Abstract
Coronary CT angiography (CCTA) is a powerful imaging technique for the noninvasive evaluation of coronary atherosclerosis, which can provide robust risk stratification based on the burden and severity of coronary artery disease (CAD). Patients without any CAD on CCTA have a very low 10-year risk of atherosclerotic cardiovascular events. In contrast, the presence of CAD on CCTA, even when nonobstructive, portends an increased risk of cardiovascular events. As a result, CCTA has a unique advantage over functional tests as it can identify nonobstructive CAD, often in cases where other imaging technique would be unrevealing. In this chapter, we discuss the role of CCTA in risk stratification and in guiding preventive therapy in symptomatic and asymptomatic patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Coronary computed tomography angiography
- Coronary artery calcium
- Prevention
- Cardiovascular disease
- Atherosclerosis
Introduction
Coronary CT angiography (CCTA) is a well-established technique for a noninvasive evaluation of the coronary anatomy in selected patients with stable chest pain syndromes or low to intermediate risk acute chest pain. When compared with functional tests which are designed to detect ischemia CCTA has two major advantages. First, CCTA has a high negative predictive value to exclude the presence of either obstructive or nonobstructive coronary artery disease (CAD). Thus, a normal CCTA (i.e., having no coronary plaque or stenosis) is associated with a very low rate of incident cardiovascular events. Second, CCTA has a unique ability to identify subclinical coronary artery disease, which has immediate implications for the initiation or intensification of preventive therapies, both behavioral and pharmacologic. This capability is particularly relevant given the recent expansion of preventive pharmacotherapy options, which now span antiplatelet agents, statin and nonstatin lipid-lowering therapies, cardiometabolic agents in patients with diabetes, and more. Herein, we highlight the power of CCTA as an adjunct tool for the diagnosis of CAD and its downstream effect in the prevention of atherosclerotic cardiovascular disease (ASCVD) outcomes.
Imaging Technique
Computed tomography (CT) imaging is based on the attenuation of X-rays in tissues. An electrical current in the X-ray tube (source) causes electrons to migrate from a cathode to an anode, generating X-rays, which in turn travel through the patient, where they are attenuated to different extents based on the types of tissue encountered. Residual X-rays that are not attenuated reach the image detector, where they are converted to light and then to an electric signal. Each pixel in the CT image is a representation of X-ray attenuation in that volume of tissue, expressed numerically in Hounsfield Units (HU).
This technology has been used in cardiovascular imaging for nearly 40 years (Lipton et al. 1984). Imaging of the coronary arteries, however, was initially challenging due to the small caliber and highly mobile nature of these vessels. Over the last few decades, technological advances in the field have resulted in sufficient spatial and temporal resolution to enable imaging of the coronary arteries. Specifically, faster gantry rotation and an increasing number of detector rows have been paramount to improve the quality of coronary imaging allowing higher resolution images while “freezing” the motion of the heart.
Modern CT scanners have a rotation time of 240–280 msec. Typically, the temporal resolution of the scanner equals to half the gantry rotation time, because a 180° rotation is sufficient to acquire data on all of the volume of interest. Therefore, the temporal resolution is approximately 120–140 msec on most modern scanners. This can be improved further by dual-source technology, in which two separate X-ray sources and detectors are hosted within the same gantry. Only one-quarter of the full gantry rotation in dual-source scanners is needed for 360° coverage, which can improve the temporal resolution to as low as 66 msec. Another significant improvement with modern cardiac CT scanners is the number of detector rows, which ranges from 64 to 320, allowing for increased patient coverage with a single rotation (up to 16-cm with 320-detector row CT systems). The narrow width of each detector now ranges from 0.5 to 0.625 mm, leading to high spatial-resolution imaging.
Parallel to improvements in temporal and spatial resolution, there has been a substantial reduction in the overall radiation dose with CCTA. The reasons are multifactorial. First, the use of lower tube voltage in appropriate candidates. The tube voltage describes the peak energy of the emitted X-rays. While 120-kVp imaging may be needed for patients who are obese, the use lower of tube voltage, when feasible, lowers the radiation dose significantly as there is an exponential association between kVp and dose. Other techniques for reducing radiation dose include current modulation, axial acquisition using prospective ECG-triggering, iterative reconstruction, and high-pitch helical CT (Hausleiter et al. 2012; Deseive et al. 2015). The randomized PROTECTION III trial found a 69% reduction in radiation exposure with prospective ECG-triggered axial scanning compared with retrospective helical scanning, with similar image quality (Hausleiter et al. 2012). Altogether, these techniques allow for CCTA imaging with very low radiation doses with modern scanners (<2 mSv) (Kosmala et al. 2019).
