Abstract
The “envelope of discrepancy” to define the limitation of tooth movement is well accepted in orthodontics. However, it has been more for illustrating possibilities of various tooth movement. The described envelopes were not determined by scientific measurements or specific anatomic boundaries. Currently, CBCT imaging has enhanced our ability to evaluate the morphology of the craniofacial and dentoalveolar gingival complex. It allows the quantitative assessment of the dimensions of alveolar bone which could not be evaluated in two-dimensional images due to the superimposition of anatomical structures. The limits of orthodontic tooth movement which is defined as “orthodontic boundary limits” may need to be established, utilizing 3D imaging technology.
The purposes of this chapter are to: (1) review the dentoalveolar gingival complex,
dentoalveolar bone deficiency, and the dimensional changes of dentoalveolar gingival complex with tooth movement, and (2) challenge to determine the orthodontic boundary limits of mandibular incisors in Skeletal Class II patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Skeletal Class II
- Cone-beam computed tomography
- Orthodontic boundary limits
- Dentoalveolar gingival complex
- Dentoalveolar bone deficiency
Orthodontic Boundary Limits
Proffit and Ackerman [1] in 1982 introduced a diagram of the “envelope of discrepancy” in order to address the challenge of the limitation of tooth movement. They estimated that, with orthodontic tooth movement alone, the limits of extrusion, retraction, intrusion, and protraction of mandibular incisors are 2 mm, 3 mm, 4 mm, and 5 mm, respectively. However, these parameters were more for manifesting the principle of limitation and were not determined by measurements or specific anatomic boundaries. When it was published, three-dimensional diagnosis with a cone-beam computed tomographic (CBCT) was not available.
The limits of orthodontic tooth movement which are determined by anatomic and biologic limits may be considered as “orthodontic boundary limits.” Anatomic limits are defined by the craniofacial, skeletal, dentoalveolar, and dentogingival complex. These limits should be evaluated prior to any treatment three dimensionally. Biologic limits are explained by the functional and structural response that periodontal tissue can tolerate without compromising during and/or after the tooth movement, which provide long-term stability from periodontal and orthodontic perspectives. The orthodontic boundary limits are not static but dynamic and modifiable in corporate with periodontal surgeries. These limits should be taken into account during the treatment planning and may dictate the amount, types, and goals of tooth movement. When force is applied to teeth by any appliances within the biologically acceptable limits, the gingival and alveolar bone response without changing the attachment level. On the contrary, invading the boundary limits with inadequate treatment planning can create undesired periodontal consequences, resulting in dentoalveolar bone deficiency (dehiscence and fenestrations) and at worst, attachment loss (gingival recessions) (Fig. 1).
(a) Pre-treatment intraoral frontal photograph demonstrating crowding, thick flat biotype, and wide width of keratinized gingiva on mandibular incisors. (b) Expanding mandibular arch with fixed appliances and proclining the incisors resulted in reducing the width of keratinized gingiva, converting to thin scalloped biotype, and creating attachment loss during the orthodontic treatment
The concept of orthodontic boundary limits is not widely recognized, and much research has not been conducted on this fundamental topic. We rarely know what the limits of tooth movement are, how to determine the parameters, and how orthodontic boundary limits are influenced by orthodontic and/or periodontal therapy.
Diagnosis of Craniofacial and Dentoalveolar Complex
Conventional periapical, panoramic, and cephalometric radiography have been used for orthodontic diagnoses and treatment planning [2, 3] despite the fact that they have geometric distortion and anatomical superimposition. Currently, the use of CBCT imaging has made it possible to visualize the related craniofacial and dentoalveolar structures with higher resolution in three dimensions. This has improved the overall diagnostic efficacy and made early diagnosis possible for certain clinical conditions. However, there was controversial opinions of taking CBCT imaging for comprehensive orthodontic assessment [4, 5].
Interestingly, history repeats itself. Larson [4] quoted the Steiner’s article [6] in 1953, he challenged orthodontists with the following words: “The cephalometer is here to stay, and those of you who are not using cephalometrics in your everyday clinical practices must soon bow to its importance, accept the added burden it imposes, and master its mysteries if you are to discharge your full obligation to your patients.” Steiner’s statement could easily be applied to the use of CBCT today. It should be emphasized that CBCT imaging is considered as a supplemental imaging technique only when practitioners expect that the diagnostic yield will benefit patient care, enhance patient safety, or improve clinical outcomes significantly [7]. Additionally, due to the difficulties to acquire the approval of extra radiation exposures from the institutional review board (IRB) academically, it is difficult to initiate and implement higher level, evidence-based studies regarding CBCT imaging such as randomized controlled and prospective studies in orthodontics. We still need much more research to comprehend how to utilize CBCT imaging to maximize the orthodontic outcomes. Therefore, with regard to the appropriateness of taking CBCT images, “Clinicians should use professional judgment in the prescription and performance of CBCT examinations by consulting recommendations from available CBCT guidelines and by considering the specific clinical situation and needs of the individual patient.” [7, 8]
2D vs 3D Imaging
Orthodontic diagnosis, treatment plans, evaluation of growth and development, and assessment of treatment outcomes have traditionally been performed on the basis of clinical examination and records that consist of extraoral and intraoral images, dental casts (or digital models), and analysis of two-dimensional (2D) radiography such as panoramic and lateral cephalometric images. The inherent limitations of 2D radiography for the assessment of craniofacial and dentoalveolar complex in orthodontics have been discussed for many years [9, 10]. They include magnification, distortion, artifacts, superimposition of anatomical details, and discrepancy between cephalometric analyses and clinical findings due to the difficulty of landmark identification. Furthermore, considering the characteristics of lateral cephalograms, there is little information in the transverse dimension.
CBCT imaging has enhanced our ability to evaluate the morphology of the craniofacial and dentoalveolar complex. It allows the quantitative assessment of the transvers and alveolar bone dimensions. As a result of anatomical visibility and volumetric accuracy, the necessity of three-dimensional (3D) imaging is expanding in orthodontic diagnosis.
In order to evaluate differences in the diagnosis and treatment planning of impacted maxillary canines between two imaging modalities, traditional 2D images and 3D volumetric images obtained from a CBCT scan were compared [11]. Twenty-seven percent of the cases that were planned with the 2D radiographs had different treatment plans after viewing the 3D CBCT images. They concluded that 2D and 3D images can produce different diagnoses and treatment plans. The similar result was reported [12].
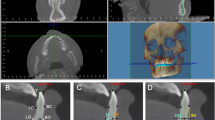
According to Fuhrmann et al. [13], there is a general overestimation of the symphysial labiolingual bone width on the lateral cephalograms when compared with physical measurements of the actual specimens, and over 80% of defects identifiable in 3D images were not readily visible on the lateral cephalograms. Similarly, another research reported that alveolar bone thickness is always overestimated on cephalograms compared with CBCT-based measurements with the range from 0.3 to 1.3 mm [14]. Therefore, the outer lines of the alveolar process that are observed on lateral cephalograms could exhibit the superimposition of other structures. Dehiscences and/or fenestrations on anterior teeth could be possibly masked due to overestimating the thickness of the cortical plates. Two-dimensional radiography does not allow us to evaluate the important sites of the alveolar process properly (Fig. 2).
