Abstract
Retroperitoneal tumors are a topic of interest to different specialties. Due to the variety of diagnoses, there are few references that contemplate the theme all together. In this chapter, we chose to analyze the different tumors that may present as retroperitoneal mass, including primary tumors of the retroperitoneal space, primary tumors of retroperitoneal organs that may occupy the retroperitoneal space, intraperitoneal tumors that simulate retroperitoneal lesions, and retroperitoneal lymph node masses. In clinical practice, diagnostic uncertainty regarding the finding of a retroperitoneal mass can lead to misconceptions and be harmful to the patient. Our goal is to address the clinical, radiological, and therapeutic aspects of the different diagnoses. We present a suggestion of the “step by step” to be followed for the diagnostic clarification and also discuss vascular problems related to each diagnosis. The idea is that specialists from different areas can take advantage of the list of diagnoses discussed and keep in mind the diversity of situations associated with the theme.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
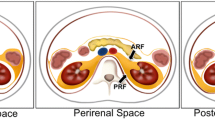
The retroperitoneal space is composed of retroperitoneal organs, connective tissue, nerves, lymphatic vessels, and blood vessels, including the abdominal aorta and its branches, and the inferior vena cava and its tributaries. Different types of lesions can occupy the retroperitoneal space and represent a true diagnostic challenge, not rarely associated with vascular problems. The retroperitoneum limits are the diaphragm, the pelvic floor, the posterior leaflet of the parietal peritoneum, the paravertebral musculature, and the posterior musculature of the abdominal wall (major psoas, minor psoas, lumbar square, internal obturator, and piriform muscles) [1,2,3].
The diagnosis of a retroperitoneal mass generally occurs as a consequence of incidental findings or during the investigation of increasing abdominal volume, mass perception, or abdominal pain. Depending on the etiology and location of the mass, neurological symptoms, ascites, and gastrointestinal symptoms may be present, as well as fever secondary to tumor necrosis, digestive hemorrhage due to hollow viscera invasion, and systemic manifestations, such as fatigue and weight loss. The presence of venous thrombosis, vascular stenosis, collateral veins in the abdominal wall, and edema of lower limbs and scrotum also can occur as a consequence of associated vascular phenomena.
In general, 80% of retroperitoneal neoplasia are malignant. With the exception of visceral tumors, 55% are sarcomas and stromal tumors, 40% are lymphomas and 5% correspond to other primary tumors and lymph node metastases. A prolonged clinical history, the scarcity of symptoms, and the radiologic appearance of a nonaggressive lesion are characteristics that favor the diagnosis of a benign lesion (20%), most often surprised during routine exams [4,5,6].
The main diagnostic hypotheses regarding a retroperitoneal mass can be divided into four groups, including lesions that are not primarily tumors of the retroperitoneal space, but, due to similarities in clinical presentation, should be included in the list of differential diagnoses: (1) intraperitoneal lesions that simulate retroperitoneal tumors; (2) primary tumors of retroperitoneal organs; (3) primary tumors of the retroperitoneal space; and (4) retroperitoneal lymph node masses. In each of these groups, we will find a list of possible diagnoses (Fig. 7.1).
2 General Considerations
Most of the time, clinical history, physical examination, and appropriate image tests allow us to think about the diagnostic hypothesis, even before obtaining material for pathological analysis. An initial total abdominal computed tomography (CT) with intravenous contrast guides the next steps. Most of the time, chest and mediastinal CT should be included since the beginning. In some cases, magnetic resonance image (MRI) allows a more detailed assessment of the nature of the lesion and its relationship to vessels, nerves, and muscles, offering complementary information to CT. Specific angiographic studies can be useful in the evaluation of invasion, displacement, and/or involvement of vascular structures, although they are not necessary in most cases. The PET/CT 18F-FDG can add value in the investigation of retroperitoneal lymphadenopathy, helping to distinguish between lymphomas, germ cell tumors, and metastatic carcinomas. Other specific tests, such as scintigraphy with metaiodobenzylguanidine (131I-MIBG), scintigraphy with somatostatin receptors (Octreoscan), and PET/CT – 68GA-Dotatate, may be necessary to elucidate the diagnosis in the suspicion of secreting tumors (pheochromocytomas, paragangliomas, and neuroendocrine tumors).
The radiological differentiation between large intraperitoneal tumors, large primary tumors of retroperitoneal organs, primary tumors of the retroperitoneal space, and large lymph node masses can be challenging. Among intraperitoneal tumors, stromal tumors (GIST and EGIST), visceral sarcomas, and adnexal masses deserve special mention. Primary epithelial tumors of intraperitoneal organs can also manifest as large tumors and simulate primary tumors of the retroperitoneal space; however, it is not our aim to discuss them. Large primary tumors of retroperitoneal organs can be difficult to differentiate radiologically from primary tumors of the retroperitoneal space and should also be remembered. Another group of lesions that can simulate primary tumors of the retroperitoneal space are lymph node masses. In addition to the specific complaints reported by the patient, one should actively question the presence of B symptoms (fever, night sweats, weight loss), recent travel story, exposure to infectious diseases, use of illicit drugs, contact with animals, family history of autoimmune diseases, personal history of fertility and cryptorchidism (men), and gynecological and obstetric history (women), in addition to personal and family cancer history. In physical examination, palpation of all lymph node bases is essential. The detection of peripheral lymphadenopathy directs the diagnostic investigation to the group of diseases that lead to diffuse lymph node involvement, including retroperitoneal lymph nodes. In men, careful testicular examination should be performed. Even in the absence of findings, the diagnosis of a primary testicular cancer metastatic to retroperitoneal lymph nodes should be considered and testicular ultrasound performed, especially in young patients.
In addition to chest, abdomen, and pelvis CT scans, initial studies should include measures of lactate dehydrogenase (LDH), alpha-fetoprotein (AFP), and beta-human chorionic gonadotropin (ß-HCG). Other tumor markers and specific serum measurements should also be done depending on the clinical suspicion. High levels of LDH are suggestive of lymphoma and high levels of AFP and ß-HCG are suggestive of germ cell tumors.
Some examples of tumors that present as retroperitoneal masses and illustrate the diversity of situations are presented below. Most of the cases that illustrate this chapter are the result of personal experiences; otherwise, the source will be mentioned in the text (Fig. 7.2).
Examples of tumors that manifest as retroperitoneal masses. See how difficult it is to predict the diagnosis without clinical history data. (a) Retroperitoneal liposarcoma. (b) Retroperitoneal ganglioneuroma. (c) Paraganglioma. (d) Leiomyosarcoma of the vena cava. (e) Gastric GIST. (f) Retroperitoneal non-Hodgkin lymphoma
3 Differential Diagnoses
3.1 Group 1. Intraperitoneal Tumors That Simulate Retroperitoneal Lesions
Gastrointestinal Stromal Tumor (GIST) and Extra-Gastrointestinal Stromal Tumor (EGIST)
Gastrointestinal stromal tumors (GISTs) represent 1% of the digestive tract tumors. GISTs are rare tumors in individuals below 40 years of age, with a mean age of 64 years at diagnosis [7]. They are most common in the stomach (60%) and small intestine (30%) and rare in the colon and rectum (6%) and in the esophagus (0.7%) [8,9,10]. These tumors arise from Cajal’s interstitial cells at the interface between the autonomic innervation of the intestinal wall and the smooth muscle, acting in the control of peristalsis (“pacemaker cells”) [11]. Occasionally, they are considered primary of the omentum, mesentery, or peritoneum, possibly originating from Cajal cells that dispersed during embryogenesis, a condition in which they are called extra-gastrointestinal stromal tumors (EGISTs) [12]. It is assumed that GISTs and EGISTs originate from CD34-positive Cajal stem cells that are differentiated from the pacemaker cell phenotype [13]. They generally appear as subepithelial lesions that can cause ulceration in the epithelial lining, but can reach large dimensions through exophytic growth and occupy the abdominal cavity, simulating retroperitoneal tumors. Although the majority is sporadic, about 5% of patients have some autosomal dominant familial syndrome, including familial GIST syndrome, type 1 neurofibromatosis (NF1), and Carney-Stratakis syndrome. Phenotypic, histological, and molecular characteristics are similar in familial and sporadic forms [14].
The CD117 antigen (KIT, kinase tyrosine) is a transmembrane receptor product of the KIT protooncogene (human homologue of the viral oncogene v-KIT). Over 80% of GISTs have a mutation in the KIT gene. Thus, the diagnosis of GIST is often made from the immunohistochemical expression of the KIT protein [15]. Other changes can also occur, such as activating mutations in the platelet-derived growth factor receptor alpha (PDGFRA) and function gains that lead to an abnormally activated structural variant of the KIT protein [16, 17]. Although some GISTs are negative for the mutation, more than 90% are positive for KIT expression. The remaining 10% negative for KIT expression may also be negative for mutations in the KIT gene, but harbor activating mutations in the PDGFRA gene [18]. Thus, only 10–15% of GISTs do not have a KIT or PDGFRA mutation. However, regardless of the mutational status of KIT and PDGFRA, DOG-1 (Discovery on GIST-1) and PKC-theta (protein kinase C theta) immunohistochemistry expression is also used for diagnosis [19]. In most suspected cases, a combination of CD117 and DOG1 in the immunohistochemistry assessment is sufficient to confirm the histological diagnosis [20].
About 10–30% of GISTs progress to malignancy, with exophytic growth observed in 79%, while intraluminal or mixed growth is less common [10]. Through exophytic growth, they are diagnosed as large masses that can manifest through gastrointestinal bleeding, increased abdominal volume, or abdominal pain (Fig. 7.3). Larger tumors can cause obstruction of the gastrointestinal lumen by endoluminal growth or by compression of the gastrointestinal tract. Perforated neoplasms show signs of peritonitis or intraperitoneal bleeding secondary to pressure necrosis and ulceration. Despite the size of the lesion, it is not uncommon for the patient to be in good general condition. On physical examination, the relative mobility of the lesion can clinically suggest the diagnosis of GIST, once the origin can be in mobile segments of the gastrointestinal tract. Bulky pelvic lesions characteristically compress the rectum and displace or involve the bladder and prostate. Large tumors can generate peritoneal and liver metastases [21].
A 60-year-old male patient, complaining of pain associated with increased abdominal volume. On physical examination, a large abdominal mobile mass was noted. A heterogeneous lesion is observed on CT scan, with areas of necrosis and a “geographical” contour. Renal anatomical variation. Operative finding of a massive primary lesion of the proximal jejunum. Segmental enterectomy was performed with complete resection. Definitive diagnosis of GIST
There are no serum tumor markers specific for GISTs and the presumptive diagnosis requires familiarity with its radiological appearance. In potentially resectable tumors, preoperative biopsy is not mandatory; however, it will be mandatory if metastatic disease is suspected or if the use of preoperative imatinib is considered.
Location, size, and rate of mitosis are independent prognostic factors, as well as information about tumor capsule integrity [22, 23]. Extra-gastric tumors are considered to be more aggressive than gastric ones, a fact that has been questioned [24]. Different classifications have been proposed to categorize the risk of recurrence, including the modified NIH classification, where lesions are classified into four groups according to the risk of recurrence: (1) Very low risk (any location and <2 cm and <5 mitoses/50HPF). (2) Low risk (any location and 2.1–5 cm and <5 mitoses/50CGA). (3) Intermediate risk (gastric location and <5 cm and 6–10 mitoses/50HPF or gastric location and 5.1–10 cm and <5 mitoses/50HPF). (4) High risk (any location with perforated tumor or >5 cm and >5 mitoses/50HPF or >10 cm and >10 mitoses/50HPF or nongastric and 2.1–5 cm and >5 mitoses/50HPF or 5.1–10 cm and <5 mitoses/50HPF) [25].
Some guidelines recommend neoadjuvant therapy with imatinib to reduce tumor size and minimize morbidity in patients with primary GISTs considered resectable with high morbidity [26, 27]. The appropriate time for surgical intervention is not standardized. In general, patients are treated for 6–9 months with the tyrosine kinase inhibitor and then considered for surgery if the tumor is amenable to complete resection [28]. Although it has been shown that the tumor burden continues to decrease even after 1 year of imatinib, the average time to obtain the best response is 3.5 months, with little decrease in size after 9 months [29]. All patients treated with preoperative imatinib should resume therapy with tyrosine kinase inhibitor postoperatively to maximize the benefit of the drug.
During laparotomy, the abdomen must be fully explored to exclude metastatic spread, with special attention to the liver and peritoneal surfaces. The goal of surgical treatment is complete resection with free margins. Surgical maneuvers must carefully avoid tumor rupture, which increases the risk of peritoneal recurrence. Very wide margins are generally not necessary; however, just-tumor resection should be avoided as opposed to segmental resection of the tumor’s origin viscera. In cases of macroscopic invasion of adjacent organs, en bloc resection is recommended. Due to the low rate of lymph node disease, routine lymphadenectomy is not necessary, being indicated only in situations of clinically compromised or suspected lymph nodes.
In the adjuvant scenario, considering high-risk patients undergoing complete resection, the rates of recurrence-free survival and overall survival are 65.6% versus 47.9% and 92% versus 81.7%, respectively, comparing 3 years and 1 year of adjuvant treatment [30].
The involvement of large vessels is not common; however, the involvement of visceral vascular trunks can occur (Fig. 7.4).
Visceral Sarcomas
Visceral sarcomas are rare tumors in general. Visceral leiomyosarcomas typically appear on CT as large masses with varying degrees of necrosis and heterogeneous contrast enhancement, sometimes with dystrophic calcification [31]. In addition to the characteristics of direct invasion and distant metastasis, other aspects may suggest malignancy in the differentiation between gastrointestinal leiomyomas and leiomyosarcomas: size >5 cm, lobed contours, heterogeneous enhancement, infiltration of mesenteric fat, ulceration, regional lymphadenopathy, and exophytic growth pattern [32]. Due to endoluminal involvement, they can lead to intestinal obstruction. In the absence of invasion of adjacent structures, segmental resection with a wide margin is the treatment of choice. En bloc resection is necessary if adjacent organs are macroscopically compromised. Lymph node metastases are rare; however, in the case of intestinal resections, in our view, the inclusion of the lymph node base relative to the affected segment should be considered (Fig. 7.5).
A 45-year-old female patient complaining of mass in the right hypochondrium, with noticeable mobility on physical examination. A cystic lesion with peripheral calcifications is observed on CT. Colonoscopy demonstrated signs of extrinsic compression and irregularity in the mucosa of the proximal transverse colon. Note the intraoperative finding of primary solid-cystic mass of the transverse colon wall. Segmental colectomy with regional lymphadenectomy was performed. Definitive diagnosis of high-grade sarcoma with epithelioid component and ossification, primary of the transverse colon
Uterine sarcomas are relatively rare tumors of aggressive behavior that represent less than 10% of cancers of the uterine body. They arise from the myometrium or from the connective tissue elements of the endometrium [33]. Uterine leiomyosarcomas represent 60–70% of cases. They must be carefully investigated in order to avoid diagnostic confusion with uterine leiomyomas. Uterine leiomyosarcomas usually occur in perimenopause, at an average age of 50 years and appear as large pelvic masses, which can cause bleeding or a sensation of vaginal or abdominal pressure. Unfortunately, the diagnosis is rarely suspected before an operation, often being detected accidentally after hysterectomies and nononcological myomectomies, which are extremely harmful for the effective control of the disease [34].
Despite its rarity, visceral sarcomas must be remembered among the differential diagnoses of retroperitoneal tumors, although in most cases they are primary tumors of intraperitoneal organs. Vascular involvement is uncommon.
Adnexal Masses
Pelvic adnexal masses that acquire large volumes are capable to occupy the extension of the abdominal cavity and generate diagnostic doubts. In the suspicion of tumors of gynecological origin, ultrasound assessment, status in relation to menopause, and the value of CA-125 are important factors to be considered in the interpretation of malignancy [35, 36]. Smooth contoured lesions (unilocular or multilocular) and the absence of intra-tumor blood flow at the doppler ultrasound suggest benign lesions, while irregular solid tumors, ascites, papillary projections, and intra-tumor blood flow are signs of malignancy [37]. Multilocular cystic lesions with solid areas, bilateral lesions, and intra-abdominal metastases also favor the possibility of an adnexal malignancy. Despite the importance of the information provided by ultrasonography, larger tumors must be evaluated by CT and/or MRI in order to accurately determine the origin of the tumor and its relationship to adjacent organs. Primary mucinous tumors of the ovary, as well as benign tumors and “borderline” tumors, can acquire large volumes, configuring among the diagnoses of intraperitoneal lesions that simulate retroperitoneal tumors. Some scoring systems using clinical, laboratory, and image data help to differentiate between benign and malignant lesions and can be useful [38]. Figures 7.5 and 7.6 show examples of large adnexal masses that may raise doubts about the possibility of a retroperitoneal tumor (Figs. 7.6 and 7.7).
An 81-year-old female patient with increased abdominal volume and normal Ca125 value. A large cystic, homogeneous, and uninoculated lesion is showed on CT, occupying the entire length of the abdominal and pelvic cavity. Intraoperative appearance shows a smooth capsule and the adnexal origin. Definitive pathological diagnosis of ovarian mucinous cystadenoma
A 29-year-old female patient complaining lumbar pain and increased abdominal volume. The Ca125 tumor marker was normal. The CT shows a complex multiseptated pelvic lesion occupying the lower abdomen and the pelvis. Intraoperative view of the mass originating from the right ovary. The surgical specimen shows the multiloculated aspect of the lesion and its mucinous content. Pathological diagnosis of ovary “borderline” mucinous tumor
Krukenberg tumors, described by Friedrich Ernst Krukenberg, represents 1–2% of ovarian tumors and are considered metastatic ovarian tumors [39]. They are characterized by the presence of adenocarcinoma with signet ring cells rich in mucin, originating mainly from primary gastrointestinal tumors, the stomach being the most common primary site (70%). Gastric and colorectal origin account for 90% of Krukenberg tumors, which are bilateral 80% of the time [40, 41]. Some hypotheses are postulated to explain the dissemination mechanism that gives rise to ovarian metastases. In Krukenberg tumors, the chances of lymphatic and hematogenous dissemination are the most likely, since they also occur in cases of early tumors, confined to the mucosa and submucosa, where there is a rich blood and lymphatic network. The lack of peritoneal involvement in part of the cases also favors this hypothesis as opposed to the transcelomic theory [42].
Ovarian metastases can be asymptomatic or manifest through nonspecific gastrointestinal symptoms, such as abdominal or pelvic pain, increased abdominal volume, ascites, or dyspareunia. Occasionally, they can become hormone-secreting tumors, leading to vaginal bleeding, irregular menstrual cycle, hirsutism, and virilization [39]. If ovarian masses are suspected, Krukenberg tumors should be distinguished from primary ovarian neoplasms with signet ring cells with or without mucinous material. In large masses, the differential diagnosis involves radiological and endoscopic evaluation and the measurement of tumor markers (CEA, Ca-72.4, Ca-125, Ca-19.9) to investigate primary gastrointestinal tumors (Fig. 7.8). Vascular involvement is not a common problem.
3.2 Group 2. Primary Tumors of Retroperitoneal Organs
The involvement of retroperitoneal organs (duodenum, pancreas, kidneys, adrenal glands, and parts of the ascending and descending colon) by nonepithelial tumors is rare. In all organs, however, we can find neoplasms represented by a spectrum of tumors similar to those that can arise in other locations: lipoma, myelolipoma, adenoma, leiomyoma, liposarcoma, leiomyosarcoma, desmoid tumor, schwannoma, peripheral nerve sheath tumor, tumor solitary fibrous tissue, neuroendocrine tumor, and lymphoma, among others. Theoretically, any of these lesions that originate in a retroperitoneal organ and reach a significant size may present radiologically as a tumor of the retroperitoneal space.
Primary malignant duodenal tumors represent only 0.3% of all gastrointestinal tumors. Despite the rarity, there is a relatively high proportion of duodenal tumors compared to other segments of the small intestine. The most common neoplasms are epithelial (adenocarcinoma, adenoma, Brunner’s glandular hyperplasia), but in the presentation simulating tumors of the retroperitoneal space, tumors of mesenchymal origin (GIST, leiomyomas, leiomyosarcomas, neurofibromas), lymphomas, and neuroendocrine tumors (carcinoid, gastrinoma, and neuroendocrine carcinoma) should be considered (Fig. 7.9) [43]. Nonampullary and periampullary duodenal adenocarcinomas constitute the largest group of lesions and must be considered in the differential diagnosis of retroperitoneal tumors; however, in our experience, the primary duodenal GIST can most commonly acquire large dimensions and, due to exophytic growth, simulate a primary tumor of the retroperitoneal space.
Case 1 – A 48-year-old female patient complaining of postprandial packing. CT shows a retroperitoneal mass displacing the structures of the hepatic hilum, with possible involvement of the duodenal-pancreatic sulcus, compressing and displacing the right renal vein. It is difficult to distinguish between a primary tumor of a retroperitoneal organ and a primary tumor of the retroperitoneal space. Upper gastrointestinal endoscopy demonstrated the duodenal involvement. Definitive diagnosis was done during the surgery. It was a leiomyosarcoma primary of the vena cava. Case 2 – A 78-year-old male patient complaining of abdominal pain in the right hypochondrium and melena. CT shows an expansive and heterogeneous solid lesion, with lobulated contours, located on the posterior wall of the second portion of the duodenum, with extensive posterior expansive component. Note the compression and displacement of the inferior vena cava and the renal vessels on the right. Echo-endoscopy biopsy revealed the diagnosis of duodenal GIST
When the organ of origin of the tumor is the pancreas, although ductal adenocarcinoma is the most common type, a variety of other benign and malignant tumors can manifest as a retroperitoneal mass, including epithelial (exocrine and endocrine) and nonepithelial tumors (mesenchymal origin from vessels, stroma, adipose cells, and neural cells), in addition to lymphomas and metastases. Most of the rare pancreatic tumors are frequently diagnosed at an advanced stage due to symptoms related to the mass effect. In general, the presence of hemorrhage in a solid-cystic tumor suggests a solid and pseudopapillary tumor; an enlarged pancreas without dilation of the main pancreatic duct may suggest primary lymphoma of the pancreas; the presence of an intralesional fat component is suggestive of a benign lesion [44]. The size of pancreatic neoplasms varies widely, from microscopic foci to large cystic neoplasms that may project in the retroperitoneum and also simulate a primary tumor of the retroperitoneal space (Fig. 7.10).
A 45-year-old female patient, complaining of discomfort on the left flank. CT scan shows a solid-cystic lesion with peripheral calcifications located near to the inferior border of the pancreas. During the surgery, a primary lesion of the pancreas projecting into the retroperitoneum was confirmed. Definitive pathological diagnosis of a pancreatic mucinous cystadenoma
The adrenal gland can be the site of several different tumors that may appear occupying the retroperitoneal space: adenomas, pheochromocytomas, carcinomas, lymphomas, myelolipomas, ganglioneuromas, neurilemomas, ganglioneuroblastomas, and also metastasis from different primary tumors (Fig. 7.11). Increases in the adrenal gland may also be secondary to tuberculosis, a disease that should be included in the list of differential diagnoses [45].
Renal masses are divided into pseudotumor, benign solid masses (adenomas, oncocytomas, angiomyolipomas, others), and malignant solid masses (renal cell carcinoma, collecting duct carcinoma, medullary carcinoma, transitional cell carcinoma, lymphomas, leukemias, sarcomas, and metastases) [46]. Larger lesions can also hamper the interpretation of the renal origin and simulate an origin in the retroperitoneal space and should be considered among the differential diagnoses.
The retroperitoneal segments of the ascending and descending colons are seats of epithelial tumors, but nonepithelial lesions are rare. As in the duodenum, lesions of mesenchymal origin, lymphomas, and neuroendocrine tumors can occur and manifest themselves simulating a tumor of the retroperitoneal space.
As we have seen, tumors of primary retroperitoneal organs, when acquiring greater volume, can simulate primary tumors of the retroperitoneal space and should be considered in the list of deferential diagnoses. In these groups of tumors, the risk of vascular involvement is varied, being associated with the organ of origin. Large primary tumors of the pancreas, adrenal, and kidney can involve the local vascular pedicles adding technical difficulty and morbidity to surgical procedures.
3.3 Group 3. Primary Tumors of the Retroperitoneal Space
3.3.1 Benign Tumors
Approximately 20% of primary neoplastic lesions in the retroperitoneal space are benign. Schwannomas, ganglioneuromas, paragangliomas, angiomyolipomas, lipomas, retroperitoneal desmoid fibromatosis, and retroperitoneal fibrosis are the most common retroperitoneal benign tumors.
