Abstract
The effective treatment of brain tumors is a considerable challenge in part due to the presence of the blood-brain barrier (BBB) that limits drug delivery. Multiple hurdles pose challenges in identifying drugs that may be effective in treating brain tumors, including limited central nervous system (CNS) distribution of therapeutics, heterogeneous disruption of the blood-brain barrier in the regions of the tumor that lead to heterogenous drug distribution within the tumor, and genetic heterogeneity of tumor drivers. This chapter discusses the current standard of care and its limitations, as well as complex challenges in the treatment of primary and metastatic brain tumors. We review a variety of prospective delivery solutions of therapeutics to the brain and CNS for the treatment of brain tumors that will in the future lead to opening new doors for more effective treatments.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Blood-tumor barrier
- Glioblastoma
- Active transporters
- Receptor mediated transport
- Antibody drug conjugates
- Immunotherapy
1 Tumors of the CNS: The Disease
More than 23,500 new cases of primary brain and CNS tumors are expected in the United States in 2020, which will account for approximately 1.3% of overall cancer cases and represent the 10th leading cause of death for men and women (Siegel et al. 2019). In addition, an estimated 10%–20% of all cancer patients will develop brain metastases (Lin and DeAngelis 2015). In the United States, an estimated 98,000–170,000 cases of brain metastases occur each year (Amsbaugh and Kim 2019). Although brain and CNS tumors are a rare occurrence in adults, they are a significant cause of mortality and are the most common solid tumors in infants and children (McNeill 2016). Brain tumors are broadly classified into two types based on their site of origin—primary brain tumors and secondary/metastatic brain tumors. Primary brain tumors are those that originate within the brain or the surrounding areas of the CNS like the meninges or spinal cord. Conversely, secondary or metastatic tumors are those that originate elsewhere in the body and later spread to the brain. Diagnosis of brain malignancies and their treatment are often very complex and are associated with serious cognitive and functional impairment of patients and psychological stress to the patients as well as their families. These tumors have a grim prognosis with a median survival ranging between 4 and 15 months after diagnosis (Parrish et al. 2015; Pan-Weisz et al. 2019). Many experimental therapies that have shown promise in preclinical studies ultimately fail clinical trials for CNS tumors, and therefore the incidences of primary and metastatic brain tumors continue to rise. Most of the drugs in the pipeline do not cross the formidable hurdle of the blood-brain barrier (BBB) to be effectively delivered to the tumor site. Therefore, it is imperative to develop therapies that take into consideration the presence of an intact BBB in the invasive regions surrounding the tumor which continue to grow even after surgical resection (Sarkaria et al. 2018). Advancements should also be made to develop novel drug delivery systems exploiting various aspects of BBB anatomy and physiology in and around the tumor. Moreover, it will be necessary to better understand the complex cellular signaling pathways that lead to tumor proliferation and invasiveness. Finally, novel technologies may be utilized to modify the BBB to deliver therapeutics across CNS barriers to the tumor site. In this chapter, we will discuss the challenges to effective treatment for both primary and metastatic brain tumors.
1.1 Primary Brain Tumors
Primary brain tumors can be classified as malignant or nonmalignant based on the presence of proliferative and invasive cancer cells within the tumor. The five-year survival rate in adults following the diagnosis of a malignant brain or other CNS tumor is 35.8%; in contrast, the five-year survival rate following diagnosis of a nonmalignant brain or other CNS tumor is 91.5%, based on the Central Brain Tumor Registry of the United States (CBTRUS) report compiling cases from 2012 to 2016 (Ostrom et al. 2019). The most common CNS tumors in children are pilocytic astrocytoma, embryonal tumors, and malignant gliomas, whereas meningiomas, pituitary tumors, and malignant gliomas are the most common brain tumor types in adults (McNeill 2016).
Gliomas are primary brain tumors that are thought to originate from neuroglial stem cells or progenitor cells. On the basis of their histological appearance, they have been traditionally classified as astrocytic, oligodendroglial, or ependymal tumors and assigned WHO grades I-IV, indicating different degrees of malignancy based on genomic, transcriptomic, and epigenetic profiling (Weller et al. 2015). These tumors vary widely in histology from benign and potentially surgically curable grade I tumors (pilocytic astrocytoma) to locally aggressive infiltrative grade IV tumors with a high risk of recurrence (glioblastoma). Survival varies by histology, with pilocytic astrocytoma having a 10-year survival of greater than 90%, whereas only about 5% of patients with glioblastoma survive up to 5 years (McNeill 2016).
