Abstract
Both orthognathic and temporomandibular joint (TMJ) surgical procedures that have been practiced separately and successfully for many years with well-established indications. However, there are some patients who may benefit from both types of surgery. These patients include those suffering from congenital and/or developmental conditions that can adversely affect facial growth and development. Other conditions include posttraumatic deformities and pathological conditions of the maxillofacial region that cause facial imbalance and malocclusions if left untreated. Management of these patients is complex and the surgeon often faces challenging dilemmas involving the diagnosis, sequencing of treatment, specific type of surgical procedure required, and long-term follow-up considerations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning Aims-
1.
What patients and indications require both types of surgical procedures?
-
2.
What type of TMJ surgery should be performed for treatment of the TMJ condition?
-
3.
Should orthognathic and TMJ surgery be performed separately as staged surgical procedures or concomitantly in one operation?
-
4.
Which type of surgery (orthognathic or TMJ) should be performed as the first procedure in concomitant surgery?
1 Introduction
Both orthognathic and temporomandibular joint (TMJ) surgical procedures have been practiced successfully for many decades with excellent outcomes. While orthognathic surgery involves performing bony osteotomies of the maxilla and mandible for correction of dentofacial deformities, TMJ surgery involves soft and/or hard tissue procedures in the jaw joint itself for management of intraarticular joint disorders. There are many TMJ conditions (congenital and developmental) that can adversely affect facial growth and development. Some of these conditions can also cause pain, TMJ and jaw dysfunction, and disability. The condyle is an integral component of the TMJs, and is the growth center of the mandible. The TMJs provide the foundation and support for jaw position, jaw function, occlusion, facial balance, normal facial growth and development, as well as comfort during mastication. In the presence of TMJ pathology that affects the condyles, growth may be significantly altered creating dentofacial deformities and treatment outcomes for corrective jaw surgery may be unsatisfactory relative to function, aesthetics, occlusion, skeletal stability, and pain if the TMJ pathology is ignored.
Patients with dentofacial deformities requiring orthognathic surgery may have coexisting TMJ pathology. While orthognathic surgery alone, performed to correct a dentofacial deformity, may help with alleviating pain and dysfunction symptoms, it will not correct an anatomic pathology of the TMJ. Additionally, some research has shown that patients with coexisting dentofacial deformities and TMJ pathology treated only with orthognathic surgery are known to develop worsening of the TMJ dysfunction with an increased incidence of unfavorable treatment outcomes. Orthognathic surgical relapse has been associated with untreated or not recognized TMJ pathology, and so there exists a cohort of patients who require both types of surgical procedures. This chapter discusses the most common TMJ pathologies and their influence on facial growth and development as well as the effects of surgical management to correct the specific TMJ conditions and associated jaw deformities.
While it is common to encounter patients with specific indications for either TMJ or orthognathic surgery to be performed separately, it is relatively infrequent to see patients requiring both types of surgery. For these infrequent patients who require both types of surgery, clinicians are likely to face numerous dilemmas. Preoperative considerations which may arise during treatment planning include the following:
-
1.
What type of TMJ surgery should be performed for treatment of the TMJ condition?
-
2.
Should Orthognathic and TMJ surgery be performed separately as staged surgical procedures or concomitantly in one operation?
-
3.
Which type of surgery should be performed first, whether in staged or concomitant manner?
This chapter will focus on the topic of “Concomitant TMJ and Orthognathic Surgery.”
2 Indications
Broadly speaking, the indications for performing orthognathic surgery in patients requiring TMJ surgery can be classified into two basic groups:
-
1.
Patients with an iatrogenic malocclusion following TMJ surgery: There are some TMJ patients who present with good occlusal and skeletal relationships, but when the TMJ pathology is surgically corrected (e.g., diskectomy, disk repositioning, or other forms of arthroplasty), the occlusion can be significantly altered, thus creating a postsurgical malocclusion. The clinician often sees a premature contact and shift of the occlusion on the ipsilateral side in patients undergoing diskectomy or arthroplasty due to loss of vertical height. In contrast, a shift of the lower incisor midline to the contralateral side with an ipsilateral open bite may be seen in cases following disk repositioning (◘ Fig. 65.1). If these postsurgical occlusal abnormalities are not correctable by nonsurgical methods, orthognathic surgery may be required.
-
2.
Patients with dentofacial deformities requiring orthognathic surgery: Some indications for orthognathic surgery in dentofacial deformity patients with TMJ pathology include internal derangement, idiopathic condylar resorption, condylar hyperplasia, condylar osteochondroma, degenerative condylar disease secondary to connective tissue and autoimmune disease, ankylosis of the TMJ, and, other end-stage conditions, such as multiply operated TMJs. In all these conditions associated with the mandibular condyle, TMJ pathology may be a causative factor of a dentofacial deformity. These conditions will most likely require orthognathic surgery to help alleviate the resultant dentofacial deformities (◘ Fig. 65.2).
2.1 Idiopathic Condylar Resorption
Idiopathic condylar resorption (ICR) is an acquired disorder that results in progressive reduction of the condylar size or mass without an identifiable etiology. The exact etiology that initiates the process of condylar resorption is not known. Classically, ICR affects young women with a class II malocclusion with a high mandibular plane angle. Although some patients can present with none to minimal symptomatology relative to TMJ dysfunction and functional limitations, the progressive reduction in condylar size, volume, and morphology results changes in facial appearance with mandibular retrognathia and anterior open bite malocclusion with a high mandibular plane angle. This can lead to significant distress and disability due to an unaesthetic profile, difficulty with chewing and speech, and possibly airway and breathing disorders in severe cases. The correction of the facial skeletal deformity and malocclusion in patients with ICR can be challenging due to the unpredictable duration period and the variable extent of abnormal condylar activity. Therefore orthognathic surgery alone for ICR should not be even considered until clinical examination and diagnostic investigation have established that the active changes in the condyles have stopped.
