Abstract
Male infertility is one of the major challenging and prevalent diseases having diverse etiologies of which bacteriospermia play a significant role. It has been estimated that approximately 15% of all infertility cases are due to infections caused by uropathogens and in most of the cases bacteria are involved in infection and inflammation leading to the development of bacteriospermia. In response to bacterial load, excess infiltration of leukocytes in the urogenital tract occurs and concomitantly generates oxidative stress (OS). Bacteria may induce infertility either by directly interacting with sperm or by generating reactive oxygen species (ROS) and impair sperm parameters such as motility, volume, capacitation, hyperactivation. They may also induce apoptosis leading to sperm death. Acute bacteriospermia is related with another clinical condition called leukocytospermia and both compromise male fertility potential by OS-mediated damage to sperm leading to male infertility. However, bacteriospermia as a clinical condition as well as the mechanism of action remains poorly understood, necessitating further research in order to understand the role of individual bacterial species and their impact in male infertility.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
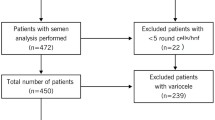
In the third decade of twenty-first century infertility remains one of the major challenging and highly prevalent global health conditions [1]. Male infertility is a multifactorial disorder and male urogenital infection is considered one of the major contributors to male infertility accounting approximately 15% of all male infertility cases [2]. Acute or chronic male urogenital tract infection is mediated by microorganisms particularly bacteria and it affects various parts of the male reproductive system such as testis, epididymis, and male accessory sex glands leading to impairment of sperm production, maturation, and movement in the seminal tract [3]. Pathogenic bacteria gain access to the male urogenital tract by sexually transmitted infection, intracanicular spread of bacteria from urine infection or hematogenous seeding of bacteria from urogenital organs [4, 5]. Development of bacteriospermia and concomitant increment of leukocytes in the male urogenital tract due to infection and inflammation may impair the fertility potential of a man through multiple mechanisms, such as deterioration of spermatogenesis, reduction in sperm motility, genital tract obstruction and/or dysfunction, and oxidative stress (OS) [5, 6]. Excessive bacterial colonization and successive infection in the urogenital tract impair male fertility through sperm adhesion, interaction and/or forming sperm agglutination thus reducing sperm motility and lowering the chance of sperm–oocyte fusion [7]. Moreover, bacterial infection causes chronic persistent inflammation and leukocyotspermia leading to increment of pro-inflammatory cytokines and reactive oxygen species (ROS) in the urogenital tract which ultimately contribute to the development of OS-associated male infertility [8, 9]. In bacteriospermia, prevalence of bacterial species varies depending on the population types, whereas their mechanism of action in male infertility is still understood poorly. A study conducted on Canadian population found 22 species in bacteriospermic ejaculates and the most prevalent bacteria were Enterococcus faecalis (56%) followed by Escherichia coli (16%), group B Streptococcus (13%), and Staphylococcus aureus (5%). These four bacterial species contribute up to 90% of all identified bacterial species [5]. Similarly, a study from India reported a total of 7 bacterial species from bacteriospermic ejaculates, and the most dominant species was E. faecalis (30%) followed by Coagulase negative Staphylococcus (23.33%), S. aureus (20%), E. coli (10%), Klebsiella pneumoniae (6.66%), Proteus sp. (6.66%), and Citrobacter sp. (3.33%) [10]. Another study on Czech population reported predominance of three species i.e., Staphylococcus sp., Streptococcus sp., and E. coli from abnormal semen samples of 116 infertile men [11]. The presence of bacterial species in the urogenital tract of bacteriospermic men and leukocytes response is still poorly understood. The bacteria may utilize multiple patho-mechanisms and develop OS thus contributing to the compromise of male fertility potential. This chapter mainly focuses on the role of bacteriospermia and OS in male infertility.
7.2 Oxidative Stress (OS) and Fertility Pattern in the Male
The reproductive organs of the male including testes, epididymis, vas deferens, and accessory glands are mainly involved in the formation, storage, and ejaculation of sperm. They also produce androgens that help in the development and maintenance of male fertility potential [12]. Impairment of reproductive organs due to low hormone synthesis, Klinefelter syndrome, cryptorchidism, autoimmune disorder, exposure to radiation, altered lifestyle, infection, OS, trauma, etc., may lead to male infertility [13, 14]. Male infertility is a multifactorial disorder and OS is considered as one of the major contributors to the disease. It is defined as an imbalance between the levels of ROS and antioxidants in the semen [15]. Free radicals are the unpaired electron containing molecules which are highly reactive against lipids, amino acids, and nucleic acids [16]. Prime sources of ROS in the semen include excessive leukocytes, immature sperm, varicocele, exposure to toxins such as radiation, smoking, alcohol consumption, etc. Excess ROS in the semen can overwhelm the antioxidant defense leading to concomitant development of OS and cause sperm dysfunction and/or death, and ultimately infertility in men [13]. However, optimum levels of ROS are crucial for facilitating sperm hyperactivation, motility [17], capacitation, and acrosomal reaction [16]. Controlled production of ROS in the sperm at the time of capacitation process increases the amount of cyclic adenosine 3′,5′- monophosphate (cAMP) that facilitates the hyperactivation of the spermatozoa. Hyperactivation is very crucial because only the hyperactivated sperm have increased motility to undergo the acrosomal reaction that may lead to successful fertilization [18]. Excessive leukocytes in respone to inflammation and immature sperm are the main source of ROS generation and mature sperm are highly susceptible to ROS due to the presence of polyunsaturated fatty acids in their membranes [19]. Uncontrolled rise in the level of ROS initiates lipid peroxidation (LPO) of the sperm membrane where up to 60% of the fatty acids are reduced thus altering the membrane fluidity, disrupting the activity of enzymes and membrane receptors which may ultimately lead to abnormal fertilization [20]. OS and elevated levels of ROS have also been associated with impaired sperm parameters such as motility, concentration, and morphology - which are the important indicators of a male’s fertility potential. Diminishing sperm motility is a result of a cascade of events including LPO of the plasma membrane, which affects axonemal protein phosphorylation and sperm immobilization [21, 22]. High levels of ROS cause significant sperm morphological abnormalities like head, neck, and tail deformities and retention of cytoplasmic droplets leading to male infertility [23]. OS also facilitates sperm DNA damage by fragmenting the single- and double-stranded DNA, direct oxidation of DNA bases, and by DNA mutations [24]. Furthermore, excessive generation of ROS directly disrupts the mitochondria electron transport chain (ETC) and has the ability to damage mitochondrial DNA which ultimately activates the stress response gene by altering the mitochondrial physiology and promote apoptosis by disrupting cell division [24, 25]. Low sperm motility due to mitochondrial dysfunction can also cause asthenozoospermia [24]. OS results into functional and metabolic disorder in germ cells, too [26]. Moreover, uncontrolled ROS can modify the protein status by oxidative reaction and generate aldehydes and ketones which reflect a negative effect on spermatogenesis and overall fertility of the male [27] (Fig. 7.1).