Glioblastoma (GBM) is the most common primary malignant brain tumor with ~14,000 new cases per year in the United States with a 2-year survival rate of 16.9% (Ostrom et al. 2014). Currently, the United States has approximately 50,000 GBM patients. In other developed countries worldwide, approximately 3.5 GBM cases per 100,000 people are newly diagnosed each year (Porter et al. 2010). According to the World Health Organization classification system, GBMs are grade IV neoplasms (where grade I refers to the least severe and grade IV to the most severe), reflecting their highly malignant behavior (Perkins and Liu 2016). GBMs are highly infiltrative and therefore not a surgically curable disease. Tumor cells invade the surrounding brain regions and have a diffused nature making complete surgical resection impossible (Cloughesy et al. 2014; Sarkaria et al. 2018).
1.2 Metastatic Brain Tumors
Cancer metastasis from primary tumors to the brain is a significant concern in cancer patient management (Sperduto et al. 2012). Brain metastases are difficult to detect and diagnose, especially in early stages of the disease and have an extremely grim prognosis (Bruzzone et al. 2012). Lung cancer, breast cancer, melanoma, renal cell carcinoma, and colorectal cancer are among the tumor types associated with high brain-metastatic prevalence (Achrol et al. 2019). While lung cancer has been reported to have the largest incidence rate of brain metastases, melanoma has the highest likelihood of metastasizing to the brain (Nayak et al. 2012). Rising incidences of brain metastases can be attributed to the improvement of advanced imaging techniques for early detection as well as effective systemic treatment of the peripheral disease that extends patient survival (Fokas et al. 2013). Another reason for limited success in the therapies for brain metastases is the restricted entry of systemically active therapeutic agents into the brain because of the BBB. The BBB creates a pharmacological sanctuary that allows the growth and development of the tumor cells within the brain (Kim et al. 2018). The mechanisms by which brain metastases occur have not been well described; however, the prevalence of these metastases for a variable duration before being detected poses a treatment challenge. In addition, after the initial detection of brain metastases, there is a high likelihood of undetected “micrometastases” that will be protected by a relatively intact BBB at those locations within the brain (Oberoi et al. 2016). Therefore, to advance treatments for brain metastases, consideration of the condition of the BBB in these regions is essential, especially in the non-contrast enhancing regions of the micrometastases where the BBB can impede the delivery of anticancer agents to the tumor cells.
2 Standard of Care for Primary Brain Tumors
The current standard of care for primary brain tumors reflects the need to develop more effective treatments that have improved delivery to the tumor target sites. Clinical signs and symptoms of primary brain tumors progress from early symptoms like headaches and seizures due to increased intracranial pressure to more focal symptoms like dizziness and change in personality traits as the tumor grows in size and infiltrates to different areas of the brain (Perkins and Liu 2016). The diagnosis of these tumors is done with the help of gadolinium enhanced magnetic resonance imaging (MRI) or computed tomography (CT). Advanced imaging techniques combined with MRI significantly help in the diagnosis of tumor subtype. Treatment decisions are individualized by an experienced multidisciplinary team consisting of medical oncology, radiation oncology, and neurosurgery. Treatment decisions are based on tumor type and location, malignancy potential, and the patient’s age and physical condition. Treatment options include a combination of surgery, chemotherapy, and radiation therapies (Alifieris and Trafalis 2015).
The current standardized treatment for GBM involves a multidisciplinary approach with maximal safe surgical resection possible, followed by concurrent radiation with temozolomide (TMZ), an oral DNA alkylating agent, followed by adjuvant chemotherapy with TMZ (McClelland et al. 2018). Following surgical resection, the chemoradiation schedule begins 4 weeks after the patient’s recovery from the surgery. Radiation using three-dimensional conformal beam or intensity-modulated radiotherapy (RT) is now the standard of care, where typical total dose delivered is 60 Gray (Gy), in 1.8–2 Gy fractions administered 5 days per week for 6 weeks (J.G. et al., 2011). A clear survival advantage has been demonstrated with postoperative RT doses to 60 Gy, but dose escalation beyond this has resulted in increased toxicity without additional survival benefits (Barani and Larson 2015). Concurrent with RT, TMZ is typically given at a dose of 75 mg/m2 daily for 6 weeks, followed by a rest period of about one month after RT is completed. When restarted, TMZ is dosed at 150 mg/m2 daily for 5 days for the first month (usually days 1–5 of 28). If tolerated, the dose is escalated up to 200 mg/m2 for five consecutive days per month for the rest of the treatment period (Davis 2016). The importance of the methylation of the O6-methylguanine DNA methyltransferase (MGMT) gene in standard GBM therapy has been demonstrated by Stupp et al. in 2008. MGMT codes for an enzyme involved with DNA repair. Patients who have methylated (not activated) MGMT exhibit compromised DNA repair. When the MGMT enzyme is activated, it can interfere with the effects of treatment. RT and alkylating chemotherapy exert their therapeutic effects by causing DNA damage and cytotoxicity and triggering apoptosis. Therefore, the expression of methylated MGMT is beneficial for patients undergoing TMZ chemotherapy and RT (Stupp et al. 2008). As one can see from above, the standard of care comprised of radiation and TMZ represents a limited choice of therapy even in light of our improved knowledge of the biology of GBM. It is important to note that radiation is a highly brain penetrant therapy and TMZ, a small molecule alkylating agent, also has comparatively good brain penetration (Portnow et al. 2009).