Schwannomas
Schwannomas (also called neurilemomas) represent the most common type of peripheral nerve tumor. They are encapsulated tumors that originate from Schwann cells and grow from peripheral nerves or nerve roots in an eccentric manner, incorporating the nerve into the lesion capsule. Sporadic schwannomas affect patients of all ages, with a higher incidence between 20 and 50 years. Many schwannomas are discovered incidentally. Lesions with a long course of evolution can suffer degenerative changes (nuclear pleomorphism, hyalinization of blood vessels, hemorrhage, focal necrosis, and calcification), a condition in which the image is distinct and can cause diagnostic misunderstanding [47]. Schwannomas and neurofibromas can occur sporadically or in association with neurofibromatosis (NF). Neurofibromas are seen in NF1 and can undergo malignant transformation. Schwannomas are associated with NF2 and do not develop into malignant lesions, with the exception of atypical variants.
Schwannomas are treated surgically; however, not all patients need to be operated. Asymptomatic patients or patients with few symptoms and high surgical risk can be observed. Sometimes, however, the lack of a definitive diagnosis can corroborate to surgical indication (Fig. 7.12). In retroperitoneal lesions, pain and symptoms resulting from compression of adjacent organs and structures are the main reasons for surgical resection. Complete resection should be sought; however, when the resection implies in partial or total nerve sacrifice and consequent functional deficit, intracapsular resection is allowed to preserve function, minimizing the residual neurological deficit [48]. Large schwannomas of the retroperitoneal space can determine vascular involvement. In this condition, when surgery is indicated, en bloc resections followed by revascularization are required (Fig. 7.13) [49].
A 47-year-old male patient. Incidental finding of retroperitoneal tumor on routine ultrasound. Complementary investigation with CT showing a solid lesion in close contact with the superior mesenteric artery. A biopsy was performed by echo-endoscopy showing a tumor of neurogenic origin. Surgery was performed with complete resection bordering the superior mesenteric artery. Definitive pathological analyses confirmed the diagnosis of schwannoma
A 53-year-old female patient complaining of abdominal pain with radiation to the posterior region of the right lower limb. The CT shows a solid retroperitoneal mass with wide contact to L5 and S1 vertebral bodies. The lesion compresses and displaces the right iliac vessels. An image-guided biopsy was performed and the diagnosis of schwannoma was confirmed
Ganglioneuromas
Ganglioneuromas, neuroblastomas, and ganglioneuroblastomas are tumors that belong to the group of peripheral neuroblastic tumors formed by mature ganglion cells. Ganglioneuromas are rare slow-growing tumors that arise from sympathetic ganglion cells derived from embryonic neural crest cells and possibly represent the final stage of neuroblastoma maturation. They are benign, large, and encapsulated tumors, more common in young women. Ganglioneuromas can occur anywhere in the sympathetic chain, being more common in the mediastinum, retroperitoneum, and adrenal glands. They are commonly asymptomatic, except when having a mass effect and compression of local organs and structures. In the presacral location, they can cause root compression and pain [50]. Immunohistochemistry shows strong S100 positivity in ganglion cells and Schwann cells [51].
The treatment of choice is complete surgical resection. In the retroperitoneum, ganglioneuromas may involve vascular trunks and nerves, making resection laborious or even contraindicated due to the risk of extensive visceral devascularization. It is not uncommon to find the tumor capsule attached to vascular structures, which makes total excision a high-risk procedure. Thus, the indication for surgery should be evaluated sparingly, since slow growth and the absence of symptoms may not interfere with quality of life, favoring active surveillance with imaging tests as an alternative to a high-risk operation. In this case, through tumor growth and onset of symptoms, the operation should be reconsidered (Figs. 7.14 and 7.15).
A 32-year-old female patient had a preaortic retroperitoneal mass found during a routine abdominal ultrasound. MRI shows a solid expansive lesion, poorly vascularized, with lobulated contours and well-defined limits measuring 8.2 × 5.0 × 4.1 cm, located in the retroperitoneum, displacing the pancreas anteriorly and maintaining contact with the left adrenal gland. The lesion involves the celiac trunk and its branches, which are patent, with normal caliber and regular contours. It also maintains contact with the superior mesenteric artery and the inferior vena cava and has a compressive effect on the splenic vein. An image-guided biopsy was performed and revealed the diagnosis of ganglioneuroma. The patient has been in follow-up for 5 years, asymptomatic, with imaging tests demonstrating the stability of the lesion
A 26-year-old female patient complaining of abdominal pain. CT shows a large heterogeneous solid retroperitoneal mass, lobulated, with calcifications in between, in the topography of the right adrenal gland. The mass almost completely surrounds the circumference of the inferior vena cava, displaces the right hepatic lobe anteriorly, the pancreas contralaterally and the right kidney inferiorly. There is no clear cleavage plane with the inferior vena cava, that is laterally displaced. (a) Wide laparotomy with visualization of the lesion occupying the upper right hemi-abdomen. (b) En bloc resection was necessary, including the right kidney and a large segment of the vena cava; note the reconstruction of the vena cava segment with a prosthesis and the reimplantation of the left renal vein in the prosthesis. (c) Operative specimen. (d) CT scan control 6 months after the operation. The patient is asymptomatic for 4 years, with no evidence of disease. (Courtesy of Frederico José Teixeira Jr – oncologic surgery and Luciana Ragazzo Araujo Teixeira – vascular surgery)
Paragangliomas
Paragangliomas are rare neuroendocrine tumors that arise from extra-adrenal autonomic paraganglia, small organs made up mainly of neuroendocrine cells derived from the embryonic neural crest, similar to those that migrate to the adrenal gland. Histologically, paragangliomas are indistinguishable from pheochromocytomas, which is why they are also called “extra-adrenal pheochromocytomas,” just as pheochromocytomas are called “intra-adrenal paragangliomas.”
Most parasympathetic paragangliomas are not functional and are distributed along the glossopharyngeal and vagus nerves, in the neck and at the base of the skull. In contrast, sympathetic paragangliomas usually secrete catecholamines and are located in the sympathetic paravertebral ganglia of the chest, abdomen, and pelvis. About 75% of the sympathetic paragangliomas arise in the retroperitoneum, most often at the junction of the vena cava with the left renal vein, in the Zuckerkandl organ or next to the aortic bifurcation, close to the emergence of the inferior mesenteric artery. Thus, more often, retroperitoneal paragangliomas originate from sympathetic ganglia and are secretory, presenting clinically as pheochromocytomas, with hypertension, episodic headache, sweating, and tachycardia [52]. Most paragangliomas are benign, diagnosed between the third and fifth decades of life [53]. Malignant paragangliomas are rare (20% of abdominal paragangliomas). Malignancy is defined by the appearance of metastases during the course of the disease [54].
Sporadic paragangliomas are more common in patients over 40 years of age and hereditary forms are more common in younger patients. The proportion between men and women is the same in hereditary forms; however, sporadic cases are more common in women (71% vs. 29%) [55]. Unlike the data suggested by the “Rule of 10” (10% bilateral or multiple, 10% familial, 10% extra-adrenal, 10% malignant), today it is considered that about 25% of paragangliomas are multiple and 30–50% are associated with some hereditary syndrome, the multiplicity being rare in sporadic cases (1.2%) [56]. Previously, hereditary paragangliomas were associated with von Hippel Lindau disease (BVS), multiple endocrine neoplasia type 2 (MEN2), and neurofibromatosis type 1 (NF1) [57]. More recently, it has been shown that 30% of them are secondary to mutations in germ lines of other genes: SDH (succinate dehydrogenase), SDHAF2, TMEM127, and MAX. SDHB mutations are associated with a higher risk of malignancy (31%) and a worse prognosis [58].
Paragangliomas are highly vascularized tumors, usually associated with blood vessels and neural structures. They are usually diagnosed by investigating symptoms related to elevated levels of metanephrines and catecholamines or as an incidental finding on imaging. Histological diagnosis is almost always required, especially when biochemical tests show increased dosage of catecholamine metabolites [59, 60]. Immunohistochemical staining confirms the neuroendocrine nature of cells, with strong diffuse positivity for specific neuron enolase (NSE), synaptophysin, and/or chromogranin, usually with negative staining for keratins [61].
Among catecholamine-secreting tumors, 15–20% are extra-adrenal, most of which are abdominal or pelvic [57]. The most common extra-adrenal sites are abdominal para-aortic regions (75%), urinary bladder (10%), chest (10%), and base of the skull, neck, and pelvis (5%) [62].
In retroperitoneal paragangliomas, due to the greater possibility of being catecholamine secretors, adequate initial investigation is essential in order to avoid potentially serious complications resulting from invasive procedures capable of causing the release of catecholamines and vasoactive peptides. A presumptive diagnosis can be made by the association of biochemical and imaging tests. The screening test recommended for initial evaluation is the measurement of free plasma metanephrines or urinary unconjugated differential metanephrines [63]. Compared to plasma or urinary catecholamines and vanillylmandelic acid, metanephrine levels are more sensitive (98%). It is important to keep in mind that some substances (caffeine) and drugs (beta-blockers, sympathomimetics, tricyclic antidepressants, monoaminoxidase inhibitors, alpha methyl dopa, levodopa, and paracetamol) and acute events (acute myocardial infarction, acute lung edema, and stroke) can increase catecholamine concentrations and generate false positive results. Plasma chromogranin A, a co-secreted protein, is often increased in functional and nonfunctional paragangliomas and also assists in the diagnosis (sensitivity 83–89%). Likewise, there is a risk of false positive results in the measurement of chromogranin A as a consequence of organic disorders (liver or kidney failure) and use of proton pump inhibitors [64].
Once a paraganglioma has been identified, functional tests will be necessary to complement the investigation and evaluate the existence of metastases and/or multiple tumors [52]. It is important to note that biopsy is contraindicated in patients with suspected paraganglioma, unless the results of the biochemical analysis for catecholamine secretion are negative or the patient is prepared with alpha-adrenergic block, otherwise the biopsy may trigger a hypertensive crisis secondary to the release of catecholamines. For the same reason, surgical interventions must be performed in reference centers, with interaction between the teams of endocrinology, anesthesia, and surgery, so that the preoperative and intraoperative periods are conducted by a team of experienced professionals. During the surgical procedure, constant communication of the operative steps is essential in order to allow the anesthesiologist to be prepared and to anticipate great variations in blood pressure. The patient must be properly monitored and have adequate vascular access (Fig. 7.16).
A 74-year-old female patient with difficult to control systemic arterial hypertension. The investigation led to the finding of retroperitoneal mass and elevation of serum catecholamines. The patient was treated with alpha-adrenergic block and prepared for surgery. (a, b) CT shows a solid vascularized lesion with signs of compression of the portal vein and inferior vena cava, insinuating itself posteriorly to the hepatic hilum. (c) MIBG scintigraphy showing the tumor in the highlight area. (d) Intraoperative appearance of the tumor and vascular control of the portal vein and inferior vena cava. (e) View of the operative field with exposure of the inferior vena cava and segment I of the liver after complete resection. Definitive diagnosis of paraganglioma. (Courtesy of Frederico José Teixeira Junior, oncologic surgery)
Angiomyolipoma and Lymphangioleiomyoma (Lymphangioma)
Angiomyolipomas are benign tumors that contain atypical blood vessels and smooth muscle in varying proportions [65]. The most common site for angiomyolipoma is the kidney, where it presents as an intrarenal mass. Occasionally, however, it can grow exophytically in the retroperitoneum, reach large dimensions and, due to its high fat content, simulate the diagnosis of liposarcoma [66, 67]. Based on the fat content, they are divided into “fat-rich” (classic type) and “fat-poor,” both benign, without metastatic potential. A third rare type is the epithelioid form, which has malignant potential and is part of the family of perivascular epithelial cell neoplasms (PEComas) [68,69,70].
Isolated sporadic angiomyolipomas represent 80% of the cases, the others being associated with the tuberous sclerosis complex (Bourneville-Pringle disease), a rare autosomal dominant genetic condition. The changes affect cell proliferation and differentiation, resulting in hamartomatous lesions in many organs, including the kidneys, with renal angiomyolipoma being the most common association (50–80%). Although rare and benign, large lesions and the association with tuberous sclerosis increase the risk of complications, including intralesional bleeding, which can be one of the initial manifestations. Sporadic angiomyolipoma occurs mainly in women in the fourth and fifth decades of life. Angiomyolipoma associated with tuberous sclerosis is typically a larger, multifocal, or bilateral tumor, more frequent in younger patients (Fig. 7.17) [71, 72].
Lymphangioleiomyomatosis (lymphangiomyomatosis; LAM) is a rare disease of unknown etiology, observed only in women, usually in the reproductive period, often associated with pulmonary involvement. Two forms of lymphangioleiomyomatosis are described: sporadic (S-LAM) and associated with the tuberous sclerosis complex (TSC-LAM). Both forms are related to mutations in the TSC1 or TSC2 genes, which results in overactivation of the mTOR pathway. Postmenopausal occurrence is very rare [73].
Extrapulmonary involvement in the form of angiomyolipomas and retroperitoneal adenopathy can occur in up to 75% of cases. The evolution tends to be slow, progressive, and hormone-dependent, characterized by the formation of diffuse thin-walled cysts in the lungs and angiomyolipomas in the kidneys [74, 75].
The lymphangioleiomyomas (lymphangiomyoma) of the retroperitoneum and pelvis are benign lymph-filled tumors that occur in 16–38% of patients with LAM They can be asymptomatic or generate nausea, bloating, abdominal pain, edema of the lower extremities, or urinary symptoms due to displacement of the bladder, in addition to chyluria due to lymphangioleiomyomatous connections with the renal collecting system. The worsening of symptoms throughout the day is explained by the variation in size due to gravity, food intake, and exercise [76]. Retroperitoneal and pelvic lymphadenopathy are more common than mediastinal lymphadenopathy, consistent with its origin in the lower abdomen or pelvis. Several reports of lymphangioleiomyomatosis describe lesions in the uterus and ovaries, in addition to uterine leiomyomas (fibroids). Sometimes, intravenous progression through the gonadal veins can reach the inferior vena cava with upward migration to the cardiac atrium (Fig. 7.18) [77, 78].
A 31-year-old female patient with a history of previous hysterectomy for large uterine leiomyoma. After hysterectomy, an atrial cardiac mass was found. The echocardiogram revealed a 4 cm mobile and heterogeneous mass partially filling the lumen of the inferior vena cava, projecting into the right atrium. MRI images demonstrate the extent of the lesion through the right gonadal vein and progression within the inferior vena cava to the right atrium. (a, b) Operative field showing dissection and repair of the inferior vena cava, the right and left renal veins and the right gonadal vein filled with tumor (upper portion of photo b). (c) View of the inferior vena cava (supra-hepatic portion) and pericardium, exposed before completing the sternotomy. (d) Ultrasonographic record of the atrial thrombus. (e) Sternotomy and opening of the right atrium with the patient in extracorporeal circulation. (f) Operative specimen showing the gonadal vein with tumor thrombus and the thrombus in the shape of the inferior vena cava with the intra-atrial portion. (g) Suture of the inferior vena cava and final aspect of the operation. The patient is asymptomatic with 2 years of follow-up, with no evidence of disease. (Courtesy of Frederico José Teixeira Junior, oncologic surgery; Nelson de Luccia, vascular surgery; and Fábio Gaiotto, cardiac surgery)
The retroperitoneal location and the possibility of associated lymphadenomegaly add angiomyolipomas and lymphangioleiomyoma in the list of differential diagnoses of retroperitoneal tumors with the possibility of vascular involvement.
Lipomas
Lipomas are benign proliferations of mature adipose cells. They are classified according to morphology into: fibrolipoma, conventional lipoma, angiolipoma, spindle cell lipoma, and myelolipoma. The occurrence in the retroperitoneal space is rare. Among primary retroperitoneal lesions, they represent only 0.2% of neoplasms. Retroperitoneal lipoma can appear in different tissues: adipose, conjunctive, muscular, lymphatic, or nervous. It can also originate from the mesentery, Gerota’s fascia, or the urogenital tract [79].
The clinical presentation is variable. They can be asymptomatic, found during routine imaging exams, or course with an increase in volume and generate symptoms resulting from the compression of adjacent organs and structures. Generally, additional tests are not necessary beyond computed tomography; however, due to its rarity occupying the retroperitoneal space, uncertainty leads to further investigation to exclude other diagnostics and MRI can help. The definitive diagnosis between a lipoma and a well-differentiated liposarcoma depends on pathological examination [80]. Fluorescent in situ hybridization (FISH) for amplification of MDM2 has been considered a useful test for definitive distinction between a lipoma and a well-differentiated liposarcoma, with the gene being amplified in the liposarcoma. Surgery is the therapeutic modality of choice. It is important to mention, however, that even in the conviction of a benign lesion, an effort must be made to achieve a complete resection, without fragmentation of the lesion. Due to its benign characteristics, vascular involvement is not expected (Fig. 7.19).
3.3.2 Malignant Tumors
Retroperitoneal Soft Tissue Sarcomas
Retroperitoneal sarcomas represent 10–15% of total soft tissue sarcomas and constitute an important diagnosis among primary malignant neoplasms of the retroperitoneal space [81]. Due to the absence of specific symptoms in the early stages, the diagnosis is usually postponed until growth leads to compression, displacement, and/or invasion of adjacent organs and structures, including large vessels. One third of patients will experience some neurological symptom secondary to the effect of compression or stretching of lumbar or pelvic nerve plexuses. Gastrointestinal symptoms and nonneoplastic ascites secondary to extrinsic compression and/or invasion of vascular structures can occur, respectively, in 10% and 15% of cases [5, 82].
In adults, the most common histological types of retroperitoneal sarcomas are liposarcomas and leiomyosarcomas, followed by nonclassifiable undifferentiated sarcomas, including pleomorphic sarcomas. Other less common histologies are malignant tumor of the peripheral nerve sheath, synovial sarcoma, solitary fibrous tumor, and small round cell desmoplastic tumor [83]. In children, the most common histological types are extra-skeletal Ewing tumor/primitive neuroectodermal tumor (PNET), alveolar rhabdomyosarcoma, and fibrosarcoma [84].
Among liposarcomas, the most common subtypes are well-differentiated and dedifferentiated sarcomas. Well-differentiated liposarcomas have no metastatic potential, but local recurrences are relatively common. Dedifferentiated liposarcomas are defined by the presence of regions of nonlipogenic sarcomatous tissue within a well-differentiated tumor, sometimes difficult to distinguish from undifferentiated pleomorphic sarcomas [85]. They are high-grade tumors, with high metastatic potential and risk of death. The other subtypes (myxoid and round cells) are less common in the retroperitoneum [86, 87]. Liposarcomas can reach large volumes and constitute a real surgical challenge (Fig. 7.20).
Case 1 – A 75-year-old female patient. CT shows an extensive well-defined lesion predominantly containing fat, suggestive of well-differentiated liposarcoma, molding itself in the retroperitoneal space through the displacement of adjacent organs and involving the right kidney. The patient was operated on and the diagnosis was confirmed. Case 2 – A 37-year-old male patient, complaining of an increase in abdominal volume for a year and a half, associated with weight loss and asthenia. The biopsy was performed in an external service, resulting in a high-grade liposarcoma. Due to the low performance status, the patient was admitted for clinical compensation and nutritional support and prepared for the operation. Note a large volume heterogeneous lesion on CT scans, occupying the entire length of the abdominal and pelvic cavity. (a) Patient in the operating room (note the large abdominal volume, the dilation of the superficial veins at the abdominal wall, and the edema of the lower limbs, compatible with compression of the vena cava). (b) Operative bed showing en bloc resection, including the right kidney and the right and transverse proximal colon. (c) Operative specimen weighing 27 kg (note the need for associated resection of the abdominal wall in the area of tumor invasion). The patient had excellent postoperative recovery and is at 1 year of follow-up, with no evidence of disease
When the hypothesis is a leiomyosarcoma, special attention should be paid to the possibility of primary origin in retroperitoneum vessels, including the origin in the inferior vena cava and its tributaries (Figs. 7.21 and 7.22). In this case, the risk of lung metastases is high and 10% of patients present with distant metastases at diagnosis [88]. Leiomyosarcomas can also originate from the wall of the gastrointestinal tract and uterus, a situation in which they are considered visceral sarcomas rather than retroperitoneal tumors and are at increased risk of peritoneal and hepatic spread.
A 59-year-old female patient noticed an abdominal mass on self-examination. MRI showed a retroperitoneal mass with lobulated contours, with heterogeneous sign, exuberant vascularization, and areas of necrosis, in contact or originating in the inferior vena cava, with involvement of the right ureter and hydronephrosis. Note that the vena cava is not seen from the confluence of the common iliac veins up to the level of L3–L4. The patient underwent an image-guided biopsy and the pathological examination revealed a high-grade leiomyosarcoma. Neoadjuvant radiotherapy was performed, followed by surgery. During the operation, the presence of liver metastases was detected, which led to the interruption of the procedure (shown in the last photo). Two years after the date of the surgery, the patient is undergoing systemic treatment with stable disease
A 63-year-old female patient previously treated for lung cancer. In follow-up exams, a solid nodule was noted in the anterior portion of the left psoas muscle with increased metabolism on PET-CT. The patient underwent an image-guided biopsy that revealed the diagnosis of high-grade leiomyosarcoma. During the operation, it was possible to conclude that it was a primary leiomyosarcoma of the left gonadal vein
Once the diagnosis of retroperitoneal sarcoma is confirmed, surgical resection is the only potentially curative approach. The most important prognostic factor is a complete resection at the initial presentation. Upon complete resection, the degree of histological malignancy is the second factor to be considered, with a worse prognosis for high-grade tumors. Depending on the size and location, a resection with microscopically negative margins (R0) is not always feasible. For this reason, complete macroscopic resections with compromised microscopic margins (R1) are common, although not desirable. This characteristic justifies the high rates of locoregional recurrence observed in different series [89, 90].
Ideally, patients with retroperitoneal sarcomas should be treated in centers with experience [91]. The lack of prospective randomized clinical trials regarding the use of neoadjuvant and adjuvant treatments leads to a wide variation in treatment protocols. Despite the lack of evidence, considering that large size, depth, and high-grade tumors have higher metastatic potential, some reference centers advocate a possible benefit of systemic chemotherapy, particularly in chemosensitive histologies. Likewise, since obtaining wide three-dimensional margins is not routine, the use of perioperative radiotherapy is also discussed in order to reduce the rates of local recurrence. In this sense, it is possible to point out some advantages of preoperative radiotherapy in relation to the postoperative one: smaller radiation field, lower dose rate, and greater safety by avoiding the irradiation of uncommitted structures, which will occupy the tumor bed after resection, making postoperative planning difficult and increasing the risk of actinic complications. In practice, despite these premises, there is great disagreement as to the best approach for the treatment of patients with retroperitoneal sarcomas. The therapeutic decision is influenced by factors such as histological type, degree of malignancy, tumor size, and tumor location in the retroperitoneal space.
Among low-grade sarcomas, the most common are the well-differentiated liposarcomas. In most cases, well-differentiated retroperitoneal liposarcomas are amenable to complete resection and the treatment begins with the operation. In larger tumors, however, where complete resection is expected to be difficult, the use of preoperative radiotherapy should be discussed on a case-by-case basis, although there is little enthusiasm for the use of radiation in low-grade retroperitoneal tumors. In general, adjuvant chemotherapy and radiotherapy are not indicated for low-grade sarcomas that are totally resected. When the histology is considered chemosensitive (synovial, myxoid liposarcomas, intermediate, and high-grade round cell liposarcoma), the use of neoadjuvant chemotherapy with or without radiotherapy should be discussed. Among sarcomas of intermediate or high grade with histology not sensitive to chemotherapy, the use of preoperative radiotherapy followed by surgery or exclusive surgery is the most common strategy. The use of intraoperative radiotherapy is an interesting option to be offered in some cases, either as an exclusive modality or as part of the strategy to minimize the necessary pre- or postoperative doses, reducing the risk of side effects (Fig. 7.23). For primary leiomyosarcomas of the inferior vena cava and dedifferentiated liposarcomas, due to the high metastatic potential, neoadjuvant chemotherapy with or without preoperative RT should be discussed.
