Abstract
Positron emission tomography (PET) imaging has increased substantially in recent years. PET allows noninvasive evaluation of myocardial blood flow, function, and metabolism. The advantages of cardiac PET imaging over SPECT are [Dilsizian et al. (J Nucl Cardiol. https://doi.org/10.1007/s12350-009-9094-9, 2009)]: improved image quality (especially in obese patients) with high both temporal and spatial resolution, relatively short imaging protocols, routine attenuation correction (depth independent), providing peak stress ejection fraction (EF)-no time delay between hyperemic response and imaging and true quantification of myocardial blood flow and myocardial metabolism. In addition, PET provides at least equal sensitivity with higher specificity and diagnostic accuracy compared to SPECT. However, cardiac PET still faces the challenges of being less available, with a greater cost, less expertise, challenges of performing exercise stress due to the short half-life of the currently available radiotracers making pharmacological stress testing the only current option, and reimbursement issues.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radionuclide imaging
- Positron emission tomography
- PET
- Cardiac imaging
- Coronary artery disease
- Rubidium-82
Positron emission tomography (PET) imaging has increased substantially in recent years. PET allows noninvasive evaluation of myocardial blood flow, function, and metabolism. The advantages of cardiac PET imaging over SPECT are [1]: improved image quality (especially in obese patients) with high both temporal and spatial resolution, relatively short imaging protocols, routine attenuation correction (depth independent), providing peak stress ejection fraction (EF)-no time delay between hyperemic response and imaging and true quantification of myocardial blood flow and myocardial metabolism. In addition, PET provides equal sensitivity with higher specificity and diagnostic accuracy compared to SPECT. Furthermore, PET allows improved detection of multivessel coronary artery disease. Cardiac PET , however still faces the challenges of being less available, with a greater cost, less expertise, challenges of performing exercise stress due to the short half-life of the currently available radiotracers making pharmacological stress testing the only current option (until the availability of new radiopharmaceutical agents), and reimbursement issues.
Indications
The indications for cardiac PET [2, 3] are similar to those for cardiac SPECT in term of myocardial perfusion imaging for the diagnosis and risk stratification of CAD. However, its role is extended to patients with an equivocal SPECT. In addition, cardiac PET is used as a viability study in patients with ischemic cardiomyopathy. Recently, there has been an increased use in heart failure and in the identification of cardiac sarcoidosis (Table 9.1).
Contraindications
The contraindications to cardiac PET are similar to SPECT (Chap. 8), which include the standard contraindications to pharmacological stress testing when PET perfusion imaging is being done. Inability to lie flat or lie still for the period of acquisition, claustrophobia and extreme weight (>350–400 lbs.) are usually preferred not to undergo PET imaging. Finally, women who are pregnant or breast-feeding are contraindication.
Equipment
The equipment required for a standard cardiac PET examination includes the radionuclides and the PET camera, mostly as a hybrid (with CT) unit. The radionuclides used for PET imaging have a considerably shorter half-life as compared to SPECT tracers. PET radionuclides are produced either from a cyclotron such as fluoro-2-deoxyglucose F-18 FDG and N-13 ammonia or a generator such as rubidium Rb-82. As the name implies, PET imaging involves a positron that collides with an electron to produce two 511 keV gamma rays/photons emitted collinear to each other at 180° angle. The PET detectors are configured to only register the photon pairs if they strike opposite detectors at approximately the same time that has been termed the coincidence detection. The summations of multiple coincidence events are used to reconstruct the PET image to be used for analysis.
The CT scanner provides addition information such as coronary artery calcium scoring and/or noninvasive coronary angiography, but more importantly for PET imaging is for accurate attenuation correction.
The PET camera, similar to SPECT, is made of multiple small detector crystals arranged in a 360° ring and photomultiplier tubes to convert the scintillation events to electrical signal and digitalization to provide the counts that are used in quantification and image processing. Three types of detector crystals are available: (1) Bismuth germanate (BGO) (2) Lutetium oxyorthosilicate (LSO) (3) Gagolinium oxyorthosilicate (GSO) .
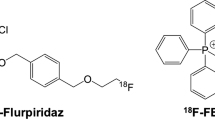
The clinically available PET tracers for myocardial perfusion studies are Rb-82, and N-13 ammonia. Figure 9.1 shows the radiotracers myocardial uptake in relation to coronary blood flow with O-15 being the ideal tracer and the roll-off phenomenon seen with other tracers at higher coronary blood flows. N-13 ammonia, due to the short half-life (10 min), requires an on-site (nearby) cyclotron. It has excellent myocardial uptake/retention with established flow quantification and applications in exercise and pharmacological stress testing. Rubidium-82 is produced on-site from a strontium-82 generator (replaced every 4 weeks) with a half-life of 76 s. Due to the short half-life, it can only be used in pharmacological stress testing. It has with high extraction at high flows (enhances the detection of moderate-severe CAD). Rb-82 is extracted by myocardial cells via the Na/K ATPase pump. The radiation dosimetry from Rb-82 varies from 1.75 to 7.5 mSv total effective dose. Depending on the left ventricular ejection fraction, typically imaging can commence 70–90 s after the injection if LVEF > 50% and delayed slightly longer (~110 s) if LVEF < 50%.
