Abstract
The past 35 years, beginning with the identification of ZO-1 in 1986, have been an exciting time during which critical tight junction proteins were discovered. We have, however, only begun to define the mechanism by which tight junctions are regulated, their impact on health and disease, and noncanonical functions of individual tight junction-associated proteins. Here, we provide an overview of advances in understanding mechanisms of tight junction barrier regulation within the intestinal epithelium and discuss recent discoveries related to claudin-2 and occludin in greater detail. We anticipate that the next 35 years will yield major advances in fundamental understanding of tight junction protein interactions, regulation, and canonical and noncanonical functions that result in translational applications in which tight junction modulation is established as a therapeutic approach.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intestinal permeability
- Intestinal barrier
- Tumor necrosis factor
- IL-13
- IL-22
- Inflammatory bowel disease
- Tight junction
Introduction
The viability of multicellular life forms requires the presence of barrier-forming tissues that partition distinct compartments within the organism and separate the external environment from the internal milieu. In mammals, examples of surfaces that interact with the external environment include the skin as well as oral, gastrointestinal, and genitourinary mucosae. At each of these sites, the tight junction creates a selectively permeable seal that restricts flux across the paracellular space between cells. Tight junctions in the skin are nearly impermeant, and, in burn patients, the extent of epidermal barrier loss is a strong prognostic indicator of outcome. The gastrointestinal epithelium, particularly within the distal gut, interfaces with a dense and complex luminal microbiome that can include invasive pathogens as well as potentially harmful bacterial components and metabolites. Dysregulated systemic exposure to these luminal materials, which could lead to immune-mediated, metabolic, and infectious diseases, emphasizes the essential nature of the intestinal epithelial barrier. However, in contrast to the skin, the intestinal barrier must allow paracellular flux of water, ions, and nutrients. The charge and size selectivity of this barrier are determined by the tight junction, which is the rate-limiting step in paracellular flux.
Tight Junctions Are Regulated by Pharmacological and Physiological Stimuli
Farquhar’s descriptions of the tight junction and apical junctional complex were remarkably consistent across samples and tissues [1]. Together with other data, this led many to conclude that tight junctions are static structures with unchanging permeabilities. Ussing’s report [2], only 1 year after Farquhar’s landmark publication, that application of an osmotic gradient could markedly increase paracellular flux across was interpreted as tight junction disassembly. Subsequent studies showing that osmotic gradients reduced [3], while phalloidin and proliferative stimuli increased [4, 5], the complexity of strand networks were generally dismissed as non-physiological. This changed in 1987 when Pappenheimer et al. published a series of papers demonstrating that increased intestinal epithelial tight junction permeability was a physiological response to Na+-nutrient cotransport [6,7,8]. These first studies showing physiological tight junction regulation also led to the discovery of “solvent drag” [8,9,10], a mechanism by which paracellular flux allows continued nutrient absorption despite saturation of transcellular transport pathways. Although initially controversial [11,12,13,14,15], subsequent in vitro and in vivo studies demonstrated that solvent drag occurs in many species, including humans [16, 17], as a result of increased paracellular permeability [18,19,20]. Subsequent work has documented similar paracellular amplification of transcellular transport in the renal tubule [21, 22].
Ex vivo studies of rodent mucosae showed that Na+-nutrient cotransport-induced tight junction permeability increases were associated with morphological changes including expansion of spaces between tight junction strands and condensation of perijunctional microfilaments [6]. This led to the hypothesis that actomyosin contraction might contribute to Na+-nutrient cotransport-induced tight junction regulation. However, methods available at that time precluded mechanistic analysis in intact mucosae. This obstacle was overcome by the development of a cell culture model of intestinal epithelial tight junction regulation in response to Na+-glucose cotransport [23]. Using a model facilitated the discovery that actomyosin contraction driven by myosin light chain kinase (MLCK)-mediated phosphorylation of myosin II regulatory light chain (MLC) was essential for physiological tight junction regulation. Moreover, enzymatic MLCK inhibition blocked Na+-glucose cotransport-induced tight junction regulation in cultured monolayers and isolated rodent mucosae [23]. Subsequent studies showed that Na+-glucose cotransport led to increased tight junction permeability and MLC phosphorylation in human intestinal mucosae [19]. Importantly, both in vitro and in vivo studies showed that these alterations were size selective in that mannitol (~7 Å diameter) permeability was increased, but there were no detectable changes in paracellular inulin (30–40 Å diameter) flux [20, 23]. Thus, MLCK activation by physiological stimuli is a canonical mechanism of epithelial tight junction regulation.
Tight Junctions Are Differentially Regulated by Inflammatory Stimuli
The discovery of MLCK as the mediator of Na+-glucose cotransport-induced permeability increases provided the first mechanistic insight into physiological tight junction regulation. This also created opportunities to discover mechanisms of pathophysiological barrier regulation. Of these, the most well-established is the discovery that MLCK also mediates tight junction regulation induced by proinflammatory cytokines, including TNF, LIGHT, and IL-1β [24,25,26]. The efficacy of anti-TNF therapies and their ability to restore barrier function in patients highlights the clinical relevance of this discovery, although efficacy is more likely due to immunomodulation [27, 28]. Experimentally, barrier loss induced by TNF was completely reversed by a specific membrane-permeant inhibitor of MLCK (PIK). MLC phosphorylation, which was increased following TNF treatment, was also corrected by PIK [29]. PIK was, however, only able to restore barrier function in response to modest degrees of barrier loss [29], indicating that the effect was due to reversal of TNF-induced tight junction regulation rather than inhibition of TNF-induced apoptosis [30,31,32,31,]. Moreover, PIK or genetic epithelial MLCK inhibition each prevented acute, TNF-induced barrier loss and diarrhea in vivo [33]. Further, epithelial MLC phosphorylation and MLCK expression were found to be increased in human inflammatory bowel disease and to correlate with disease activity [34]. Thus, TNF and more complex inflammatory stimuli hijack physiological mechanisms of tight junction regulation to increase intestinal permeability. There are, however, differences between tight junction regulation by physiological Na+-glucose cotransport and that induced by TNF in that only TNF increases permeability of molecules larger than small sugars [23, 30]. Thus, although both are driven by MLCK, the barrier loss induced by TNF is qualitatively different from that induced by Na+-glucose cotransport. This may reflect a second signal induced by TNF, as TNF, but not Na+-glucose cotransport, triggers occludin endocytosis in vivo [33, 34].
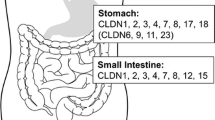
Once claudins were discovered and antibodies became available, several groups began to assess patterns of expression in health and disease [35,36,37,38]. These demonstrated markedly increased claudin-2 expression during active inflammatory bowel disease and showed that IL-13, which is elevated in both ulcerative colitis and Crohn’s disease, was able to induce claudin-2 expression in cultured intestinal epithelial monolayers [36, 37]. Further study showed that, although IL-13, like TNF, reduced transepithelial electrical resistance (TER), only TNF increased paracellular permeability to 4 kDa dextran (28 Å diameter) and reduced charge selectivity [39]. In contrast to TNF, IL-13-induced barrier loss, was due to a claudin-2-mediated increase in paracellular Na+ permeability and was unaffected by PIK [39]. In vivo studies confirmed that IL-13 was sufficient to increase cation permeability, and subsequent studies demonstrated that IL-13 was unable to affect paracellular permeability of claudin-2 knockout mice, while transgenic claudin-2 overexpression was sufficient to replicate the effects of IL-13 in the absence of cytokine treatment [40]. These data demonstrated that the IL-13 and TNF modify paracellular permeability by different mechanisms, claudin-2 upregulation and MLCK activation, respectively, that have distinct functional effects.
