Abstract
Surgical management of the frontal sinus (FS) is considered one of the most difficult and challenging procedures of endoscopic sinus surgery. Surgery in the FS and frontal recess (FR) remains a challenge because of the complex and variable anatomy, important structures surrounding the drainage pathway, and the anatomical disposition that demands the surgeon to perform the surgery in an oblique direction in a narrow space with a hard visualization and instrumentation. Imaging techniques, especially computed tomography images, provide the surgeon with information about anatomical structures and variants for planning the surgery to avoid complications or failure. Similarly, as with any surgery, thorough anatomical knowledge is part of a successful surgical procedure. In this chapter we will discuss the frontal sinus and frontal recess classical anatomy and we will correlate it to the endoscopic and radiological anatomy. A clear 3D configuration of the frontal area before surgery is necessary to perform a safe and confident procedure. Otherwise, insecurity in the FR will often either result in inadequate surgery with functional failure or increase the risk of orbit, brain, or vascular injury.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Surgical management of the FS is considered one of the most difficult and challenging procedures of endoscopic sinus surgery. Operating endoscopically in the FS is challenging not only because of the complex anatomy and its anatomical relationships (anterior skull base, anterior ethmoidal artery, orbit) but also because of ergonomic factors that lead the surgeon to perform the surgery in an oblique plane in a narrow space with a hard visualization and instrumentation. Finally, due to the great individual variability in this region, anatomy may vary among individuals. Thus, specific radiologic studies are mandatory for surgical planning.
Imaging techniques, especially computed tomography (CT) images, provide the surgeon with information about anatomical structures and variants for planning the surgery to avoid complications or failure. Similarly, as with any surgery, thorough anatomical knowledge is part of a successful surgical procedure. In this chapter, we will go through the main anatomical references to perform a safe endoscopic approach to the FS. We will review the FR anatomical limits and we will discuss how to manage the different anatomical variants in this region. We will correlate the FS and FR classical anatomy to the endoscopic and radiological anatomy. The key point to perform a safe and successful frontal surgery is to unify the three concepts and to be able to create and reconstruct mentally a 3D configuration with the important landmarks and risky regions before coming to the operating room.
2 Frontal Bone
The frontal bone is located at the most anterior part of the cranium. It is made up of two main parts: a horizontal and a vertical portion (Fig. 3.1). The horizontal or orbital portion forms part of the roof of the orbital and nasal cavities and acts to floor the frontal lobes of the brain. The vertical or squamous portion is flat and marks the main region of the forehead (Fig. 3.2.). It contains the FS which is surrounded by two walls of cortical bone. The posterior wall of the FS, which separates the sinus from the anterior cranial fossa, is much thinner (less than a millimeter in some areas) than its anterior wall [1] (Fig. 3.3).
Frontal bone I. (a) The frontal bone is located at the most anterior part of the cranium. The external portion consists of two parts. (b) Vertical or squamous portion. It builds up the main region of the forehead. (c) Horizontal or orbital portion. It projects posteriorly at almost a 90° angle from the vertical portion. (d) Horizontal portion. Laterally it makes up a great part of the roof of the orbits. Medially, it contributes to the roof of the nasal cavity. (e) Both portions are divided by the nasorbital crest (dotted line). At around 3 cm from the midline, the supraorbital foramen (right) and notch (left) can be identified (blue circle)
The FS is not present in the newborn but makes its appearance in the orbital plate between the end of the first year and the beginning of the third year. They are generally well developed and functional between the sixth and the eighth years, although they continue to grow slowly until reaching their maximum size after puberty [2]. Frontal sinuses are rarely symmetrical as they develop independently. They assume the shape of a pyramid and their average measurements are as follows: height 28 mm, breadth 24 mm, depth 20 mm, creating a space of 6–7 ml [3].
A triangular-shaped intersinus septum separates the frontal sinuses into separately draining sinus cavities. It is the continuation, anteriorly, of the ossified embryologic sagittal suture line. Although the intersinus septum may vary in direction and thickness as it proceeds superiorly, the base of the intersinus septum will almost always be close to the midline at the level of the infundibulum. At this level, the intersinus septum is continuous with the crista galli posteriorly, the perpendicular plate of the ethmoid inferiorly, and the nasal spine of the frontal bone anteriorly. The falx cerebri inserts into the posterior table of the frontal sinus, at a point corresponding to the posterior edge of the intersinus septum [1].
There are wide variations in the pneumatization of the FS: the frequency of bilateral absence of the FS has been reported in 3–4% to 10% of several populations [4]. Superior pneumatization can extent variably, and it reaches the nasal bones inferiorly. The main issue for endoscopic approaches is to check out the lateral pneumatization: when extending far lateral in the coronal plane, the endoscopic approach can be limited or even discarded.