For metabolism imaging, the F-18 FDG tracer (the only FDA approved agent), an analog to glucose, is used. F-18 is produced in a cyclotron and decays with a half-life of 110 min, which allows sufficient time to be produced and distributed in a radius of several hours from the production site. FDG is transported into the cells similar to glucose and is then phosphorylated by hexokinase to FDG-6-phosphate, which is then trapped in the myocardium for PET imaging. The whole body dosimetry from 10 mCi dose is 7 mSv (Tables 9.2 and 9.3 [1]).
Technique
Patient preparation for vasodilator stress testing and myocardial perfusion imaging is similar to what was previously described in the previous Chaps. 6 (Pharmacologic Stress) and 8 (SPECT). For myocardial perfusion imaging (Fig. 9.2), an overnight fast of at least 6 h is required. Following the stress portion, Rb-82 or N-13 is injected at peak hyperemia through a peripheral IV line and emission scans are performed.
Viability studies require a specified protocol for glucose manipulation. In order to allow the myocardium to utilize glucose, an overnight fast of at least 6–12 h (Step 1) is required as patient metabolic preparation is key to successful F-18 FDG imaging to assess viability. The most common metabolic preparation for viability imaging is the use of an oral load of glucose 25–100 g (Step 2) followed by supplemental IV insulin (Step 3) as needed.
In addition to viability imaging, F-18 FDG imaging is being used in the detection of inflammation and infection such as in the identification of active cardiac sarcoidosis and in the identification of active infections involving prosthetics (such as valves and annular rings) and device infections (including pacemakers, implantable cardiac defibrillators/ICD, and left ventricular assist devices/LVADs). The underlying mechanism is that of upregulation of glucose metabolism at the sites of inflammation or infection. The study protocol for the detection of active cardiac sarcoidosis or infection is quite similar with the exception that a rest perfusion study is required with a sarcoidosis protocol for co-localization of inflammation within the myocardium and to determine whether inflammation is present in the hypoperfusion region (mismatch defect). For sarcoidosis imaging, a dietary preparation is required to suppress the physiological cardiomyocytes uptake of F-18 FDG uptake such that tracer uptake is limited to the active inflammatory cells in the myocardium. This involves avoidance of carbohydrate containing food for 24 h prior to the test with intake of high fat and protein foods for at least two meals 24 h prior followed by an overnight fast. Suppression of myocyte glucose uptake can be assisted by giving IV unfractionated heparin 15–45 min prior to F-18 FDG administration.
The imaging parameters include patient positioning supine with the arms raised above the shoulder level. To localize the heart within the field of view (FOV), a tomogram or scout CT is performed followed by a transmission scan for attenuation correction. Rest or stress emission scans are then performed. For the FDA approved radiotracers, the dose used are: for Rb-82 is 40–60 mCi, N-13 ammonia 10–20 mCi, and for F-18 FDG 5–10 mCi. The scan duration for Rb-82 is 3–7 min, N13 ammonia 10–15 min, and for F-18 FDG 10–30 min.
Of note, rest-stress MPI and viability PET protocols (Fig. 9.2) may be combined to provide information on both ischemia and viability.
Data Interpretation
As outlined by the ASNC guidelines on radionuclide imaging [4, 5], the sequence involves analyzing the raw images, followed by assessment of perfusion abnormalities, evaluation of gated images for left ventricular function, quantification of myocardial blood flow. In addition, with hybrid PET/CT scans, coronary artery calcium and/or coronary CT angiography may be included in the report. Non-cardiac findings should be reviewed and mentioned such as pleural or pericardial effusions, aortic disease, and calcifications, mediastinal or lung masses or nodules. The rest and stress perfusion images and metabolism images should be analyzed for the extent and severity of abnormalities. Extra-cardiac findings should be carefully examined for uptake in organs other than the myocardium particularly the lungs and the mediastinum. Similar to SPECT imaging, PET images are presented in short axis from apex to base, horizontal long axis with septal and lateral walls, and vertical long axis showing the anterior and inferior walls. Interpretation of PET perfusion data (similar to what is described in Chap. 8) should be performed visually/qualitatively first with identification of location and defect severity and extent . The extent can be qualitatively described as small (5–10% of the LV), medium (10–20% of the LV), or large (>20%) of the LV. Defect severity is expressed as mild, moderate, or severe. Myocardium with stress induced perfusion abnormalities, which have normal stress imaging represent ischemia. Perfusion abnormalities present both at rest and stress i.e. fixed defects represents an area of scan or infarction. The 17-segment model with the 5-point scale (Fig. 8.4) is used for the semi-quantitative analysis as outlined in the SPECT chapter.