In addition, a humanized monoclonal antibody, bevacizumab, targeting vascular endothelial growth factor (VEGF) has been approved for the treatment of recurrent GBM, but it has not shown any improvement in the overall survival of patients (Chowdhary and Chamberlain 2013). In 2015, the FDA approved another local treatment option called Optune for newly diagnosed and recurrent GBM with concomitant TMZ. Optune is a device delivering electrical fields to the brain. It emits low intensity electricity (100–300 kHz frequency) delivered through a series of transducer arrays placed regionally around the tumor region. These electrical fields have been shown to selectively disrupt cell division in the case of brain tumors. Patients with a 90% or greater compliance rate of using Optune had a median overall survival of 24.9 months (28.7 months from diagnosis) and a 5-year survival rate of 29.3% (Toms et al. 2019). Again, similar to the above standard of care, this treatment option clearly has excellent BBB penetration.
3 Standard of Care for Metastatic Brain Tumors
Approximately 80% of brain metastases are localized in the cerebral hemispheres (Delattre et al. 1988). Initial symptoms range from seizures and headaches to cognitive dysfunction and neurological deficits; however in some early stages, asymptomatic brain metastases are also commonly found using imaging techniques (Kim et al. 2018). Clinical treatment in most cases is mostly palliative and rarely ever curative. The prognosis and treatment modalities are affected by a variety of factors, including size, number, and location of metastases; age and performance status of the patient; type of the tumor; and active extracranial disease presence (Arvanitis et al. 2018). Given the prevalence and grim prognosis of metastatic tumors in the brain, there is a great unmet need in improving specific treatments that will require adequate penetration across the BBB.
Treatment of brain metastases closely mirrors the treatment of primary brain tumors (Fig. 24.1). Stereotactic radiosurgery or gamma knife radiation can be used as the first option for the maximum safe surgical resection where there are few (typically <4) metastases present (Oberoi et al. 2016; Stupp 2019). In many cases, due to the size, number, or location of the tumor, surgery is not possible, and hence patients are treated with whole brain radiation therapy (WBRT). TMZ is the first-line chemotherapeutic used for GBM; however, no such proven chemotherapeutic options have been specifically effective in brain metastases (Oberoi et al. 2016). CNS metastases often express similar characteristics and sensitivities to their primary tumors and hence are treated based on their subtype and primary source of origin (Rick et al. 2019). The use of molecularly targeted agents has been on the rise in the case of non-small cell lung carcinoma (NSLC) metastases over the last 15 years in cases with evidence of drug sensitivity for specific tumor mutations (Lim et al. 2019). The use of epidermal growth factor receptor tyrosine kinase (EGFR-TKI) inhibitors gefitinib, erlotinib, and more recently the effective use of a third-generation EGFR-TKI inhibitor, osimertinib, on EGFR-mutated NSLC brain metastases are examples of such therapy (Dempke et al. 2015; Reungwetwattana et al. 2018; Soria et al. 2018; Ramalingam et al. 2020). In anaplastic lymphoma kinase (ALK) fusion protein-positive NSLC metastases, which are rare, two inhibitors—crizotinib and alectinib—have demonstrated treatment benefit (Shaw et al. 2017; Tran and Klempner 2017; Gadgeel et al. 2018). Importantly, an ALK inhibitor, lorlatinib, a molecule designed for improved BBB penetration through decreased efflux liability, showed substantial intracranial activity in a phase II study in patients with pretreated ALK-positive NSCLC (with or without baseline CNS metastases), whose disease had progressed on crizotinib or other second-generation ALK TKIs (Bauer et al. 2020). CNS metastases from breast cancer have been very difficult to effectively treat. There have been no FDA-approved systemic therapies until April 2020 with the approval of tucatinib, an oral small-molecule tyrosine kinase inhibitor of HER2 in combination with trastuzumab and capecitabine (Murthy et al. 2018, 2020). In the case of melanoma metastases, FDA approvals in recent years have included BRAF inhibitors vemurafenib and dabrafenib; a MEK inhibitor, trametinib; and an anti-CTLA4 antibody, ipilimumab (Parrish et al. 2015). However, for patients with brain tumor metastasis, the standard of care remains radiation and surgery due to limited brain distribution of these agents.
