Abstract
-
1.
Pilonidal disease is a common problem in the adolescent population. It is usually associated with entrapped hairs.
-
2.
While there is lack of literature and research designated to the pediatric population, growing evidence supports minimally invasive measures. These include “pit picking” and placement of vessel loops/seton to be as effective as wide incisions.
-
3.
Midline incisions should not be used. Off midline incisions are more effective to promote wound healing.
-
4.
Occasional flap procedures are required for severe refractory disease.
-
5.
Ongoing care and hygiene are required for successful healing. Laser ablation of hair in the sacral region has been effective in preventing recurrence.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
1)
Pilonidal disease is a common problem in the adolescent population. It is usually associated with entrapped hairs.
-
2)
While there is lack of literature and research designated to the pediatric population, growing evidence supports minimally invasive measures. These include “pit picking” and placement of vessel loops/seton to be as effective as wide incisions.
-
3)
Midline incisions should not be used. Off midline incisions are more effective to promote wound healing.
-
4)
Occasional flap procedures are required for severe refractory disease.
-
5)
Ongoing care and hygiene are required for successful healing. Laser ablation of hair in the sacral region has been effective in preventing recurrence.
Pilonidal disease is an inflammatory condition of the skin and subcutaneous tissues overlying the sacrum that affects primarily adolescents and young adults. The disease is more common in males. Pilonidal disease is the result of entrapped hairs in the midline natal cleft overlying the sacrum. The entrapped foreign body hair and debris leads to sinus tracts which may drain through the pit at the base of the hair follicle. Entrapped hairs may lead to abscesses. The hairs become ingrown as a result of shed hair that becomes burrowed into the skin due to friction. Pilonidal disease may present acutely with a painful abscess, or as a subacute or chronic infection manifest by draining pilonidal sinus tracts.
-
1.
Epidemiology
The incidence of pilonidal disease in the adolescent population is increasing. It is most commonly encountered in adolescents and young adults. The disease occurs about 3–4 times more frequently in males than females. It affects approximately 2.5 per 10,000. Peak incidence in the adolescent and young adult population is aged 14–25 years.
-
2.
Pathophysiology:
-
a.
Anatomy: Pilonidal disease occurs in the gluteal cleft. The gluteal cleft is the indented area between the gluteus maximus muscles overlying the sacrum. Pilonidal disease should be distinguished from perirectal abscess. Pilonidal disease is not near the anus and overlies the sacrum. There may be sinus tracts known as “pits” with protruding hairs. There may be a midline or off-midline fluctuant mass.
-
b.
Physiology: Pilonidal disease is caused by inflammation and/or infection of the gluteal cleft and sacrococcygeal region. Typical presentation of pilonidal disease is sinus or abscess formation along the midline near the sacrum with small pits or openings. The openings contain entrapped or ingrown hair and debris. The disease can be relatively minor with small pits to large infected areas with multiple sinus tracts or fistulas away from the midline. Risk factors associated with pilonidal disease are obesity, deep gluteal cleft, hirsutism, and friction, which causes the hairs to become ingrown or embedded.
-
c.
Classification Schemes: Pilonidal disease may present as an acute or subacute infection or chronic condition which has been present for months to years.
-
a.
-
3.
Clinical features: Clinical feature of pilonidal disease is sinus or abscess formation near gluteal cleft with small pits or openings. The openings contain entrapped or ingrown hair and debris. Patients often report pain, bleeding, or drainage from the area. The disease may present acutely as an abscess or as a chronic condition that may be present for prolonged periods.
-
4.
Diagnosis: The diagnosis of pilonidal disease is based on history and physical examination findings. The patient may report an acute onset or waxing and waning symptoms including drainage over months to years.
-
a.
Symptoms: Acute pilonidal disease presents with a painful fluctuant mass in the intergluteal area overlying the sacrum. Chronic disease presents as draining sinus tracts with a history of staining of undergarments.
-
b.
Examination: Physical examination is typically done with the patient lying prone or on their side. A fluctuant mass may be present in acute disease. The mass is typically off midline but tracts to the gluteal cleft. There may be overlying erythema and pain to palpation. Sinus tracts are often midline and may have protruding hairs or debris, which are loose. Midline pit openings represent classic pilonidal disease.
-
c.