Distinct Tight Junction Pore and Leak Pathways
In parallel with the studies above, analyses of genetically modified MDCK monolayers showed that claudin-2 expression increased paracellular permeability of small molecules across pores with diameter of ~8 Å but had no effect on paracellular flux of larger probes [41]. In contrast, knockdown of either ZO-1 or occludin increased paracellular permeability to larger macromolecules [42, 43]. Specifically, occludin knockdown increased flux across a pathway that accommodates macromolecules up to ~125 Å in diameter [43]. Thus, TNF treatment or occludin knockdown increased macromolecular permeability and reduced charge selectivity, while IL-13 treatment or claudin-2 overexpression increased cation selectivity without affecting macromolecular permeability. This confluence of observations led to the hypothesis that two distinct pathways, termed pore and leak, mediate paracellular flux (Fig. 1) [44, 45]. The pore pathway, exemplified by claudin-2 channels, is a high-conductance route that is both charge- and size-selective, with a maximum diameter of 6 to 8 Å. The low-capacity leak pathway is size-selective, with an estimated maximum diameter of 100 to 125 Å and is not charge-selective. In contrast to the pore pathway, which is created by claudin-based, gated channels [46], the anatomy of the leak pathway has not been defined; some have suggested that leak pathway flux may occur primarily at tricellular tight junctions [47].
The intestinal barrier. The space between epithelial cells is sealed by selectively permeable tight junctions that allow paracellular flux by two distinct pathways. The pore pathway (left) is a size- and charge-selective, high-conductance pathway that accommodates molecules up to 6–8 Å in diameter. Upregulation of claudin-2, which forms paracellular channels, increases pore pathway permeability. The mucosal immune system can induce claudin-2 transcription via IL-13 or IL-22 secretion. The leak pathway (center) is a charge-nonselective, low-capacity macromolecular flux route that accommodates molecules up to 100–125 Å in diameter. TNF and IL-1β are each able to increase leak pathway permeability by upregulating myosin light chain kinase (MLCK) expression and activity and recruiting the MLCK1 splice variant to the perijunctional actomyosin ring. This triggers removal of occludin by caveolar endocytosis and leads to increased leak pathway flux. A potential third route, the unrestricted pathway (right panel), is tight junction-independent, size-nonselective, and charge-nonselective. It is created by epithelial damage and can become the dominant route of intestinal barrier loss
The increases in intestinal epithelial tight junction permeability induced by Na+-nutrient cotransport to amplify transcellular nutrient absorption are charge-nonselective, permit flux of molecules too large to traverse claudin channels, and are regulated by the cytoskeleton [8, 19, 23, 48]. These changes, therefore, reflect leak pathway flux. In an analogous fashion, claudin-2-mediated pore pathway flux allows paracellular Na+ absorption to amplify transcellular Na+ absorption in the renal proximal tubule [21]. Thus, defined flux across both pore and leak pathways is of physiological benefit.
Claudin-2: A Paracellular Cation and Water Channel
In normal human and rodent development, intestinal epithelial claudin-2 expression is highest in the immediate perinatal period, where it is expressed in villous and crypt epithelial cells [35, 49, 50]. Claudin-2 expression is then progressively downregulated until, by weaning, expression is low and restricted to crypt epithelial cells [35, 49, 50]. Claudin-15, which also forms a paracellular cation and water channel [51,52,53,54,55], has a reciprocal temporal expression pattern and is present at low levels prior to weaning but is expressed at higher levels in both villous and crypt epithelia by adulthood [35, 49, 50].
Although the reasons for developmental regulation of claudin-2 expression have not been defined, it may reflect differences in nutrient demand, which is greatest during the rapid growth that characterizes the neonatal and pre-weaning periods. This is best understood by recognizing that expression of claudin-2 or claudin-15 is required for ongoing Na+-nutrient cotransport; mice lacking either claudin survive while those lacking both die of malnutrition by 3 weeks of age [56]. It is also notable that paracellular Na+ conductance is significantly greater in neonatal mice, relative to adults [49]. Thus, it may be that claudin-2 is able to more effectively conduct Na+ than claudin-15. This has not, however, been demonstrated experimentally. In the context of inflammatory stimuli, including disease, intestinal epithelial claudin-2 expression is upregulated, while claudin-15 expression is largely unchanged (Fig. 2) [36, 39, 40, 50,58,59,, 57,58,59,60]. This could therefore represent a compensatory mechanism that restores nutrient absorption in the face of mucosal damage. However, the observation that claudin-2 is not upregulated in claudin-15-deficient mouse intestine [61] suggests that alternative explanations should also be considered.
Regulation of claudin-2, claudin-15, and occludin expression in healthy and diseased adult human intestine. Claudin-2 (green) is primarily expressed in the crypts of the small intestine and colon, and this is increased in inflammatory disease. In contrast, expression of claudin-15 (green), which also forms paracellular cation-selective pores, is present throughout the crypt-villus axis and is unchanged in disease. Occludin (green) expression is reduced in inflammatory disease. E-cadherin (magenta), ZO-1 or γ-actin (red), and nuclei (blue) are shown for reference. Bar, 50 μm; 20 μm (insets)
Claudin-2-Dependent Fluid Efflux Promotes Pathogen Clearance
One major limitation of most in vivo studies of permeability is that the probe or probes used do not allow discrimination between changes in pore, leak, and damage-induced (unrestricted pathway) permeability. Lactulose and mannitol, the most extensively used probes in human studies, are both able to traverse leak and unrestricted pathways. Mannitol is too large to be accommodated by claudin-2 channels in vitro, but it remains to be determined if it can cross the pore pathway in vivo [41]. In mouse models, most investigators simply use 4 kDa FITC-conjugated dextran. Serum recovery of this probe can reflect increased permeability across both leak and unrestricted, but not pore, pathways [62]. Experimental data suggest that greater than two-fold increases in 4 kDa dextran flux are most likely to reflect unrestricted pathway activation as consequence of epithelial damage [62]. To overcome this limitation, we established a method using creatinine (6 Å diameter), 4 kDa dextran (28 Å diameter), and 70 kDa dextran (120 Å diameter), to measure flux across pore, leak, and unrestricted pathways, respectively [60, 62]. This approach, which has been validated by other groups [63], readily distinguishes between barrier defects induced by C. rodentium infection, TNF, and DSS [62].
Using the three-probe in vivo permeability assay, we discovered that creatinine flux is uniquely increased 2 days after C. rodentium infection in mice [60]. This correlated with increased epithelial expression of claudin-2, but not other tight junction proteins, and elevated mucosal IL-22 levels [60]. Analyses using recombinant IL-22 demonstrated that this member of the IL-10 superfamily is responsible for the increased intestinal epithelial claudin-2 transcription and translation seen after C. rodentium infection.
In order to understand the impact of claudin-2 upregulation in C. rodentium infectious colitis, we took advantage of claudin-2 knockout and claudin-2 transgenic mice [60]. The very low claudin-2 expression observed in healthy adults was similar to the absence of claudin-2 in knockout mice, while the increased expression in claudin-2 transgenic mice was comparable to levels detected at the peak of C. rodentium infection [60]. The genetically modified mice therefore model the extremes of claudin-2 expression in wild-type mice.