Despite these major advances, there are still technical challenges in certain patient groups that limit CT imaging of the coronaries with low radiation dose and high temporal and spatial resolution. Notably, patients who are obese still require higher tube voltage, which increases radiation dose. Also, individuals with fast or irregular heart rates may require a helical acquisition using retrospective gating or a wider acquisition window within the RR interval, both techniques which increase radiation exposure. Even with increased radiation exposure, image quality may still be limited in these patients. Patients who are unable to hold their breath are also unsuitable for CCTA imaging. Therefore, many of the attributes of CCTA described in this chapter and elsewhere can only be fully achieved when scanner technology and patient factors allow for good image quality. Furthermore, because the main applications of CCTA in this chapter relate to plaque identification for optimizing preventive therapies, it is noteworthy that in challenging situations (e.g., obesity, irregular heart rate), a coronary artery calcium scan (see Chap. 22) may be technically easier to perform and less susceptible to some of the technical limitations of CCTA.
Safety of Contrast Administration
Unlike CAC scans, CCTA requires the administration of iodine contrast to opacify the coronary arteries. Patients require an intravenous access capable of flows of 5–7 mL/s for a total contrast volume of 50–90 mL. Adverse reactions to contrast media are infrequent. They can be divided into anaphylactoid (or hypersensitivity) and nonanaphylactoid reactions. Serious hypersensitivity reactions are quite rare. In a study with 29,508 patients undergoing contrast-enhanced CT with a low osmolar, nonionic contrast agent, moderate or severe reactions occurred in 23 patients (0.08%) (Mortele et al. 2005). Pretreatment with corticosteroids and antihistamines is routinely administered for patients with a history of mild reactions to iodinated contrast. Those with a history of severe or breakthrough reactions should be considered for alternative imaging or undergo evaluation by an allergist/immunologist.
Whereas anaphylactoid reactions are idiosyncratic and independent of dose, nonanaphylactoid reactions are dependent on dose and concentration of contrast media. These reactions are also infrequent and include gastrointestinal symptoms, pulmonary edema, vasovagal reactions, and contrast-induced nephropathy (CIN). CIN is characterized by an increase in serum creatinine of at least 0.5 mg/dL within 24–72 hours. Recovery of renal function typically occurs in 7–10 days. The major risk factors for CIN include baseline renal dysfunction, diabetes, volume of contrast, and high osmolality agents (Tao et al. 2016). Intravenous administration of iodinated contrast, such as for CCTA, carries a lower risk of CIN than intra-arterial administration of contrast for coronary and other arterial interventions. Indeed, several observational studies have shown that the incidence of acute kidney injury may be no different in those who receive contrast media for CT scans compared with controls who do not (McDonald et al. 2013, 2014; Davenport et al. 2013).
CCTA Use in Symptomatic Patients
The aforementioned advances in CCTA technology, together with a robust evidence base supporting the accuracy and efficacy of CCTA testing, have established CCTA as a first-line noninvasive testing option for patients with acute or stable chest patients who do not have known CAD (Marwick et al. 2015; Knuuti et al. 2020; Moss et al. 2017; Gulati et al. 2021). Accordingly, the most recent guidelines from the United States, United Kingdom, and Europe have assigned a prominent role for CCTA for the evaluation of symptomatic patients (Knuuti et al. 2020; Moss et al. 2017; Gulati et al. 2021). CCTA has an outstanding negative predictive value for obstructive epicardial atherosclerotic plaque, exceeding that of functional studies aimed at detecting ischemia (Stein et al. 2008). In a systematic review, the negative predictive value for excluding significant (≥50%) coronary stenosis with CCTA was approximately 96% compared with invasive angiography in studies with an average CAD prevalence of 61% (Stein et al. 2008). The negative likelihood ratio of CCTA is less than 0.1 (Stein et al. 2008; Budoff et al. 2008).
Absence of Plaque on CCTA
The prognosis of patients without any CAD by CCTA is excellent. In a study with 1304 patients who underwent CCTA for suspected CAD, 46% of whom had moderate or high pretest probability, there were no major cardiovascular events over a mean follow-up of 52 months among the 503 (42%) patients who had no CAD (Andreini et al. 2012). In a meta-analysis including 9592 symptomatic patients with a median follow-up of 20 months, the annualized rate of major adverse cardiovascular events was 0.17% per year in patients without CAD on CCTA, compared with 8.8% per year in those with obstructive epicardial disease (>50% luminal stenosis) (Hulten et al. 2011).
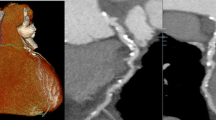
Patients with no CAD (i.e., no plaque or stenosis) on CCTA, as shown in Fig. 23.1, have a very low event rate and benefit from preventive pharmacotherapies may be more limited. Although data on CCTA-guided preventive care for asymptomatic patients are limited, CAC data may be considered in this regard. In a cohort of 13,644 individuals from a military population who underwent CAC testing, statin therapy in patients without plaque (i.e., CAC = 0) was not associated with a significant reduction in adverse cardiovascular events over a median follow-up of 9.4 years (Mitchell Joshua et al. 2018). Although a negative CCTA should be even more reassuring than a CAC of zero (as it denotes the absence of both calcified and noncalcified plaque), this data should be considered with caution due to its observational nature. Moreover, it is conceivable that despite the very low risk of patients who do not have any plaque on CCTA, there could be long-term benefits to some preventive therapies, albeit the magnitude of such a benefit would be expected to be lower in patient who do not have any plaque when compared with individuals who have significant plaque. Another caveat is that outcomes data in asymptomatic individuals may be less applicable to symptomatic populations.