Absolute quantification of myocardial blood flow is an important aspect of PET imaging that helps in assessing the physiological significance of a known coronary artery stenosis especially if it is in the intermediate range. Both relative and absolute quantification is possible. Quantitative assessment of blood flow is in ml of blood per min per gram of myocardium and is validated for N-13 and Ru-82. Typical values for myocardial flow reserve >2.3 indicated a favorable prognosis whereas a ratio of less than 1.5 suggest diminished blood flow reserve and carries an elevated cardiac risk.
ECG Gated PET images at rest and peak stress provides information on LV function and volumes. Unlike post-stress SPECT, PET images are obtained at peak hyperemia and stress. Regional and global wall motion abnormalities can be identified.
Assessment of myocardial viability plays a central role in PET imaging. Viability studies are able to differentiate a scarred or infarcted myocardium from a hibernating myocardium, which upon revascularization might restore LV function. Rest perfusion imaging is compared to metabolism imaging using FDG uptake (Fig. 9.3). A myocardial perfusion abnormality in combination with no FDG uptake signifies an infarcted and scarred myocardium. An increase in FDG uptake relative to a perfusion abnormality i.e. a mismatch signifies a viable myocardium (Table 9.4).
Assessment of active cardiac sarcoidosis or inflammation involves the uptake of F-18 FDG into the inflamed or infected cells following the dietary patient preparation described [6]. In sarcoidosis imaging, a resting MPI study is obtained and compared to an F-18 FDG study side by side in a the standard short/horizontal/vertical axis views. An F-18 FDG “hot spot” indicated areas of abnormal cardiac inflammation. Different uptakes have been described including focal, diffuse uptake and focal on diffuse uptake. A typical pattern in active sarcoidosis is a “mismatch defect” in which a hot spot or diffuse uptake is localized within a hypoperfused myocardium (Fig. 9.4).
The standard reporting algorithm of myocardial perfusion and metabolism PET studies includes: patient information, indication for the study, history and key clinical findings, type of the study, summary of stress data with stress ECG interpretation, image description and interpretation for perfusion and metabolism, and final impression whether the study is normal or abnormal.
Complications
The complications to pharmacological stress perfusion imaging are presented elsewhere. The risk of PET imaging includes radiation exposure and risk of solid cancers and leukemia due to stochastic effects of ionizing radiation. For instance, the total body effective dose of radiation exposure from a myocardial perfusion using rubidium Rb-82 is approximately 4.1 mSv and from F-18 fluorodeoxyglucose myocardial viability scan is approximately 7.0 mSv. In order to prevent or limit the effects of ionizing radiation, the principle of ALARA (As low as reasonably achievable) should be followed. Hence, appropriate indications for testing should be followed per the ACC/AHA and ASNC appropriate use criteria. Once a proper indication is confirmed, it is important to limit the amount of radiation and to use the lowest possible dose of radioisotopes to obtain accurate images for interpretation.
Clinical Vignettes
Case 1
Seventy-two year old man presents with mild stroke and chest pain . History includes smoking (50 pack year), elevated cholesterol, diabetes. During hospitalization, the resting ECG demonstrated mild inverted t-waves and TnI elevation, also mild. The patient was obese, BMI 35. The patient underwent a rest/ stress dipyridamole PET study with mild chest pain but no ECG changes. Images are shown in Fig. 9.5 .
There was TID and two separate perfusion abnormalities. There was a medium moderate/severe completely reversible antero/lateral and inferolateral defect as well as medium moderate/severe reversible anteroseptal, apical and inferoseptal defect confined to the apical regions. These findings were consistent with two vessel ischemia, circumflex and left anterior descending arteries. The patient underwent coronary catheterization which showed LAD which was occluded in the mid region, a ramus with 60–70% stenosis and circumflex proximal 90% stenosis. This case demonstrates the ability of rest/stress PET to identify not only CAD, but the severity. The accuracy of PET to predict multivessel CAD is significantly better than SPECT (Courtesy of Gary V Heller, MD, PhD).
Case 2
Sixty-eight-year-old female patient presents with congestive heart failure and chest pain. The patient’ s history includes hypertension, and prior MI several years previous. The patient had no history of diabetes. She had been stable until recent chest pain.