A 60-year-old female patient complaining of pain and edema of the left lower limb for 6 months. (a, b) MRI shows an expansive (20 cm × 16 cm) heterogeneous lesion in the lower left retroperitoneal region, insinuating itself through the femoral canal, medially displacing the iliac vessels, the gonadal vein, and the ureter, with a necrotic and hematic component and peripheral nodular foci. Observe the contact of the lesion with the iliac and femoral vessels, without signs of invasion or irregularities, in addition to wide contact with the left iliac muscle and extension below the inguinal ligament, following the ileo-psoas tendon in the plane of the myotendinous transition. An image-guided biopsy was performed which revealed the diagnosis of pleomorphic sarcoma (high grade). (c) Neoadjuvant radiotherapy planning. (d) Patient in the operating room with planning to perform Karakousis incision. (e) View of the operative field with the lesion occupying the retroperitoneal space in the lower left quadrant. (f) Operative bed after complete marginal resection with wide dissection of the iliac vessels and left ureter. (g) Positioning the applicator to perform a complementary dose of intraoperative radiotherapy. (h) Rotation of an omentum flap interposed between the iliac vessels and the ureter to protect the retroperitoneal space. (i) Surgical specimen with a high rate of necrosis. After postoperative recovery, the patient received adjuvant chemotherapy and is at 3 years of follow-up, with no signs of disease
The role of neoadjuvant radiotherapy in retroperitoneal sarcomas is being evaluated in a prospective randomized trial [92]. In this study, patients were randomized to receive preoperative radiation therapy (50.4 Gy), followed by surgery or exclusive surgery. In an exploratory analysis, preoperative radiotherapy benefited exclusively the subgroup of liposarcomas (71.6% vs. 60.4%; HR = 0.64, 95% CI 0.40–1.01, p = 0.049).
Some factors are pointed out to justify the nonresectability and/or contraindication for surgical approach: extensive vascular involvement, peritoneal implants, nonresectable distant metastases, and involvement of the mesentery root or spinal cord. In our view, vascular involvement, in most cases, does not represent a contraindication to surgery or even to achieve a radical operation and will be discussed later. When complete resection is not possible, partial resections are contraindicated and will be performed exceptionally for palliation and relief of symptoms.
Solitary Fibrous Tumor
Solitary fibrous tumor comprises a histological spectrum of fibroblastic mesenchymal neoplasms that are rarely metastatic. They can occur at any location and age, with no preference for gender, and are most common between the fifth and seventh decades, in the pleura, peritoneum, and meninges. About 30% of solitary fibrous tumors appear in the peritoneal cavity, retroperitoneal soft tissues, and pelvis, the retroperitoneum being the most common intra-abdominal site (Fig. 7.24). Large tumors can involve multiple organs that can make differential diagnosis difficult [93].
The characterization of malignancy based on histological aspects (mitotic activity, necrosis, hemorrhage, size, cellularity, nuclear pleomorphism, and stromal or vascular invasion) is controversial, as these criteria have a low correlation with clinical outcome [94, 95]. The anaplastic variant represents a clearly malignant tumor, with aggressive behavior and rapid progression, but occurs in less than 1% of cases [96]. The lipomatous variant is even more rare. Most are benign, although they are included among malignant variants due to the possibility of an immature lipoblastic component. A focal myxoid change is common, probably resulting from increased mucin production by connective neoplastic cells tissue [97]. The solitary fibrous tumor has a broad spectrum of biological behavior. Most are indolent and have a low risk of local recurrence or metastasis. Late recurrences can occur, even for tumors initially classified as “benign.” Among tumors classified as malignant, 10–40% will have liver metastases after 5 years, which highlights the need for continued long-term follow-up, especially for individuals of high risk (≥4 mitoses for 10 high magnification fields, presence of necrosis or hemorrhage, large size, high cellularity, nuclear pleomorphism, and stromal or vascular invasion) [98, 99].
The most common symptom is a palpable abdominal mass, followed by pain and weight loss. Small tumors are typically asymptomatic, and symptoms begin when the lesion reaches larger sizes (>20 cm). The presentation can rarely be secondary to hypoglycemia as a manifestation of para-neoplastic syndrome. Refractory hypoglycemia (Doege-Potter syndrome) occurs in less than 5% of cases and is seen mainly in large peritoneal and pleural tumors, caused by the secretion of insulin-like growth factor 2 (IGF-2). The IGF-2 gene is among the target genes of EGR, possibly deregulated by the chimeric transcription factor NAB2-STAT6, a molecular characteristic of solitary fibrous tumor [100].
Solitary fibrous tumors are characterized by a recurrent inversion of the long arm of chromosome 12 (12q13). This inversion results in the fusion of two genes, NAB2 (NGFI-A binding protein 2) and STAT6 (signal transducer and transcription activator factor 6). The fusion creates a chimeric transcription factor NAB2-STAT6 that is constitutively located in the nucleus, being a distinct molecular characteristic of solitary fibrous tumor, present in up to 100% of cases, not detected in other tumors [101, 102].
For localized disease, complete surgical resection with negative margins (R0) is the standard treatment. There is not enough evidence to justify the use of neoadjuvant or adjuvant therapy in a systematic way, although the use of adjuvant radiotherapy for tumors considered to be at high risk is discussed [103]. After incomplete resections or resections with compromised microscopic margins, the use of radiotherapy should be discussed individually. Given the rarity of these tumors, the role of adjuvant chemotherapy is unknown.
For unresectable or metastatic disease, there is no established standard of treatment. The use of oral antiangiogenic tyrosine kinase inhibitors associated with temozolomide provides therapeutic benefits similar to traditional chemotherapy with less toxicity and has been considered a therapeutic option [104]. The use of target drugs with agents directed to vascular endothelial growth factor (VEGF) and other tyrosine kinase signaling pathways are being evaluated for the treatment of advanced disease (sunitinib, sorafenib, axitinib) [105,106,107].
Although rare, the solitary fibrous tumor must be part of the list of differential diagnoses of retroperitoneal tumors. In the image, the finding of a solid, circumscribed, richly vascularized tumor nourished by prominent vessels should resemble the hypothesis of a solitary fibrous tumor. When there is a risk of intraoperative bleeding, preoperative arterial embolization should be considered (Fig. 7.25).
A 71-year-old male patient with retroperitoneal mass found during routine ultrasound. On physical examination, the patient had a palpable mass in the right iliac fossa, with a noticeable thrill and audible murmur. (a) CT shows an expansive process with intense post-contrast enhancement in the arterial, portal, and venous phases, with lobulated contour and foci of hypodense images suggestive of a fibrous component. (b) Arteriography showing that the lesion is nourished by two dominant arteries, branches of the right internal and external iliac arteries. Due to the rich vascularization, biopsy was contraindicated, and preoperative embolization was programmed. (c) Selective microcatheterization of the arterial branches responsible for the vascularization of the lesion, followed by embolization with PVA microparticles until vascular stasis. The control arteriography showed adequate devascularization of the lesion. (d) View of the lesion occupying the retroperitoneal space in the right iliac fossa. (e) View of the operative field with exposure of the right ureter and iliac vessels. There was no bleeding because the arterial branches were properly occluded by preoperative embolization, performed hours before the operation; (f) Surgical specimen: definitive diagnosis of solitary fibrous tumor. (Preoperative embolization: Francisco Carnevale, interventional radiologist)
Ewing’s Sarcoma
Ewing’s sarcoma is a rare malignancy in adults. In children, it usually presents as a primary bone tumor. Occasionally, they appear in the soft tissues (extra-osseous Ewing’s sarcoma). Tumors of the Ewing family include the primitive peripheral neuroectodermal tumor (PNET). As these tumors share histological, immunohistochemical, and unique chromosomal translocations, they are considered to be of common origin [108]. The involvement of the extra-osseous site is reported in up to 11%, including the retroperitoneum, the adrenal glands, and the soft parts of the extremities [109]. Despite the rarity, they should be remembered in the differential diagnosis of retroperitoneum tumors, particularly in young people (Fig. 7.26).
A young male patient with a large retroperitoneal mass, previously submitted to image-guided biopsy resulting in a tumor of the Ewing/PNET family. The patient received systemic chemotherapy according to the specific protocol, with partial response. (a) CT shows the appearance of the mass after chemotherapy, displacing the bladder, the small intestine, and the colon and compressing the rectum. Note the extensive area of necrosis and the involvement of retroperitoneal lymph nodes. (b) Operative field after bilateral Karakousis incision: repair of the spermatic cord, the inferior vena cava, and the right ureter – observe the displacement of the adjacent organs. (c) Operative specimen: observe the groove determined by the impression of the vessels in the lesion. (d, e) Operative field after tumor complete resection with vascular preservation – observe the wide retroperitoneal and pelvic dissection and the return of the organs to the usual position
Both extra-osseous Ewing tumors and PNET respond to the same chemotherapy regimens as osseous Ewing’s sarcoma and are treated in the same way [110]. Ewing’s sarcomas of the retroperitoneal space should be discussed in a multidisciplinary setting once treatment may involve chemotherapy, radiation, and surgery.
Malignant Paraganglioma
Since it is not possible to define the malignancy based on histological findings, the determination of malignancy in paragangliomas is not straightforward. Nuclear pleomorphism, necrosis, rate of mitosis, and local invasion, characteristics commonly seen in malignant tumors, can also be seen in benign paragangliomas. About 25% of paragangliomas are malignant, defined by the development of metastases. The highest rates of malignancy are observed in paragangliomas associated with mutations inherited in the ß-subunit of the succinate dehydrogenase gene (SDHB), which are usually abdominally located and secretory. In multiple endocrine neoplasia syndrome type 2 (MEN2), 3–5% of paragangliomas are malignant [57].
Several scoring systems have been proposed to calculate the risk of malignancy for pheochromocytomas considering invasion, histological growth patterns, cytological characteristics, and mitotic activity. One of the most used is the “Pheochromocytoma of the adrenal gland scoring scale (PASS)” and can also be applied to paragangliomas. A PASS score <4 or >6 suggests benign and malignant lesions, respectively, while a value between 4 and 6 suggests an intermediate risk [111, 112] (Fig. 7.27). The biochemical phenotype also does not allow the differentiation between benign and malignant paragangliomas; however, the presence of large noradrenaline-producing paragangliomas and increased levels of plasma dopamine or its metabolite suggest malignancy. Malignancy is also more often associated with very high plasma levels of chromogranin A [52].
A 21-year-old female patient with abdominal mass found during obstetric ultrasound. Increased plasma catecholamines were found. After pregnancy, she was prepared for surgery with adrenergic block. The definitive diagnosis was paraganglioma. PASS calculation: Wide nests or diffuse architecture (in more than 10% of the tumor): 0 out of (2); central or confluent tumor necrosis: 2 out of (2); high cellularity: 0 out of (2); cell monotony: 0 of (2); spindle cell component: 0 of (2); mitosis figures >3/10 CGA: 0 of (2) (identified 01 mitosis in 10 HPF); atypical mitosis figures: 0 of (2); extension in adipose tissue: 0 of (2); vascular invasion: 1 of (1); capsular invasion: 1 of (1); accentuated nuclear pleomorphism: 0 of (1); nuclear hyperchromasia: 0 of (1) – total score: 04 = intermediate risk for malignancy. (Courtesy of Tibério Moura de Andrade Lima, surgical oncology)
The diagnostic approach of paraganglioma requires evidence of excessive catecholamine release and anatomical documentation of a tumor. The increase in plasma metanephrine fractions has high sensitivity (97%) and specificity (93%) for diagnosis. On the other hand, the measurement of catecholamine fractions (epinephrine and dopamine) is less sensitive, although clearly high values (>2 times the upper limit of the normal range) are also diagnostic. Mild elevations in the levels of metanephrine and catecholamine fractions in plasma and urine may be secondary to the use of drugs leading to false positive results (tricyclic antidepressants, antipsychotic agents, levodopa, and serotonin and norepinephrine reuptake inhibitors). Thus, when investigating catecholamine-secreting tumors, tricyclic antidepressants and other psychoactive agents should be reduced and discontinued at least 2 weeks before any hormonal assessment [52].
Combined α- and β-adrenergic block should be proposed for patients with secretory paragangliomas that are candidates for surgery. Treatment must begin at least 7 days before the operation, in order to control blood pressure and prevent intraoperative hypertensive crises. Adrenergic blockade can be performed with a nonselective or selective α-adrenergic receptor antagonist, accompanied by a sodium-rich diet and generous fluid intake. The β-adrenergic antagonist should be administered to control tachycardia after α-adrenergic block has been effective in normalizing blood pressure. Only with β-adrenergic block, severe hypertension or cardiopulmonary decompensation can occur as a result of unopposed adrenergic stimulation. However, care should be taken with the risk of sustained postoperative hypotension as a consequence of preoperative α-adrenergic block [52].
Although a laparoscopic approach may be recommended for benign paragangliomas, malignant tumors are usually large and/or located in areas that are difficult to manage laparoscopically. In cases of proven or suspected malignancy, open surgery is recommended, preserving the principles of oncological surgery to avoid capsule rupture and minimize the risk of local recurrence [113, 114].
Radionuclide treatment should be considered in patients with nonresectable metastatic disease. Likewise, external radiotherapy can also be considered in the treatment of inoperable paragangliomas and for pain control of bone metastases. In recurrent or metastatic disease, “debulking” palliative surgery, ablation, and radiotherapy procedures represent alternatives to decrease tumor burden and catecholamine secretion [52]. Patients with secretory retroperitoneal paragangliomas require special attention and should be treated at referral centers.
Extragonadal Germinal Tumor
Germ cell tumors are classified as extragonadal if there is no evidence of a primary tumor in the testicles or ovaries. They are classified as seminomatous (dysgerminomas, in women), nonseminomatous (non-dysgerminomas, in women), mature teratomas, and immature teratomas. Nonseminomatous tumors include yolk sac tumors, choriocarcinomas, embryonic carcinomas, teratomas, and mixed tumors. They usually appear in midline locations, most commonly in the anterior mediastinum and retroperitoneum.
The differential diagnosis is made mainly with retroperitoneal metastasis of a primary testicular germ cell tumor and other poorly differentiated histologies. As testicular palpation is not sufficient to exclude a primary testicular tumor, testicular ultrasound should be performed in all patients [115]. The distinction between true extragonadal germ cell tumors and retroperitoneal metastasis from primary regressed testicular tumors is difficult [116, 117]. Extragonadal nonseminomatous tumors are associated with elevations in serum AFP and/or HCG-ß in 85% of cases. The frequency of abnormalities in tumor markers is different between mediastinal and retroperitoneal tumors. Mediastinal nonseminomatous tumors are more likely to result in pronounced elevations of serum AFP and less likely to result in elevations of HCG-ß compared to gonadal and retroperitoneal tumors [118].
Extragonadal germ cells tumors usually present as bulky masses in the retroperitoneal space. Clinical behavior, prognosis, and treatment are similar to those of metastatic testicular germ cell tumors. Generally, systemic chemotherapy with cisplatin-based regimens is the initial approach. Thus, surgery is not the first step, being reserved for the rescue of residual masses [119].
Mature cystic teratomas are extremely rare and usually appear as a well-circumscribed complex cystic mass that contains a variable amount of fluid, fat or sebum, and calcification. Although most teratomas are benign, a variety of malignant components may be present or develop from clonal transformation, but in the retroperitoneum, they rarely undergo malignant transformation.
Most malignant retroperitoneal germ cell tumors are metastases from primary gonadal tumors, seen in 30% of patients of gonadal GCTs [120]. As mentioned earlier, careful examination of the testicles is essential in all patients with retroperitoneal masses. Occasionally, the primary testicular tumor is not visible or small intratesticular scars are found in patients with retroperitoneal GCT. These scars represent regressed GCTs, a phenomenon known as “burnout” [121]. Retroperitoneal GCTs are usually large in presentation. Symptoms and signs include a palpable mass with or without pain, weight loss, constipation, back and hip pain, dyspnea, leg swelling, fever, varicocele, and urinary retention. Involvement, displacement, and compression of the abdominal vessels are common (Fig. 7.28).
A 31-year-old male patient who sought medical attention complaining of low back pain on the right. The images showed a large retroperitoneal mass, predominantly solid with areas of necrosis and involvement of the right common, the common iliac artery and the right renal pedicle. The inferior vena cava also seems to be involved. The patient did not report testicular changes, however, as part of the investigation; AFP and HCG-ß were collected and proved to be increased. The testicular ultrasound performed in the sequence revealed a 6 mm lesion in the right testicle. The patient underwent radical orchiectomy, and the pathological examination confirmed the presence of a small area of embryonic carcinoma. The patient was treated according to a systemic chemotherapy protocol, with normalization of the markers, but with persistence of a large residual retroperitoneal mass. He is currently scheduled for surgery with the possibility of associated vascular resection
Retroperitoneal teratomas represent 1–11% of primary retroperitoneal tumors. The incidence is bimodal, with peaks in the first 6 months of life and early adulthood, usually identified after reaching large sizes. The chance of malignancy is around 25%. Surgical resection remains the basis of therapy and is necessary for a definitive diagnosis. As the preoperative diagnosis is based on needle biopsy, it is possible that complete resection reveals the presence of germ cell tumor elements and the patient will be a candidate for adjuvant chemotherapy [122].
Large retroperitoneal masses and recurrences are associated with a greater chance of involvement of large vessels. Upon surgical indication, the possibility of vascular resections should be provided. Depending on previous chemotherapy regimens, there is a possibility of impaired renal function. During surgery, there may be a need for transient clamping of the renal vessels or nephrectomy, contributing to the risk of postoperative renal failure. In this condition, the possibility of renal revascularization or renal auto-transplantation should be considered.
3.3.3 Fibromatoses and Fibroses
Desmoid Fibromatosis
Desmoid fibromatosis (DF), also known as “desmoid tumor,” “aggressive fibromatosis,” or “deep musculoaponeurotic fibromatosis,” is a disease characterized by locally aggressive behavior. It can develop anywhere, being more common on the trunk, extremities, abdominal wall, and intra-abdominal region (small bowel and mesentery). In patients with Familial Adenomatous Polyposis (FAP), they are more common in the intra-abdominal region. Most of the time, DF appears as a painless mass with slow growth. In progression, intra-abdominal masses can cause intestinal obstruction, ischemia, and perforation [123].
The conclusive diagnosis is established by pathological examination. Nuclear positivity for beta-catenin in immunohistochemistry suggests the diagnosis of DF, although the lack of expression does not exclude the diagnosis. Other entities (superficial fibromatosis, low-grade myofibroblastic sarcomas, solitary fibrous tumors) may also show nuclear positivity for beta-catenin [124]. The diagnosis can be improved through Next-Generation Sequence with detection of mutations in the CTNNB1 gene. Changes that result in the activation of the Wnt pathway may be present and also help in the diagnosis [125].
Most of the time, DFs have slowed an indolent growth. Periods of growth arrest and even spontaneous regression can occur [126,127,128]. Intra-abdominal desmoids acquire singular importance in FAP patients and can be the cause of death in up to 11%, once the possibility of complete resection is low due to diffuse infiltration of the mesentery or due to multiplicity [129]. Resection can lead to severe morbidity, resulting in extensive enterectomy, intestinal ischemia, risk of obstruction, and intestinal fistulas [130]. In addition, recurrence rates are high and the recurrent disease tends to be more aggressive compared to the initial one [131]. For these reasons, conservative treatment strategies have been advocated rather than a surgical approach, at least in the early stages of treatment [132].
The most current strategy for treating DF is multimodal. Some options are watchful-waiting, systemic therapy with noncytotoxic drugs (nonhormonal anti-inflammatory ± tamoxifen), radiotherapy, target drugs (imatinib), and cytotoxic chemotherapy. For patients with large resectable intra-abdominal DF, surgery should be considered, although the chance of insufficient margins and incomplete resection is high, particularly if there is involvement of the mesentery, vessels, or vital organs (Fig. 7.29) [133].
A 27-year-old male patient with familial adenomatous polyposis associated with a mesentery desmoid tumor (Gardner’s syndrome). History of previous surgeries for resection of the desmoid tumor without success and failure of drug treatments. He presented with disease progression and intestinal perforation generating an abdominal sepsis. CT images show the presence of a large mass involving the root of the superior mesenteric artery and encompassing practically the entire small bowel. Presence of air in the bile ducts can be observed. In these moments, the patient was in the ICU, intubated, with vasoactive drugs. After discussion with family members and the ethics committee, a laparotomy was proposed, knowing the possibility of total enterectomy and the need for permanent parenteral nutrition. The diagram in the figure represents the surgery performed, with total enterectomy associated with total colectomy and closure of the duodenum distally to the duodenal papilla. The intraperitoneal rectum was closed. In order to create a drainage pathway for bile, saliva, and gastric juice and to allow the intake of fluids orally for patient comfort, we chose to split the stomach by creating a tube of the great gastric curvature and perform a gastrostomy. The patient evolved well, with discharge on the 30th postoperative day. He received home parenteral nutrition for 1 year until he underwent a multivisceral transplant at a specialized service in Indiana, United States. The patient has 10 years of follow-up after transplantation, is fed by mouth, has no stoma, and has a good quality of life. The case illustrates the difficulty in managing desmoid fibromatosis of the mesentery and, at the same time, the evolution of surgery in the area of transplants, which makes it possible to offer survival and quality of life in extreme situations
Mesentery desmoid fibromatosis is part of the list of differential diagnoses of retroperitoneal masses and should be remembered. The diagnosis must be confirmed ideally by image-guided biopsy.
Retroperitoneal Fibrosis
Retroperitoneal fibrosis, also known as “Ormond’s disease,” “fibrous periureteritis,” “plasma periureteritis,” “chronic periureteritis,” “sclerosing retroperitoneal granuloma,” and “fibrous retroperitonitis,” encompasses a series of diseases characterized by the presence of fibrous-inflammatory tissue that usually surrounds the abdominal aorta and the iliac arteries, extending into the retroperitoneum, involving neighboring structures and enveloping the ureters. In general, it is an idiopathic manifestation; however, it can be related to the use of drugs, malignant neoplasms, infections, and previous surgeries [134].
The pathological findings of idiopathic and secondary retroperitoneal fibrosis forms are indistinguishable. Idiopathic disease seems to be related to a local inflammatory reaction to antigens in abdominal aortic arteriosclerosis plaques; however, constitutional symptoms, high levels of acute phase proteins, the association with other autoimmune conditions, and manifestation in other organs suggest that retroperitoneal fibrosis is a manifestation of systemic autoimmune and/or inflammatory disease. For this reason, clinical treatments are generally recommended as the use of steroids, immunosuppressive agents, and tamoxifen. The patient generally appears in good clinical condition; however, there is a risk of renal failure secondary to ureteral involvement [134].
The idiopathic form is an immune-mediated disease that can be isolated, associated with autoimmune diseases or related to immunoglobulin G4 disease. Although there are no standardized classification criteria, idiopathic retroperitoneal fibrosis is part of the spectrum of chronic peri aortitis, which includes inflammatory aneurysms of the abdominal aorta and retroperitoneal fibrosis. In one third of the cases, the perivascular tissue is not limited to the abdominal aorta and the iliac arteries, but also involves the thoracic aorta and the origin of the epi-aortic arteries (diffuse peri aortitis) [135, 136].
Although retroperitoneal fibrosis may belong to the spectrum of IgG4-related disease, there appears to be no major difference between IgG4-related and unrelated retroperitoneal fibrosis, except for a higher frequency of extra-retroperitoneal lesions in the IgG4-related disease subset [137]. The inflammatory infiltrate is represented by B and T lymphocytes, macrophages, and plasma cells and can be diffused or arranged in pseudo-nodular perivascular aggregates.
The clinical features of idiopathic or secondary retroperitoneal fibrosis are nonspecific and the diagnosis is generally not considered until there is significant involvement of retroperitoneal organs, most often the kidneys. The most common symptom is lower back and abdominal pain. Malaise, anorexia, weight loss, fever, nausea, and vomiting can be reported, as well as testicular pain, varicocele, and hydrocele secondary to compression of retroperitoneal vessels [138, 139]. There may be complaints of lameness related to arterial involvement of the lower extremities or symptoms of mesenteric ischemia due to compression of the mesenteric arteries. When the thoracic aorta and/or epi-aortic arteries are involved, patients may experience dry cough, hoarseness secondary to recurrent laryngeal nerve palsy, and claudication of the upper limbs. Stenosis of the arteries is rare, but venous compression (mainly of the inferior vena cava) is common and can cause edema in the lower limbs through a combination of venous and lymphatic compression, leading to the appearance of collateral circulation. Despite vascular compression, inferior vena cava syndrome, deep vein thrombosis, and pulmonary embolism are rare events [134, 140].
Although rare, retroperitoneal fibrosis should be included in the list of diagnoses of retroperitoneal masses. Due to the inflammatory nature of the lesion, treatment is done with nonsteroidal anti-inflammatory agents. As mentioned, there is a risk of different associated vascular problems.
Erdheim-Chester Disease
Erdheim-Chester disease is a rare systemic histiocytic disorder of non-Langerhans cells, most common in men (3:1), in the age group between 50 and 60 years old [141, 142]. It manifests most commonly through multifocal sclerotic lesions of long bones, with or without histiocytic infiltration of extra-osseous tissues. It is caused by the clonal proliferation of myeloid progenitor cells, as demonstrated by the detection of the characteristic BRAF V600E mutation in subsets of dendritic cells, mature monocytes, compromised myeloid progenitors, and CD34 + cells [142].