Comparison of the lateral cephalograms (a and b magnified mandibular anterior region of A) and CBCT imaging (c reconstructed 3D imaging and d a sagittal cross-section of the left mandibular central incisor from CBCT scans). CBCT imaging provides novel information, morphology of the symphysis, and the relationships between the alveolar process and the incisors that are not discernible from 2D radiographs, which may impact treatment planning. The mandibular left central incisor is positioned labially, and the root is out from the alveolar process. There are severe concavities between the roots on the alveolar process
The American Academy of Periodontology published the consensus statement on CBCT [15] and the review [16] focusing on risk assessment of the dentoalveolar bone changes influenced by tooth movement. In the consensus statement, CBCT imaging has demonstrated that changes occur to the buccal plate and general alveolar bone structure following orthodontic tooth movement. They concluded that CBCT imaging is the only radiographic modality with which such changes can be objectively detected and preoperative risk determined. In the review, in order to prevent periodontal complications or assess risks after orthodontic treatment, CBCT imaging can improve the periodontal diagnostic acumen regarding alveolar bone alterations influenced by orthodontic treatment. Furthermore, clinicians are better informed to determine risk assessment and develop preventative or interceptive periodontal augmentation (soft tissue and/or bone augmentation) therapies for patients undergoing orthodontic treatment.
In summary, 3D imaging provides us critical information in order to diagnose accurately, evaluate the anatomical structures that we need to consider prior to treatment planning, and improve the clinical outcomes of orthodontic treatment.
Efficacy of CBCT
Accurate evaluation of alveolar bone height and thickness is important prior to periodontal and orthodontic treatments. Dimensional changes in alveolar bone have been found to be associated with orthodontic tooth movement, especially in skeletal Class II treatment due to excessive proclination of mandibular anterior teeth, often creating dehiscences and/or fenestrations around teeth. Research showed that dentoalveolar bone deficiency is not pathologic but a pre-existing condition. Therefore, measurements of alveolar bone height, thickness, and volume play critical roles not only in the initial assessment for tooth movement but also in the final evaluation after orthodontic treatment in order to provide long-term stability.
Advantages of CBCT are visualization of anatomic structures in the three dimensions, precision for diagnosis, and accuracy of analysis. A number of studies have demonstrated that CBCT can be used to measure alveolar bone height and thickness with accuracy and reliability [17,18,19]. However, some research reported there was a systematic overestimation of the CBCT measurements and alerted that a severe dehiscence might not be as serious as the CBCT showed [20, 21].
Menezes et al. [17] found excellent interexaminer and intraexaminer reproducibility of buccal and lingual bone plate thickness measurements in CBCT images on dried human mandibles and demonstrated good precision for voxel dimensions of 0.2, 0.3, and 0.4 mm. On the other hand, Leung et al. [20] reported that alveolar bone height can be measured to an accuracy of about 0.6 mm and the specificity was high at 0.95, but the sensitivity was low at 0.40 by using a voxel size of 0.38 mm. However, compared with CBCT of alveolar bone in vivo, direct assessment of dry skulls lacks the image of the periodontal apparatus (soft tissue); thus, it may result in drastic errors. To resolve this discrepancy, Timock et al. [18] evaluated human cadaver specimens. They found that mean absolute errors between CBCT at 0.3 mm voxel size and direct measurements of buccal bone height and buccal bone thickness were small (0.30 and 0.13 mm, respectively) and showed no statistically significant differences or bias to underestimate or overestimate. Interoperator reliability had great agreement for CBCT measurements of buccal bone height (0.98) and buccal bone thickness (0.91) while intraoperator reliability was high as interoperator correlations for CBCT buccal bone height (>0.97) and buccal bone thickness (0.90). In a current study with an 0.3-mm voxel size that was selected due to the balance of the amount of radiation exposure and clinical relevance [19], for intraoperator reliability, the mean absolute differences in alveolar bone thickness estimates were 0.24 mm with a Pearson correlation (0.93) and 0.44 mm with a correlation (0.91) for alveolar bone height. Between operators, the mean absolute difference was 0.29 mm (0.92) for the thickness, and 0.28 mm (0.95) for the height. The high correlation between and within operators suggested that these measurements were replicable and robust. The measurements of alveolar bone thickness and height may be accurate while the sensitivity might not be as high as the specificity. These different reports suggested that further attention should be paid to defining the accuracy of CBCT measurements and evaluation. However, with careful assessment of each research, they might have been associated with variables in the study designs, such as the different subjects (hard tissue only with human dry skulls, hard and soft tissues with human cadavers, or patients), voxel sizes utilized for the CBCT measurements, CBCT manufactures, and software. In the latest systematic review, Li et al. [22] reported that the mean differences between CBCT and direct physical measurements for alveolar bone height (mean difference = 0.03 mm) and alveolar bone thickness (mean difference = 0.11 mm) were not statistically significant. They concluded that there is no significant difference between CBCT and direct measurements for the alveolar bone height and thickness.
Orthodontics and Gingival Recession
Dimensional Changes of Dentoalveolar Gingival Complex
In orthodontics, the consideration of tooth movement is not only bone resorption and apposition but also the response of soft tissue. For instance, when pure extrusion is implemented on an intact tooth, the orthodontic force creates a tension on the dentoalveolar fibers, making them stretched and elongated. This extension of the fibers on the surface of the bone can lead to the new bone formation [23]. As a result, not only bone apposition on the cervical and apical parts of the alveolar bone but also increase in the width of keratinized gingiva, decrease of sulcus depth in a short-term, and movement of mucogingival junction occur [24]. In order to comprehend the tooth movement, the concept of “Dentoalveolar gingival complex” become essential. Dentoalveolar gingival complex consists of enamel, dentin, cementum, junctional epithelium, gingiva, alveolar mucosa, mucogingival junction, periosteum, alveolar bone, and periodontal ligament. These components are intricately connected with each other through homeostasis. Dimensions of the complex can be changed pre- and post-orthodontic treatment.
In animal studies, following extensive bodily movement of incisors in a labial direction through the alveolar bone, most teeth clinically demonstrated some apical displacement of the gingival margin [25]. However, when evaluated histologically, there was no attachment loss, but alveolar bone resorption was found. Karring et al. [26] concluded that dehiscences can be produced by labial tipping but bone will reform in such defects when the teeth are moved back to their original position without attachment loss.
Prevalence of Gingival Recession: No Orthodontic Treatment
Prevalence of gingival recession is diverse in research due to the different criteria such as various age groups, regions, observation periods, or definition of recessions. In general, the prevalence and severity of gingival recession are less in children and increase with age. In Saudi Arabia, 1336 children aged 10–15 years, gingival recession was found in 9.9% of the patients [27]. In Germany, adolescents who were diagnosed as Class II div1 were investigated and the prevalence for teeth with gingival recession >0.5 mm was 1.1% [28]. The prevalence of gingival recession (≥1 mm) was 29.5% of the subjects and 2.9% of teeth in adolescents (14–19 year old) in Brazil [29]. In Sweden [30], 62% of the 15-year-old subjects presented gingival recession. The number of affected teeth per individual was low, one tooth in about 35% and teeth in 25% of the individuals. In untreated 17-year-olds, 8.7% of teeth had recessions in Finland [31]. In Israel, healthy patients (18–22 years old) who had routine dental examinations at a military dental center presented gingival recession in 14.6% of the subjects and in 1.6% of all examined teeth [32].