Bacteriospermia induce infection and inflammation in the urogenital tract of men and concomitantly increases leukocytes infiltration in the infected location. Both bacteriospermia and leukocytes increase ROS in urogenital tract leading to OS. ROS can cause sperm agglutination and reduce sperm motility. On the contrary OS damages sperm morphology, sperm DNA, mitochondrial DNA and reduce sperm acrosomal integrity, cause premature capacitation, induces lipid peroxidation and apoptosis in sperm which ultimately contribute to male infertility. ROS- reactive oxygen species, OS- oxidative stress, DNA- deoxyribonucleic acid
7.3 Bacteriospermia and Male Infertility
Infertility is defined as a disease of the reproductive system characterized by the failure of a couple to establish a clinical pregnancy after one year or more of regular unprotected sexual intercourse [28]. Like females, the males are more or less equal contributors to the infertility cases with a prevalence of 30–50% of all cases reported globally [29]. However, the prevalence varies according to the geographical regions as higher prevalence has been documented from Central and Eastern Europe, Africa, the Middle East, and South and Central Asia [1, 30]. Compromised fertility potential of the male may be attributed to multiple factors including anatomical abnormalities of the reproductive system, cryptorchidism, ejaculatory duct dysfunction, genetic and hormonal imbalance, varicocele, leukocytospermia, gonadal toxicity, environmental pollutants, male urogenital tract infections, and bacteriospermia, among others [9, 31]. Male urogenital infections are caused by microorganisms that include bacteria, virus, protozoa, and fungi. Among these, infections mediated by bacteria is the most prevalent one leading to the impairment of both sperm quality and function as well as seminal tract obstruction [32]. Both infection and inflammation can reduce spermatogenesis and deteriorate sperm quality and function [29] leading to an array of clinical conditions such as oligozoopspermia, asthenozoospermia, azoospermia, and dysfunction of male accessory glands [29]. Bacterial infection and inflammatory responses have been linked with poor male fertility potential; however, the exact mechanism remains inadequately understood. In case of chronic bacterial infection inflammatory responses may be asymptomatic but can still impose a long-lasting negative effect on sperm function, motility, count and spermatogenesis, and affect the permeability of the vas deferens and/or ejaculatory duct or may even induce apoptosis of spermatozoa [33,34,35].
According to the World Health Organization (WHO), bacteriospermia can be defined as the presence of more than 103 bacterial/ml of ejaculate and such condition is generally used as an indicator of active urogenital infection in men [36]. Bacteriospermia is associated with excessive generation of leukocytes in the male urogenital tract and concomitant OS. Moreover, bacteriospermia is a substantial cause of male infertility as it is associated with sperm DNA fragmentation, poor sperm motility and count, [37], genital tract dysfunction, deterioration of spermatogenesis [5], and poor assisted reproductive technology (ART) outcomes [38].
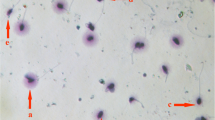
Sperm has the ability to recognize bacterial endotoxin, glycoprotein, and lipopolysaccharide by toll-like receptors (TLR-2 and TLR-4) expressed in the plasma membrane. Activated TLRs trigger local inflammatory response, create obstruction, and ultimately induce male infertility [39]. Inflammatory response also triggers excessive infiltration of leukocytes that may lead to the development of a clinical condition referred to as leukocytospermia. It is characterized by the presence of more than 1 × 106 leukocytes/ml of ejaculate [36]. Excess seminal leukocytes also trigger overproduction of ROS and introduce an imbalance between antioxidant and free radicals resulting in OS [40]. Elevated OS may cause significant biological and biochemical changes in the outer and inner mitochondrial membranes of sperm, which may in turn negatively affect sperm morphology, acrosome integrity and promote premature capacitation [37]. Moreover, excess ROS produced by leukocytes can stimulate LPO in polyunsaturated fatty acids of sperm membrane [41]. On the contrary, ROS has been linked directly to sperm agglutination, reduced sperm motility and increased DNA fragmentation, enhanced apoptosis in mature sperm, and increased risk of compromised male fertility [5] (Fig. 7.2).
Role of bacteriospermia in male infertility. Bacteriospermia initiates host immune response that concomitantly increases leukocytes in the male reproductive tract leading to production of reactive oxygen species (ROS) such as OH ̅ and H2O2, and proinflammatory cytokines. Some bacterial species also produce ROS leading to overproduction of ROS that cause sperm DNA damage, lipid peroxidation (LPO), and inhibits mitochondrial ATP production, which are in turn associated with reduction of sperm motility, inhibition of acrosome reaction ultimately contributing to male infertility
7.4 Bacteria-Associated Male Urogenital Infection
7.4.1 Urinary Tract Infection (UTI)
Urinary tract infections (UTIs) are considered as the most common bacterial infections in the urogenital tract of the male. Infection in the lower urinary tract is characterized by cystitis and in the upper urinary tract it is characterized by pyelonephritis where patients easily develop bacteremia. Cystitis is associated with dysuria and pollakisuria while pyelonephritis involves flank pain and fever along with the symptoms of cystitis [42]. In case of diabetic patients, stone-associated obstructed pyelonephritis is a major risk factor for fatal septic shock [43]. Common causal agents of UTIs include uropathogens such as E. coli, K. pneumoniae, Staphylococcus saprophyticus [44], Proteus mirabilis, and E. faecalis [45] (Table 7.1).
7.4.2 Male Accessory Gland Infection (MAGI)
Male accessory tract infection (MAGI) occurs due to the spreading of microorganisms via epididymis, deferent duct, prostate gland, seminal vesicles, testis, and urethra [42]. Epididymitis is considered as an inflammatory condition in epididymis, which is characterized by pain and acute unilateral or bilateral swelling of the scrotum and involvement of testicular inflammation along with epididymis, which is termed as epididymo-orchitis [46]. Bacterial epididymitis is commonly associated with low sperm count, stenosis in epididymal duct, and impairment in sperm function ultimately leading to male infertility. Occurrence of azoospermia is often associated with unclear unilateral epididymitis [47]. The most common bacteria involved in such infection are Chlamydia trachomatis, Escherichia coli, and Neisseria gonorrhoeae [48]. Prostatitis is another common urological inflammatory disease among men of all age groups and it affects sperm motility, count and morphology [47]. Typical features of prostatitis include voiding disturbances, sexual dysfunction, and chronic pelvic pain which are most prominent signs of prostate inflammation. Prostatitis is classified into four categories - i) chronic bacterial prostatitis, ii) acute bacterial prostatitis, iii) chronic prostatitis, and iv) asymptomatic inflammatory prostatitis [49]. The most common bacteria associated with prostatitis are Chlamydia trachomatis, Escherichia coli, Ureaplasma urealyticum, Nesisseria gonorrhea, and Klebsiella sp. [50]. On the contrary, urethritis is the inflammation of urethra and the most prevalent bacteria associated include Chlamydia trachomatis, Neisseria gonorrhoea, and Ureaplasma urealyticum [51]. Urethritis can be divided into two types i) non-gonococcal urethritis, and ii) gonococcal urethritis [52]. Urethritis is commonly associated with penile itching, dysuria, urethral discharge [53], and seminiferous tubular necrosis [54].
7.4.3 Sexually Transmitted Infection (STI)
Sexually transmitted infections (STIs)-mediated male infertility depends mainly on the local prevalence of sexually transmitted diseases (STDs). Prevalence of STDs are more prominent in Africa or South-East Asian regions compared to Western countries [55]. Most common bacteria associated in STIs include Chlamydia trachomatis, C. trachomatis, Chancroid haemophilus, Calymmatobacterium granulomatis, Neisseria gonorrhoea, Treponema pallidum, and Ureaplasma urealyticum [55]. Men with gonorrhoeic urethritis commonly develop urethral strictures and unilateral epididymo-orchitis [54].
7.5 Prevalence of Bacteriospermia-Associated Male Infertility
Approximately 48.5 million couple face the challenge of infertility globally after having unprotected intercourse for one year or long [56]. Approximately 15% of male infertility is linked with microorganisms-mediated UTIs [2]. Among the bacterial species responsible for bateriospermic condition in male, E. coli is the most prevalent and frequently isolated from the semen of infertile men accounting for 65–80% cases of male infertility [2]. E. coli is associated with the infection of the prostate, seminal vesicle, urethra, epididymis, and testis [37]. The second most prevalent bacterium is Chlamydia trachomatis, an obligate pathogen involved in 30–40% of urethritis cases [57]. According to WHO, C. trachomatis may cause up to 92 million urogenital tract infections per year [58]. U. urealyticum and Mycoplasma genitalium are other two bacterial species frequently present in bacteriospermic semen. U. urealyticum can contribute to 10–40% of all cases [59]. The two most common Mycoplasma species are M. hominis and M. genitalium that are responsible for 10.8% and 5% of all infection associated male infertility, respectively [60]. According to WHO, sexually transmitted infections caused by N. gonorrhoeae represented 106.1 million of cases globally which have been associated with epididymitis, urethritis, and prostatitis along with abnormal urethral discharge [61].