Radiologic studies and laboratory tests are not helpful for this condition, except in the rare circumstance in which osteomyelitis of the sacrum is suspected. The patient may present with fever and leukocytosis if an abscess is present.
-
a.
-
5.
Treatment: Optimal treatment for pilonidal disease has not been defined. Treatment can range from relatively minor disease with non-operative management to advanced disease with wide excisions and flaps.
-
a.
Initial Measures: Non-operative management may be considered if the pits are relatively small and asymptomatic without abscess. Non-operative management should include removal of hair or debris from the openings, hygiene, and surrounding hair removal. Removal of hair and debris from the pits requires frequent attention by the patient and the assistance of a caregiver at home. Bathing with soaking the area in warm water twice per day is recommended. Non-infected sinus tracts can be resected in an elliptical fashion with primary closure. Postoperative wound complications such as dehiscence are common. Primary closure has been shown to be superior to open wounds, particularly midline wounds.
-
b.
Acute Disease with Abscess: Initial treatment for pilonidal disease begins with infection control with oral antibiotics for infection including abscess if there is a delay to operation or drainage. Acute disease with an abscess requires incision and drainage, as with any abscess. Off midline incisions should be used. Midline incisions are avoided due to delayed healing. The abscess cavity should be debrided of hair, granulation tissue, and debris. Midline sinus tracts should be opened with a punch biopsy instrument. Typically a 2 or 3 mm punch biopsy instrument is used. Vessel loops in the form of seton may be placed from the sinus tracts through the incision. Packing of the wound may be indicated for hemostasis with the removal of the packing in 2–3 days. The patient is instructed to shower or bathe and keep the area clean once packing is removed. Abscess are typically polymicrobial. Typical organisms are Bacteroides, Staphylococcus, Streptococcus, Escherichia Coli, Proteus, and Pseudomonas. Postoperative antibiotics are controversial. Once the abscess is drained, antibiotics are no longer needed.
-
c.
Chronic Pilonidal Disease without abscess: There is rising evidence to support minimally invasive techniques as the first line operative treatment. For chronic disease with draining sinus, a minimalistic approach described by Dr. Gips has been used. A punch biopsy instrument is used to open the sinus tract. The tract is debrided of hair and debris using a curette instrument. Often multiple interventions are required with this technique. Seton may also be placed to keep the tract open for drainage. Excision of the midline sinus tracts with primary closure may be appropriate when there are multiple midline sinus tracts. Primary closure has the advantage of faster healing when successful but is associated with higher recurrence rates than wounds healing by secondary intention.
-
d.
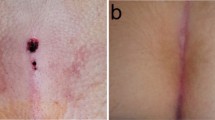
Severe or Chronic Recurrence: For chronic, severe, or recurring disease, flap procedures may be necessary to obliterate the gluteal cleft. Several techniques have been described over the past 60 plus years, including the Bascom cleft lift, Limberg / rhomboid flap, Karydakis flap, V-Y flaps, and Z-plasty. These techniques allow for wide debridement, tension-free closure off midline and flattening of the gluteal cleft. No single technique has been shown to be superior (Fig. 1).
-
e.
Preoperative Preparation: If abscess is present, prompt drainage should be the primary treatment. If there is a lag until drainage, the patient should be treated with oral antibiotics. Patient should begin good hygiene of the area leading up to surgery. This includes daily showers, avoiding prolonged periods of sitting, and hair removal from the area.
-
f.
Postoperative Treatment: Entrapped hairs are a major contributing factor to pilonidal disease. Therefore, hair removal would make sense as part of the treatment plan. However, there is no consensus on the most effective method of hair removal. Hair shaving with razors has been shown to increase risk of recurrence and infection and should be avoided. Laser hair ablation has shown decreased recurrence rates. This technique requires multiple treatments and insurance coverage is problematic due paucity of strong evidence supporting the efficacy of the method in preventing recurrence.
-
g.
Potential Complications: While not a complication, it is important to note pilonidal disease as a whole has a high rate of recurrence. Recurrence rates occur in about 20% after complete healing. It is important that patients and families are taught proper hygiene and wound care, both pre- and post-operatively. Complete healing takes commitment and diligence by both providers and patients.
-
a.
