Abstract
The reported incidence and prevalence of primary Sjögen’s Syndrome in the literature vary greatly depending on the applied classification criteria. Furthermore, factors such as age, gender, geographic, and ethnicity-specific differences greatly impact the reported incidence and prevalence including the clinical presentation and mortality.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Sjogren’s syndrome
- Primary
- Secondary
- Incidence
- Prevalence
- Geo-location
- Ethnic
- Age
- Gender
- Pediatric
- Mortality
- Malignancy
- Genetics
Introduction
Sjogren’s syndrome (SS) is an autoimmune connective tissue disease, characterized by lymphocytic infiltration and chronic inflammation of exocrine glands, especially salivary and lacrimal glands. In addition to extra-glandular symptoms such as arthritis, arthralgia, and fatigue, the typical sicca symptoms include a dry mouth and dry eyes, but may extend to other mucous membranes. A limited few patients presents with severe systemic involvement affecting the pulmonary, neurological, dermatological, renal, and hematological systems. SS can occur in the absence of other systemic diseases, that is, primary SS (pSS), or in context of underlying connective tissue disease, secondary SS (sSS).
The diagnosis of SS is based on a constellation of subjective symptoms such as dry mouth, dry eyes, and objective measures including a demonstration of decreased function of exocrine glands, serologic evidence of specific autoantibodies, and histological proof of lymphocytic infiltration on labial salivary glands biopsy. The heterogeneity of signs and symptoms in patients with SS has led to the development of several classification criteria for pSS. The first to be presented in 1986 was the Copenhagen criteria [1]. Since then, several classification criteria for pSS have been proposed over the years among which are the European Community classification criteria for pSS in 1993 [2] and the American–European Consensus Group Criteria (AECG) in 2002 [3]. In contrast to previous suggested criteria, the AECG criteria focused on a more objective disease diagnosis including exclusion criteria. The AECG criteria were revised in 2016 [4]. The purpose of developing classification criteria is to ensure comparability between different cohorts of patients.
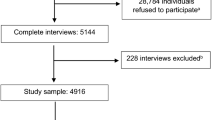
Prevalence and Incidence
Incidence and prevalence are two important indicators in the epidemiology of a disease. Incidence of pSS represents the proportion of newly diagnosed cases in a well-defined population over a given period of time, while prevalence is the proportion of a population found to have pSS. Knowledge on the incidence and prevalence of pSS may facilitate a better understanding of the etiology – especially in relation to gender, age, and possible ethnic differences but it may also play a role in the process of diagnosing patients. However, due to the many proposed and applied classification criteria, and due to the lack of one universally accepted set of classification criteria for pSS, the reported estimated incidence and prevalence of pSS differ greatly between studies. The estimate of pSS prevalence have been reported to vary between 0.1% and 4% in studies selecting patients from different populations and age groups [5,6,7,8]. Furthermore, pooled prevalence rates in studies that used the 1993 European Classification Criteria was reported to be 12-fold higher than pooled prevalence rates in studies that used the 2002 AECG criteria [9]. Similar differences have been reported for population-based epidemiological studies, where the pooled prevalence rates were slightly lower than prevalence rates calculated in the total population [10]. The variations may be related to differences in the applied epidemiological methods including selection bias and bias related to low response rates in population surveys.
A potential way to overcome the differences is to use Big Data. The Big Data Sjögren Project Consortium is an international, multicenter registry created in 2014 and included 11,421 pSS patients from 24 countries by January 2019 [11]. The project used a data-sharing approach to standardize, harmonize, and share data from several different centers conducting clinical research in pSS. However, the data might still be skewed as data from studies based on hospital registers include patients with higher disease burden and are missing subclinical and underdiagnosed cases especially from the primary care.
Unfortunately, there are no Big Data available on incidence and prevalence for pSS so another way to eliminate some of the reported differences is to perform a meta-analysis of published literature in the field. A recent meta-analysis-study estimated the prevalence of pSS in the total population to be 60.82 (95%CI, 43.69–77.94) cases per 100,000 individuals and the pooled incidence ratio for pSS is estimated to be 6.92 (95% CI, 4.98–8.86) per 100, 000 persons a year [9]. All these data may provide some insight in the incidence and prevalence rates, yet the “true” prevalence and incidence of pSS are difficult to estimate.
