuroendocrinology, 20, 489–496. https://doi.org/10.1111/j.1365-2826.2008.01659.x
Sharp, D. M., Power, K. G., & Swanson, V. (2004). A comparison of the efficacy and acceptability of group versus individual cognitive behaviour therapy in the treatment of panic disorder and agoraphobia in primary care. Clinical Psychology & Psychotherapy, 11, 73–82. https://doi.org/10.1002/cpp.393
Stangier, U., Heidenreich, T., Peitz, M., Lauterbach, W., & Clark, D. M. (2003). Cognitive therapy for social phobia: Individual versus group treatment. Behaviour Research and Therapy, 41, 991–1007. https://doi.org/10.1016/s0005-7967(02)00176-6
Storch, E. A., et al. (2008). Cognitive-behavioral therapy for obsessive–compulsive disorder: A non-randomized comparison of intensive and weekly approaches. Journal of Anxiety Disorders, 22, 1146–1158. https://doi.org/10.1016/j.janxdis.2007.12.001
Teixeira, J. M., Fisk, N. M., & Glover, V. (1999). Association between maternal anxiety in pregnancy and increased uterine artery resistance index: Cohort based study. BMJ (Clinical research ed), 318, 153–157. https://doi.org/10.1136/bmj.318.7177.153
Tietz, A., Zietlow, A., & Reck, C. (2014). Maternal bonding in mothers with postpartum anxiety disorder: The crucial role of subclinical depressive symptoms and maternal avoidance behaviour. Archives of Women’s Mental Health, 17, 433–442. https://doi.org/10.1007/s00737-014-0423-x
Van den Bergh, B. R., Mulder, E. J., Mennes, M., & Glover, V. (2005). Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms. A review Neuroscience and Biobehavioral Reviews, 29, 237–258. https://doi.org/10.1016/j.neubiorev.2004.10.007
Viswasam, K., Eslick, G. D., & Starcevic, V. (2019). Prevalence, onset and course of anxiety disorders during pregnancy: A systematic review and meta analysis. Journal of Affective Disorders, 255, 27–40. https://doi.org/10.1016/j.jad.2019.05.016
Wootton, B. M., & MacGregor, A. (2018). Accelerated outpatient individual cognitive-behaviour therapy for panic disorder: A case study. Clinical Psychologist, 22, 92–98. https://doi.org/10.1111/cp.12100
Yildiz, P. D., Ayers, S., & Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders, 208, 634–645. https://doi.org/10.1016/j.jad.2016.10.009
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Challacombe, F.L., Jansen, M.A. (2022). Exposure Therapy with Patients Who Are Pregnant. In: Smits, J.A.J., Jacquart, J., Abramowitz, J., Arch, J., Margraf, J. (eds) Clinical Guide to Exposure Therapy. Springer, Cham. https://doi.org/10.1007/978-3-031-04927-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-04927-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04926-2
Online ISBN: 978-3-031-04927-9
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)