Infiltration of perirenal tissues as a “shell” is common and can cause hydronephrosis due to ureteral involvement. This aspect should alert to the possibility of the syndrome among the differential diagnoses of retroperitoneal masses. Different sites may be involved, including the retroperitoneum (60%), with long bones being the most common sites (95%). Other sites of involvement are maxillary sinus, large vessels, heart, lungs, central nervous system, skin, pituitary gland, and orbit (Fig. 7.30) [143]. The circumferential lining of the soft tissues of the thoracic and abdominal aorta (“coated aorta”) is visualized by CT in two thirds of the patients and is often confused with primary or secondary retroperitoneal fibrosis, sclerosing mesenteritis, and other retroperitoneal neoplasms, including lymphomas and germ cell tumors [144].
A 50-year-old asymptomatic female patient with history of ischemic stroke at a young age. A retroperitoneal mass was found during check-up exams. (a) Note in CT scan the Infiltration of perirenal tissues as a “shell” and bilateral mild hydronephrosis due to ureteral involvement. (b) Additional images show the involvement of other organs associated with the disease. Brain MRI shows multiple intra-axial, oval, and linear lesions with distribution along the perivascular encephalic spaces; PET-CT shows an increase in metabolic expression in retroperitoneal tissues, especially in peri and pararenal spaces, and peritoneal densification in parietocolic gutters, greater omentum, and pelvic excavation; in bones, gross, irregular, heterogeneous, diffuse spinal cord sclerosis is observed in the femurs and tibiae. The immunohistochemical profile observed in the biopsy in correlation with the histological aspects was consistent with fibrosis associated with lymphoplasmocytic infiltrate and histiocytes. In the molecular analysis, a mutation was observed in codon 600 c.1799T> A (V600E) of the BRAF gene
3.4 Group 4. Retroperitoneal Lymph Node Masses
The location of lymphadenopathy can be useful in identifying the etiology of different diseases that are associated with lymph node involvement [145]. When the location includes the retroperitoneal lymph node base, lymphomas and Castleman’s disease must be remembered. Another cause is the secondary involvement by metastases of primary tumors of the digestive and genitourinary tracts, with emphasis on testicular tumors. Among the infectious causes, bacterial and fungal infections are the main ones. Among inflammatory and autoimmune diseases, one possibility is the Rosai-Dorfman disease.
3.4.1 Neoplastic Etiology
The finding of a retroperitoneal lymph node mass in association with the presence of lymphadenopathy in superficial chains (supraclavicular, axillae, and inguinal regions) favors the diagnosis of lymphoproliferative or infectious diseases. However, the absence of peripheral lymphadenopathy does not exclude these diagnoses, because, although more rarely, in both situations the manifestation can be exclusively in the retroperitoneum. When there is primary involvement of retroperitoneal lymph nodes, the diagnosis of lymphoma must be remembered. For this reason, as previously exposed, it is important to actively inquire about the presence of “B symptoms” (fever, night sweats, weight loss). The presence of hepato-splenomegaly should also be investigated, as it contributes to the hypothesis of lymphoproliferative, infectious, and autoimmune diseases, although it does not allow the differentiation between them.
Non-Hodgkin’s Lymphoma
Non-Hodgkin’s lymphoma (NHL) consists of a diverse group of malignant neoplasms derived from B cell progenitors (bone marrow-derived), T cell progenitors (thymus-derived), mature B cells (B cells or plasma cells), mature T cells (cytotoxic T cells, helper T cells, or T regulatory cells) or, more rarely, natural killer cells. The clinical presentation of NHL is variable, depending on the subtype and areas affected.
Aggressive forms of NHL account for 50%. They present in an acute or subacute form with a rapidly growing mass, B symptoms, and high levels of lactic dehydrogenase (LDH) and uric acid. Five percent are classified as very aggressive. The rest are indolent lymphomas, with slow-growing lymphadenopathy, hepatomegaly, splenomegaly, or cytopenia at blood count [146, 147]. Some aspects should be valued in the suspicion of NHL: personal or family history of lymphoma or other previous hematopoietic malignancy, history of radiation or chemotherapy, use of immunosuppressive agents, organ transplantation, and other associated diseases. Some infectious agents may also be related: human immunodeficiency virus (HIV), human T lymphotropic virus type I (HTLV-I), Epstein-Barr virus (EBV), hepatitis B virus, hepatitis C virus, Borrelia burgdorferi, and Chlamydia psittaci [148,149,150,151,152]. Other associated disorders include autoimmune diseases: lupus erythematosus, rheumatoid arthritis, Sjogren’s syndrome, and Hashimoto’s thyroiditis [153]. Some rarer conditions are also associated: immunodeficiency disorders, mixed cryoglobulinemia, multicentric Castleman’s disease, inflammatory gastrointestinal diseases (gastrointestinal nodular lymphoid hyperplasia, chronic gastritis associated with Helicobacter pylori, and celiac disease), and also obesity [154].
Up to 40% of patients with NHL have B symptoms, more common in patients with aggressive and highly aggressive histology (47%), especially when there is hepatic and extra nodal involvement. In indolent lymphomas, less than 25% of patients have B symptoms, which, when present, are usually associated with advanced stage and large lymph node masses [155]. In general, retroperitoneal lymphadenomegaly does not lead to vascular obstruction or compression to the point of impairing blood flow, an aspect that may contribute to the formulation of the diagnostic hypothesis.
More than two thirds of patients with NHL have peripheral lymphadenopathy, usually painless. Both in NHL and in infectious conditions, the presence of lymphocytosis and lymphadenopathy is observed. For this reason, the initial assessment should focus on excluding bacterial (pertussis, tuberculosis), viral (infectious mononucleosis, cytomegalovirus, and human immunodeficiency virus), and parasitic (toxoplasmosis) etiologies.
The involvement of retroperitoneal and mesenteric lymph nodes is common in most histological subtypes of NHL; however, in general it does not produce symptoms. Biopsy is necessary and should be done before starting steroid treatment. The choice of the biopsy site depends on clinical features and location of the involved lymph nodes. Increased lymph nodes (>2 cm) undergoing progressive increase should preferably be chosen. The enlarged peripheral lymph nodes are generally preferred because of their easy access. When choosing peripheral lymph nodes, the diagnostic rates vary according to the lymph node base: supraclavicular (75–90%), cervical and axillary (60–70%), and inguinal (30–40%) [156]. In general, a tissue biopsy is necessary for the complete histopathological evaluation, preferably of an intact lymph node. Fine needle aspiration biopsies that suggest the presence of lymphoma, in most cases, should be followed by a definitive tissue biopsy [157]. In patients with exclusively retroperitoneal disease, image-guided thick needle or laparoscopic biopsies can provide sufficient tissue for diagnosis [158, 159]. The PET/CT can help in selecting a biopsy site (Fig. 7.31) [160].
A 46-year-old female patient, complaining of abdominal pain for 3 months. CT shows a large volume abdominal mass, characterized by multiple confluent mesenteric lesions that may represent lymph node clusters, involving the superior mesenteric vein and its branches and the duodenal arch, with wide contact with the head of the pancreas. Image-guided biopsy revealed the diagnosis of diffuse large B-cell NHL. Staging PET-CT confirms tomography findings (SUV max: 14.8), with additional finding of multiple focal areas in the axial and appendicular skeleton, compatible with lymphoproliferative disease in activity
Hodgkin’s Lymphoma
Hodgkin’s lymphomas (HLs) are lymphoid neoplasms in which the malignant Hodgkin/Reed-Sternberg cells are mixed with a heterogeneous population of nonneoplastic inflammatory cells. They are divided into two main categories, classic and predominant in nodular lymphocytes, based on morphology and immunophenotype. The classic form comprises 90% of Hodgkin’s lymphomas, generally progressing slowly, and is subdivided into nodular sclerosis, mixed cellularity, rich in lymphocytes, and with lymphocyte depletion forms [161].
“B” symptoms are present in 40% of HL cases. Most patients present with asymptomatic lymphadenopathy; however, constitutional symptoms, fatigue, and itching can be referred. Retroperitoneal lymphadenopathy can cause abdominal discomfort or pain. Some patients have increased abdominal volume secondary to splenomegaly, hepatomegaly and, more rarely, ascites. Extensive intra-abdominal disease can cause ureteral obstruction and compression of the renal veins, but gastrointestinal tract involvement is rare. Common affected lymph node bases are cervical and supraclavicular (60–80%), axillary (30%), and inguinal (10%). Although not detectable on physical examination, mediastinal and retroperitoneal lymph nodes are involved in 50% and 30% of patients, respectively; however, isolated infra-diaphragmatic lymphadenopathy is uncommon (<10%). Thus, finding isolated retroperitoneal lymph node mass, the diagnosis of Hodgkin’s Lymphoma is less likely. When peripheral lymphadenopathy is not identified, CT and PET-CT can identify a suspicious site to guide the biopsy [162].
Castleman’s Disease
Castleman’s disease (angiofollicular lymph node hyperplasia) includes a heterogeneous group of lymphoproliferative disorders. The histopathological characteristics of lymph nodes in patients with Castleman’s disease are believed to be exacerbated reactive changes in response to normal antigenic stimuli or represent a low-grade neoplastic process.
Castleman’s disease (CD) is classified based on the number of regions of enlarged lymph nodes and the presence or absence of infection with human herpes virus 8 (HHV-8). The cases must be classified because clinical characteristics and treatments are different. The unicentric form (UCD – 75%) involves one or more enlarged lymph nodes in a single region of the body. The multicentric form (MCD – 25%) involves several lymph nodes chains. Castleman’s disease can also be associated with other cancers, including non-Hodgkin’s lymphoma, Hodgkin’s lymphoma, and POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, myeloma protein, and skin changes) [163].
Although UCD can occur at any age, it is usually a disease of young adults (30–35 years old) with a slightly increased incidence in women. It can affect any lymph node chain. The sites referenced are abdomen/retroperitoneum (30–40%; isolated retroperitoneum 14%), neck (20–23%), chest/mediastinum (16–24%; 70% in some series), inguinal (9%), pulmonary hilum (7%), and armpit (7%). The presentation in the form of retroperitoneal lymph node mass may occur in young adults, being diagnosed incidentally or in the investigation of general symptoms such as fever, growth failure, and weight loss. The duration of symptoms and lymph adenomegaly can vary from weeks to months [163, 164].
Although it is a rare condition, the diagnosis of hyaline vascular UCD is part of the differential diagnosis of solid and heterogeneous mass in the retroperitoneum. Lesions are typically confined to the lymph node tissue. Laboratory studies are generally normal, but there may be an increase in C-reactive protein and erythrocyte sedimentation rate, as well anemia, thrombocytopenia, hypoalbuminemia, renal dysfunction, and polyclonal hypergammaglobulinemia. Complete surgical resection of the lymph nodes involved is considered the standard approach for the UCD, almost always curative. In unresectable disease, embolization strategies and the use of rituximab can convert to a resectable condition.
In MCD, the etiology is not well known. It seems to be related to autoimmune, autoinflammatory, neoplastic, and infectious mechanisms. IL-6 is a multifunctional cytokine involved in a wide range of activities, including plasmacytosis, hypergammaglobulinemia, thrombocytosis, production of proteins in the acute phase by the liver, and activation of macrophages and T cells. Apparently, IL-6 is related to symptomatology, histopathology, and pathogenesis in part of the patients [165]. MCD patients have lymphadenopathy in several lymph node chains, including the retroperitoneum [166]. The disease development course is variable. Most patients have fever and nonspecific symptoms suggestive of inflammatory disease, including night sweats, weight loss, weakness, and fatigue. Other signs and symptoms include hepatosplenomegaly, cytopenia, organ dysfunction, and skin manifestations (rashes, pemphigus, hemangioma), in addition to loss of appetite, nausea, vomiting, severe abdominal pain, fatigue, and peripheral neuropathy. Neuropathy can range from mild sensory neuropathy to severe sensory and motor neuropathy, associated with POEMS syndrome [167,168,169].
A diagnosis of idiopathic CMD/HHV-8 (iMCD) should be suspected in patients with peripheral lymphadenopathy, constitutional symptoms, and elevated C-reactive protein. PET-CT demonstrate several regions of enlarged lymph nodes, usually with a relatively low SUV. The established diagnostic criteria require characteristic pathological lymph node biopsy, enlargement of multiple lymph node chains, and multiple clinical and laboratory abnormalities, besides exclusion of infectious disorders, malignancies, and autoimmune diseases [168]. If available, treatment with anti-IL-6 monoclonal antibody has been recommended, with or without association with corticosteroids. Surgery has no role in the treatment of CDM [163].
From a microscopic point of view, Castleman’s disease can be classified according to the type of lymphoid tissue. The microscopic subtypes are divided into (1) hyaline-vascular type (most common), tends to be localized and is rarely multicentric; (2) plasmocytic type, more likely to be multicentric and more rarely located; and (3) mixed type, the combination of both (rare) (Fig. 7.32).
(a) Example of the hyaline-vascular type: vascularized nodular lesion superior to the head of the pancreas and close to the hepatic hilum, with enhancement in the arterial phase, with calcifications inside. In the present case, the lesion has contact with the portal vein and is associated with some adjacent arterial collaterals, probably related to its irrigation. (b) Example of the plasmocytic type: An infiltrative and vascularized lesion next to the medial aspect of the left kidney, involving the collecting structures, with homogeneous contrast enhancement observed on CT. The liver lesion is a hemangioma. (Courtesy of Hilton Leão Filho, radiologist)
Lymph Node Metastases
When the image is suggestive of retroperitoneal lymph node involvement, the hypotheses must include the possibility of secondary involvement due to metastasis of different primary tumors. Male patients, especially at a young age, should be questioned about testicular changes, history of cryptorchidism, fertility, and sperm test results. Even with a normal testicular examination, testicular ultrasound should be performed. Testicular germ neoplasms occur between 15 and 35 years and after 60 years. It is not uncommon to find a large retroperitoneal mass without evidence of a primary testicular tumor (Fig. 7.33a). For this reason, in addition to scrotum ultrasound, it is imperative to request the tumor markers AFP and HCG-ß, in addition to LDH measurement. Once the presence of a testicular lesion is verified, radical orchiectomy will allow the definitive diagnosis, without intervention on the retroperitoneal mass. When there is no testicular alteration in the presence of increased markers, a thick needle image-guided biopsy of the retroperitoneal mass may be necessary.
(a) A 32-year-old male patient, complaining of increased abdominal volume and weight loss. Absence of peripheral lymphadenomegaly. Absence of clinical detectable changes in testicular palpation. Ultrasound of testicles and tumor markers was requested as part of the initial investigation, with the finding of a 10 mm nodule in the left testis and a slight increase in HCG-ß. Radical orchiectomy was performed, and the pathological analysis showed a pure seminoma. The patient was treated with chemotherapy with complete response, without intervention on the retroperitoneal mass. (b) A 70-year-old female patient complaining of vaginal bleeding and pelvic pain. Vaginal touch showed a tumor on the uterine cervix. Note on CT the presence of secondary retroperitoneal lymphadenomegaly from a primary squamous cell carcinoma of the uterine cervix. Double J catheter was placed on the right kidney due to uretero-hydronephrosis
In women with retroperitoneal lymphadenomegaly, genital tract neoplasms should be investigated, starting with the interrogation of gynecological complaints (bleeding, discharge, and dyspareunia), use of medications (contraceptives and hormone replacement), and family history of neoplasms. The gynecological examination must be complete and include a Pap smear. If some abnormality is detected, the investigation follows with complementary exams (Fig. 7.33b).
In general, data from clinical history, physical examination, and imaging aspects direct us to the suspicion of retroperitoneal lymph node metastases secondary to tumors of the digestive and genitourinary tract, which should be investigated. Metastases from solid tumors from other sites may also occur, although are uncommon to present as a retroperitoneal mass simulating a primary tumor of the retroperitoneal space.
3.4.2 Nonneoplastic Etiology (Autoimmune, Inflammatory, Infectious)
Autoimmune, inflammatory, and infectious diseases that lead to retroperitoneal lymphadenomegaly are included in the list of differential diagnoses and should be considered in the investigation. Active questioning about past infections, reports of infectious conditions in the social environment, place of last trips, use of drugs and medications, in addition to the possibility of immunosuppression, are aspects to be questioned.
Rosai-Dorfman Disease
Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) is a rare non-Langerhans cell histiocytosis [170]. It often presents with marked cervical adenopathy, but other lymph node sites, including the retroperitoneum, may be involved. Patients usually have fever when there is massive lymphadenopathy. Laboratory evaluations show leukocytosis, polyclonal hypergammaglobulinemia, hypochromic or normocytic anemia, and elevated ESR.
Treatment is variable, depending on the involvement of the lymph node chain. Slow spontaneous resolution (months to years) may occur [171]. The most common sites of extra-nodal involvement are skin, upper respiratory tract, and bone; however, other sites may also be affected: genitourinary tract, lower respiratory tract, oral cavity, and soft tissues. The prognosis is correlated with the number of lymph node bases involved and the number of extra-nodal sites affected [170].
Although retroperitoneal involvement is uncommon, the diagnosis of Rosai-Dorfman disease is among the entities capable of generating retroperitoneal masses and should be remembered [172, 173].
IgG4-Related Disease
The disease related to immunoglobulin G4 (IgG4-RD) is an immune-mediated fibroinflammatory condition that affects multiple organs, with different forms of presentation: autoimmune pancreatitis, sclerosing cholangitis, enlarged salivary glands or sclerosing sialadenitis, orbital disease, and retroperitoneal fibrosis. It is often accompanied by chronic peri-aortitis and ureteral involvement, with consequent hydronephrosis and kidney damage [174, 175].
IgG4-RD is characterized by dense lymphoplasmacytic infiltration, with a predominance of IgG4-positive plasma cells, fibrosis, obliterative phlebitis, and an increased number of eosinophils [176]. In histology, fibrosis associated with IgG4-RD has a “storiform” pattern, characterized by the arrangement of fibroblasts and inflammatory cells in a “wagon wheel” shape [177]. Serum IgG4 levels are elevated in two thirds of patients, but all cases have typical histopathological changes in the tissue [178].
Lymphadenopathy is usually seen with other clinical or laboratory manifestations, although it can be an isolated manifestation [179]. Lymph nodes rarely undergo storiform differentiation, which makes diagnosis from biopsies difficult. In addition, a large number of plasma IgG4-positive cells can be found in several diseases, the specificity of this finding being low. Different histological patterns with an abundance of IgG4-positive cells are possible, most with eosinophil infiltration, which also contributes to confusing the diagnoses with other entities as Castleman’s multicentric disease, follicular hyperplasia, interfollicular expansion, progressive transformation of the germinal center, and nodal inflammatory aspect, similar to a pseudotumor [177]. In this sense, retroperitoneal fibrosis is one of the most common subsets of IgG4-positive and some series suggest that IgG4-RD is responsible for most cases of retroperitoneal fibrosis previously considered “idiopathic” [180, 181]. When presenting as a retroperitoneal tumor, the difficulty of defining the diagnosis sometimes leads to surgical intervention and the definitive diagnostic conclusion is postoperative, which justifies the existence of patients operated on without having received previous medical treatment (Fig. 7.34).
A 62-year-old diabetic male with renal function deficit. In a routine consultation, an abdominal mass was palpated on the left flank. The CT shows a homogeneous infrarenal solid mass. Thick needle image-guided biopsy was inconclusive. The patient was taken to surgery with a finding of a retroperitoneal mass in contact with Gerotta’s fascia, adhered to retroperitoneal muscle planes, with no signs of macroscopic invasion of the kidney. The freezing test was inconclusive for malignancy. Due to the deficit in renal function and the absence of conclusive malignancy, complete marginal resection with renal preservation was performed. The definitive diagnosis was compatible to an IgG4-related inflammatory pseudotumor, with positive immunohistochemistry and increased serum dosage
The presence of IgG4-RD appears to be associated with an increased risk of malignancy; however, these data need to be confirmed. On the other hand, a history of malignancy appears to be associated with the subsequent development of IgG4-RD [182, 183].
Initial therapy with glucocorticoids or with an immunosuppressive agent and/or biological agent (rituximab) is necessary in most patients to achieve disease remission [184]. Many patients follow an indolent course and respond well to treatment, but a significant proportion can have high morbidity or fatal complications, such as peri-aortitis, severe retroperitoneal fibrosis, or pachymeningitis. Vascular surgical interventions, including stenting to relieve mechanical obstruction as well as other vascular procedures, may be indicated in selected patients.
Tuberculosis
Extrapulmonary tuberculosis can simulate different diseases, including retroperitoneal lymph node mass of different etiologies. The manifestations are usually subacute or chronic, with complaints of fever, night sweats, and organic dysfunction associated with anorexia and weight loss. Hepatomegaly and splenomegaly may also be present.
Up to 20% of tuberculosis cases are extrapulmonary. The most common extra-pulmonary sites are lymph nodes, bones, joints, liver, central nervous system, and adrenal glands [185]. The prevalence of tuberculosis increases in areas of less favored socioeconomic conditions and malnutrition. Any lymph node base can be involved; however, the hilar and paratracheal lymph nodes are the most commonly affected. In the retroperitoneal space, it may present as lymphadenopathy, involvement of retroperitoneal organs or, more rarely, as retroperitoneal fibrosis. As in other entities, in the suspicion of retroperitoneal tuberculosis, the search for peripheral lymph nodes must precede the indication for biopsy of the retroperitoneal mass.
Isolated peripheral tuberculous lymphadenopathy is usually caused by reactivation of the disease from hematogenous dissemination that occurred during primary infection a few years earlier. Abdominal tuberculous lymphadenopathy can occur due to ingestion of sputum or milk infected with Mycobacterium tuberculosis. Although most cases of tuberculous lymphadenitis occur in the setting of reactivation of latent infection, miliary spread with prominent involvement of the lymph nodes in the setting of primary infection can also occur [186]. In countries where tuberculosis is endemic, extrapulmonary tuberculosis occurs in up to 60% of HIV-infected patients, often accompanied by pulmonary involvement [187]. Most extrapulmonary cases, including tuberculous lymphadenitis, occur among HIV patients with CD4 counts <300 cells/μL (usually below 100 cells/μL) [188].
Clinical manifestations depend on the location of the lymphadenopathy and the patient’s immune status [189]. The most common presentation in young adults is chronic nonisolated lymphadenopathy. Fever can be present in 20–50% in patients not infected with HIV and 60–80% in infected patients [190]. When there is peripheral involvement, the physical examination reveals firm lymph nodes or lymph node clusters attached to adjacent structures, with hardened overlying skin. Other possibilities of findings include fluctuation, drainage, or nodular erythema. Peritoneal tuberculous lymphadenopathy usually involves lymph nodes in the periportal, peripancreatic, and mesenteric chains [191].
In the peritoneum and retroperitoneum, the involvement is predominantly from mesenteric, anterior pararenal, superior para-aortic, and omentum lymph nodes. The anatomical distribution and specific patterns of lymphadenopathy seen on CT can be useful in differentiating between tuberculosis and lymphomas [192].
4 Image Diagnostics
The correct interpretation of images of retroperitoneal tumors, in addition to the experience of the radiologist, depends on complete clinical information, which is fundamental for the formulation of the diagnostic hypothesis and to guide the choice of the appropriate imaging method. CT of the abdomen and pelvis, in line with the story and physical examination, guides the first steps of radiological investigation. Chest and mediastinal CT, whose presence or absence of additional findings helps in making the diagnostic hypothesis, should also be performed in the beginning of the investigation. Depending on the clinical suspicion, other imaging tests and specific laboratory tests may be necessary.
According to the division proposed in our chapter, our suggestion is to start trying to classify the type of retroperitoneal finding in one of the four groups presented: (1) intraperitoneal lesions that simulate retroperitoneal tumors; (2) primary tumors of retroperitoneal organs; (3) primary tumors of the retroperitoneal space; and (4) retroperitoneal lymph node masses.
4.1 First Step: Differentiation Between Retroperitoneal and Intraperitoneal Lesions
Distortion of the anatomy by large masses can make it difficult to distinguish between true retroperitoneal tumors and intraperitoneal lesions [1]. The displacement of retroperitoneal organs suggests primarily retroperitoneal tumor. On the other hand, the wide mobility on physical examination, as well as the change of location in the image with the change of position, is the aspect that favors the diagnosis of intraperitoneal lesion (Fig. 7.35). A simple test that can help in the investigation is to ask the radiologist to acquire complementary images in different positions.
