Abstract
Cancer cell invasion is regulated by extracellular matrix (ECM) chemical signaling and gene expression but it also consists in a mechanical process controlled by ECM’s array. Scanning electron microscope analysis, invasion test, and real-time PCR demonstrated that Matrigel mimicking basement membrane (BM) doesn’t promote epithelial–mesenchymal transition (EMT) in both low and very aggressive breast cancer cells (MCF-7 and MDA-MB-231). A loose network of type I collagen mimicking the sub-BM favors EMT in MCF-7 cells but physically limits their invasion ability vs. Matrigel, as collagen does not induce an increase of metalloproteases (MMPs) in cells following ameboid-invasion mode. Collagen doesn’t change MDA-MB-231 phenotypes but further improves their invasion capability vs. Matrigel, by stimulating MMPs production. Concentrated type I collagen mimicking deeper ECM induces cells adhesion, further development of microvesicles, microvilli, long filopodia, and tunneling nanotubes (TNTs). Nonaligned fibronectin favors breast cancer cells adhesion, microvesicles, and TNTs development. Densely packed and parallel collagen fibers mimicking a collagen array in mammary tumor progression oppose invasion. In colon cancer, LoVo-R cells, resistant to doxorubicin, concentrated collagen favors development of invaginating phenotypes with invadopodia. We suggest that collagen acts as a physical factor inducing EMT in breast cancer cells and drug resistance in LoVo-R cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Basement membrane
- Collagen
- Fibronectin
- Breast cancer cells
- Colon cancer cells
- EMT
- Drugs resistance
- Cultures
- SEM
10.1 The Biomechanical Role of ECM in Cancer Progression
In normal conditions, extracellular matrix (ECM) connects but also separates different tissues and provides the gaseous and metabolic support to most of them. Similarly, progression of most diseases depends on the physical status and chemical properties of ECM which interacts and responds to the biological changes of the pathological processes. This is what usually happens in wounds, foreign body granulomas, as well as in cancer (Schäfer and Werner 2008; Fouad and Aanei 2017; Foster et al. 2018; Paolillo and Schinelli 2019).
Malignant transformation is related to an uncontrolled cells growth, dissociation of cells with loss of intercellular adhesiveness and acquisition of migration capability. These changes allow cells to breach the basement membrane (BM), invade the peri-tumoral microenvironment, and then colonize distant anatomical sites by forming metastatic points. In addition, the peri-tumoral ECM undergoes significant structural alterations which can also induce the epithelial–mesenchymal transition (EMT) in cancer cells (Zolota et al. 2021; Karamanos et al. 2021). As a matter of fact, the uncontrolled tumor growth generates by itself compressive stresses within tumor which can stimulate cancer cells migration by developing of invading leader cells and improving cell–substrate adhesion for grouped cell invasion (Tse et al. 2012).
Cancer cell invasion is foremost a mechanical process, and many experimental studies and reviews concerning the interactions between cancer cells and surrounding tissues have mainly focused on gene regulation and signaling that lead to the development of the tumor. However, the knowledge on the role that physical properties of tumor microenvironment exert in affecting cancer cell behavior is relatively limited (Brabek et al. 2010; Baker et al. 2011; Balkwill et al. 2012; Kim et al. 2018; Wang et al. 2018; Malandrino et al. 2018; Scott et al. 2019). In particular, changes in structural and biomechanical properties of ECM which favor cancer cell adhesion ability and development of new cell phenotypes with an improved motility just exerted by generations of mechanical actions like contractile and tensional forces are undervalued (Friedl and Brocker 2000; Ridley et al. 2003; Zaman et al. 2006; Mierke et al. 2008; Zanotelli et al. 2021). When cancer cells migrate and travel through the ECM, they encounter a mechanical resistance which cells must overcome in order to reach blood and lymphatic vessels.
From a chemo-mechanical point of view, ECM consists in a meshwork of insoluble proteins like collagen, assembling in collagen fibrils and then in fibers, and in minor amount elastin which forms the elastic fibers; but ECM also contains a high molecular mass of anionic substances of predominant carbohydrate nature including proteoglycans (PGs) and glycosaminoglycans (GAGs), which are particularly able to sequester high amount of water. The insoluble collagen fibrils, mainly resisting to tensile stresses (Franchi et al. 2007, 2009, 2010; Pissarenko et al. 2019), are held together by GAGs and PGs which fill the interfiber spaces and acting like elastic strings in solution oppose compression. In ECM, these components interact with water and contribute to form a functional dynamic scaffold which can control the shape of tissues, organs, and whole body (Scott 1975, 2002, 2003; Yue 2014). ECM can bind cells of different tissues and offer anchorage sites for cell movement and migration, but also plays the role of a physical barrier separating different tissues or opposing to cell migration (Mould and Humphries 2004; Larsen et al. 2006; Lu et al. 2011; Yue 2014; Kular et al. 2014; Ringer et al. 2017).
ECM architecture has a significant effect on cell motility and the ability of cells to adhere and sense the mechano-chemical environment is particularly discussed. It is widely recognized that the chemical, mechanical, and topographical properties of the extracellular environment of peri-tumoral tissue can also play a possible primary role in affecting both tumor progression and cancer cells invasion (Lu et al. 2011; Baker et al. 2011). Collagen, the main component of ECM, is widely used as substrate in three-dimensional (3D) cultures of cancer cells. The chemical composition and physical characteristics of the ECM, such as geometry, macro-microporosity, collagen alignment, density, and stiffness, strongly contribute to cancer cell adhesion, migration, and invasion (Wolf and Friedl 2011). Moreover, both cancer and stromal cells can activate an enzymatic-dependent pericellular proteolysis which generates micro- and macrotracks delimited by relatively aligned collagen bundles which further favor cell adhesion and invasion (Gaggioli et al. 2007; Wolf et al. 2007; Provenzano et al. 2008).
Among other factors, also confinement and topology can affect modes of cell migration (Kurniawan et al. 2016; Pandya et al. 2017). Microporosity of ECM can depend on caliber, density, and array of collagen fibers, but also on the hydration level of tissue which is directly related to the content of GAGs like hyaluronic acid. Tissue mesh size, related to microporosity, represents a physical limit to cancer cell invasion and is related to deformation capability of the nucleus. Smaller than 7 μm2 mesh sizes in ECM do not allow cancer cells to directly invade the peri-tumoral ECM (Wolf et al. 2013), whereas larger mesh sizes allow globular-shaped cells to migrate through the network by the so-called amoeboid movement. Even though collagen network plays a contrasting role to cancer cell invasion, some aggressive cancer cells can degrade the matrix architecture by releasing proteolytic enzymes named metalloproteases (MMPs) (Wolf et al. 2007; Friedl and Wolf 2010; Brabek et al. 2010; Scott et al. 2019).
Alterations of ECM mechanical properties can also affect cancer cell phenotypes as cells can sense the physical status and array of peri-tumoral ECM and respond by adapting their phenotypes to the new environment. For instance, an increase of ECM stiffness induces cancer cells to gain an elongated shape and re-enforce focal adhesions, cytoplasmic protrusions, and ability to exert high-traction forces (Peyton et al. 2008; Koch et al. 2012; Ringer et al. 2017). An increased collagen stiffness also affects cells in microenvironment surrounding tumor by modulating remodeling cytoskeleton of fibroblasts and cancer associated fibroblasts (CAFs) (Stylianou et al. 2019).
Particular attention should be given to the different invasion modes and cancer cells ability in switching them or “plasticity.” The different invasion modes are related to different cell phenotypes and cell shape seems to predict ECM-driven 3D cell invasion in breast cancer (Baskaran et al. 2020). Both individual and collective invasions can occur: the first mode concerns cells loosing cell–cell contacts, whereas the second one involves cells which still maintain cell–cell junctions. Cells which invade in a collective mode can move as multicellular streams, budding, or larger clusters, whereas cells invading individually can develop elongated-mesenchymal phenotypes, contractility-driven rounded-amoeboid, and filopodial spike-mediated invading strategies. Cells adopting an elongated phenotype are characterized by actin-rich protrusions, focal adhesion formation, MMPs activity, and actomyosin contractility at the rear of the cells (Pandya et al. 2017). In general, these mesenchymal-like cells develop a highly motile phenotype and can easily cross basement membranes, interstitial spaces, and endothelial barriers in a single-cell migration. The strong cohesive intercellular forces favor the collective invasion and offer potential advantages for tumor survival such as covering different cell roles and improving resistance to immunologic attack (Christiansen and Rajasekaran 2006). Transition from collective to single-cell invasion or tumor plasticity may enhance a metastatic ability (Friedl et al. 2012). Anyway, all migration movement or invasion mode is related to intracellular actin polymerization with development of different cytoskeletons and new cell phenotypes.
To colonize distant organs, cancer cells must start a journey through different body tissues, at first by spreading from the body epithelial outer layer to the neighboring deeper tissues and then by invading blood and lymphatic vessels. In the first step of their journey, cancer cells have to cross ECM of connective tissues which contains different biological barriers opposing cell migration. ECM “biological barriers” can physically opposite but also favor migration/invasion of cancer cells: the first barrier comprises the basement membrane (BM) which serves as a scaffold for all epithelial cells; under the BM, the second one is represented by an interstitial loose connective tissue called papillary and subpapillary dermis in skin, lamina propria in hollow organs, or interstitial stroma in solid organs; a third biological barrier may be constituted by the deeper dense connective tissue which contains higher amount of collagen fibers of different size and array. As an example, in skin under the subpapillary dermis, we find the reticular dermis layer whose collagen accounts for about 70% of the weight of dried tissue. Both density and collagen array change from the papillary and subpapillary dermis, where collagen fibers composed of thin fibrils are sparse and show a low aggregation, to the deeper reticular dermis which contains thicker collagen fiber bundles with a horizontal laminar organization, densely distributed and including long and thick fibrils (Ribeiro et al. 2013; Breitkreutz et al. 2013; Limbert 2017; Ueda et al. 2019). As shown in Fig. 10.1a, b ECM just beneath the epithelium includes thin loose collagen fibrils, whereas the deep connective tissue layer comprises thicker collagen fibril bundles (Ottani et al. 1998).