The severity of C. rodentium colitis was exacerbated by claudin-2 knockout, as indicated by increased histopathology scores, increased mucosa-associated C. rodentium, prolonged C. rodentium shedding, and markedly elevated mucosal TNF, IL-1β, IL-6, and IL-22 (Fig. 3) [60]. The observation that fecal water and Na+ were increased in healthy claudin-2 transgenic mice suggested that the greater severity of disease in claudin-2 knockout mice might be secondary to reduced water and Na+ efflux. Consistent with this hypothesis, induction of mild osmotic diarrhea by adding polyethylene glycol to the drinking water reduced histopathology scores, mucosa-associated C. rodentium, fecal C. rodentium shedding, and mucosal TNF, IL-1β, IL-6, and IL-22 levels such that all measures of disease were similar in polyethylene glycol-treated claudin-2 knockout, transgenic, and wild-type mice [60]. These data suggest that the primary means by which claudin-2 upregulation accelerates pathogen clearance and reduces infectious enterocolitis severity is by promoting paracellular water and Na+ efflux [60]. Because epithelial cell turnover is accelerated in C. rodentium-induced colitis, this cannot be simply due to bacterial washing from the epithelial surface but is more likely to reflect disruption of the cycle by which newly formed epithelial cells are infected (Fig. 3a). The increased fecal water resulting from claudin-2 overexpression likely also dilutes and reduces local DSS concentrations to attenuate mucosal damage, thereby explaining the protection fromm DSS-induced injury observed in claudin-2 transgenic mice [64]. Thus, claudin-2 increases luminal water efflux to promote pathogen clearance and dilute offending chemical agents in infectious and chemical colitis, respectively. Intestinal claudin-2 upregulation and the water efflux that follows can therefore be considered a primitive form of innate immunity.
IL-22 upregulates epithelial claudin-2 to drive diarrhea and enteric pathogen clearance. (a) IL-22 released in response to enteric infection upregulates claudin-2 expression to enhance paracellular Na+ and water efflux and promote pathogen clearance. Here, polyethylene glycol (PEG) is shown as an inducer of osmotic diarrhea. (b) C. rodentium (red) and nuclei (blue) 11 days after infection. Colonization of crypt spaces in claudin-2 knockout mice is prevented by PEG treatment. Bar, 50 μm. (c) Mucosa-associated C. rodentium numbers are reduced in Cldn2Tg and increased in Cldn2−/−, relative to wild-type (Cldn2+/+), mice. PEG treatment eliminated differences between genotypes. (d) Histopathology was increased in Cldn2−/− mice and reduced by PEG treatment. (e and f) Mucosal TNF and IL-22 were markedly greater in Cldn2−/− mice relative to wild-type or Cldn2Tg mice, at day 11 after infection in the absence, but not presence, of PEG treatment. (Data from Tsai et al. Cell Host Microbe, 2017, with permission)
Claudin-2 Exacerbates Immune-Mediated Colitis
Although claudin-2 upregulation reduces severity of infectious and chemical colitis, it is not clear if it represents a beneficial adaptation or contributes to progression of immune-mediated colitis. To address this, claudin-2 knockout and transgenic mice were crossed onto an immunodeficient Rag1 knockout background and studied using the adoptive T-cell transfer colitis model [40, 65]. In contrast to infectious and chemical colitis models, immune-mediated disease severity was increased by transgenic claudin-2 expression and reduced by claudin-2 knockout, as measured by weight loss, disease activity index, cytokine production, T-cell infiltration, and histopathology scores (Fig. 4) [40]. Conversely, the same measures showed that claudin-2 knockout ameliorated immune-mediated colitis [40]. It therefore appears that claudin-2 upregulation is a maladaptive response to mucosal immune activation in the absence of offending exogenous agents, such as pathogenic bacteria or toxic chemicals. Further study is needed to understand how claudin-2 modifies mucosal immune activation and whether this contributes to the relative protection afforded by claudin-2 overexpression in C. rodentium colitis.
Intestinal epithelial claudin-2 overexpression exacerbates, and claudin-2 knockout limits immune-mediated colitis severity. (a) Weight loss and disease activity induced by T-cell transfer in Cldn2+/+Rag1−/− mice (blue circles), Cldn2−/–Rag1−/− mice (red circles), and Cldn2TgRag1−/− mice (green circles). (b) Histopathology of mice sacrificed at day 56 after T-cell transfer shows more severe disease in Cldn2TgRag1−/− mice and milder disease in Cldn2−/–Rag1−/− mice, relative to Cldn2+/+Rag1−/− mice. (c) T-cell recruitment (CD3, green) parallels disease severity. ZO-1 or E-cadherin (red) and nuclei (blue) are shown for reference. Bars, 50 μm (Data from Raju et al. J Clin Invest, 2020, with permission)
Despite reduced disease severity, survival after T-cell transfer was reduced in claudin-2 knockout mice. This was unexpected and, in most cases, followed an unusual clinical pattern. Wild-type and claudin-2 transgenic mice displayed progressive increases in disease activity and weight loss over weeks. In contrast, claudin-2 knockout mice appeared well until they became acutely ill in the few days before death. Necropsy showed that these mice suffered from intestinal obstruction [40]. This was not due to fibrosis or dysmotility. We therefore considered the possibility that insufficient luminal hydration could result in fecalith formation and obstruction. In contrast to humans, this led to obstruciton in mice, where the luminal space is dramatically narrowed by mucosal inflammatory expansion. To prevent obstruction, polyethylene glycol was added to the drinking water of claudin-2 knockout and wild-type mice. This did not affect disease severity but improved survival of claudin-2 knockout mice [40]. Thus, increasing luminal water was sufficient to prevent obstruction and death in claudin-2 knockout mice. Notably, claudin-2 knockout, but not wild-type, mice upregulated intestinal epithelial claudin-15 expression during colitis. This can be taken as an additional piece of evidence that, despite our inability to detect functional differences at present [52], claudin-2 and claudin-15 are not functionally interchangeable, as such claudin-15 upregulation did not disrupt the effects of claudin-2 knockout.
Occludin S408 Phosphorylation Regulates Claudin-2 Channel Function
The occludin C-terminal tail can be separated into membrane-proximal and distal portions. The distal half (residues 373 to 522) is most highly conserved [66] and can be broken into an unstructured region (373–412) and a coil-coil domain (413–522) composed of three alpha helices [67]. Biochemical studies found that the unstructured region within the distal occludin tail contains multiple sites that can be phosphorylated by casein kinase 2 (CK2) [68,69,70]. The development of highly specific CK2 inhibitors as pharmacological therapies for neoplastic disease created an opportunity to assess the impact of CK2-mediated occludin phosphorylation on a barrier function. In Caco-2 intestinal epithelial cell monolayers, enzymatic CK2 inhibition reduced paracellular permeability of small cations, consistent with inhibition of the claudin-2 channel [71]. CK2 inhibitors had no effect in the absence of CK2, occludin, or claudin-2 expression [71]. Mutagenesis studies showed that serine-408 dephosphorylation was required for the effect of CK2 inhibition on barrier function. Fluorescence recovery after photobleaching (FRAP) studies showed that CK2 inhibition reduced the occludin mobile fraction and that this behavior also mapped to serine-408 [71]. Further analyses using pull-down assays showed that the non-phosphorylatable tail of occludinS408A captured greater amounts of endogenous occludin, claudin-1, and claudin-2 from Caco-2 cell lysates than the phosphomimetic occludinS408D [71]. Although no direct binding sites between claudins and occludin are known, ZO-1 includes PDZ1 and U5-GuK domains that bind to each of these, respectively [72, 73]. Consistent with an essential role for ZO-1-mediated interactions between occludin and claudins, neither S408A nor S408D occludin tails effectively recovered claudin-2 from ZO-1-deficient Caco-2 cell lysates [71]. Moreover, CK2 inhibitors had no effect on TER of ZO-1-deficient Caco-2 monolayers. The TER response to CK2 inhibition could be restored by expression of full-length ZO-1, but not ZO-1ΔPDZ1 or ZO-1ΔU5GuK [71]. Together, these data demonstrate that dephosphorylation of occludinS408 triggers assembly of an occludin-ZO-1-claudin-2 complex that interferes with claudin-2 channel function (Fig. 5a) [73]. As a final test of this hypothesis, T84 cell monolayers, which do not ordinarily express significant levels of claudin-2, were treated with IL-13 to induce claudin-2 expression. This reduced TER and increased cation selectivity, and both of these changes could be reversed by CK2 inhibition. Thus, occludin phosphorylation at S408 is a molecular switch that, indirectly, regulates claudin-2 channels [71].