Focusing on mandibular incisors, the prevalence was 5% at age 7 years in Finnish children [31] and similar value (4.8%) was shown in Brazilian study [33]. Parfitt and Mjör [34] reported the prevalence of gingival recession in the mandibular central incisors was 7.7% in a group of 668 children aged 9–12 years. In high school children aged 14–19 years, gingival recession was noted in the mandibular incisors in 13.1% of 766 students, frequently in association with malposition of the teeth [35]. In Class II malocclusion, 7.7% of mandibular central incisors from 98 children exhibited gingival recession [36] and the highest prevalence (approximately 5.2%) was seen for the mandibular central incisors whom less than 1% exhibited gingival recession with a magnitude >2.0 mm, comparing with other teeth [28].
In the population above 30 years old, using data representative of the United States population (NHANES III), Albander and Kingman [37] reported that 22.5% of teeth exhibited at more than 3 mm of recession, 5.5% at more than 5 mm, respectively. They stated that the prevalence and extent of recession among untreated subjects increase steadily with age. Susin et at. [29] assessed untreated Brazilians (aged 14 years and older) and found that gingival recession ≥3 mm was 17.0% of teeth while recession ≥5 mm was 5.8% of teeth. Also, they mentioned that the prevalence, extent, and severity of recession correlated with age. Approximately, 96% of the subjects in their 30 to 39-year-old cohort demonstrated gingival recessions on at least 1 tooth, and 44.3% of teeth had recessions of 1 mm or more. In France, subjects (age range: 35 to 65 years) were evaluated and a total of 84.6% of the sample had at least one gingival recession. While gingival recession (1–3 mm) was 76.9% of the population, severe recession depths (>6 mm) were only found in 1.8% of the subjects [38]. A multivariate linear regression model showed that age was associated with the extent of gingival recession. In a long-term follow-up study with dental students [39], the prevalence of gingival recession was 85% and did not change after 10 years.
Regarding gingival recession of mandibular incisors, 19.7% of mandibular central incisors had recessions of 1 mm or more in persons 30–55 years old while 49.7% had recessions in the group above 55 years old [37].
Depending upon research, the prevalence of very mild gingival recession has been reported up to 30% in young children. However, severe gingival recession seems to be less than 1%. In adults, the prevalence, extent, and severity of recession increase steadily with age. Yet, severe recession was only found in less than 10% of subjects or teeth. The data showed that higher prevalence was seen on mandibular central incisors.
Post-Orthodontic Treatment and Gingival Recession
In children, there were no statistically significant differences between the treated (with premolars extraction) and untreated adolescents before, during, and after the period of active treatment [40]. Closs et al. [33] evaluated gingival recessions on mandibular anterior teeth in Caucasian adolescents and concluded that gingival recessions occurred in patients after orthodontic therapy, but the extent and severity of this finding were low.
In adult patients, the mean difference of gingival recession between the treated adults and the controls was 0.14 mm, which was not clinically relevant [41]. New recessions developed in 10% of the investigated teeth but no change in 85%. Melsen and Allais [42] followed adult patients (Angle Class I or II malocclusion) who were treated with labial proclination of mandibular incisors and non-extraction. No significant increase in the mean gingival recession was observed during treatment. The prevalence of gingival recession greater than 0.1 mm increased from 21% before to 35% after treatment. Vasconcelos et al. [43] found that the prevalence of gingival recessions after orthodontic treatment was 10.4%. Most (8.6%) were classified as Miller CI, and 1.7% were classified as Miller CII. There were no Miller CIII or CIV.
In long term, Gebistorf et al. [44] reported that the prevalence of labial gingival recession increased during orthodontic treatment with further increases during 10 to 15 years posttreatment; 98.9% of the orthodontically treated participants had at least 1 labial recession, which was similar to the untreated controls. Orthodontically treated patients were not compromised in the long term compared with those with malocclusion that was untreated for many years. In New Zealand, Thomas et al. [45] evaluated 12-year-old children and the prevalence of gingival recession (1 mm or larger) was in 66–70% of the subjects after 14 years. In treated patients, 6.9% of the teeth exhibited recessions while 7.0% of the teeth in untreated subjects. There was no statistically significant difference between them. Morris et al. [46] evaluated adolescents including all malocclusion (premolar extractions were 60% of the sample). Only 5.8% of teeth exhibited recession at the end of orthodontic treatment (only 0.6% had recession >1 mm). After 16 years follow-up, 41.7% of the teeth showed recession, but the severity was limited (only 7.0% >1 mm). As a conclusion, orthodontic treatment is not a major risk factor for the development of gingival recession. In the systematic review on the effects of orthodontic therapy on periodontal health, Bollen et al. [47] found that orthodontic treatment was associated with 0.03 mm of gingival recession and 0.23 mm of increased pocket depth when compared with no treatment. They mentioned that orthodontic therapy has a minimum effect on the periodontal tissues. Another systematic review [48], similarly, concluded that the amount of gingival recession did not increase significantly after treatment with normal occlusion.
In contrast, a positive association between the past orthodontic therapy and the development of gingival recessions in orthodontically treated young adults (18–22 years old) doubled in comparison to untreated individuals (22.9% versus 11.4%, respectively) [32]. Moreover, orthodontic treatment tended to have more severe (>3 mm) and more extensive (3 or more recession sites) gingival recessions. Renkema et al. [49] reported that there was a continuous increase in gingival recessions after treatment from 6.6% at the end of treatment to 38% at 5 years post-treatment. Patients under 16 years of age at the end of treatment were less likely to develop gingival recessions than patients over 16 years. The prevalence of gingival recessions steadily increased after orthodontic treatment in older patients. The ability of the periodontium to withstand orthodontic treatment appears to decrease with age. Renkema et al. [50] compared 100 orthodontic subjects and 120 controls in Norwegian Caucasians approximately after 8 years post-orthodontic treatment. At least one recession site in all the teeth presented in 31% of the treated cases and 16.7% of the controls (ratio; 2:1). The odds ratio for orthodontic patients as compared with controls to have recessions was 4.48. The OR for the increase of age/year to have recessions was 1.53. The mean number of recessions for treated cases was estimated to be 142% higher than for controls. They concluded that orthodontic treatment may be risk factors for the development of labial gingival recessions. Sawan et al. [51] found that non-extraction orthodontic treatment had 1.31 times higher odds of gingival recession (Fig. 3).
