Abstract
The biochemical composition of synovial fluid is made up of lubricants, proteins, and small molecules working synergistically to protect the joint from impact, friction, and disease. Breakdown of one or all of these components can lead to degeneration, infection, autoimmunity, and crystalline arthropathies. Competency in synovial fluid analysis is paramount in distinguishing septic from aseptic inflammatory and non-inflammatory arthritis. Changes in color, clarity, viscosity, and shifts in the composition of synovial fluid can provide insight and important clinical information on health and disease of the joint.
Synovial fluid (SF) is normally a clear, straw-colored, viscous liquid, with a volume of approximately 1 ml in the normal human knee joint (Hui, Wiley Interdiscip Rev Syst Biol Med 4:15–37, 2012). A main function of SF is to lubricate cartilage, allowing for low-friction and low-wear movement of the joint. Synovial fluid also provides important metabolic support to the avascular joint cartilage and both permits and modulates synovial inflammation (Hui, Wiley Interdiscip Rev Syst Biol Med 4:15–37, 2012). SF is composed of blood plasma ultrafiltrate including some proteins and additional molecules secreted by synovium cells including the lubricant molecules hyaluronan (HA) and proteoglycan 4 (also known as lubricin), cytokines, and metabolic byproducts.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hyaluronan
- Hyaluronic acid
- Viscosupplementation
- Joint lubrication
- Lubricin
- Synovial lactate
- PRG4 gene
- Cathelicidin LL-37
- α-defensin
- Calprotectin
- Synovial proteins
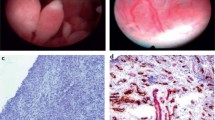
- Synovial inflammation
- Rheumatoid arthritis synovium
- Synovial urate
- Synovial small molecules
Lubricant Molecules
A primary function of SF is to lubricate the joint reducing friction and mechanical stress on the articular cartilage. Large molecules of SF such as hyaluronan (HA), products of the proteoglycan 4 (PRG4) gene including lubricin and superficial zone protein work synergistically to decrease friction and mechanical damage [1]. Hyaluronan is a non-sulfated glycosaminoglycan composed of repeating disaccharide units of D-glucuronic acid and D-N-acetylglucosamine. It was discovered in 1934 by Myer and Palmer, deriving its name from the Greek-derived haylos combined with uronic acid [2]. Produced by fibroblast-derived type B synovial cells, HA has the viscosity of an egg white, and is the most abundant large molecule of SF with concentrations ranging from 1–4 mg/ml [3]. It is a biopolymer molecule several million daltons in size. HA can take the form of hyaluronic acid, or at physiological pH can take the form of a sodium salt [2].
Hyaluronan is a rheological marvel that is extremely lubricious and hydrophilic. In solution, the hyaluronan polymer chain takes on the form of an expanded coil allowing it to hold 1000 times its weight in water [2]. The chains entangle with each other at very low concentrations, and at higher concentrations have an extremely high shear-dependent viscosity separating tissue surfaces that slide along each other. These characteristics give SF the empirical “string sign” that can be demonstrated by letting the thick normal fluid drip out of a syringe one drop at time or by pinching a drop between the thumb and forefinger [4]. A fluid “string sign” of 3 cm or more before breaking is considered normal, while <2.5 cm (more similar to water) is considered abnormal and indicative of inflammatory fluid with degraded HA.
Hyaluronan has other important biological functions. The constant secretion, then degradation has led to the suggestion that it acts as a scavenger for cellular debris [5]. Since the 1940s it has been known that HA is degraded by oxidizing systems via chain cleavage induced by hydroxy radicals, and through this reaction molecular “debris” can be caught in the network of HA and removed at the same rate as the polysaccharide [6, 7]. HA also has a concentration and molecular weight-dependent effect on angiogenesis [2, 8]. High molecular weight and concentrations of HA inhibit capillary formation which may contribute to the avascularity of the joint capsule and cartilage. Interestingly, under certain conditions HA binds to cell surface proteins. Synovial cells can change their expression of HA-binding receptors in disease states, thus HA can influence immunological reactions and inflammatory cell traffic in and out of the synovial fluid [9]. Finally, HA may interact directly or indirectly with pain receptors within the joint, perhaps explaining transient analgesic benefit experienced by some patients following intra-articular HA injections [2, 10].