CK2 inhibition limits immune-mediated colitis severity by inactivating claudin-2 channels. (a) Casein kinase-2 (CK2) inhibition results in occludin S408 dephosphorylation and triggers assembly of a trimolecular complex composed of occludin, ZO-1, and claudin-2 to inactivate claudin-2 Fig. 5 (continued) channels. (b) IL-13 administration increased claudin-2 (green) expression in proximal colonic crypt epithelium. This was not affected by CK2 inhibition. Nuclei (blue) are shown for reference. (c) Ussing chamber analyses of proximal colonic mucosae from IL-13-treated mice (red squares) shows specific increases in permeability of small cations relative to vehicle-treated mice (blue circles). Treatment with CK2 inhibitor (green-outlined symbols) blocked IL-13-induced permeability increases but had no effect in the absence of IL-13. (d) Weight loss following T-cell transfer was attenuated in Rag1−/− mice treated with a CK2 inhibitor (green diamonds) relative to controls receiving vehicle (blue circles). (e) Histopathology was reduced by CK2 inhibitor treatment. (f) T-cell (CD3, green) infiltration was reduced by CK2 inhibition. E-cadherin (red) and nuclei (blue) are shown for reference. Bars, 50 μm (Data from Raju et al. J Clin Invest, 2020, with permission)
Inhibition of Occludin Phosphorylation Is Therapeutic in Experimental, Immune-Mediated Colitis
In order to determine whether CK2 inhibition could also block claudin-2 channel function in vivo, mice were treated with saline or IL-13, to induce claudin-2 expression, in combination with a CK2 inhibitor or vehicle [40]. Bi-ionic potential measurements were then used to characterize excised proximal colonic mucosae [40, 53, 74, 75]. As expected, IL-13 specifically increased claudin-2 expression (Fig. 5b) as well as paracellular permeability to Na+, methylamine, and, to a lesser degree, ethylamine (Fig. 5c) [40]. CK2 inhibition failed to prevent increased claudin-2 expression but reversed changes in paracellular permeability (Fig. 5b, c). In contrast, CK2 inhibition had no effect on permeability in the absence of IL-13 treatment. CK2 inhibition is, therefore, able to block claudin-2 channel function in vivo.
Daily treatment with an orally bioavailable CK2 inhibitor, beginning 10 days after T-cell transfer, dramatically reduced immune-related colitis severity by all measures in claudin-2 wild-type, Rag1−/− mice [40]. In contrast, CK2 inhibition afforded no benefit to claudin-2 knockout Rag1−/− mice [40]. Thus, although the nearly ubiquitous expression and substrate promiscuity of CK2 make it impossible to fully exclude other targets, the requirement for claudin-2 expression suggests that the effect of CK2 inhibition reflects claudin-2 channel inactivation [40]. Thus, in vivo inhibition of CK2-mediated occludin phosphorylation prevents progression and attenuates severity of immune-mediated colitis [40]. CK2 inhibition can affect many processes and, therefore, is not an ideal therapeutic approach. However, future definition of how S408 phosphorylation regulates occludin tail interactions may lead to more specific means of inhibiting claudin-2 function.
Occludin Endocytosis Is Required for TNF-Induced, MLCK-Dependent Leak Pathway Permeability Increases
Remarkably, beyond the perijunctional actomyosin condensation seen by transmission electron microscopy, occludin internalization was the primary morphologic change associated with T-cell activation-induced, TNF-dependent barrier loss [33]. Further study showed that occludin was internalized into caveolin-1-positive endosomes. Although TNF-induced MLCK activation and MLC phosphorylation were increased, caveolin-1 knockout mice failed to internalize occludin and were protected from TNF-induced barrier loss [76]. Caveolar endocytosis is, therefore, required for TNF-induced, MLCK-mediated leak pathway permeability increases. Occludin was the only tight junction protein consistently identified within these endosomes, but the data do not exclude the possibility that occludin is merely a marker of some other critical change in tight junction structure. To assess this, transgenic mice that overexpress occludin within intestinal epithelial cells were treated with TNF. Although endocytosis did occur, tight junction-associated occludin pools were preserved in transgenic, relative to wild-type, mice [76]. Moreover, the magnitude of barrier loss was attenuated, and TNF-induced diarrhea was prevented by transgenic occludin expression [76]. Occludin is, therefore, an essential regulator of leak pathway permeability. Finally, this result is consistent with leak pathway barrier loss and reduced occludin expression in human inflammatory bowel disease [36, 77, 78].
Occludin Regulates Epithelial Survival
The initial reports of occludin knockout mice failed to identify intestinal or renal barrier defects or spontaneous disease involving these organs [79]. Nevertheless, occludin knockout was associated with male infertility, inability of females to effectively suckle pups, gastric epithelial hyperplasia, brain calcifications, testicular atrophy, and osteoporosis, and subsequent studies showed that occludin knockout mice became deaf over time [80]. Finally, our unpublished experience that the frequency of knockout pups when occludin heterozygotes were bred was far less than the expected 25% predicted by Mendelian genetics suggests embryonic loss; crosses of occludin floxed and occludin floxed;villin-cre transgenic mice resulted in equal numbers of cre-positive and cre-negative pups. Embryonic loss of occludin-deficient embryos is, therefore, not due to Ocln deletion within the intestinal epithelium.
The absence of intestinal disease in occludin-deficient mice could be due to compensatory mechanisms that overcome occludin loss. Universal and intestinal epithelial-specific occludin knockout mice were, therefore, stressed in order to unmask functional deficits. Remarkably, dextran sulfate sodium (DSS) failed to induce weight loss in occludin knockout mice (Fig. 6a) [81]. Thus, intestinal epithelial occludin expression sensitizes mice to chemically induced colitis.