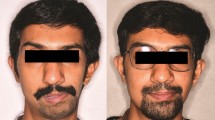
Controversy does exist as to when to proceed with surgical treatment, and to what surgical treatment will provide the most favorable outcome. One of most challenging aspects of treatment is the inability to assess whether condylar resorption is active. Condylar resorption may continue in most individuals for a variable period of time and its duration is unpredictable. Some authors have suggested that the condylar resorption in patients with ICR is mediated by secretory changes in the hypertrophied bilaminar zone of the meniscus. Wolford found stable results with concomitant articular disk repositioning and orthognathic surgery. A later study showed that patients treated with only orthognathic surgery showed significant skeletal and occlusal instability and relapse versus those patients treated with concomitant TMJ and orthognathic surgery. The treatment objectives for patients with ICR are to achieve a stable occlusion without relapse, improved jaw function, and balanced facial proportions. Historically, surgical treatment options for the dentofacial deformity as a result of ICR have included orthognathic surgery with or without TMJ surgery. Many reports have presented limited successful treatment of ICR with orthognathic surgery alone. Over the last two decades, orthognathic surgery and concomitant TMJ surgery have become the gold standard for management of such patients (◘ Fig. 65.3).
21 year old female with progressive mandibular retrusion and open bite formation due to TMJ condylar resorption. This is the same patient shown in Fig. 65.6
2.2 Condylar Hyperplasia
Condylar hyperplasia can affect the mandibular condyles causing overgrowth of the mandible. Unilateral condylar hyperplasia can produce a progressive deviated prognathism, with facial asymmetry (◘ Fig. 65.4). The condition of “bilateral condylar hyperplasia” is rare and controversial, but it can produce progressive prognathism which keeps progressing beyond skeletal maturity timelines of other bones. It should be noted that not all prognathic mandibles are the result of bilateral condylar hyperplasia. Condylar hyperplasia can continue into the patient’s mid-20s. A careful history of accelerated mandibular growth initiating at the time of puberty, which continues beyond normal growth years is diagnostic for condylar hyperplasia. Posterior open bite may be observed as super-eruption of the maxillary dentition may not keep up with the accelerated condylar growth. Contemporary treatment protocols include a high condylectomy to arrest condylar growth, articular disk repositioning (questionable value in staged surgery, but shown to be of value in concomitant surgery), and concomitant orthognathic surgery to address the facial asymmetry and class III skeletal sequelae of condylar hyperplasia.
2.3 Osteochondroma of the Mandibular Condyle
An osteochondroma of the mandibular condyle is an exophytic lesion that arises from the cortex of bone and is cartilage capped. Enlargement of the mandibular condyle creates a progressive, asymmetric dentofacial deformity (◘ Fig. 65.5). Although classic treatment recommendation involves condylar sacrifice and immediate or staged reconstruction with autogenous or alloplastic TMJ replacements, more recently, a conservative low condylectomy procedure which involves preserving the condylar neck has been shown to predictably treat an osteochondroma. The remaining condylar neck can be recontoured as functional condyle with the articular disk stabilized to it, when indicated. Concomitant orthognathic surgery after osteochondroma resection with a sagittal split ramus osteotomy allows the residual condylar neck to be positioned more superiorly into the fossa.
As mentioned above, placement of joint replacement prostheses can also be performed to reconstruct the mandibular condyle. Other orthognathic procedures may be indicated such as repositioning the posterior maxillary segment if supra-eruption of the segment has occurred as a result of the osteochondroma growth. A segmental posterior maxillary osteotomy (Kufner technique) allows the condylar neck to be elevated more superiorly by creating vertical space to reposition the condylar stump more superiorly.
2.4 Autoimmune/Connective Tissue (CT) TMJ Diseases
Many disorders that affect any joint in the body can also affect the TMJ as well. The autoimmune/CT diseases are broadly divided between rheumatoid arthritis (RA), and the seronegative spondyloarthropathies that are negative for the presence of rheumatoid factor. These include psoriatic arthritis, lupus arthritis, scleroderma, ankylosing spondylitis, arthritis associated with inflammatory bowel disease, and reactive arthritis. All have been reported to affect the TMJ. Juvenile idiopathic arthritis, which can be positive or negative for rheumatoid factor, can also commonly affect the TMJ leading to destruction of the condylar growth center. The metabolic diseases of gout and pseudogout have also been known to affect the TMJ. These systemic diseases induce degenerative joint disease characterized by abnormal disk position, abnormal disk morphology, osseous changes in the mandibular condyle, deformity of the articular eminence/glenoid fossa, and abnormal bone marrow signal of the mandibular condyle. The resultant degenerative changes of the mandibular condyle typically result in a decrease in condylar height that subsequently leads to the presence of a high occlusal plane angle, antegonial notching, increased mandibular plane angle, decreased chin projection, and A-P mandibular deficiency (◘ Fig. 65.6). Compensatory vertical maxillary excess, anterior open bite, decreased posterior airway space, and sleep apnea symptoms can all result. Spatially, the maxillomandibular complex is rotated downward and backward by the loss of volume and decrease in the height of the mandibular condyle/ramus. A decrease in maximal incisal opening and pain upon opening commonly occurs and has been shown to have high specificity with TMJ synovitis. Many studies have shown extremely predictable outcomes with surgical management of TMJ pathology and dentofacial deformity concomitantly in these patients. Recent studies have shown that patients with autoimmune or connective tissue disease had worse treatment outcomes when treated with autogenous tissues versus TMJ reconstruction with alloplastic total joint prostheses. TMJ reconstruction with costochondral grafting in patients with rheumatoid arthritis had relapse and resultant open bite malocclusion of approximately 20%. In contrast, many studies have shown better and more predictable outcomes with surgical management involving concomitant orthognathic surgery and alloplastic joint replacement.
21 year-old female with the typical dentofacial deformity that is seen in patients suffering from condylar resorption during growth. Note mandibular retrognathism, steep mandibular and occlusal planes, lip incompetence, vertical maxillary excess, short chin-neck length, and loss of posterior facial height
2.5 Craniofacial Syndromes
Patients with congenital conditions such as hemifacial microsomia and Treacher-Collins syndrome may benefit from TMJ reconstruction and concomitant orthognathic surgical procedures. When the condyles are congenitally missing or hypoplastic , autogenous grafts, i.e., rib grafts, or custom-made total joint prosthesis can be utilized to reconstruct the condyle/ramus unit. Additionally the mandible can be advanced and/or vertically lengthened, as indicated, to help alleviate the accompanying dentofacial deformity. A custom-fitted fossa component can be fabricated and fixated to the temporal bone in cases where the fossa or zygomatic arch are either underdeveloped or absent. Surgery in these cases involves an open arthroplasty-type procedure with or without joint reconstruction to lengthen the posterior ramus and facial height, and jaw osteotomies from intraoral and/or extraoral approaches . Additional facial bone augmentation or reduction procedures with autogenous bone and/or alloplastic implants are often performed at the same time as concomitant surgery to further improve facial balance and symmetry.