The patient was diagnosed as angle Class II malocclusion with severe crowding on mandible (a–c). The patient rejected tooth extraction and requested clear aligner treatment. During the treatment, gingival manifestation changed thick to thin. Eventually, loss of keratinized gingiva and attachment loss (d, e) occurred prior to completion of leveling and alignment (f)
In terms of mandibular incisors, fewer than 10% of subjects had gingival recession greater than 2 mm after treatment [42]. The prevalence of gingival recessions after orthodontic treatment was 10.4%, and the recession was predominantly found on mandibular central incisors (87% of affected teeth with gingival recession) but of minor prevalence and severity [43]. The mandibular central incisors showed the most recession, with 12.8% exhibiting <1 mm of recession and 0.7% with >1.0 mm at the end of treatment. After 16 years follow-up, it showed almost 53% exhibiting recession, and 10.3% showing >1 mm of recession on mandibular central incisors [46]. At least one mandibular incisor with a recession was found in 13% orthodontically treated cases and 1.7% controls (ratio; 8:1) after 8 years post-orthodontic treatment [50]. In orthodontically treated subjects, mandibular incisors seem to be the most vulnerable to the development of gingival recessions. The risk for orthodontic patients to present with labial gingival recession seemed to increase at 6 years post-treatment (mandibular incisors: odds ratio: 8.81) [48]. However, these findings should be viewed cautiously until more studies of high quality become available. It is important to identify patients at potential risk and consider the possible implications for orthodontic treatment.
Inclination of Mandibular Incisors and its Limitation
The etiology of gingival recession is multifactorial, and history of orthodontic treatment can be considered as a part of it. However, orthodontic treatment includes different types of tooth movement, mechanics, treatment modalities, malocclusion, or skeletal discrepancies. In this chapter, we focus on only orthodontic-related factors at the mandibular anterior region, especially the relationships between labiolingual tooth movement, symphysis, and gingival recession.
Lingual tooth movement increased labiolingual thickness of the tissue at the facial aspect of the tooth which resulted in coronal migration of the soft tissue margin (Fig. 4) [52]. Dorfman [53] evaluated adolescents who began with minimal keratinized gingiva (<2 mm). In this group of patients, 67% of the patients showed a decrease in the width of keratinized gingiva with either minimal or some labial movement of the mandibular incisors; the keratinized gingival width increased in 33% of the patients who had about 3 mm total lingual tooth movement of the incisors during orthodontic treatment. This might be the combination of the retraction and extrusion during the time of treatment. Similarly, the gingival recessions were reduced in all patients after retracting the roots that were positioned outside the alveolar bone [54]. However, the reduction in recession depth did not result in increased width of the keratinized gingiva in most patients. As a conclusion, orthodontic correction of the root toward the center of the alveolar housing consistently improves gingival recessions but not necessary always increases the width of the keratinized gingiva. Kalina et al. [55] reported that multiple regression analysis confirmed that more tooth proclination was associated with a higher risk for an increase in gingival recession and showed improvement with retroclining mandibular incisors (mean change in inclination of −7.2°).
The patient was diagnosed as angle Class I malocclusion, anterior spacing, anterior open bite, and negative overjet (a–c). The mandibular incisors proclined labially and the root were labially positioned. Clinically, minimum attached gingiva, gingival inflammation, loss of attachment, and thin scalloped gingival biotype on mandibular incisors were found. After the completion of the treatment and lingual tooth movement (d–f), an increased gingival thickness and width at the facial aspect of the tooth occurred, which resulted in coronal migration of the soft tissue margin
On the other hand, the association between the amount of mandibular incisor proclination and the gingival recession during orthodontic treatment has been controversial. Some studies showed no relationship [36, 46, 56,57,58,59,60] and others did [55, 63,64,65]. Ruf et al. [36] found that proclining mandibular incisors in adolescents who had Class II malocclusion by 8.9° did not increase the risk of recession. Artun and Grobéty [56] followed the young patients who had Class II malocclusion. The post-treatment inclination of mandibular incisors was 99.1° (the change +9.98°) in the proclined group and 96.2° (+1.67°) in the control group, respectively. Clinical examinations revealed no differences in the amount of recession between the groups and gingival recession that occurred during the period of active treatment was not progressive. Djeu et al. [57] found that the changes of IMPA and L1-NB during the treatment were 5.0° and 0.87 mm in the excessive proclination group, −4.3° and −0.41 mm in the non-proclination group, respectively. They concluded that there was no increased risk of development of gingival recession. Renkema et al. [58] divided adolescents into 3 groups: retroclined (IMPA ≤ −1°), stable (>−1°, ≤1°), and proclined (>1°) groups. At the 5-year post-treatment, gingival recessions were present in all groups, but the difference was not significant. They concluded that the change of inclination of mandibular incisors during orthodontic treatment did not affect development of labial gingival recessions in this patient group. Yared et al. [59] concluded that the final IMPA>95° had no statistically significant correlation with gingival recession in the Angle Class I and Class II malocclusion patients (aged from 18 to 33). Morris [46] reported a similar result that there were no statistically significant differences in gingival recession between the subjects with IMPA >95° and <95° at 16 years post-treatment. Correspondingly, Renkema et al. [60] found that no difference in gingival recession between patients with a final IMPA <95° and IMPA >100.5° 5 years after orthodontic treatment. The result might be explained by a lack of excessive proclination during the treatment. The changes of inclination of mandibular incisors pre- and post-treatment were 1.3° and 6.6° in the non-proclined and proclined groups, respectively. Antonarakis et al. [61] reported that there were no significant differences in gingival recessions on mandibular incisors between the proclined group (Initial; 87.2°, post-orthodontic treatment; 95.4°, change; 8.2°) and non-proclined group (Initial; 91.6°, post-treatment; 91.8°, change; 0.2°). A recent review [62] showed no strong evidence that orthodontic proclination of mandibular incisors increases the risk of recession development.
Artun and Krogstad [63], contrarily, reported significantly more teeth developing gingival recession both during and 3 years after the treatment in the patients with excessive proclination (IMPA ≧ 10°) than with minimal inclination change. Only minimal changes of gingival margin were observed from 3 years postoperatively to 8-year follow-up examination. They concluded that development of gingival recession during excessive proclination of mandibular incisors seems to be inevitable, especially in patients with thin alveolar housing. However, the long-term prognosis for such teeth with extensive gingival recessions may not be critical. Most of the gingival recession seems to take place during or shortly after active therapy. Pernet et al. [64] found that excessive proclination (≥10°) of the lower incisors demonstrated an association with the onset of recessions in 25% of the cases. Kalina et al. [55] found teeth in which recession increase had a mean change in inclination of 7.6° in adult patients. Multiple regression analysis confirmed that more tooth proclination was associated with a higher risk for developing gingival recession. Lee et al. [65] reported that tooth inclination had a significant association with gingival recession, and as tooth inclination increased labially, gingival recession increased by approximately 0.2 mm per 1°.