Tumor-Associated Collagen Signatures (TACS). (a) In the first stage, a peri-tumoral deposition of collagen occurs (TACS-I). (b) When tumor grows, the collagen fibers around the pathological mass change their array and appear aligned and parallel to the tumor surface (TACS-II). (c) When cancer cells lose contact with each other and become able to penetrate the basement membrane, which is the first biological physical barrier opposing invasion, they can invade ECM of connective tissues. As an example, in skin cancer, cells pierce the basement membrane and then begin to migrate into the papillary and sub-papillary dermis containing sparse and thin collagen fibers. They further penetrate the depth of the tissue by invading the reticular dermis which contains thick collagen fibers. (d) With further development of the tumor mass, the collagen fibers develop a radial array that can favor cancer cell invasion (TACS-III)
The previously described biological barriers: (a) the BM, (b) the interstitial loose connective tissue/lamina propria/interstitial stroma, and (c) the deeper dense connective tissue, not only oppose cancer cells invasion but also offer anchorage and adhesion to MDA-MB-231 breast cancer cells which can better invade ECM by improving cell contraction and adapting their cytoskeleton (Byrne et al. 2021). In particular, type I and type III collagen assembled in fibrils and fibrillar fibronectin represent the main molecules composing physical scaffolds opposing and supporting the cells migratory movement. During tumor growth, changes of architecture of peri-tumoral collagen network are related to tumor progression and clinical prognosis (Egeblad et al. 2010; Conklin et al. 2011).
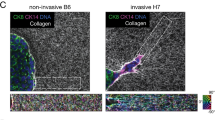
Markers of mammary carcinoma progression have been identified in a clinical-histological Tumor-Associated-Collagen-Signatures (TACS) classification. In a first step, only an increase in collagen deposition or desmoplasia around the tumor occurs (TACS-I) and no metastasis are reported. When tumor mass grows in size, the randomly arranged peri-tumoral collagen fibers are substituted by straight and aligned collagen fibers showing a circumferential orientation (TACS-II), and at this histological stage, no clinical metastasis occurs. However, a further remodeling of the collagen fibers can occur, collagen fibers arrange running perpendicularly to the tumor boundary (TACS-III). Unfortunately, this radial collagen fiber array seems to be strongly related to a higher risk of cancer cell invasion into peri-tumoral microenvironment, because the stretched and radially arranged collagen fibers allow but also favor interfiber cancer cell migration and colonization in distant organs (Provenzano et al. 2008; Riching et al. 2014; Bredfeldt et al. 2014; Wang et al. 2018; Franchi et al. 2019). From a mechanical point of view, the remodeling of ECM promotes matrix alignment and compaction that favors higher tractions exerted by cancer cells (Anguiano et al. 2020) (Fig. 10.1a–c).
Besides collagen, fibronectin (FN) is one of the most abundant proteins mediating cell adhesion and migration in ECM. It can develop into fibrils that widely differ in their thickness, between 10 and 1000 nm (Kular et al. 2014). FN regulates collagen assembly, and the presence of collagen fibrils induces the formation of highly colocalized FN fibrils (Paten et al. 2019). In tumor stroma, both type I collagen and fibronectin are strongly increased and create a denser and mechanically stiffer tissue if compared to normal tissue (Tlsty and Coussens 2006; Rick et al. 2019). FN, arranged into a mesh of fibrils like collagen, but also connected to and within the (BM) of ECM, has been investigated as a possible ECM component which can favor cancer invasion and metastasis and is linked to cell surface receptors (integrins) (Kular et al. 2014). Tumor growth promotes compressive forces within tumor which are accomplished by a coordinated migration of invasive phenotypes in mammary carcinoma cells accompanied by fibronectin deposition and stronger cell–matrix adhesion (Tse et al. 2012).
Experimental mechanical stimulation applied to a collagen–fibronectin matrix highly enhanced invasion ability of HT1080 fibrosarcoma cancer cells only when FN was present. This suggests a primary potential role of this ECM component in governing the mechanical response of tumor cells and tumor progression (Menon and Beningo 2011). Even though its role in tumorigenesis and malignant progression has been highly controversial (Lin et al. 2019), it was reported that cancer-associated fibroblasts (CAFs), through increased contractility and traction forces, can assemble aligned FN matrix which seem to regulate directional migration of cancer cells (Erdogan et al. 2017). The stretching of fibronectin can activate a mechanical response pathway also in normal fibroblasts (Friedland et al. 2009), even though induced mechanical extension of single FN fibers seems to limit the spreading and migration of endothelial cells (Hubbard et al. 2015).
In this chapter, we present and critically discuss the changes of phenotypes and behavior of different breast cancer cell lines (MCF-7, MDA-MB-231) and colon cancer cells (LoVo-R) in 3D cultures mimicking the natural ECM barriers to cancer invasion. To mimic the natural BM, we prepared a layer of Matrigel at standard concentration (0.18 μg/mL) for PCR analysis (Albini et al. 1987), and at higher concentration (3.0 μg/mL) for scanning electron microscope (SEM) observations, as at lower concentration, we never observed a continuous layer of this coating at SEM (Franchi et al. 2019). To reproduce the loose collagen meshwork below the BM (subpapillary and papillary dermis in skin, lamina propria in hollow organs or interstitial stroma in solid organs), we prepared low concentrated type I collagen network (50 μg/mL), whereas to mimic the deeper dense connective tissue we prepared high concentrated (3000 μg/mL) similar collagen on Millipore filters. We also tested FN (130 μg/mL) which functioning as ECM “biological glue” is critical for the attachment and guides directional movement of breast cancer cells (Yue 2014; Oudin et al. 2016).
Finally, just to mimic ECM collagen array of peri-tumoral denser connective tissues as described in TACS-II (collagen fibers arrayed parallel to the tumor boundary, i.e., orthogonal to the cancer cell invasion), we cultivated breast cancer cells on commercial lyophilized and compressed collagen membranes of tightly packed type I collagen fibers (Franchi et al. 2019).
10.2 2D Polystyrene Flask Cultures Partially Transformed in 3D Cultures Induce EMT in MCF-7 Breast Cancer Cells
The role that the physical aspect of substrate surface plays in governing the cancer cell phenotypes was evident when we casually observed an occasional line corresponding to a physical defect of some polystyrene flasks surface. An irregular culture surface may represent by itself a 3D substrate for both normal and cancer cells which become able to move in all spatial directions. When we use flat and smooth polystyrene flasks to cultivate cells, we perform 2D cultures. Where the flask surface was regular and very smooth, the low aggressive MCF-7 breast cancer cells grew exhibiting an epithelial shape and characteristics: cobblestone or flattened polygonal cells showed cell–cell contacts by short filopodia and some of them looked melted together by intercellular tight junctions. Only few globular isolated cells rich in cytoplasmic microvesiscles were detectable (Fig. 10.2a–d). But when the flask surface where cells were seeded showed a line, about 10 μm deep, the 2D substrate transformed the 2D cultures to 3D cultures and the cells which were very next to the flask line completely changed their shape exhibiting a morphological aggressive phenotype: these cells assuming an elongated or fusiform shape developed a morphological epithelial–mesenchymal transition (EMT). Moreover, some of them partially lost intercellular adhesiveness and seemed also to migrate and even cross the line. We demonstrated that changes of the physical aspect of the flask surface, such as a line, seem to induce migration in the low aggressive MCF-7 cells (Fig. 10.2a–d). They seem to adapt to the new microenvironment: to cross the line the cells develop a long filopodia, which exhibiting lateral short filopodia runs from one edge of the line to the other one (Fig. 10.2b) or a lamellipodia (Fig. 10.2d).
MCF-7 cells on polystyrene flask 2D culture observed at SEM. (a) MCF-7 cells appear like flattened and smooth epithelial polygonal cells in contact with each other by short filopodia or in tight contact so to appear melted. Very few globular isolated cells with cytoplasmic microvesicles are detectable (large arrow). On the right of the picture, an occasional and regular line of the flask surface is present. MCF-7 cells very next to the line assume a mesenchymal elongate shape (thin arrows) to cross from one side to the other of the line edges. Note that cells crossing the line do not adhere to the bottom of the line (White bar = 100 μm). (b) A higher magnification of the previous picture shows a crossing cell developing a long filopodia. The surrounding cells appear like epithelial poligonal flattened cells (White bar = 10 μm). (c) The MCF-7 cells next to the flask line partially lose their cell–cell contact, exhibit an elongated and fusiform shape and develop lamellipodia (large arrow) or long filopodia (thin arrow) which demonstrate that they are moving. All the other cells show an epithelial phenotype and look in contact with each other (White bar = 100 μm). (d) A higher magnification of the previous picture shows elongated cells crossing the line and developing filopodia or lamellipodia (White bar = 10 μm)
Cancer invasion consists of a translocation of the cancer cell body and must be considered as a heterogeneous and adaptive process of cancer cells involving morphological changes and generation of cell polarity (Pandya et al. 2017). Physical aspect (line) of a culture substrate can affect phenotypes of low-aggressive breast cancer MCF-7 cells which develop more aggressive morphological shapes. In particular, we observed that these cancer cells cultivated on flasks in 2D cultures appeared isolated and developed EMT phenotypes when they casually grew on an irregular line which transformed the 2D culture in a 3D one (Balachander et al. 2015).
10.3 MCF-7 Breast Cancer Cells in 2D and 3D Cultures (Millipore Filter, Concentrated Matrigel-Covered Millipore, Low Concentrated Type I Collagen-Covered Millipore and Membrane of Densely Packed Collagen Fibers)
To investigate if ECM can affect phenotypes of a low aggressive breast cancer cell line (MCF-7), we reproduced in vitro the biological barriers which cancer cells must invade in order to colonize distant organs. The first biological barrier of outer ECM which cancer cells have to breach is the BM. To obtain continuous layer of culture substrate mimicking the BM and visible at SEM, we covered a Millipore filter with a thick layer of Matrigel. Then we also investigated how others deeper matrix biological barriers, which were mimicked with different concentrations and array of type I collagen fibrils or using a membrane of densely collagen fibers, could induce changes of MCF-7 cancer cell phenotypes.