The patient underwent cardiac catheterization which demonstrated a 60% stenosis of the left anterior descending (LAD) artery and occluded obtuse marginal artery as well as an occluded right coronary artery with collateralization from the LAD. The patient underwent a rest/ stress dipyridamole PET protocol to evaluate for stress-induced ischemia and myocardial viability, in view of the diseased LAD and occluded vessels. The patient had no symptoms or ECG changes during the pharmacologic stress ( Fig. 9.6 ).
Illustrates the rest/stress Rb-82 results, with an FDG viability assessment . There was normal perfusion in the anterior region with severe fixed defects in the lateral and inferior regions. Gated PET imaging revealed akinesis of portions of the lateral wall as well as inferior, with LVEF at both rest and stress of 34%. The conclusion was that there was no stress-induced-ischemia and non-viability of the inferior and lateral regions consistent with the occluded vessels. Because the ischemia work-up did not demonstrate myocardial viability in areas of concern, a cardiac PET FDG study was performed, which demonstrated marked FDG activity in both the inferior and lateral walls as well as the anterior wall (“mismatch”) consistent with myocardial metabolic viability in both the circumflex and right coronary arteries.
The patient underwent successful by-pass surgery with revascularization of all three major arteries. Six months later the patient was asymptomatic and an echocardiogram revealed mild/moderate hypokinesis of the lateral/inferior walls, with a global ejection fraction of 46% (Courtesy of Gary V Heller, MD, PhD).
Case 3
Fifty-six-year-old female with history of diabetes and morbid obesity (BMI 48) presented with atypical chest pain and dyspnea on exertion for 2 weeks duration. A regadenoson stress SPECT study was ordered by her PCP and performed 10 days prior to her current presentation at an outside hospital with an equivocal stress test report mentioning a small reversible defect in the anterolateral wall that is consistent with ischemia vs differential breast tissue attenuation and a medium fixed defect in the inferior wall consistent with either a prior infarction or inferior wall attenuation. On further interview, she reports the pain as sharp left sided worsened with movement and exercise and lasting less than a minute reproducible with palpation. Due to the atypical features, obesity and equivocal SPECT study, she underwent a regadenoson PET stress test with the images shown in Fig. 9.7 . The myocardial flow reserve (MFR) was calculated at 3.6.
This case represents a typical scenario comparing the superior image quality of PET compared to SPECT especially in the morbidly obese patients. The PET images show normal myocardial perfusion with normal flow reserve (>2). The perfusion defects noted on the SPECT study are most likely due to artifact. Since the quality of the pain is atypical, reproducible by palpation and the PET perfusion is normal, no further cardiac workup is necessary.
Case 4
Sixty-year-old male with a prior history of a relatively late presentation anterior myocardial infarction 20 years prior treated with thrombolytics followed by PCI who has been referred to cardiology for preoperative cardiovascular evaluation prior to vascular surgery. He is asymptomatic from a cardiac perspective but has limited ambulation with METS < 4. Due to the prior history of CAD and low METS, a regadenoson PET stress test was ordered with the images shown shown in Fig. 9.8 .
The above image shows an abnormal PET perfusion study with a medium size stress perfusion defect of severe intensity in the mid to apical anterior, apical septum, apical inferior wall and LV apex that remained essentially unchanged and fixed on rest images. The findings are suggestive of prior myocardial infarction in the mid-LAD territory. No evidence of myocardial ischemia. This patient can likely undergo his surgery without the need for an invasive strategy with a cardiac catheterization. There is also no need to obtain alternate stress testing due to the good quality of the PET study.
References
Dilsizian V, Bacharach SL, Beanlands RS, et al. PET myocardial perfusion and metabolism clinical imaging. J Nucl Cardiol. 2009; https://doi.org/10.1007/s12350-009-9094-9.
Hendel RC, et al. CCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53(23):2201–29.
Klocke FJ, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging – executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 guidelines for the clinical use of cardiac radionuclide imaging). J Am Coll Cardiol. 2003;42(7):1318–33.
Douglas PS, et al. ACCF/ACR/AHA/ASE/ASNC/HRS/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR 2008 health policy statement on structured reporting in cardiovascular imaging. Endorsed by the Society of Nuclear Medicine [added]. Circulation. 2009;119(1):187–200.
Tilkemeier PL, et al. ASNC imaging guidelines for nuclear cardiology procedures. J Nucl Cardiol. 2017;24:2064–128.
Dilsizian V, et al. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 2016;23:1187–226.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Karnabi, E. (2022). Positron Emission Tomography. In: Hendel, R.C., Kimmelstiel, C. (eds) Cardiology Procedures. Springer, Cham. https://doi.org/10.1007/978-3-030-95259-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-95259-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95258-7
Online ISBN: 978-3-030-95259-4
eBook Packages: MedicineMedicine (R0)