Case 1 – Gastric GIST: in large tumors primary of intraperitoneal organs, there may be some difficulty in the differential diagnosis to retroperitoneal primary tumors. In the case presented, upper gastrointestinal endoscopy with biopsy revealed the diagnosis of GIST primary of the stomach. Note the aspect of a heterogeneous lesion with lobulated contours. Case 2 – Well-differentiated liposarcoma primary of the large omentum. This tumor was mobile on physical examination. Note that the retroperitoneal organs were not involved by the lesion. Case 3 – Primary dedifferentiated liposarcoma of the retroperitoneal space. Note the well-differentiated component of the lesion, with a lipomatous aspect, and the undifferentiated component, represented by a more solid area. Observe the displacement and involvement of the left kidney by the lesion, favoring the diagnosis of primary lesion of the retroperitoneal space
When the lesion is found to be intraperitoneal, the diagnoses will generally be considered among the following possibilities: GIST, EGIST, visceral sarcomas, and adnexal masses. It is important to remember that large primary tumors of intraperitoneal organs and visceral metastases from different primary tumors can generate intraperitoneal masses; however, in general, the primary site is identified. On CT, GISTs and EGISTs appear as heterogeneous lobulated tumors, with the possibility of infiltration of mesenteric fat and low probability of lymph node involvement. Tumors with low metastatic potential tend to be more homogeneous and have an endoluminal growth pattern [21, 193]. Visceral sarcomas usually present as masses with varying degrees of necrosis and heterogeneous contrast enhancement. The presence of secondary pulmonary lesions favors the diagnosis of visceral sarcoma [31]. In women, the hypothesis of large-volume adnexal masses simulating retroperitoneal tumors should be considered. The presence of multilocular cystic lesions, solid areas, bilateral lesions, ascites, and peritoneal metastases should alert to the possibility of large gynecological tumors. The adnexal masses can be either primary of the ovary or metastatic, such as Krukenberg tumors. Thus, previous history of tumors of the digestive system must be considered [37].
4.2 Second Step: Differentiation Between Retroperitoneal Tumors and Lymph Node Masses
Excluding the diagnosis of intraperitoneal lesions, the next step may be to differentiate between retroperitoneal tumors and lymph node masses. The presence of peripheral lymphadenopathy favors the hypothesis that the retroperitoneal lesion corresponds to a lymph node mass. In the absence of peripheral lymphadenomegaly, the location of the lesion in the retroperitoneum must be considered. Thus, when the location is not central, the tendency will be to direct the reasoning to the hypothesis of primary tumors of retroperitoneal organs or primary tumors of the retroperitoneal space. The greatest difficulty in distinguishing occurs in situations of large masses involving large vessels, when both primary retroperitoneal lesions and lymph node masses can occur (Fig. 7.36). In this condition, clinical aspects, specific imaging characteristics, and other complementary exams must be done. If the hypothesis is compatible with a lymph node mass, the next step will be the differentiation between the diseases that develop with retroperitoneal lymph node masses, which is our fifth step, discussed later. Excluding the diagnosis of lymph node mass, our suggestion is to progress in the distinction between primary tumors of retroperitoneal organs and primary tumors of the retroperitoneal space.
Case 1 – Diffuse non-Hodgkin’s lymphoma of large B cells. The mass represents a lymph node conglomerate. When all CT sections are observed in detail, the presence of lymphadenomegaly is also noted in the latero-cava, intercavo-aortic, and later aortic chains. Case 2 – Dedifferentiated liposarcoma. Note on the CT the aspect of an expansive solid lesion, with a hypervascularized component and areas of liquefaction/necrosis, with an infiltrative aspect, occupying the epiploic retro cavity, with densification of adjacent fatty planes. Despite the dimensions and aspect of a high-grade lesion, there is no associated lymphadenomegaly
4.3 Third Step: Differentiation Between Primary Tumors of Retroperitoneal Organs and Primary Tumors of the Retroperitoneal Space
Excluding the hypotheses of intraperitoneal tumor and lymph node mass, the next step is to try to differentiate whether the origin occurs from a retroperitoneal organ (duodenum, pancreas, adrenal gland, kidney, and colon segments) or corresponds to a primary tumor of the retroperitoneal space. The determination of whether a lesion arises from a retroperitoneal organ or from tissues in the retroperitoneal space can be suggested by the relationship between the lesion and adjacent structures. Some signs help with image evaluation: “beak sign,” “embedded organ sign,” “crescent shape sign,” “phantom organ sign,” and the “prominent feeding artery sign.” As explained by Shaaban et al., the “beak sign” relates to the shape of a solid organ at the edge of its interface with an adjacent mass. A sharp beak shape implies that the mass arises from the adjacent organ. If the mass is incorporated and completely surrounded by the parenchyma of an organ, it is assumed that it is primary of that organ (the “embedded organ sign”), while organs with rounded edges suggest displacement by the mass. If the mass displaces the organ, but does not originate from it, the organ can take the form of a “crescent moon” (“crescent shape”). The “phantom organ sign” occurs when a large mass arises from a small organ, so that the original organ is obliterated and not seen. Hypervascular retroperitoneal masses can have large nourishing arteries that help in the identification of the organ of origin (the “prominent feeding artery sign”) (Fig. 7.37) [194].
(a) The “beak sign” reports to the shape of a solid organ at the edge of its interface with an adjacent mass. Note the sign of the acute beak in the lower portion of the lesion, close to the right kidney, suggesting that the origin of the lesion is in the adjacent organ, I this case, a primary GIST of the duodenum. (b) Two examples of “embedded organ sign,” a neuroendocrine tumor of the right colon and a renal clear cells carcinoma, where the mass is incorporated and surrounded by the parenchyma of an organ, what suggests that it is primary of the organ. (c, d) If the mass displaces the organ, but does not originate from it, the organ can take the form of a “crescent moon” (“crescent shape”). Note this aspect in the relation of the mass with the lower border of the liver in (c) (retroperitoneal liposarcoma) and in the relationship of the mass with the right kidney and the aorta in (d) (metastasis of ovarian teratoma). (e) The “phantom organ sign” occurs when a large mass arises from a small organ, so that the original organ is obliterated and not seen, as in this example of a borderline tumor of the right ovary (the ovary is not seen). (f) Note the large nourishing arteries that help in the identification of the origin (the “prominent feeding artery sign”). In the figure, the prominent nourishing arteries are branches of right iliac arteries, suggesting a retroperitoneal origin (retroperitoneal solitary fibrous tumor)
The assessment of the presence of fat in a retroperitoneal lesion is one of the useful “tools” for the differential diagnosis. Fat is easily recognized in imaging studies, with the consideration that while CT is limited in demonstrating small amounts of fat, MRI is more sensitive in detecting microscopic fat. Among primary lesions of retroperitoneal organs, adenomas are the most common adrenal tumors that contain microscopic fat, while myelolipomas are the most common adrenal masses that contain macroscopic fat. Other adrenal masses, such as pheochromocytoma and adrenocortical carcinoma, rarely contain fat. Among renal masses, angiomyolipomas are the ones that most commonly contain fat. Changes in renal cortex, prominent vessels, and well-defined contours favor the diagnosis of angiomyolipoma [195].
Among the diagnoses of pancreatic lesions, the solitary fibrous tumor of the pancreas is predominantly solid, without fat content, may contain calcifications, and is enhanced in the arterial phase. Pancreatoblastoma is predominantly cystic, may contain calcifications, and has contrast washout. Acinar cell carcinoma is generally solid, with calcifications, circumscribed and hypovascular. Hemangiomas are cystic, may contain calcifications, develop areas of hemorrhage, and are enhanced in the arterial phase. Lymphangiomas are generally polycystic, with septa that are highlighted. Lymphomas are predominantly solid and cause diffuse involvement, without ductal dilation, and generally present associated lymph node enlargement. Pancreatic dermoid cysts can contain solid areas, calcifications, fatty content, and have areas of hemorrhage. Other tumors such as leiomyosarcomas, lipomas, schwannomas, and pancreatic hamartomas can have variable image characteristics [44].
If a lesion of duodenal origin is suspected, upper gastrointestinal endoscopy and endoscopic ultrasound may help. In the face of larger masses, the diagnosis of primary GIST of the duodenum must be remembered. If primary lesions of the retroperitoneal segments of the ascending and descending colon are suspected, further colonoscopy investigation should be performed.
4.4 Fourth Step: Differentiation Between Primary Tumors of the Retroperitoneal Space
Excluding origin from retroperitoneal organs, we will move on to the most difficult moment of image interpretation, differentiating between primary solid tumors of the retroperitoneal space. Based on the frequency of appearance, an idea is to start from the hypothesis of retroperitoneal sarcoma and analyze specific characteristics that may allow confirmation or direct the reasoning towards other hypotheses.
Sarcomas usually appear on CT as masses that laterally displace hollow viscera and parenchymal organs. Most retroperitoneal sarcomas are liposarcomas (about 70%), so assessing the presence or absence of fat in the lesion is an additional step. If the fat component is not clearly the result of a retroperitoneal organ, the diagnosis of liposarcoma must be considered, remembering that the presence of septations, dense areas, and calcifications may suggest dedifferentiation or the sclerosing and inflammatory variants of liposarcomas [196].
Well-differentiated liposarcomas appear as well-defined lesions, predominantly containing fat. The appearance may be indistinguishable from the lipoma and, for this reason, any purely fatty retroperitoneal lesion should be considered a well-differentiated liposarcoma until the definitive pathological diagnosis. Areas of dedifferentiation occur within a well-differentiated liposarcoma and dedifferentiation is suggested by nonlipomatous focal nodular regions. The myxoid variant generally presents less attenuation than the adjacent muscle, with low signal intensity in T1-weighted images and high signal intensity in T2-weighted images. Most myxoid liposarcomas have enough fat to suggest a diagnosis of liposarcoma. It is common to see thick septa and irregular or nodular soft tissue components. Round cell and pleomorphic liposarcomas, on the other hand, exhibit attenuation of the soft tissue tumor and signal intensity with a minimum amount of fat [194].
The presence of fat from the well-differentiated component of liposarcomas is not always recognized and is sometimes interpreted as a normal part of retroperitoneal fat. Failure to recognize the presence of abnormal fat (the well-differentiated component of liposarcoma) can result in incomplete resections, leading the less experienced surgeon to remove the undifferentiated portion of the lesion and not remove the well-differentiated component. Several foci of dedifferentiation contained in a single lesion can also be misinterpreted as a multifocal disease and lead to a contraindication to surgery due to suspected sarcomatosis [196]. The following examples illustrate these points (Figs. 7.38, 7.39, and 7.40).
(a) Well-differentiated liposarcoma in its entirety, without areas of dedifferentiation. Radiologically, it can be difficult to differentiate by CT a well-differentiated liposarcoma from a lipoma. (b) Liposarcoma with lipomatous aspect (well-differentiated component) and dense solid area (differentiated component). The operation should be a “en bloc” resection, taking care not to consider the well-differentiated area as part of the retroperitoneal fatty tissue. (c) Dedifferentiated liposarcoma without lipogenic sarcomatous tissue, sometimes difficult to distinguish from undifferentiated pleomorphic sarcomas. (d) Dedifferentiated liposarcoma with an epithelioid/pleomorphic pattern and areas of calcification
CT scan shows a certain heterogeneity inside the lesion. In PET-CT, we observed intra-tumor variations in glycolytic metabolism, with variations in SUV values. This finding can guide the most appropriate place to perform image-guided biopsy. The definitive pathologic diagnosis was an inflammatory liposarcoma with de-differentiated areas
Although rare in the retroperitoneum, lipomas can also simulate liposarcomas. Lipoma is a benign mesenchymal tumor composed of mature adipose tissue. On CT, lipomas appear as well-defined homogeneous masses with attenuation of fat. Areas of soft tissue attenuation can be seen in the tumor and represent fatty necrosis, septa, or adjacent normal structures. Other benign conditions with a fat content should be remembered: retroperitoneal lipomatosis, lipodystrophy, retroperitoneal panniculitis (mesenteric panniculitis), retroperitoneal fat necrosis, encapsulated fat necrosis, and hibernoma [194].
Leiomyosarcomas correspond to the second most common histological type of sarcoma in the retroperitoneum. The presence of a large, heterogeneous, necrotic retroperitoneal mass, contiguous to a vessel, should resemble the diagnosis of primary leiomyosarcoma of retroperitoneal vessels, which most commonly originate in the inferior vena cava, below the level of the hepatic veins, but can also be primary from other veins, such as the renal and gonadal veins, among others. There is usually an exophytic component, which can make it difficult to differentiate from other retroperitoneal lesions that cause extrinsic vascular compression (Fig. 7.41). Specifically, for inferior vena cava leiomyosarcomas, the extent of involvement and the relationship with renal and retrohepatic veins should be described in image evaluation. Lumbar vessels and collateral veins in the retroperitoneum can be a significant source of intraoperative blood loss and must also be identified in preoperative CT. The compressive venous effects increase the risk of venous and pulmonary thromboembolism and preventive care should be taken [197].
The MRI shows two solid nodular lesions on the right flank, located anterior to the inferior vena cava, causing slight compression on it, in close relationship with the duodenum. The lesions exhibit a heterogeneous signal, enhanced by contrast and restriction to diffusion, the largest measuring 5.2 × 4.4 × 3.8 cm and the other measuring 3.2 × 2.6 cm. Note that it is difficult to determine whether the lesion is primary of the vena cava or causes compression on it; however, if the biopsy reveals the diagnosis of leiomyosarcoma, the chance of primary vascular lesion is high, as in the example
Excluding the diagnoses of liposarcoma and leiomyosarcoma, in some situations specific characteristics of the image may suggest other diagnoses. Some subtypes of sarcoma usually have cystic elements and can be confused with an abscess or even a hematoma.
The finding of a solid, circumscribed, vascularized tumor with prominent vessels must resemble the hypothesis of a solitary fibrous tumor. They usually have a homogeneous appearance, although cystic areas, calcifications, myxoid degeneration, or hemorrhage may be present, particularly in large tumors. They can be lobulated, with a tendency to displace rather than invading adjacent organs and tissues. The edges are rarely infiltrative and are commonly well-defined. In MRI, usually solitary fibrous tumors exhibit low signal intensity in T1 and variable signal in T2, with a significant increase in signal intensity after intravenous gadolinium administration. Hypocellular tumors generally show low signal in T2-weighted images, whereas hypercellular tumors, highly vascular edematous tumors, or those with necrosis or myxoid degenerative changes demonstrate high signal intensity [198]. In the image, the main differential diagnoses of solitary fibrous tumor are synovial sarcoma, de-differentiated liposarcoma, leiomyosarcoma, GIST and, when present in the mesentery, desmoid fibromatosis. In the pelvis, other tumors with a fibrous component constitute differential diagnoses: mesothelioma, Brenner’s ovarian tumor, fibroma or fibrotecoma, and uterine leiomyoma [199,200,201].
Among the other primary tumors of the retroperitoneal space, benign tumors of the peripheral nerve sheath are generally rounded and well defined, but malignant lesions may show invasion of local structures. The appearance of a tumor in dumbbells with expansion of the intervertebral foramen is suggestive of neurofibroma. Schwannomas and paragangliomas can be confused with sarcomas, particularly if located in the midline, adjacent to the aorta or vena cava. In CT, schwannomas and neurofibromas can be similar, appearing as hypodense lesions in relation to the muscle and enhance with contrast. In MRI with T1-weighted image, schwannomas appear with intermediate signal intensity, similar to muscle, and very clear signal in T2-weighted image, although cystic lesions have low signal intensity. Schwannomas grow uniformly and often have a border with low signal strength, consistent with the capsule. Fusiform appearance and “target” image can be seen in both schwannomas and neurofibromas. Sometimes it is possible to identify the nerve from which the lesion originates, usually positioned eccentrically. A heterogeneous appearance with cystic degeneration can also occur, characterizing the so-called “ancient schwannoma” [47].
Ganglioneuromas, because they originate from sympathetic ganglia, appear more commonly in the retroperitoneum in a central or paravertebral position or next to the adrenal glands, in addition to the intraspinal canal. They can be regular or irregular in shape, round, oval, lobular, or in dumbbells. In pre-contrast CT, they appear as a hypodense mass. With the increase in cellularity and the decrease in the mucous matrix, the density of the lesions may be slightly increased, but less than the density of the local musculature. The components of myxoid matrix delay the absorption of contrast, which is observed in later stages of image acquisition. In MRI, ganglioneuromas appear as hypodense lesions in T1-weighted image, hyperintense in heterogeneous form in T2-weighted image, and hyperintense in SPAIR (Spectral Attenuated Inversion Recovery). A “twisted” pattern (a low signal part is found in T2WI when the mass is shown in a high signal) can be a characteristic finding that corresponds to the microscopic interweaving patterns of Schwann cells and collagen fibers. Calcifications can be observed, as well as the “pseudopod sign,” formed by growth between adjacent tissues. Blood vessels are usually pushed and moved, with no signs of stenosis or invasion, although they can often be involved, which can make dissection laborious and risky [202].
Paragangliomas are part of the list of differential diagnoses. When paraganglioma is suspected, CT and MRI are the exams of choice for the first approach, with MRI being more sensitive and specific, especially in the detection of extra-adrenal disease. They are highly vascularized tumors, with high intracellular water content and frequent intra-tumor cystic areas, with high signal in the T2-weighted image and strong enhancement after the administration of intravenous contrast. In large tumors with hemorrhagic and/or necrotic areas (more common in malignant lesions), the signal intensity may be low in T2-weighted images [203]. With the diagnostic hypothesis of paraganglioma, a functional image is generally recommended. Whole-body studies allow for better assessment of extra-adrenal disease localization, as well as identification of multiple tumors and/or metastatic sites [204]. Scintigraphy with 123I-metaiodobenzylguanidine (MIBG) has high rates of sensitivity (83–100%) and specificity (95–100%), although in malignant paragangliomas sensitivity is lower since dopamine-secreting tumors generally do not capture MIBG. MIBG has chemical similarities to norepinephrine and is concentrated in the tissues of chromaffin cells through the human norepinephrine transporter factor (hNET), responsible for the capture of catecholamines [60]. So, in patients with negative MIBG, somatostatin analogs can be used. The somatostatin analogs marked with gallium-68 are also part of the research arsenal. PET 68Ga-DOTATOC (DOTA0-D-Phe1-Tyr3-octreotide) has high sensitivity, especially in the detection of small lesions or neoplasms with low density of somatostatin receptors. In addition, it allows a better identification of metastases located in the lungs and bones. Particularly in the detection of pheochromocytomas and malignant paragangliomas, PET 68Ga-DOTATOC is superior to PET-18F-FDG. Dopamine (DA) and dihydroxyphenylalanine (DOPA) are also transported by hNET to chromaffin cells and, therefore, can be used as radiolabels (PET 6- [18F] -fluoroDOPA). However, like MIBG, they have low sensitivity (70–88%) in detecting paragangliomas with mutations in the SDHB gene, where PET 18F-FDG is superior (sensitivity 97–100%), making it useful in identifying metastatic glucose-hungry lesions, especially if they are negative for MIBG [205].
Germ cell tumors in the retroperitoneal space are usually large in presentation. The involvement, displacement, and compression of the abdominal vessels are common. In the images, primary and metastatic malignant teratomas appear as enlarged soft tissue masses with foci of fat and calcifications. Clinical characteristics and tumor markers are fundamental for the diagnostic conclusion in the suspicion of germ cell tumors and must be considered in line with the aspects of the image.
Some specific image characteristics may suggest the diagnosis of retroperitoneal fibrosis. CT-evaluated retroperitoneal fibrosis exhibits attenuation numbers similar to those of the muscle. The mass is usually confluent, involving (but not dislocating) the aorta, often surrounding and compressing the inferior vena cava and causing medial deviation of the ureters. Lymphadenopathy located adjacent to the mass can be observed. The radiologist must assess the involvement of the renal vessels. In the evaluation of retroperitoneal fibrosis, MRI has a higher resolution compared to CT and can provide a better definition of the lesion limits in relation to adjacent tissues when using fat saturation techniques. On MRI, idiopathic retroperitoneal fibrosis appears as a hypointense lesion in T1-weighted images. In T2-weighted images, the signal intensity is proportional to the disease activity. Diffusion-weighted image characteristics and signal intensity values in T2-weighted MRI may contribute to clarify the differential diagnosis of retroperitoneal fibrosis and fibrosis-like malignancies. Differentiating between desmoid fibromatosis and malignant neoplasms of the retroperitoneum can be difficult. In MRI, the findings are variable and related to cellularity and fibrous content. They can be hypointense or isointense to muscle in T1-weighted images and predominantly hyperintense in T2-weighted images, with hypointense bands that represent dense collagen bundles. T2 hyperintensity may decrease over time, as the tumor’s cellularity decreases and collagen deposition increases. With gadolinium administration, desmoids generally show moderate to marked enhancement. Hypointense bands may become more apparent because the collagen bundles are not enhanced by contrast [206, 207] (Fig. 7.42).
Examples of desmoid fibromatosis. The lesions can reach a large volume and generate diagnostic doubt. The MRI brings additional information to the CT, as it allows to evaluate the cellularity and the fibrosis content, which helps in monitoring the response to drug treatments. (a, b) DF originated in the abdominal wall and protruded into the peritoneal cavity. (c) Example of pelvic DF with hypersignal on MRI, suggesting active disease and hypercellularity. (d) Extensive DF of mesentery in a patient with familial adenomatous polyposis
4.5 Fifth Step: Diagnostic Differentiation Between Retroperitoneal Lymph Node Masses
Considering the aspect of the image suggestive of retroperitoneal lymph node mass, once again the data of clinical history and physical examination are crucial for the formulation of the diagnostic hypothesis. All lymph node chains should be evaluated, including the findings of chest, mediastinal, and abdominal CT. In lymphomas, CT usually shows a homogeneous retroperitoneal mass, with imprecise limits, which surrounds but does not deform the great vessels. Sometimes there are signs of infiltration of the mesentery. Among FDG-avid NHL staging exams, the PET-CT contributes to the investigation [160].
In the unicentric form of Castleman’s disease, the most common radiological presentation is a mediastinal or hypervascular pulmonary hilar mass [208]. When seen in the retroperitoneum, it appears as a circumscribed mass with soft tissue attenuation. Smaller masses have homogeneous enhancement after contrast, while larger masses have heterogeneous enhancement. Calcification is uncommon, but when present, it can have varying patterns. MRI generally demonstrates a solid mass with slightly increased signal at T1 in relation to the muscle and hyperintense at T2. There may be intralesional “voids” in the T1 and T2 images, reflecting the vascularization of the lesion, in addition to central linear hypointense septa. In PET-CT, lesions generally have SUV values (average 3.91) lower than those seen in lymphomas. In Castleman’s disease, additional extra-abdominal findings aid in suspected diagnosis. Reticular or ground-glass opacities, mediastinal enlargement, pleural effusion and, more rarely, pulmonary nodules or rounded areas of consolidation may be observed in the chest. Most patients have multiple enlarged mediastinal and hilar lymph nodes. Parenchymal findings can also be observed, including subpleural nodules, interlobular septal thickening, and peri-bronchial vascular thickening. On PET-CT, retroperitoneal fibrosis related to the idiopathic multicentric form of Castleman’s disease has relatively low SUV values (2.5–8). Higher values should raise the suspicion of lymphoma [163].
Metastases from solid tumors to retroperitoneal lymph nodes appear as solid or solid-cystic masses, single or multiple, in different locations. A previous history of malignancy or positive serum markers may suggest a diagnosis of metastatic adenocarcinoma, melanoma, or germ cell tumor. Once again, in young male patients with undefined retroperitoneal masses, testicular ultrasound should be considered. With the exception of epithelioid sarcomas, rhabdomyosarcomas, and clear cell sarcomas, the majority of sarcomas generally do not metastasize to lymph nodes. Therefore, the presence of lymph nodes with a neoplastic aspect increases the possibility of metastatic disease or lymphoma.
In some countries, including Brazil, extrapulmonary tuberculosis can present as retroperitoneal lymphadenopathy and must be remembered among the differential diagnoses. Large retroperitoneal mass, however, is a rare condition. The encapsulation of the abdominal aorta is also described. Tuberculosis can also spread from “Pott’s disease” and form an abscess in the psoas muscle, inflammatory retroperitoneal mass, or retroperitoneal fibrosis.
5 Indications and Types of Biopsy
A frequent question in the approach of the retroperitoneal masses is to decide on the need for biopsy and to define the best way to do it. When the clinical-radiological aspects suggest with a high degree of suspicion that the retroperitoneal tumor corresponds to a diagnosis whose treatment is surgical in the first instance, preoperative biopsy may be dispensed. However, in case of diagnostic doubt or when therapeutic planning implies performing preoperative treatments, biopsy will be necessary and, in most cases, should preferably be image guided with a thick needle, avoiding surgical biopsies. Thick needle image-guided biopsies can be performed on an outpatient basis and have lower morbidity and cost. Another relevant advantage is the possibility of choosing intralesional areas containing viable tissue or areas that may suggest dedifferentiation [209]. The benefits of diagnostic completion using a minimally invasive procedure outweigh any considerations against performing the biopsy. The risk of complications is low, as well as the potential for neoplastic dissemination [210]. In retroperitoneal biopsies, special care must be taken to assess the quality and representativeness of the material, avoiding inconclusive results. If necessary, a new material acquisition can be made before the patient leaves the CT scan. For this reason, the interaction between the interventional radiologist and the specialized pathologist is essential.