Occludin deletion reduces caspase-3 expression, limits epithelial apoptosis, and attenuates experimental disease in mice; both occludin and caspase-3 expression are reduced in Crohn’s disease. (a) DSS-induced colitis severity and weight loss were reduced in Ocln−/− (red circles) relative to wild-type (WT, blue squares) mice. (b) Numbers of apoptotic (ISOL-positive, red) epithelial cells were increased in DSS-treated wild-type, but not intestinal epithelial-specific occludin knock Fig. 6 (continued) out (KOIEC), mice. Nuclei (blue) are shown for reference. Bar, 20 μm. (c) Systemic T-cell activation induced by anti-CD3 treatment increased ISOL-positive (red) cell numbers in wild-type, but not KOIEC, mice. Nuclei (blue) are shown for reference. Bar, 50 μm. (d) Western blot of intestinal epithelia isolated from vehicle- and TNF-treated WT and Ocln−/− mice. With the exception of cleaved caspase-3, signaling events downstream of TNF signaling were not affected by occludin deletion. (e) Ileal biopsies from healthy subjects and Crohn’s disease patients show reduced occludin (green) and caspase-3 (green) expression in disease. E-cadherin (red) and nuclei (blue) are shown for reference. Bar, 50 μm. (f) Quantitative morphometry confirms similar reductions in occludin and caspase-3 expression intensity in ileal epithelium from Crohn’s disease patients (green diamonds) relative to healthy controls (yellow circles) (Data from Kuo et al. Gastroenterology, 2019, with permission)
Further analyses showed that histopathology, inflammatory cytokine production, and epithelial apoptosis induced by DSS or trinitrobenzenesulfonic acid (TNBS) were suppressed in intestinal epithelial occludin knockout mice (Fig. 6b). To better define the mechanism by which occludin loss reduced epithelial apoptosis, mice were treated with 5-fluorouracil, which triggers intrinsic pathway apoptosis, systemic T-cell activation using anti-CD3, or TNF treatment to activate the extrinsic apoptotic pathway [81]. Occludin knockout protected intestinal epithelial cells from all three stimuli (Fig. 6c). Biochemical analysis of apoptotic signaling induced by TNF showed that ERK, p38 MAPK, IκB, and caspase-9 were all activated similarly in occludin-sufficient and knockout intestinal epithelia (Fig. 6d). However, TNF-induced caspase-3 cleavage was only detected in occludin-expressing epithelia (Fig. 6d). Further characterization showed that this was due to a ~ 50% reduction in overall caspase-3 mRNA and protein expression in the absence of occludin. Although it was surprising that an only 50% decrease in expression would be sufficient to prevent apoptosis, mice heterozygous for Casp3 knockout (Casp3+/−) , which express caspase-3 at ~50% of normal levels, were also protected from intestinal epithelial apoptosis induced by DSS or TNF [81]. Thus, occludin promotes caspase-3 transcription, and the reduced caspase-3 expression that follows occludin loss is sufficient to prevent intrinsic and extrinsic pathway apoptosis.
Similar to mice, Caco-2 cells lacking occludin displayed reduced CASP3 transcription and protein expression. Inducible occludin expression in these cells activated the CASP3 promoter and restored transcription to normal levels [81]. Thus, although occludin has not been detected within nuclei, it promotes CASP3 transcription, either directly or indirectly [81]. To assess the effect of inflammation-induced loss of occludin expression on epithelial survival, Caco-2 monolayers were treated with TNF at a low concentration that was insufficient to cause apoptosis. This was, however, sufficient to reduce both occludin and caspase-3 expression and protect cells from staurosporine-induced intrinsic pathway or high-dose TNF-induced extrinsic pathway apoptosis. In contrast, pretreatment of occludin-deficient Caco-2 monolayers with low-dose TNF had no effect on subsequent responses to staurosporine or high-dose TNF. Thus, low-grade inflammation, modeled in vitro by low-dose TNF, may lead to reduced occludin and caspase-3 expression that results in cytoprotection [81].
In order to determine whether occludin downregulation in human disease is associated with reduced caspase-3 expression, small intestinal and colonic biopsies from Crohn’s disease and ulcerative colitis patients and age- and sex-matched healthy control subjects were analyzed by quantitative immunohistochemistry (Fig. 6e). Occludin expression was significantly reduced in both Crohn’s disease and ulcerative colitis and was accompanied by caspase-3 downregulation (Fig. 6f). Moreover, reductions in caspase-3 expression correlated directly with decreased occludin expression. Thus, occludin downregulation in inflammatory disease may be an adaptive response that promotes epithelial survival. Further studies will be needed to understand how this cytoprotective function interfaces with the role of occludin in tight junction barrier regulation.
Summary and Future Directions
The studies discussed here demonstrate the important contributions of pore and leak pathway permeability to intestinal disease. They also highlight the importance of considering these mechanisms as separate processes that are regulated by different signaling events and have distinct effects on barrier function and pathophysiology. The data also show that the impact of increased tight junction permeability may not be the same in infectious and immune-mediated disorders. Although available data cannot explain the reasons for these differences, one might hypothesize that increased claudin-2 expression in infectious disease both enhanced water efflux and augmented mucosal immune activation. Evolutionarily, where infectious diseases had much greater impact on survival than immune-mediated disorders, increased pathogen clearance and immune activation might be considered synergistic. The contradiction only occurs in the context of immune-mediated disease. Although the effects of occludin downregulation in infectious disease have not been defined, one could hypothesize that increased leak pathway permeability might promote pathogen clearance while simultaneously downregulating caspase-3 expression to limit tissue damage. Thus, regulatory mechanisms that evolved over billions of years to promote survival may now have unintended consequences in the context of modern maladies.
The growing synergy between in vitro and in vivo models makes this an exciting time for tight junction biology in which future studies will address the questions raised in this text and many others. Ultimately, we hope that both fundamental, foundational advances and translational studies will lead to clinical trials in which barrier and tight junction modulation are validated as therapeutic interventions for a broad range of intestinal and systemic diseases.
Abbreviations
- CK2:
-
Casein kinase 2
- DSS:
-
Dextran sulfate sodium
- FRAP:
-
Fluorescence recovery after photobleaching
- MLC:
-
Myosin II regulatory light chain
- MLCK:
-
Myosin light -chain kinase
- TER:
-
Transepithelial electrical resistance
- TNBS:
-
Trinitrobenzenesulfonic acid
- TNF:
-
Tumor necrosis factor
References
Farquhar M, Palade G (1963) Junctional complexes in various epithelia. J Cell Biol 17 (2):375-412
Ussing HH, Windhager EE (1964) Nature of Shunt Path and Active Sodium Transport Path through Frog Skin Epithelium. Acta Physiol Scand 61:484-504
Wade JB, Karnovsky MJ (1974) Fracture faces of osmotically disrupted zonulae occludentes. J Cell Biol 62 (2):344-350. https://doi.org/10.1083/jcb.62.2.344
Montesano R, Gabbiani G, Perrelet A, Orci L (1976) In vivo induction of tight junction proliferation in rat liver. J Cell Biol 68 (3):793-798. https://doi.org/10.1083/jcb.68.3.793
Bentzel CJ, Hainau B, Edelman A, Anagnostopoulos T, Benedetti EL (1976) Effect of plant cytokinins on microfilaments and tight junction permeability. Nature 264 (5587):666-668. https://doi.org/10.1038/264666a0
Madara JL, Pappenheimer JR (1987) Structural basis for physiological regulation of paracellular pathways in intestinal epithelia. J Membr Biol 100 (2):149-164
Pappenheimer JR (1987) Physiological regulation of transepithelial impedance in the intestinal mucosa of rats and hamsters. J Membr Biol 100 (2):137-148
Pappenheimer JR, Reiss KZ (1987) Contribution of solvent drag through intercellular junctions to absorption of nutrients by the small intestine of the rat. J Membr Biol 100 (1):123-136. https://doi.org/10.1007/bf02209145
Meddings JB, Westergaard H (1989) Intestinal glucose transport using perfused rat jejunum in vivo: model analysis and derivation of corrected kinetic constants. Clin Sci (Lond) 76 (4):403-413. https://doi.org/10.1042/cs0760403
Atisook K, Carlson S, Madara JL (1990) Effects of phlorizin and sodium on glucose-elicited alterations of cell junctions in intestinal epithelia. Am J Physiol 258 (1 Pt 1):C77-85. https://doi.org/10.1152/ajpcell.1990.258.1.C77
Turner JR, Madara JL (1995) Physiological regulation of intestinal epithelial tight junctions as a consequence of Na+-coupled nutrient transport. Gastroenterol 109 (4):1391-1396
Uhing MR, Arango V (1997) Intestinal absorption of proline and leucine in chronically catheterized rats. Gastroenterol 113 (3):865-874
Schwartz RM, Furne JK, Levitt MD (1995) Paracellular intestinal transport of six-carbon sugars is negligible in the rat. Gastroenterol 109 (4):1206-1213
Fine KD, Ana CAS, Porter JL, Fordtran JS (1994) Mechanism by Which Glucose Stimulates the Passive Absorption of Small Solutes by the Human Jejunum in-Vivo. Gastroenterol 107 (2):389-395
Fine KD, Santa Ana CA, Porter JL, Fordtran JS (1993) Effect of D-glucose on intestinal permeability and its passive absorption in human small intestine in vivo. Gastroenterol 105 (4):1117-1125
Turner JR, Cohen DE, Mrsny RJ, Madara JL (2000) Noninvasive in vivo analysis of human small intestinal paracellular absorption: regulation by Na+-glucose cotransport. Dig Dis Sci 45 (11):2122-2126. https://doi.org/10.1023/a:1026682900586
Pappenheimer JR (1998) Scaling of dimensions of small intestines in non-ruminant eutherian mammals and its significance for absorptive mechanisms. Comp Biochem Physiol A Mol Integr Physiol 121 (1):45-58.