Prognostic Implications of Plaque Burden by CCTA
In addition to its role in ruling out disease and identifying patients without CAD who are at low risk of cardiovascular events, CCTA has a major advantage over ischemic testing with functional imaging: its ability to identify subclinical coronary atherosclerosis. Approximately 1 in 3 patients with suspected CAD who undergo CCTA are found to have nonobstructive CAD (Shaw et al. 2021). Visualization of CAD on anatomical imaging, even if nonobstructive, identifies patients at increased risk for future events despite the absence of obstructive disease, who may benefit from more intense preventive therapy (Bittencourt et al. 2014; Hulten et al. 2014).
A comprehensive meta-analysis of nearly 50,000 patients over a median follow-up of 2.5 years found an 8-fold higher annual event rate in those with nonobstructive CAD (1.6%) compared with those with no CAD (0.2%) (Shaw et al. 2021). Patients with a small burden of atherosclerotic plaque, as shown in Fig. 23.2, may benefit from intensification of medical therapy for prevention of atherosclerotic events, even without obstructive plaque.
The importance of overall plaque burden was demonstrated in the Western Denmark Heart Registry. Among 23,759 symptomatic participants who underwent CCTA and were followed for a median of 4.3 years, the presence of obstructive CAD was not associated with a higher risk than nonobstructive disease when stratified by five groups of CAC score. In other words, patients with a similar plaque burden, as measured by the CAC score, had similar event rates regardless of whether there was obstructive plaque or not (Mortensen et al. 2020).
High-Risk Plaque Features
Certain high-risk plaque features may also add to the risk prediction of CCTA imaging. Specifically, the presence of low-attenuation plaque (typically defined as plaque that has a noncalcified component with <30 HU), positive remodeling, spotty calcifications, and the napkin-ring sign (central area of low-attenuation plaque with a peripheral rim of high attenuation) are all associated with a high risk of downstream events (Shaw et al. 2021; Cury et al. 2016). These plaque attributes can be identified during routine CCTA interpretation and do not require the need of any specific software. However, similar to the identification of high-risk plaque features using invasive techniques, the positive predictive value of CCTA high-risk plaque to identify the site of a future acute coronary syndrome event is low.
In the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) study, 676 (15%) of 4415 patients who underwent CCTA for suspicion of CAD had high-risk plaques, which was associated with a higher risk of major adverse cardiac events even after adjustment for the ASCVD risk score and the presence of significant stenosis (aHR 1.72; 95% CI 1.3–2.62) (Ferencik et al. 2018). Similarly, in the Scottish Computed Tomography of the Heart (SCOT-HEART) trial, the presence of positive remodeling or low attenuation plaque had a threefold higher incidence of coronary heart disease death or nonfatal myocardial infarction relative to those without high-risk plaque features (Williams et al. 2019). However, high-risk plaque was not associated with a higher event rate once adjusted for coronary artery calcium (CAC), which is a surrogate measure of total coronary plaque burden.
Estimating Plaque Burden
Given the increased evidence supporting the prognostic value of plaque burden, a recent Expert Consensus Document on Coronary CT Imaging of Atherosclerotic Plaque from the Society of Cardiovascular Computed Tomography and the North American Society of Cardiovascular Imaging emphasized the importance of adding an assessment of the total burden of atherosclerotic plaque on CCTA reports, as well as whether high-risk plaque features are present (Shaw et al. 2021). Although fully quantitative and automated measurements of plaque burden are not widely available, there are several methods that can be used to estimate overall plaque burden: (a) Quantify CAC score – this requires performing an additional noncontrast CT scan during the CCTA acquisition, which is associated with a small increase in radiation dose; (b) Determine the segment involvement score (SIS) – a semi-quantitative assessment which represents the number of coronary artery segments which have plaque, using a 16-segment model (left main and proximal, mid, and distal segments of left anterior descending artery, diagonal or ramus branch, left circumflex, obtuse marginal, and right coronary artery); (c) Provide a visual estimation of overall plaque burden which incorporate an estimate of the overall amount of calcified and noncalcified plaque.
Supporting the role of measuring the SIS, a study of 3243 patients found that those with nonobstructive, but extensive CAD (defined as a segment involvement score > 4) had a similar risk of cardiovascular death or myocardial infarction over a median follow-up of 3.6 years compared with those with obstructive, but nonextensive CAD (14.5 vs. 13.6/1000 patient-years, respectively) (see Figs. 23.3 and 23.4 for examples of moderate and extensive amount plaque on CCTA) (Bittencourt et al. 2014).
Using the above methods to estimate overall plaque burden on CCTA, extensive plaque is often defined when the CAC score is greater than 300 (if quantified, or visually assessed), or if the segment involvement score is 5 or greater. Individuals with extensive plaque will often have plaque involving all three coronary arteries, with at least one vessel demonstrating plaque which involves most of the vessel. When the CAC score exceeds 1000 (if quantified or visually assessed), the overall amount of plaque can be categorized as very extensive, a finding which corresponds to a very high risk of future cardiovascular events (Peng et al. 2020).