In states of inflammation and oxidative stress there is accelerated (beyond physiologic) degradation of HA resulting in impairment and loss of viscosity. Degraded HA of low-molecular-weight has different biological activities compared to the high-molecular-weight HA in the healthy joint [2]. Smaller HA chains can serve as endogenous immunostimulating danger signals contributing to inflammation and angiogenesis [2, 11, 12].
There are many commercially available products for HA “viscosupplementation” in OA which may decrease pain and improve function in some patients with mild to moderate disease [13]. An intent with intra-articular injection of exogenous HA is to temporarily improve intra-articular viscosity, stimulate endogenous HA production, stimulate chondrocytes and synthesis of cartilage matrix components, and inhibit enzymatic degradation of chondrocytes and inflammatory processes [14].
Lubricin is a surface-active mucin-like glycoprotein, encoded by the PRG4 gene, which is produced by synovial fibroblasts and chondrocytes along the surface of articular cartilage [15]. The role of lubricin is to retain a protective layer of water molecules, lubricate the joint, and prevent cell and protein adhesion. Along with hyaluronan, it provides protection of the joint by reducing friction. Patients with inflammatory arthritis, joint trauma, or genetic lubricin deficiencies have insufficient amounts to protect the cartilage. There are recombinant forms of lubricin in clinical development for the treatment of OA, autoimmune arthritis, as well as dry eyes and other applications [16].
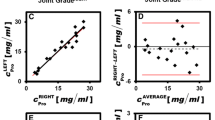
Proteins
There are similarities between blood plasma and SF protein composition, with the synovial membrane selectively blocking very large plasma proteins from entering into the joint space under normal physiological conditions [17]. The average joint SF contains approximately one-third of the protein concentration found in plasma, or 19–28 mg/ml [17, 18]. The major protein found in SF is albumin (approximately 12 mg/ml or 37% of the plasma concentration); transferrin and globulins make up most of the rest. In contrast, large molecular weight plasma proteins such as fibrinogen are at very low concentrations.
In joint inflammation the concentration and quantity of proteins increase. Patients with synovial inflammation including osteoarthritis (OA), rheumatoid arthritis (RA), gout, systemic lupus erythematosus (SLE), and traumatic arthritis have increased protein concentrations [17]. The inflammation of the synovium compromises the ability of the synovium to selectively filter and retain proteins [2, 17]. For example, active RA patients will have high levels of large plasma proteins such as fibrinogen, β2 macroglobulin, β1 lipoprotein, α2 glycoprotein, and α2 macroglobulin [17]. Small proteins such as C-reactive protein, calprotectin, and defensins also more readily influx into SF during joint inflammation, and may have clinical significance and some diagnostic value. But measurement of the SF protein level, unlike the situation with other body fluids, is not diagnostically useful.
Fibrinogen levels are relatively low in the healthy joint SF, but during inflammatory states such as RA and gout, levels can increase 3–5-fold [19]. Studies have shown influx of fibrinogen and other coagulation proteins into synovial fluid that is not paralleled by increased fibrinolytic activity. While normal joint fluid does not clot, the increased fibrinogen in inflamed synovial fluid can cause clotting when transported in a test tube without EDTA or sodium heparin [20, 21]. In the RA patient, forms of citrullinated fibrinogen may bind to anti-citrullinated protein antibodies (anti-CCP ab) within the synovial fluid and joint [22].
Similar to serum CRP, synovial CRP increases in states of inflammation, particularly infection. Serum CRP is commonly used as a screening test for acute infection, but synovial fluid has been found to have a sensitivity and specificity of 92% and 90%, respectively, in periprosthetic joint infection (PJI). High concentrations of CRP are also found in the synovial fluid of inflammatory arthropathies such as RA [23]. Although thought to be exclusively produced in the liver, there is evidence that fibroblast-like synoviocytes may produce CRP, releasing it into the SF [24] and perhaps into the blood.