Karlsson J, Ungell A, Grasjo J, Artursson P (1999) Paracellular drug transport across intestinal epithelia: influence of charge and induced water flux. Eur J Pharm Sci 9 (1):47-56
Berglund JJ, Riegler M, Zolotarevsky Y, Wenzl E, Turner JR (2001) Regulation of human jejunal transmucosal resistance and MLC phosphorylation by Na(+)-glucose cotransport. Am J Physiol - Gastrointest Liver Physiol 281 (6):G1487-1493. https://doi.org/10.1152/ajpgi.2001.281.6.G1487
Fihn BM, Sjoqvist A, Jodal M (2000) Permeability of the rat small intestinal epithelium along the villus-crypt axis: effects of glucose transport. Gastroenterol 119 (4):1029-1036. https://doi.org/10.1053/gast.2000.18148
Pei L, Solis G, Nguyen MT, Kamat N, Magenheimer L, Zhuo M, Li J, Curry J, McDonough AA, Fields TA, Welch WJ, Yu AS (2016) Paracellular epithelial sodium transport maximizes energy efficiency in the kidney. J Clin Invest 126 (7):2509-2518. https://doi.org/10.1172/JCI83942
Larsen EH, Mobjerg N (2006) Na+ recirculation and isosmotic transport. J Membr Biol 212 (1):1-15. https://doi.org/10.1007/s00232-006-0864-x
Turner JR, Rill BK, Carlson SL, Carnes D, Kerner R, Mrsny RJ, Madara JL (1997) Physiological regulation of epithelial tight junctions is associated with myosin light-chain phosphorylation. Am J Physiol 273 (4):C1378-1385. https://doi.org/10.1152/ajpcell.1997.273.4.C1378
Taylor CT, Dzus AL, Colgan SP (1998) Autocrine regulation of epithelial permeability by hypoxia: role for polarized release of tumor necrosis factor alpha. Gastroenterol 114 (4):657-668
Marano CW, Lewis SA, Garulacan LA, Soler AP, Mullin JM (1998) Tumor necrosis factor-alpha increases sodium and chloride conductance across the tight junction of CACO-2 BBE, a human intestinal epithelial cell line. J Membr Biol 161 (3):263-274
Rodriguez P, Heyman M, Candalh C, Blaton MA, Bouchaud C (1995) Tumour necrosis factor-alpha induces morphological and functional alterations of intestinal HT29 cl.19A cell monolayers. Cytokine 7 (5):441-448. https://doi.org/10.1006/cyto.1995.0060
Baert FJ, D'Haens GR, Peeters M, Hiele MI, Schaible TF, Shealy D, Geboes K, Rutgeerts PJ (1999) Tumor necrosis factor alpha antibody (infliximab) therapy profoundly down-regulates the inflammation in Crohn's ileocolitis. Gastroenterol 116 (1):22-28
Suenaert P, Bulteel V, Lemmens L, Noman M, Geypens B, Van Assche G, Geboes K, Ceuppens JL, Rutgeerts P (2002) Anti-tumor necrosis factor treatment restores the gut barrier in Crohn's disease. Am J Gastroenterol 97 (8):2000-2004. https://doi.org/10.1111/j.1572-0241.2002.05914.x
Zolotarevsky Y, Hecht G, Koutsouris A, Gonzalez DE, Quan C, Tom J, Mrsny RJ, Turner JR (2002) A membrane-permeant peptide that inhibits MLC kinase restores barrier function in in vitro models of intestinal disease. Gastroenterol 123 (1):163-172. https://doi.org/10.1053/gast.2002.34235
Wang F, Graham WV, Wang Y, Witkowski ED, Schwarz BT, Turner JR (2005) Interferon-gamma and tumor necrosis factor-alpha synergize to induce intestinal epithelial barrier dysfunction by up-regulating myosin light chain kinase expression. Am J Pathol 166 (2):409-419. https://doi.org/10.1016/s0002-9440(10)62264-x
Pongkorpsakol P, Turner JR, Zuo L (2020) Culture of Intestinal Epithelial Cell Monolayers and Their Use in Multiplex Macromolecular Permeability Assays for In Vitro Analysis of Tight Junction Size Selectivity. Curr Protoc Immunol 131 (1):e112. https://doi.org/10.1002/cpim.112
Bruewer M, Luegering A, Kucharzik T, Parkos CA, Madara JL, Hopkins AM, Nusrat A (2003) Proinflammatory cytokines disrupt epithelial barrier function by apoptosis-independent mechanisms. J Immunol 171 (11):6164-6172
Clayburgh DR, Barrett TA, Tang Y, Meddings JB, Van Eldik LJ, Watterson DM, Clarke LL, Mrsny RJ, Turner JR (2005) Epithelial myosin light chain kinase-dependent barrier dysfunction mediates T cell activation-induced diarrhea in vivo. J Clin Invest 115 (10):2702-2715. https://doi.org/10.1172/JCI24970
Blair SA, Kane SV, Clayburgh DR, Turner JR (2006) Epithelial myosin light chain kinase expression and activity are upregulated in inflammatory bowel disease. Lab Invest 86 (2):191-201. https://doi.org/10.1038/labinvest.3700373
Holmes JL, Van Itallie CM, Rasmussen JE, Anderson JM (2006) Claudin profiling in the mouse during postnatal intestinal development and along the gastrointestinal tract reveals complex expression patterns. Gene Expr Patterns 6 (6):581-588. https://doi.org/10.1016/j.modgep.2005.12.001
Heller F, Florian P, Bojarski C, Richter J, Christ M, Hillenbrand B, Mankertz J, Gitter AH, Burgel N, Fromm M, Zeitz M, Fuss I, Strober W, Schulzke JD (2005) Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterol 129 (2):550-564. https://doi.org/10.1016/j.gastro.2005.05.002
Prasad S, Mingrino R, Kaukinen K, Hayes KL, Powell RM, MacDonald TT, Collins JE (2005) Inflammatory processes have differential effects on claudins 2, 3 and 4 in colonic epithelial cells. Lab Invest 85 (9):1139-1162. https://doi.org/10.1038/labinvest.3700316
Zeissig S, Burgel N, Gunzel D, Richter J, Mankertz J, Wahnschaffe U, Kroesen AJ, Zeitz M, Fromm M, Schulzke JD (2007) Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn's disease. Gut 56 (1):61-72. https://doi.org/10.1136/gut.2006.094375
Weber CR, Raleigh DR, Su L, Shen L, Sullivan EA, Wang Y, Turner JR (2010) Epithelial myosin light chain kinase activation induces mucosal interleukin-13 expression to alter tight junction ion selectivity. J Biol Chem 285 (16):12037-12046. https://doi.org/10.1074/jbc.M109.064808
Raju P, Shashikanth N, Tsai PY, Pongkorpsakol P, Chanez-Paredes S, Steinhagen PR, Kuo WT, Singh G, Tsukita S, Turner JR (2020) Inactivation of paracellular cation-selective claudin-2 channels attenuates immune-mediated experimental colitis in mice. J Clin Invest 130 (10):5197-5208. https://doi.org/10.1172/JCI138697