Additional Notes
Pilonidal disease was first described by the famous surgeon Herbert Mayo in the nineteenth century. It was originally thought to be a congenital condition but is now known to be an acquired condition. As the term implies from its Latin roots of pilus meaning hair and nidal meaning nest; the condition arises from ingrown hairs in the skin overlying the sacrum. It has been referred to as pilonidal cyst but this is a misnomer since it lacks an epithelial lining. It was often described after World War II as “jeep driver’s disease” because of the propensity of soldiers to acquire this condition. It is a major source of disability for military personnel in the past and present. The disease is commonly seen in those with deep gluteal cleft, hirsutism, obesity, and friction which causes the hairs to become impaled in the gluteal region. Traditional techniques of wide local excision with primary or delayed closure done in the past are no longer standard of care. Midline incisions need to be avoided whenever possible as they are associated with increased recurrence and complication.
Lord and Millar first suggested a less invasive approach with limited excision of the involved area and debridement. Bascom described the technique of lateral drainage and pit picking. There is a current resurgence toward these less invasive techniques which have been shown to have similar recurrence rates with less morbidity associated with open wounds.
Flap procedures are done in some cases as primary procedures but more commonly for chronic and recurrent diseases. Flap procedures were first introduced by Limberg in 1946 to close midline wounds using a full-thickness rhomboid-shaped rotational flap which flattens the gluteal cleft. Karydakis described an advancement flap in using an off-midline incision on the more affected side with excision of the diseased skin. The flap is secured in layers with a deep layer to the sacrococcygeal fascia. Karydakis reported recurrence rates of less than 2% in over 6500 patients using the flap procedure that bears his name. Bascom and Bascom described the cleft-lift technique which involves excision of an ellipse of the diseased skin with advancement across the midline decreasing the depth of the gluteal cleft. A 7-mm flap is raised opposite the elliptical incised tissue and advanced across the midline with primary closure. Abscess walls are left removing granulation tissue from the surfaces of cavities and tunnels. The difference in this technique from Karydakis’s technique is that the flaps are not full thickness and the underlying tissue including the fat and cavity wall are not excised.
Dr. Gips described a variation to the original Bascom pit-picking procedure in which skin trephines (cylindrical excision typically using an instrument similar to a punch biopsy but able to penetrate deeper into the tissue by lacking the shelf at 8 mm) are used to core out all tracts. Curettes and cotton swabs with hydrogen peroxide were placed through the opening to remove hair, debris, and granulation tissue leaving the wounds open and unpacked to heal by secondary intention. The procedure can be repeated if necessary. The authors report recurrence rates associated with this technique of 6.5% at 1 year, 13.2% at 5 years, and 16.2% at 10 years. We have modified this technique by placing vessels loops as setons.
At present, the most optimal management needs to be determined on a case-by-case basis. Minimal invasive techniques should be the initial management with avoidance of large open incisions. When incisions are necessary, off-midline incisions with circular skin incisions of midline sinuses should be the first modality. Large midline incisions should be avoided. For recurrent disease, flap procedures should be considered.
Study Questions
-
1.
Sixteen-year-old male presents with chronic drainage on the underwear. Physical examinations show several sinus tracts in the midline with protruding hairs. What is the most appropriate treatment?
-
a.
Wide elliptical incision with primary closure.
-
b.
Wide elliptical incision with open wound and packing
-
c.
Punch biopsy of the opening with debridement of hair follicles
-
d.
Off midline incision with debridement from lateral to medial
-
a.
Answer to Question 1: Option C. Several of the options may be acceptable but a minimally invasive approach for the primary procedure is the most appropriate choice. An off- midline incision with primary closure has been shown to effectuate better healing than midline incisions. The Gips procedure described by Dr. Gips as opposed to an elliptical midline incision with or without open wounds has been shown to have similar recurrence rates, faster healing with earlier return to activity, and less morbidity.
-
2.
17-year-old female presents with one-week history of acute onset of pain over the pilonidal region. The patient has a fever of 101° and complains of an inability to sit. On exam, there is erythema overlying the sacrum with a fluctuant mass extending to the left of midline. There are 2 midline sinus tracts with hairs protruding. The patient is morbidly obese with a BMI=36 kg/m2. The patient has significant hair growth in the gluteal area and a deep gluteal cleft. The most appropriate initial treatment is?
-
a.
Bedside incision and drainage midline with oral antibiotics.
-
b.