There are several small proteins and antimicrobial peptides (AMPs) released by neutrophils and macrophages as part of the innate immune response that can be found in SF during states of infection or sterile inflammation. Cathelicidin LL-37, α-defensin, and calprotectin in SF have potential clinical utility when used with other markers such as CRP, white blood count (WBC) with differential and cultures when a septic joint is suspected. Commercial point-of-care testing is available to detect calprotectin and α-defensin in SF [25, 26], but their clinical utility to differentiate between septic and aseptic inflammatory arthropathies is not fully understood.
Cathelicidin LL-37 is a 37 amino acid peptide produced by neutrophils that has been implicated in the pathogenesis of several inflammatory diseases including SLE, RA, psoriasis, and atherosclerosis [27]. It has been found in SF of RA patients and found to associate with inflammation and to increase apoptosis of osteoblasts [27]. Defensins are small (29–35 amino acids) proteins produced by circulating white blood cells and tissue cells [26]. Defensins are classified into alpha and beta families with α-defensin found in and released by neutrophils, macrophages, and Paneth cells of the intestine. In the presence of pathogens in SF, neutrophils release α-defensin inducing the depolarization of the bacterial cell membrane promoting lysis and death [26]. In addition to direct antimicrobial activity, α-defensin also contributes to chemotaxis, cytokine induction, and phagocytosis [28]. Consistently high levels of α-defensin observed in the SF of infected joints have led to it being established as a biomarker and part of the diagnostic criteria for PJI [26, 29]. Interestingly, α-defensin is not influenced by prior antibiotic administration, comorbid conditions of the patient (with the possible exception of an autoimmune disease), or type of infectious organism [30]. Elevated levels can be found in inflammatory arthropathies including crystalline (gout and calcium pyrophosphate deposition disease (CPPD)), psoriatic arthritis, and rheumatoid arthritis [29, 31]. Similar to α-defensin levels, increased numbers of neutrophils within the SF contribute to the levels of lactate dehydrogenase (LD), while the serum LD levels remain normal [4].
Calprotectin is another AMP secreted by neutrophils and monocytes that has chemotactic properties. It has been shown to be more sensitive and specific for the diagnosis of PJI than erythrocyte sedimentation rate, CRP, and SF WBC [32, 33]. Unlike cathelicidin LL-37 and α-defensin, calprotectin has been shown to have potential clinical utility as a biomarker to differentiate septic arthritis from other inflammatory arthropathies including CPPD and RA [34].
Small Molecules
Small molecules in SF include glucose, urate, and lactate. Unlike other body fluids where active transport dictates the movement of many molecules, in SF smaller molecule concentrations typically parallel serum levels under normal conditions. For example, glucose levels in SF are typically ~10 mg/dL less than serum levels. In inflammatory states there are often significantly larger decreases in SF glucose levels in a septic joint compared to serum glucose levels [4], but there is too much overlap with other inflammatory joint conditions for this to be a reliable diagnostic test for infection.
Uric acid in the plasma and SF circulates as urate, the mono-deprotonated ionic form of uric acid under normal physiologic conditions [35]. Elevated serum urate levels will elevate SF levels with subsequent monosodium urate monohydrate (MSU) deposition (MSU being the most common crystallized urate) which may ultimately result in gouty arthritis (see Chap. 10). The various factors that cause crystallization of uric acid have not been fully illuminated, and data on how HA and its degradation products influence urate solubility have been conflicting [35].