CCTA and Cardiovascular Outcomes
Whether the prognostic implications of CCTA findings can ultimately improve patient outcomes was the subject of two large randomized controlled trials: SCOT-HEART and PROMISE (Newby et al. 2018; Douglas et al. 2015). In the SCOT-HEART trial, 4146 individuals with stable chest pain were randomized to standard care with or without CCTA. Standard care included a stress ECG study in 85% of the patients. Preventive therapies, such as aspirin and statin therapy, were recommended to patients with nonobstructive disease on CCTA or those with a high cardiovascular risk score (Newby et al. 2018). The rate of invasive coronary angiography (24%) or coronary revascularization (13%) was not significantly different between groups (Newby et al. 2018; Investigators S-H 2015). During a median follow-up of 4.8 years, more patients in the CCTA group were started on preventive therapies (19.4%) as compared with patients on standard care alone (14.7%). In addition to a higher rate of initiation of preventive therapies, it is likely that preventive therapies in the CCTA group were allocated to higher-risk patients, more likely to benefit from these therapies, as guided by anatomic evidence of atherosclerosis. Approximately two-thirds of patients in the CCTA group were found to have an abnormal test, either nonobstructive or obstructive CAD, whereas only 15% of patients had an abnormal stress ECG study (Investigators S-H 2015).
The primary endpoint of death from coronary heart disease or nonfatal myocardial infarction was significantly lower among patients who underwent CCTA (2.3%) relative to those who received standard-care alone (3.9%) (HR 0.59; 95% CI 0.41–0.84; p = 0.004), driven primarily by a lower incidence of nonfatal myocardial infarction in the CCTA group (HR 0.60; 95% CI 0.41–0.87) (Newby et al. 2018). Results were consistent among subgroups of age, sex, and baseline cardiovascular risk (Newby et al. 2018).
Important limitations of the SCOT-HEART trial include the nonblinded adjudication of clinical endpoints and the paucity of ischemic imaging in the standard of care group. This was not the case in the PROMISE study, in which 10,003 symptomatic patients were randomized to CCTA or functional testing, with blinded adjudication of outcomes (Douglas et al. 2015). In the functional-testing group, approximately two-thirds of patients underwent nuclear stress imaging, 22% had an exercise echocardiogram, and 10% had an exercise ECG. Over a follow-up of 2 years, the primary composite endpoint of death, myocardial infarction, hospitalizations for unstable angina, or major procedural complications was not significantly different between groups (3.3% CTA vs. 3.0% functional testing; HR 1.04; 95% CI 0.83–1.29) (Douglas et al. 2015).
So how does one reconcile the discrepant results between PROMISE and SCOT-HEART? The answer may lie in the differences in the endpoints used by each trial as well as the differences in study population. In the PROMISE study, there was an excess of hospitalizations for unstable angina – which is a softer endpoint – among patients who were randomized to CCTA, possibly reflecting the consequences of informing patients that they have significant plaque in their coronary arteries. With respect to the different patient populations, the PROMISE study enrolled a lower risk group: only 12% of patients had typical angina and 25% had no chest pain (Douglas et al. 2015). In contrast, all patients in SCOT-HEART had chest pain, including 35% with typical angina, and it is likely that such patients were more likely to benefit from downstream preventive therapies (Newby et al. 2018).
In the PROMISE study, the proportion of patients taking statin therapy at 60 days was higher in the CCTA group for patients with diabetes (71.4% CCTA vs. 64.3% functional testing; OR 1.40; 95% CI 1.14–1.72; p = 0.001) and without diabetes (53% CCTA vs. 46% functional testing; OR 1.36; 95% CI 1.23–1.50; p < 0.001) (Sharma et al. 2019). The same was noted for aspirin in patients with diabetes (62.1% vs. 57.3%; p = 0.04) or without diabetes (52.4% vs. 47.5%; p < 0.001). Overall, results from SCOT-HEART and PROMISE indicate that CCTA-mediated knowledge of the coronary anatomy and global atherosclerotic burden leads to an intensification of preventive therapies. Nevertheless, the intensification of preventive therapies in both the SCOTH-HEART and PROMISE trials were suboptimal, likely reflecting the pragmatic nature of these trials, and the lack of strict guidance to treating physicians on how use CCTA results to optimize preventive therapies.
The impact of atherosclerosis imaging on patient management has also been observed in patients who are found to have a CAC > 0. A systematic review and meta-analysis including more than 11,000 participants who underwent CAC testing showed that identifying coronary atherosclerosis significantly improves the likelihood of initiating or continuing preventive therapies for cardiovascular disease – both pharmacological and lifestyle-related (Gupta et al. 2017).
CCTA Use in Symptomatic Patients with Diabetes
In the subgroup of patients with diabetes, both the SCOT-HEART and PROMISE trials showed favorable outcomes with CCTA relative to standard care or functional imaging. In the SCOT-HEART study, among 444 patients with diabetes, the absolute risk reduction in the composite endpoint of death from coronary heart disease or nonfatal myocardial infarction with CCTA was 4.6% (3.1% CCTA vs. 7.7% in standard care; HR 0.36; 95% CI 0.15–0.87) (Newby et al. 2018).