Operative drainage off-midline with opening of the pilonidal sinus tracts with debridement and vessel loops (as Seton) from the incision to one or both of the pilonidal sinus tracts.
-
c.
Operative drainage off midline with packing of the wound.
-
d.
Midline elliptical incision of the sinus tracts with debridement of the abscess cavity with open wound and packing.
-
a.
Answer to Question 2: B. Patient presenting with a pilonidal abscess requires drainage and debridement as would be required for any abscess. Midline incisions should be avoided. It is important to open the midline pilonidal sinus tracts and debride both from the lateral incision and through the sinus tracts. Packing may be placed in the off midline wound but should be removed in 2–3 days. Seton suture can be used for long-term drainage.
-
3.
You have just performed a minimally invasive Gips procedure on a 15-year-old male for chronic pilonidal disease. His family is asking for post-op instructions. Which of the following is the most appropriate answer?
-
a.
Shower daily. Remove hair by shaving the gluteal cleft once per week. Resume normal physical activity as tolerated.
-
b.
Bathe and remove any entrapped hair daily. Shave the gluteal cleft once per week or undergo laser hair ablation. Activity restrictions should be in place for 2–4 weeks with limited daily physical activity.
-
c.
Shower or bathe one to two times per day. Hair and debris from the pilonidal pits should be removed multiple times per week if someone at home is able to assist. Shave the gluteal cleft once per week but do not use a razor. May resume normal physical activity as tolerated and avoid sitting for prolonged periods of time.
-
d.
Shower or bathe one to two times per day. For infection, treat with antibiotics for 7 days. May resume normal physical activity as tolerated and avoid sitting for prolonged periods of time.
-
a.
Answer to Question 3: C. Patients should be encouraged to shower/bathe at minimum once per day. Hair removal is important to prevent recurrence and allow for healing. However, razor shaving should be avoided as it is associated with increased recurrence. If the patient is awaiting either an appointment for or insurance authorization for laser hair ablation, hair removal products can be used in the meantime. Hair and debris prevents the pilonidal sinus tracts and pits from healing. It is important to remove hair/debris frequently. It should be done multiple times per week and waiting for follow-up appointments will not be adequate. Family can be taught to remove debris with fine tweezers. There is no need for physical activity restrictions within reason and as patient tolerates. Prolonged sitting or immobilization should be avoided. Antibiotics typically do not play a role in chronic disease. If there is no active infection and the site has been adequately debrided, no post-op antibiotics are indicated.
Further Reading
Al-Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010;1:CD006213.
Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980;87(5):567–72.
Bascom J, Bascom T. Failed pilonidal surgery: new paradigm and new operation leading to cures. Arch Surg. 2002;137(10):1146–50.
Delshad HR, Dawson M, Melvin P, et al. Pit-picking resolves pilonidal disease in adolescents. J Pediatr Surg. 2019;54(1):174–6.
Di Castro A, Guerra F, Sandri GBL, Etorre GM. Minimally invasive surgery for the treatment of pilonidal disease. The Gips procedure on 2347 patients. Int J Surg. 2016;36(Part A):201–5.
Gips M, Melki Y, Salem L, et al. Minimal surgery for pilonidal disease using trephines; description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum. 2008;51(11):1656–63.
Grabowski J, Oyetunji TA, Goldin AB, et al. The management of pilonidal disease: a systematic review. J Pediatr Surg. 2019;54(11):2210–1.
Halleran DR, Onwuka AJ, Lawrence AE, et al. Laser depilation in the treatment of pilonidal disease: a systematic review. Surg Infect (Larchmont). 2018;19(6):566–72.
Karydakis G. Easy and successful treatment of pilonidal sinus after explanation of its causative process. ANZ J Surg. 1992;62(5):385–9.
Millar DM, Lord PH. The treatment of acute postanal pilonidal abscess. Br J Surg. 1965;54:598–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rausch, S., Lessin, M.S. (2022). Pilonidal Disease. In: Coppola, C.P., Kennedy, Jr, A.P., Lessin, M.S., Scorpio, R.J. (eds) Pediatric Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-96542-6_74
Download citation
DOI: https://doi.org/10.1007/978-3-030-96542-6_74
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96541-9
Online ISBN: 978-3-030-96542-6
eBook Packages: MedicineMedicine (R0)