4 Challenges in the Treatment of Brain Tumors
Despite the aggressive multimodal approach of surgery, chemotherapy, and radiation for the treatment of brain tumors, the expected survival for patients with GBM is approximately 15 months, and for patients with brain metastases, it is approximately 4–6 months (Bi and Beroukhim 2014; Liu, Tong and Wang, 2019). As described earlier, extensive and complete surgical resection of brain tumors is difficult because they are frequently invasive and are often in areas of the brain that control speech, motor function, and the senses. TMZ, used as the first-line chemotherapeutic for the treatment of GBM, is only beneficial for a subset of patients (~50%) having the MGMT promoter methylation, and this limits its effectiveness in a broad patient population (Lee 2016). In the case of radiation, the side effects range from short-term conditions like inflammation and edema to long-term effects like radiation necrosis, blindness, and cognitive dysfunction (Laack and Brown 2004).
The identification and development of drug delivery strategies that can be used with the current standard of care of radiation and chemotherapy is a significant challenge in oncology, with multiple hurdles to be overcome. These hurdles are depicted in Fig 24.2. First, an important reason drug molecules often have limited brain penetration is due to the presence of efflux transporters at the blood-brain barrier (BBB) and the blood-tumor barrier (Omidi and Barar 2012). Second, the complex tumor microenvironment communicates with other cells in the brain environment in a manner that leads to the promotion of tumor progression and resistance to treatments (Trédan et al. 2007; Perus and Walsh 2019). Third, spatial heterogeneity of drug distribution is a critical consideration in the context of brain tumors, many of which exhibit both a partially intact BBB as well as heterogenous BBB disruption in different regions of the tumor and area surrounding the tumor (Sarkaria et al. 2018). Fourth, the highly heterogenous genetic makeup of GBM from patient to patient as well as within the tumor of a single patient presents significant additional challenges. This highlights the need to understand these complexities to be able to successfully identify agents that can selectively and significantly benefit a subset of the GBM population (Bastien et al. 2015). Finally, given the limited understanding of how molecularly targeted agents assist radiation and chemotherapy, understanding heterogenous distribution is critical to avoid the development of resistance. Moreover, determining the delivery of these agents to normal tissues leading to toxic side effects needs to be examined in conjunction with measuring specific pharmacodynamic effects that can demonstrate efficacy in tumor cells and toxicity in normal tissues.
5 Transporter Expression in Brain Tumors
The brain depends on nutrients for its growth and development and also needs to be protected from circulating xenobiotics and toxins. This selective entry into the brain is modulated by the presence of membrane-embedded receptors that act as transport systems (Cardoso et al. 2010). While active influx transporters and facilitated carriers are necessary for the transport of essential nutrients and growth factors, a second type of transporters, critical for brain delivery of therapeutic agents, is the efflux transport systems that are mainly comprised of the ABC (ATP binding cassette) super family that uses ATP hydrolysis to provide energy to efflux molecules from the brain back to the blood. The most relevant ABC transporters expressed in the brain endothelial cells are P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and the multidrug resistance-associated proteins (MRP) (Löscher and Potschka 2005). The expression of these transporters is depicted in Fig. 24.3.
Transporter expression at the blood-brain and blood-tumor barriers. (a) Expression of P-glycoprotein and breast cancer resistance protein at the healthy blood-brain barrier. (b) Expression of P-glycoprotein and breast cancer resistance protein at the blood-tumor barrier and in brain tumor cells of different origin
P-glycoprotein (P-gp, ABCB1)
P-gp expression was first detected in the BBB by Cordon-Cardo et al. (Cordon-Cardo et al. 1989) using immunohistochemistry. Thereafter several groups have demonstrated increased P-gp protein and ABCB1 mRNA expression levels using western blotting or quantitative PCR in whole tumor lysate from a wide range of primary and secondary human brain tumors (Demeule et al. 2001; Spiegl-Kreinecker et al. 2002; Ginguene et al. 2010; Uchida et al. 2011). Some immunohistochemistry studies have demonstrated that increase in P-gp protein expression levels was due to P-gp expression in tumor-associated brain capillary endothelial cells and not due to P-gp expression in tumor cells (Tanaka et al. 1994; Korshunov et al. 1999; Tews et al. 2000; Ginguene et al. 2010; Veringa et al. 2013). Toth et al. showed a particularly heterogenous P-gp expression pattern in patient GBM samples and demonstrated that P-gp expression was significantly decreased in capillary endothelial cells surrounding necrotic areas of the tumor core and in areas with high angiogenesis such as the tumor rim (Toth et al. 1996; Demeule et al. 2001; Bhagavathi and Wilson 2008). While P-gp protein expression is increased in brain tumor cells when compared to their healthy counterparts, the overall transporter expression has been reported to be relatively low in the tumor cell (Marroni et al. 2003). Therefore, unlike the blood-brain barrier where P-gp expression levels are high and correlate with low survival, expression in brain tumor cells did not appear to correlate with tumor grade, survival, or chemoresistance (Abe et al. 1998; Tews et al. 2000; Valera et al. 2007; Wu et al. 2019; Yan et al. 2019). However, a contrasting report does show that P-gp expressed by endothelial cells may be a negligible component of the human GBM multidrug resistance (MDR). In this report the authors indicate that the tumor perivascular astrocytes may dedifferentiate and resume a progenitor-like P-gp activity and contribute to the MDR profile of GBM vessels as well as perivascular P-gp expressing glioma stemlike cells. This study lends credence to P-gp efflux activity contributing to therapeutic failure in both vascular and parenchymal cells (de Trizio et al. 2020).