In the presence of peripheral lymphadenopathy, if the investigation moves towards the need for biopsy, the peripheral lymph nodes should preferably be accessed, without intervention on the retroperitoneum. The surgical approach in the case of retroperitoneum lymphomas is restricted to situations where simpler and less invasive ways of reaching a histological diagnosis were not conclusive or not possible, indicating a surgical biopsy, which can be performed by laparoscopy or laparotomy. Once again, it is advisable to have the pathologist in the operating room to assess the quality of the material and the amount of material available for further diagnostic complementation studies, such as conducting immunohistochemical reactions or even molecular tests.
When GIST is suspected, special care must be taken. Biopsies should preferably be performed by endoluminal endoscopic accesses, through puncture guided by echo-endoscopy, avoiding rupture of the capsule and peritoneal dissemination. Violation of the integrity of the tumor capsule as a result of percutaneous or open biopsy is associated with a higher risk of peritoneal recurrence. In echo-endoscopy biopsies, the sample is limited and so it is important to inform the pathologist about the diagnostic suspicion, which will allow a directed histopathological analysis, with the inclusion of c-KIT and DOG-1 in the immunohistochemistry panel.
6 Considerations About Surgical Indications and Preoperative Care
Operations related to primary tumors of the retroperitoneal space are often highly complex surgical situations. It is not possible to list the diversity of situations in which the complexity is secondary to problems imposed by the neoplasia; however, aspects associated with vascular problems certainly constitute a point of greater relevance. Examples are the involvement of large vessels (aorta, vena cava, and iliac vessels), primary tumors of the vena cava, intra-caval tumor thrombus, high risk of visceral devascularization due to involvement of vascular trunks, and the need for multivisceral resection, among others.
The complexity imposed by the neoplasm can be worsened by clinical problems such as old age, precarious nutritional status, sarcopenia, and organ dysfunction (cardiac, respiratory, renal, liver, neurological, endocrine, etc.). In this sense, the choice of the therapeutic path and decisions must be taken in a multidisciplinary way, in the presence of surgeon oncologists, clinical oncologists, radiotherapists, radiologists, pathologists, and other specialties, with emphasis on vascular surgery.
In addition to the clinical decision, equally important is the transparent clarification to the patient and his family about the therapeutic proposal and its risks, when clinical issues, risks, the possibility of sequelae, and the impact on quality of life must be addressed. In the scenario of high complexity, other aspects are of extreme importance, such as the structure of perioperative and transoperative care, including the anesthesia, intensive care, and blood bank teams. The support of nursing, physiotherapy, physiatry, speech therapy, nutrition, rehabilitation, and psychology is also a fundamental part of the treatment process in all its phases so that the objectives are reached safely.
In addition to a careful clinical evaluation, the expectation and understanding of the proposal must be worked on in a particular way. In operations where a high risk of major complications and even death is expected, the indication is always difficult. Deep knowledge about the biological behavior of the disease is essential to avoid unsuccessful decisions. Concerns about pre- and postoperative care, hospital structure, and team composition are fundamental aspects for safety and good result of the procedures, respecting ethical issues in order to protect the patient, the doctor, and the hospital. It is mandatory filling out of terms of responsibility for surgery, anesthesia, transfusion, and others. In situations of high complexity, the wrong judgment can seal the patient’s only chance to be free of the disease, either by an inappropriate indication or by the wrong contraindication. The cases presented in Figs. 7.43 and 7.44 illustrate the aspects discussed.
A 12-year-old female patient underwent right adnexectomy with pathological result of immature teratoma. Two years later, she had a large volume peritoneal recurrence. A laparotomy was performed, and the lesion was considered unresectable. She was treated with systemic chemotherapy and evolved with disease stability followed by progression and loss of follow-up for a period of 8 years, when she returned to the institution due to clinical worsening. CT showed a massive lesion, cranially dislocating the diaphragm with pulmonary compression and dislocating the liver and other abdominal organs and structures, in addition to invading the abdominal wall. There was also a second mediastinal lesion. After a multidisciplinary discussion and agreement by the patient (at that time with 23 years old) and family members, a new resection attempt was proposed. (a) Positioning the patient in the operating room. (b) Intraoperative view: wide mobilization of the lesion achieved by total resection of the right diaphragm. (c) Aspect of the surgical bed after removal of the surgical specimen (tumor and diaphragm). Note the lower lobe of the right lung, the inferior vena cava repaired close to the heart and the aspect of liver deformity secondary to years of tumor compression. (d) Detail of the repair of the inferior vena cava close to the right atrium and the wide freno-laparotomy. (e) Replacement of the removed diaphragm with patches of bovine pericardium. (f) The patient had an excellent evolution with discharge on the 13th postoperative day. CT shows absence of abdominal disease and the presence of mediastinal lesion not removed in the abdominal intervention. (g) The mediastinal lesion was resected in a new operation. CT shows the final appearance after the end of the treatment. The patient has a follow-up period of 5 years, with no evidence of disease. She became pregnant and gave birth to a healthy child through cesarean delivery. The case illustrates the need for a surgical, anesthetic, and specialized intensive care team, in addition to adequate hospital structure and resources, so that there is a chance of therapeutic success in situations of high complexity, common points in the surgical treatment of different large retroperitoneal and intraperitoneal tumors
A 47-year-old female patient with large local recurrence of a retroperitoneal liposarcoma. The CT images at the upper part of the figure shows a predominantly adipose expansive mass, with multiple septa and some solid nodular images, occupying the retroperitoneal space of the left flank and iliac fossa, insinuating itself posteriorly to the psoas and pelvis. The mass contacts the left side wall of the urinary bladder and compresses the left ureter at the intersection with the iliac vessels, without hydronephrosis. It dislocates the left colon and the small intestine loops and has contact with the external iliac, internal iliac, and obturator vessels on this side. The patient underwent neoadjuvant systemic chemotherapy and was then taken to surgery with an intraoperative radiotherapy schedule. (a, b) The surgery consisted of “en bloc” resection of the tumor with the left colon (descending, sigmoid, and high rectum) and left external iliac artery, which was replaced by a 6Fr Dacron prosthesis. (c, d) Intraoperative radiation with linear accelerator. She had a good postoperative recovery. The pathological result showed a low-grade “lipoma-like” liposarcoma with areas of necrosis at its largest extent and areas of dedifferentiation (high-grade) next to the iliac vessels. She was referred to receive a complementary dose of external radiotherapy. (e) Control tests 6 years after the end of treatment. The patient has been followed up for 10 years, with no evidence of disease. The case illustrates the importance of multidisciplinary interaction in therapeutic planning, in order to minimize the risk of recurrence in situations of marginal resections, common in retroperitoneal tumors. (Fábio Ferreira, surgical oncology; Kenji Nishinari, vascular surgery; João Luís Fernandes, radiotherapy)
7 Associated Vascular Problems
We will discuss some situations whose knowledge is essential to allow patients in extreme situations to be properly evaluated and have the possibility to benefit from complete oncological resections, not being considered as having unresectable tumors due to associated vascular problems.
7.1 Circumferential Involvement of Large Vessels
The need for complete or partial resection of large vessels is not uncommon in retroperitoneum tumors, situations in which one of the concerns is the risk of massive bleeding. When there is circumferential involvement of the aorta and vena cava, surgery usually proceeds safely until vascular repair. After total vascular clamping, the “en bloc” resection phase of the tumor containing the large vessels is also safe; however, depending on the extent of the lesion, there may be considerable bleeding from lumbar and retroperitoneal vessels and visual access for hemostasis is impaired by the tumor volume. After resection, upon reestablishing arterial flow through aortic reconstruction, there is a significant increase in venous return pressure, with the risk of massive retroperitoneal bleeding until the reestablishment of venous flow with reconstruction of the vena cava. Depending on the time of ischemia, arterial flow is usually reestablished with priority. To minimize the risk of bleeding, both in the resection phase and after the restoration of arterial flow, an alternative is to create an arterial and venous vascular bypass as an initial measure, preceding the resection phase. One way is to perform the “bypass” with the vascular prostheses themselves, leaving them redundant, keeping the arterial and venous flow diverted from the area to be resected with the tumor. After resection, prostheses are shortened easily, with wide exposure, minimizing the risk of excessive bleeding [211] (Figs. 7.45 and 7.46). In smaller tumors, where the resection phase is faster, the tactic of using a temporary bypass is not mandatory; however, it is essential that the proximal and distal vascular stumps are fully prepared, and the vascular surgery team is present to discuss reconstruction alternatives before the resection is completed. Lesions that involve the confluence of common iliac veins and aortic artery bifurcation, even if they are not large in volume, may require even more elaborate planning and reconstruction care (Figs. 7.47 and 7.48).
A 29-year-old female patient, complaining of pain and abdominal swelling associated with lower limb edema. CT shows an extensive solid mass with circumferential involvement of the aorta and vena cava. A thick needle biopsy revealed the diagnosis of Schwannoma. Considering that she was a very young patient without clinical problems, surgery planning was carried out between the oncological and vascular surgery teams. To minimize the risk of bleeding, the alternative was to create an arterial and venous vascular bypass preceding the resection phase. The “by-pass” was performed with the vascular prostheses themselves, maintaining the arterial and venous flow. After the “en bloc” resection, the prostheses were shortened with wide exposure and without excessive bleeding. She had a postoperative recovery without complications. Later, she had venous thrombosis, but without clinical repercussion. This patient was operated on in 1998 (first CT image) and the control CT image shown in the lower part of the figure was done in 2012. Currently, she has a follow-up period of 22 years and still doing well. (Drawings authorized for reprinting by the authors: Nishinari et al. [211])
A 29-year-old male patient diagnosed with a right testicle tumor was submitted to a radical orchiectomy. The pathological exam showed a nonseminomatous tumor with a teratoma component. During follow-up, he presented an extensive retroperitoneal recurrence that was treated with systemic chemotherapy with normalization of tumor markers, but with persistence of a large volume retroperitoneal residual mass. The patient was prepared for surgical intervention by the oncology and vascular surgery teams. Note the large volume of disease and extensive vascular involvement in CT sections. (a) Wide median laparotomy with left lateral extension. (b) Mobilization of the lesion with exposure and repair of the inferior vena cava and aorta. (c) Temporary “by-pass” made with the vascular prosthesis itself. (d) Operative bed after tumor resection showing the “redundancy” of the prosthesis. (e) Operative bed after shortening of the prosthesis. (f) Surgical specimen showing the “en bloc” resection of the tumor with the segments of the aorta and iliac arteries, and vena cava and iliac veins. No venous reconstruction was performed, and the vena cava was interrupted below the right renal vein. The patient had a good postoperative recovery, without major complications. The pathology showed a teratoma with a rhabdomyosarcoma component. The patient is at 3 years of follow-up, with no evidence of disease. (Courtesy of André Luís de Freitas Perina, surgical oncology and Fávio Duarte, vascular surgery)
A 68-year-old male patient with retroperitoneal pleomorphic sarcoma. MRI shows vascular involvement at the bifurcation of the aorta and at the confluence of common iliac veins. The surgery was jointly scheduled by the oncology and vascular surgery teams. In this case, the option was to precede the resection without doing a temporary “by-pass.” During the resection phase, however, there was a significant bleeding, which was only adequately controlled after the reestablishment of the venous flow. (a) Isolation and proximal repair of the aorta, vena cava, and ureters. (b) Isolation and distal repair of the external iliac vessels bilaterally. (c) Operative bed after “en bloc” resection of the tumor with a segment of the aorta and common iliac arteries and a segment of the inferior vena cava and common iliac veins. (d) Arterial reconstruction with bifurcated Dacron prosthesis and venous reconstruction with bifurcated PTFE prosthesis. (Fábio Ferreira, surgical oncology and Kenji Nishinari, vascular surgery)
A 47-year-old male patient with extensive dedifferentiated liposarcoma of retroperitoneum with clear involvement of the right iliac vessels (CT). He was treated according to institutional protocol with preoperative radiation followed by surgery. (a) View of the tumor after wide laparotomy – note the signs of visceral involvement. (b) Operative bed after “en bloc” resection (duodenum segment, ileum segment, right colon, transverse colon segment, right kidney, ureter, and right iliac vessels). Observe the iliac-femoral vascular reconstruction with prosthesis. Due to hemodynamic instability, option was made for nonvenous reconstruction. (c) Omentum flap to protect the prosthesis and isolate the areas of intestinal anastomosis. (d) Final view of the operative field after intestinal anastomoses. The patient had a prolonged recovery, being discharged 30 days after the operation. He has a follow-up period of 1 year, with no signs of recurrence, without functional restriction, with mild edema of the right lower limb. (Courtesy of Tibério Moura de Andrade Lima, surgical oncology and Luciana Ragazzo Araujo Teixeira, vascular surgery)
7.2 Primary Leiomyosarcoma of the Vena Cava
Retroperitoneal leiomyosarcomas are often primary tumors of the inferior vena cava [212]. When the need for segmental resection of the inferior vena cava is expected, depending on the location of the tumor, there is a chance of nephrectomy as a consequence of the involvement of the renal pedicle vessels. Static renal scintigraphy (99mTc-DMSA) to assess renal tubular function is useful for deciding whether nephrectomy is an alternative. If there is an absolute need for renal preservation, in cases of single kidney or dominant kidney at risk for resection, renal revascularization should be planned.
When the resection of large retroperitoneal vessels is foreseen, wide exposure is necessary. We prefer a wide median laparotomy. In large-volume tumors, if necessary, transverse incisions can be associated, both to the right and to the left, creating a wide exposure. Ample mobilization of the right colon, duodenum, and right kidney is generally necessary. Then, proximal and distal isolation of the vena cava is performed in the region of interest. Depending on the height of the lesion, it is essential to identify and isolate the vessels of the renal pedicle. In addition to the proximal and distal repairs to the area of interest, in situations where it is intended to open the vena cava for partial resections, some precautions must be respected: (1) Isolate and repair the right and left renal veins. (2) If possible, isolate and repair of the renal arteries for clamping if there is a need to interrupt the arterial flow in order to decrease the venous return to the vena cava through the renal veins. (3) After isolating the vena cava and the vessels of the renal pedicle, the venous flow of lumbar veins that drain into the vena cava must be stopped before opening (the lumbar veins must be connected or clipped individually along the entire length between proximal and distal cava repairs). (4) Immediately before clamping the vessels, the anesthetist is asked to infuse heparin intravenously; only then the clamping is proceeded. The infrarenal segment of the vena cava should be clamped first, the renal arteries second (if necessary), the renal veins in third and, finally, the proximal vena cava. This sequence allows “emptying” the vena cava in the territory of interest, minimizing the outflow of blood that can impair vision. If necessary, clamping of the renal arteries should be done for the shortest possible time, with intermittent unclamping if the ischemia time is prolonged. To avoid gas embolism, vascular clamping should not be released if the vena cava is opened. (5) During the reconstruction phase, small segments can be treated by primary suture as long as it does not cause stenosis. Partial loss of a larger segment may imply reconstruction with a pericardium patch or similar. Wider resections require replacement with prostheses. After the reconstruction of the vena cava, the vessels are sequentially unclamped, one at a time, observing if there are any bleeding points and the hemostasis is reviewed (Fig. 7.49).
A 74-year-old female patient had a retroperitoneal mass found during an image exam performed to investigate diverticulitis symptoms. MRI shows two solid nodular lesions located anterior to the inferior vena cava. The patient underwent an image-guided biopsy and was diagnosed with leiomyosarcoma. A diagnostic hypothesis of primary leiomyosarcoma of the inferior vena cava was made. (a) The patient was taken to surgery with the finding of two primary distinct lesions of the inferior vena cava, with the right renal artery passing between the lesions and the right renal vein free from invasion, which allowed renal preservation. (b) Primary suture of the vena cava after resection of the smaller and more cranial lesion. (c) Resection of the second lesion with a segment of the vena cava wall. (d) Repair of the vena cava segment with a bovine pericardium patch. (Fábio Ferreira, surgical oncology and Kenji Nishinari, vascular surgery)
This series of cases illustrates some of the most common situations of the association of vascular problems found in the surgical management of retroperitoneal tumors.
8 Conclusion
Retroperitoneal tumors represent a real challenge for different medical specialties. The variety of diagnoses, presentations, and treatments makes the search for the correct diagnosis a path to be followed step by step, in order to avoid errors potentially harmful to the patient. Upon diagnosis of retroperitoneal mass, singular importance must be given to the clinical-radiological characteristics in order to classify retroperitoneal tumors according to their etiology, facilitating further investigation and referral among specialists. In our chapter, we chose to combine retroperitoneal tumors into four major groups: (1) intraperitoneal lesions that simulate retroperitoneal tumors; (2) primary tumors of retroperitoneal organs; (3) primary tumors of the retroperitoneal space; and (4) retroperitoneal lymph node masses. As we have seen, many retroperitoneal tumors are treated surgically, and the involvement of large retroperitoneal vessels is not uncommon. Even when the diagnosis does not require surgical treatment, associated vascular problems can occur. Thus, the knowledge of the theme brings an additional contribution to oncologists and vascular surgeons, who will certainly be consulted for joint action in oncological surgeries or to solve vascular problems secondary to different etiologies.
References
Tirkes T, Sandrasegaran K, Patel AA, Hollar MA, Tejada JG, Tann M, et al. Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging. Radiographics. 2012;32(451):437–52.
Goenka AH, Shah SN, Remer EM. Imaging of the retroperitoneum. Radiol Clin N Am. 2012;50(2):333–55.
Coffin A, Boulay-Coletta I, Sebbag-Sfez D, Zins M. Radioanatomy of the retroperitoneal space. Diagn Interv Imaging. 2015;96(2):171–86.
Storm FK, Eilber FR, Mirra J, Morton DL. Retroperitoneal sarcomas: a reappraisal of treatment. J Surg Oncol. 1981;17(1):1–7.
Storm FK, Mahvi DM. Diagnosis and management of retroperitoneal soft-tissue sarcoma. Ann Surg. 1991;214(1):2–10.
Merran S. Tumeurs rétropéritonéales primitives de l’adulte. J Radiol. 2004;85(2):252–64.
Ma GL, Murphy JD, Martinez ME, Sicklick JK. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomark Prev. 2015;24(1):298–302.
Miettinen M, Monihan JM, Sarlomo-Rikala M, Kovatich AJ, Carr NJ, Emory TS, et al. Gastrointestinal stromal tumors/smooth muscle tumors (GISTs) primary in the omentum and mesentery. Am J Surg Pathol. 1999;23(9):1109.
Miettinen M, Lasota J. Gastrointestinal stromal tumors – definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438(1):1–12.
Parab TM, DeRogatis MJ, Boaz AM, Grasso SA, Issack PS, Duarte DA, et al. Gastrointestinal stromal tumors: a comprehensive review. J Gastrointest Oncol. 2019;10(1):144–54.
Fletcher CDM, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol. 2002;10(2):81–9.
Yamamoto H, Oda Y, Kawaguchi K-i, Nakamura N, Takahira T, Tamiya S, Saito T, Oshiro Y, Ohta Y, Yao T, Tsuneyoshi T. c-kit and PDGFRA mutations in extragastrointestinal stromal tumor (gastrointestinal stromal tumor of the soft tissue). Am J Surg Pathol. 2004;28(4):479–88.
Sircar K, Hewlett BR, Huizinga JD, Chorneyko K, Berezin I, Riddell RH. Interstitial cells of Cajal as precursors of gastrointestinal stromal tumors. Am J Surg Pathol. 1999;23(4):377–89.
Miettinen M, Fetsch JF, Sobin LH, Lasota J. Gastrointestinal stromal tumors in patients with neurofibromatosis 1: a clinicopathologic and molecular genetic study of 45 cases. Am J Surg Pathol. 2006;30(1):90–6.
Rubin BP, Singer S, Tsao C, Duensing A, Lux ML, Ruiz R, et al. KIT activation is a ubiquitous feature of gastrointestinal stromal tumors. Cancer Res. 2001;61(22):8118–21.
Rubin BP, Fletcher JA, Fletcher CDM. Molecular insights into the histogenesis and pathogenesis of gastrointestinal stromal tumors. Int J Surg Pathol. 2000;8(1):5–10.
Hirota S, Isozaki K, Moriyama Y, Hashimoto H, Nishida T, Ishiguro S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science (80-). 1998;279(5350):577–80.
Heinrich MC. PDGFRA activating mutations in gastrointestinal stromal tumors. Science (80- ). 2003;299(5607):708–10.
Miettinen M, Wang ZF, Lasota J. DOG1 antibody in the differential diagnosis of gastrointestinal stromal tumors: a study of 1840 cases. Am J Surg Pathol. 2009;33(9):1401–8.
Novelli M, Rossi S, Rodriguez-Justo M, Taniere P, Seddon B, Toffolatti L, et al. DOG1 and CD117 are the antibodies of choice in the diagnosis of gastrointestinal stromal tumours. Histopathology. 2010;57(2):259–70.
Ghanem N, Altehoefer C, Furtwängler A, Winterer J, Schäfer O, Springer O, et al. Computed tomography in gastrointestinal stromal tumors. Eur Radiol. 2003;13(7):1669–78.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23(2):70–83.
Joensuu H, Vehtari A, Riihimäki J, Nishida T, Steigen SE, Brabec P, et al. Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. Lancet Oncol. 2012;13(3):265–74.
Giuliano K, Nagarajan N, Canner J, Najafian A, Wolfgang C, Schneider E, et al. Gastric and small intestine gastrointestinal stromal tumors: do outcomes differ? J Surg Oncol. 2017;115(3):351–7.
Lanke G, Lee JH. How best to manage gastrointestinal stromal tumor. World J Clin Oncol. 2017;8(2):135–44.
Balachandran VP, DeMatteo RP. Gastrointestinal stromal tumors: who should get imatinib and for how long? Adv Surg. 2014;48:165–83.
DeMatteo RP, Ballman KV, Antonescu CR, Corless C, Kolesnikova V, Von Mehren M, et al. Long-term results of adjuvant imatinib mesylate in localized, high-risk, primary gastrointestinal stromal tumor: ACOSOG Z9000 (Alliance) intergroup phase 2 trial. Ann Surg. 2013;258(3):422–8.
DeMatteo RP, Maki RG, Singer S, Gonen M, Brennan MF, Antonescu CR. Results of tyrosine kinase inhibitor therapy followed by surgical resection for metastatic gastrointestinal stromal tumor. Ann Surg. 2007;245(3):347–52.
Verweij J, Casali PG, Zalcberg J, LeCesne A, Reichardt P, Blay JY, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomised trial. Lancet. 2004;364(9440):1127–34.
Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39(10):1411–9.
Lee SH, Ha HK, Byun JY, Kim AY, Cho KS, Lee YR, et al. Radiological features of leiomyomatous tumors of the colon and rectum. J Comput Assist Tomogr. 2000;24(3):407–12.
Chun HJ, Byun JY, Chun KA, Rha SE, Jung SE, Lee JM, et al. Gastrointestinal leiomyoma and leiomyosarcoma: CT differentiation. J Comput Assist Tomogr. 1998;22(1):69–74.
Tropé CG, Abeler VM, Kristensen GB. Diagnosis and treatment of sarcoma of the uterus. A review. Acta Oncol. 2012;51(6):694–705.
Juhasz-Böss I, Gabriel L, Bohle RM, Horn LC, Solomayer EF, Breitbach GP. Uterine leiomyosarcoma. Oncol Res Treat. 2018;41(11):680–6.
Romagnolo C, Leon AE, Fabricio ASC, Taborelli M, Polesel J, Del Pup L, et al. HE4, CA125 and risk of ovarian malignancy algorithm (ROMA) as diagnostic tools for ovarian cancer in patients with a pelvic mass: an Italian multicenter study. Gynecol Oncol. 2016;141(2):303–11.
Campos C, Sarian LO, Jales RM, Hartman C, Araújo KG, Pitta D, et al. Performance of the risk of malignancy index for discriminating malignant tumors in women with adnexal masses. J Ultrasound Med. 2016;35(1):143–52.
Timmerman D, Testa AC, Bourne T, Ameye L, Jurkovic D, Van Holsbeke C, et al. Simple ultrasound-based rules for the diagnosis of ovarian cancer. Ultrasound Obstet Gynecol. 2008;31(6):681–90.
Yanaranop M, Tiyayon J, Siricharoenthai S, Nakrangsee S, Thinkhamrop B. Rajavithi-ovarian cancer predictive score (R-OPS): a new scoring system for predicting ovarian malignancy in women presenting with a pelvic mass. Gynecol Oncol. 2016;141(3):479–84.