2.6 TMJ Ankylosis
TMJ bony pathology, particularly ankylosis in young, growing patients can cause profound morphological changes in the mandible, resulting in significant facial asymmetry. These pathologic anatomical changes are especially pronounced when they occur unilaterally and can be significantly worse when the insult occurs during the growing years of the patient’s life. The morphological changes caused by ankylosis have the potential to disseminate their effects to surrounding facial soft tissues and bones, especially the maxilla, further complicating treatment. Proper management and surgical treatment of these patients must aim to correct both the functional and aesthetic sequelae associated with these pathologies.
Treatment of patients with TMJ ankylosis presents a unique challenge to surgeons for multiple reasons. Growth of the patient and the timing of the surgery must be carefully considered, as alloplastic solutions do not grow with the patient. Autograft techniques usually provide unpredictable growth and may be susceptible to the original disease process, causing recurrence. As craniofacial syndromes and TMJ ankylosis disease processes often effect the growing patient, the surgeon may decide to proceed with early surgery to restore function and aesthetics with the potential drawback of needing future surgical correction of any growth that compromises the results. Alternatively, the surgeon may decide to wait until growth is complete prior to definitive reconstruction that would secure a stable result, but may leave the patient with a dentofacial deformity, functional limitations, and a decreased quality of life throughout the remainder of their growing years. Concomitant orthognathic surgery is often necessary to help correct the dentofacial deformity involving the surrounding skeletal and soft tissue structures. Due to the 3-dimensional complexity of craniofacial syndromes, TMJ ankylosis, and associated asymmetries, virtual surgical planning (VSP) is an indispensable tool to achieve optimal outcomes.
3 Clinical Scenarios Benefiting from Concomitant Surgery Procedures
3.1 TMJ Disk Repositioning Causing Malocclusion
Displacement of the articular disk usually results in decreased posterior and superior joint spaces. Over time, the displaced disks usually tend to thicken, lose flexibility, and shorten anteroposteriorly. Thus, when such deformed disks are repositioned, the condyle is displaced downward and forward, thereby shifting the mandible anteriorly. In patients with a class I dental occlusion before surgery, the mandible often shifts forward, leading to an end-to-end incisor relationship and a posterior open bite (“iatrogenic” malocclusion caused by the TMJ disk repositioning surgery). In these cases, the performance of an ipsilateral mandibular ramus sagittal split osteotomy after the disk-repositioning procedure concomitantly at the same operation maintains the presurgical occlusion. The concomitant surgery has the benefit of harmonizing the occlusal relationship immediately, thereby avoiding class III elastics mechanics and active orthodontic therapy, which could cause increased pressure and loading on the recently operated joint. An alternative, nonsurgical approach would be not to perform orthognathic surgery, but rather manage the iatrogenically created malocclusion with splints, guiding elastics, and orthodontics.
3.2 Patient with TMJ Internal Derangement and a Coexisting Dentofacial Deformity
There is controversy regarding the management of patients with internal derangement of the TMJ (including degenerative joint disease) and/or patients with pain who also require orthognathic surgery for the correction of coexisting malocclusion and jaw deformities. There are currently two significantly divergent philosophies relative to surgical treatment options for these patients: a) some clinicians contend that orthognathic surgical procedures help in the reduction of TMJ dysfunction and symptoms; and b) others have shown that orthognathic surgery may cause deleterious effects on the TMJ, and thus worsen the symptoms and dysfunction after surgery. The proponents of the latter philosophy propose surgical management of the TMJ either as an initial separate procedure or in the same operation as the orthognathic surgery procedure (concomitant surgery). The basis for this approach is that orthognathic surgery by itself alone in the presence of TMJ internal derangement can result in unsatisfactory outcomes, including worsening pain, condylar resorption, and relapse in many patients. A study published in 2003 showed that patients with preexisting TMJ dysfunction undergoing orthognathic surgery, particularly mandibular advancement, were likely to have significant worsening of the TMJ dysfunction after surgery. The conclusions of the study were that TMJ dysfunction must be closely evaluated, surgically treated with disk repositioning when necessary, and continuously monitored after surgery in the orthognathic surgery patient.
3.3 TMJ Arthroplasty (Osseous Condylar Procedures) and Concomitant Orthognathic Surgery
Condylar hyperactivity conditions, as mentioned previously in this chapter, are surgically managed by intrarticular TMJ surgery, which involves removal of variable portions of the mandibular condyle. Three distinct levels of condylectomy have been published (◘ Fig. 65.7): a) high condylectomy: removal of the cartilage cap (usually 2–4 mm of the condylar head) – used for condylar hyperplasia; b) low condylectomy: mid-level condylar cut used for management of lesions such as osteochondromas and early ankylosis; and c) complete condylectomy: complete removal of the condyle used in cases such as advanced ankylosis. The change in occlusion and facial symmetry is often dependent on the amount of condylar bone removed. Ipsilateral shift of dental midlines, with premature dental contact on the operated side and open bite formation on the contralateral side is expected. The lower face and chin point deviate to the affected side. Orthognathic correction of the dentofacial deformity has been historically performed secondarily as a separate, staged procedure, but many surgeons prefer to perform concomitant surgery in the same operation for one-stage, comprehensive correction of the dentofacial deformity.
4 Expected Outcomes of Concomitant TMJ Disk Surgery and Orthognathic Surgery
Although there is extensive literature regarding concomitant surgery, most published data is limited to a few practitioners, as this type of surgery is not performed by most surgeons in high volumes. Wolford and colleagues evaluated the outcome of concomitant temporomandibular joint and orthognathic surgery in patients with TMJ articular disk dislocation and coexisting dentofacial deformities. The records of 70 patients treated with TMJ articular disk-repositioning surgery and concomitant orthognathic surgery (double jaw or only mandibular surgery) were retrospectively evaluated. Patients were divided into the following three groups: group 1 patients had mandibular advancement; group 2 patients had mandibular setback; and, group 3 patients had a mandible that remained in the original position. The results of their study showed that subjective TMJ pain levels and mouth opening improved in all three groups after surgery. Only one patient had significant condylar resorption after surgery. The orthognathic procedures were found to be stable in the long term. Concomitant TMJ disk repositioning and orthognathic surgery had an overall success rate of 91.4% for patients with less than 4 years of TMJ pain history but significantly lower success (approximately 60%) for patients who had a longer duration of history of TMJ pain and disk displacement.