Similarly, among patients with diabetes in the PROMISE study (n = 1908), the outcome of cardiovascular death or myocardial infarction was significantly lower with CCTA (1.1%) relative to stress testing (2.6%) over a period of 2 years (HR 0.38; 95% CI 0.18–0.79; p = 0.01) (Sharma et al. 2019). Altogether, these data suggest that patients with diabetes and stable chest pain syndromes without known CAD may benefit from a testing strategy of CCTA over functional testing. This anatomical approach with identification of clinical or subclinical atherosclerosis can lead to an intensification of prevention therapies and ultimately to the reduction in atherosclerotic cardiovascular events.
CCTA Use in Asymptomatic Patients
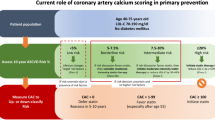
CAC is well established as an imaging technique for advanced risk stratification and guidance of preventive therapies in patients at intermediate-risk for atherosclerotic events who have no symptoms of CAD. A CAC score of zero indicates a low risk of events in the next 10 years, more so than several other “negative” risk markers, such as absence of carotid plaque, low C-reactive protein, absence of family history, and others (Blaha et al. 2016). Even among patients with risk factors or risk-enhancing conditions, such as diabetes, HIV, or a positive family history of premature ASCVD, CAC can provide valuable risk stratification beyond risk factors to guide personalized patient management (Cardoso et al. 2020; Pereira et al. 2020; Patel et al. 2015). Table 23.1 outlines a summary comparison of CAC vs. CCTA.
Whether CCTA has an incremental value over CAC for risk stratification and guidance of preventive therapies, with an impact on hard endpoints, is unclear. In the CONFIRM registry, 7590 participants without chest pain or known CAD from 6 countries underwent CCTA and CAC testing. After a median follow-up of 24 months, both CAC and CCTA improved the performance of risk factor-based prediction models, but the improvement in net risk reclassification from adding CCTA to a model with the CAC score was trivial (Cho et al. 2012). A subanalysis of the CONFIRM registry focused on 400 asymptomatic individuals with diabetes showed an improvement in the C-statistic from 0.64 to 0.77 by adding CCTA to a model of age, gender, and CAC score (Min et al. 2014).
Other single-center studies have shown incremental value of CCTA over CAC score in select populations of asymptomatic patients. Among 591 asymptomatic individuals with type 2 diabetes from South Korea, followed for a median of 5.3 years, CCTA parameters, such as number of obstructive lesions and severity of CAD (obstructive, nonobstructive, or no CAD), had incremental value in risk stratification over a model with traditional risk factors and CAC. The C-index for prediction of cardiac events improved from 0.72 with risk factors and CAC score to 0.82 with risk factors, CAC score, and the number of vessels with obstructive CAD (Kang et al. 2016).
Another study followed 665 patients with mean age 56 years and at least one major risk factor for CAD who underwent CCTA and CAC scoring for a median of 3.0 years. Approximately 81% of patients had CAD on CCTA. The composite endpoint of myocardial infarction, unstable angina, or coronary revascularization occurred in 6.0% of individuals. The addition of CCTA to a model including risk factors and CAC scoring significantly improved prediction and reclassification, particularly among patients with a positive CAC score. The C-statistic increased from 0.81 to 0.84 (Dedic et al. 2016).
The use of CCTA to screen for CAD in asymptomatic patients was evaluated in the FACTOR-64 randomized trial, in which 900 asymptomatic participants with type 1 or type 2 diabetes for at least 3 years were randomized to standard diabetes care with or without CCTA for screening of CAD (Muhlestein et al. 2014). Patients randomized to CCTA were recommended specific interventions for risk factors modification according to the results of CCTA: (1) standard diabetes care if no CAD; (2) patients with CAD were instructed to initiate aggressive risk factor modification, including lower LDL-C (<70 mg/dL), A1C (<6.0%), and systolic blood pressure goals (<120 mmHg). Patients randomized to standard care alone were treated according to guideline recommendations for diabetes care.
The study enrolled 900 patients, with a mean age of 61 years, mean A1C 7.5%, and average diabetes duration of ~13 years. In the CCTA group, 46%, 12%, and 11% had mild, moderate, or severe coronary stenosis, respectively. Additional testing with protocol-driven functional imaging was indicated in 14% of patients in the CCTA group, whereas invasive coronary angiography and revascularization were performed in 8% and 6% of patients, respectively (Muhlestein et al. 2014). In the control group, 5% and 2% underwent invasive angiography and revascularization, respectively.
Over a mean follow-up time of 4 years, the incidence of the primary outcome of all-cause mortality, nonfatal myocardial infarction or unstable angina requiring hospitalization was not significantly different between groups (CCTA 6.2%, control 7.6%; HR 0.80; 95% CI 0.49–1.32; p = 0.38). Although the outcomes of FACTOR-64 dampened enthusiasm for CAD screening with CCTA in asymptomatic patients, the results of the study corroborated the notion that plaque visualization has the potential to improve risk factor management. When compared with subjects in the control group, individuals in the CCTA group had significant improvements in LDL-C, HDL-C, and blood pressure parameters (Muhlestein et al. 2014). Nevertheless, the overall event rates in this well-treated population were low which reduced the ability to identify a difference between the two groups.