7.5.1 Escherichia Coli
The most common bacteria isolated from the semen of bacteriospermic male is E. coli, which possibly causes asexually transmitted epididymo-orchitis and is responsible for acute or chronic prostatitis leading to male infertility, too [2]. Semen analysis of 88 infertile male patients revealed the dominance of E. coli (10.22%) followed by Staphylococci (9.09%), Enterococci (5.88%), Staphylococcus aureus (2.27%), Gonococci (2.27%), and Klebsiella sp. (1.13%), [62].
Binding of E. coli with sperm leads to agglutination of sperm and induces damage in plasma membrane resulting in swelling of midpiece and tail invagination, which promote the rate of immobilization of sperm [63]. Interaction between E. coli and sperm is mediated by mannose binding receptors present on E. coli and mannose residues present on the sperm surface that can bind with type 1 fimbriae on E. coli [64]. An in vitro study confirmed that incubation of sperm with E. coli reduces the ability of sperm acrosomal reaction [65] and mitochondrial membrane potential [66]. Thereafter, Fraczek et al. 2012 [67] confirmed that binding of sperm with E. coli can alter sperm membrane stability and mitochondrial activity which increase the chances of male infertility. Lipopolysaccharide and porin protein of E. coli can produce cellular lysis in sperm and promote infection leading to temporary sterility [68].
7.5.2 Pseudomonas Aeruginosa
Infertility in men is frequently associated with uropathogenic microbes. Pseudomonas aeruginosa, a Gram-negative pathogenic bacterium is a possible cause of male infertility. 3-oxododecanoyl-L-homoserine lactone, a signaling molecule secreted from P. aeruginosa has been reported to possess detrimental effects on spermatozoa [69]. Incubation of sperm with P. aeruginosa has been shown to reduce sperm motility in a dose-dependent manner, and this bacterial signaling molecule acts on the acrosome of spermatozoa and promote premature acrosomal loss through a calcium dependent mechanism. P. aeruginosa infection can also lead to apoptosis and necrosis of sperm without affecting immune cells [69, 70]. A cytotoxic molecule, exotoxin A, released from P. aeruginosa induces chromosomal aberrations and sperm abnormalities including two heads, amorphous head, head without hook, banana head, coiled tail, and divided tail, which is believed to occur due to toxic effect of the protein on the sperm tail [70]. Porin, another protein secreted from the membrane of P. aeruginosa, is toxic to sperm and has been shown to induce apoptosis directly in the epithelial cell line of seminal vesicles of rats. Porin causes mitochondrial damage after binding with sperm and impairs sperm motility, too [71].
7.5.3 Chlamydia Trachomatis
Chlamydia trachomatis is an obligate intracellular Gram-negative bacterium [72]. It has species-specific lipopolysaccharide (LPS) antigen, other species-specific and immune-specific antigens as investigated through immunofluorescence. Its biphasic life cycle consists of an elementary and reticulate body [73]. This pathogen causes urethritis in the male and untreated infection of C. trachomatis in the male leads to epididymitis and prostatitis. Most of the time C. trachomatis infection remains asymptomatic in the male and may contribute up to 50% of infection [72]. Co-incubation of C. trachomatis with sperm promotes reduction of motile sperm and increases premature sperm death. LPS from C. trachomatis has also been shown to generate sperm apoptosis inducing molecules and can alter all other essential sperm parameters, too [74]. IgA Chlamydial antibodies promote LPO of sperm membrane which alter membrane fluidity, membrane-associated enzyme activities, capacitation, and acrosome reaction [75]. Furthermore, Chlamydial infection increases the level of interleukin (IL-8) in semen, which acts as a biomarker of MAGI [76]. C. trachomatis-induced infection also increases the rate of sperm DNA fragmentation and alters sperm morphology [77]. If the infection caused by the pathogen remains untreated it may cause long-term damage to organs of the male reproductive system such as the ejaculatory ducts, seminal vesicles, and spermatogonial cells [78].
7.5.4 Neisseria Gonorrhoeae
These Gram-negative, immotile diplococci cause the common UTI and develop gonorrhea which in turn alters testicular functions and promotes male infertility. This pathogen is responsible for about 86.9 million of gonorrhea cases globally [79]. Leukocytospermia is associated with gonorrhea which enhances the cytokines and ROS resulting in the impairment of spermatogenesis and sperm function [80]. Asymptomatic infection in the male with gonorrhea does not alter sperm count, semen volume, and sperm morphology but citric acid level drops in the male with gonorrhoea [81]. Movement of this pathogen is facilitated by the presence of pili on their surface that also help them cling onto other cells [80]. Bacterial pili type IV (T4P) and LPS can bind to sperm and asialoglycoprotein receptor on the sperm surface thereby facilitating the binding. Binding of N. gonorrhoeae LPS on the sperm cell surface receptor can also cause sperm cell death by inducing apoptosis [82].
7.5.5 Staphylococcus Aureus
The ubiquitous Gram-positive bacterium, Staphylococcus aureus is mostly found in the male genital tract. S. aureus infection has been associated with impairment of sperm motility and semen volume and increasing semen pH [83, 84]. Dominance of this pathogen in the semen of infertile patients has been confirmed with a prevalence of 68.2–75% in some cases [85, 86]. Incubation of S. aureus with sperm causes sperm agglutination and reduction of motility [87]. According to a recent report, 16% of infertile men may face the challenge of infertility due to S. aureus infection with abnormal semen fluid density, sperm abnormal morphology, and reduced sperm motility [88].
7.5.6 Ureaplasma sp.
The most prevalent species of the genus Ureplasma are U. urealyticum and U. parvum, and their prevalence in the semen of infertile men is 9% and 3%, respectively [89]. U. urealyticum is a main causative agent of prostatitis and epididymitis in the infertile male. U. urealyticum infection is also associated with low semen concentration and pH, and high seminal viscosity [90]. Infection reduces the level of seminal plasma alpha-glucosidase but not the levels of acid phosphatase and fructose in the seminal plasma [91]. U. urealyticum may also attach massively to sperm at the midpiece leading to looped tangling of tails and multiple agglutination thereby causing sperm immobility [92]. U. urealyticum infection increases seminal ROS level, too, thus causing LPO and sperm DNA fragmentation. It also reduces sperm fertilization capacity [93]. Metabolic products of U. urealyticum are able to generate ROS such as H2O2 and hydroxide anion (OH-) which are highly toxic to sperm. Furthermore, U. urealyticum infection decreases the amounts of essential microelements such as zinc and selenium, which are crucial for antioxidant defense mechanism of semen [93].
7.5.7 Mycoplasma sp.
Mycoplasma genitalium is another pathogen frequently isolated from the urogenital tract and is one of the potent causative organisms of urethritis in the male [94]. This bacterium has the ability to interact directly with the sperm and render them immobile [35]. The prevalence of M. genitalium has been reported between 19 and 41% in patients with urethritis [95]. Another species M. hominis has shown strong interaction with sperm parameters such as reduced motility, deformed morphology, and low count in infected men [96]. Also, M. genitalium has the capability to bind with the head, neck, and tail regions of the sperm and render sperm bulky thus reducing the capacity of travelling in the reproductive tract of the female [94].
7.5.8 Klebsiella Pneumoniae
The Gram-negative bacterium Klebsiella pneumoniae is another important causative organism of MAGI and are responsible for 2.3% of male infertility [97]. The pathophysiology of K. pneumoniae infection is not clearly understood due to the lack of evidence. However, K. pneumoniae infection impacts sperm parameters negatively and may also be a cause of necrozoospermia [10]. K. pneumoniae may impair male fertility by altering progressive motility, LPO, and apoptosis leading to sperm death [98].