5 Autogenous Versus Alloplastic TMJ Reconstruction in Concomitant Surgery
Debilitated mandibular condyles, whether from trauma, pathology, developmental abnormalities, autoimmune/CT disease, TMJ ankylosis, or multiply operated joints, have been historically reconstructed with autogenous tissue to re-establish the condylar/ramus unit, and to improve jaw function. Autogenous tissues used have included metatarsal, fibula, tibia, iliac crest, costochondral, and sternoclavicular grafts. The use of costochondral grafts has been advocated in the growing child; however, this growth potential has been stated to be unpredictable. Costochondral grafts often result in overgrowth, or growth with an incorrect vector that is horizontal rather than vertical, and can commonly become ankylosed. The introduction of alloplastic TMJ total joint reconstruction has resulted in improvement in the quality of life for many TMJ patients that have unsalvageable, debilitated anatomic and dysfunctional joints. The use of alloplastic materials to reconstruct the TMJ also obviates the need for a donor site, and provides a stable base for subsequent orthognathic procedures.
6 Diagnosis and Treatment Planning
A comprehensive diagnosis, including identification of the causative factors, as well as an inclusive treatment plan that can be achieved through a thorough and complete workup, including clinical (general and face/jaw-focused), radiographic (basic and advanced imaging), dental model (stone models or digital models), and establishing specific surgical treatment objectives (standard or three-dimensional virtual planning).
6.1 General Patient Evaluation
A thorough evaluation of the patient begins with data gathering from various sources at the initial consultations. These include a comprehensive intra- and extra-oral examination, clinical photographs, diagnostic imaging, and mounted dental models. One must take into account the periodontal and restorative health of the oral cavity. Gingival/periodontal inflammation must be controlled before orthodontic or surgical treatment is started. Comprehensive periodontal therapy may be necessary to ensure optimal health of oral tissues during the entire course of treatment. The importance of good oral hygiene must be stressed to the patient. A restorative check-up is done to evaluate for any faulty restorations or carious lesions. Carious lesions should be restored and hopeless teeth should be extracted.
6.2 Problem-Focused Specific Evaluation
Patients requiring concomitant TMJ and orthognathic surgery need detailed examination of the head and neck region. From an orthognathic perspective, examination from multiple angles, including frontal, profile, and submentovertex views is recommended. Asymmetry often is least at the cranial base level and increases at lower levels of the face with the mandible and chin commonly exhibiting the greatest asymmetry. Clinical photographs help in assessing the facial aesthetics and symmetry. Standard vertical and transverse facial proportions are recorded. Relative to assessment of facial profile, it is important to remember that patients with facial deformities often hold their heads abnormally for functional and/or aesthetic reasons. In patients with deficient mandibles, it is not unusual to find the head is often tipped upward to improve chin projection and also open the oropharyngeal airway. Therefore, it is helpful to posture the head so that the clinical Frankfort horizontal plane (a line from the tragus of the ear through the palpable bony infraorbital rim) is parallel to the floor.
A standard yet comprehensive TMJ examination is essential to record baseline examination. At a minimum, this should include assessment of subjective parameters, preferably with visual analog scores to evaluate jaw function, disability, TMJ dysfunction, and pain. Objective TMJ evaluation should include maximal interincisal opening, both with and without pain or discomfort, deviation on opening, excursive measurements during lateral movements and protrusion, and myofascial pain.
6.3 Age for Surgical Intervention
The general age considerations for concomitant surgery are not different than routine orthognathic surgery guidelines. Although there are individual variations, females usually have the majority of their facial growth (98%) complete by the age of 15 years and males by the age of 17 to 18 years. So, for the most part, concomitant surgery can be performed any time after an individual has reached these ages. Additionally, the surgeon and orthodontist should familiarize themselves with the following concepts:
-
1.
Le Fort I osteotomy with downfracture will essentially stop most, if not all anteroposterior growth of the maxilla after surgery.
-
2.
Sagittal split osteotomies do not affect postsurgical mandibular growth directly.
-
3.
Some TMJ procedures will interfere with postsurgical mandibular growth, while others may not. For example, a high condylectomy (condylar shave) type of procedure which is recommended for the management of condylar hyperplasia is effective in stopping further growth on the operated site. A complete condylectomy procedure may be used for removal of a tumor and also leads to cessation of postsurgical growth on the operated side. Contrary to these procedures, a TMJ disk repositioning procedure may or may not affect postsurgical growth, depending on trauma from surgery, condylar cartilage cap damage, etc.
Generally speaking, the predictability of results with correction of the jaw and TMJ-related deformities with one major operation are best achieved by waiting until facial growth is relatively complete. However, there are some indications for performing surgery during the growing years such as progressive TMJ deterioration, ankylosis, masticatory dysfunction, tumor removal, pain, sleep apnea, etc. Performing surgery during growth may result in the need for additional surgery at a later time to correct a resultant deformity and malocclusion that may develop during the completion of growth. When concomitant surgery is performed during the growing years, there is a greater probability for additional revision surgery later, especially with unilateral prosthetic TMJ replacement. In addition, as mentioned above, some orthognathic surgical procedures have a profound affect on subsequent facial growth and development, including maxillary Le Fort I osteotomies, as maxillary A-P growth is stopped, but the vertical alveolar growth of the maxilla and mandible continues contributing to a downward and backward rotation vector of facial growth. In these cases, occlusion may remain intact. Therefore, bilateral TMJ patient-fitted total joint prostheses and maxillary osteotomies can be performed at an earlier age with predictable results, since both upper and lower jaw postsurgical growth would be eliminated by the respective TMJ and maxillary surgical procedures.
7 Preoperative Considerations
The initial presurgical workup includes a thorough history and physical, including evaluation of range of motion, with the recording of objective and subjective findings. Use of a standardized examination technique is recommended. If concomitant orthognathic surgery is to be performed, complete maxillary and mandibular impressions with face-bow record, plain films, bite registration, and dedicated maxillofacial CT scan using a specific scanning protocol are required. Intraoral scanning with digitization of the preoperative workup is becoming more popular and is likely to replace traditional impressions and model surgery in the near future.