Breast Cancer Resistance Protein (BCRP, ABCG2)
ABCG2 mRNA expression at the BBB was first detected in 2002 in primary porcine endothelial cells (Eisenblaetter and Galla 2002). Cooray et al. (2002) were the first to show BCRP protein expression at the human blood-brain barrier, where BCRP is located in the luminal membrane of endothelial cells and actively contributes to outwardly directed efflux transport (Cooray et al. 2002; Zhang et al. 2003; Aronica et al. 2005). In brain cancer tissue resected from patients, BCRP expression is mainly restricted to the brain tumor barrier (BTB) (Aronica et al. 2005; Bhagavathi and Wilson 2008; Ginguene et al. 2010; Sakata et al. 2011; Shawahna et al. 2011; Bhatia et al. 2012; Veringa et al. 2013).
In contrast to capillary endothelial cells of the BTB, most brain tumor cells in patient samples do not express BCRP (Sakata et al. 2011; Veringa et al. 2013). However, in those cases where BCRP is expressed in brain tumor cells, these cells often display stem cell characteristics and BCRP expression correlates with poor prognosis (Bleau et al. 2009; Emery et al. 2017). Given these studies, BCRP may be more critical in brain tumor cells compared to P-gp. However, anticancer drug efflux from tumor cells appears to be secondary to efflux at the BBB and BTB as a mechanism of drug resistance in brain tumors (Emery et al. 2017).
6 Transporter Regulation
A newly emerging strategy to overcome BBB P-gp/BCRP is targeting transporter regulation. Targeting the signaling pathways that regulate P-gp/BCRP and result in decreased transporter expression and activity at the BBB can potentially be exploited to improve brain delivery of anticancer drugs, which have been described in Fig. 24.4.
6.1 Transcriptional Regulation
6.1.1 Transporter Regulation Through p53
The tumor suppressor p53 (wildtype) binds to the p53 response element in the promotor region of its target genes, which stops the cell cycle and thus cell division. p53 binds to the ABCB1 promotor suppressing its activation (Johnson et al. 2001). Mutant p53, however, acts as an activator of the ABCB1 promotor, stimulating transcription and resulting in increased P-gp expression and activity levels (Sampath et al. 2001).
Marroni et al. showed that wild-type p53 inhibits ABCB1 and ABCG2 transcription resulting in decreased P-gp and BCRP expression levels in healthy human astrocytes (Marroni et al. 2003). In contrast, inactivation or loss of p53 increased P-gp/BCRP expression levels in several human glioma cell lines (El-Osta et al. 2002; Sarkadi et al. 2006). Kondo et al. showed that expression levels of murine double minute 2 mRNA (Mdm2), a negative regulator of p53, are increased in human U87 cells in vitro. Mdm2 overexpression inhibited p53, resulting in increased P-gp expression. On the other hand, transfecting U87 cells with antisense Mdm2 microRNA reduced P-gp expression. Thus, mutant p53 increases P-gp and BCRP expression and activity, thereby contributing to chemoresistance (Kondo et al. 1996). Understanding mutant p53 functions will lead to the development of novel approaches to restore p53 activity or promote mutant p53 degradation for future GBM therapies.
6.1.2 Transporter Regulation by Nuclear Receptors
Nuclear receptors are ligand-activated transcription factors that target genes including ABCB1 and ABCG2 (Nakanishi and Ross 2012, Sugawara et al. 2010, Hellmann-Regen et al. 2012, Mani et al. 2013). Nuclear receptor activation has been shown to increase P-gp/BCRP expression and activity, which reduces anticancer drug bioavailability and lowers anticancer drug levels in the brain, resulting in decreased drug efficacy (Sarkadi et al. 2006; Nakanishi and Ross 2012).