The BM is a specialized form of ECM which underlies or surrounds most tissues, including epithelial, endothelial, muscle, and adipose tissues. BM is a sheet-like structure of more than 200 nm thickness composed by two independent polymeric networks, one of laminin and one of type IV collagen, which are probably linked by several additional ECM proteins, including nidogen and perlecan (Breitkreutz et al. 2013; Jayadev and Sherwood 2017; Scott et al. 2019). Glycoproteins and PGs, including fibulin, hemicentin, SPARC, agrin, and type XVIII collagen are also present in BMs, creating biochemically and biophysically distinct structures serving different functions (Jayadev and Sherwood 2017). BM was described at the transmission electron microscope (TEM) as composed of two layers: the lighter-stained layer closer to the epithelium and called lamina lucida, and the denser-stained layer one closer to the connective tissue and called lamina densa.
BM physically supports epithelia but also acts like a tissue scaffold separating but also connecting two different tissues: BM laminin interacts with both integrins on epithelial cell surfaces and type VII collagen of stromal anchoring fibrils which interact with types I and III collagen fibrils of ECM. At the same time, also BM provides essential functions of barrier as it separates epithelial cells from stromal connective tissues: usually cells cannot pass through the very thin pores (10–140 nm) of this barrier without degrading it. BM is an important regulator of cell behavior because it sends signals to epithelial cells about the external microenvironment. Moreover, BM is also a component of blood vessels and represents an extracellular microenvironment sensor for endothelial cells in intravasation events of cancer cells (Kalluri 2003a, b). To mimic the natural BM, we prepared a highly concentrated (3.0 μg/mL) layer of Matrigel because at standard concentration (0.18 μg/mL), we never observed at SEM the physical presence of this coating. Matrigel mimics the because it contains laminin, entactin/nidogen, type IV collagen, and heparan sulfate proteoglycans. Moreover, we prepared a layer of low concentrated type I collagen (50 μg/mL) as coating for a Millipore filter so to reproduce the collagen array in ECM of loose connective tissues (subpapillary and papillary dermis, lamina propria, interstitial stroma).
Both 2D and all 3D cultures were observed at the SEM to evaluate the changes of cancer cells phenotypes growing on ECM components. Always function is related to shape but at the same time structural morphology depends on function. The morphological investigations on the shape of cancer cells allow us to better understand their behavior during invasion of the surrounding tissues and the biological events which lead to metastasis.
MCF-7 cells cultivated on smooth polystyrene substrate displayed epithelial phenotypes: cobblestone flattened polygonal shape with cell–cell contacts through many thin and short filopodia. No microvesicles were detectable on their cytoplasmic surface (Fig. 10.3a).
SEM analysis of MCF-7 cells. (a) MCF-7 cells cultivated on polystyrene flasks in 2D cultures show epithelial phenotypes with cell–cell contact through many thin and short filopodia. (b) MCF-7 cells on the Millipore filter in 3D cultures show a globular shape and are grouped together. They can easily pass through the free Millipore pores (arrows) (White bar = 10 μm). (c) MCF-7 cells on Millipore filter covered by a concentrated Matrigel (3.0 μg/mL) in 3D cultures. Concentrated Matrigel appears like a relatively thick and very smooth layer on which very grouped globular MCF-7 cells array in tight contact with each other. They intimately adhere to Matrigel and it seems that they are invaginating the collagen fibrils (large arrow). They develop cytoplasmic protrusions which might morphologically correspond to invadopodia (thin arrows) (White bar = 10 μm). (d) The same MCF-7 cells cultivated on a Millipore filter covered by low concentrated (50 μg/mL) type I collagen fibrils occluding all the Millipore filter pores in a 3D culture. More flattened and isolated cells show a mesenchymal elongated shape with large lamellipodia binding collagen fibrils (large arrows), and intercellular cytoplasmic connections which morphologically correspond to tunneling nanotubes (thin arrows) (White bar = 10 μm). (e) MCF-7 cells cultured on a commercial membrane of densely packed collagen fibers appear grouped with cell–cell contacts and show a globular shape, but develop many microvilli on their surface (White bar = 10 μm). (f) At higher magnification, a polygonal and globular cell adhering to the membrane of densely collagen fibers are in tight contact and develop many cytoplasmic microvilli (White bar = 10 μm)
When the same MCF-7 cells were cultivated in a 3D culture on a Millipore filter, they lost their flattened epithelial phenotype observed in 2D flask cultures. All cells still appeared gathered but exhibited a globular shape and developed a collective invasion ability through an ameboid movement when they crossed the Millipore holes (Fig. 10.3b).
This invasion mode was not directly observed when the same cells were seeded on a Millipore filter covered with concentrated Matrigel (3.0 μg/mL), which appeared like a relative thick and very smooth layer: MCF-7 cells still maintained strong cell–cell contacts but tried to invaginate the thick Matrigel layer and developed short invadopodia breaching the artificial basement membrane (Fig. 10.3c). It was reported that laminin receptors and collagen IV of BM can induce EMT thus favoring cancer progression (Scott et al. 2019).
When MCF-7 cells were cultivated on a Millipore filter covered by low concentrated (50 μg/mL) type I collagen, mimicking ECM of the loose interstitial connective tissues below the BM, the fibrils occluded all the Millipore filter pores thus partially limiting the invasion through an ameboid movement. MCF-7 cells completely changed their phenotypes as many of them looked like isolated cells exhibiting a mesenchymal elongated shape which suggested an EMT induced by collagen fibrils. Cells showed also large lamellipodia strongly adhering to collagen fibrils and binding to them, but other ones developed intercellular cytoplasmic connections morphologically corresponding to tunneling nanotubes (Fig. 10.3d).
If MCF-7 cells are cultivated on a membrane of densely packed fibers of type I collagen mimicking TACS-II, the stage of breast cancer with collagen fibers densely packed and parallel to the tumor boundary and no clinical metastasis, they show grouped globular and few polygonal-shaped cells with cell–cell contacts and short microvilli on their surface, but they seem unable to invade the collagen membrane (Fig. 10.3e, f) (Provenzano et al. 2008; Franchi et al. 2019).
10.4 MDA-MB-231 Breast Cancer Cells in 2D and 3D Cultures (Millipore Filter, Concentrated Matrigel-Covered Millipore, FN, Low and High Concentrated Type I Collagen-Covered Millipore and Membrane of Densely Packed Collagen Fibers)
To explore whether ECM can affect phenotypes of a high aggressive breast cancer cell line (MDA-MB-231 cells), we reproduced in vitro the biological barriers which cancer cells have to break and invade in vivo to develop metastasis. We reproduced the first biological barrier of outer ECM, the BM, by covering a Millipore filter with a thick layer of Matrigel, but to mimic the other deeper matrix biological barriers, we covered a Millipore filter with different concentrations and array of type I collagen fibrils or we used a collagen membrane of densely packed collagen fibers.
Both 2D and 3D cultures were then observed at SEM to detect eventual changes of cancer cells phenotypes and cytoplasmic protrusions when cells grow on different ECM components. When MDA-MB-231 cells are cultivated on smooth polystyrene flasks in 2D cultures, they show different isolated phenotypes exhibiting cytoplasmic microvesicles: elongated fusiform-shaped cells, globular ones, and few flattened polygonal ones (Fig. 10.4a). When the same cells are cultivated on a Millipore filter in 3D cultures, they do not change their phenotypes but exhibit more microvesicles on their cytoplasmic surface. Single isolated cells can migrate through the Millipore holes developing filopodia or lamellipodia (Fig. 10.4b). It is interesting to observe that MDA-MB-231 cell phenotypes do not drastically change from 2D to 3D cultures. The thick layer of Matrigel covering the Millipore filter and mimicking the BM does not induce any phenotypes changes in MDA-MB-231 cells even though cells seem to better adhere to the substrate and some of them develop ventral cytoplasmic protrusions which are morphologically comparable to invadopodia (Fig. 10.4c). This data confirms the results of Anguiano et al. (2017, 2020) who demonstrated that at high concentrations, Matrigel slows down cancer cells migration, possibly due to excessive attachment, whereas at low concentration, it may facilitates migration. From a morphological point of view, at the standard concentration, Matrigel distribution does not covers all the Millipore pores so indirectly allows free cancer cell migration.