Using the CT data, a three-dimensional stereolithographic model of the TMJ and associated structures is then fabricated. This model can be ordered as a one-piece (if no jaw repositioning is required) or two-piece model if orthognathic movements are to be performed. Models should then be mounted on an articulator if traditional model surgery is used without VSP. Using the original cephalometric tracing and predictions tracing, surgery is then performed on the stereolithographic model, which includes removal of the condyle, bony recontouring of the fossa and the ramus components, and correcting the spatial positioning of the mandible, if concomitant lower jaw repositioning is included as part of the surgical treatment plan. The mandible on the stereolithic model is virtually placed into its future predetermined position using the planned measurements for correction of mandibular anteroposterior and vertical positions as well as pitch, yaw, roll. The stereolithic model is then trimmed until the desired changes in anatomy are achieved. The surgeons with the software personnel and bioengineers together review the model to ensure that a sufficient gap has been created between the base of the skull and ramus, and to determine if the coronoid process will be resected at the time of surgery (often impinges on the zygomatic bone if significant mandibular advancements are to be performed using the joint prostheses). All changes that are made to the stereolithographic model must be reproduced by the surgeon during the actual surgical procedure. Custom-made templates are then fabricated by the manufacturer duplicating the topography of the final prosthesis. The fit, anatomy, angulation, and placement of screw holes are verified by the surgeon and any changes to the template are discussed with the manufacturer before construction of the custom-made prosthesis. The mandible is placed in its new position based on the cephalometric surgical treatment objectives. Standard model surgery or virtual surgical planning is performed with the jaw repositioning movements duplicated as on the stereolithic model, and a surgical splint fabricated. If computerized VSP is to be used for concomitant TMJ and orthognathic surgery planning (◘ Fig. 65.8a), the data from the CT scan can be transferred from the TMJ prosthesis manufacturer to the medical modeling vendor. Dental models or intraoral dental scans are sent to the medical modeling vendor for scanning and simulation into the virtual surgical models. Construction of intermediate and final surgical splints is then completed from the computer simulated surgery, and the prostheses are manufactured with the lower jaw in the new anatomically correct, repositioned position (◘ Fig. 65.8b and c). Use of cone beam CT scan data, integrated models or intraoral digital occlusion scans, and computer-based VSP in the presurgical phase can facilitate precision planning and splint fabrication. Use of VSP reduces laboratory time by eliminating the need for model surgery, increases operator efficiency, and accuracy besides aiding in fabrication of better quality splints.
Use of computer-guided digital planning in combined orthognathic and TMJ surgery. A high resolution CT scan is obtained and the orthognathic jaw repositioning movements are finalized digitally, usually in an interactive computer conference with engineers and designers over a virtual platform. This data is then used to fabricate surgical splints. The data is also separately transmitted to the TMJ prostheses manufacturing company so their engineers can integrate it into their system, and fabricate the prostheses to conform to the repositioned jaws
8 Surgical Sequencing
The surgical sequencing of concomitant orthognathic and TMJ surgery is important in achieving optimal surgical outcomes. When performing disk procedures, TMJ surgery is always performed first, followed by mandibular sagittal split ramus osteotomies with rigid fixation, and, finally, maxillary osteotomies with rigid fixation. This sequence allows the change in mandibular position as a result of TMJ disk surgery to be of little consequence as the mandibular ramus sagittal split osteotomies will allow the best occlusal fit with the maxilla in single jaw surgery or with the intermediate splint with two-jaw surgery. TMJ arthroplasty remains the first procedure when using TMJ total joint prostheses also. This allows for sterile access to the joint and neck regions. In most instances, the usual sequence is as follows:
-
1.
Extraoral surgery – TMJ surgery.
-
(a)
Condylectomy
-
(b)
Coronoidotomy or coronoidectomy, if required (performed from either TMJ or neck incision(s))
-
(a)
-
2.
Mandible repositioning.
-
(a)
Muscular detachment – masseter and medial pterygoid muscles from ramus
-
(b)
Mobilize mandible
-
(a)
-
3.
Isolation of extraoral surgical sites followed by intraoral placement of maxillomandibular fixation with intermediate surgical splint in position.
-
4.
Extraoral surgery – TMJ total joint prostheses placement followed by closure of all external incisions in the sterile field.
-
5.
Intraoral maxillary surgery.
9 Intraoperative Considerations
The operative management of patients needing both TMJ reconstruction of condyle/ramus unit and correction of a coexisting dentofacial deformity requires the coordination of operative sterile and “dirty” fields. The head wrap as well as stabilization of the endotracheal tube will be critical due to the length of surgery, rotating the head side to side to obtain adequate visualization of both TMJs, especially if bilateral TMJ surgery is indicated. Surgery then proceeds in a sterile manner. The oral cavity is isolated from the operative field by an occlusive dressing. The TMJ is usually approached via an endaural or preauricular incision, and the mandibular ramus is approached via some form of a submandibular or retromandibular incision. Condylectomy, debridement, and bone recontouring are accomplished as previously determined during model surgery and joint fabrication process. The sterile field is then covered and draped with new drapes prior to entering the oral cavity. Instruments that are used in the mouth to place the patient into maxillomandibular fixation and the splint are passed to a designated dirty table until all TMJ incisions are closed and dressed. The oral cavity is then isolated again with an occlusal dressing. The now dirty drapes are removed. Depending on operator preference, some recommend that the surgeon(s) regown, reglove, and redrape the patient for the subsequent sterile surgical procedures. In our experience, regloving is usually sufficient as long as the surgical drapes and gowns can be kept sterile by covering them with sterile sheets during the transient intraoral access part for maxillomandibular fixation. It should be noted that efficiently rotating sterile and contaminated fields multiple times during a long surgical procedure requires considerable experience. Contamination of the field or prostheses with intraoral contents could be detrimental, and can lead to serious infections and morbidity.