3 Frontal Recess
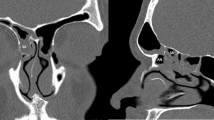
The frontal sinus drainage pathway is highly variable and it has been classically compared to an hourglass shape. The FS narrows down inferiorly and medially into a funnel shape point, which is the frontal infundibulum. It ends in almost a circular area: the FS ostium which lies in an oblique plane between the skull base and the frontal beak. The ostium is the area of transition from the FS to the FR (Figs. 3.4 and 3.5). The inferior portion of the drainage corresponds to the FR. This morphology is more evident on the sagittal plane in CT images.
Frontal recess I. (a) The superior compartment corresponds to the frontal sinus, the inferior portion corresponds to the frontal recess, and the narrowest part is the frontal ostium. (b) The superior boundary of the FR slopes down posteriorly at a 15° angle and becomes more horizontal at the junction with the fovea ethmoidalis. Frontal Sinus: FS; Dotted yellow Line: frontal sinus drainage pathway. Red asterisk: frontal ostium
The FR is a three-dimensional space occupied by several anterior ethmoidal cells that surround and address the direction of the drainage [5]. Its configuration has a great variability among individuals and depends mostly on the degree of pneumatization of the different ethmoidal cells.
Its posterior wall consists of the anterior wall of the bulla ethmoidalis. If this lamella does not reach the skull base, the frontal recess may open into the suprabullar recess. Anteriorly, the recess is limited by the superior part of the agger nasi cell (ANC) (Fig. 3.6.). Its medial limit is represented by the vertical lamella of the middle turbinate and the lateral lamella of the cribriform plate [6]. The FS drainage is located in the center of the recess in 53% of cases, lateral in 29%, and anterior in 11%. Asymmetry between both sides is present in 46% of cases [7] (Fig. 3.7).
Frontal recess limits. Complex and varied anatomy, whose direction, size, bending, and relationship with the ethmoid infundibulum are altered by the configuration of air cells within it and the different attachments of the UP (u). Located posterior to the frontal beak (red asterisk) and agger nasi cell (ANC), anterior to the bulla ethmoidalis (BE), and the anterior ethmoidal artery (AEA) in between the lamina papyracea (dotted red line) and the vertical lamella of the middle turbinate and the vertical lamella of the cribriform plate (green line). Yellow dotted line: frontal sinus drainage pathway. (a) Schematic sagittal drawing of the frontal recess. (b) Sagittal CT view of the frontal recess. Note the structures that build up the anterior and posterior limits of the frontal sinus drainage pathway. (c) Coronal CT view. Note the lateral and medial limits of the frontal recess. (d–f) Sagittal CT view of the frontal recess
Endoscopic limits of frontal bone. (a) Endoscopic view after Draf III procedure. (b) Inferior view of frontal bone. (c) Inferior view of the frontal bone showing the roof of the orbits laterally and the fovea ethmoidalis (blue area or FE). (d) Inferior view of frontal bone showing the roof of the orbits laterally and the ethmoidal notch medially filled up by the cribriform plate (yellow area or CP). AEA: Anterior ethmoidal artery; AEP: Posterior ethmoidal artery; LP: Lamina papyracea; FS: Frontal sinus; Red asterisk: Vertical lamella, cribriform plate; EN: Ethmoidal notch; FE: Fovea ethmoidalis
4 Anatomical Structures
Despite all the “fixed” limits, the anatomy of the FR is highly variable and the FS outflow tract is determined in general terms by the pneumatization pattern of the FR cells, the attachment of the uncinate process (UP), the size of the frontal beak, and shape of the skull base. These anatomical factors vary among individuals and races [8, 9].
4.1 Agger Nasi Cell
The ANC is currently considered the key to accessing the frontal pathway drainage. It is the most anteriorly placed frontoethmoid cell and it is present in 98.5% of patients [10]. On endoscopic examination, this cell appears as a prominence on the lateral nasal wall just anterior to the attachment of the middle turbinate (Fig. 3.8). It is thought to be the most superior remnant of the first ethmoturbinal (nasoturbinal) [11].
The ANC pneumatizes into the frontal process of the maxilla and lacrimal bone area and it can be easily identified on the coronal CT scan as the first ethmoidal cell after the lacrimal duct and anterior to the middle turbinate. However, sagittal reconstructions allow for a better analysis, visualization, and understanding of its variants. When present, it appears as part of the anterior ethmoidal cells building up the anterior and inferior limit of the frontal recess. Due to its localization, a large ANC may push the frontal recess posteriorly and/or medially but it is also often associated with a larger anteroposterior surgical frontal opening [12, 13].