The nuclear receptor pregnane X receptor (PXR , NR1I2) is activated by a number of xenobiotics. This includes the anticancer drugs cisplatin, carboplatin, tamoxifen, and etoposide, as well as small-molecule tyrosine kinase inhibitors (e.g., lapatinib, sorafenib, and dasatinib) that have been demonstrated to activate PXR, thereby inducing P-gp expression in several human brain, colon, and liver cancer cell lines in vitro (Mani et al. 2005, Harmsen et al. 2013, Yasuda et al. 2019). Han et al. (2015) have shown a similar mechanism for peroxisome proliferator-activated receptor γ (PPARγ) in cisplatin-resistant human U87 glioblastoma cells, where PPARγ activation increased P-gp expression and activity levels, which contributed to anticancer drug resistance in vitro.
These studies may indicate that anticancer drugs can increase P-gp and BCRP mRNA and protein expression levels through nuclear receptor activation. While this phenomenon has been demonstrated in various glioma, glioblastoma, and neuroblastoma cancers, there are currently no in vivo data showing that this restricts anticancer drug uptake into the brain and brain tumor tissue.
6.2 Growth Factors
Growth factors stimulate proliferation and tumor growth and regulate the expression and activity of P-gp/BCRP both at the BBB and BTB (Takada et al. 2005; Zhou et al. 2006; Bleau et al. 2009; Nakanishi and Ross 2012; Munoz et al. 2014). One growth factor that is a major regulator of P-gp and BCRP is endothelial growth factor (EGF) acting through endothelial growth factor receptor (EGFR) (Chen et al. 2006; Nakanishi et al. 2006). In 57% of glioblastoma, EGFR is either mutated, amplified, or both, leading to constitutive activation of downstream signaling (Brennan et al. 2013; Eskilsson et al. 2018). Nakanishi et al. demonstrated that stimulation of EGF signaling increased the number of BCRP-positive glioma cells in vitro, making it a likely cause for drug resistance in glioblastoma cells (Nakanishi et al. 2006). Additionally, the EGFR inhibitor gefitinib decreased BCRP expression and activity levels in vitro, opening an avenue for overcoming BCRP-mediated drug resistance as well as the treatment of glioblastoma.
6.3 PI3K/Akt Signaling
In many cancers, overactivity of growth factor signaling overstimulates downstream targets including the phosphoinositide-3 kinase (PI3K, PIK3 genes)/protein kinase B (Akt, AKT1/2) pathway (Cancer Genome Atlas Research, 2008) (Brennan et al. 2013). Additionally, 90% of GBM patients have at least one alteration in the PI3K/Akt pathway, including loss of the tumor suppressor and negative regulator phosphatase and tensin homolog (PTEN) (Brennan et al. 2013). Bleau et al. demonstrated that the PI3K/Akt pathway is overactive in a subpopulation of primary human glioma cells with stem cell characteristics leading to increased BCRP protein levels (Bleau et al. 2009). Several groups have published corroborating evidence demonstrating that this regulatory pathway is present in brain tumors as well as at the healthy BBB (Takada et al. 2005; Bleau et al. 2009; Hartz et al. 2010b; Nakanishi and Ross 2012; Huang et al. 2013, 2014). We have shown that inhibiting PI3K/Akt in isolated brain capillaries decreased P-gp and BCRP protein expression and transport activity levels, potentially opening a window in time for anticancer drug delivery into the brain (Hartz et al. 2010a, b). Thus, inhibition of PI3K/Akt is a potential promising strategy to overcome P-gp/BCRP-mediated efflux at the BBB and BTB.
6.4 Adenosine Signaling
Several groups have demonstrated that the FDA-approved adenosine receptor A2B agonist regadenoson increases P-gp ubiquitination, thereby inducing P-gp proteasomal degradation (Kim and Bynoe 2015, 2016; Yan et al. 2019). Jackson et al. developed a therapeutic strategy using regadenoson to decrease P-gp protein expression and activity at the BBB and BTB (Jackson et al. 2016). The authors showed, in rats, that regadenoson co-administration significantly increased temozolomide brain levels compared to control animals that only received temozolomide. When regadenoson was administered to patients with angina or previous heart attacks (no brain tumors) that underwent cardiac stress testing, brain levels of the P-gp substrate 99mTc-sestamibi were increased (Jackson et al. 2017). Despite these promising results, a phase I clinical trial in patients with recurrent GBM testing TMZ with and without regadenoson was unsuccessful (Jackson et al. 2018).