Relation to Gender
All studies of incidence and prevalence of pSS have shown a most unbalanced gender ratio with females having a predisposition to pSS as they do to autoimmune disease in general. Some studies suggest that the disease is related to estrogen deficiency as seen in menopause or induced by ovariectomy [12, 13], the cause of the gender difference is still unclear.
The female-to-male prevalence ratio was recently estimated in Big Data studies across different countries and populations, and was even found to vary from country to country and even in different areas of the same country. The Big Data Google-driven study found the female–male ratio prevalence to be 10:1 [14], whereas the study from The Big Data Sjögren Project Consortium found the female-to-male ratio prevalence somewhat higher – 14:1 [11]. However, the female–male imbalance has huge geographical differences with the highest female-to-male ratio (27:1) in China [15] – see Table 2.1.
Relation to Age
In the two Big Data studies, the overall mean age at diagnosis have been reported to be 53 years of age [11, 14]. However, as to the mean age at disease onset, geographical and gender differences exists [11, 14].
The mean age in European cohorts of pSS patients are significantly higher than in non-European patients, and the age of disease onset has further been reported to be younger among Asians than in Western populations [15, 18, 19, 23, 26]. For instance, the mean age was 44.5 and 43.7 years in India [18] and Turkey [19], but 57, 55, and 52 years in South Australia [20], Greece [27], and Slovenia, respectively [28].
Though the prevalence is lower in the male population, they are also reported to be older at the time of diagnosis with an average of 58 years as compared to 53 years among women [22]. No significant difference in age-adjusted incidence by race/ethnicity has been reported for men [22].
Finally, the prevalence of pSS increases with age and has been reported to be 6% in adults over 65 years, increasing to 14% in persons older than 70 years [7, 9, 29, 30].
Geographical and Ethnic Differences
The incidence and prevalence are reported to have geographical and ethnic differences – see Table 2.2. Comparing global data, Asian populations seem to have an overall a higher incidence and prevalence of pSS as compared to Caucasians. For example, the incidence rates of pSS in Western populations have been reported to vary from 2.1 in the USA [22], 3.9 in Slovenia [28], and 5.3 in Greece [27] per 100,000 persons, the pooled incidence rate in Asian countries is reported to be 6.6/100,000 persons [35, 38, 39].
Furthermore, variations between ethnic groups are seen despite having the same geolocation as reported in studies from multiethnic populations in Paris, France, and New York, USA. The French study found a twofold higher prevalence of pSS in patients with non-European backgrounds (from northern Africa, sub-Saharan Africa, Caribbean, and Oceania) as compared to those with a European background [23], whereas the American study found a higher incidence rate of pSS among Asian women and white women compared with Hispanic and black women [22].
In relation to symptom presentation, geographic/ethnic differences are also reported. From the Big Data consortium study, sicca symptoms had the lowest frequency in Asian populations who instead had a higher frequency of antibody positivity and certain extra-glandular manifestations such as lung and renal involvement as compared to whites, blacks, and Hispanics [11].
Even a potential north–south autoimmune gradient has been suggested, with symptom rates increasing according to distance from the Equator, regarding the prevalence and incidence of several autoimmune diseases [10]. A recent study investigated potential differences between the northern and southern countries in three continents (Europe, America, and Asia) [11]. A north–south gradient was seen with respect to a lower frequency of ocular involvement and a higher frequency of cryoglobulinemic-related tests in northern compared with southern countries within the same continent, however not identical across the three continents. In Europe, salivary gland involvement had the highest rates of abnormal results in patients from northern countries, while in America and Asia the highest rates were reported in patients from southern countries. Similarly, having autoantibodies was found most frequently in the northern countries in America and Asia but in the southern countries in Europe.
The clinical relevance of the north–south gradient hypothesis is not clear.
Primary Sjogren’s Syndrome in Children
In contrast to adulthood, pSS is a very rare disease in children and the number of studies and published case reports are very limited. The Big Data Sjögren Project Consortium study reported a childhood-onset disease in about 1% of patients with pSS. The age at diagnosis have been reported to range from 5 to 16 years, with a mean age at time of diagnosis of 14.2 years and a female-to-male ratio of 5–7:1 [16, 17].