The posterior and superior portion of the UP together with the medial wall of the ANC is the key that unlocks the frontal recess. Most of the ANC is anterior to the uncinate, but the posterior half of the ANC has an intimate relationship with the upward extension of the UP [14]. Stamm [15] calls this relationship “vertical bar” and supports that usually the frontal recess drains medial or posterior to this structure.
In fact, to perform a type I Draf frontal sinusotomy, which is really part of the anterior ethmoidectomy [16], the ANC has to be removed. For that purpose, a Kerrison forceps can be used to eliminate its anterior wall. Once it is open, the posterior wall can be assessed and removed, entering directly into the frontal recess that can be permeable or occupied by other FR cells. This has to be established as a key landmark for the FR dissection in basic and advanced surgery [17].
Because surgeons lack confidence when exploring this area, inadequate removal of cells and eventually disease often occurs. The strong correlation of ANC disease with FS disease assessed by sinus CT scans in patients undergoing revision surgery has been described in the literature [18,19,20].
4.2 Uncinate Process
The UP is the most anterior bony lamella, of the four lamellae that traverse the entire ethmoid (UP, bulla lamella, basal lamella of the middle turbinate, and basal lamella of the superior turbinate). There is a fifth lamella that corresponds to the supreme turbinate. It has a prevalence of 60% and may present unilaterally or bilaterally [21].
It is a thin sickle-shaped bony structure with an almost sagittal orientation, running from anterosuperior to posteroinferior. Its free posterior margin runs parallel to the anterior surface of the ethmoid bulla. The course of the free inferior edge of the UP usually attaches to the perpendicular process of the palatine bone and the ethmoid process of the inferior turbinate (Fig. 3.9). For frontal endoscopic surgery, understanding the superior attachment is more useful.
Traditionally, the superior attachment of the UP has been considered as the key to treating the FR with its three types of insertion: lamina papyracea, skull base, and middle turbinate [22].
When the UP attaches to the lamina papyracea, which is the most common situation as it is seen in 60–88% of cases, the ethmoid infundibulum ends up in a blind recess known as the recessus terminalis and the superior portion of the UP makes up the posterior wall of the ANC. In such cases, the frontal drainage runs directly into the middle meatus medial to the UP (Fig. 3.10).
Superior attachment of the uncinate process. Schematic coronal drawing and CT views of the most frequent variations of the attachments of the vertical portion of the UP (red) and its relationship with the frontal recess and frontal outflow tract (yellow) as proposed by Stammberger. (a) Attachment to the lamina papyracea (60–88%). Frontal recess drains medial to the UP, separated from the ethmoidal infundibulum. It forms a blind end to the ethmoidal infundibulum superiorly called the terminal recess (recessus terminalis: rt). (b) Attachment to the skull base. Frontal recess drains lateral to the UP and joins to the ethmoidal infundibulum. (c) Attachment to the middle turbinate. Frontal recess drains lateral to the UP and joins to the ethmoidal infundibulum
In cases where the UP attaches to the skull base or the middle turbinate, the frontal drainage is directed into the ethmoidal infundibulum, lateral to the UP which can be seen in around 12–40% of cases [23].
However, Wormald showed that the location of the superior insertion of the UP is often a secondary effect of the degree of pneumatization and morphology of the ANC [24].
In addition, the UP, similar to other structures of the ethmoid, can present a great variability with multiple superior attachments [25].
For all these reasons the upper classification has to be taken into account but it should be completed with a proper interpretation of the CT scan. DICOM readers like Horos or Osirix can be a useful tool before surgery to draw a 3D configuration of the frontal drainage and to be able to establish if the FS is draining in a medial or a lateral disposition.
4.3 Frontal Cells
The FR is the most inferior portion along the frontal drainage pathway and corresponds to the anterior ethmoid. It can be very variable in shape and dimensions among individuals depending on the different ethmoidal cells that may narrow the airspace: in the sagittal plane they can be identified in an anterior or posterior disposition in relation to the pathway.
These cells and the different anatomical variants have been well described by Bent and Kuhn [26, 27] and their identification requires careful analysis of CT images in the 3 planes of space.
They describe the frontal cells at the anterior portion of the FR and propose four main cell types: type 1 is defined when there is only one cell above the ANC; type 2 occurs when two or more cells pneumatize above the ANC; type 3 occurs when a large single cell pneumatizes above the ANC into the FS; and type 4 when there is an isolated cell within the FS.
Recently, Wormald described an anatomical classification based on three cell types: the anterior cells (ANC, supra-agger cell, supra-agger frontal cell) that push the FS drainage pathway medial, posterior, or posteromedially; the posterior cells (suprabulla cell, suprabulla frontal cell, supraorbital ethmoid cell) that push the drainage pathway anteriorly; and medial cells (frontal septal cell) that push the drainage pathway laterally [12].