SEM analysis of MDA-MB-231 cells. (a) MDA-MB-231 cells cultivated on polystyrene flasks in 2D cultures display different isolated phenotypes exhibiting cytoplasmic microvesicles: elongated-fusiform shaped cells, globular ones, and flattened polygonal ones (White bar = 100 μm). From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (b) MDA-MB-231 cells on Millipore filter in 3D cultures show the same phenotype described in flask cultures but microvesicles are more present. Individual cells are migrating through the free Millipore filter holes (White bar = 10 μm). (c) MDA-MB-231 cells in 3D cultures on concentrated Matrigel-covered Millipore. The three phenotypes observed in Millipore filter cultures are still visible: many isolated elongated-fusiform and globular cells and fewer flattened polygonal ones (White bar = 100 μm). (d) MDA-MB-231 cells in 3D cultures on low concentrated (50 μg/mL) type I collagen-covered Millipore. The three isolated previously described different phenotypes of MDA-MB-231 cells are still recognizable but show more microvesicles on their cytoplasmic surface. From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (e) MDA-MB-231 cells in 3D cultures on Millipore filter covered by fibronectin (130 μg/mL) occluding all filter holes. MDA-MB-231 cells cultured on fibronectin seem to be more grouped and better adhere to the substrate. They show many “cobblestone” flattened polygonal cells and globular-shaped ones, but only a few elongated ones. All cells exhibit many short filopodia or microvilli and microvesicles (White bar = 100 μm). From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (f) MDA-MB-231 cells in 3D cultures on Millipore filter covered by fibronectin (130 μg/mL). Polygonal cells show microvilli and appear to be connected by thin single TNTs (thin arrow) and forming thicker ones composed of single thin TNTs tightly bundled together (large arrows). On the right, a globular cell exhibits many microvesicles on the cytoplasmic surface (White bar = 10 μm). From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (g, h) MDA-MB-231 cells in 3D cultures on Millipore filter covered by high concentrated type I collagen (3000 μg/mL). Breast cancer cells grow in more than one layer, but no tight cell–cell contact is visible. Only the flattened polygonal cells lay in direct contact with the collagen fibrils, whereas both the elongated or fusiform cells and globular ones grow over the flattened ones. All cells show both microvilli and microvesicles. TNTs were apparently distinguishable in all phenotypes and long and thin filopodia originating from elongated cells exhibit exosomes and microvesicles (arrows) on their surface (White bar = 10 μm). From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (i) The MDA-MB-231 cells attached to densely packed and parallel collagen fibers include a few isolated flattened polygonal cells, globular and elongated or also “squid”-shaped ones developing lamellipodia. All cells produce many microvesicles. Thin intercellular connections corresponding to TNTs are visible between adjacent cells. From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release. (j) In areas where fibrils of the collagen membrane are more exposed, elongated and fusiform shaped cells appear arrayed parallel to the fibrils axis (White bar = 10 μm). From CELLS, 2020, 9, 2031, Franchi M. et al. Extracellular Matrix-Mediated Breast Cancer Cells Morphological Alterations, Invasiveness, and Microvesicles/Exosomes Release
The MDA-MB-231 cells growing on low concentrated type I collagen (50 μg/mL) network still show the same phenotypes described in previous cultures, but cells display more evident and numerous cytoplasmic microvesicles (Fig. 10.4d). As both Matrigel and low concentrated collagen meshwork do not affect MDA-MB-231 phenotypes, we investigated in our experiments if FN, another ECM fibrillar component, could affect breast cancer phenotypes. Differently from previous samples, MDA-MB-231 cells cultured on fibronectin show many “cobblestone” flattened polygonal cells and globular shaped ones and only few elongated ones mainly growing on the previous ones. All cells appear more grouped with cell–cell contacts but exhibit many microvesicles and microvilli (Fig. 10.4e). Some of them are connected by thin single and thicker composed intercellular cytoplasmic protrusions which are morphologically comparable to tunneling nanotubes (TNTs) (Franchi et al. 2020a) (Fig. 10.4f). These data are explained considering that tested FN is arrayed in a network, so that the main effect of FN is just to favor cell adhesion. Only highly aligned FN is strongly related with EMT and high-speed migration (Wang et al. 2018). However, the presence of many microvesicles and the intercellular connections (TNTs) which allow a direct transfer of microvesicles and mitochondria between the connected cells suggest an increased metabolic activity in MDA-MB-231 cells. The observation of an increased number of polygonal cell phenotypes, which showing many microvesicles cannot be morphologically considered as low aggressive cells, suggest MDA-MB-231 cells develop a high adhesion to the FN substrate. Park and Helfman (2019) demonstrated that MDA-MB-231 cells develop a high FN expression in 3D suspension culture and an increase of FN facilitates cell-attachment via integrin β-5. FN matrix can affect both cancer cells phenotypes and guide migration via integrins which connecting FN fibrils to cell’s cytoskeleton might act as “stretch sensors” representing a “mechanical continuity” between the inner and outer environment of the cells (Kular et al. 2014; Oudin et al. 2016).
To observe possible stronger phenotypic changes, we covered the Millipore filter with higher concentrated type I collagen (3000 μg/mL). In these cultures, the previously described phenotypes showing both microvilli and microvesicles are equally distributed and grow in more than one layer: both elongated cells showing a fusiform shape and globular ones lay on flattened and polygonal ones which are the only ones in direct contact and adhering to the collagen fibrils. In elongated or fusiform cells, the higher concentration of type I collagen seems to induce the development of long and thin filopodia with exosomes and microvesicles on their surface. All phenotypes show microvilli and microvesicles (Fig. 10.4g, h). The higher concentration of collagen fibrils seems to further favor the metabolic activity and adhesion of MDA-MB-231 cells.
To mimic the collagen fiber array described in TACS-II (collagen fibers run parallel to the tumor boundary, i.e., orthogonal to the direction of cancer cell invasion) and corresponding to patient with no metastasis, we cultivated breast cancer cells on a commercial lyophilized and compressed membrane of tightly packed type I collagen fibers. It was described that at this stage, the remodeled collagen arrangement does not allow breast cancer cell invasion both in vivo and in vitro (Provenzano et al. 2008; Franchi et al. 2019). Cells include very few isolated flattened polygonal cells adhering to collagen fibrils of the membrane, globular and many elongated-fusiform ones and “squid”-shaped ones showing lamellipodia. All cells show microvesicles and TNTs (Fig. 10.4i). Where collagen fibrils are more exposed the fusiform cells are arrayed parallel to the fibril axis (Fig. 10.4j) (Franchi et al. 2020a).
10.5 Migration Test and Real-Time PCR of MCF-7 and MDA-MB-231 Cells
The migration/invasion process of cancer cells is the expression of their invasiveness properties. MDA-MB-231 cells have a higher ability in migrating/invading vs. MCF-7 cells, thus confirming the worst clinical prognosis of some patients. BM (Matrigel at standard concentration: 0.18 μg/mL) seems not to strongly affect both MCF-7 and MDA-MB-231 breast cancer cells phenotypes because when they are cultivated on both Millipore filter and Matrigel-covered Millipore filter all cells show the same rate of migration. However, when cells grow on collagen fibrils network-covered Millipore filter, MDA-MB-231 cells show a higher invasion capacity, whereas MCF-7 cells even decrease their ability in penetrating the barrier of collagen fibrils (Fig. 10.5). This different behavior between the different cancer cell lines in contact with collagen might be explained by the strong and higher increase of MMP-2 and MMP-9 expression observed in MDA-MB-231 but not in MCF-7 (Fig. 10.6). It is well known that the release of MMPs from cancer cells cause an ECM digestion. This suggests an individual mesenchymal protease-dependent invasion mode for the MDA-MB-231 cultivated on a collagen network which instead represents a resistant biological barrier for the collective ameboid-dependent invasion of the MCF-7 cells (Bozzuto et al. 2015). In fact, if MCF-7 cells did not follow a protease-dependent invasion mode which creates wide spaces in ECM through MMPs of invadopodia, the very small pores size of the relative dense collagen network could not allow the crossing of cancer cell nuclei (Wolf et al. 2013). Anyway, collagen substrate seems to affect the MCF-7 cells phenotypes which show mesenchymal, elongated, or fusiform phenotypes (Fig. 10.3c): in fact, they display a VIM and FN-expression improvement and loss of cell–cell contacts as confirmed by a strong decrease of E-cadherin which was not observed in MDA-MB-231 cells collagen group (Khalil et al. 2017) (Fig. 10.6). It was reported that cadherin complexes act also as mechano-transducers that can sense changes in tension and trigger adaptive reinforcement of intercellular junctions (Leckband and de Rooij 2014).
Migration of breast cancer cells cultured on different substrates. MDA-MB-231 and MCF-7 cells were seeded on Millipore filters or Millipore filters covered with Matrigel (0.18 μg/mL) or collagen type I and incubated for 5 h. Double asterisks indicate statistically significant differences (p ≤ 0.01). From J. Clin. Med. 2019, 8, 213, Franchi M. et al., Collagen Fiber Array of Peritumoral Stroma Influences Epithelial-to-Mesenchymal Transition and Invasive Potential of Mammary Cancer Cells
Type I collagen induces striking changes in EMT markers and significant alterations in the expression of ECM components of breast cancer cells. Real-time PCR analysis of a-SMA, E-cadherin, vimentin, fibronectin, MMP-2 and MMP-9 on MDA-MB-231 and MCF-7 cells seeded on uncoated Millipore filter or filter covered with collagen type I and incubated for 24 h. Expression was normalized to GAPDH expression. Single and double asterisks indicate statistically significant differences (p ≤ 0.05 and p ≤ 0.01, respectively). From J. Clin. Med. 2019, 8, 213, Franchi M. et al., Collagen Fiber Array of Peritumoral Stroma Influences Epithelial-to-Mesenchymal Transition and Invasive Potential of Mammary Cancer Cells
10.6 Collagen as a Triggering Factor Inducing EMT in Breast Cancer Cells
The irregular surface of 3D cultures represents the first factor favoring the EMT of breast cancer cells, particularly evident in low aggressive (MCF-7) vs. higher aggressive (MDA-MB-231) cells, but also in 3D cultures, Matrigel (BM) does not affect so much the morphological phenotypes of all breast cancer cells. This data may be explained by the fact that even cancer cells like all normal epithelial cells lie, adhere, and grow in direct physical contact with a very flat and smooth scaffold, which epithelial cells sense and recognize as the BM (a smooth 2D surface). But when even some of the low aggressive MCF-7 cells lose their cell–cell contacts and breach, the BM they come in contact with a new unknown microenvironment represented by the ECM: very rough and porous collagen fibril loose meshwork, GAGs, PGs, glycoproteins, and water. They find a new and never sensed irregular and hostile physical microenvironment, so they adapt their phenotypes by developing cytoplasmic protrusions and phenotype changes which allow them to best invade ECM and reach vessels to provide nutrients. We can say that collagen itself induces morphological EMT in MCF-7 cells even though it could not enhance cell’s ability to perform clinical metastasis, as it does not improve the production of MMP2 and MMP9 which allow cancer cells to penetrate lymphatic and blood vessels in metastatic process. This is confirmed by Invasion Test data which show that MCF-7 cells invasion decreases in collagen cultures, vs. Millipore and Matrigel substrates.
A molecular EMT in MCF-7 cultivated on type I collagen meshwork was, however, confirmed by a strong decrease of E-cadherin and an increase of both VIM and FN-expression. In conclusion, MCF-7, usually preferring a collective ameboid-dependent migration by squeezing through pliable barriers, could find a valid barrier in the irregular and resistant collagen network (Christiansen and Rajasekaran 2006; Bozzuto et al. 2015).
Deposition of collagen in human solid tumors is associated with higher incidence of metastasis (Ramaswamy et al. 2003). Even though collagen seems to not markedly promote morphological changes or EMT in MDA-MB-231 phenotypes, type I collagen fibrils even at low concentration are able to strongly improve MDA-MB-231 cells migration vs. the same cells cultivated in Millipore filter or in Matrigel-covered Millipore filter. Also, real-time PCR shows that type I collagen slightly promoted VIM-expression, but reveals a strong increase of α-SMA expression, FN-expression, MMP-2, and MMP-9 expression. The physical impact with the sub-BM collagen network could itself represent a “shock” for MDA-MB-231 cells which try to improve their invasiveness ability by increasing the production of MMPs. Moreover MDA-MB-231 cells showed at SEM a slight development of cytoplasmic microvesicles which contain also MMPs as reported in literature (Rilla et al. 2014).