The clinical phenotype in childhood-onset pSS is dominated by systemic disease and infrequent involving of articular, pulmonary, peripheral nerve, and central nervous system [16]. Salivary gland enlargement affects one out of two children with pSS [40].
Secondary SS
Secondary SS (sSS) is associated with other connective tissue diseases, such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), systemic sclerosis (SSc), or dermatomyositis.
The difference in the prevalence of sSS in patients with other connective tissue diseases can be explained by different definition of SS diagnosis, different applied classification criteria, and geographical differences Sjogren’s syndrome (SS) epidemiology. Hence, the prevalence of secondary SS in patients with SLE has been reported to range 5–22%, in RA 3.6–55%, in SSc 10–23%, and in dermatomyositis 10–23% [41].
The incidence rate of sSS is as pSS higher in women than in men, regardless of the underlying autoimmune disease [40].
There are no data regarding the relationship between the duration of the underlying autoimmune disease and the development of sSS [41] but sSS phenotype is related to the underlying autoimmune disease. For instance, Raynaud’s phenomenon, autoimmune thyroiditis, and anti-SSA/SSB positivity occur more frequently in patients with sSS in SLE than in patients with SLE alone [42]. Patients with sSS in RA have more limitations in daily activities and more fatigue than patients with RA alone [41] and patients with sSS in combination with either SLE or SSc have the highest risk of lymphoma [43, 44].
Malignancy Risk and Mortality
Patients with pSS have an increased risk of cancer compared to the general population with a higher risk for malignancy in hospital-based studies than in population-based studies.
A meta-analysis of studies from Asia, USA, and Europe reported the overall cancer risk ratio (RR) to be 1.53 (95% CI, 1.17–1.88), for non-Hodgkin lymphoma (NHL) 13.76 (95% CI, 8.53–18.99), and 2.58 (95% CI, 1.14–4.03) for thyroid cancer, but was not reported higher for other solid tumors. The high risk for NHL was independent of geolocation, the applied diagnostic criteria, study design, mean age in the studied cohorts, and follow-up time [45].
Some studies have reported that the risk of lymphoma may be related to age at disease onset, with a higher incidence in pSS patients with disease onset at <35 years and severe systemic disease activity [46].
Patients with pSS are reported to have a slightly higher mortality rate as compared with the general population. The increased mortality is especially associated with the development of lymphoproliferative disease such as B-cell lymphoma [36, 46, 47]. In a meta-analysis, the pooled standardized mortality ratio in patients with pSS was estimated to be to 1.38 (95% CI, 0.94–2.01) with lymphoid and solid-organ malignancies, cardiovascular diseases, and infections as the major causes [33]. In the meta-analysis, different risk factors were identified to be related to increased mortality. These were advanced age at diagnosis [RR 1.09 (95% CI, 1.07, 1.12)], male gender [RR 2.18 (95% CI, 1.45–3.27)], parotid enlargement [RR 1.81 (95% CI, 1.02–3.21)], abnormal parotid scintigraphy [RR 2.96 (95% CI, 1.36–6.45)], extra-glandular involvement [RR 1.77 (95% CI, 1.06–2.95)], vasculitis [RR 7.27 (95% CI, 2.70–19.57)], autoantibodies (anti-SSB/La positivity [RR 1.45 (95% CI, 1.03–2.04)]), low C3 [RR 2.14 (95% CI, 1.38–3.32)] and C4 [RR 3.08 (95% CI, 2.14–4.42)], and cryoglobulinemia [RR 2.62 (95% CI, 1.77–3.90)] [33].
Genetics
Since 35% of patients with pSS have relatives with pSS or related autoimmune disease [48], a hereditary link has been suggested in pSS. A possible hereditary link is further supported by data from twins showing that if one twin sibling has pSS, the other twin has a 662-fold higher risk of developing pSS than in twins without an affected sibling [49]. However, the genetic basis of pSS is complex and relatively unexplored.