The fossa component of the prosthesis is inserted through the endaural or preauricular incision and is stabilized to the zygomatic arch with three to four screws. The mandibular component is inserted via the neck incision and fixated to the lateral surface of the ramus with eight to ten screws. Autogenous fat grafts, harvested from the abdomen or buttocks, may be packed around the joint prosthesis. In our experience, this is recommended only in cases where there is increased chance of heterotropic bone formation (ankylosis, multiply operated patient, etc.), and not for resorptive cases. Once all TMJ incisions are closed and dressed, surgical repositioning of the maxilla and other indicated surgical procedures are then performed using standard clean techniques. At completion of surgery, light guiding elastics are placed. Prior to emergence from general anesthesia, a nasogastric tube is passed to evacuate blood, which may cause postoperative nausea due to gastric irritation.
10 Postsurgical Management
Postsurgical patient management is critical for high-quality patient treatment outcomes that are predictable. Both the surgeon and the orthodontist can positively affect treatment outcome with combined understanding of the treatment objectives. A good initial surgical outcome can be adversely compromised by a lack of proper patient management by the surgeon and orthodontist. Conversely, a compromised surgical result may be salvaged by aggressive postsurgical orthodontics. The surgeon should see the patient weekly during the first month to check the occlusion, patient progress, and make any indicated changes in the elastics or orthodontic mechanics to maximize the occlusal relationships. Use of appropriate elastic mechanics can often help correct minor anteroposterior occlusal discrepancies, especially as the alloplastic joints are relatively “mobile” as all muscles are detached.
The postsurgical course for any patient is based upon individual variability to the psychological and physical challenges of surgery. The severity, duration, impact of preexisting dentofacial and TMJ functional deficiencies can adversely affect the postsurgical recovery. The challenges of recovery involve all the major systems for daily life. Breathing, swallowing, nutrition, speech, muscle forces, and facial sensation are affected to varying degrees due to the repositioned dentofacial structures and “new “ TMJ function. Fatigue from the long general anesthetic is also expected. Postoperative facial swelling usually reaches maximum levels at 3–4 days after surgery before dissipating slowly over weeks and this can be distressing psychologically. Simple reassurance and ice packs with an elevated head position will help. Postsurgical nasal and pharyngeal bloody drainage is to be expected if maxillary osteotomies have been performed. The drainage usually slows down within 6–12 hours. Local hemostatic agents placed into the pterygomaxillary region after maxillary downfracture may reduce postoperative bloody sinus drainage. As it is often difficult for patients to swallow following surgery because of a sore throat, numbness, altered tongue position, and splints, a nasogastric tube can be utilized to feed patients overnight with nutritious protein drinks and can help reduce the calorie deficiency that occurs during the day of surgery and start postoperative day 1 with improved nutrition prior to resuming PO intake. Active jaw function is encouraged immediately. Most patents do not require formal physical therapy referral. Simple jaw opening and closing type exercises, advancing PO intake as tolerated are sufficient for jaw movement. Patients are placed on a soft diet for approximately 3–4 months to allow initial phase of bone healing to occur especially if maxillary osteotomies and bone grafting were performed. Postsurgical finishing orthodontics can resume after about 4–6 or so weeks of healing time.
11 Complications
As with any surgical procedure, there is always an inherent risk of complications, each of which may need to be adequately managed. Poor surgery outcomes usually are related to wrong diagnosis, wrong surgical procedure, poorly executed surgery, surgical complications, inadequate follow-up care, and/or unrecognized or untreatable local and/or systemic factors. Adverse outcomes may be related to preexisting medical conditions, patient compliance, previous surgical history, and complexity of the operation. Unrecognized or untreated TMJ pathology can be a primary factor leading to postsurgical complications that result in undesirable and unpredictable outcomes. The most common complications associated with TMJ surgery include the following: Infection, pain/worsening of TMJ symptoms, breakdown and loosening of the prosthesis, facial nerve injuries, and metal hypersensitivity. TMJ total joint replacement infections are challenging to treat due to difficulty in diagnosing low grade infections and poor antibiotic availability within the biofilm formation. Infection commonly occurs from skin flora, with the oral cavity, nasal cavity, ear canal, and hair follicles as possible sites from which contamination may occur. Staphylococcus species are the most commonly associated micro-organism with TMJ surgery. Orthognathic complications are not discussed as they are beyond the scope of this chapter.
12 Case Presentations
12.1 Active Condylar Resorption and Dentofacial Deformity (◘ Figs. 65.9 and 65.10)
A 23-year old female presented with TMJ-related complications following orthognathic surgery performed previously by an outside surgeon. Her postoperative course was complicated by relapse and significant bilateral condylar resorption, with progressive mandibular retrusion. Clinical examination revealed a retrognathic mandible, class II skeletal and dental malocclusion with an anterior open bite (◘ Figs. 65.9 and 65.10). The patient had severe TMJ pain with significant dietary limitations and maximum interincisal opening of 16 mm.
(a) Cephalometric radiograph after initial orthognathic surgery showing an existing open bite and class II skeletal relationship. (b) Cephalometric exam after concomitant TMJ and orthognathic surgery showing correction of the skeletal and occlusal deformity with surgery including bilateral alloplastic TMJ replacement. (c) Panoramic radiograph after initial orthognathic surgery showing bilateral TMJ degeneration which caused progressive mandibular retrusion. (d) Final postoperative panoramic radiograph after revision orthognathic surgery, bilateral TMJ alloplastic replacement, and genioplasty
This patient was treated by a single-stage, concomitant TMJ and orthognathic surgery operation with the following procedures:
-
1.
Bilateral TMJ condylectomy and glenoid fossa debridement.
-
2.
Bilateral TMJ reconstruction with patient-fitted TMJ Concepts prosthesis.
-
3.
Mandibular advancement in counterclockwise direction.
-
4.
Le Fort I osteotomy of maxilla with rigid fixation and bone grafting.
-
5.
Bilateral mandibular coronoidectomies.
-
6.
Sliding genioplasty.
At the 3-year postoperative period, patient had no significant TMJ pain with maximal interincisal opening greater than 35 mm, and minimal to no dietary restrictions. The orthognathic movements have been stable (◘ Fig. 65.10). She completed orthodontic treatment and has stable and reproducible occlusion.
Note: the case was finished by the orthodontist with a crossbite tendency on the right side; this was planned preoperatively as the patient decided against segmental maxillary surgery in view of her previous complication.
12.2 TMJ Connective Tissue Disease and Dentofacial Deformity (◘ Fig. 65.11)
An adult female patient with degenerative TMJ arthritis secondary to systemic connective tissue disease who developed progressive mandibular retrusion and worsening class II deformity. This patient was treated by a single concomitant TMJ and orthognathic surgery operation with the following procedures for comprehensive functional and aesthetic correction of the dentofacial deformity:
-
1.