Highly invasive MDA-MB-231 cells can induce metastasis in vivo so they are also capable of invading the deeper ECM including a higher concentration of collagen. In Millipore filter covered by high concentrated type I collagen (3000 μg/mL) MDA-MB-231 flattened cells strongly adhere to the collagen network; on these cells, globular and elongated mesenchymal cells grow and develop microvilli, microvesicles, and TNTs which suggest an increased invasive potential (Franchi et al. 2020b). Also, when MDA-MB-231 cells were cultivated on FN-covered Millipore filter, they developed a higher number of flattened cells, expression of a good adhesion to FN, but showed a uniform and complete distribution of microvesicles on their cytoplasmic surface (Byrne et al. 2021). These different aspects in the same cells agree with the consideration that transition to an aggressive malignant phenotype is not an “all or nothing” event, so that we could not always observe morphological pure epithelial or pure mesenchymal phenotypes (Christiansen and Rajasekaran 2006).
Collagen and in particular the collagen fibrils/fibers array in tumor microenvironment plays a fundamental role in regulating tumor development and cancer cell invasion. Maller et al. (2013) found that collagen architecture in pregnancy can induce protection from breast cancer. They demonstrated that collagen organization, rather than density alone, is a fundamental contributor to induce an invasive phenotype. In fact, high density nonfibrillar type I collagen seems to suppress the tumor development by increasing junctional E-cadherin, upregulation of cell–cell junction genes, and downregulation of mesenchymal and metalloproteinase genes, whereas aligned fibrillar type I collagen favor cellular aggressive cancer cells phenotypes in mammary tumor cells and alters β1 integrin subcellular distribution.
Considering the particular peri-tumoral collagen array described in TACS-II and including the densely packed collagen fibers parallel to each other and to the tumor boundary, both MCF-7 and MDA-MB-231 cells seem to be unable to penetrate the collagen membrane used to mimic histological TACS-II stage. This ECM response is mediated by CAFs which seem to play an important role in changing the collagen array of tumor ECM: firstly opposing to cancer cell invasion (TACS-I and TACS-II) and then favoring the cancer cell invasion (TACS-III) (Provenzano et al. 2008; Egeblad et al. 2010; Conklin et al. 2011; Luhr et al. 2012; Bredfeldt et al. 2014; Costanza et al. 2017; Franchi et al. 2019, 2020a). Densely packed and parallel collagen fibers array observed in TACS-II are usually described in other anatomical situations and sites: the response of ECM in foreign body granuloma develops a tissue-encapsulation to limit diffusion of exogenous material by sheets of collagen fibers running parallel to the implant surface. Moreover, gingival ECM around titanium dental implants contains densely packed collagen fibers which following a circular array around the neck of the implants are presumably able to physically opposite virus and bacteria invasions from the oral plaque (Ruggeri et al. 1992, 1994). Which and how do the mechanical events which favor or also induce changes of collagen array in tumor ECM from TACS-II to TACS-III act? The densely packed, straight, and parallel collagen fibers array described in TACS-II are comparable to that of tendons. Tendon collagen fibers resist tension but when they are compressed, tenocytes change their phenotypes and ECM responds by developing a fibrocartilage, which protect both tenocytes and collagen fibers integrity. In particular, compressed tenocytes produce large amount of large PGs like aggrecan and versican which linking significant amount of water oppose compression (Docking et al. 2013). However, considering the peri-tumoral microenvironment in cancer, HA acts as a modulator of the tumor microenvironment through signal transduction mechanisms, but also regulating the hydration and osmotic balance in tumor microenvironment. We also know that a very hydrated peri-tumor ECM could create interfibers spaces where cancer cells enter to invade the surrounding deeper tissue and a HA synthesis is increased in different cancers, such as breast, prostate, lung, colon, and ovarian (Tavianatou et al. 2019, 2021). Moreover, HA can increase the integrin-mediated transduction thus favoring cancer cell adhesion and invasion (Chopra et al. 2014).
If epithelial cell dissociation or loss of cell–cell adhesion related to E-cadherin decrease and changes of ECM physical array are the main factors which favor cancer cell invasion, clinical data suggest that cancer progression and metastasis occur also without E-cadherin deregulation (Khalil et al. 2017). Thus, the collagen fiber array in peri-tumor microenvironment seems to be the first actor in affecting tumor development and cancer cell invasion. The epithelial E-cadherin-positive MCF-7 cells, lacking the expression of membrane type 1-matrix metalloproteinase 1 (MT1-MMP)/MMP14) and not possessing the ability to proteolytically remodel the ECM, are able to invade collectively the ECM when they find a low dense collagen network rich in relatively wide spaces. Interestingly, repressing E-cadherin MCF-7 cells loose cell–cell contacts but do not invade high-density collagen which they can cross only when the MT1-MMP/MMP14 is ectopically expressed (Ilina et al. 2020).
10.7 LoVo-R Colon Cancer Cells in 2D Cultures and 3D Cultures (Matrigel-Covered Millipore, High Concentrated Type I Collagen-Covered Millipore)
The tumor microenvironment and in particular collagen array play an “epigenetic” role in influencing primary tumor growth, migration, and metastatic potential, but also can favor the ability of cancer cells to resist chemotherapy (Provenzano et al. 2008; Conklin et al. 2011; Franchi et al. 2019; Montagner and Dupont 2020). ECM concentration is an important and crucial parameter to evaluate drug screening. An increase of collagen concentration in 3D microenvironment induces an increase of the intracellular stiffness and motor activity of cancer cells and seems to influence the intracellular fluctuations even in the presence of chemotherapeutic and anti-MMP drugs (Kim et al. 2018). To evaluate the possible role that collagen can play in influencing the drug resistance in cancer, we cultivated a colon cancer cell line which is resistant to doxorubicin (LoVo-R) in a Matrigel-covered Millipore filter (control) and in a concentrated type I collagen network (3000 μg/mL). LoVo-R cells cultivated on Matrigel mimicking the basement membrane appeared grouped with relative cell–cell contacts through intercellular thin and short cytoplasmic processes; they exhibited a smooth surface and a polygonal and flattened shape which resemble epithelial cells phenotype (Fig. 10.7a, b). The same cells cultivated on highly concentrated collagen showed a rounded shape and assembled in groups of few cells but some of them appeared isolated and showed a particular phenotype which resembles a “donut” shape (Fig. 10.7c, d). These cells displayed thin and short cytoplasmic protrusions which were in tight contact with the collagen fibrils or connected adjacent cells. We suggest that these cells were invading the collagen fibrils layer through a “funnel” invagination (Fig. 10.7e). From sectioned areas of the collagen-covered Millipore filter, we were able to detect thin and short cytoplasmic protrusions which developing from the ventral side of some cells penetrated the collagen fibrils network and morphologically corresponded to invadopodia (Fig. 10.7f). Moreover, a loss of collagen next to the cytoplasmic protrusions or invadodia suggests that a proteolitic activity next to the same protrusions occurred.
SEM analysis of LoVo-R cells. (a) LoVo-R cells cultivated on a Matrigel-covered Millipore filter show a smooth surface and a polygonal-flattened shape like normal epithelial cells (White bar = 100 μm). (b) They appear distributed in a single cell layer and grouped with cell–cell contacts through intercellular thin and short cytoplasmic processes (White bar = 10 μm). (c) LoVo-R cells on high concentrated type I collagen (3000 μg/mL)-covered Millipore filter show rounded-shaped phenotypes assembled in small groups (White bar = 100 μm). (d) Some cells appear isolated and exhibit a particular phenotype that resembles a “donut” shape (White bar = 10 μm). (e) At a higher enlargement the “donut”-shaped cells show thin and short cytoplasmic protrusions in tight contact with the collagen fibrils or connecting adjacent cells (arrows). These cells are invading the collagen fibrils layer through a “funnel” invagination (Co = collagen) (White bar = 10 μm). (f) A lateral view of a sectioned collagen-covered Millipore filter shows that LoVo-R cells cultivated on high concentrated type I collagen (3000 μg/mL)-covered Millipore filter develop thin and short cytoplasmic protrusions from their ventral side which are penetrating the collagen fibrils network. These cytoplasmic protrusions correspond to invadopodia degrading adjacent collagen fibrils (arrows) (Co = collagen) (White bar = 10 μm)
The ultrastructural data of LoVo-R cells cultivated in Matrigel or collagen substrates suggest that type I collagen induces EMT with drastic morphological changes of phenotypes observed in BM cultures: cells on collagen appeared more isolated and invading the collagen layer by developing invadopodia.