Primary SS has been demonstrated to have a solid genetic association within MHC genes, including those in the human leukocyte antigen (HLA) region. The HLA region contains hundreds of genes that are responsible for antigen presentations and other functions in immune cells. In genome-wide studies, strong associations have between demonstrated for pSS and the HLA class I, class II, and class III regions, with multiple associations observed for HLA class II molecules, HLA-antigen D related (HLADR), and HLADQ loci [50,51,52]. HLA class II proteins carry the largest genetic predisposition for autoimmune disease, including pSS, and some HLA class II alleles are associated with the production of autoantibodies in pSS [52]. A meta-analysis identified the DRB1*0301, DQA1*0501, DQB1*0201, and DRB1*03 alleles as risk factors for pSS, while the DQA1*0201, DQA1*0301 and DQB1*0501 alleles were protective [53].
There are, however, different gene expressions across ethnic groups. For instance, there is a markedly increased frequency of HLA-DQB1*0201 and HLA-DQA1*0501 in Caucasian patients with primary SS [54] while in Han Chinese patients multiple associations exist with DRB1*0803-DQA1*0103-DQB1*0601 [55] and DRB1*0405-DRB4*0101-DQA1*0301-DQB1*0401 in Japanese patients [54].
The most significant genetic association to pSS outside the HLA region is in the interferon-regulatory factor (IRF)-5 locus [50]. Expression of IRF-5 activates transcription of proinflammatory cytokines such as type 1 IFN, interleukins (IL) IL-6, IL-12-p40, and tumor necrosis factor alpha.
Furthermore, there is a strong evidence of B- and T-cell abnormalities in pSS and includes elevated gamma globulins, lymphocyte retention in glands as well as a low peripheral lymphocyte count [56]. An imbalance between Th1 and Th2 cell activity has further been demonstrated, and T follicular helper cells which is crucial for B-cell activation and differentiation in lymphoid structures have been found to correlate with disease activity [57, 58]. The B lymphocyte tyrosine kinase (BLK) is involved in the development and activation of T and B cells, and the nuclear factor kappa-B (NF-κB) plays a role in downregulation of BLK. Gene studies in SS patient have reported associations in several genes in the NF-κB pathway, including the IL-1 receptor-associated kinase 1-binding protein 1 (IRAK1BP), which activates the NF-κB [59].
Further understanding of the genetics in pSS may facilitate future treatment options.
References
Manthorpe R, Oxholm P, Prause JU, Schiødt M. The Copenhagen criteria for Sjögren’s syndrome. Scand J Rheumatol Suppl. 1986;61:19–21.
Vitali C, Bombardieri S, Moutsopoulos HM, Balestrieri G, Bencivelli W, Bernstein RM, et al. Preliminary classification criteria for Sjögren’s syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheum. 1993;36:340–7.
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH, European Study Group on Classification Criteria for Sjögren’s syndrome. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002;61(6):554–8.
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, Rasmussen A, Scofield H, Vitali C, Bowman SJ, Mariette X, International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European league against rheumatism classification criteria for primary Sjogren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017;69(1):35–45.
Binard A, Devauchelle-Pensec V, Fautrel B, Jousse S, Youinou P, Saraux A. Epidemiology of Sjögren’s syndrome: where are we now? Clin Exp Rheumatol. 2007;25:1–4. 5.
Thomas E, Hay EM, Hajeer A, Silman J. Sjögren’s syndrome: a community-based study of prevalence and impact. Br J Rheumatol. 1998;37:1069–76. 6.
Bowman SJ, Ibrahim GH, Holmes G, Hamburger J, Ainsworth JR. Estimating the prevalence among Caucasian women of primary Sjogren’s syndrome in two general practices in Birmingham, UK. Scand J Rheumatol. 2004;33:39–43. 8.
Haugen AJ, Peen E, Hultén B, Johannessen AC, Brun JG, Halse AK, et al. Estimation of the prevalence of primary Sjögren’s syndrome in two age-different community-based populations using two sets of classification criteria: the Hordaland health study. Scand J Rheumatol. 2008;37:30–4.
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang F, Zhong R. Epidemiology of primary Sjögren’s syndrome: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(11):1983–9.