7.6 Bacteriospermia and ROS-Mediated Damage
Human body has mainly three defense systems for protecting against invasion by foreign particles: i) tight junctions between skin epithelium, ii) innate immune response, and iii) adaptive immune response. Bacteria potentially infect the biological system through tissue barrier [100]. In the male, bacteria are considered responsible in 50% cases of prostatitis including 10% cases of chronic prostatitis [101]. Among infertile men, 11.6–45% cases occur due to urethral discharge as a marker of infection [59]. All bacterial inflammation associated with response to influx of leukocytes result in increase in ROS formation [102]. ROS are highly reactive chemical molecules including oxygen ions, peroxides, and hydrogen peroxide (H2O2), which contribute to male infertility by causing damage to sperm membrane and sperm DNA [103]. The huge amount of polyunsaturated fatty acids (PUFAs) present in the plasma membrane gives membrane fluidity to spermatozoa. The ROS directly attack the unconjugated double-bond groups of the PUFAs and generate a radical chain reaction pathway [104] resulting in the formation of 4-hydroxynonenal, malondialdehyde, and acrolein.
These reactive aldehydes undergo further reaction with hydrophilic amino acids in the protein which leads to mitochondrial dysfunction and leakage of further ROS from inner membrane of mitochondria [100, 105]. The direct damage of mitochondria through ROS decreases the energy availability which deteriorates the motility of sperm and alters normal sperm morphology and induce premature capacitation [102]. ROS directly attack the protamines-coated purine, pyrimidine bases and deoxyribose bases of sperm [106], which induce apoptosis of sperm cell and cause sperm death [107]. ROS also can induce apoptosis in sperm by altering the intercellular calcium ion concentration, which ultimately leads to infertility in the male [108]. In relation to higher level of ROS in semen, cytochrome c, and caspases 9 and 3 levels also increase simultaneously indicating apoptosis in the infertile male [109]. Bacteriospermia can also induce mitochondria-dependent apoptosis in sperm which increases the percentage of fragmented DNA in sperm and decreases mitochondrial transmembrane potential. These reports indicate negative alterations in sperm density, motility and morphology which ultimately contribute to male infertility [67]. Also, anti-bacterial IgA antibody forms in response to Chlamydial infection which is associated with increased ROS [75]. When the amount of ROS exceeds the antioxidant defense mechanism of semen, sperm membrane may undergo LPO and is associated with decreased flexibility of sperm and premature capacitation. Overproduction of free radicals negatively affects spermiogenesis and promotes the release of abnormal spermatozoa with excess cytoplasmic retention from the germinal epithelium. Enzymes of additional cytoplasm activate plasma membrane redox system and promote further production of ROS resulting in the loss of sperm motility and fertilizing capacity [110].
7.7 Management of Bacteriospermia in the Infertile Male
According to European Association of Urology (EAU) guidelines, a urine culture is the first step towards the detection of bacteria or any type of microorganism present in the male urogenital tract. Besides this, history of disease, symptoms check, and physical examination are carried out as a part of routine diagnosis. Additionally, the presence of leukocytes, erythrocytes, and nitrite are investigated for better evaluation [111]. Whereas according to WHO, semen analysis is of utmost importance to detect the MAGI [36]. Four-glass and two-glass tests can also be performed along with semen analysis for the diagnosis of localization of inflammation [46, 112]. Blood count including C-reactive protein (CRP), prostate-specific antigen (PSA), and hormone status (follicle stimulating hormone - FSH, luteinizing hormone-LH, and testosterone) are also recommended for the detection of acute urogenital inflammation [46]. In the case of acute cystitis, preliminary diagnosis can be done on the basis of clinical symptoms including lower abdominal pain [113] and newly developed dysuria, polyuria, and urinary urgency [114]. For the evaluation of acute cystitis, laboratory diagnosis include urine dipstick test and antibiotic susceptibility test by using cultured pathogens and microscopic analysis [115]. Urine culture test is performed for the diagnosis of acute pyelonephritis in the laboratory; however, sometimes blood culture can be done in cases of acute pyelonephritis [116, 117]. Bacteria- or any microorganism-mediated urinary tract obstruction can also be screened by computed tomography (CT), ultrasonography, and intravenous pyelography of kidney, bladder, and ureter [118]. Acute bacterial prostatitis is diagnosed on the basis of clinical symptoms such as heat around the prostate, soft and swollen state of prostate, frequent urination, painful urination, genital pain, chill, and joint pain along with fever [119].
For the initial management of bacteriospermia in the male, clinicians usually prefer two common guidelines - the American Urological Association (AUA) guideline and the European Association of Urology (EAU) guideline [120]. However, these are inadequate to provide the complete management strategy to treat bacteriospermia in the infertile male. Most of the times the chronic or acute bacterial infections are treated using a broad spectrum of antibiotics as an only effective medication against bacterial infections, without considering the partial effects of antibiotic therapy in the human body that may include nausea, bloating, vomiting, diarrhoea, abdominal ache, low appetite, and allergic surge. Additionally, high use of antibiotics increases the risk of bacterial resistance [121]. However, for management of bacteria mediated chronic urogenital infections and inflammations oral supplementation of ciprofloxacin, norfloxacin, ofloxacin are commonly recommended by clinicians [50]. Oral administration of either ciprofloxacin or fosfomycin and cefpodoxime proxetil, cefcapene pivoxil, cefdinir, nitrofurantoin, cefditoren pivoxil, cefixime, pivmecillinam and amoxicillin/clavulanate are prescribed for domestic cases of acute uncomplicated cystitis [119]. Whereas in case of complicated cystitis caused by Gram-negative rods and Gram-positive cocci, recommended antibacterial medications include LVFX (levofloxacin), CPFX (Ciprofloxacin Hydrochloride), TFLX (Tosufloxacin), STFX (Sitafloxacin), CVA/AMPC (Clavulanate/Amoxicillin), SBTPC (Sultamicillin), and sometimes CFDN (Cefdinir), CPDX-PR(cefpodoxime proxetil), and CFPN-PI (Cefcapene pivoxil hydrochloride) can also be used as alternative to antibiotic therapy [122]. Similarly, for the treatment of acute pyelonephritis supplementation of ciprofloxacin [123], levofloxacin [124], and trimethoprim/sulfamethoxazole are recommended [125]. In order to treat specific bacterial infection, medications can be of use after diagnosis. In the case of E. coli infection ciprofloxacin, amoxicillin, and aminoglycosides are the commonly used antibiotics [126]. In the case of N. gonorrhoeae and C. trachomatis infection tetracyclines form the most effective and widely prescribed antibiotics [111]. An initial intravenous administration of MINO for 3 to 5 days can be used to manage severe infections caused by C. trachomatis [122]. Plumbago zeylanica [127] and Piper lanceaefolium can be used as alternative or supplementary herbal medicine for infection of N. gonorrhoeae [128]. For the treatment of Klebsiella sp. mediated infection, empirical therapies include the use of trimethoprim-sulfamethoxazole and fluoroquinolones [129].Moreover, extract from the plant Aframomum melegueta has been used against Klebsiella sp. infection which may also be used as a supplementary or alternative medicine after proper toxicological evaluation [130]. A wide variety of African traditional herbs including Kigellia africana, Ballota africana, Carpobrotus edulis, and Pelargonium fasiculata are used in the management of K. pneumoniae infection [131]. In the case of Staphylococcus aureus infection, nafcillin [132], and imipenem have demonstrated more effective antibacterial medicine [133]. Nigerian traditional medical practitioners also recommend the use of medicinal plants such as Acalypha wilkesiana, Ageratum conyzoides, Bridella ferruginea, Ocimum gratissimum, Phylantus discoideus, and Terminalia avicennioides against S. aureus infection [134]. In Persian and European traditional medicines the fruit of Apium graveolens is used against uncomplicated urinary infection [135]. Current findings suggested that phthalide, an active compound isolated from show strong antiadhesive activity against the uropathogen E. coli [135]. Essential oils from Ocimum gratissimum, Salvia officinalis, and Cymbopogon citratus have the ability to neutralize the infections mediated by K. pneumoniae, E. coli, and Enterobacter sp. Similarly, chloroform, ethanol, methanol, and petroleum ether extract of Callistemon lanceolatus have been found effective in cases of S. aureus, E. faecalis, E. coli, and K. pneumoniae infection [136, 137]. Vaccinium macrocarpon popularly known as cranberry is considered one of the potent plant products that can inhibit bacterial attachment to the uroepithelial cells thus reducing bacterial load in the urogenital tract [138]. An in vitro study from India confirmed that aqueous, ethanolic and chloroform extracts of Hybanthus enneaspermus possess strong antibacterial activity against common uropathogens including E. coli, P. aeruginosa, K. pneumoniae, E. faecalis, and S. aureus [139]. Another potent candidate herb is Moringa oleifera that is used widely in the management of various human ailments and showed strong antibacterial action against E. coli, P. aeruginosa, and S. aureus infections [140]. One of the major mechanisms of bacteriospermia associated male fertility is through the production of ROS by bacteria directly or by initiating leukocytes response at the site of infection [5]. The potent herbal candidate that may be used in the management of OS-induced damages include Tribulus terrestris - a highly antioxidant rich herb that can neutralize ROS action and, also prevent membrane lipid peroxidation [141]. Similarly, a bioactive molecule thymol from Trachyspermum copticum also exerts strong antioxidant activity against ROS-induced OS [142]. Other potent herbs that can be utilized to minimize ROS-mediated damages to the male reproductive system are Cinnamomum verum [143], Terminalia chebula [144], Ocimum sanctum [145], Juniperus communis [146], and Taraxacum officinale [147].