The role of CCTA in primary prevention is being explored further in the Computed Tomography Coronary Angiography for the Prevention of Myocardial Infarction (SCOT-HEART 2) Trial (NCT03920176). The study is enrolling 6000 individuals 40–70 years of age, with at least one major risk factor. Patients will be randomized to CCTA or a risk factor-based assessment and followed for the primary outcome of coronary death or nonfatal myocardial infarction.
CCTA vs. CAC Testing in Primary Prevention: Understanding the Trade-Offs
While current guidelines suggest that CCTA should be mostly reserved for symptomatic patients while CAC may be used when there is uncertainty regarding the role of preventive therapies for asymptomatic patients, it is reasonable to question whether CCTA should have a bigger role in assessing risk among selected asymptomatic individuals. Collectively, the studies discussed above suggest that the incremental prognostic value of CCTA beyond CAC is small. However, it is conceivable that the added value of CCTA may be greater in several sub-groups: (1) younger individuals – especially if they have significant risk factors (e.g., heterozygote familial hypercholesterolemia, systemic inflammatory diseases, strong family history of premature MI in several family members). Such individuals are less likely to have calcified plaque and the identification of plaque at an early age may prompt preventive therapies that may lower long-term risk. (2) Patients who have a larger burden of noncalcified plaque or who are more likely to have exclusively noncalcified plaque – this would include patients with systemic inflammatory conditions, HIV, and tobacco use. However, when considering the potential advantages of identifying noncalcified plaque burden via use of CCTA, it is important to recognize several limitations of CCTA, especially when applied to asymptomatic patients. When compared with CAC testing, CCTA is more likely to be associated with higher cost, higher rate of downstream testing, and higher radiation dose. Of particular concern, is the potential for asymptomatic patients to be referred for unnecessary noninvasive or invasive testing following CCTA. Thus, it is imperative that when CCTA is used for the purposes of plaque imaging and prevention among asymptomatic patients that medical therapy remains the focus of subsequent patient management.
There are a few other potential attributes and future developments in CCTA that may further strengthen the role of this test in preventive cardiology. As discussed above, automatic plaque quantification may enable a more reproducible assessment of plaque volume that can be performed on any CCTA, and which integrates information on the location, amount, and type of plaque (Williams et al. 2022). Another technique that may be particularly useful for prevention is the identification of coronary inflammation by analyzing the pericoronary fat attenuation index (FAI), which provided incremental risk assessment beyond CCTA (Fig. 23.5) (Oikonomou et al. 2018). In fact, abnormalities in this signal may precede the development of plaque, and may also signify a specific role for anti-inflammatory therapies (Klüner et al. 2021).
Perivascular Fat Attenuation Index Stratifies the Risk Associated With High Risk Plaque Features. (a) A visual example of pericoronary fat attenuation index (FAI) mapping. (b) Unadjusted Kaplan–Meier curves with adjusted hazard ratios for patients stratified based on FAI around the right coronary artery (cutoff: −70.1 HU) and high-risk plaque (HRP) presence, illustrating how FAI mapping identifies distinct risk groups among HRP(+) and HRP(−) patients. CCTA coronary computed tomography angiography. (Source: Fig. 1 from JACC. 2020;76(6):755–756)
Summary and Recommendations
CCTA is an established noninvasive imaging modality to evaluate for nonobstructive and obstructive CAD in symptomatic patients. When used in this context, one of the greatest advantages of CCTA is the ability to identify the presence, amount, and type of plaque, and thus enhance risk assessment and guide the need for more aggressive preventive therapies (Table 23.2). Several decades of research in atherosclerosis imaging with either CAC (mostly in asymptomatic patients) or CCTA (mostly in symptomatic patients) has reinforced the concept that the total burden of atherosclerosis (or its absence) is strongly associated with future cardiovascular events. Randomized controlled trials have subsequently demonstrated that the use of CCTA among patients who have chest pain results in higher use of preventive therapies and may result in a lower rate of major adverse cardiovascular events. Prior trials have reinforced that in order to derive maximal risk reduction with the use of CCTA it is important that testing is done in patients who have sufficient risk (i.e., lower risk patients are less likely to benefit from such testing). Moreover, it is imperative that CCTA test results are used in defining the need and intensity of future preventive therapies. After all, the CCTA test results do not impact patient outcomes, but how clinicians and patients act on these results is what ultimately matters most. Given the strong association between plaque burden and future cardiovascular risk, it is useful to consider preventive therapies for all patients who are found to have plaque on CCTA. However, patients who have large amount of plaque should be considered for a multipronged intervention incorporating lifestyle changes and aggressive secondary prevention pharmacotherapies (Fig. 23.6).