Brito-Zerón P, Acar-Denizli N, Zeher M, Rasmussen A, Seror R, Theander E, Li X, Baldini C, Gottenberg JE, Danda D, Quartuccio L, Priori R, Hernandez-Molina G, Kruize AA, Valim V, Kvarnstrom M, Sene D, Gerli R, Praprotnik S, Isenberg D, Solans R, Rischmueller M, Kwok SK, Nordmark G, Suzuki Y, Giacomelli R, Devauchelle-Pensec V, Bombardieri M, Hofauer B, Bootsma H, Brun JG, Fraile G, Carsons SE, Gheita TA, Morel J, Vollenveider C, Atzeni F, Retamozo S, Horvath IF, Sivils K, Mandl T, Sandhya P, De Vita S, Sanchez-Guerrero J, van der Heijden E, Trevisani VFM, Wahren-Herlenius M, Mariette X, Ramos-Casals M, EULAR-SS Task Force Big Data Consortium. Influence of geolocation and ethnicity on the phenotypic expression of primary Sjogren’s syndrome at diagnosis in 8310 patients: a cross-sectional study from the Big Data Sjogren Project Consortium. Ann Rheum Dis. 2017;76(6):1042–50.
Acar-Denizli N, Kostov B, Ramos-Casals M, Sjögren Big Data Consortium. The big data Sjögren Consortium: a project for a new data science era. Clin Exp Rheumatol. 2019;37 Suppl 118(3):19–23.
Suri V, Suri V. Menopause and oral health. J Life Health. 2014;5(3):115–20.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136(2):318–26.
Ramos-Casals M, Brito-Zerón P, Kostov B, Sisó-Almirall A, Bosch X, Buss D, Trilla A, Stone JH, Khamashta MA, Shoenfeld Y. Google-driven search for big data in autoimmune geoepidemiology: analysis of 394,827 patients with systemic autoimmune diseases. Autoimmun Rev. 2015;14(8):670–9.
Li X, Xu B, Ma Y, Li X, Cheng Q, Wang X, Wang G, Qian L, Wei L. Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: a retrospective analysis of 315 patients. Int J Rheum Dis. 2015;18(4):439–46.
Ramos-Casals M, Acar-Denizli N, Vissink A, Brito-Zerón P, Li X, Carubbi F, Priori R, Toplak N, Baldini C, Faugier-Fuentes E, Kruize AA, Mandl T, Tomiita M, Gandolfo S, Hashimoto K, Hernandez-Molina G, Hofauer B, Mendieta-Zerón S, Rasmussen A, Sandhya P, Sene D, Trevisani VFM, Isenberg D, Sundberg E, Pasoto SG, Sebastian A, Suzuki Y, Retamozo S, Xu B, Giacomelli R, Gattamelata A, Bizjak M, Bombardieri S, Loor-Chavez RE, Hinrichs A, Olsson P, Bootsma H, Lieberman SM, Sjogren Big Data Consortium. Childhood-onset of primary Sjogren’s syndrome: phenotypic characterization at diagnosis of 158 children. Rheumatology (Oxford). 2021:keab032.
Virdee S, Greenan-Barrett J, Ciurtin C. A systematic review of primary Sjögren’s syndrome in male and paediatric populations. Clin Rheumatol. 2017;36(10):2225–36.
Sandhya P, Jeyaseelan L, Scofield RH, Danda D. Clinical characteristics and outcome of primary Sjogren’s syndrome: a large Asian Indian cohort. Open Rheumatol J. 2015;9:36–45.
Birlik M, Akar S, Gurler O, Sari I, Birlik B, Sarioglu S, Oktem MA, Saglam F, Can G, Kayahan H, Akkoc N, Onen F. Prevalence of primary Sjogren’s syndrome in Turkey: a population-based epidemiological study. Int J Clin Pract. 2009;63(6):954–61.
Lyne SA, Downie-Doyle S, Lester SE, Quinlivan A, Toby Coates P, Gordon TP, Rischmueller M. Primary Sjögren’s syndrome in South Australia. Clin Exp Rheumatol. 2020;38 Suppl 126(4):57–63.
Maciel G, Crowson CS, Matteson EL, Cornec D. Prevalence of primary Sjogren’s syndrome in a US population-based cohort. Arthritis Care Res (Hoboken). 2017;69(10):1612–6.
Izmirly PM, Buyon JP, Wan I, Belmont HM, Sahl S, Salmon JE, Askanase A, Bathon JM, Geraldino-Pardilla L, Ali Y, Ginzler EM, Putterman C, Gordon C, Helmick CG, Parton H. The incidence and prevalence of adult primary Sjögren’s syndrome in New York County. Arthritis Care Res (Hoboken). 2019;71(7):949–60.