Overall, the majority of the study designs were retrospective [36, 46, 56,57,58,59,60,61, 63,64,65] in nature, and only one prospective study [55] has been conducted in terms of the relationship between incisor inclination and gingival recession. A systematic review [62] found no strong evidence between proclination of mandibular incisors and the risk for gingival recession. However, only two observational studies were included in the qualitative analysis, and a meta-analysis could not be applied. The discrepancy between the various findings and the results can be explained by the high heterogeneity between studies. There were numerous variables in the inclusion/exclusion criteria, such as different age groups, angle malocclusion, measurements (casts, pictures, periodontal charts), orthodontic mechanics, treatment modalities (extraction/non-extraction), and directions of tooth movement in each study. For example, a case selection such as only Class II malocclusion with non-extraction treatment gives the impact that the mandibular incisal inclination may increase and determine the direction of the tooth movement labially in the subjects. However, if Class III patients with camouflage treatment which is mandibular two premolars extraction are included in a study, reduced mandibular incisal inclination and lingual tooth movement in the group will be expected. So, if some study included all malocclusion, it is very difficult to see a statistically significant difference. If only young children are observed for a short period of time after orthodontic treatment, gingival recession may not be detected regardless of directions of tooth movement. Currently, due to the absence of higher-level studies and the high heterogeneity of the studies, there is a limitation to determine the orthodontic boundary limits through the association between mandibular incisor inclination and gingival recession so far. The findings should be viewed cautiously until a higher quality of evidence becomes available.
Symphysis and Gingival Recession
Mulie and Ten Hoeve [66] demonstrated that anatomic limitations in the symphysis were associated with compromised periodontal outcomes when these limits are invaded. However, it should be noted that the evaluation of the symphysis has not been standardized or established yet, especially due to the superimposition of anatomical landmarks on cephalometric radiographs. Consequently, the findings may not show any associations between symphysis shape or alveolar ridge changes after orthodontic treatment and gingival recession [64, 67, 68]. Pernet et al. [64] evaluated 126 orthodontically treated patients before, immediately after treatment and at long-term retention (mean 7.3 years). No association was found between the width of the alveolar bone process at the level of the crest, symphysis width, the vertical skeletal pattern, and the onset of gingival recessions. The vertical facial morphology was not associated with the development of new recessions. They found some evidence that increased symphysis height and ratio between the symphysis height and the width at the crest level are associated with the development of recessions. Closs et al. [67] treated adolescents without extractions and found gingival recession increased after orthodontic therapy. However, no association was observed on average of symphysis dimensions and the development of gingival recessions. They concluded that pre-treatment symphysis dimensions may not be used as predictors of gingival recession after orthodontic therapy. Mazurova et al. [68] reported that gingival labial recession was present in 19.3% of patients with narrow symphysis, 20.6% with average symphysis, and 14% of patients with wide symphysis at 5 years post-treatment.
In conclusion, there is no evidence that the overall morphology of the mandibular symphysis is associated with developing gingival recessions. Evaluation of symphysis morphology on cephalometric radiographs might not be a solid method aimed at predicting gingival recession in the anterior region of the mandible yet. Utilizing CBCT imaging may be a better option to evaluate morphology of symphysis. Further studies are required to explain the relationship between the symphysis dimensions, alveolar width, and the risk of gingival recession.
Does Compensatory Bone Formation Occur After Labial Tooth Movement?
Compensatory Bone Formation
The “compensatory bone formation” theory of tooth movement [69] was when teeth were moved labially and passed the original cortical plate, the bone around dehiscences would have remodeled and the alveolar bone thickness would have maintained or increased if light force had been applied or the teeth had been retained in the facially moved position for a longer time period. Wingard and Bowers [70] studied male monkeys where mandibular incisors were moved labially 2.1–5 mm resulting in dehiscences failing to develop with forces up to 170 gm over 36 to 95 days followed by 4 months of retention. Their results supported the compensatory bone formation after labial tooth movement and are frequently quoted in literature. On the other hand, in the Steiner’s study with female monkeys [71], after the mandibular central incisors were bodily moved 2–4 mm (mean distance: 3.05 mm) in a labial direction without extrusion and retained 3 weeks, the crest of the marginal bone receded apically by 2.7 mm to 9.1 mm (mean: 5.89 mm). Similarly, other studies [25, 26, 72] developed dehiscences with 50 gm light force for a period of 3–5 months after 1-, 5- and 8-month retention period. In addition, none of the histologic studies [25, 26, 71, 72] indicates that the labial plate was reestablished. These studies agreed with the previous Reitan’s studies [73, 74] where dehiscences formed when teeth were tipped labially due to a lack of compensatory bone formation on the labial side. There might be various reasons why no dehiscence occurred in the Wingard and Bowers study [70]. One possible explanation could be incomplete labial movement to push the roots enough from the alveolar process with a 0.018-in. round wire due to the crown tipping. The magnitude of developing dehiscences on the labial plate with labial tipping is less than with bodily movement.
These results indicate that the discrepancy on each study regarding compensatory bone formation may not be related to the difference of the magnitude of force application or retention periods, but rather the difference of the amount of labiolingual tooth movement. It can be concluded that compensatory bone formation does not occur around newly developed dehiscences after the tooth movement, even though the force application is terminated, and the teeth are retained in their facially displaced position. Therefore, it should be emphasized that dimensions of dentoalveolar gingival complex change after tooth movement and are not maintained once the tooth moves beyond “orthodontic boundary limits.”
Dentoalveolar Bone Deficiency
Boney defects under gingiva which are determined by dehiscences and fenestrations may be considered as “dentoalveolar bone deficiency.” The etiology of dentoalveolar bone deficiency during orthodontic treatment is multifactorial and includes the direction of tooth movement, the magnitude of orthodontic forces, the amount of tooth movement, the alveolar bone dimensions, and anatomic integrity of dentoalveolar gingival complex [52, 75]. Anatomically, the alveolar bone becomes thinner from the posterior to the anterior region in the mandible [76]. While fenestration was seen in the maxillary premolar region, dehiscence was seen in the mandibular anterior region [77]. Dentoalveolar bone deficiency is not uncommon on mandibular central incisors and the prevalence was reported, approximately 24–45% (dehiscence, Fig. 5) and 5–21% (fenestration, Fig. 6) [77,78,79,80].
The prevalence of dentoalveolar bone deficiency in mandibular central incisors has been reported based upon various facial, vertical growth, and skeletal types in untreated subjects. Evangelista et al. [79] compared the presence of dehiscences and fenestrations in patients with Class I and Class II division 1 malocclusions and different facial types (brachyfacial, mesofacial, and dolichofacial), and found that the incidence of dehiscences and fenestrations was 24.3% and 21.1%, respectively. No difference was found between facial types. Enhos et al. [77] reported the presence of dehiscences and fenestrations with different vertical growth patterns (hyper-, normo-, and hypo-divergent) and it was 25.0–30.6% and 14.3–16.7%, respectively. Yagci et al. [78] evaluated the presence of dehiscences among patients with skeletal Class I, II, and III malocclusions and showed the incidence, 27.9%, 27.1%, and 25.9%, respectively. There was no difference in the prevalence of dehiscence among the three groups. In another study [19] that specifically focused on skeletal Class II cases, the incidence of dehiscence was 32% of teeth in males and 24% of teeth in females prior to the orthodontic treatment.