Van Itallie CM, Holmes J, Bridges A, Gookin JL, Coccaro MR, Proctor W, Colegio OR, Anderson JM (2008) The density of small tight junction pores varies among cell types and is increased by expression of claudin-2. J Cell Sci 121 (Pt 3):298-305. https://doi.org/10.1242/jcs.021485
Van Itallie CM, Fanning AS, Bridges A, Anderson JM (2009) ZO-1 stabilizes the tight junction solute barrier through coupling to the perijunctional cytoskeleton. Mol Biol Cell 20 (17):3930-3940. https://doi.org/10.1091/mbc.E09-04-0320
Buschmann MM, Shen L, Rajapakse H, Raleigh DR, Wang Y, Wang Y, Lingaraju A, Zha J, Abbott E, McAuley EM, Breskin LA, Wu L, Anderson K, Turner JR, Weber CR (2013) Occludin OCEL-domain interactions are required for maintenance and regulation of the tight junction barrier to macromolecular flux. Mol Biol Cell 24 (19):3056-3068. https://doi.org/10.1091/mbc.E12-09-0688
Turner JR (2009) Intestinal mucosal barrier function in health and disease. Nat Rev Immunol 9 (11):799-809. https://doi.org/10.1038/nri2653
Anderson JM, Van Itallie CM (2009) Physiology and function of the tight junction. Cold Spring Harb Perspect Biol 1 (2):a002584. https://doi.org/10.1101/cshperspect.a002584
Weber CR, Liang GH, Wang Y, Das S, Shen L, Yu AS, Nelson DJ, Turner JR (2015) Claudin-2-dependent paracellular channels are dynamically gated. eLife 4:e09906. https://doi.org/10.7554/eLife.09906
Krug SM, Amasheh S, Richter JF, Milatz S, Gunzel D, Westphal JK, Huber O, Schulzke JD, Fromm M (2009) Tricellulin forms a barrier to macromolecules in tricellular tight junctions without affecting ion permeability. Mol Biol Cell 20 (16):3713-3724. https://doi.org/10.1091/mbc.E09-01-0080
Pappenheimer JR (1993) On the coupling of membrane digestion with intestinal absorption of sugars and amino acids. Am J Physiol 265 (3 Pt 1):G409-417. https://doi.org/10.1152/ajpgi.1993.265.3.G409
Tamura A, Hayashi H, Imasato M, Yamazaki Y, Hagiwara A, Wada M, Noda T, Watanabe M, Suzuki Y, Tsukita S (2011) Loss of claudin-15, but not claudin-2, causes Na+ deficiency and glucose malabsorption in mouse small intestine. Gastroenterol 140 (3):913-923. https://doi.org/10.1053/j.gastro.2010.08.006
Ong M, Yeruva S, Sailer A, Nilsen SP, Turner JR (2020) Differential regulation of claudin-2 and claudin-15 expression in children and adults with malabsorptive disease. Lab Invest 100 (3):483-490. https://doi.org/10.1038/s41374-019-0324-8
Colegio OR, Van Itallie CM, McCrea HJ, Rahner C, Anderson JM (2002) Claudins create charge-selective channels in the paracellular pathway between epithelial cells. Am J Physiol - Cell Physiol 283 (1):C142-147. https://doi.org/10.1152/ajpcell.00038.2002
Rosenthal R, Gunzel D, Piontek J, Krug SM, Ayala-Torres C, Hempel C, Theune D, Fromm M (2020) Claudin-15 forms a water channel through the tight junction with distinct function compared to claudin-2. Acta Physiol (Oxf) 228 (1):e13334. https://doi.org/10.1111/apha.13334
Angelow S, Yu AS (2009) Structure-function studies of claudin extracellular domains by cysteine-scanning mutagenesis. J Biol Chem 284 (42):29205-29217. https://doi.org/10.1074/jbc.M109.043752
Yu AS, Cheng MH, Angelow S, Gunzel D, Kanzawa SA, Schneeberger EE, Fromm M, Coalson RD (2009) Molecular basis for cation selectivity in claudin-2-based paracellular pores: identification of an electrostatic interaction site. J Gen Physiol 133 (1):111-127. https://doi.org/10.1085/jgp.200810154
Rosenthal R, Gunzel D, Krug SM, Schulzke JD, Fromm M, Yu AS (2017) Claudin-2-mediated cation and water transport share a common pore. Acta Physiol (Oxf) 219 (2):521-536. https://doi.org/10.1111/apha.12742
Wada M, Tamura A, Takahashi N, Tsukita S (2013) Loss of claudins 2 and 15 from mice causes defects in paracellular Na+ flow and nutrient transport in gut and leads to death from malnutrition. Gastroenterol 144 (2):369-380. https://doi.org/10.1053/j.gastro.2012.10.035
Kinugasa T, Sakaguchi T, Gu X, Reinecker HC (2000) Claudins regulate the intestinal barrier in response to immune mediators. Gastroenterol 118 (6):1001-1011
Nishiyama R, Sakaguchi T, Kinugasa T, Gu X, MacDermott RP, Podolsky DK, Reinecker HC (2001) Interleukin-2 receptor beta subunit-dependent and -independent regulation of intestinal epithelial tight junctions. J Biol Chem 276 (38):35571-35580. https://doi.org/10.1074/jbc.M106013200. M106013200 [pii]
Suzuki T, Yoshinaga N, Tanabe S (2011) Interleukin-6 (IL-6) regulates claudin-2 expression and tight junction permeability in intestinal epithelium. J Biol Chem 286 (36):31263-31271. https://doi.org/10.1074/jbc.M111.238147
Tsai PY, Zhang B, He WQ, Zha JM, Odenwald MA, Singh G, Tamura A, Shen L, Sailer A, Yeruva S, Kuo WT, Fu YX, Tsukita S, Turner JR (2017) IL-22 Upregulates Epithelial Claudin-2 to Drive Diarrhea and Enteric Pathogen Clearance. Cell Host Microbe 21 (6):671-681 e674. https://doi.org/10.1016/j.chom.2017.05.009
Tamura A, Kitano Y, Hata M, Katsuno T, Moriwaki K, Sasaki H, Hayashi H, Suzuki Y, Noda T, Furuse M, Tsukita S, Tsukita S (2008) Megaintestine in claudin-15-deficient mice. Gastroenterol 134 (2):523-534. https://doi.org/10.1053/j.gastro.2007.11.040
Chanez-Paredes SD, Abtahi S, Kuo W-T, Turner JR (2021) Differentiating Between Tight Junction-Dependent and Tight Junction-Independent Intestinal Barrier Loss In Vivo. In: Methods in Molecular Biology. Springer US. https://doi.org/10.1007/7651_2021_389
Oami T, Coopersmith CM (2021) Measurement of Intestinal Permeability During Sepsis. Methods Mol Biol 2321:169-175. https://doi.org/10.1007/978-1-0716-1488-4_15