4.4 Frontobullar, Suprabullar and Supraorbital Cells
The Draf I procedure consists of removing the ethmoidal cells that surround the FR. Thus, computed tomography is mandatory for the understanding of the anatomy of the patient and individualized surgical planning.
While the frontal cells are anatomic variants of anterior ethmoid pneumatization located on the anterior margin of the FR that potentially extend within the airspace of the frontal ostium above the ANC, at the posterior margin of the FR, the bulla ethmoidalis forms the posterior boundary. In some cases, the anterior bulla wall does not reach the skull base, creating a suprabullar recess. This space can be filled up by one or more suprabullar cells. In addition, there are other ethmoidal cells that may narrow the drainage of the frontal sinus posteriorly: frontobullar or supraorbital cells (Fig. 3.11).
Suprabullar recess and supraorbital cells. Blue asterisk *: Suprabullar recess: air containing space bordered inferiorly by the roof of the ethmoidal bulla (b), medially by the middle turbinate, laterally by the lamina papyracea, and superiorly by the roof of the ethmoid. Green asterisk *: Supraorbital recess or cell: lateral extension of suprabullar recess or another aerated part of the ethmoidal roof extending over the orbit. B: bulla ethmoidalis
The frontobullar cells extend through the posterior aspect of the frontal ostium within the sinus. Supraorbital cells are cells originating from the anterior ethmoid extending posteriorly and superiorly over the orbit from the FR. They may mimic septated frontal sinuses as their posterior wall is the skull base. These cells are present in 28–54% of subjects and express the pneumatization of the orbital plate of the frontal bone posterior to the FR and the FS, as it can be seen in axial cuts. They appear in the sagittal reconstruction of the CT scan as triangular air cells with posterior vertex [28, 29].
When a supraorbital cell is present, the anterior ethmoidal artery is usually seen freely running within the ethmoid air cells and this increases the risk of intraoperative vascular injury (Fig. 3.12). The cell usually opens to the ethmoid anterior to the AEA [30]. They have also been significantly associated with the presence of FS septations [31]. Finally, their presence has been associated with orbital proptosis in patients with chronic rhinosinusitis [32].
Supraorbital cells. (a–c) CT reconstruction in the sagittal, axial, and coronal planes showing a supraorbital cell. These cells appear in the sagittal reconstruction as triangular air cells with posterior vertex [28, 29]. (c, d) In these variants, the anterior ethmoidal artery (AEA) runs far from the ethmoid roof surrounded by a mesentery, increasing the risk during surgery. (e) Endoscopic view after Draf III procedure and complete ethmoidectomy. Note the pneumatization over the orbit. Red asterisk: AEA; Blue asterisk: supraorbital cell
5 Anatomical Landmarks
5.1 Lateral Lamella of the Cribriform Plate
The ethmoid labyrinth is covered by the fovea ethmoidalis of the frontal bone. In the midline it attaches the lateral lamella of the cribriform plate, a very thin, sagittally oriented bone that defines the lateral wall of the olfactory fossa and entails the posteromedial limit of the FR.
The height of the lateral lamella defines the depth of the olfactory fossa into the nasal cavity. Three classic heights have been described by Keros [33]: type 1: has a depth of 1–3 mm (26.3% of the population), type 2: has a depth of 4–7 mm (73.3% of the population), and type 3: has a depth of 8–16 mm (0.5% of the population) (Fig. 3.13). Depending on the Keros type, the amount of lateral lamella exposed is different. This means that Keros type 1 is the most favorable situation as the lateral lamella exposure is just 1-3 mm, whereas Keros type 3 is the most challenging scenario as more cribriform plate is exposed and can be potentially damaged during manipulation, creating a cerebrospinal fluid (CSF) leak.
Keros classification: 3 types of the lateral lamella [33]. (a) Type I. The lateral lamella is very short, rendering the olfactory fossa almost flat (1–3 mm) (26.3%). (b) Type II. The lateral lamella is longer, creating a moderately deep fossa (4-7 mm) (73.3%). (c) Type III. The lateral lamella is very long (8-16 mm) producing a very deep olfactory fossa (0.5%). (d, e) Coronal view of the perfunded specimen. Dotted blue line: fovea ethmoidalis of the frontal bone; yellow dotted line vertical and horizontal lamella of the cribriform plate
5.2 Anterior Ethmoidal Artery (AEA)
The AEA is a key landmark for the fovea ethmoidalis, the anterior cranial base, and the FR. The FR lies just anterior to its course along the ethmoidal labyrinth. The superior boundary of the FR slopes down posteriorly at a 15° angle and becomes more horizontal at the junction with the fovea ethmoidalis. Just behind the junction, the AEA crosses the medial orbital wall to the lateral lamella of the cribriform plate [34].