Focusing on the patients after orthodontic treatment, the incidence of dehiscence on mandibular central incisors significantly increased based on CBCT studies. Castro et al. [81] evaluated patients who had non-extraction treatment with angle Class I malocclusion and mild to moderate crowding. The incidence of dehiscence was changed from 13% of the teeth before orthodontic treatment to 37% after treatment. Garlock et al. [82] found that the average labial vertical bone loss was 1.16 ± 2.26 mm after orthodontic treatment in Class I and II cases. Matsumoto et al. [19] reported that the incidence of dehiscences increased to 58% in males and to 45% in females at the end of the orthodontic treatment. There was no significant association between sex and dehiscence frequency at either time point. Additionally, they mentioned that the total average loss of the alveolar bone height was −1.42 mm. In non-extraction cases, the current systematic review [83] concluded that the dehiscence deteriorated significantly on the labial side −0.97 mm on mandibular incisors.
To minimize these problems, the alveolar bone morphology must be evaluated before orthodontic treatment as a part of diagnosis. CBCT imaging has been shown to be an excellent modality in assessing bone topography and anatomy [13]. Taking the presence of pre-existing dehiscences and fenestrations into consideration in a comprehensive treatment plan reduces the risk of future attachment loss, especially when teeth are moved in a labiolingual direction. It has also been shown that the presence of dentoalveolar bone deficiency in the alveolar bone is not pathognomonic but is a potential risk for exacerbating gingival recession.
Orthodontic Boundary Limits of Mandibular Incisor Advancement
What Is the Limitation of Tooth Movement?
There is the risk for developing gingival recessions in conjunction with orthodontic tooth movement only if the tooth is moved out of the alveolar bone housing [52]. However, gingival recession is simply a clinical manifestation of an underlying alveolar bone deficiency [ 84]. Gingival recession has been thought as a part of the limitation of tooth movement and gingival augmentation can be considered for teeth with a lack of keratinized tissue or thin phenotype prior to orthodontic treatment [85]. Nevertheless, if dehiscence is one of the contributing factors for gingival recession, it might be preferable to evaluate alveolar bone deficiency to determine the orthodontic boundary limits of tooth movement instead.
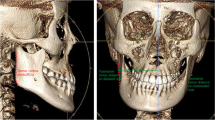
Recently, with more and more research incorporating CBCT images into the orthodontic boundary limits, Matsumoto et al. [ 19] addressed the limits of mandibular incisor advancement. In 60 skeletal Class II patients, CBCT images were obtained and the patients were divided into four groups based on the presence of dehiscences at pre- and post-orthodontic treatment. The alveolar bone height and width were measured on the CBCT images. One of the four groups was designated for dehiscence prior to the treatment with no remaining dehiscences upon completion of orthodontic therapy. No patients were identified with that group. This result indicates that orthodontic treatment alone does not help reduce the pre-existing dehiscences in the patients who have skeletal Class II (ANB > 3°) with a retrognathic mandible without extraction. Their thought-provoking finding in this study was the relationship between dehiscences and tooth movement. It demonstrated through the segmented-regression analysis that for each 1 mm increase in L1-NB over 0.71 mm, there was a predictable loss of 1.49 mm in alveolar crestal bone height. Similarly, for each 1° increase in IMPA over 3.0°, there was a predictable loss of −0.48 mm in alveolar crestal bone height. In addition, excessive protrusion (L1-NB > 3 mm) and proclination (IMPA > 9°) of mandibular central incisors caused dehiscences, while patients with tooth movement controlled within L1-NB <1 mm and IMPA <4° had less possibility to develop dehiscences. Based upon the logistic regression analysis on L1-NB and IMPA, each 0.5 mm change in L1-NB was predicted to increase the odds of developing by dehiscence by 2.62-fold while a 1° change in IMPA was predicted to increase the odds by 1.73-fold. This translated into a 50% probability of vertical bone loss at an L1-NB change 2.00 mm, or equivalently, an IMPA change of 8.02°. Therefore, L1-NB = 2 mm and IMPA = 8° might be considered as the orthodontic boundary limits of protrusion and proclination in order to prevent development of dehiscences after conventional orthodontic treatment in skeletal Class II patients.
As we reviewed previously, similar results were reported regarding the relationship between incisor inclination and gingival recession. In skeletal Class III studies [63], it found significantly more recessions during and after orthodontic treatment in the patients with excessive proclination (IMPA ≥ 10°) than minimal change (IMPA < 2°). The excessive proclination of mandibular central incisors (IMPA = 10°) prior to orthognathic surgery showed that the vertical alveolar bone level and the alveolar bone thickness of the labial were significantly reduced [86]. Pernet et al. [64] found that excessive proclination (≥10°) of the mandibular incisors demonstrated an association with the onset of recessions in 25% of the cases. Kalina et al. [55] evaluated adult patients and found teeth in which recession increased had a mean change in inclination of 7.6°.
The difference of focusing on dehiscences [19] or gingival recessions [55, 63, 64] in research is how to manage the risk of iatrogenic sequelae. Since gingival recessions are the consequence of the underlying alveolar bone deficiency, gingival recessions may or may not occur after excessive proclination at the time of evaluation, especially in young children. In order to determine the orthodontic boundary limits, focusing on rather alveolar bone deficiency than gingival recession allows us to obtain more accurate information and prevent undesired periodontal sequelae during the time of orthodontic treatment.
Additionally, the various initial conditions such as the root position, the tooth angulation, the hard and soft tissue thickness around the teeth, and surrounding muscles may impact the orthodontic boundary limits of mandibular incisor advancement in skeletal Class II cases.
Conclusion
When treating skeletal Class II patients, CBCT imaging elucidated that the orthodontic boundary limits might be less than previously thought, and the negative impacts on the dentoalveolar gingival complex should be considered. Additionally, pre-existing dehiscences in the mandibular central incisors were evident in the patients that had skeletal Class II malocclusion. In order to maintain a healthy periodontium after orthodontic treatment, a thorough and comprehensive evaluation of the dentoalveolar gingival complex and careful three-dimensional diagnosis must be performed prior to orthodontic treatment. Furthermore, if excessive protrusion and/or proclination is contemplated in the treatment plan, additional treatment modalities such as orthognathic surgery, tooth extraction, and corticotomy with bone grafting (periodontally accelerated osteogenic orthodontics: PAOO, surgically facilitated orthodontic therapy: SFOT, corticotomy-assisted orthodontic therapy: CAOT) should be taken into consideration to avoid inadvertent periodontal complications (dehiscences, fenestrations, and gingival recessions) during and/or after orthodontic treatment.
References
Proffit WR, Ackerman JL. Diagnosis and treatment planning. In: Graber TM, Swain BF, editors. Current orthodontic concepts and techniques, chapter 1. St. Louis: Mosby; 1982. p. 3–100.
Graber TM, Vanarsdall RL, Vig KWL. Orthodontics: current principles & techniques. 4th ed. St. Louis: Mosby; 2000. p. 3–70.
Proffit WR, Fields HW Jr, Sarver DM. Contemporary orthodontics. 4th ed. St. Louis: Mosby; 2007. p. 167–233.
Larson BE. Cone-beam computed tomography is the imaging technique of choice for comprehensive orthodontic assessment. Am J Orthod Dentofac Orthop. 2012;141(4):402–10.
Halazonetis DJ. Cone-beam computed tomography is not the imaging technique of choice for comprehensive orthodontic assessment. Am J Orthod Dentofac Orthop. 2012;141(4):403–11.