Bilateral TMJ reconstruction with patient-fitted TMJ Concepts prostheses
-
2.
Mandibular advancement in counterclockwise direction.
-
3.
Le Fort I osteotomy of maxilla with rigid fixation and bone grafting
-
4.
Augmentation genioplasty with chin implant.
(a) Preoperative frontal and profile facial photographs of the patient. She gave a history of progressive mandibular retrusion and worsening open bite. (b) Preoperative panoramic radiograph showing bilateral TMJ degenerative arthritic changes. (c) Preoperative cephalometric radiograph showing the skeletal open bite, a Class II deformity with mandibular retrognathism and decreased posterior airway space. (d) Postoperative profile and frontal facial photographs after concomitant TMJ and orthognathic surgery. (e) Postoperative cephalometric radiograph showing correction of the dentofacial deformity with concomitant surgery. (f) Postoperative panoramic radiograph demonstrating skeletal structures after bilateral TMJ alloplastic reconstruction, Le Fort I osteotomy, large mandibular advancement, and alloplastic chin augmentation
At the 2-year postoperative period, patient had no TMJ pain and maximal interincisal opening greater than 40 mm. The orthognathic movements have been stable.
12 Conclusion
TMJ pathology can be present at birth or develop during growth, creating facial deformities. During the past three decades, major advancements have been made in TMJ diagnostics and the development of surgical procedures to treat and rehabilitate the pathological, dysfunctional, and painful TMJ. With the appropriate selection of the surgical procedure and age factors taken into consideration, predictable results can be achieved in many patients with concomitant TMJ and orthognathic surgery. Research has repeatedly demonstrated that TMJ and orthognathic surgery can be performed safely and predictably at the same operation, but it does necessitate making the correct diagnosis and accurate treatment planning. Concomitant surgery requires the surgeon to have expertise in both TMJ and orthognathic surgical procedures.
Although autogenous TMJ reconstruction has its place, current trends in concomitant surgery and evidence-based literature suggest that alloplastic joint replacement with orthognathic surgery is the preferred approach for most patients. The ultimate goal of treatment, whichever method used, is to ensure that TMJ condition correction remains stable and the surgeon is able to achieve a stable occlusion with a functional jaw joint, and, maintain and/or or improve airway and facial aesthetics. Alloplastic total joint prostheses have the benefit of immediate return to function, decreased pain, and resistance to the original pathological process with no potential for recurrence, which makes this surgical option very predictable. Traditional orthognathic surgery, especially Le Fort I osteotomies, are often required to correct the concomitant asymmetries or dentofacial deformities that are often present in these patients. In the hands of an experienced surgeon, concomitant TMJ and orthognathic surgery can lead to stable and reproducible outcomes and ultimately, profound improvements in a patient’s quality of life.
Bibliography
Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg. 2003;61:655.
Fuselier C, Wolford LM, Pitta M, et al. Condylar changes after orthognathic surgery with untreated TMJ internal derangement. J Oral Maxillofac Surg. 1998;56:61(suppl 1).
Moore KG, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption in orthognathic surgery: a retrospective study. J Oral Maxillofac Surg. 1991;49:448.
Wolford LM, Karras SC, Mehra P. Concomitant temporomandibular joint and orthognathic surgery: a preliminary report. J Oral Maxillofac Surg. 2002;60:356.
Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion--idiopathic condylar resorption. Part I Am J Orthod Dentofac Orthop. 1996;110:8.
Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II Am J Orthod Dentofac Orthop. 1996;110:117.
Chuong R, Piper MA. Avascular necrosis of the mandibular condyle-pathogenesis and concepts of management. Oral Surg Oral Med Oral Pathol. 1993;75:428.
Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofac Orthop. 1999;116:667.
Arnett GW, Gunson MJ. Management of condylar resorption before, during, and after orthognathic surgery. Int J Oral Maxillofac Surg. 2011;40:1021.
Morales-Ryan CA, Garcia-Morales P, Wolford LM. Idiopathic condylar resorption: outcome assessment of the TMJ disc repositioning and orthognathic surgery. J Oral Maxillofac Surg. 2002;59:(suppl 1)53.
Crawford JG, Stoelinga PJ, et al. Stability after reoperation for progressive condylar resorption after orthognathic surgery: report of seven cases. J Oral Maxillofac Surg. 1994;52(5):460.
Hoppenreijs TJ, Stoelinga PJ, et al. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999;28(6):411.
Mercuri LG. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar resorption. J Oral Maxillofac Surg. 2007;65(8):1600.
Huang YL, Pogrel MA, et al. Diagnosis and management of condylar resorption. J Oral Maxillofac Surg. 1997;55(2):114.
Troulis MJ, Tayebaty FT, et al. Condylectomy and costochondral graft reconstruction for treatment of active idiopathic condylar resorption. J Oral Maxillofac Surg. 2008;66(1):65.
Wolford LM, Goncalves JR. Condylar resorption of the temporomandibular joint:how do we treat it? Oral Maxillofac Surg Clin North Am. 2015;27(1):47.
Zuleima C, Breton P, et al. Management of dentoskeletal deformity due to condylar resorption: literature review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121(2):126.
Sansare KM, Raghav, et al. Management-related outcomes and radiographic findings of idiopathic condylar resorption: a systematic review. Int J Oral Maxillofac Surg. 2015;44(2):209.
Teitelbaum J, Bouletreau P, et al. Is condylar resorption a contra-indication for surgery? Rev Stomatol Chir Maxillofac. 2007;108(3):193.
Gunson MJ, Arnett GW, et al. Pathophysiology and pharmacologic control of osseous mandibular condylar resorption. J Oral Maxillofac Surg. 21012;70(8):1918.
Chung CJ, Choi YJ, et al. (2011). Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption.; am J Orthod Dentofacial Orthop 2011;140(3):404.
Movahed R, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery using computer-assisted surgical simulation. Oral Maxillofac Surg Clin North Am. 2015;27(1):37.
Mehra P, He J, Norris O. Idiopathic condylar resorption: Analysis of outcomes following total joint replacement. J Oral Maxillofac Surg. 2012;70:Supplement e30.