Ahmad R, Chaturvedi R, Olivares-Villagomez D, Habib T, Asim M, Shivesh P, Polk DB, Wilson KT, Washington MK, Van Kaer L, Dhawan P, Singh AB (2014) Targeted colonic claudin-2 expression renders resistance to epithelial injury, induces immune suppression, and protects from colitis. Mucosal Immunol 7 (6):1340-1353. https://doi.org/10.1038/mi.2014.21
Powrie F, Correa-Oliveira R, Mauze S, Coffman RL (1994) Regulatory interactions between CD45RBhigh and CD45RBlow CD4+ T cells are important for the balance between protective and pathogenic cell-mediated immunity. J Exp Med 179 (2):589-600. https://doi.org/10.1084/jem.179.2.589
Ando-Akatsuka Y, Saitou M, Hirase T, Kishi M, Sakakibara A, Itoh M, Yonemura S, Furuse M, Tsukita S (1996) Interspecies diversity of the occludin sequence: cDNA cloning of human, mouse, dog, and rat-kangaroo homologues. J Cell Biol 133 (1):43-47. https://doi.org/10.1083/jcb.133.1.43
Li Y, Fanning AS, Anderson JM, Lavie A (2005) Structure of the conserved cytoplasmic C-terminal domain of occludin: identification of the ZO-1 binding surface. J Mol Biol 352 (1):151-164. https://doi.org/10.1016/j.jmb.2005.07.017
Cordenonsi M, Mazzon E, De Rigo L, Baraldo S, Meggio F, Citi S (1997) Occludin dephosphorylation in early development of Xenopus laevis. J Cell Sci 110 (Pt 24):3131-3139
Cordenonsi M, Turco F, D'Atri F, Hammar E, Martinucci G, Meggio F, Citi S (1999) Xenopus laevis occludin. Identification of in vitro phosphorylation sites by protein kinase CK2 and association with cingulin. Eur J Biochem 264 (2):374-384. https://doi.org/10.1046/j.1432-1327.1999.00616.x
Smales C, Ellis M, Baumber R, Hussain N, Desmond H, Staddon JM (2003) Occludin phosphorylation: identification of an occludin kinase in brain and cell extracts as CK2. FEBS Lett 545 (2-3):161-166.
Raleigh DR, Boe DM, Yu D, Weber CR, Marchiando AM, Bradford EM, Wang Y, Wu L, Schneeberger EE, Shen L, Turner JR (2011) Occludin S408 phosphorylation regulates tight junction protein interactions and barrier function. J Cell Biol 193 (3):565-582. https://doi.org/10.1083/jcb.201010065
Itoh M, Furuse M, Morita K, Kubota K, Saitou M, Tsukita S (1999) Direct binding of three tight junction-associated MAGUKs, ZO-1, ZO-2, and ZO-3, with the COOH termini of claudins. J Cell Biol 147 (6):1351-1363. https://doi.org/10.1083/jcb.147.6.1351
Fanning AS, Jameson BJ, Jesaitis LA, Anderson JM (1998) The tight junction protein ZO-1 establishes a link between the transmembrane protein occludin and the actin cytoskeleton. J Biol Chem 273 (45):29745-29753
Yu AS (2011) Electrophysiological characterization of claudin ion permeability using stably transfected epithelial cell lines. Methods Mol Biol 762:27-41. https://doi.org/10.1007/978-1-61779-185-7_3
Shashikanth N, Rizzo HE, Pongkorpsakol P, Heneghan JF, Turner JR (2021) Electrophysiologic Analysis of Tight Junction Size and Charge Selectivity. Curr Protoc 1 (6):e143. https://doi.org/10.1002/cpz1.143
Marchiando AM, Shen L, Graham WV, Weber CR, Schwarz BT, Austin JR, 2nd, Raleigh DR, Guan Y, Watson AJ, Montrose MH, Turner JR (2010) Caveolin-1-dependent occludin endocytosis is required for TNF-induced tight junction regulation in vivo. J Cell Biol 189 (1):111-126. https://doi.org/10.1083/jcb.200902153
Pearson AD, Eastham EJ, Laker MF, Craft AW, Nelson R (1982) Intestinal permeability in children with Crohn's disease and coeliac disease. Br Med J (Clin Res Ed) 285 (6334):20-21
Olaison G, Leandersson P, Sjodahl R, Tagesson C (1988) Intestinal permeability to polyethyleneglycol 600 in Crohn's disease. Peroperative determination in a defined segment of the small intestine. Gut 29 (2):196-199. https://doi.org/10.1136/gut.29.2.196
Saitou M, Furuse M, Sasaki H, Schulzke JD, Fromm M, Takano H, Noda T, Tsukita S (2000) Complex phenotype of mice lacking occludin, a component of tight junction strands. Mol Biol Cell 11 (12):4131-4142. https://doi.org/10.1091/mbc.11.12.4131
Kitajiri S, Katsuno T, Sasaki H, Ito J, Furuse M, Tsukita S (2014) Deafness in occludin-deficient mice with dislocation of tricellulin and progressive apoptosis of the hair cells. Biology open 3 (8):759-766. https://doi.org/10.1242/bio.20147799
Kuo WT, Shen L, Zuo L, Shashikanth N, Ong M, Wu L, Zha J, Edelblum KL, Wang Y, Wang Y, Nilsen SP, Turner JR (2019) Inflammation-induced Occludin Downregulation Limits Epithelial Apoptosis by Suppressing Caspase-3 Expression. Gastroenterol 157 (5):1323-1337. https://doi.org/10.1053/j.gastro.2019.07.058
Acknowledgments
We thank previous and current members of the Laboratory of Mucosal Barrier Pathobiology for their intellectual contributions to the development of studies described herein and for allowing the reuse of their published data. We are also indebted to Tiffany S. Davanzo (Slaybaugh Studios) and Heather Marlatt (Nationwide Histology) for their contributions to the figures. Finally, although we have attempted to cite previous work correctly and completely, we are certain to have omitted some studies, either unintentionally or due to space limitations, and offer our apologies to those we have failed to acknowledge.
Funding: This work was supported by the National Institutes of Health grants R01DK061931 (JRT), R01DK068271 (JRT), and P30DK034854 (The Harvard Digestive Disease Center).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
JRT is a founder and shareholder of Thelium Therapeutics and has served as a consultant for Entrinsic, Immunic, and Kallyope.
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sweat, Y.Y. et al. (2022). Modulation of Intestinal Disorders by Claudin-2 and Occludin Via Canonical and Noncanonical Mechanisms. In: González-Mariscal, L. (eds) Tight Junctions. Springer, Cham. https://doi.org/10.1007/978-3-030-97204-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-97204-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-97203-5
Online ISBN: 978-3-030-97204-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)