Steiner C. Cephalometrics for you and me. Am J Orthod. 1953;39:729–55.
American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143(8):899–902.
American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. [corrected]. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(2):238–57.
Baumrind S, Miller D, Molthen R. The reliability of head film measurements. 3. Tracing superimposition. Am J Orthod Dentofac Orthop. 1976;70:617–44.
Moyers RE, Bookstein FL. The inappropriateness of conventional cephalometrics. Am J Orthod Dentofac Orthop. 1979;75(6):599–617.
Haney E, Gansky SA, Lee JS, Johnson E, Maki K, Miller AJ, Huang JC. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofac Orthop. 2010;137(5):590–7.
Botticelli S, Verna C, Cattaneo PM, Heidmann J, Melsen B. Two versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur J Orthod. 2011;33(4):344–9.
Fuhrmann R. Three-dimensional interpretation of labiolingual bone width of the lower incisors. Part II. J Orofac Orthop. 1996;57(3):168–85.
Wei D, Zhang L, Li W, Jia Y. Quantitative comparison of cephalogram and cone-beam computed tomography in the evaluation of alveolar bone thickness of maxillary incisors. Turk J Orthod. 2020;33(2):85–91.
Mandelaris GA, Scheyer ET, Evans M, Kim D, McAllister B, Nevins ML, Rios HF, Sarment D. American academy of periodontology best evidence consensus statement on selected oral applications for cone-beam computed tomography. J Periodontol. 2017;88(10):939–45.
Mandelaris GA, Neiva R, Chambrone L. Cone-beam computed tomography and interdisciplinary dentofacial therapy: an American academy of periodontology best evidence review focusing on risk assessment of the dentoalveolar bone changes influenced by tooth movement. J Periodontol. 2017;88(10):960–77.
Menezes CCD, Janson G, Massaro CDS, Cambiaghi L, Garib DG. Reproducibility of bone plate thickness measurements with cone-beam computed tomography using different image acquisition protocols. Dent Press J Orthod. 2010;15(5):143–9.
Timock AM, Cook V, McDonald T, Leo MC, Crowe J, Benninger BL, Covell DA Jr. Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofac Orthop. 2011;140(5):734–44.
Matsumoto K, Sherrill-Mix S, Boucher N, Tanna N. A cone-beam computed tomographic evaluation of alveolar bone dimensional changes and the periodontal limits of mandibular incisor advancement in skeletal Class II patients. Angle Orthod. 2020;90(3):330–8.
Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofac Orthop. 2010;137(4 Suppl):S109–19.
Sun L, Zhang L, Shen G, Wang B, Fang B. Accuracy of cone-beam computed tomography in detecting alveolar bone dehiscences and fenestrations. Am J Orthod Dentofac Orthop. 2015;147(3):313–23.
Li Y, Deng S, Mei L, Li J, Qi M, Su S, Li Y, Zheng W. Accuracy of alveolar bone height and thickness measurements in cone beam computed tomography: a systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128(6):667–79.
Oppenheim A. Artificial elongation of teeth. Am J Orthod Oral Surg. 1940;26:931–8.
Kajiyama K, Murakami T, Yokota S. Gingival reactions after experimentally induced extrusion of the upper incisors in monkeys. Am J Orthod Dentofac Orthop. 1993;104(1):36–47.
Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14(3):121–9.
Karring T, Nyman S, Thilander B, Magnusson I. Bone regeneration in orthodontically produced alveolar bone dehiscences. J Periodontal Res. 1982;17(3):309–15.
Younes SA, El Angbawi MF. Gingival recession in the mandibular central incisor region of Saudi schoolchildren aged 10-15 years. Community Dent Oral Epidemiol. 1983;11(4):246–9.
Bock NC, Ruehl J, Ruf S. Prevalence, magnitude, and incidence of labial gingival recession with Herbst-multibracket appliance treatment: a retrospective cohort study. Angle Orthod. 2019;89(4):535–43.
Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J Periodontol. 2004;75(10):1377–86.
Björn AL, Andersson U, Olsson A. Gingival recession in 15-year-old pupils. Swed Dent J. 1981;5(4):141–6.
Ainamo J, Paloheimo L, Nordblad A, Murtomaa H. Gingival recession in schoolchildren at 7, 12 and 17 years of age in Espoo, Finland. Community Dent Oral Epidemiol. 1986;14(5):283–6.
Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofac Orthop. 2008;134(5):652–6.
Closs LQ, Grehs B, Raveli DB, Rösing CK. Occurrence, extension, and severity of gingival margin alterations after orthodontic treatment. World J Orthod. 2008;9(3):e1–6.
Parfitt GJ, Mjör IA. A clinical evaluation of local gingival recession in children. J Dent Child. 1964;31:257–62.
Trott JR, Love B. An analysis of gingival recession in 766 Winnipeg school children. Dent Pract Dent Rec. 1966;16(6):209–13.
Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession? Am J Orthod Dentofac Orthop. 1998;114(1):100–6.
Albandar JM, Kingman AA. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70(1):30–43.
Sarfati A, Bourgeois D, Katsahian S, Mora F, Bouchard P. Risk assessment for buccal gingival recession defects in an adult population. J Periodontol. 2010;81(10):1419–25.
Matas F, Sentís J, Mendieta C. Ten-year longitudinal study of gingival recession in dentists. J Clin Periodontol. 2011;38(12):1091–8.
Alstad S, Zachrisson BU. Longitudinal study of periodontal condition associated with orthodontic treatment in adolescents. Am J Orthod. 1979;76(3):277–86.
Allais D, Melsen B. Does labial movement of lower incisors influence the level of the gingival margin? A case-control study of adult orthodontic patients. Eur J Orthod. 2003;25(4):343–52.
Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofac Orthop. 2005;127(5):552–61.
Vasconcelos G, Kjellsen K, Preus H, Vandevska-Radunovic V, Hansen BF. Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatment. Angle Orthod. 2012;82(1):42–7.
Gebistorf M, Mijuskovic M, Pandis N, Fudalej PS, Katsaros C. Gingival recession in orthodontic patients 10 to 15 years posttreatment: a retrospective cohort study. Am J Orthod Dentofac Orthop. 2018;153(5):645–55.
Thomson WM. Orthodontic treatment outcomes in the long term: findings from a longitudinal study of New Zealanders. Angle Orthod. 2002;72(5):449–55.
Morris JW, Campbell PM, Tadlock LP, Boley J, Buschang PH. Prevalence of gingival recession after orthodontic tooth movements. Am J Orthod Dentofac Orthop. 2017;151(5):851–9.
Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139(4):413–22.
Bin Bahar BSK, Alkhalidy SR, Kaklamanos EG, Athanasiou AE. Do orthodontic patients develop more gingival recession in anterior teeth compared to untreated individuals? A systematic review of controlled studies. Int Orthod. 2020;18(1):1–9.
Renkema AM, Fudalej PS, Renkema A, Kiekens R, Katsaros C. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofac Orthop. 2013;143(2):206–12.