The AEA usually runs along the skull base inside the anterior ethmoidal canal between the second and the third lamella in around 100% of cases, in between the anterior and the posterior walls of the bulla. With an angle of about 35°, it runs along the skull base in a very constant oblique direction from posterolateral to anteromedial from the orbit to the olfactory groove. Finally, it reaches the olfactory groove in the vertical lamella of the cribriform plate, which is the weakest point in the anterior cranial base [30] (Fig. 3.14).
Anterior ethmoidal artery (AEA). (a–d) CT From the orbit, the AEA crosses the ethmoid labyrinth until it reaches the olfactory fossa through the lateral lamella of the cribriform plate, forming the anterior ethmoid sulcus. It runs along the anterior skull base between the second and the third lamellas in 90% of cases. In the presence of some variants (supraorbital and suprabullar cells (a)), it runs far from the ethmoid roof surrounded by a mesentery with bone dehiscence in 40% of cases. (e) Endoscopic view: Right AEA after removing the anterior wall of the bulla ethmoidalis. The posterior wall of the bulla is not opened. (f) Endoscopic view. Right AEA crossing from the orbit to the vertical lamella of the cribriform plate. Note the typical posteroanterior and lateromedial direction. (g) Endoscopic view: Left AEA. There is an average distance of 8.58 ± 5.56 mm between the posterior border of the frontal sinus and the AEA
The AEA is a good endoscopic reference as it shows the posterior endoscopic limit of the frontal recess at the fovea ethmoidalis. There is an average distance of 8.58 ± 5.56 mm between the posterior border of the frontal sinus and the AEA [35].
It lies at a mean distance of 21 mm from the axilla of the middle turbinate and 10 mm from the ostium of the FS [34] (Fig. 3.15).
There is a wide anatomical variation in the course of the anterior ethmoid canal along the skull base. According to the relationship with the anterior skull base, the AEA can run attached to the skull base bone, can run freely along the ethmoid, or in other cases the ethmoid canal may be connected to the skull base through a bony mesentery. Conversely, the canal may be dehiscent, which increases the risk of bleeding during the dissection [30].
Care should be taken at this point as if transected at its lateral portion, retraction may occur within the orbit leading to a retroorbital hematoma which may increase the intraorbital pressure that can result in an occlusion of the central retinal artery. A medial injury where the artery enters the lateral lamella of the cribriform plate may result in a CSF leak.
5.3 First Olfactory Fiber and Nasal Branch of the Anterior Ethmoidal Artery
Extended drainage of the frontal sinus involves resection of the floor of the frontal sinus between the lamina papyracea and the middle turbinate (Draf IIa) or the nasal septum (Draf IIb) anterior to the ventral margin of the olfactory fossa. Draf type III drainage involves bilateral type IIb drainage with the addition of resection of the superior aspect of the nasal septum in the area adjacent to the frontal sinus floor. The posterior limit of the dissection remains anterior to the olfactory fossa [36].
Thus, the first olfactory fiber has been proposed as a reliable landmark to identify the posterior wall of the frontal sinus when performing a Draf III frontal sinusotomy or modified Lothrop especially when carrying out an “Outside-In” frontal drill-out technique [37] (Fig. 3.16).
First olfactory fiber and nasal branch of the anterior ethmoidal artery. (a) Endoscopic image showing the level of the posterior aspect of the superior septectomy. (b) The same as (a): (anterior to the first olfactory fiber: white asterisk). (c) Endoscopic image (Draf IIa) showing the branch of the anterior ethmoidal artery as it courses through the roof of the nasal cavity (black arrow) and the first olfactory fiber in relation to the frontal sinuses. (d) Endoscopic image of a Draf IIb. (e) Endoscopic image of a Draf IIb procedure showing the first olfactory fiber on the left side in relation to the frontal sinus. (f) Endoscopic image after completing a Draf III procedure
In addition, the first olfactory fiber marks the posterior limit of the superior septectomy during the procedure (Fig. 3.17). However, this landmark presents some limitations: it is not always easy to find as in some cases there is fibrosis or anatomical distortion. Conversely, its exposure carries the potential risk of creating a CSF leak by opening the canal in which the fiber runs. Besides, the ventral limit of the olfactory fossa often lies a few millimeters anterior to the posterior wall of the frontal sinus [36]. Thus, recently the septal branch of the anterior ethmoidal artery has been proposed as a safer landmark for identification of the posterior wall of the frontal sinus. The origin of these vessels lies in close proximity to the posterior wall of the frontal sinus in the medial aspect of the anterior ethmoidal roof, it runs within the lateral fissure of the cribriform plate (also known as criboethmoidal foramen) a few millimeters anterior to the first olfactory fiber. Given its localization, it represents a safer landmark for the identification of the posterior wall of the FS. This enables the surgeon to maximize the drilling procedure by opening the medial frontal drainage without risking iatrogenic CSF leaks [38].