Aggressive prevention therapies that should be considered for individuals who have extensive amount of plaque on coronary CTA. The presence of a large amount of plaque identifies individual who have a significantly higher risk of future cardiovascular events, often similar to the level of risk observed in secondary prevention trials. Accordingly, it is important to identify all sources of modifiable risk, and to implement both lifestyle and pharmacologic therapies. While not all therapies on this figure will be appropriate for all patients, all are reasonable to consider for lowering the risk of cardiovascular events. Illustration courtesy of Ana Vitória Cordeiro Rocha, Federal University of Goias, Brazil
In asymptomatic patients, the wider availability and lower cost of CAC testing make it the preferred imaging test for risk stratification and guidance of primary prevention therapies (Cardoso et al. 2020). Although some studies have shown that CCTA in asymptomatic patients can improve risk prediction beyond CAC testing, its current role remains limited, but may evolve over time. A wider adoption of CCTA in this context will require more data on subgroups that are more likely to benefit from CCTA (vs. CAC testing), as well as future clinical trials demonstrating improved cardiovascular outcomes among individuals who are selected based on CCTA findings. Current studies are ongoing to define the role of CCTA among asymptomatic patients, as well as its impact on downstream patient management and outcomes.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CAC:
-
Coronary artery calcium
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- CIN:
-
Contrast-induced nephropathy
- CT:
-
Computed tomography
- FAI:
-
Fat attenuation index
- HU:
-
Hounsfield Units
References
Andreini D, Pontone G, Mushtaq S, Bartorelli AL, Bertella E, Antonioli L, et al. A long-term prognostic value of coronary CT angiography in suspected coronary artery disease. JACC Cardiovasc Imaging. 2012;5(7):690–701.
Bittencourt MS, Hulten E, Ghoshhajra B, O’Leary D, Christman MP, Montana P, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging. 2014;7(2):282–91.
Blaha MJ, Cainzos-Achirica M, Greenland P, McEvoy JW, Blankstein R, Budoff MJ, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the multi-ethnic study of atherosclerosis (MESA). Circulation. 2016;133(9):849–58.
Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52(21):1724–32.
Cardoso R, Dudum R, Ferraro RA, Bittencourt M, Blankstein R, Blaha MJ, et al. Cardiac computed tomography for personalized management of patients with type 2 diabetes mellitus. Circ Cardiovasc Imaging. 2020;13(9):e011365.
Cho I, Chang HJ, Sung JM, Pencina MJ, Lin FY, Dunning AM, et al. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry). Circulation. 2012;126(3):304–13.
Cury RC, Abbara S, Achenbach S, Agatston A, Berman DS, Budoff MJ, et al. CAD-RADS(TM) Coronary Artery Disease - Reporting and Data System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr. 2016;10(4):269–81.
Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH. Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology. 2013;268(3):719–28.
Dedic A, Ten Kate GJ, Roos CJ, Neefjes LA, de Graaf MA, Spronk A, et al. Prognostic value of coronary computed tomography imaging in patients at high risk without symptoms of coronary artery disease. Am J Cardiol. 2016;117(5):768–74.
Deseive S, Chen MY, Korosoglou G, Leipsic J, Martuscelli E, Carrascosa P, et al. Prospective randomized trial on radiation dose estimates of CT angiography applying iterative image reconstruction: the PROTECTION V study. JACC Cardiovasc Imaging. 2015;8(8):888–96.
Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291–300.
Ferencik M, Mayrhofer T, Bittner DO, Emami H, Puchner SB, Lu MT, et al. Use of high-risk coronary atherosclerotic plaque detection for risk stratification of patients with stable chest pain: a secondary analysis of the PROMISE randomized clinical trial. JAMA Cardiol. 2018;3(2):144–52.
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain. J Am Coll Cardiol. 2021;78(22):e187–285.
Gupta A, Lau E, Varshney R, Hulten EA, Cheezum M, Bittencourt MS, et al. The identification of calcified coronary plaque is associated with initiation and continuation of pharmacological and lifestyle preventive therapies: a systematic review and meta-analysis. JACC Cardiovasc Imaging. 2017;10(8):833–42.
Hausleiter J, Meyer TS, Martuscelli E, Spagnolo P, Yamamoto H, Carrascosa P, et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging. 2012;5(5):484–93.
Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;57(10):1237–47.
Hulten E, Bittencourt MS, Singh A, O’Leary D, Christman MP, Osmani W, et al. Coronary artery disease detected by coronary computed tomographic angiography is associated with intensification of preventive medical therapy and lower low-density lipoprotein cholesterol. Circ Cardiovasc Imaging. 2014;7(4):629–38.
Investigators S-H. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet. 2015;385(9985):2383–91.
Investigators S-H, Newby DE, Adamson PD, Berry C, Boon NA, Dweck MR, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med. 2018;379(10):924–33.
Kang SH, Park GM, Lee SW, Yun SC, Kim YH, Cho YR, et al. Long-term prognostic value of coronary CT angiography in asymptomatic type 2 diabetes mellitus. JACC Cardiovasc Imaging. 2016;9(11):1292–300.
Klüner LV, Oikonomou EK, Antoniades C. Assessing cardiovascular risk by using the fat attenuation index in coronary CT angiography. Radiol Cardiothorac Imaging. 2021;3(1):e200563.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77.