Chigurupati R, Mehra P. Surgical management of idiopathic condylar resorption: orthognathic surgery versus temporomandibular total joint replacement. Oral Maxillofac Surg Clin North Am. 2018;30:355.
Wolford LM, Mehra P, Reiche-Fischel O, et al. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofac Orthop. 2002;121:136.
Garcia-Morales P, Wolford LM, Mehra P, et al. Efficacy of high condylectomy for management of condylar hyperplasia. J Oral Maxillofac Surg. 2001;59:106(suppl 1).
Henry CH, Granite EL, Rafeto LK. Osteochondroma of the mandibular condyle: report of a case and review of the literature. J Oral Maxillofac Surg. 1992;50:1102.
Wolford LM, Mehra P, Franco P. Use of conservative condylectomy for treatment of osteochondroma of the mandibular condyle. J Oral Maxillofac Surg. 2002;60:262.
Mehra P, Arya V, Henry CH. Temporomandibular joint condylar osteochondroma: complete condylectomy and joint replacement versus low condylectomy and joint preservation. J Oral Maxillofac Surg. 2016;74:911.
Hirahara N. Characteristic MR findings of rheumatic arthritis in the temporomandibular joints. J Oral Maxillofac Surg. 2014;72:e219.
Susarla H, Kim S, Kaban L. Temporomandibular joint involvement in children with systemic arthritis - preliminary report. J Oral Maxillofac Surg. 2011;69:e48.
Henry CH, Hughes CV, Gérard HC, Hudson AP, Wolford LM. Reactive arthritis: preliminary microbiological analysis of the human temporomandibular joint. J Oral Maxillofac Surg. 2000;58:1137.
MacIntosh B, Shivapuja PK, Naqvi R. Scleroderma and the temporomandibular joint: reconstruction in 2 variants. J Oral Maxillofac Surg. 2014;73:1199.
Scolozzi P, Bosson G, Jacques B. Severe isolated temporomandibular joint involvement in juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2005;63:1368.
Müller L, Kellenberger CJ, Cannizzaro E, et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology. 2009;48:680.
Ascani G, Pieramici T, Filosa A, et al. Pseudogout of the temporomandibular joint. J Oral Maxillofac Surg. 2008;66:386.
Suba Z, Takacs D. Gyulai-Gaal, et al.: Tophaceous gout of the temporomandibular joint: a report of 2 cases. J Oral Maxillofac Surg. 2009;67:1526.
Abramowicz S, Cheon JE, Kim S, et al. Magnetic resonance imaging of temporomandibular joints in children with arthritis. J Oral Maxillofac Surg. 2011;69:2321.
Bessa-Nogueira R, Vasconcelos BCE, Duarte A, et al. Targeted assessment of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg. 2008;66:1804.
Abramowicz S, Susarla HK, Kim S, et al. Physical findings associated with active temporomandibular joint inflammation children with juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2013;71:1683.
Mehra P, Henry CH, Giglou KR. Temporomandibular joint reconstruction in patients with autoimmune/connective tissue disease. J Oral Maxillofac Surg. 2018;76:1660.
Stringer DE, Gilbert DH, Herford AS, et al. A method of treating the patient with postpubescent juvenile rheumatoid arthritis. J Oral Maxillofac Surg. 2007;65:1998.
MacIntosh RB, Henny FA. A spectrum of application of autogenous costochondral grafts. J Maxillofac Surg. 1977;5:257.
Padwa BL, Mulliken JB, Maghen A, et al. Midfacial growth after costochondral graft construction of the mandibular ramus in hemifacial microsomia. J Oral Maxillofac Surg. 1998;56:122.
Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994;52:2.
Mercuri LG, Wolford LM, Sanders B, et al. Long-term follow-up of the CAD/CAM patient fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2002;60:1440.
Dingman RO, Grabb WG. Reconstruction of both mandibular condyles with metatarsal bone grafts. J Maxillofac Surg. 1964;34:441.
Macintosh RB, Renny FA. A spectrum of application of autogenous costochondral grafts. J Maxillfac Surg. 1977;5:257.
Matukas VJ, Szymela VF, Schmidt JF. Surgical treatment of bony ankylosis in a child using a composite cartilage-bone iliac crest graft. J Oral Surg. 1980;38:903.
Synder CG, Benson AK, Slater PV. Construction of the temporomandibular joint by transplanting the autogenous sternoclavicular joint. South Med J. 1971;64:807.
Wolford LM, Cottrell DA, Henry CH. Sternoclavicular grafts for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1994;52:119.
Guyuron B, Lasa CI. Unpredictable growth pattern of costochondral graft. Plast Reconstr Surg. 1992;90:880.
Link JO, Hoffman DC, Laskin DM. Hyperplasia of a costochondral graft. J Oral Maxillofac Surg. 1993;51:1392.
Samman, N., Cheung, L.K., Tideman, H. Overgrowth of a costochondral graft in an adult male. Int J Oral Maxillofac Surg. 1995;24:333.
Wolford LM, Mehra P. Simultaneous temporomandibular joint and mandibular reconstruction in an immunocompromised patient with rheumatoid arthritis: a case report with 7 year follow-up. J Oral Maxillofac Surg. 2001;59:345.
Cassano DS. Postsurgical outcomes using total joint prostheses for single-stage reconstruction of the rheumatoid arthritis patient. J Oral Maxillofac Surg. 2008;66:Supplement 63.
Mehra P, Wolford LM, Barau S, et al. Single-stage comprehensive surgical treatment of the rheumatoid arthritis temporomandibular joint patient. J Oral Maxillofac Surg. 2009;67:1859.
Movahed R, Teschke M, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral Maxillofac Surg. 2013;71:2123.
Dela Coleta KE, Wolford LM, Goncalves JR, et al. Maxillo-mandibular counterclockwise rotation and mandibular advancement with TMJ concepts total joint prosthesis. Part 1 - skeletal and dental stability. Int J Oral Maxillofac Surg. 2009;38:126.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mehra, P., Henry, C. (2022). Concomitant Orthognathic and Temporomandibular Joint Surgery. In: Miloro, M., Ghali, G.E., Larsen, P.E., Waite, P. (eds) Peterson’s Principles of Oral and Maxillofacial Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-91920-7_65
Download citation
DOI: https://doi.org/10.1007/978-3-030-91920-7_65
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91919-1
Online ISBN: 978-3-030-91920-7
eBook Packages: MedicineMedicine (R0)