All these data suggest that collagen type I inducing an increase of cancer cells aggressiveness could also play a key role in favoring the development of a drug resistance. In fact, the previously described shock of MCF-7 and MDA-MB-231 cells when come in contact with the rough and irregular sub-BM microenvironment, could affect also LoVo-R cells, which developing a more aggressive phenotype could further increase their intrinsic resistance to therapeutic treatments. The development of drug resistance is a significant complication to successful of therapeutic procedures and seems partially favored by type I collagen composition of peri-tumoral ECM, which can significantly vary from patient to patient like clinical results suggest. The question is how can collagen improve cancer cells resistance to therapy? This could be partially explained because T-cell proliferation significantly reduces in a high-density matrix when compared to a low-density one (Kuczek et al. 2019). Other researchers suggest that tumor microenvironment could control the transport and thus efficacy of free doxorubicin in vitro (Brancato et al. 2018). Drug resistance is related to cancer cell lines but also tumor microenvironment: MDA-MB-231 cells displayed a stiffness-dependent response to the chemotherapeutic doxorubicin, whereas low aggressive MCF7 breast carcinoma cells cultured in the same conditions did not exhibit this stiffness-dependent resistance to the drug (Joyce et al. 2018). Anyway, the role of tumor ECM in modulating elasticity, adhesion, senescence, and EMT of MDA-MB-231 cells cancer cells seems associated with an improving of integrins upregulations (Poincloux et al. 2011; Mierke et al. 2011; Brandão-Costa et al. 2020; Byrne et al. 2021). Integrins are transmembrane proteins that physically connect cells to different proteins of ECM like fibronectin, vitronectin, collagens, and laminins but also to other cell surface receptors (Hynes 2002; Ringer et al. 2017). If the cadherin-based adherens junctions transduce the intercellular stresses (Leckband and de Rooij 2014), both chemical composition and all mechanical properties of the ECM are sensed by multimolecular complexes which are called focal adhesions (FAs) and include integrin receptors associated with the ECM (Geiger et al. 2009; Case and Waterman 2015). In particular, Ringer et al. (2017) described an outer FA layer including ECM-specific anchorage by integrin receptors, an intermediate layer where chemical and mechanical signals are processed, and an inner layer that is dominated by the actomyosin cytoskeleton of cells (Ringer et al. 2017). FAs complexes, linking integrins to the actin cytoskeleton either directly or indirectly by interacting with vinculin and α-actinin, act as mechanically elastic springs which enforce by talin unfolding when mechanical tension increases but remain small and short-lived when forces decrease in ECM. Therefore, they allow FAs to transmit the chemo-mechanical stimuli from ECM to the inner actomyosin cytoskeleton (Ringer et al. 2017). The main role of type I collagen in affecting the tumor progression is also supported by the fact that cells adhering to collagen type I by integrin α2β1 induce a very different signaling response compared to cells which bind collagen type IV with α1β1 integrin (Ivaska et al. 1999; Borza et al. 2012,; Ringer et al. 2017). To support the role for integrin expression and activation in regulating the development of oncogenic processes, it was reported that also hyaluronan, a soft polymeric glycosaminoglycan ECM component which is also considered a marker of breast cancer, can affect the cellular response by increasing the integrin mechano-transduction, thus suggesting the interaction of signaling between hyaluronan receptors and specific integrins. In particular, hyaluronan augments or overrides mechanical signaling by some classes of integrins to produce a spread morphology of cells otherwise observed only on very rigid substrates (Chopra et al. 2014). It is evident that in further experiments, it will be necessary to reproduce the in vivo conditions and include most of the ECM components in 3D cultures. Even though we explored the critical role of collagen and FN in affecting cancer cell phenotype and behavior vs. the BM, further investigations concerning the other molecules of ECM will help to better understand how tumor microenvironment could play a primary role in regulating cancer cell invasion. It is also plausible that only through evaluation and comparison of the interplay among all different ECM components, we will be able to suggest innovative therapeutic strategies to prevent or limit cancer invasion.
10.8 Conclusions: Take Home Message
-
1.
Just a physically irregular surface of a culture substrate can transform 2D to 3D cultures simply because cells are free to move in all three spatial directions and may induce EMT in the low aggressive MCF-7 breast cancer cells.
-
2.
In 3D cultures, a thick layer of Matrigel mimicking the BM does not promote changes in morphological phenotypes of both low aggressive MCF-7 and very aggressive MDA-MB-231 cells, probably because all epithelial cells recognize the smooth BM on which they usually grow.
-
3.
In 3D cultures, a loose network of type I collagen fibrils mimicking ECM of sub-BM induces different effects on low aggressive MCF-7 cells vs. very aggressive MDA-MB-231 ones. Collagen favors the development of mesenchymal phenotypes morphology in MCF-7 cells but limits the invasion ability of the same cells if compared to Matrigel cultures, as collagen induces a reduction in MMPs production in cells preferring an ameboid-invasion mode. On the contrary, type I collagen fibrils do not improve the EMT-related morphological changes in MDA-MB-231 cells which, however, in invasion test, show a strong increased ability to invade the collagen layer if compared to the same cells cultivated on Matrigel, as collagen seems to stimulate MMPs production.
-
4.
In 3D cultures, nonaligned FN favors both MCF-7 and MDA-MB-231 cancer cells adhesion by developing more flattened and polygonal cells suggesting that nonaligned FN favors cancer cells adhesion. The increase of cytoplasmic microvesicles and the development of TNTs suggest an improve of cell–cell communications.
-
5.
In 3D cultures, high concentrated type I collagen fibrils mimicking the deeper ECM induce breast cancer cells to grow in more than one layer, thus suggesting that concentrated collagen favors a further adhesion of cancer cells. The development of microvilli, microvesicles, long filopodia, and TNTs suggests that collagen may also stimulate communications among both adjacent and distant cells.
-
6.
In 3D cultures, densely packed and parallel collagen fibers mimicking TACS-II stage in mammary tumor progression contrast both MCF-7 and MDA-MB-231 breast cancer cells invasion.
-
7.
In 3D cultures of high concentrated type I collagen network, the LoVo-R colorectal cancer cells, resistant to doxorubicin, develop new morphological invaginating phenotypes and invadopodia. These morphological aspects suggest that the increased invasion ability of cancer cells could be related to the drug resistance.
-
8.
Collagen, also in different arrays, could act as a physical factor inducing EMT in MCF-7 and MDA-MB-231 cells and drug resistance in LoVo-R cells.
References
Albini A, Iwamoto Y, Kleinman HK, Martin GR, Aaronson SA, Kozlowski JM, McEwan RN (1987) A rapid in vitro assay for quantitating the invasive potential of tumor cells. Cancer Res 47:3239–3245
Anguiano M, Castilla C, Maska M, Ederra C, Pelaez R, Morlaes X, Munoz-Arrieta G, Mujika M, Kozubek M, Munoz-Barrutia A, Rouzaut A, Arana S, Garcia-Aznar JM, Ortiz-De-Solorzano C (2017) Characterization of three-dimensional cancer cell migration in mixed collagen-Matrigel scaffolds using microfluidics and image analysis. PLoS One 12(2):e0171417. https://doi.org/10.1371/journal.pone.0171417
Anguiano M, Morales X, Castilla C, Pena AR, Ederra C, Martinez M, Ariz M, Esparza M, Amaveda H, Mora M, Movilla N, Garcia-Aznar JM, Cortes-Dominquez I, Ortiz-De-Solorzano C (2020) The use of mixed collagen-Matrigel matrices of increasing complexity recapitulates the biphasic role of cell adhesion in cancer cell migration: ECM sensing, remodeling and forces at the leading edge of cancer invasion. PLoS One 15(1):e0220019. https://doi.org/10.1371/journal.pone.0220019
Baker EL, Srivastava J, Yu D, Bonnecaze RT, Zaman MH (2011) Cancer cell migration: integrated roles of matrix mechanics and transforming potential. PLoS One 6(5):e20355. https://doi.org/10.1371/journal.pone.0020355. Epub 2011 May 27
Balachander GM, Balaji SA, Rangarajan A, Chatterjee K (2015) Enhanced metastatic potential in a 3D tissue scaffold toward a comprehensive in vitro model for breast cancer metastasis. ACS Appl Mater Interfaces 7(50):27810–27822. https://doi.org/10.1021/acsami.5b09064. Epub 2015 Dec 8
Balkwill FR, Capasso M, Hagemann T (2012) The tumor microenvironment at a glance. J Cell Sci 125:5591–5596
Baskaran JP, Weldy A, Guarin J, Munoz G, Shpilker PH, Kotlik M, Subbiah N, Wishart A, Peng Y, Miller MA, Cowen L, Oudin MJ (2020) Cell shape, and not 2D migration, predicts extracellular matrix-driven 3D cell invasion in breast cancer. APL Bioeng 4:026105. https://doi.org/10.1063/1.5143779
Borza CM, Su Y, Chen X, Yu L, Mont S, Chetyrkin S, Voziyan P, Hudson BG, Billings PC, Jo H, Bennett JS, Degrado WF, Eckes B, Zent R, Pozzi A (2012) Inhibition of integrin alpha2beta1 ameliorates glomerular injury. J Am Soc Nephrol 23(6):1027–1038