Superior septectomy during Draf III procedure. (a) Sagittal dissection. The green area shows the superior septectomy. (b) Endoscopic image showing the incision in the roof of the nasal cavity some millimeters anterior to the axilla of the middle turbinate. (c) First olfactory fibers on the right and left side. The branch of the anterior ethmoidal artery can be identified as it courses through the roof of the right nasal fossa. (d) Endoscopic image showing the posterior limit of the septectomy. (e) Endoscopic picture after Draf IIb procedure. The first olfactory fibers lie some millimeters anterior to the posterior wall of the frontal sinus. White asterisk: First olfactory fiber; Black arrow: Points the branch of the anterior ethmoidal artery as it courses through the roof of the nasal cavity
5.4 Frontal Beak (FB)
The FB is the midline bony thickening that made up the anterior limit of the frontal sinus ostium and the anterior limit of the FR. It is formed by the nasal and orbital process of the frontal bone medially, the frontal process of the maxilla laterally, with a potential contribution from the nasal bone infero-anteriorly. “Frontal beak” is a non-anatomical term that generally refers to the posterior aspect of the nasal process of the frontal bone that can cause narrowing of the ostium [39].
The thickness of the FB may vary eventually according to the pneumatization of the ANC. Wormald supports that a large ANC and frontal ethmoidal cell pneumatization will often reduce the size of the beak, whereas the absence of these cells would produce a thick beak [24].
The FB contributes to the anterior to posterior length of the frontal isthmus defined as the shortest length between the most prominent portion of the FB and the anterior aspect of the olfactory fossa. Sagittal reformatted CT images are helpful in evaluating the size of the beak and its distance to the skull base which has to be reviewed before surgery (Fig. 3.18). These measurements usually offer the degree of difficulty in dissecting the FR. Under normal conditions, the wider the diameter, the easier the surgical dissection. At the level of the frontal ostium, the mean anteroposterior distance between the posterior edge of the FB and the anterior aspect of the olfactory fossa is around 9–12 mm in the midline and around 6 mm laterally. During Draf III procedure, the posterior edge of the FB serves as a reliable landmark for avoiding iatrogenic CSF leak during the superior septectomy [39].
Frontal beak. (a) Sagittal dissection showing the FB (red asterisk). (b) Sagittal view of the frontal bone showing the nasal spine which forms part of the inferior aspect of the frontal sinus. (c) Sagittal dissection showing the FB (red asterisk) as the posterior limit of the superior septectomy. (d) CT scan in the sagittal axial and coronal plane of a specimen showing the anteroposterior distance between the posterior edge of the FB and the anterior aspect of the olfactory fossa
Although it does not predict exactly the level of the skull base, it lies anterior to the olfactory fossa. Thus, it seems to be a safer landmark than the identification of the first olfactory fiber during the superior septectomy.
5.5 Posterior Table of the Frontal Sinus
One of the most feared complications that can occur during endoscopic frontal surgery is the creation of a CSF leak. The reported incidence of CSF leak following a modified Lothrop procedure oscillates between 1 and 6.6% [40, 41].
The Draf III procedure consists of the resection of the FS floor bilaterally, the resection of the frontal intersinus septum, and the creation of a superior septal window (2 × 2 cm). This can be done through an “inside-out” traditional technique that consists of the initial identification of the frontal recesses, followed by the bony removal in a medial direction. Or, as an alternative, the “outside-in” technique that involves drilling down most of the frontal beak before the identification of the FRs [42].
Whatever the case may be, the early identification of the posterior wall of the frontal sinus during the opening of the floor of the sinus provides an essential landmark for safe surgery as CSF leaks can occur mostly at the level of the olfactory fossa and/or at the posterior frontal table of the FS.
The anterior limit of the cribriform plate lies a few millimeters anterior to the posterior wall of the frontal sinus. Therefore, once the posterior wall of the frontal sinus and the anterior limit of the cribriform plate have been identified, the dissection can be extended laterally.
6 Conclusions
In summary, surgery in the FR and FS remains a challenge because of the complex and variable anatomy, the important structures that surround the drainage pathway, and the anatomical disposition that demands the surgeon to perform the surgery in an oblique direction. Imaging techniques and computer-guided navigation systems provide the surgeon with information about anatomical landmarks and variants for planning the surgery to avoid complications or failure. A clear 3D configuration of the frontal area before surgery is necessary to perform a safe and confident procedure. Computer-guided navigation systems based on CT or MR images use preoperatively acquired three-dimensional imaging data. 3D viewers are designed for navigation and visualization of multimodality and multidimensional images and offer all modern rendering modes (multiplanar reconstructions, surface rendering, volume rendering, and maximum intensity projection). Otherwise, insecurity in the frontal recess will often either result in inadequate surgery with functional failure or an increase in the risk of orbit, brain, or vascular injury.