The best advantage of herbal medicine over conventional antibiotic use is that the bacteria do not develop any sort of resistance against them. Also, medicinal herbs contain a wide range of bioactive molecules which are responsible for the medicinal property and synergistic effect [138]. However, further experiments are needed to validate the effectiveness and toxicity of the herbal medicines as well as the identification of specific bioactive compounds and their exact mechanism of action for future potential use in the clinical management of bacteriospermia.
7.8 Conclusions
Male infertility is a minacious global health threat that has not been clearly understood till date and more research is needed to perceive the underlying etiologies and proper management of the disease [148]. Bacteriospermia is one of the significant etiologies of male infertility that develops as a result of chronic or mild bacterial infection of the male urogenital tract. The mechanism of infection of bacteria varies from species to species, thus in order to develop better treatment approaches, identification of virulence determinants (that help bacteria in initial attachment and disease development including adhesin molecules, siderophores, and urease) is essential. This may also help develop vaccination for preventing bacterial infection in the male reproductive system [45]. Moreover, establishment of better prevention strategy for bacteriospermia may be achieved by switching towards the use of traditional herbal medicine as alternative or complementary medicine. Traditional herbs such as Acalypha wilkesiana, Ageratum conyzoides, Bridella ferruginea, Ocimum gratissimum, Phylantus discoideus, Terminalia avicennioides [134], and Aframomum melegueta have been used in the management of male UTIs particularly against common uropathogens that are responsible for bacteriospermia [130]. Similarly, bacteriospermia-mediated OS can be restrained by the use of antioxidant rich extract of Tribulus terrestris, Trachyspermum copticum, Cinnamomum verum, Terminalia chebula, Ocimum sanctum, Juniperus communis, and Taraxacum officinale. However, detailed toxicological studies of these herbs are needed prior to use either as an alternative or complementary medicine for effective clinical management of bacteriospermia.
References
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21(4):411–26.
Pellati D, Mylonakis I, Bertoloni G, Fiore C, Andrisani A, Ambrosini G, Armanini D. Genital tract infections and infertility. Eur J Obstetrics Gynecol Reproduct Biol. 2008;140(1):3–11.
Diemer T, Huwe P, Ludwig M, Hauck EW, Weidner W. Urogenital infection and sperm motility. Andrologia. 2003;35(5):283–7.
Andrada JA, Von der Walde FE, Andrada EC. Immunologic studies of male infertility. Immunol Ser. 1990;52:345–78.
Domes T, Lo KC, Grober ED, Mullen JB, Mazzulli T, Jarvi K. The incidence and effect of bacteriospermia and elevated seminal leukocytes on semen parameters. Fertil Steril. 2012;97(5):1050–5.
Sharma RK, Pasqualotto FF, Nelson DR, Agarwal A. Relationship between seminal white blood cell counts and oxidative stress in men treated at an infertility clinic. J Androl. 2001;22(4):575–83.
Keck C, Gerber-Schäfer C, Clad A, Wilhelm C, Breckwoldt M. Seminal tract infections: impact on male fertility and treatment options. Hum Reprod Update. 1998;4(6):891–903.
Askienazy-Elbhar M. Male genital tract infection: the point of view of the bacteriologist. Gynecol Obstetrique Fertilite. 2005;33(9):691–7.
Brunner RJ, Demeter JH, Sindhwani P. Review of guidelines for the evaluation and treatment of leukocytospermia in male infertility. World J Men’s health. 2019;37(2):128–37.
Vilvanathan S, Kandasamy B, Jayachandran AL, Sathiyanarayanan S, Tanjore Singaravelu V, Krishnamurthy V, Elangovan V. Bacteriospermia and its impact on basic semen parameters among infertile men. Interdiscip Perspect Infect Dis. 2016;6:2016.
Matousková I, Oborná I, Fingerová H, Kohnová I, Novotný J, Svobodová M, Brezinová J, Vyslouzilová J, Radová L. Bacteriospermia and the production of reactive oxygen species in the semen of males from infertile couples. Klinicka mikrobiologie a infekcni lekarstvi. 2009;15(6):192–5.
Tiwana MS, Leslie SW.: Anatomy, Abdomen and Pelvis, Testicle. (2017)
Agarwal A, Roychoudhury S, Bjugstad KB, Cho CL. Oxidation-reduction potential of semen: what is its role in the treatment of male infertility? Ther Adv Urol. 2016;8(5):302–18.
Gurung P, Yetiskul E Jialal I.: Physiology, male reproductive. (2020)
Barati E, Nikzad H, Karimian M. Oxidative stress and male infertility: current knowledge of pathophysiology and role of antioxidant therapy in disease management. Cell Mol Life Sci. 2020;77(1):93–113.
Kefer JC, Agarwal A, Sabanegh E. Role of antioxidants in the treatment of male infertility. Int J Urol. 2009;16(5):449–57.
Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reproduct Immunol. 2008;59:2–11. https://doi.org/10.1111/j.1600-0897.2007.00559.x.
Agarwal A, Tvrda E, Sharma R. Relationship amongst teratozoospermia, seminal oxidative stress and male infertility. Reproduct Biol Endocrinol. 2014;12(1):1–8. https://doi.org/10.1186/1477-7827-12-45.
Henkel RR. Leukocytes and oxidative stress: dilemma for sperm function and male fertility. Asian J Androl. 2011;13(1):43.
Dutta S, Majzoub A, Agarwal A. Oxidative stress and sperm function: a systematic review on evaluation and management. Arab J Urol. 2019;17(2):87–97.
Cocuzza M, Sikka SC, Athayde KS, Agarwal A. Clinical relevance of oxidative stress and sperm chromatin damage in male infertility: an evidence based analysis. Int Brazilian J Urol. 2007;33(5):603–21.
Ko EY Jr, Agarwal SS. Male infertility testing : reactive oxygen species and antioxidant capacity. Fertil Steril. 2014;102(6):1518–27. https://doi.org/10.1016/j.fertnstert.2014.10.020.
Rahiminia T. Etiologies of sperm oxidative stress. Iranian J Reproduct Med. 2016;14(4):231–40.
Ritchie C, Ko EY. Oxidative stress in the pathophysiology of male infertility. Andrologia. 2021;53(1):e13581.
Kumar DP, Sangeetha N. Mitochondrial DNA mutations and male infertility. Indian J Human Genet. 2009;15(3):93–7.
Kasperczyk MDS, Birkner SHDCE, Kasperczyk A.: Oxidative stress and motility impairment in the semen of fertile males, (2017), 1–8. https://doi.org/10.1111/and.12783.
Baskaran S, Finelli R, Agarwal A, Henkel R. Reactive oxygen species in male reproduction: a boon or a bane? Andrologia. 2021;53(1):e13577.
World Health Organization (WHO). International Classification of Diseases, 11th Revision (ICD-11) Geneva: WHO (2018)
Henkel R, Offor U, Fisher D. The role of infections and leukocytes in male infertility. Andrologia. 2020;53(1):e13743.