Bozzuto G, Condello M, Molinari A (2015) Migratory behaviour of tumour cells: a scanningelectron microscopy study. Ann Ist Super Sanita 51(2):139–147. https://doi.org/10.4415/ANN_15_02_12
Brabek J, Mierke CT, Rosel D, Vesely P, Fabry B (2010) The role of the tissue microenvironment in the regulation of cancer cell motility and invasion. Cell Commun Signal 8:22. http://www.biosignaling.com/content/8/1/22
Brandão-Costa RM, Helal-Neto E, Vieira AM, Barcellos-de-Souza P, Morgado-Diaz J, Barja-Fidalgo C (2020) Extracellular matrix derived from high metastatic human breast cancer triggers epithelial-mesenchymal transition in epithelial breast cancer cells through αvβ3 integrin. Int J Mol Sci 21:2995. https://doi.org/10.3390/ijms21082995
Bredfeldt JS, Liu Y, Conklin MW, Keely PJ, Mackie TR, Eliceiri KW (2014) Automated quantification of aligned collagen for human breast carcinoma prognosis. J Pathol Inform 5:28. https://doi.org/10.4103/2153-3539.139707
Breitkreutz D, Koxolt I, Thiemann K, Nischt R (2013) Skin basement membrane: the foundation of epidermal integrity—BM functions and diverse roles of bridging molecules nidogen and Perlecan. BioMed Res Int 2013:179784. https://doi.org/10.1155/2013/179784
Byrne CE, Decombe JB, Bingham GC, Remont J, Miller LG, Khalif L, King T, Hamel K, Bunnell BA, Burow ME, MA E.C. (2021) Evaluation of extracellular matrix composition to improve breast cancer modeling. Tissue Eng Part A 27(7-8):500–511. https://doi.org/10.1089/ten.TEA.2020.0364
Case LB, Waterman CM (2015) Integration of actin dynamics and cell adhesion by a three-dimensional, mechanosensitive molecular clutch. Nat Cell Biol 17(8):955–963
Chopra A, Murray ME, Byfield FJ, Mendez MG, Halleluyan R, Restle DJ, Raz-Ben Aroush D, Galie PA, Pogoda K, Bucki R, Marcinkiewicz C, Prestwich GD, Zarembinski TI, Chen CS, Pure E, Kresh JY, Janmey PA (2014) Augmentation of integrin-mediated mechanotransduction by hyaluronic acid. Biomaterials 35(1):71–82
Christiansen JJ, Rajasekaran AK (2006) Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res 66:8319–8326
Conklin MW, Eickhoff JC, Riching KM, Pehlke CA, Eliceiri KW, Provenzano PP, Friedl A, Keely PJ (2011) Aligned collagen is a prognostic signature for survival in human breast carcinoma. Am J Pathol 178:1221–1232. https://doi.org/10.1016/j.ajpath.2010.11.076
Costanza B, Umelo IA, Bellier J, Castronovo V, Turtoi A (2017) Stromal modulators of TGF-beta in cancer. J Clin Med 6:7. https://doi.org/10.3390/jcm6010007
Docking S, Samiric T, Scase E, Purdam C, Cook J (2013) Relationship between compressive loading and ECM changes in tendons. Muscles Ligaments Tendons J 3(1):7–11. https://doi.org/10.11138/mltj/2013.3.1.007. Published online 2013 May 21
Egeblad M, Rasch MG, Weaver VM (2010) Dynamic interplay between the collagen scaffold and tumor evolution. Curr Opin Cell Biol 22:697–706. https://doi.org/10.1016/j.ceb.2010.08.015
Erdogan B, Ao M, White LM, Means AL, Brewer BM, Yang L, Washington MK, Shi C, Franco OE, Weaver AM, Hayward SW, Li D, Webb J (2017) Cancer-associated fibroblasts promote directional cancer cell migration by aligning fibronectin. Cell Biol 216(11):3799–3816. https://doi.org/10.1083/jcb.201704053. Epub 2017 Oct 11
Foster DS, Jones RE, Ransom RC, Longaker MT, Norton JA (2018) The evolving relationship of wound healing and tumor stroma. JCI Insight 3:e99911
Fouad YA, Aanei C (2017) Revisiting the hallmarks of cancer. Am J Cancer Res 7:1016–1036
Franchi M, Fini M, Quaranta M, De Pasquale V, Raspanti M, Giavaresi G, Ottani V, Ruggeri A (2007) Crimp morphology in relaxed and stretched rat Achilles tendon. J Anat 210(1):1–7
Franchi M, Quaranta M, Macciocca M, De Pasquale V, Ottani V, Ruggeri A (2009) Structure relates to elastic recoil and functional role in quadriceps tendon and patellar ligament. Micron 40(3):370–377
Franchi M, Ottani V, Stagni R, Ruggeri A (2010) Tendon and ligament fibrillar crimps give rise to left-handed helices of collagen fibrils in both planar and helical crimps. J Anat 216(3):301–309
Franchi M, Masola V, Bellin G, Onisto M, Karamanos KA, Piperigkou Z (2019) Collagen fiber array of peritumoral stroma influences epithelial-to-mesenchymal transition and invasive potential of mammary cancer cells. J Clin Med 8:213. https://doi.org/10.3390/jcm8020213
Franchi M, Piperigkou Z, Karamanos K-A, Franchi L, Masola V (2020a) Extracellular matrix-mediated breast cancer cells morphological alterations, invasiveness, and microvesicles/exosomes release. Cells 9(9):2031
Franchi M, Piperigkou Z, Riti E, Masola V, Onisto M, Karamanos NK (2020b) Long filopodia and tunneling nanotubes define new phenotypes of breast cancer cells in 3D cultures. Matrix Biol Plus 6-7:100026
Friedl P, Brocker EB (2000) The biology of cell locomotion within threedimensional extracellular matrix. Cell Mol Life Sci 57:41–64
Friedl P, Wolf K (2010) Plasticity of cell migration: a multiscale tuning model. J Cell Biol 188:11–19
Friedl P, Locker J, Sahai E, Segall JE (2012) Classifying collective cancer cell invasion. Nat Cell Biol 14:777–783
Friedland JC, Lee MH, Boettiger D (2009) Mechanically activated integrin switch controls alpha5beta1 function. Science 323:642–644
Geiger B, Spatz JP, Bershadsky AD (2009) Environmental sensing through focal adhesions. Nat Rev Mol Cell Biol 10(1):21–33
Hubbard B, Buczek-Thomas JA, Nugent MA, Michael L, Smith ML (2015) Fibronectin fiber extension decreases cell spreading and migration. J Cell Physiol 231(8):1728–1736. https://doi.org/10.1002/jcp.25271. Epub 2015 Dec 28
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110(6):673–687
Ilina O, Gritsenko PG, Syga S, Lippoldt J, La Porta CAM, Chepizhko O, Grosser S, Vullings M, Bakker G-J, Starruß J, Bult P, Zapperi S, Käs JA, Deutsch A, Friedl P (2020) Cell-cell adhesion and 3D matrix confinement determine jamming transitions in breast cancer invasion. Nat Cell Biol 22(9):1103–1115. https://doi.org/10.1038/s41556-020-0552-6. Epub 2020 Aug 24
Ivaska J, Reunanen H, Westermarck J, Koivisto L, Kahari VM, Heino J (1999) Integrin alpha2beta1 mediates isoformspecific activation of p38 and upregulation of collagen gene transcription by a mechanism involving the alpha2 cytoplasmic tail. J Cell Biol 147(2):401–416
Jayadev R, Sherwood DR (2017) Basement membranes. Curr Biol 27:R207–R211
Joyce MH, Lu C, James ER, Hegab R, Allen SC, Suggs LJ, Brock A (2018) Phenotypic basis for matrix stiffness-dependent chemoresistance of breast cancer cells to doxorubicin. Front Oncol 8:337. https://doi.org/10.3389/fonc.2018.00337
Kalluri R (2003a) Basement membranes: structure, assembly and role in tumour angiogenesis. Nat Rev Cancer 3:422–433
Kalluri R (2003b) Basement membranes: structure, assembly and role in tumour angiogenesis. Nat Rev Cancer 3(6):422–433. https://doi.org/10.1038/nrc1094
Karamanos NK, Piperigkou Z, Passi A, Götte M, Rousselle P, Vlodavsky I (2021) Extracellular matrix-based cancer targeting. Trends Mol Med 27(10):1000–1013
Khalil AA, Ilina O, Gritsenko PG, Bult P, Span PN, Friedlc P (2017) Collective invasion in ductal and lobular breast cancer associates with distant metastasis. Clin Exp Metastasis 34:421–429. https://doi.org/10.1007/s10585-017-9858-6
Kim JE, Reynolds DS, Zaman MH, Mak M (2018) Characterization of the mechanical properties of cancer cells in 3D matrices in response to collagen concentration and cytoskeletal inhibitors. Integr Biol (Camb) 10(4):232–241. https://doi.org/10.1039/c8ib00044a
Koch TM, Munster S, Bonakdar N, Butler JP, Fabry B (2012) 3D traction forces in cancer cell invasion. PLoS One 7(3):e33476
Kuczek DE, Larsen AMH, Thorseth ML, Carretta M, Kalvisa A, Siersbæk MS, Simões AMC, Roslind A, Engelholm LH, Noessner E, Donia M, Svane IM, Straten PT, Grøntved L, Madsen DH (2019) Collagen density regulates the activity of tumor-infiltrating T cells. J Immunother Cancer 7(1):68. https://doi.org/10.1186/s40425-019-0556-6
Kular JK, Basu S, Sharma RI (2014) The extracellular matrix: structure, composition, age-related differences, tools for analysis and applications for tissue engineering. J Tissue Eng 5:2041731414557112. https://doi.org/10.1177/2041731414557112
Kurniawan NA, Vos BE, Biebricher A, Wuite GJL, Peterman EJG, Koenderink GH (2016) Fibrin networks support recurring mechanical loads by adapting their structure across multiple scales. Biophys J 111(5):1026–1034. https://doi.org/10.1016/j.bpj.2016.06.034
Larsen M, Artym VV, Green JA et al (2006) The matrix reorganized: extracellular matrix remodeling and integrin signaling. Curr Opin Cell Biol 18:463–471
Leckband DE, de Rooij J (2014) Cadherin adhesion and mechanotransduction. Annu Rev Cell Dev Biol 30:291–315
Lin TC, Yang CH, Cheng LI, Chang WT, Lin YR, Cheng HC (2019) Fibronectin in cancer: friend or foe. Cell 9(1):27. https://doi.org/10.3390/cells9010027
Lu P, Takai K, Weaver VM, Werb Z (2011) Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol 3:a005058
Luhr I, Friedl A, Overath T, Tholey A, Kunze T, Hilpert F, Sebens S, Arnold N, Rosel F, Oberg HH et al (2012) Mammary fibroblasts regulate morphogenesis of normal and tumorigenic breast epithelial cells by mechanical and paracrine signals. Cancer Lett 325:175–188. https://doi.org/10.1016/j.canlet.2012.06.014
Malandrino A, Kamm RD, Moeendarbary E (2018) In vitro modeling of mechanics in cancer metastasis. ACS Biomater Sci Eng 4:294–301. https://doi.org/10.1021/acsbiomaterials.7b00041
Maller O, Hansen KC, Lyons TR, Acerbi I, Weaver VM, Prekeris R, Tan AT, Schedin P (2013) Collagen architecture in pregnancy-induced protection from breast cancer. J Cell Sci 126(Pt 18):4108–4110. https://doi.org/10.1242/jcs.121590. Epub 2013 Jul 10