Maldini C, Seror R, Fain O, Dhote R, Amoura Z, De Bandt M, Delassus JL, Falgarone G, Guillevin L, Le Guern V, Lhote F, Meyer O, Ramanoelina J, Sacré K, Uzunhan Y, Leroux JL, Mariette X, Mahr A. Epidemiology of primary Sjögren’s syndrome in a French multiracial/multiethnic area. Arthritis Care Res (Hoboken). 2014;66(3):454–63.
Narváez J, Sánchez-Fernández SÁ, Seoane-Mato D, Díaz-González F, Bustabad S. Prevalence of Sjögren’s syndrome in the general adult population in Spain: estimating the proportion of undiagnosed cases. Sci Rep. 2020;10(1):10627.
Gøransson LG, Haldorsen K, Brun JG, Harboe E, Jonsson MV, Skarstein K, Time K, Omdal R. The point prevalence of clinically relevant primary Sjogren’s syndrome in two Norwegian counties. Scand J Rheumatol. 2011;40(3):221–4.
Lin D-F, Yan S-M, Zhao Y, et al. Clinical and prognostic characteristics of 573 cases of primary Sjogren’s syndrome. Chin Med J. 2010;123:3252–7.
Alamanos Y, Tsifetaki N, Voulgari PV, Venetsanopoulou AI, Siozos C, Drosos AA. Epidemiology of primary Sjögren’s syndrome in north-West Greece, 1982-2003. Rheumatology (Oxford). 2006;45(2):187–91.
Plesivcnik Novljan M, Rozman B, Hocevar A, Grmek M, Kveder T, Tomsic M. Incidence of primary Sjogren’s syndrome in Slovenia. Ann Rheum Dis. 2004;63(7):874–6.
Botsios C, Furlan A, Ostuni P, Sfriso P, Andretta M, Ometto F, Raffeiner B, Todesco S, Punzi L. Elderly onset of primary Sjögren’s syndrome: clinical manifestations, serological features and oral/ocular diagnostic tests. Comparison with adult and young onset of the disease in a cohort of 336 Italian patients. Joint Bone Spine. 2011;78(2):171–4.
García-Carrasco M, Cervera R, Rosas J, Ramos-Casals M, Morlà RM, Sisó A, Jiménez S, Pallarés L, Font J, Ingelmo M. Primary Sjögren’s syndrome in the elderly: clinical and immunological characteristics. Lupus. 1999;8(1):20–3.
Zhang NZ, Shi CS, Yao QP, Pan GX, Wang LL, Wen ZX, Li XC, Dong Y. Prevalence of primary Sjogren’s syndrome in China. J Rheumatol. 1995;22(4):659–61.
Eaton WW, Rose NR, Kalaydjian A, Pedersen MG, Mortensen PB. Epidemiology of autoimmune diseases in Denmark. J Autoimmun. 2007;29(1):1–9.
Singh AG, Singh S, Matteson EL. Rate, risk factors and causes of mortality in patients with Sjögren’s syndrome: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford). 2016;55(3):450–60.
Sardu C, Cocco E, Mereu A, Massa R, Cuccu A, Marrosu MG, Contu P. Population based study of 12 autoimmune diseases in Sardinia, Italy: prevalence and comorbidity. PLoS One. 2012;7(3):e32487.
See L-C, Kuo C-F, Chou I-J, Chiou M-J, Yu K-H. Sex- and age-specific incidence of autoimmune rheumatic diseases in the Chinese population: a Taiwan population-based study. Semin Arthritis Rheum. 2013;43:381–6.
Pertovaara M, Pukkala E, Laippala P, Miettinen A, Pasternack A. A longitudinal cohort study of Finnish patients with primary Sjögren’s syndrome: clinical, immunological, and epidemiological aspects. Ann Rheum Dis. 2001;60(5):467–72.
Tolentino Júnior DS, de Oliveira CM, de Assis EM. Population-based study of 24 autoimmune diseases carried out in a Brazilian microregion. J Epidemiol Glob Health. 2019;9(4):243–51.