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356.
Dohle GR, Weidner W, Jungwirth A, Colpi G, Papp G, Pomerol J, Hargreave TB.: Guidelines on male infertility. European Association of Urology. (2004)
Moretti E, Capitani S, Figura N, Pammolli A, Federico MG, Giannerini V, Collodel G. The presence of bacteria species in semen and sperm quality. J Assist Reprod Genet. 2009;26(1):47–56.
Eley A, Pacey AA, Galdiero M, Galdiero M, Galdiero F. Can Chlamydia trachomatis directly damage your sperm? Lancet Infectious Dis. 2005;5(1):53–7.
Gimenes F, Souza RP, Bento JC, Teixeira JJ, Maria-Engler SS, Bonini MG, Consolaro ME. Male infertility: a public health issue caused by sexually transmitted pathogens. Nat Rev Urol. 2014;11(12):672–87.
Stojanov M, Baud D, Greub G, Vulliemoz N. Male infertility: the intracellular bacterial hypothesis. New Microbes New Infect. 2018;26:37–41.
World Health Organization. WHO laboratory manual for the examination and processing of human semen. (2010)
Farsimadan M, Motamedifar M. Bacterial infection of the male reproductive system causing infertility. J Reprod Immunol. 2020;3:103183.
Ghasemian F, Esmaeilnezhad S, Moghaddam MJ. Staphylococcus saprophyticus and Escherichia coli: tracking from sperm fertility potential to assisted reproductive outcomes. Clin Exp Reprod Med. 2021;48(2):142.
Fujita Y, Mihara T, Okazaki T, Shitanaka M, Kushino R, Ikeda C, Negishi H, Liu Z, Richards JS, Shimada M. Toll-like receptors (TLR) 2 and 4 on human sperm recognize bacterial endotoxins and mediate apoptosis. Hum Reprod. 2011;26(10):2799–806.
Iommiello VM, Albani E, Di Rosa A, Marras A, Menduni F, Morreale G, Levi SL, Pisano B, Levi-Setti PE. Ejaculate oxidative stress is related with sperm DNA fragmentation and round cells. Int J Endocrinol. 2015;2015
Parks JE, Lynch DV. Lipid composition and thermotropic phase behavior of boar, bull, stallion, and rooster sperm membranes. Cryobiology. 1992;29(2):255–66.
La Vignera S, Condorelli RA, Vicari E, Salmeri M, Morgia G, Favilla V, Cimino S, Calogero AE. Microbiological investigation in male infertility: a practical overview. J Med Microbiol. 2014;63(1):1–4.
Yamamichi F, Shigemura K, Kitagawa K, Fujisawa M. Comparison between non-septic and septic cases in stone-related obstructive acute pyelonephritis and risk factors for septic shock: a multi-center retrospective study. J Infect Chemother. 2018;24(11):902–6.
Hayami H, Takahashi S, Ishikawa K, Yasuda M, Yamamoto S, Wada K, Kobayashi K, Hamasuna R, Minamitani S, Matsumoto T, Kiyota H. Second nationwide surveillance of bacterial pathogens in patients with acute uncomplicated cystitis conducted by Japanese surveillance committee from 2015 to 2016: antimicrobial susceptibility of Escherichia coli, Klebsiella pneumoniae, and staphylococcus saprophyticus. J Infect Chemother. 2019;25(6):413–22.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–84.
Schuppe HC, Pilatz A, Hossain H, Diemer T, Wagenlehner F, Weidner W. Urogenital infection as a risk factor for male infertility. Dtsch Arztebl Int. 2017;114(19):339.
Weidner W, Colpi GM, Hargreave TB, Papp GK, Pomerol JM. EAU working group on male infertility. EAU guidelines on male infertility. Eur Urol. 2002;42(4):313–22.
Henkel R, Offor U, Fisher D. The role of infections and leukocytes in male infertility. Andrologia. 2021;53(1):e13743.
Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999;282(3):236–7.
Naber KG, Weidner W. Chronic prostatitis—an infectious disease? J Antimicrob Chemother. 2000;46(2):157–61.
Ness RB, Markovic N, Carlson CL, Coughlin MT. Do men become infertile after having sexually transmitted urethritis? An epidemiologic examination. Fertil Steril. 1997;68(2):205–13.
Horner PJ, Blee K, Falk L, van der Meijden W, Moi H. 2016 European guideline on the management of non-gonococcal urethritis. Int J STD AIDS. 2016;27(11):928–37.
Brill JR. Diagnosis and treatment of urethritis in men. Am Fam Physician. 2010;81(7):873–8.
Osegbe DN. Testicular function after unilateral bacterial epididymo-orchitis. Eur Urol. 1991;19:204–8.
Ochsendorf FR. Sexually transmitted infections: impact on male fertility. Andrologia. 2008;40(2):72–5.
Martinez G, Daniels K, Chandra A: Fertility of men and women aged 15–44 years in the United States: National Survey of family growth, 2006–2010. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; (2012)
Stamm WE. Chlamydia trachomatis infections: progress and problems. J Infect Dis. 1999;179(Supplement_2):S380–3.
World Health Organization. Global prevalence and incidence of selected curable sexually transmitted infections: overview and estimates. (2001)
Solomon M, Henkel R. Semen culture and the assessment of genitourinary tract infections. Indian J Urol: IJU: J Urol Soc India. 2017;33(3):188.
Gdoura R, Kchaou W, Chaari C, Znazen A, Keskes L, Rebai T, Hammami A. Ureaplasma urealyticum, Ureaplasma parvum, mycoplasma hominis and mycoplasma genitalium infections and semen quality of infertile men. BMC Infect Dis. 2007;7(1):1–9.
World Health Organization. Global incidence and prevalence of selected curable sexually transmitted infections-2008. (2012)
Golshani M, Taheri S, Eslami G, Soleymani RA, Falah F, Goudarzi H.: Genital tract infection in asymptomatic infertile men and its effect on semen quality (2006): 81–84.
Diemer T, Weidner W, Michelmann HW, SCHIEFER HG, Rovan E, Mayer F. Influence of Escherichia coli on motility parameters of human spermatozoa in vitro. Int J Androl. 1996;19(5):271–7.
Wolff H, Panhans A, Stolz W, Meurer M. Adherence of Escherichia coli to sperm: a mannose mediated phenomenon leading to agglutination of sperm and E. coli. Fertil Steril. 1993;60(1):154–8.
El-Mulla KF, Kohn FM, Dandal M, El Beheiry AH, Schiefer HG, Weidner W, Schill WB. In vitro effect of Escherichia coli on human sperm acrosome reaction. Arch Androl. 1996;37(2):73–8.
Schulz M, Sánchez R, Soto L, Risopatrón J, Villegas J. Effect of Escherichia coli and its soluble factors on mitochondrial membrane potential, phosphatidylserine translocation, viability, and motility of human spermatozoa. Fertil Steril. 2010;94(2):619–23.
Fraczek M, Piasecka M, Gaczarzewicz D, Szumala-Kakol A, Kazienko A, Lenart S, Laszczynska M, Kurpisz M. Membrane stability and mitochondrial activity of human-ejaculated spermatozoa during in vitro experimental infection with E scherichia coli, S taphylococcus haemolyticus and B acteroides ureolyticus. Andrologia. 2012;44(5):315–29.
Galdiero F, Gorga F, Bentivoglio C, Mancuso R, Galdiero E, Tufano MA. The action of LPS porins and peptidoglycan fragments on human spermatozoa. Infection. 1988;16(6):349–53.
Rennemeier C, Frambach T, Hennicke F, Dietl J, Staib P. Microbial quorum-sensing molecules induce acrosome loss and cell death in human spermatozoa. Infect Immun. 2009;77(11):4990–7.
Altaee MF, Nafee SK, Hamza SJ. Evaluation for the cytotoxic effect of exotoxin a produced by Pseudomonas aeruginosa on mice by using cytogenetic parameters. Curr Microbiol. 2013;1:257–61.