Menon S, Beningo KA (2011) Cancer cell invasion is enhanced by applied mechanical stimulation. PLoS One 6(2):e17277. https://doi.org/10.1371/journal.pone.0017277
Mierke CT, Rosel D, Fabry B, Brabek J (2008) Contractile forces in tumor cell migration. Eur J Cell Biol 87:669–676
Mierke CT, Frey B, Fellner M, Herrmann M, Fabry B (2011) Integrin α5β1 facilitates cancer cell invasion through enhanced contractile forces. J Cell Sci 124:369–383
Montagner M, Dupont S (2020) Mechanical forces as determinants of disseminated metastatic cell fate. Rev Cells 9(1):250. https://doi.org/10.3390/cells9010250
Mould AP, Humphries MJ (2004) Regulation of integrin function through conformational complexity: not simply a kneejerk reaction? Curr Opin Cell Biol 16:544–551
Ottani V, Franchi M, De Pasquale V, Leonardi L, Morocutti M, Ruggeri A (1998) Collagen fibril arrangement and size distribution in monkey oral mucosa. J Anat 192(3):321–328
Oudin MJ, Jonas O, Kosciuk T, Broye LC, Guido BC, Wyckoff J, Riquelme D, Lamar JM, Asokan SB, Whittaker C, Ma D, Langer R, Cima MJ, Wisinski KB, Hynes RO, Lauffenburger DA, Keely PJ, Bear JE, Gertler FB (2016) Tumor cell-driven extracellular matrix remodeling drives haptotaxis during metastatic progression. Cancer Discov 6(5):516–531. https://doi.org/10.1158/2159-8290.CD-15-1183
Pandya P, Orgaz JL, Sanz-Moreno V (2017) Modes of invasion during tumour dissemination. Mol Oncol 11:5–27. https://doi.org/10.1002/1878-0261.12019
Paolillo M, Schinelli S (2019) Extracellular matrix alterations in metastatic processes. Int J Mol Sci 20:4947
Park HJ, Helfman DM (2019) Up-regulated fibronectin in 3D culture facilitates spreading of triple negative breast cancer cells on 2D through integrin β-5 and Src. Sci Rep 9(1):19950. https://doi.org/10.1038/s41598-019-56,276-3
Paten JA, Martin CA, Wanis JT, Siadat SM, Figueroa-Navedo AM, Ruberti JW, Deravi LF (2019) Molecular interactions between collagen and fibronectin: a reciprocal relationship that regulates de novo fibrillogenesis. Chem. 5(8):2126–2145. https://doi.org/10.1016/j.chempr.2019.05.011
Peyton SR, Kim PD, Ghajar CM, Seliktar D, Putnam AJ (2008) The effects of matrix stiffness and RhoA on the phenotypic plasticity of smooth muscle cells in a 3-D biosynthetic hydrogel system. Biomaterials 29:2597–2607
Pissarenko A, Yang W, Quan H, Brown KA, Williams A, Proud WG, Meyers MA (2019) Tensile behavior and structural characterization of pig dermis. Acta Biomaterialia 86:77–95. https://doi.org/10.1016/j.actbio.2019.01.023
Poincloux R, Collin O, Lizárraga F, Romao M, Debray M, Piel M et al (2011) Contractility of the cell rear drives invasion of breast tumor cells in 3D Matrigel. Proc Natl Acad Sci U S A 108:1943–1948. https://doi.org/10.1073/pnas.1010396108. PMID: 21245302
Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, White JG, Keely PJ (2008) Collagen density promotes mammary tumor initiation and progression. BMC Med 6:11. https://doi.org/10.1186/1741-7015-6-11
Ramaswamy S, Ross KN, Lander ES, Golub TR (2003) A molecular signature of metastasis in primary solid tumors. Nat Genet 33:49–64. https://doi.org/10.1038/ng1060. PMID: 12469122
Ribeiro JF, dos Anjos EHM, Mello MLS, de Campos Vidal B (2013) Skin collagen fiber molecular order: a pattern of distributional fiber orientation as assessed by optical anisotropy and image analysis. PLoS ONE 8:e54724. https://doi.org/10.1371/journal.pone.0054724
Riching KM, Cox BL, Salick MR, Pehlke C, Riching AS, Ponik SM, Bass BR, Crone WC, Jiang Y, Weaver AM et al (2014) 3D collagen alignment limits protrusions to enhance breast cancer cell persistence. Biophys J 107:2546–2558. https://doi.org/10.1016/j.bpj.2014.10.035
Rick JW, Chandra A, Ore CD, Nguyen AT, Yagnik G, Aghi MK (2019) Fibronectin in malignancy: cancer-specific alterations, protumoral effects, and therapeutic implications. Semin Oncol 46(3):284–290. https://doi.org/10.1053/j.seminoncol.2019.08.002
Ridley AJ, Schwartz MA, Burridge K, Firtel RA, Ginsberg MH, Borisy G, Parsons JT, Horwitz AR (2003) Cell migration: integrating signals from front to back. Science 302:1704–1709
Rilla K, Siiskonen H, Tammi M, Tammi R (2014) Hyaluronan-coated extracellular vesicles-a novel link between hyaluronan and cancer. Adv Cancer Res 123:121–148. https://doi.org/10.1016/B978-0-12-800,092-2.00005-8
Ringer P, Colo G, Fässler R, Grashoff C (2017) Sensing the mechano-chemical properties of the extracellular matrix. Matrix Biol 64:6–16. https://doi.org/10.1016/j.matbio.2017.03.004
Ruggeri A, Franchi M, Marini N, Trisi P, Piattelli A (1992) Supracrestal circular collagen fiber network around osseointegrated nonsubmerged titanium implants. Clin Oral Implants Res 3:169–175
Ruggeri A, Franchi M, Trisi P, Piattelli A (1994) Histologic and ultrastructural findings of gingival circular ligament surrounding osseointegrated nonsubmerged loaded titanium implants. Int J Oral Maxillofac Implants 9(6):1–15
Schäfer M, Werner S (2008) Cancer as an overhealing wound: an old hypothesis revisited. Nat Rev Mol Cell Biol 9:628–638
Scott JE (1975) Composition and structure of the pericellular environment. Physiological function and chemical composition of pericellular proteoglycan (an evolutionary view). Philos Trans R Soc Lond B Biol Sci 271(912):135–142. https://doi.org/10.1098/rstb.1975.0047
Scott JE (2002) The first and second ‘laws’ of chemical morphology, exemplified in mammalian extracellular matrices. Eur J Histochem 46(2):111–124. https://doi.org/10.4081/1660
Scott LE (2003) Elasticity in extracellular matrix ‘shape modules’ of tendon, cartilage, etc. A sliding proteoglycan-filament model. J Physiol 553(Pt 2):335–343. https://doi.org/10.1113/jphysiol.2003.050179. Published online 2003 Aug 15
Scott LE, Weinberg SH, Lemmon CA (2019) Mechanochemical signaling of the extracellular matrix in epithelial-mesenchymal transition. Front Cell Dev Biol 7:135. https://doi.org/10.3389/fcell.2019.00135
Stylianou A, Gkretsi V, Louca M, Zacharia LC, Stylianopoulos T (2019) Collagen content and extracellular matrix cause cytoskeletal remodelling in pancreatic fibroblasts. J R Soc Interface 16:20190226. https://doi.org/10.1098/rsif.2019.0226
Tavianatou AG, Piperigkou Z, Barbera C, Beninatto R, Masola V, Caon I, Onisto M, Franchi M, Galesso D, Karamanos NK (2019) Molecular Size-Dependent Specificity of Hyaluronan on Functional Properties, Morphology and Matrix Composition of Mammary Cancer Cells. Matrix Biol Plus 3:100008. https://doi.org/10.1016/j.mbplus.2019.100008
Tavianatou AG, Piperigkou Z, Koutsakis C, Barbera C, Beninatto R, Franchi M, Karamanos NK (2021) The action of hyaluronan in functional properties, morphology and expression of matrix effectors in mammary cancer cells depends on its molecular size. FEBS J 288(14):4291–4310. https://doi.org/10.1111/febs.15734
Tlsty TD, Coussens LM (2006) Tumor stroma and regulation of cancer development. Annu Rev Pathol 1:119–150
Tse JM, Cheng G, Tyrrell JA, Wilcox-Adelman SA, Boucher Y, Jain RK, Munn LL (2012) Mechanical compression drives cancer cells toward invasive phenotype. PNAS 109(3):911–916. https://doi.org/10.1073/pnas.1118910109
Ueda M, Saito S, Murata T, Hirano T, Bise R, Kabashima K, Suzuki S (2019) Combined multiphoton imaging and biaxial tissue extension for quantitative analysis of geometric fiber organization in human reticular dermis. Sci Rep 9:10644. https://doi.org/10.1038/s41598-019-47,213-5
Wang WY, Pearson AT, Kutys ML, Choi CK, Wozniak MA, Baker BM, Chen CS (2018) Extracellular matrix alignment dictates the organization of focal adhesions and directs uniaxial cell migration. APL Bioeng 2:046107
Wolf K, Friedl P (2011) Extracellular matrix determinants of proteolytic and non-proteolytic cell migration. Trends Cell Biol 21(12):736–744. https://doi.org/10.1016/j.tcb.2011.09.006. Epub 2011 Oct 27
Wolf K, Wu YI, Liu Y, Geiger J, Tam E, Overall C, Stack MS, Friedl P (2007) Multistep pericellular proteolysis controls the transition from individual to collective cancer cell invasion. Nat Cell Biol 9:893–904
Wolf K, te Lindert M, Krause M, Alexander S, te Riet J, Willis AL, Hoffman RM, Figdor CG, Weiss SJ, Friedl P (2013) Physical limits of cell migration: control by ECM space and nuclear deformation and tuning by proteolysis and traction force. J Cell Biol 201(7):1069–1084. https://doi.org/10.1083/jcb.201210152
Yue B (2014) Biology of the extracellular matrix: an overview. J Glaucoma 23:S20–S23
Zaman MH, Trapani LM, Sieminski AL, Mackellar D, Gong H, Kamm RD, Wells A, Lauffenburger DA, Matsudaira P (2006) Migration of tumor cells in 3 D matrices is governed by matrix stiffness along with cell-matrix adhesion and proteolysis. Proc Natl Acad Sci USA 103:10889–10894
Zanotelli MR, Zhang J, Reinhart-King CA, Nancy E, Peter C (2021) Mechanoresponsive metabolism in cancer cell migration and metastasis. Cell Metab 33(7):1307–1321. https://doi.org/10.1016/j.cmet.2021.04.002
Zolota V, Tzelepi V, Piperigkou Z, Kourea H, Papakonstantinou E, Argentou MA, Karamanos NK (2021) Epigenetic alterations in triple-negative breast cancer-the critical role of extracellular matrix. Cancers (Basel) 13(4):713. https://doi.org/10.3390/cancers13040713
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Franchi, M. et al. (2022). Basement Membrane, Collagen, and Fibronectin: Physical Interactions with Cancer Cells. In: Kovalszky, I., Franchi, M., Alaniz, L.D. (eds) The Extracellular Matrix and the Tumor Microenvironment. Biology of Extracellular Matrix, vol 11. Springer, Cham. https://doi.org/10.1007/978-3-030-99708-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-99708-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-99707-6
Online ISBN: 978-3-030-99708-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)