Weng M-Y, Huang Y-T, Liu M-F, Lu T-H. Incidence and mortality of treated primary Sjogren’s syndrome in Taiwan: a population-based study. J Rheumatol. 2011;38:706–8.
Yu K-H, See L-C, Kuo C-F, Chou I-J, Chou M-J. Prevalence and incidence in patients with autoimmune rheumatic diseases: a nationwide population-based study in Taiwan. Arthritis Care Res. 2013;65:244–50.
Alani H, Henty JR, Thompson NL, Jury E, Ciurtin C. Systematic review and meta-analysis of the epidemiology of polyautoimmunity in Sjögren’s syndrome (secondary Sjögren’s syndrome) focusing on autoimmune rheumatic diseases. Scand J Rheumatol. 2018;47(2):141–54.
Moerman RV, Arends S, Mossel E, Kroese FGM, Vissink A, Bootsma H. 10-year follow-up of patients with rheumatoid arthritis and secondary Sjögren’s syndrome or sicca symptoms in daily clinical practice. Clin Exp Rheumatol. 2020;38 Suppl 126(4):64–72.
Baer AN, Maynard JW, Shaikh F, Magder LS, Petri M. Secondary Sjogren’s syndrome in systemic lupus erythematosus defines a distinct disease subset. J Rheumatol. 2010;37(6):1143–9.
Baldini C, Mosca M, Della Rossa A, Pepe P, Notarstefano C, Ferro F, et al. Overlap of ACA-positive systemic sclerosis and Sjogren’s syndrome: a distinct clinical entity with mild organ involvement but at high risk of lymphoma. Clin Exp Rheumatol. 2013;31:272–80.
Martens PB, Pillemer SR, Jacobsson LT, O’Fallon WM, Matteson EL. Survivorship in a population based cohort of patients with Sjögren’s syndrome, 1976-1992. J Rheumatol. 1999;26(6):1296–300.
Liang Y, Yang Z, Qin B, Zhong R. Primary Sjogren’s syndrome and malignancy risk: a systematic review and meta-analysis. Ann Rheum Dis. 2014;73(6):1151–6. https://doi.org/10.1136/annrheumdis-2013-203305.
Goules AV, Argyropoulou OD, Pezoulas VC, Chatzis L, Critselis E, Gandolfo S, Ferro F, Binutti M, Donati V, Zandonella Callegher S, Venetsanopoulou A, Zampeli E, Mavrommati M, Voulgari PV, Exarchos T, Mavragani CP, Baldini C, Skopouli FN, Fotiadis DI, De Vita S, Moutsopoulos HM, Tzioufas AG. Primary Sjögren’s syndrome of early and late onset: distinct clinical phenotypes and lymphoma development. Front Immunol. 2020;11:594096.
Ioannidis JP, Vassiliou VA, Moutsopoulos HM. Long-term risk of mortality and lymphoproliferative disease and predictive classification of primary Sjögren’s syndrome. Arthritis Rheum. 2002;46(3):741–7.
Reveille JD, Wilson RW, Provost TT, Bias WB, Arnett FC. Primary Sjögren’s syndrome and other autoimmune diseases in families. Prevalence and immunogenetic studies in six kindreds. Ann Intern Med. 1984;101(6):748–56.
Kuo CF, Grainge MJ, Valdes AM, See LC, Luo SF, Yu KH, Zhang W, Doherty M. Familial risk of Sjogren’s syndrome and co-aggregation of autoimmune diseases in affected families: a nationwide population study. Arthritis Rheumatol. 2015;67(7):1904–12.
Lessard CJ, et al. Variants at multiple loci implicated in both innate and adaptive immune responses are associated with Sjögren’s syndrome. Nat Genet. 2013;45:1284–92.
Li Y, et al. A genome-wide association study in Han Chinese identifies a susceptibility locus for primary Sjögren’s syndrome at 7q11.23. Nat Genet. 2013;45:1361–5.
Gottenberg J-E, et al. In primary Sjögren’s syndrome, HLA class II is associated exclusively with autoantibody production and spreading of the autoimmune response. Arthritis Rheumatol. 2003;48:2240–5.