6.5 Temozolomide
Riganti et al. (2013) found that Wnt3a and P-gp protein expression levels are higher in glioblastoma stem cells compared to healthy astrocytes. They also found that activating Wnt signaling increased P-gp expression levels in glioblastoma cells. However, following temozolomide treatment of primary glioblastoma cells in vitro, Wnt signaling was decreased, resulting in decreased P-gp expression levels. From these data the authors concluded that temozolomide reversed drug resistance by decreasing P-gp protein expression through the Wnt pathway (Riganti et al. 2013). In contrast, Munoz et al. showed that temozolomide increased P-gp expression and activity in U87 and T98G glioblastoma cells in a biphasic manner. In the early treatment phase, temozolomide induced P-gp trafficking to the cell membrane and, therefore, increased P-gp efflux function in glioblastoma cells in vitro. During later stages of treatment, temozolomide activated ERK1/2-JNK-AP1 signaling, which increased ABCB1 mRNA and P-gp protein expression levels (Munoz et al. 2014). To date, the effect of temozolomide on drug resistance remains controversial and needs further evaluation.
7 Strategies to Improve Treatment of Brain Tumors
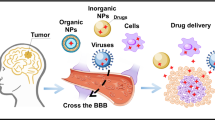
As outlined in the previous sections, the delivery of adequate concentrations of anticancer-targeted therapies to tumor cells residing in the brain has proven to be a significant challenge. Various approaches to overcome the delivery barrier have been studied, and some are described in the following. These approaches are depicted in Fig. 24.5.
Drug delivery strategies for the treatment of brain tumors. (a) Transcellular diffusion, (b) utilizing influx transporters, (c) paracellular transport, (d) receptor-mediated endocytosis, (e) adsorptive endocytosis, (f) osmotic BBB disruption, (g) focused ultrasound using microbubbles, (h) local delivery of cytotoxic agents, (i) convection enhanced delivery
7.1 Designing Molecules with Increased Brain Penetration and Reduced Efflux Liability
Designing drug molecules that can permeate the BBB and attain effective concentrations in the brain should be a priority for CNS drug discovery programs. This can be achieved by incorporating key physicochemical properties that aid in BBB penetration and rational structural modifications. Critical physicochemical properties have been identified and computational models developed to optimize these properties for successful brain delivery (Rankovic 2015, 2017; Heffron 2016). Wager et al. (Wager et al. 2010) have developed a multiparameter optimization (MPO) approach to screen molecules for optimal neuro-pharmacokinetic and safety profiles. The key physicochemical properties were: (1) lipophilicity, with a partition coefficient (ClogP) ≤ 3 being desirable; (2) a distribution coefficient (ClogD) ≤ 2; (3) molecular weight (MW) ≤ 360 Daltons; (4) topological polar surface area (tPSA) between 40 and 90Å2; (5) number of hydrogen bond donors (HBD) ≤ 0.5; and (6) most basic functional group with a pKa ≤ 8. The six properties were equally weighted with a score between 0 and 1, resulting in a final CNS MPO score ranging from 0 to 6, thereby allowing multiple combinations of the parameters to achieve a particular MPO score. This algorithm was applied to 119 marketed CNS drugs, and 74% of those drugs showed high (>4.5) CNS MPO scores. The compounds with a high MPO score also displayed desirable ADME properties like high permeability, low P-gp efflux liability, and higher stability as might be expected for drugs that have been approved for CNS indications (Wager et al. 2010). Additional refinements have been made to this original algorithm, using the same six parameters for optimization, to improve the structural design enhancement and quality of compounds nominated for clinical development of CNS therapeutics (Wager et al. 2016).