References
Duque CS, Casiano RR. Surgical anatomy and embryology of the frontal sinus. In: Kountakis SE, Senior BA, Draf W, editors. The frontal sinus. Berlin Heidelberg: Springer; 2005. p. 21–31.
Lillie EM, Urban JE, Weaver AA, Powers AK, Stitzel JD. Estimation of skull table thickness with clinical CT and validation with microCT. J Anat. 2015;226(1):73–80.
Levine HL, Clemente MP. Sinus surgery: endoscopic and microscopic approaches. In: Clemente MP, editor. Surgical anatomy of the paranasal sinus. Stuttgart: Thieme; 2003. p. 1–55.
Aydinlioğlu A, Kavakli A, Erdem S. Absence of frontal sinus in turkish individuals. Yonsei Med J. 2003;44(2):215–8.
Kew J, Rees GL, Close D, Sdralis T, Sebben RA, Wormald PJ. Multiplanar reconstructed computed tomography images improves depiction and understanding of the anatomy of the frontal sinus and recess. Am J Rhinol. 2002;16(2):119–23.
de Carvalho Ximendes R, Mangussi-Gomes J, et al. Anatomical relations between the frontal sinus drainage pathway and the agger nasi cell. J Otolaryngol ENT Res. 2018;10(3):118–21.
Patel NS, Dearking AC, O’Brien EK, Pallanch JF. Virtual mapping of the frontal recess: guiding safe and efficient frontal sinus surgery. Otolaryngol Head Neck Surg. 2017;156(5):946–51.
Cho JH, Citardi MJ, Lee WT, Sautter NB, Lee HM, Yoon JH, et al. Comparison of frontal pneumatization patterns between Koreans and Caucasians. Otolaryngol Head Neck Surg. 2006;135(5):780–6.
Lee WT, Kuhn FA, Citardi MJ. 3D computed tomographic analysis of frontal recess anatomy in patients without frontal sinusitis. Otolaryngol Head Neck Surg. 2004;131(3):164–73.
Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope. 1991;101:56–64.
Lund VJ, Stammberger H, Fokkens WJ, Beale T, Bernal-Sprekelsen M, Eloy P, et al. European position paper on the anatomical terminology of the internal nose and paranasal sinuses. Rhinol Suppl. 2014;24:1–34.
Wormald P-J, Hoseman W, Callejas C, et al. The international frontal sinus anatomy classification (IFAC) and classification of the extent of endoscopic frontal sinus surgery (EFSS). Int Forum Allergy Rhinol. 2016;6(07):677–96.
Park SS, Yoon BN, Cho KS, Roh HJ. Pneumatization pattern of the frontal recess: relationship of the anterior-to-posterior length of frontal isthmus and/or frontal recess with the volume of agger nasi cell. Clin Exp Otorhinolaryngol. 2010;3:76–83.
Kim KS, Kim HU, Chung IH, et al. Surgical anatomy of the nasofrontal duct: anatomical and computed tomographic analysis. Laryngoscope. 2001;111:603–8.
Stamm A, Nogueira JF, Americo RR, Solferini Silva ML. Frontal sinus approach: the ‘vertical bar’ concept. Clin Otolaryngol. 2009;34(4):407–8.
Draf W. Frontal sinus. In: Kountakis S, Senior B, Draf W, editors. Endonasal frontal sinus drainage type I–III according to draf. Berlin: Springer; 2005.
Dassi CS, Demarco FR, Mangussi-Gomes J, Weber R, Balsalobre L, Stamm AC. The frontal sinus and frontal recess: anatomical, radiological and surgical concepts. Int Arch Otorhinolaryngol. 2020 Jul;24(3):e364–75.
Bradley DT, Kountakis SE. The role of agger nasi air cells in patients requiring revision endoscopic frontal sinus surgery. Otolaryngol Head Neck Surg. 2004;131(4):525–7.
Kennedy DW, Senior BA. Endoscopic sinus surgery: a review. Otolaryngol Clin N Am. 1997;30:313–30.
Thawley SE, Deddens AE. Transfrontal endoscopic management of frontal recess disease. Am J Rhinol. 1995;9:307–11.
Orhan M, Govsa F, Saylam C. A surgical view of the superior nasal turbinate: anatomical study. Eur Arch Otorhinolaryngol. 2010;267(6):909–16.
Stammberger H, Posawetz W. Functional endoscopic sinus surgery. Concept, indications and results of the Messerklinger technique. Eur Arch Otorhinolaryngol. 1990;247(2):63–76.