Cruz-Tapias P, Rojas-Villarraga A, Maier-Moore S, Anaya JM. HLA and Sjögren’s syndrome susceptibility. A meta-analysis of worldwide studies. Autoimmun Rev. 2012;11(4):281–7.
Kang HI, Fei HM, Saito I, Sawada S, Chen SL, Yi D, Chan E, Peebles C, Bugawan TL, Erlich HA, et al. Comparison of HLA class II genes in Caucasoid, Chinese, and Japanese patients with primary Sjögren’s syndrome. J Immunol. 1993;150(8 Pt 1):3615–23.
Li Y, Zhang K, Chen H, Sun F, Xu J, Wu Z, Li P, Zhang L, Du Y, Luan H, Li X, Wu L, Li H, Wu H, Li X, Li X, Zhang X, Gong L, Dai L, Sun L, Zuo X, Xu J, Gong H, Li Z, Tong S, Wu M, Li X, Xiao W, Wang G, Zhu P, Shen M, Liu S, Zhao D, Liu W, Wang Y, Huang C, Jiang Q, Liu G, Liu B, Hu S, Zhang W, Zhang Z, You X, Li M, Hao W, Zhao C, Leng X, Bi L, Wang Y, Zhang F, Shi Q, Qi W, Zhang X, Jia Y, Su J, Li Q, Hou Y, Wu Q, Xu D, Zheng W, Zhang M, Wang Q, Fei Y, Zhang X, Li J, Jiang Y, Tian X, Zhao L, Wang L, Zhou B, Li Y, Zhao Y, Zeng X, Ott J, Wang J, Zhang F. A genome-wide association study in Han Chinese identifies a susceptibility locus for primary Sjögren’s syndrome at 7q11.23. Nat Genet. 2013;45(11):1361–5. https://doi.org/10.1038/ng.2779. Epub 2013 Oct 6.
Fox RI, et al. Primary Sjögren syndrome: clinical and immunological features. Semin Arthritis Rheum. 1984;14(2):77–105.
van Woerkom JM, Kruize AA, Wenting-van Wijk MJ, Knol E, Bihari IC, Jacobs JW, Bijlsma JW, Lafeber FP, van Roon JA. Salivary gland and peripheral blood T helper 1 and 2 cell activity in Sjögren’s syndrome compared with non-Sjögren’s sicca syndrome. Ann Rheum Dis. 2005;64(10):1474–9.
Szabo K, Papp G, Barath S, Gyimesi E, Szanto A, Zeher M. Follicular helper T cells may play an important role in the severity of primary Sjögren’s syndrome. Clin Immunol. 2013;147(2):95–104.
Lessard CJ, Li H, Adrianto I, Ice JA, Rasmussen A, Grundahl KM, Kelly JA, Dozmorov MG, Miceli-Richard C, Bowman S, Lester S, Eriksson P, Eloranta ML, Brun JG, Gøransson LG, Harboe E, Guthridge JM, Kaufman KM, Kvarnström M, Jazebi H, Cunninghame Graham DS, Grandits ME, Nazmul-Hossain AN, Patel K, Adler AJ, Maier-Moore JS, Farris AD, Brennan MT, Lessard JA, Chodosh J, Gopalakrishnan R, Hefner KS, Houston GD, Huang AJ, Hughes PJ, Lewis DM, Radfar L, Rohrer MD, Stone DU, Wren JD, Vyse TJ, Gaffney PM, James JA, Omdal R, Wahren-Herlenius M, Illei GG, Witte T, Jonsson R, Rischmueller M, Rönnblom L, Nordmark G, Ng WF, UK Primary Sjögren’s Syndrome Registry, Mariette X, Anaya JM, Rhodus NL, Segal BM, Scofield RH, Montgomery CG, Harley JB, Sivils KL. Variants at multiple loci implicated in both innate and adaptive immune responses are associated with Sjogren’s syndrome. Nat Genet. 2013;45(11):1284–92.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fana, V., Terslev, L. (2022). Epidemiology. In: Bruyn, G.A.W. (eds) Sjögren’s Syndrome and the Salivary Glands. Contemporary Rheumatology. Springer, Cham. https://doi.org/10.1007/978-3-030-90977-2_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-90977-2_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-90976-5
Online ISBN: 978-3-030-90977-2
eBook Packages: MedicineMedicine (R0)