Measurement of SF protein, glucose, and even the presence of crystals will not aid in differentiating between septic and aseptic arthritis. While WBC with differential, gram stain and culture remain the most important tests to obtain, lactate may have diagnostic potential to distinguish septic arthritis from other inflammatory states including gout [36,37,38]. SF lactate levels above 10 mmol/L suggest septic arthritis, and levels lower than 4.3 mmol/L are more likely to be aseptic [36]. Another potential biomarker to distinguish septic arthritis from crystalline and aseptic inflammatory arthropathies is the SF lactate/glucose ratio [39]. A large European study evaluating 233 SF specimens found elevated lactate/glucose ratio had a greater area under curve, sensitivity, specificity, and likelihood ratio in septic arthritis, outperforming individual SF lactate and glucose levels.
References
Jahn S, Seror J, Klein J. Lubrication of articular cartilage. Annu Rev Biomed Eng. 2016;18:235–58.
Tamer TM. Hyaluronan and synovial joint: function, distribution and healing. Interdiscip Toxicol. 2013;6(3):111–25.
Mazzucco D, Scott R, Spector M. Composition of joint fluid in patients undergoing total knee replacement and revision arthroplasty: correlation with flow properties. Biomaterials. 2004;25(18):4433–45.
Mundt LA, Shanahan K. Graff's textbook of urinalysis and body fluids. 3rd ed. Burlington: Jones & Bartlett; 2016.
Laurent TC, Laurent UB, Fraser JR. Functions of hyaluronan. Ann Rheum Dis. 1995;54(5):429–32.
Myint P, et al. The reactivity of various free radicals with hyaluronic acid: steady-state and pulse radiolysis studies. Biochim Biophys Acta. 1987;925(2):194–202.
Rapta P, et al. High-molar-mass hyaluronan behavior during testing its radical scavenging capacity in organic and aqueous media: effects of the presence of manganese(II) ions. Chem Biodivers. 2009;6(2):162–9.
Sattar A, Kumar S, West DC. Does hyaluronan have a role in endothelial cell proliferation of the synovium? Semin Arthritis Rheum. 1992;22(1):37–43.
Edwards J. Second international meeting on synovium. Cell biology, physiology and pathology. 21-23 September, Canterbury, United Kingdom. Ann Rheum Dis. 1995;54(5):389–91.
Adams ME. An analysis of clinical studies of the use of crosslinked hyaluronan, hylan, in the treatment of osteoarthritis. J Rheumatol Suppl. 1993;39:16–8.
Kotla NG, et al. Recent advances and prospects of hyaluronan as a multifunctional therapeutic system. J Control Release. 2021;336:598–620.
Tavianatou AG, et al. Molecular size-dependent specificity of hyaluronan on functional properties, morphology and matrix composition of mammary cancer cells. Matrix Biol Plus. 2019;3:100008.
Conrozier T, et al. Viscosupplementation for the treatment of osteoarthritis. The contribution of EUROVISCO group. Ther Adv Musculoskelet Dis. 2021;13:1759720X211018605.
Strand V, et al. Safety and efficacy of US-approved viscosupplements for knee osteoarthritis: a systematic review and meta-analysis of randomized, saline-controlled trials. J Pain Res. 2015;8:217–28.
Szychlinska MA, et al. Altered joint tribology in osteoarthritis: reduced lubricin synthesis due to the inflammatory process. New horizons for therapeutic approaches. Ann Phys Rehabil Med. 2016;59(3):149–56.
Jay GD, Waller KA. The biology of lubricin: near frictionless joint motion. Matrix Biol. 2014;39:17–24.
Hui AY, et al. A systems biology approach to synovial joint lubrication in health, injury, and disease. Wiley Interdiscip Rev Syst Biol Med. 2012;4(1):15–37.
Levick JR. Permeability of rheumatoid and normal human synovium to specific plasma proteins. Arthritis Rheum. 1981;24(12):1550–60.
Barnhart MI, et al. Fibrin promotion and lysis in arthritic joints. Ann Rheum Dis. 1967;26(3):206–18.
Carmassi F, et al. Fibrin degradation in the synovial fluid of rheumatoid arthritis patients: a model for extravascular fibrinolysis. Semin Thromb Hemost. 1996;22(6):489–96.