Kosmala A, Petritsch B, Weng AM, Bley TA, Gassenmaier T. Radiation dose of coronary CT angiography with a third-generation dual-source CT in a “real-world” patient population. Eur Radiol. 2019;29(8):4341–8.
Lipton MJ, Higgins CB, Farmer D, Boyd DP. Cardiac imaging with a high-speed Cine-CT Scanner: preliminary results. Radiology. 1984;152(3):579–82.
Marwick TH, Cho I, Hartaigh BÓ, Min JK. Finding the gatekeeper to the cardiac catheterization laboratory: coronary CT angiography or stress testing? J Am Coll Cardiol. 2015;65(25):2747–56.
McDonald JS, McDonald RJ, Comin J, Williamson EE, Katzberg RW, Murad MH, et al. Frequency of acute kidney injury following intravenous contrast medium administration: a systematic review and meta-analysis. Radiology. 2013;267(1):119–28.
McDonald RJ, McDonald JS, Carter RE, Hartman RP, Katzberg RW, Kallmes DF, et al. Intravenous contrast material exposure is not an independent risk factor for dialysis or mortality. Radiology. 2014;273(3):714–25.
Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ, et al. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis. 2014;232(2):298–304.
Mitchell Joshua D, Fergestrom N, Gage Brian F, Paisley R, Moon P, Novak E, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol. 2018;72(25):3233–42.
Mortele KJ, Oliva MR, Ondategui S, Ros PR, Silverman SG. Universal use of nonionic iodinated contrast medium for CT: evaluation of safety in a large urban teaching hospital. AJR Am J Roentgenol. 2005;184(1):31–4.
Mortensen MB, Dzaye O, Steffensen FH, Botker HE, Jensen JM, Ronnow Sand NP, et al. Impact of plaque burden versus stenosis on ischemic events in patients with coronary atherosclerosis. J Am Coll Cardiol. 2020;76(24):2803–13.
Moss AJ, Williams MC, Newby DE, Nicol ED. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep. 2017;10(5):15.
Muhlestein JB, Lappe DL, Lima JA, Rosen BD, May HT, Knight S, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA. 2014;312(21):2234–43.
Oikonomou EK, Marwan M, Desai MY, Mancio J, Alashi A, Hutt Centeno E, et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet. 2018;392(10151):929–39.
Patel J, Al Rifai M, Blaha MJ, Budoff MJ, Post WS, Polak JF, et al. Coronary artery calcium improves risk assessment in adults with a family history of premature coronary heart disease: results from multiethnic study of atherosclerosis. Circ Cardiovasc Imaging. 2015;8(6):e003186.
Peng AW, Mirbolouk M, Orimoloye OA, Osei AD, Dardari Z, Dzaye O, et al. Long-term all-cause and cause-specific mortality in asymptomatic patients with CAC >/=1,000: results from the CAC consortium. JACC Cardiovasc Imaging. 2020;13(1 Pt 1):83–93.
Pereira B, Mazzitelli M, Milinkovic A, Moyle G, Ranasinghe S, Mandalia S, et al. Use of coronary artery calcium scoring to improve cardiovascular risk stratification and guide decisions to start statin therapy in people living with HIV. J Acquir Immune Defic Syndr. 2020;85(1):98–105.
Sharma A, Coles A, Sekaran NK, Pagidipati NJ, Lu MT, Mark DB, et al. Stress testing versus CT angiography in patients with diabetes and suspected coronary artery disease. J Am Coll Cardiol. 2019;73(8):893–902.
Shaw LJ, Blankstein R, Bax JJ, Ferencik M, Bittencourt MS, Min JK, et al. Society of Cardiovascular Computed Tomography/North American Society of Cardiovascular Imaging - expert consensus document on coronary CT imaging of atherosclerotic plaque. J Cardiovasc Comput Tomogr. 2021;15(2):93–109.
Stein PD, Yaekoub AY, Matta F, Sostman HD. 64-slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med. 2008;121(8):715–25.
Tao SM, Wichmann JL, Schoepf UJ, Fuller SR, Lu GM, Zhang LJ. Contrast-induced nephropathy in CT: incidence, risk factors and strategies for prevention. Eur Radiol. 2016;26(9):3310–8.
Williams MC, Moss AJ, Dweck M, Adamson PD, Alam S, Hunter A, et al. Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol. 2019;73(3):291–301.
Williams MC, Earls JP, Hecht H. Quantitative assessment of atherosclerotic plaque, recent progress and current limitations. J Cardiovasc Comput Tomogr. 2022;16(2):124–37.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cardoso, R., Blankstein, R. (2022). Cardiac Computed Tomography Angiography for Prevention of Cardiovascular Events. In: Shapiro, M.D. (eds) Cardiovascular Risk Assessment in Primary Prevention. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-030-98824-1_23
Download citation
DOI: https://doi.org/10.1007/978-3-030-98824-1_23
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-98823-4
Online ISBN: 978-3-030-98824-1
eBook Packages: MedicineMedicine (R0)