Renkema AM, Fudalej PS, Renkema AA, Abbas F, Bronkhorst E, Katsaros C. Gingival labial recessions in orthodontically treated and untreated individuals: a case - control study. J Clin Periodontol. 2013;40(6):631–7.
Sawan NM, Ghoneima A, Stewart K, Liu S. Risk factors contributing to gingival recession among patients undergoing different orthodontic treatment modalities. Interv Med Appl Sci. 2018;10(1):19–26.
Wennström JL. Mucogingival considerations in orthodontic treatment. Semin Orthod. 1996;2(1):46–54.
Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod. 1978;74(3):286–97.
Laursen MG, Rylev M, Melsen B. The role of orthodontics in the repair of gingival recessions. Am J Orthod Dentofac Orthop. 2020;157(1):29–34.
Kalina E, Zadurska M, Górski B. Postorthodontic lower incisor and canine inclination and labial gingival recession in adult patients: a prospective study. J Orofac Orthop. 2020;82(4):246–56.
Artun J, Grobéty D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. Am J Orthod Dentofac Orthop. 2001;119(1):2–10.
Djeu G, Hayes C, Zawaideh S. Correlation between mandibular central incisor proclination and gingival recession during fixed appliance therapy. Angle Orthod. 2002;72(3):238–45.
Renkema AM, Fudalej PS, Renkema A, Bronkhorst E, Katsaros C. Gingival recessions and the change of inclination of mandibular incisors during orthodontic treatment. Eur J Orthod. 2013;35(2):249–55.
Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop. 2006;130(1):6.e1–8.
Renkema AM, Navratilova Z, Mazurova K, Katsaros C, Fudalej PS. Gingival labial recessions and the post-treatment proclination of mandibular incisors. Eur J Orthod. 2015;37(5):508–13.
Antonarakis GS, Joss CU, Triaca A, Kuijpers-Jagtman AM, Kiliaridis S. Gingival recessions of lower incisors after proclination by orthodontics alone or in combination with anterior mandibular alveolar process distraction osteogenesis. Clin Oral Investig. 2017;21(8):2569–79.
Tepedino M, Franchi L, Fabbro O, Chimenti C. Post-orthodontic lower incisor inclination and gingival recession-a systematic review. Prog Orthod. 2018;19(1):1–7.
Artun J, Krogstad O. Periodontal status of mandibular incisors following excessive proclination. A study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofac Orthop. 1987;91(3):225–32.
Pernet F, Vento C, Pandis N, Kiliaridis S. Long-term evaluation of lower incisors gingival recessions after orthodontic treatment. Eur J Orthod. 2019;41(6):559–64.
Lee JB, Baek SJ, Kim M, Pang EK. Correlation analysis of gingival recession after orthodontic treatment in the anterior region: an evaluation of soft and hard tissues. J Periodontal Implant Sci. 2020;50(3):146–58.
Mulie RM, Ten Hoeve A. The limitations of tooth movement within the symphysis, studied with laminagraphy and standardized occlusal films. J Clin Orthod. 1976;10(12):882–93.
Closs LQ, Bortolini LF, dos Santos-Pinto A, Rösing CK. Association between post-orthodontic treatment gingival margin alterations and symphysis dimensions. Acta Odontol Latinoam. 2014;27(3):125–30.
Mazurova K, Kopp JB, Renkema AM, Pandis N, Katsaros C, Fudalej PS. Gingival recession in mandibular incisors and symphysis morphology-a retrospective cohort study. Eur J Orthod. 2018;40(2):185–92.
Gottlieb B, Orban B. Die Veränderungen der Gewebe bei ubermässiger Beanspruchung der Zahne. Leipzig: Georg Thieme; 1931.
Wingard CE, Bowers GM. The effects of facial bone from facial tipping of incisors in monkeys. J Periodontol. 1976;47(8):450–4.
Steiner GG, Pearson JK, Ainamo J. Changes of the marginal periodontium as a result of labial tooth movement in monkeys. J Periodontol. 1981;52(6):314–20.
Batenhorst KF, Bowers GM, Williams JE. Tissue changes resulting from facial tipping and extrusion of incisors in monkeys. J Periodontol. 1974;45(9):660–8.
Reitan K. Some factors determining the evaluation of forces in orthodontics. Am J Orthod. 1957;43(1):32–45.
Reitan K. Continuous bodily movement and its histological significance. Acta Odontol Scand. 1947;6:115–44.
Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone and symphysis after orthodontic treatment: a retrospective study. Am J Orthod Dentofac Orthop. 1996;110(3):239–46.
Swasty D, Lee JS, Huang JC, Maki K, Gansky SA, Hatcher D, Miller AJ. Anthropometric analysis of the human mandibular cortical bone as assessed by cone-beam computed tomography. J Oral Maxillofac Surg. 2009;67(3):491–500.
Enhos S, Uysal T, Yagci A, Veli İ, Ucar FI, Ozer T. Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod. 2012;82(5):868–74.
Yagci A, Veli I, Uysal T, Ucar FI, Ozer T, Enhos S. Dehiscence and fenestration in skeletal Class I, II and III malocclusions assessed with cone-beam computed tomography. Angle Orthod. 2012;82(1):67–74.
Evangelista K, Vasconcelos Kde F, Bumann A, Hirsch E, Nitka M, Silva MA. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138(2):133.e1–7.
Coşkun İ, Kaya B. Appraisal of the relationship between tooth inclination, dehiscence, fenestration, and sagittal skeletal pattern with cone beam computed tomography. Angle Orthod. 2019;89(4):544–51.
Castro LO, Castro IO, de Alencar AHG, Valladares-Neto J, Estrela C. Cone beam computed tomography evaluation of distance from cementoenamel junction to alveolar crest before and after nonextraction orthodontic treatment. Angle Orthod. 2016;86(4):543–9.
Garlock DT, Buschang PH, Araujo EA, Behrents RG, Kim KB. Evaluation of marginal alveolar bone in the anterior mandible with pretreatment and posttreatment computed tomography in nonextraction patients. Am J Orthod Dentofac Orthop. 2016;149(2):192–201.
Guo R, Zhang L, Hu M, Huang Y, Li W. Alveolar bone changes in maxillary and mandibular anterior teeth during orthodontic treatment: a systematic review and meta-analysis. Orthod Craniofac Res. 2021;24(2):165–79.
Richman C. Is gingival recession a consequence of an orthodontic tooth size and/or tooth position discrepancy? “A paradigm shift”. Compend Contin Educ Dent. 2011;32:e73–9.
Kim DM, Neiva R. Periodontal soft tissue non-root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(2 Suppl):S56–72.
Lee KM, Kim YI, Park SB, Son WS. Alveolar bone loss around lower incisors during surgical orthodontic treatment in mandibular prognathism. Angle Orthod. 2012;82(4):637–44.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Matsumoto, K. (2023). Management of Skeletal Class II Malocclusion: Historical Challenges and New Opportunities. In: Mandelaris, G.A., Vence, B.S. (eds) Surgically Facilitated Orthodontic Therapy. Springer, Cham. https://doi.org/10.1007/978-3-030-90099-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-90099-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-90098-4
Online ISBN: 978-3-030-90099-1
eBook Packages: MedicineMedicine (R0)