Kubeček O, Laco J, Špaček J, Petera J, Kopecký J, Kubečková A, et al. The pathogenesis, diagnosis, and management of metastatic tumors to the ovary: a comprehensive review. Clin Exp Metastasis. 2017;34(5):295–307.
Bennett JA, Oliva E. Pathology of the adnexal mass. Clin Obstet Gynecol. 2015;58(1):3–27.
Al-Agha OM, Nicastri AD. An in-depth look at Krukemberg tumor: an overview. Arch Pathol Lab Med. 2006;130(11):1725–30.
Agnes A, Biondi A, Ricci R, Gallotta V, D’Ugo D, Persiani R. Krukenberg tumors: seed, route and soil. Surg Oncol. 2017;26(4):438–45.
Bal A, Joshi K, Vaiphel K, Wig JD. Primary duodenal neoplasms: a restrospective clinico-pathological analysis. World J Gastroenterol. 2007;13(7):1108–11.
Barral M, Faraoun SA, Fishman EK, Dohan A, Pozzessere C, Berthelin MA, et al. Imaging features of rare pancreatic tumors. Diagn Interv Imaging. 2016;97(12):1259–73.
Park JJ, Park BK, Kim CK. Adrenal imaging for adenoma characterization: imaging features, diagnostic accuracies and differential diagnoses. Br J Radiol. 2016;89(1062):1–13.
Weston MJ. Virtual special issue: renal masses. Clin Radiol. 2017;72(10):826–7.
Pilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol. 2004;52(3):229–39.
Golan JD, Jacques L. Nonneoplastic peripheral nerve tumors. Neurosurg Clin N Am. 2004;15(2):223–30.
Krutman M, Nishinari K, Pignataro BS, Yazbek G, Zottele Bomfim GA, Cavalcante RN, et al. Twenty years of experience in vascular reconstructions associated with resection of malignant neoplasms in a single cancer center. J Vasc Surg. 2019;69(6):1880–8.
Modha A, Paty P, Bilsky MH. Presacral ganglioneuromas. J Neurosurg Spine. 2009;2(3):366–71.
Skovronsky DM, Oberholtzer JC. Pathologic classification of peripheral nerve tumors. Neurosurg Clin N Am. 2004;15(2):157–66.
Neumann HPH, Young WF, Eng C. Pheochromocytoma and paraganglioma. N Engl J Med. 2019;381(6):552–65.
Erickson D, Kudva YC, Ebersold MJ, Thompson GB, Grant CS, Van Heerden JA, et al. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab. 2001;86(11):5210–6.
Lee JH, Barich F, Karnell LH, Robinson RA, Zhen WK, Gantz BJ, et al. National cancer data base report on malignant paragangliomas of the head and neck. Cancer. 2002;94(3):730–7.
Boedeker CC, Neumann HPH, Maier W, Bausch B, Schipper J, Ridder GJ. Malignant head and neck paragangliomas in SDHB mutation carriers. Otolaryngol Head Neck Surg. 2007;137(1):126–9.
Elder EE, Elder G, Larsson C. Pheochromocytoma and functional paraganglioma syndrome: no longer the 10% tumor. J Surg Oncol. 2005;89(3):193–201.
Parenti G, Zampetti B, Rapizzi E, Ercolino T, Giach V, Mannelli M. Updated and new perspectives on diagnosis, prognosis, and therapy of malignant pheochromocytoma/paraganglioma. J Oncol. 2012;2012:872713.
Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. Nat Clin Pract Endocrinol Metab. 2007;3(2):92–102.
Welander J, Söderkvist P, Gimm O. Genetics and clinical characteristics of hereditary pheochromocytomas and paragangliomas. Endocr Relat Cancer. 2011;18(6):253–76.
Eisenhofer G, Tischler AS, De Krijger RR. Diagnostic tests and biomarkers for pheochromocytoma and extra-adrenal paraganglioma: from routine laboratory methods to disease stratification. Endocr Pathol. 2012;23(1):4–14.
Lenders JWM, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SKG, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915–42.
Kliewer KE, Wen DR, Cancilla PA, Cochran AJ. Paragangliomas: assessment of prognosis by histologic, immunohistochemical, and ultrastructural techniques. Hum Pathol. 1989;20(1):29–39.
Plouin PF, Gimenez-Roqueplo AP, La Batide Alanore A, Salenave S, Duclos JM. Evolving concepts in the diagnosis, prognosis, and treatment of pheochromocytoma. Rev Med Interne. 2000;21(12):1075–85.
Lenders JWM, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, et al. Biochemical diagnosis of pheochromocytoma. JAMA. 2002;287(11):1427–34.
Davidson FD. Phaeochromocytoma with normal urinary catecholamines: the potential value of urinary free metadrenalines. Ann Clin Biochem. 2002;39(6):557–66.
Garg PK, Jain BK, Kumar A, Bhatt S, Vibhav V. Fat poor angiomyolipoma with lymphadenopathy: diagnostic dilemma. Urol Ann. 2012;4(2):126–9.
Sharma G, Jain A, Sharma P, Sharma S, Rathi V, Garg PK. Giant exophytic renal angiomyolipoma masquerading as a retroperitoneal liposarcoma: a case report and review of literature. World J Clin Oncol. 2018;9(7):162–6.
Jinzaki M, Silverman SG, Akita H, Mikami S, Oya M. Diagnosis of renal angiomyolipomas: classic, fat-poor, and epithelioid types. Semin Ultrasound CT MR. 2017;38(1):37–46.
Tsai HY, Lee KH, Ng KF, Kao YT, Chuang CK. Clinicopathologic analysis of renal epithelioid angiomyolipoma: consecutively excised 23 cases. Kaohsiung J Med Sci. 2019;35(1):33–8.
Luna NT, Mosquera JE, Comba IY, Kinaan M, Otoya J. A primary adrenal epithelioid angiomyolipoma (PEComa) in a patient with tuberous sclerosis complex: report of a case and review of the literature. Case Rep Med. 2020;2020:4–7.
Redkar N, Patil MA, Dhakate T, Kolhe P. Tuberous sclerosis complex presenting as bilateral large renal angiomyolipomas. BMJ Case Rep. 2012;2012:1–4.
Shankar S, Hulikanthimatt KS, Awatti SM, Narayanrao ST. Bilateral multifocal renal angiomyolipoma associated with Wunderlich’s syndrome in a tuberous sclerosis patient. J Clin Diagn Res. 2015;9(8):ED01–3.
Kebria M, Black D, Borelli C, Modica I, Hensley M, Chi DS. Primary retroperitoneal lymphangioleiomyomatosis in a postmenopausal woman: a case report and review of the literature. Int J Gynecol Cancer. 2007;17(2):528–32.
Słodkowska J, Patera J, Breborowicz J, Jarzemska A, Korzeniewska-Kosela M, Siemiatkowska K, et al. Extrapulmonary lymphangioleiomyomatosis presented as the asymptomatic retroperitoneal tumours--two cases report. Pol J Pathol. 2006;57(4):205–7.
Sandrini A, Silverstone E, Yates DH. Menstrual cycle variation of retroperitoneal lymphangioleiomyomas in lymphangioleiomyomatosis. Intern Med J. 2011;41(12):832–5.
Derweduwen AM, Verbeken E, Stas M, Verschakelen J, Coolen J, Verleden G, et al. Extrapulmonary lymphangioleiomyomatosis: a wolf in sheep’s clothing. Thorax. 2013;68(1):111–3.
Avila NA, Bechtle J, Dwyer AJ, Ferrans VJ, Moss J. Lymphangioleiomyomatosis: CT of diurnal variation of lymphangioleiomyomas. Radiology. 2001;221(2):415–21.
Tobino K, Johkoh T, Fujimoto K, Sakai F, Arakawa H, Kurihara M, et al. Computed tomographic features of lymphangioleiomyomatosis: evaluation in 138 patients. Eur J Radiol. 2015;84(3):534–41.
Terada T. Giant fibrolipoma of the spermatic cord: short communication. Pathol Int. 2010;60(4):330–2.
Weniger M, D’Haese JG, Kunz W, Pratschke S, Guba M, Werner J, et al. En-bloc resection of a giant retroperitoneal lipoma: a case report and review of the literature. BMC Res Notes. 2015;8(1):8–11.
Pisters PWT, O’Sullivan B. Retroperitoneal sarcomas: combined modality treatment approaches. Curr Opin Oncol. 2002;14(4):400–5.
Stoeckle E, Coindre J-M, Bonvalot S, Kantor G, Terrier P, Bonichon F, et al. Prognostic factors in retroperitoneal sarcoma. Cancer. 2001;92(2):359–68.
Renne SL, Iwenofu OH. Pathology of retroperitoneal sarcomas: a brief review. J Surg Oncol. 2018;117(1):12–24.
Pham TH, Iqbal CW, Zarroug AE, Donohue JH, Moir C. Retroperitoneal sarcomas in children: outcomes from an institution. J Pediatr Surg. 2007;42(5):829–33.
Mariño-Enríquez A, Fletcher CDM, Cin PD, Hornick JL. Dedifferentiated liposarcoma with “homologous” lipoblastic (pleomorphic liposarcoma-like) differentiation: clinicopathologic and molecular analysis of a series suggesting revised diagnostic criteria. Am J Surg Pathol. 2010;34(8):1122–31.
Singer S, Antonescu CR, Riedel E, Brennan MF, Pollock RE. Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg. 2003;238(3):358–71.
Lahat G, Tuvin D, Wei C, Anaya DA, Bekele BN, Lazar AJ, et al. New perspectives for staging and prognosis in soft tissue sarcoma. Ann Surg Oncol. 2008;15(10):2739–48.
Alldinger I, Yang Q, Pilarsky C, Saeger HD, Knoefel WT, Peiper M. Retroperitoneal soft tissue sarcomas: prognosis and treatment of primary and recurrent disease in 117 patients. Anticancer Res. 2006;26(2 B):1577–81.
Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998;228(3):355–65.
Anaya DA, Lev DC, Pollock RE. The role of surgical margin status in retroperitoneal sarcoma. J Surg Oncol. 2008;98(8):607–10.
Toulmonde M, Bonvalot S, Méeus P, Stoeckle E, Riou O, Isambert N, et al. Retroperitoneal sarcomas: patterns of care at diagnosis, prognostic factors and focus on main histological subtypes: a multicenter analysis of the French Sarcoma Group. Ann Oncol. 2014;25(3):735–42.
van Houdt WJ, Raut CP, Bonvalot S, Swallow CJ, Haas R, Gronchi A. New research strategies in retroperitoneal sarcoma. The case of TARPSWG, STRASS and RESAR: making progress through collaboration. Curr Opin Oncol. 2019;31(4):310–6.
Ronchi A, Cozzolino I, Zito Marino F, Accardo M, Montella M, Panarese I, et al. Extrapleural solitary fibrous tumor: a distinct entity from pleural solitary fibrous tumor. An update on clinical, molecular and diagnostic features. Ann Diagn Pathol. 2018;34:142–50.
Gold JS, Antonescu CR, Hajdu C, Ferrone CR, Hussain M, Lewis JJ, et al. Clinicopathologic correlates of solitary fibrous tumors. Cancer. 2002;94(4):1057–68.
Demicco EG, Park MS, Araujo DM, Fox PS, Bassett RL, Pollock RE, et al. Solitary fibrous tumor: a clinicopathological study of 110 cases and proposed risk assessment model. Mod Pathol. 2012;25(9):1298–306.
Mosquera JM, Fletcher CDM. Expanding the spectrum of malignant progression in solitary fibrous tumors: a study of 8 cases with a discrete anaplastic component-is this dedifferentiated SFT? Am J Surg Pathol. 2009;33(9):1314–21.
Lee JC, Fletcher CDM. Malignant fat-forming solitary fibrous tumor (so-called “lipomatous hemangiopericytoma”): clinicopathologic analysis of 14 cases. Am J Surg Pathol. 2011;35(8):1177–85.
Baldi GG, Stacchiotti S, Mauro V, Dei Tos AP, Gronchi A, Pastorino U, et al. Solitary fibrous tumor of all sites: outcome of late recurrences in 14 patients. Clin Sarcoma Res. 2013;3(1):4.
Gholami S, Cassidy MR, Kirane A, Kuk D, Zanchelli B, Antonescu CR, et al. Size and location are the most important risk factors for malignant behavior in resected solitary fibrous tumors. Ann Surg Oncol. 2017;24(13):3865–71.
Tay CKJ, Teoh HL, Su S. A common problem in the elderly with an uncommon cause: hypoglycaemia secondary to the Doege-Potter syndrome. BMJ Case Rep. 2015;2015:1–5.
Chmielecki J, Crago AM, Rosenberg M, O’Connor R, Walker SR, Ambrogio L, et al. Whole-exome sequencing identifies a recurrent NAB2-STAT6 fusion in solitary fibrous tumors. Nat Genet. 2013;45(2):131–2.
Doyle LA, Vivero M, Fletcher CDM, Mertens F, Hornick JL. Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Mod Pathol. 2014;27(3):390–5.
Cardillo G, Lococo F, Carleo F, Martelli M. Solitary fibrous tumors of the pleura. Curr Opin Pulm Med. 2012;18(4):339–46.
Park MS, Patel SR, Ludwig JA, Trent JC, Conrad CA, Lazar AJ, et al. Activity of temozolomide and bevacizumab in the treatment of locally advanced, recurrent, and metastatic hemangiopericytoma and malignant solitary fibrous tumor. Cancer. 2011;117(21):4939–47.
Stacchiotti S, Negri T, Libertini M, Palassini E, Marrari A, De Troia B, et al. Sunitinib malate in solitary fibrous tumor (SFT). Ann Oncol. 2012;23(12):3171–9.
Valentin T, Fournier C, Penel N, Bompas E, Chaigneau L, Isambert N, et al. Sorafenib in patients with progressive malignant solitary fibrous tumors: a subgroup analysis from a phase II study of the French Sarcoma Group (GSF/GETO). Investig New Drugs. 2013;31(6):1626–7.
Stacchiotti S, Simeone N, Lo Vullo S, Morosi C, Greco FG, Gronchi A, et al. Activity of axitinib in progressive advanced solitary fibrous tumour: results from an exploratory, investigator-driven phase 2 clinical study. Eur J Cancer. 2019;106:225–33.
Grier HE. Ewing’s sarcoma and primitive neuroectodermal tumors. Pediatr Clin N Am. 1997;44(4):991–1004.
Patnaik S, Yarlagadda J, Susarla R. Imaging features of Ewing’s sarcoma: special reference to uncommon features and rare sites of presentation. J Cancer Res Ther. 2018;14(5):1014.
Cash T, McIlvaine E, Krailo MD, Lessnick SL, Lawlor ER, Laack N, et al. Comparison of clinical features and outcomes in patients with extraskeletal versus skeletal localized Ewing sarcoma: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2016;63(10):1771–9.
Thompson LDR. Pheochromocytoma of the adrenal gland scaled score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol. 2002;26(5):551–66.
Strong VE, Kennedy T, Al-Ahmadie H, Tang L, Coleman J, Fong Y, et al. Prognostic indicators of malignancy in adrenal pheochromocytomas: clinical, histopathologic, and cell cycle/apoptosis gene expression analysis. Surgery. 2008;143(6):759–68.
Adjallé R, Plouin PF, Pacak K, Lehnert H. Treatment of malignant pheochromocytoma. Horm Metab Res. 2009;41(09):687–96.
Li ML, Fitzgerald PA, Price DC, Norton JA. Iatrogenic pheochromocytomatosis: a previously unreported result of laparoscopic adrenalectomy. Surgery. 2001;130(6):1072–7.
Bohle A, Studer UE, Sonntag RW, Scheidegger JR. Primary or secondary extragonadal germ cell tumors? J Urol. 1986;135(5):939–43.
Comiter CV, Renshaw AA, Benson CB, Loughlin KR. Burned-out primary testicular cancer: sonographic and pathological characteristics. J Urol. 1996;156(1):85–8.
Richie JP. Spontaneous regression of testicular germ cell tumors: an analysis of 42 cases. Balzer BL, Ulbright TM, Department of Pathology, Stanford University Hospital and Clinics, Stanford, CA. Urol Oncol. 2007;25(2):171.
Bokemeyer C, Nichols CR, Droz JP, Schmoll HJ, Horwich A, Gerl A, et al. Extragonadal germ cell tumors of the mediastinum and retroperitoneum: results from an international analysis. J Clin Oncol. 2002;20(7):1864–73.
McAleer JJA, Nicholls J, Horwich A. Does extragonadal presentation impart a worse prognosis to abdominal germ-cell tumours? Eur J Cancer. 1992;28(4–5):825–8.
Rajiah P, Sinha R, Cuevas C, Dubinsky TJ, Bush WH, Kolokythas O. Imaging of uncommon retroperitoneal masses. Radiographics. 2011;31(4):949–76.
Tasu J-P, Faye N, Eschwege P, Rocher L, Bléry M. Imaging of burned-out testis tumor. J Ultrasound Med. 2003;22(5):515–21.
Gatcombe HG, Assikis V, Kooby D, Johnstone PAS. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004;86(2):107–13.
Church JM. Mucosal ischemia caused by desmoid tumors in patients with familial adenomatous polyposis: report of four cases. Dis Colon Rectum. 1998;41(5):661–3.
Carlson JW, Fletcher CDM. Immunohistochemistry for β-catenin in the differential diagnosis of spindle cell lesions: analysis of a series and review of the literature. Histopathology. 2007;51(4):509–14.
Aitken SJ, Presneau N, Kalimuthu S, Dileo P, Berisha F, Tirabosco R, et al. Next-generation sequencing is highly sensitive for the detection of beta-catenin mutations in desmoid-type fibromatoses. Virchows Arch. 2015;467(2):203–10.
Fiore M, Rimareix F, Mariani L, Domont J, Collini P, Le Péchoux C, et al. Desmoid-type fibromatosis: a front-line conservative approach to select patients for surgical treatment. Ann Surg Oncol. 2009;16(9):2587–93.
Salas S, Dufresne A, Bui B, Blay JY, Terrier P, Ranchere-Vince D, et al. Prognostic factors influencing progression-free survival determined from a series of sporadic desmoid tumors: a wait-and-see policy according to tumor presentation. J Clin Oncol. 2011;29(26):3553–8.
Burtenshaw SM, Cannell AJ, McAlister ED, Siddique S, Kandel R, Blackstein ME, et al. Toward observation as first-line management in abdominal desmoid tumors. Ann Surg Oncol. 2016;23(7):2212–9.
Arvanitis ML, Jagelman DG, Fazio VW, Lavery IC, McGannon E. Mortality in patients with familial adenomatous polyposis. Dis Colon Rectum. 1990;33(8):639–42.
Nieuwenhuis MH, Mathus-Vliegen EM, Baeten CG, Nagengast FM, Van Der Bijl J, Van Dalsen AD, et al. Evaluation of management of desmoid tumours associated with familial adenomatous polyposis in Dutch patients. Br J Cancer. 2011;104(1):37–42.
Soravia C, Berk T, McLeod RS, Cohen Z. Desmoid disease in patients with familial adenomatous polyposis. Dis Colon Rectum. 2000;43(3):363–9.
Guillem JG, Wood WC, Moley JF, Berchuck A, Karlan BY, Mutch DG, et al. ASCO/SSO review of current role of risk-reducing surgery in common hereditary cancer syndromes. J Clin Oncol. 2006;24(28):4642–60.
Bertagnolli MM, Morgan JA, Fletcher CDM, Raut CP, Dileo P, Gill RR, et al. Multimodality treatment of mesenteric desmoid tumours. Eur J Cancer. 2008;44(16):2404–10.
Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet [Internet]. 2006;367(9506):241–51. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673606680355
Vaglio A, Palmisano A, Alberici F, Maggiore U, Ferretti S, Cobelli R, et al. Prednisone versus tamoxifen in patients with idiopathic retroperitoneal fibrosis: an open-label randomised controlled trial. Lancet. 2011;378(9788):338–46.
Palmisano A, Maritati F, Vaglio A. Chronic periaortitis: an update. Curr Rheumatol Rep. 2018;20(12):80.
Maritati F, Rocco R, Buttini EA, Marvisi C, Nicastro M, Urban ML, et al. Clinical and prognostic significance of serum IgG4 in chronic periaortitis. An analysis of 113 patients. Front Immunol. 2019;10:1–10.
Zen Y, Onodera M, Inoue D, Kitao A, Matsui O, Nohara T, et al. Retroperitoneal fibrosis: a clinicopathologic study with respect to immunoglobulin G4. Am J Surg Pathol. 2009;33(12):1833–9.
Scheel PJ, Feeley N. Retroperitoneal fibrosis: the clinical, laboratory, and radiographic presentation. Medicine (Baltimore). 2009;88(4):202–7.
Palmisano A, Urban ML, Corradi D, Cobelli R, Alberici F, Maritati F, et al. Chronic periaortitis with thoracic aorta and epiaortic artery involvement: a systemic large vessel vasculitis? Rheumatology (Oxford). 2015;54(11):2004–9.
Cavalli G, Guglielmi B, Berti A, Campochiaro C, Sabbadini MG, Dagna L. The multifaceted clinical presentations and manifestations of Erdheim-Chester disease: comprehensive review of the literature and of 10 new cases. Ann Rheum Dis. 2013;72(10):1691–5.
Milne P, Bigley V, Bacon CM, Néel A, McGovern N, Bomken S, et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim-Chester disease in adults. Blood. 2017;130(2):167–75.
Arnaud L, Gorochov G, Charlotte F, Lvovschi V, Parizot C, Larsen M, et al. Systemic perturbation of cytokine and chemokine networks in Erdheim-Chester disease: a single-center series of 37 patients. Blood. 2011;117(10):2783–90.
Serratrice J, Granel B, De Roux C, Pellissier JF, Swiader L, Bartoli JM, et al. “Coated aorta”: a new sign of Erdheim-Chester disease. J Rheumatol. 2000;27(6):1550–3.
Habermann TM, Steensma DP. Lymphadenopathy. Mayo Clin Proc. 2000;75(7):723–32.
Altieri A, Bermejo JL, Hemminki K. Familial risk for non-Hodgkin lymphoma and other lymphoproliferative malignancies by histopathologic subtype: the Swedish Family-Cancer Database. Blood. 2005;106(2):668–72.
Smedby KE, Hjalgrim H, Askling J, Chang ET, Gregersen H, Porwit-MacDonald A, et al. Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst. 2006;98(1):51–60.
Wang SS, Slager SL, Brennan P, Holly EA, De Sanjose S, Bernstein L, et al. Family history of hematopoietic malignancies and risk of non-Hodgkin lymphoma (NHL): a pooled analysis of 10 211 cases and 11 905 controls from the International Lymphoma Epidemiology Consortium (InterLymph). Blood. 2007;109(8):3479–88.
Clarke CA, Morton LM, Lynch C, Pfeiffer RM, Hall EC, Gibson TM, et al. Risk of lymphoma subtypes after solid organ transplantation in the United States. Br J Cancer. 2013;109(1):280–8.
Luo D, Zhou T, Tao Y, Feng Y, Shen X, Mei S. Exposure to organochlorine pesticides and non-Hodgkin lymphoma: a meta-analysis of observational studies. Sci Rep. 2016;6:1–11.
Zhang Y, De Sanjose S, Bracci PM, Morton LM, Wang R, Brennan P, et al. Personal use of hair dye and the risk of certain subtypes of non-Hodgkin lymphoma. Am J Epidemiol. 2008;167(11):1321–31.
Wang F, Xu RH, Han B, Shi YX, Luo HY, Jiang WQ, et al. High incidence of hepatitis B virus infection in B-cell subtype non-Hodgkin lymphoma compared with other cancers. Cancer. 2007;109(7):1360–4.
Fallah M, Liu X, Ji J, Försti A, Sundquist K, Hemminki K. Autoimmune diseases associated with non-Hodgkin lymphoma: a nationwide cohort study. Ann Oncol. 2014;25(10):2025–30.
Larsson SC, Wolk A. Body mass index and risk of non-Hodgkin’s and Hodgkin’s lymphoma: a meta-analysis of prospective studies. Eur J Cancer. 2011;47(16):2422–30.
Anderson T, Chabner BA, Young RC, Berard CW, Garvin AJ, Simon RM, et al. Malignant lymphoma. 1. The histology and staging of 473 patients at the National Cancer Institute. Cancer. 1982;50(12):2699–707.
Sriwatanawongsa V, Cardoso R, Chang P. Incidence of malignancy in peripheral lymph node biopsy. Am Surg. 1985;51(10):587–90.
Hehn ST, Grogan TM, Miller TP. Utility of fine-needle aspiration as a diagnostic technique in lymphoma. J Clin Oncol. 2004;22(15):3046–52.
Lachar WA, Shahab I, Saad AJ. Accuracy and cost-effectiveness of core needle biopsy in the evaluation of suspected lymphoma: a study of 101 cases. Arch Pathol Lab Med. 2007;131(7):1033–9.