Faryna A, Goldenberg K. In: Walker HK, Hall WD, editors. Joint fluid, in clinical methods: the history, physical, and laboratory examinations. Boston: Butterworths; 1990.
Raijmakers R, et al. Elevated levels of fibrinogen-derived endogenous citrullinated peptides in synovial fluid of rheumatoid arthritis patients. Arthritis Res Ther. 2012;14(3):R114.
Sukenik S, et al. Serum and synovial fluid levels of serum amyloid A protein and C-reactive protein in inflammatory and noninflammatory arthritis. J Rheumatol. 1988;15(6):942–5.
Fang Z, et al. C-reactive protein promotes the activation of fibroblast-like Synoviocytes from patients with rheumatoid arthritis. Front Immunol. 2020;11:958.
Warren J, et al. Diagnostic utility of a novel point-of-care test of calprotectin for Periprosthetic joint infection after Total knee arthroplasty: a prospective cohort study. J Bone Joint Surg Am. 2021;103(11):1009–15.
Zeng YQ, et al. Diagnostic accuracy of the synovial fluid alpha-Defensin lateral flow test in Periprosthetic joint infection: a meta-analysis. Orthop Surg. 2021;13(3):708–18.
Kahlenberg JM, Kaplan MJ. Little peptide, big effects: the role of LL-37 in inflammation and autoimmune disease. J Immunol. 2013;191(10):4895–901.
Fruitwala S, El-Naccache DW, Chang TL. Multifaceted immune functions of human defensins and underlying mechanisms. Semin Cell Dev Biol. 2019;88:163–72.
Phillips DS, Workman KK, Kelly M. Nonoperative treatment of a Periprosthetic gout flare in the setting of a positive alpha-Defensin result. Arthroplast Today. 2021;9:65–7.
Deirmengian C, et al. Validation of the alpha Defensin lateral flow test for Periprosthetic joint infection. J Bone Joint Surg Am. 2021;103(2):115–22.
Plate A, et al. Inflammatory disorders mimicking periprosthetic joint infections may result in false-positive alpha-defensin. Clin Microbiol Infect. 2018;24(11):1212 e1–6.
Zhang Z, et al. The value of calprotectin in synovial fluid for the diagnosis of chronic prosthetic joint infection. Bone Joint Res. 2020;9(8):450–7.
Salari P, et al. Synovial fluid calprotectin for the preoperative diagnosis of chronic Periprosthetic joint infection. J Arthroplast. 2020;35(2):534–7.
Baillet A, et al. Calprotectin discriminates septic arthritis from pseudogout and rheumatoid arthritis. Rheumatology (Oxford). 2019;58(9):1644–8.
Martillo MA, Nazzal L, Crittenden DB. The crystallization of monosodium urate. Curr Rheumatol Rep. 2014;16(2):400.
Lenski M, Scherer MA. Analysis of synovial inflammatory markers to differ infectious from gouty arthritis. Clin Biochem. 2014;47(1–2):49–55.
Long B, Koyfman A, Gottlieb M. Evaluation and management of septic arthritis and its Mimics in the Emergency Department. West J Emerg Med. 2019;20(2):331–41.
Carpenter CR, et al. Diagnostic accuracy of synovial lactate, polymerase chain reaction, or clinical examination for suspected adult septic arthritis. J Emerg Med. 2020;59(3):339–47.
Berthoud O, et al. Performance of a new rapid diagnostic test the lactate/glucose ratio of synovial fluid for the diagnosis of septic arthritis. Joint Bone Spine. 2020;87(4):343–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Keenan, R.T. (2022). Biochemical Composition of Synovial Fluid in Health and Disease. In: Mandell, B.F. (eds) Synovial Fluid Analysis and The Evaluation of Patients With Arthritis. Springer, Cham. https://doi.org/10.1007/978-3-030-99612-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-99612-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-99611-6
Online ISBN: 978-3-030-99612-3
eBook Packages: MedicineMedicine (R0)