Huang BY, Lloyd KM, DelGaudio JM, Jablonowski E, Hudgins PA. Failed endoscopic sinus surgery: spectrum of CT findings in the frontal recess. Radiographics. 2009;29(1):177–95.
Wormald PJ. The agger nasi cell: the key to understanding the anatomy of the frontal recess. Otolaryngol Head Neck Surg. 2003;129(5):497–507.
Landsberg R, Friedman M. A computer-assisted anatomical study of the nasofrontal region. Laryngoscope. 2001;111(12):2125–30.
Bent JP 3rd, Cuilty-Siller C, Kuhn FA. The frontal cell as a cause of frontal sinus obstruction. Am J Rhinol. 1994;8:185–91.
Kuhn FA. Chronic frontal sinusitis: the endoscopic frontal recess approach. Oper Tech Otolaryngol Head Neck Surg. 1996;7:222–9.
Choby G, Thamboo A, Won TB, Kim J, Shih LC, Hwang PH. Computed tomography analysis of frontal cell prevalence according to the International Frontal Sinus Anatomy Classification. Int Forum Allergy Rhinol. 2018;8(7):825–30.
Jang DW, Lachanas VA, White LC, Kountakis SE. Supraorbital ethmoid cell: a consistent landmark for endoscopic identification of the anterior ethmoidal artery. Otolaryngol Head Neck Surg. 2014 Dec;151(6):1073–7.
Monjas-Cánovas I, García-Garrigós E, Arenas-Jiménez JJ, Abarca-Olivas J, Sánchez-Del Campo F, Gras-Albert JR. Radiological anatomy of the ethmoidal arteries: CT cadaver study. Acta Otorrinolaringol Esp. 2011;62(5):367–74.
Comer BT, Kincaid NW, Smith NJ, Wallace JH, Kountakis SE. Frontal sinus septations predict the presence of supraorbital ethmoid cells. Laryngoscope. 2013;123(9):2090–3.
Comer BT, Kincaid NW, Kountakis SE. The association between supraorbital ethmoid air cells and orbital proptosis in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2013;3(2):147–9.
Keros P. On the practical value of differences in the level of the lamina cribrosa of the ethmoid. Z Laryngol Rhinol Otol. 1962;41:809–13.
Lee WC, Ming Ku PK, van Hasselt CA. New guidelines for endoscopic localization of the anterior ethmoidal artery: a cadaveric study. Laryngoscope. 2000;110(7):1173–8.
Ko YB, Kim MG, Jung YG. The anatomical relationship between the anterior ethmoid artery, frontal sinus, and intervening air cells; can the artery be useful landmark? Korean J Otorhinolaryngol-Head Neck Surg. 2014;57(10):687–91.
Upadhyay S, Buohliqah L, Vieira Junior G, Otto BA, Prevedello DM, Carrau RL. First olfactory fiber as an anatomical landmark for frontal sinus surgery. Laryngoscope. 2016;126(5):1039–45.
Knisely A, Barham HP, Harvey RJ, Sacks R. Outside-in frontal drill-out: how I do it. Am J Rhinol Allergy. 2015;29(5):397–400.
Turri-Zanoni M, Arosio AD, Stamm AC, Battaglia P, et al. Septal branches of the anterior ethmoidal artery: anatomical considerations and clinical implications in the management of refractory epistaxis. Eur Arch Otorhinolaryngol. 2018;275(6):1449–56.
Craig JR, Petrov D, Khalili S, Brooks SG, et al. The nasofrontal beak: a consistent landmark for superior septectomy during Draf III drill out. Am J Rhinol Allergy. 2016;30(3):230–4.
Wormald PJ. Salvage frontal sinus surgery: the endoscopic modified Lothrop procedure. Laryngoscope. 2003;113:276–83.
Batra PS, Cannady SB, Lanza DC. Surgical outcomes of drillout procedures for complex frontal sinus pathology. Laryngoscope. 2007;117:927–31.
Chin D, Snidvongs K, Kalish L, Sacks R, Harvey RJ. The outside-in approach to the modified endoscopic Lothrop procedure. Laryngoscope. 2012;122(8):1661–9.
Acknowledgments
To the anatomy laboratory of the Faculty of Medicine from the Miguel Hernández University of Elche (Alicante), for their great collaboration and help to prepare the specimens for dissection.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cánovas, I.M., Garrigós, E.G. (2022). Frontal Sinus Classical and Endoscopic Anatomy. In: Lobo, D.R., Artiles, J.V., Ospina, J.A. (eds) Atlas of Frontal Sinus Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-98128-0_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-98128-0_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-98127-3
Online ISBN: 978-3-030-98128-0
eBook Packages: MedicineMedicine (R0)