Asoglu O, Porter L, Donohue JH, Cha SS. Laparoscopy for the definitive diagnosis of intra-abdominal lymphoma. Mayo Clin Proc. 2005;80(5):625–31.
Barrington SF, Mikhaeel NG, Kostakoglu L, Meignan M, Hutchings M, Müeller SP, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the international conference on malignant lymphomas imaging working group. J Clin Oncol. 2014;32(27):3048–58.
Choi SM, O’Malley DP. Diagnostically relevant updates to the 2017 WHO classification of lymphoid neoplasms. Ann Diagn Pathol. 2018;37:67–74.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–67.
Talat N, Belgaumkar AP, Schulte KM. Surgery in Castleman’s disease: a systematic review of 404 published cases. Ann Surg. 2012;255(4):677–84.
Yu L, Tu M, Cortes J, Xu-Monette ZY, Miranda RN, Zhang J, et al. Clinical and pathological characteristics of HIV-and HHV-8-negative Castleman disease. Blood. 2017;129(12):1658–68.
Kishimoto T. IL-6: from its discovery to clinical applications. Int Immunol. 2010;22(5):347–52.
Murakami M, Johkoh T, Hayashi S, Ohshima S, Mizuki M, Nakatsuka S, et al. Clinicopathologic characteristics of 342 patients with multicentric Castleman disease in Japan. Mod Rheumatol. 2020;30(5):843–51.
Liu AY, Nabel CS, Finkelman BS, Ruth JR, Kurzrock R, van Rhee F, et al. Idiopathic multicentric Castleman’s disease: a systematic literature review. Lancet Haematol. 2016;3(4):e163–75.
Fajgenbaum DC, Uldrick TS, Bagg A, Frank D, Wu D, Srkalovic G, et al. International, evidence-based consensus diagnostic criteria for HHV-8-negative/idiopathic multicentric Castleman disease. Blood. 2017;129:1646–57.
Naddaf E, DIspenzieri A, Mandrekar J, Mauermann ML. Clinical spectrum of Castleman disease-associated neuropathy. Neurology. 2016;87(23):2457–62.
Abla O, Jacobsen E, Picarsic J, Krenova Z, Jaffe R, Emile JF, et al. Consensus recommendations for the diagnosis and clinical management of Rosai-Dorfman-Destombes disease. Blood. 2018;131:2877–90.
Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol. 1990;7(1):19–73.
Sodhi KS, Suri S, Nijhawan R, Kang M, Gautam V. Rosai-Dorfman disease: unusual cause of diffuse and massive retroperitoneal lymphadenopathy. Br J Radiol. 2005;78(933):845–7.
Krishnan A, Nassar A, Nieh PT. Rosai-Dorfman disease presenting as extranodal renal mass. Urology. 2005;66(6):1319.e17–9.
Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366(6):539–51.
Kamisawa T, Zen Y, Pillai S, Stone JH. Review IgG4-related disease. Lancet. 2015;385(9976):1460–71.
Deshpande V, Zen Y, Chan JKC, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181–92.
Chen G, Cheuk W, Chan JKC. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Chin J Pathol. 2010;39(12):851–68.
Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis. 2015;74(1):14–8.
Cheuk W, Yuen HKL, Chu SYY, Chiu EKW, Lam LK, Chan JKC. Lymphadenopathy of IgG4-related sclerosing disease. Am J Surg Pathol. 2008;32(5):671–81.
Neild GH, Rodriguez-Justo M, Wall C, Connolly JO. Hyper-IgG4 disease: report and characterisation of a new disease. BMC Med. 2006;4:1–18.
Stone JR. Aortitis, periaortitis, and retroperitoneal fibrosis, as manifestations of IgG4-related systemic disease. Curr Opin Rheumatol. 2011;23(1):88–94.
Hirano K, Tada M, Sasahira N, Isayama H, Mizuno S, Takagi K, et al. Incidence of malignancies in patients with IgG4-related disease. Intern Med. 2014;53(3):171–6.
Wallace ZS, Wallace CJ, Lu N, Choi HK, Stone JH. Association of IgG4-related disease with history of malignancy. Arthritis Rheumatol. 2016;68(9):2283–9.
Hegade VS, Sheridan MB, Huggett MT. Diagnosis and management of IgG4-related disease. Frontline Gastroenterol. 2019;10(3):275–83.
Sharma SK, Mohan A, Sharma A, Mitra DK. Miliary tuberculosis: new insights into an old disease. Lancet Infect Dis. 2005;5(7):415–30.
Selwyn PA, Hartel D, Lewis VA, Schoenbaum EE, Vermund SH, Klein RS, et al. A prospective study of the risk of tuberculosis among intravenous drug users with human immunodeficiency virus infection. N Engl J Med. 1989;320(9):545–50.
Atomiya AN, Uip DE, Leite OHM. Evaluation of disease patterns, treatment and prognosis of tuberculosis in AIDS patient. Braz J Infect Dis. 2002;6(1):29–39.
Hill AR, Premkumar S, Brustein S, Vaidya K, Powell S, Li PW, et al. Disseminated tuberculosis in the acquired immunodeficiency syndrome era. Am Rev Respir Dis. 1991;144(5):1164–70.
Artenstein AW, Kim JH, Williams WJ, Chung RCY. Isolated peripheral tuberculous lymphadenitis in adults: current clinical and diagnostic issues. Clin Infect Dis. 1995;20(4):876–82.
Fontanilla JM, Barnes A, Von Reyn CF. Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis. 2011;53(6):555–62.
Baydur A. The spectrum of extrapulmonary tuberculosis. West J Med. 1977;126(4):253–62.
Yang ZG, Min PQ, Sone S, He ZY, Liao ZY, Zhou XP, et al. Tuberculosis versus lymphomas in the abdominal lymph nodes: evaluation with contrast-enhanced CT. Am J Roentgenol. 1999;172(3):619–23.
Levy AD, Remotti HE, Thompson WM, Sobin LH, Miettinen M. From the archives of the AFIP. Radiographics. 2003;23(2):283–304.
Shaaban AM, Rezvani M, Tubay M, Elsayes KM, Woodward PJ, Menias CO. Fat-containing retroperitoneal lesions: imaging characteristics, localization, and differential diagnosis. Radiographics. 2016;36(3):710–34.
Hamer OW, Aguirre DA, Casola G, Lavine JE, Woenckhaus M, Sirlin CB. Fatty liver: imaging patterns and pitfalls. Radiographics. 2006;26(6):1637–53.
Messiou C, Moskovic E, Vanel D, Morosi C, Benchimol R, Strauss D, et al. Primary retroperitoneal soft tissue sarcoma: imaging appearances, pitfalls and diagnostic algorithm. Eur J Surg Oncol [Internet]. 2017;43(7):1191–8. Available from: https://doi.org/10.1016/j.ejso.2016.10.032
Ganeshalingam S, Rajeswaran G, Jones RL, Thway K, Moskovic E. Leiomyosarcomas of the inferior vena cava: diagnostic features on cross-sectional imaging. Clin Radiol. 2011;66(1):50–6.
Chick JFB, Chauhan NR, Madan R. Solitary fibrous tumors of the thorax: nomenclature, epidemiology, radiologic and pathologic findings, differential diagnoses, and management. Am J Roentgenol. 2013;200(3):W238–48.
Shanbhogue AK, Prasad SR, Takahashi N, Vikram R, Zaheer A, Sandrasegaran K. Somatic and visceral solitary fibrous tumors in the abdomen and pelvis: cross-sectional imaging spectrum. Radiographics. 2011;31(2):393–408.
Rosenkrantz AB, Hindman N, Melamed J. Imaging appearance of solitary fibrous tumor of the abdominopelvic cavity. J Comput Assist Tomogr. 2010;34(2):201–5.
Zhanlong M, Haibin S, Xiangshan F, Jiacheng S, Yicheng N. Variable solitary fibrous tumor locations: CT and MR imaging features. Medicine (Baltimore). 2016;95(13):e3031.
Luo L, Zheng X, Tao KZ, Zhang J, Tang YY, Han FG. Imaging analysis of ganglioneuroma and quantitative analysis of paraspinal ganglioneuroma. Med Sci Monit. 2019;25(3671):5263–71.
Ilias I, Pacak K. Current approaches and recommended algorithm for the diagnostic localization of pheochromocytoma. J Clin Endocrinol Metab. 2004;89(2):479–91.
Mannelli M, Colagrande S, Valeri A, Parenti G. Incidental and metastatic adrenal masses. Semin Oncol. 2010;37(6):649–61.
Shulkin BL, Ilias I, Sisson JC, Pacak K. Current trends in functional imaging of pheochromocytomas and paragangliomas. Ann N Y Acad Sci. 2006;1073:374–82.
Azizi L, Balu M, Belkacem A, Lewin M, Tubiana J-M, Arrivé L. MRI features of mesenteric desmoid tumors in familial adenomatous polyposis. Am J Roentgenol. 2005;184(4):1128–35.
Lee JC, Thomas JM, Phillips S, Fisher C, Moskovic E. Aggressive fibromatosis: MRI features with pathologic correlation. Am J Roentgenol. 2006;186(1):247–54.
Madan R, Chen JH, Trotman-Dickenson B, Jacobson F, Hunsaker A. The spectrum of Castleman’s disease: mimics, radiologic pathologic correlation and role of imaging in patient management. Eur J Radiol. 2012;81(1):123–31.
Lahat G, Madewell JE, Anaya DA, Qiao W, Tuvin D, Benjamin RS, et al. Computed tomography scan-driven selection of treatment for retroperitoneal liposarcoma histologic subtypes. Cancer. 2009;115(5):1081–90.
Wilkinson MJ, Martin JL, Khan AA, Hayes AJ, Thomas JM, Strauss DC. Percutaneous core needle biopsy in retroperitoneal sarcomas does not influence local recurrence or overall survival. Ann Surg Oncol. 2015;22(3):853–8.
Nishinari K, Yazbek G, Malavolta LC, Ferreira FO, Lopes A. Resection of retroperitoneal sarcoma with reconstruction of the infra-renal aorta and vena cava using temporary bypass: a case report. J Pelvic Med Surg. 2002;8:259–64.
Teixeira FJR, Netto SDC, Perina ALF, Torricelli FCM, Teixeira LR, Zerati AE, et al. Leiomyosarcoma of the inferior vena cava: survival rate following radical resection. Oncol Lett. 2017;14(4):3909–16.
Serrano C, Georges S. Leiomyosarcoma. Hematol Oncol Clin North Am. 2013;27(5):957–74.
Wibmer C, Leithner A, Zielonke N, et al. Increasing incidence rates of soft tissue sarcomas? A population-based epidemiologic study and literature review. Ann Oncol. 1994;21(5):1106–11.
Kieffer E, Aoui M, Piette JC, et al. Leiomyosarcoma of the inferior vena cava: experience in 22 cases. Ann Surg. 2006;244:289–95.
Dzsinich C, Gloviczki P, van Heerden JA, et al. Primary venous leiomyosarcoma: a rare but lethal disease. J Vasc Surg. 1992;15:595–603.
Howlader N, Noone AM, Yu M, Cronin KA. Use of imputed population-based câncer registry data as a method of accounting for missing information: application to estrogen receptor status for breast câncer. Am J Epidemiol. 2012;176(4):347–56.
Teixeira FJR Jr, do Couto Netto SD, Perina ALF, Torricelli FCM, Ragazzo Teixeira L, Zerati AE, et al. Leiomyosarcoma of the inferior vena cava: survival rate following radical resection. Oncol Lett. 2017;14(4):3909–16.
Wachtel H, Gupta M, Bartlett EK, et al. Outcomes after resection of leiomyosarcomas of the inferior vena cava: a pooled data analysis of 377 cases. Surg Oncol. 2015;24(1):21–7.
Hollenbeck ST, Grobmyer SR, Kent KC, et al. Surgical treatment and outcomes of patients with primary inferior vena cava leiomyosarcoma. J Am Coll Surg. 2003;197:575–9.
Azoulay D, Lim C, Salloum C, editors. Surgery of the inferior vena cava. A multidisciplinary approach. Springer; 2017.
Dull BZ, Smith B, Tefera G, et al. Surgical management of retroperitoneal leiomyosarcoma arising from the inferior vena cava. J Gastrointest Surg. 2013;17(12):2166–71.
Laskin WB, Fanburg-Smith JC, Burke AP, et al. Leiomyosarcoma of the inferior vena cava: clinicopathologic study of 40 cases. Am J Surg Pathol. 2010;34(6):873–81.
Fiore M, Colombo C, Locati P, et al. Surgical technique, morbidity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava. Ann Surg Oncol. 2012;19(2):511–8.
Hartman DS, Hayes WS, Choyke PL, et al. Leiomyosarcoma of the retroperitoneum and the inferior vena cava: radiologic and pathologic correlation. Radiographics. 1992;12:1203–20.
Webb EM, Wang ZJ, Westphalen AC, et al. Can CT features differentiate between inferior vena cava leiomyosarcomas and primary retroperitoneal masses? AJR Am J Roentgenol. 2013;200(1):205–9.
Nishinari K, Valentim LA, Yazbek G, et al. Concomitant aortic and vena caval reconstruction associated with germ-cell tumor resection with creation of a new venous bifurcation. J Vasc Surg Venous Lymphat Disord. 2013;1(2):209–11.
Krutman M, Nishinari K, Pignataro BS, Yazbek G, Zottele Bomfim GA, Cavalcante RN, Centofanti G, Imagawa Fonseca IY, Passos Teivelis M. Twenty years of experience in vascular reconstructions associated with resection of malignant neoplasms in a single cancer center. J Vasc Surg. 2019;69(6):1880–8.
Nishinari K, Wolosker N, Yazbek G, Zerati AE, et al. Arterial reconstructions associated with the resection of malignant tumors. Clinics. 2006;61(4):339–44.
Hünerbein M, Hohenberger P, Stroszczynski C, et al. Resection of soft tissue sarcoma of the lower limb after evaluation of vascular invasion with intraoperative intravascular ultrasonography. Br J Surg. 2007;94(2):168–73.
Larena-Avellaneda A, Timm S, Kickuth R, Kenn W, Steger U, Jurowich C, Germer CT. Intraarterial ultrasound in pancreatic cancer: feasibility study and preliminary results. Cardiovasc Intervent Radiol. 2010;33(4):726–31.
Zerati AE, Nishinari K, Yazbek G, Wolosker N, Fonseca FP. Abdominal aortic pseudoaneurysm associated with a metastatic germ cell tumor: a rare complication. Clinics (Sao Paulo). 2007;62(5):657–60.
Nishinari K, Wolosker N, Yazbek G, Nakagawa WT, Lopes A. Idiopathic aneurysm of inferior vena cava associated with retroperitoneal ganglioneuroma: case report. J Vasc Surg. 2003;37(4):895–8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Editor’s Comments
Editor’s Comments
Retroperitoneum tumors often require the vascular surgeon’s participation in surgical treatment, either in the rare primary vascular tumors or in tumors involving large vessels or trunk vessels.
1.1 Leiomyosarcoma of the Vein Cava
Leiomyosarcoma (LMS) is the histological type most associated with large vessels’ primary tumors, with the inferior vena cava (IVC) being the most frequent location, representing 0.5% of soft tissue sarcomas in adults [213, 214]. Its prognosis is reserved, with 5-year survival after tumor resection between 25% and 50% [215,216,217,218]. Surgical resection is the only chance of cure for patients with this diagnosis.
LMS mainly affects middle-aged or elderly individuals, with female predominance (3:1) when the LMS is primary in the vena cava [219].
1.2 Localization
For classification concerning location, the IVC is divided into three segments: segment I (lower) – below the renal veins; segment II (medium) – from the renal veins to the retrohepatic vena cava; segment III (superior) – from the hepatic veins to the right atrium. About 80% of the tumors originate in segments I and II (with a slight predominance in the last) and only 20% in segment III [215, 216, 220]. The tumor may be present in more than one segment concomitantly.
1.3 Signals and Symptoms
Abdominal pain is a nonspecific symptom, but it is frequent [221]. Lower limb edema is a sign found in about 1/3 of the patients since the slow growth of the tumor favors the development of collateral circulation that reduces the clinical repercussion of IVC obstruction. Often, edema results from deep venous thrombosis in the lower limbs, being a more frequent sign in tumors located in segment I. Tumors of segment II can cause nephrotic syndrome due to obstruction of renal venous drainage. Tumors located in the upper segment, on the other hand, can impair drainage through the hepatic veins, causing hepatomegaly, jaundice, and ascites, in addition to a higher risk of pulmonary embolism [215, 216, 219, 220, 222,223,224].
IVC LMS may have extraluminal, endoluminal, or both growth, with the first being the most frequent (about 62% of cases) and the endoluminal being the rarest (5% of cases) [225]. Extraluminal growth can cause symptoms by compression or invasion of adjacent structures, such as stomach and duodenum.
The most frequent sites of metastases are the liver and lungs. Cachexia is a sign that can accompany patients with advanced disease.
1.4 Diagnosis
Computed tomography shows a tumor with an irregular, lobulated shape, which may partially obstruct the IVC lumen. Tumor necrosis and hemorrhage generate a heterogeneous aspect of the tumor mass. Since it provides greater tissue resolution, magnetic resonance imaging tends to be more useful in diagnosing the origin of the tumor and planning surgical treatment. Differential diagnosis with kidney tumors, lymphoma, and liposarcoma can be difficult. Webb et al. demonstrated that IVC light was imperceptible in 75% of patients with IVC LMS, which did not occur in tumors of another nature [226].
An echocardiogram is useful in segment III tumors to assess the extent of the tumor to the atrium.
PET-CT is an option to investigate images suspected of metastasis, a situation in which percutaneous biopsy may be necessary to assess a possible indication for neoadjuvant palliative therapy.
1.5 Staging
The staging of the LCI of the IVC obeys the TNM classification: TX – nonaccessible primary tumor; T1 – tumor ≤5 cm in the most extensive measure; T2 – tumor >5 cm in the most extensive measure; N0 – without evidence of positive lymph nodes; N1 – with evidence of positive lymph nodes; M0 – without metastasis; M1 – with metastasis [221].
The classification according to the degree of differentiation adopted is proposed by the French Federation Nationale des Centers de Lutte Contre le Cancer (FNCLCC), based on differentiation (score 1–3, depending on the differentiation of mesenchymal tissue), on the number of mitoses (score 1–3, depending on the number of mitoses per 10 high magnification fields – 10 high power field), and in the presence of tumor necrosis (score 1–3, depending on the presence of tumor necrosis). This histological classification is determined as Grade 1 for total score 2–3; Grade 2, total score 4–5; and Grade 3, total score 6–8 [221].
1.6 Treatment
Treatment consists of resection of the IVC segment affected by the tumor en bloc with neighboring tissues or organs that may be affected. Information regarding chemotherapy and radiotherapy is scarce, both as adjuvant and neoadjuvant therapy, and chemoradiotherapy may be an option in particular situations such as complementary or palliative treatment [218, 221].
The IVC approach depends on the segment of origin of the tumor, the extension of the involved vascular wall (partial or circumferential), and the venous collateral circulation development.
A ligature is an option described in the treatment of tumors in segment I. However, resection of the tumor may compromise a previously efficient collateral circulation so that the editors prefer, whenever possible, to reconstruct the circulation through the inferior vena cava. Extensive venous thrombosis downstream or upstream can prevent the reconstruction of venous flow.
In cases of small tumors that involve less than 75% of the lumen and without infiltration of adjacent organs, partial resection of the IVC and reconstruction with a patch may be an option. The choice for a patch depends on the extent of the affected IVC and eventual contamination of the surgical bed that can occur when invasion and resection of organs of the gastrointestinal tract take place. In the latter case, autologous substitutes such as the saphenous vein or the external jugular vein are preferred. Heterologous substitutes (cadaver veins) have more restricted use due to less availability. Primary raffia, without a patch, can also be an option, as long as the suture is not done under tension. Bovine pericardium graft and synthetic vascular prostheses, both Dacron and PTFE (expanded polytetrafluoroethylene), are also options, especially in cases of more extensive circumferential involvement.
When there is a need to resect a segment of the VCI, the bypass with Dacron or PTFE is the option. The preference in venous reconstructions is for the use of reinforced PTFE. The making of arteriovenous fistula, to increase the patency of venous reconstruction, is less and less performed [220].
Reconstruction of the renal vein is always desirable, especially of the left renal vein when the right kidney is resected en bloc with the tumor.
1.7 Retroperitoneal Tumors with Vascular Involvement
Retroperitoneum tumors usually cause few symptoms in the early stages, so they are often diagnosed already quite bulky and often involving vascular structures [227]. Vascular reconstruction can transform unresectable tumors into resectable ones so that the involvement of arteries and veins no longer represents a contraindication for tumor resection [228, 229]. The involvement may be of trunk (visceral) vessels or the great vessels of the retroperitoneum (vena cava and aorta), either by invasion or by circumferential involvement (see Chap. 13).
Computed tomography and nuclear magnetic resonance show possible vessel entrapment by the tumor mass. However, when there is intimate contact, it may fail to differentiate this contact by proximity, which does not prevent the preservation of vessels from vascular invasion itself, which could require en bloc resection and vascular reconstruction. In some situations, intravascular ultrasound (IVUS) can increase the accuracy of vascular invasion diagnosis [230, 231]. The need for vascular reconstruction, however, is often defined only with intraoperative findings. Doppler ultrasound can help assess the caliber and patency of vessels potentially eligible as substitutes (e.g., internal saphenous vein).
Reconstruction techniques, as discussed above in the VCI LMS, include patchmaking – when the vessel wall is partially resected in its circumference, bridges – when a segment of the vessel is removed en bloc with the tumor, in addition to the primary anastomosis end-to-end if there is no tension in the suture to approach the stumps. A ligature is an alternative in treating nonvital vessels for nutrition or venous drainage of a specific organ or tissue or if a venous segment presents with proximal and/or distal thrombosis to the segment removed en bloc with the tumor.
Arterial substitutes can be autologous (internal and external saphenous veins, femoral veins, internal and external jugular veins, upper limb veins, radial artery, hypogastric artery), normally used in the reconstruction of visceral branches and situations of contamination of the surgical bed. Among the synthetic substitutes, the main ones are the Dacron and PTFE vascular prostheses, essential in treating larger caliber vessels. Heterologous vessels (from cadaver donors) are a less available alternative in most centers. Reinforced PTFE is preferred for venous reconstructions and when the bridge exceeds joints. Patches can be made with autologous substitutes and bovine pericardium foil, in addition to the aforementioned synthetic material.
Reinforced PTFE prostheses with a suitable caliber for IVC reconstruction are rarely available in our country. The creation of a new IVC bifurcation is a relatively simple technique that allows the use of a smaller caliber prosthesis [227].
Concerning the surgical time, the ideal is that the vessels be connected, after systemic anticoagulation, as the last act before the en bloc removal of the tumor, followed by vascular reconstruction. If the artery and vein have to be reconstructed, the first is done before the second to minimize ischemia time. When vascular ligation is necessary before the tumor is fully mobilized, the artery and vein receive bridges with long vascular prostheses proximally and distally to the segment affected by the neoplasia, allowing vascular ligation and the sequence the oncological time. After the dissection, the tumor is removed en bloc, and the bridges are shortened (Figs. 7.45 and 7.46 of Chap. 7).
Whenever possible, patients who have received venous bridges are kept on full anticoagulation for a minimum of 6 months. Regardless of the substitute used, exclusive arterial reconstruction does not require full anticoagulation in the postoperative period.
Results of the patency of reconstructions are found in Chap. 13.
1.8 Other Situations That Require Vascular Intervention
Rare cases of aortic pseudoaneurysm after chemotherapy in patients with germinal tumors and large retroperitoneal masses have been described (see comments in Chap. 4) [232]. These pseudoaneurysms occur when there is tumor invasion in the aortic wall and are attributed to tumor necrosis following treatment chemotherapy, including neoplastic cells that inhabit the arterial wall [232]. The treatment can be reconstruction with a synthetic vascular prosthesis in the same surgical procedure as the en bloc resection of the tumor or, in case of rupture, endovascular treatment with an endoprosthesis implant can be an alternative [232].
Venous aneurysms are very uncommon. A rare case of idiopathic infrarenal vena cava sac aneurysm has been described in association with a retroperitoneum ganglioneuroma, treated with sacculation resection and primary raffia of the lateral wall of the vena cava in the same act of tumor resection [233].
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
de Oliveira Ferreira, F. (2022). Retroperitoneal Tumors. In: Zerati, A.E., Nishinari, K., Wolosker, N. (eds) Vascular Surgery in Oncology. Springer, Cham. https://doi.org/10.1007/978-3-030-97687-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-97687-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-97686-6
Online ISBN: 978-3-030-97687-3
eBook Packages: MedicineMedicine (R0)