Buommino E, Morelli F, Metafora S, Rossano F, Perfetto B, Baroni A, Tufano MA. Porin from Pseudomonas aeruginosa induces apoptosis in an epithelial cell line derived from rat seminal vesicles. Infect Immun. 1999;67(9):4794–800.
Malhotra M, Sood S, Mukherjee A, Muralidhar S, Bala M. Genital chlamydia trachomatis: an update. Indian J Med Res. 2013;138(3):303.
Saka HA, Thompson JW, Chen YS, Kumar Y, Dubois LG, Moseley MA, Valdivia RH. Quantitative proteomics reveals metabolic and pathogenic properties of chlamydia trachomatis developmental forms. Mol Microbiol. 2011;82(5):1185–203.
Eley A, Hosseinzadeh S, Hakimi H, Geary I, Pacey AA. Apoptosis of ejaculated human sperm is induced by co-incubation with Chlamydia trachomatis lipopolysaccharide. Human Reproduct. 2005;20(9):2601–7.
Segnini A, Camejo MI, Proverbio F. Chlamydia trachomatis and sperm lipid peroxidation in infertile men. Asian J Androl. 2003;5(1):47–50.
Kokab A, Akhondi MM, Sadeghi MR, Modarresi MH, Aarabi M, Jennings R, Pacey AA, Eley A. Raised inflammatory markers in semen from men with asymptomatic chlamydial infection. J Androl. 2010;31(2):114–20.
Gallegos G, Ramos B, Santiso R, Goyanes V, Gosálvez J, Fernández JL. Sperm DNA fragmentation in infertile men with genitourinary infection by chlamydia trachomatis and mycoplasma. Fertil Steril. 2008;90(2):328–34.
Jiminez G, Villanveva Diaz CA. Epididymal stereocilia in semen of infertile men: evidence of chronic epididymitis? Int J Androl. 2006;38:26–30.
Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, Chico RM, Smolak A, Newman L, Gottlieb S, Thwin SS. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548.
Krause W. Male accessory gland infection. Andrologia. 2008;40(2):113–6.
Pérez-Plaza M, Padrón RS, Más J, Peralta H. Semen analyses in men with asymptomatic genital gonorrhoea. Int J Androl. 1982;5(1):6–10.
Harvey HA, Jennings MP, Campbell CA, Williams R, Apicella MA. Receptor-mediated endocytosis of Neisseria gonorrhoeae into primary human urethral epithelial cells: the role of the asialoglycoprotein receptor. Mol Microbiol. 2001;42(3):659–72.
Onemu SO, Ibeh IN. Studies on the significance of positive bacterial semen cultures in male fertility in Nigeria. Int J Fertil Womens Med. 2001;46(4):210–4.
Marconi M, Pilatz A, Wagenlehner F, Diemer T, Weidner W. Impact of infection on the secretory capacity of the male accessory glands. Int Braz J Urol. 2009;35(3):299–309.
Emokpae MA, Uadia PO, Sadiq NM. Contribution of bacterial infection to male infertility in Nigerians. Online J Health Allied Sci. 2009;8(1)
Momoh AR, Idonije BO, Nwoke EO, Osifo UC, Okhai O, Omoroguiwa A, Momoh AA. Pathogenic bacteria-a probable cause of primary infertility among couples in Ekpoma. J Microbiol Biotechnol Res. 2011;1(3):66–71.
Kaur S, Prabha V, Shukla G, Sarwal A. Interference of human spermatozoal motility by live Staphylococcus aureus. Am J Biomed Sci. 2010;2(1):91–7.
Esmailkhani A, Akhi MT, Sadeghi J, Niknafs B, Bialvaei AZ, Farzadi L, Safadel N. Assessing the prevalence of Staphylococcus aureus in infertile male patients in Tabriz, Northwest Iran. Int J Reproduct BioMed. 2018 Jul;16(7):469.
Zeighami H, Peerayeh SN, Yazdi RS, Sorouri R. Prevalence of Ureaplasma urealyticum and Ureaplasma parvum in semen of infertile and healthy men. Int J STD AIDS. 2009;20(6):387–90.
Wang Y, Liang CL, Wu JQ, Xu C, Qin SX, Gao ES. Do Ureaplasma urealyticum infections in the genital tract affect semen quality? Asian J Androl. 2006;8(5):562–8.
Zheng J, Yu SY, Jia DS, Yao B, Ge YF, Shang XJ, Huang YF. Ureaplasma urealyticum infection in the genital tract reduces seminal quality in infertile men. Zhonghua nan ke xue=. Natl J Androl. 2008;14(6):507–12.
Abdel Razzak AA, Bakr SS. Role of mycoplasma in male infertility. EMHJ-Eastern Mediterranean Health J. 2000;6(1):149–55.
Potts JM, Sharma R, Pasqualotto F, Nelson D, Hall G, Agarwal A. Association of Ureaplasma urealyticum with abnormal reactive oxygen species levels and absence of leukocytospermia. J Urol. 2000;163(6):1775–8.
Svenstrup HF, Fedder J, Abraham-Peskir J, Birkelund S, Christiansen G. Mycoplasma genitalium attaches to human spermatozoa. Hum Reprod. 2003;18:2103–9.
Wikstrom A, Jensen JS. Mycoplasma genitalium: a common cause of persistent urethritis among men treated with doxycycline. Sex Transm Infect. 2006;82:276–9.
Ahmadi MH, Mirsalehian A, Sadighi Gilani MA, Bahador A, Talebi M. Asymptomatic infection with mycoplasma hominis negatively affects semen parameters and leads to male infertility as confirmed by improved semen parameters after antibiotic treatment. Urology. 2017;100:97–102.
Ibadin OK, Ibeh IN. Bacteriospermia and sperm quality in infertile male patient at University of Benin Teaching Hospital, Benin City, Nigeria. Malaysian J Microbiol. 2008;4(2):65–7.
Zuleta-González MC, Zapata-Salazar ME, Guerrero-Hurtado LS, Puerta-Suárez J, Cardona-Maya WD. Klebsiella pneumoniae and Streptococcus agalactiae: passengers in the sperm travel. Archivos espanoles de Urolgia. 2019;72(9):939–47.
Prabha V, Sandhu R, Kaur S, Kaur K, Sarwal A, Mavuduru RS, Singh SK. Mechanism of sperm immobilization by Escherichia coli. Adv Urol. 2010;30:2010.
Agarwal A, Rana M, Qiu E, AlBunni H, Bui AD, Henkel R. Role of oxidative stress, infection and inflammation in male infertility. Andrologia. 2018;50(11):e13126.
Schaefler AJ. Epidemiology and demographics of prostatitis. Andrologia. 2003;35(5):252–7.
Tremellen K. Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update. 2008;14(3):243–58.
Cheeseman KH, Slater TF. An introduction to free radical biochemistry. Br Med Bull. 1993;49(3):481–93.
Aitken RJ. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol Reprod Dev. 2017;84(10):1039–52.
Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003;79(4):829–43.
Oliva R. Protamines and male infertility. Hum Reprod Update. 2006;12(4):417–35.
Moustafa MH, Sharma RK, Thornton J, Mascha E, Abdel-Hafez MA, Thomas AJ, Agarwal A. Relationship between ROS production, apoptosis and DNA denaturation in spermatozoa from patients examined for infertility. Hum Reprod. 2004;19(1):129–38.
Ha HK, Park HJ, Park NC. Expression of E-cadherin and α-catenin in a varicocele-induced infertility rat model. Asian J Androl. 2011;13(3):470.
Sanocka D, Kurpisz M. Reactive oxygen species and sperm cells. Reprod Biol Endocrinol. 2004;2(1):1–7.
Aitken RJ, Sawyer D. The human spermatozoon—not waving but drowning. Adv Male Mediated Dev Toxicity. 2003:85–98.
Grabe M, Bjerklund-Johansen TE, Botto H, Çek M, Naber KG, Tenke P, Wagenlehner F. Guidelines on urological infections. Eur Assoc Urol. 2015;182:237–57.
Wagenlehner FME, Naber KG, Bschleipfer T, Brähler E, Weidner W. Prostatitis and male pelvic pain syndrome: diagnosis and treatment. Dtsch Arztebl Int. 2009;106:175–83.
Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin. 2014;28(1):75–89.
Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287(20):2701–10.
Rubin RH, Shapiro ED, Andriole VT, Davis RJ, Stamm WE. Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Clin Infect Dis. 1992;15(Supplement_1):S216–27.
Hooton TM. Uncomplicated urinary tract infection. N Engl J Med. 2012;366(11):1028–37.
Lee HN, Yoon H. Management of antibiotic-resistant acute pyelonephritis. Urogenital Tract Infect. 2017;12(3):95–102.
Roy C, Pfleger DD, Tuchmann CM, Lang HH, Saussine CC, Jacqmin D. Emphysematous pyelitis: findings in five patients. Radiology. 2001;218(3):647–50.
Kang CI, Kim J, Park DW, Kim BN, Ha US, Lee SJ, Yeo JK, Min SK, Lee H, Wie SH. Clinical practice guidelines for the antibiotic treatment of community-acquired urinary tract infections. Infect Chemotherapy. 2018;50(1):67–100.
Trost LW, Nehra A. Guideline-based management of male infertility: why do we need it? Indian J Urol: IJU: J Urol Soc India. 2011;27(1):49.
Mohsen S, Dickinson JA, Somayaji R. Update on the adverse effects of antimicrobial therapies in community practice. Can Fam Physician. 2020;66(9):651–9.
Yamamoto S, Ishikawa K, Hayami H, Nakamura T, Miyairi I, Hoshino T, Hasui M, Tanaka K, Kiyota H, Arakawa S. JAID/JSC guidelines for clinical management of infectious disease 2015− urinary tract infection/male genital infection. J Infect Chemother. 2017;23(11):733–51.
Talan DA, Klimberg IW, Nicolle LE, Song J, Kowalsky SF, Church DA. Once daily, extended release ciprofloxacin for complicated urinary tract infections and acute uncomplicated pyelonephritis. J Urol. 2004;171(2):734–9.
Klausner HA, Brown P, Peterson J, Kaul S, Khashab M, Fisher AC, Kahn JB. A trial of levofloxacin 750 mg once daily for 5 days versus ciprofloxacin 400 mg and/or 500 mg twice daily for 10 days in the treatment of acute pyelonephritis. Curr Med Res Opin. 2007;23(11):2637–45.
Talan DA, Stamm WE, Hooton TM, Moran GJ, Burke T, Iravani A, Reuning-Scherer J, Church DA. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA. 2000;283(12):1583–90.
Adamus-Białek W, Wawszczak M, Arabski M, Majchrzak M, Gulba M, Jarych D, Parniewski P, Głuszek S. Ciprofloxacin, amoxicillin, and aminoglycosides stimulate genetic and phenotypic changes in uropathogenic Escherichia coli strains. Virulence. 2019;10(1):260–76.
Gundidza M, Manwa G. Activity of chloroform extract from Plumbago zeylanica against Neisseria gonorrhoeae. Fitoterapia. 1990;61(1):47–9.
Ruddock PS, Charland M, Ramirez S, López A, Towers GN, Arnason JT, Liao M, Dillon JA. Antimicrobial activity of flavonoids from Piper lanceaefolium and other Colombian medicinal plants against antibiotic susceptible and resistant strains of Neisseria gonorrhoeae. Sex Transm Dis. 2011;38(2):82–8.
Bouza E, Cercenado E: Klebsiella and enterobacter: antibiotic resistance and treatment implications. InSeminars in respiratory infections 2002; (Vol. 17, No. 3, pp. 215–230).
Doherty VF, Olaniran OO, Kanife UC. Antimicrobial activities of Aframomum melegueta (Alligator pepper). Int J Biol. 2010;2(2):126–31.
Cock IE, Van Vuuren SF. The potential of selected South African plants with anti-Klebsiella activity for the treatment and prevention of ankylosing spondylitis. Inflammopharmacology. 2015;23(1):21–35.
Chang FY, Peacock JE Jr, Musher DM, Triplett P, MacDonald BB, Mylotte JM, O’Donnell A, Wagener MM, Victor LY. Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study. Medicine. 2003;82(5):333–9.
Isaiah IN, Nche BT, Nwagu IG, Nnanna II. Current studies on bacterospermia the leading cause of male infertility: a protégé and potential threat towards mans extinction. N Am J Med Sci. 2011;3(12):562.
Akinyemi KO, Oladapo O, Okwara CE, Ibe CC, Fasure KA. Screening of crude extracts of six medicinal plants used in South-West Nigerian unorthodox medicine for anti-methicillin resistant Staphylococcus aureus activity. BMC Complement Altern Med. 2005;5(1):1–7.
Grube K, Spiegler V, Hensel A. Antiadhesive phthalides from Apium graveolens fruits against uropathogenic E. coli. J Ethnopharmacol. 2019;237:300–6. system. StatPearls
Noormandi A, Dabaghzadeh F. Effects of green tea on Escherichia coli as a uropathogen. J Tradit Complement Med. 2015;5(1):15–20.
Das S. Natural therapeutics for urinary tract infections—a review. Future J Pharm Sci. 2020;6(1):1–13.
Shaheen G, Akram M, Jabeen F, Ali Shah SM, Munir N, Daniyal M, Riaz M, Tahir IM, Ghauri AO, Sultana S, Zainab R. Therapeutic potential of medicinal plants for the management of urinary tract infection: a systematic review. Clin Exp Pharmacol Physiol. 2019;46(7):613–24.
Sahoo S, Kar DM, Mohapatra S, Rout SP, Dash SK. Antibacterial activity of Hybanthus enneaspermus against selected urinary tract pathogens. Indian J Pharm Sci. 2006;68(5)
Amabye TG, Tadesse FM. Phytochemical and antibacterial activity of moringa oleifera available in the market of Mekelle. J Analyt Pharm Res. 2016;2(1):1–4.
Zheleva-Dimitrova D, Obreshkova D, Nedialkov P. Antioxidant activity of tribulus terrestris—a natural product in infertility therapy. Int J Pharm Pharm Sci. 2012;4(4):508–11.
Nickavar B, Adeli A, Nickavar A. TLC-bioautography and GC-MS analyses for detection and identification of antioxidant constituents of Trachyspermum copticum essential oil. Iranian J Pharm Res: IJPR. 2014;13(1):127.
Mathew S, Abraham TE. In vitro antioxidant activity and scavenging effects of Cinnamomum verum leaf extract assayed by different methodologies. Food Chem Toxicol. 2006;44(2):198–206.
Saha S, Verma RJ. Antioxidant activity of polyphenolic extract of Terminalia chebula Retzius fruits. J Taibah Univ Sci. 2016;10(6):805–12.
Hakkim FL, Shankar CG, Girija S. Chemical composition and antioxidant property of holy basil (Ocimum sanctum L.) leaves, stems, and inflorescence and their in vitro callus cultures. J Agric Food Chem. 2007;55(22):9109–17.
Elmastaş M, Gülçin İ, Beydemir Ş, İrfan Küfrevioğlu Ö, Aboul-Enein HY. A study on the in vitro antioxidant activity of juniper (Juniperus communis L.) fruit extracts. Anal Lett. 2006;39(1):47–65.
Ghaima KK, Hashim NM, Ali SA. Antibacterial and antioxidant activities of ethyl acetate extract of nettle (Urtica dioica) and dandelion (Taraxacum officinale). J Appl Pharm Sci. 2013;3(5):96.
Kumar N, Singh AK. Trends of male factor infertility, an important cause of infertility: a review of literature. J Human Reproduct Sci. 2015 Oct;8(4):191.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Das, S. et al. (2022). Bacteriospermia and Male Infertility: Role of Oxidative Stress. In: Kesari, K.K., Roychoudhury, S. (eds) Oxidative Stress and Toxicity in Reproductive Biology and Medicine. Advances in Experimental Medicine and Biology, vol 1358. Springer, Cham. https://doi.org/10.1007/978-3-030-89340-8_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-89340-8_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-89339-2
Online ISBN: 978-3-030-89340-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)