The use of an algorithm to optimize key physicochemical properties, in conjunction with rational structural modifications to reduce efflux liability, led to the identification of brain penetrant PI3K inhibitors, GNE-317 and GDC-0084. These molecules showed significantly greater tumor growth inhibition in GBM mouse models as compared to BBB impenetrant PI3K inhibitors (Sutherlin et al. 2010; Salphati et al. 2012; Heffron et al. 2016). Importantly, the PI3K inhibitor GDC-0084 showed promising initial results in a phase I study that was conducted in patients with recurrent high-grade glioma (Wen et al. 2020). Another example is AZD3759, a potent brain penetrant EGFR inhibitor, which was developed using gefitinib as the initial lead. Techniques like repositioning of fluoro moiety and reduction of rotatable side chain were employed for overcoming P-gp and BCRP efflux to improve brain penetration, while maintaining the quinazoline scaffold necessary for activity (Zeng et al. 2015). In a study using cassette dosing to examine the brain penetration of eight EGFR TKIs, AZD 3759 showed the greatest brain penetration (Kim et al., 2019a, b). AZD3759 is now in a phase I clinical trial to assess its safety, tolerability, and primary efficacy in patients with advanced NSLC (NCT02228369). Considering the high propensity of developing brain metastases from NSLC, the development of AZD3759 can be a significant step in the treatment of these patients. One more example of structural modification to improve BBB permeability to evade efflux is of crizotinib, an ALK inhibitor, leading to the development of BBB penetrant lorlatinib (PF-06463922) (Basit et al. 2017). This was achieved by cyclization of crizotinib to form the macrocyclic lorlatinib leading to a reduction in the effective HBDs through the formation of intramolecular hydrogen bonds. This strategy and a reduction in rotatable bond count decreased its interaction with efflux transporters and improved CNS distribution (Basit et al. 2017). In an ongoing phase II study (NCT01970865), lorlatinib showed substantial intracranial activity in patients with recurrent ALK-positive NSCLC, with or without baseline CNS metastases, whose disease progressed on crizotinib or other second-generation ALK TKIs (Bauer et al. 2020). And finally, AZD1390, a selective and potent ATM inhibitor, synthesized to be brain penetrant using strategies informed by AZD0156 another potent ATM inhibitor that is a substrate of efflux transporters. This compound is now in early clinical trials for use as a radiosensitizer in CNS malignancies (Durant et al. 2018). Taken together, these examples clearly demonstrate that computational models and structure-guided drug design early in CNS drug discovery programs can support the development of brain penetrant drugs for brain tumors, with structural modifications to reduce the affinity for efflux transporters, a key component.
7.2 Inhibition of Efflux Transporters at the BBB
Inhibition of transporters particularly P-gp and BCRP as a strategy to overcome transporter-mediated drug delivery limitations has been investigated (Huisman et al. 2003; Baumert and Hilgeroth 2012). The first-generation inhibitors were comprised of marketed drugs known to inhibit efflux transporters, which includes verapamil, cyclosporine-A, and quinidine (Shen et al. 2008; Bui et al. 2016). However, these inhibitors have low potency and selectivity and require high doses. An analog of cyclosporine-A, valspodar (PSC-833), was developed as a second-generation inhibitor with more potent inhibition of P-gp, but it also interfered with cytochrome P450 function. As a consequence, third-generation inhibitors, including tariquidar, elacridar, and zosuquidar, were developed (Gampa et al. 2020). Although co-administration of tariquidar improved the brain exposure of targeted agents and corresponding efficacy in preclinical studies without any toxicity concerns, two phase III clinical trials in NSCLC patients were terminated due to toxicity when used in combination with paclitaxel/carboplatin or vinorelbine (Fox and Bates 2007). Similarly, toxicity concerns were reported in clinical studies investigating the use of zosuquidar and elacridar (Sandler et al. 2004; Kuppens et al. 2007). The clinical efficacy of pharmacological inhibition of efflux transporters to increase brain distribution clearly requires a potent efflux influx transport inhibitor that does not increase the toxicity of the CNS active agents. If very potent inhibitors are used to improve CNS delivery of toxic compounds, a careful assessment of CNS toxicity due to increase in brain delivery will be required.
7.3 Utilizing Influx Transporters at the BBB
An alternative to overcoming efflux transporters is designing drugs to take advantage of innate influx transporter systems already expressed at the BBB. Targeting a transport system at the BBB for drug development and improved delivery can be used in the treatment of primary brain tumors. Glucose transporters (GLUT) are known to facilitate transport of glucose from blood to the brain. It was observed that when a mannose derivative was incorporated onto a liposome, the delivery system exhibited better penetration across the BBB via the glucose transporter (GLUT1) into the mouse brain (Wei et al. 2014). Choline transporters are another group of transport systems responsible for binding with positively charged quaternary ammonium groups or simple cations. A 60-nm size particles coated with quaternary ammonium ligands have shown enhanced penetrability across an in vitro BBB model (bovine BCEC) (Gil et al. 2009). Histidine/peptide (peptide/histidine transporter), large neutral amino acid transporter (LAT1), and vitamin transporters [sodium-dependent multivitamin transporter (SMVT) and sodium-dependent vitamin C transporter (SVCT)] are some of the influx transporters that have gained attention (Castro et al. 2001; Bhardwaj et al. 2006; Uchida et al. 2015; Puris et al. 2020) These transporters are being studied extensively for targeted drug delivery to the brain.
7.4 Targeting Receptor-Mediated Transport Systems at the BBB
Receptor-mediated transcytosis is one of the promising strategies for targeted delivery across the BBB with high specificity, selectivity, and affinity (Xu et al. 2013). However, there might be a possibility of competition between endogenous substrates and drug ligands for the same receptor leading to reduced targeting efficiency. Receptors expressed on the brain capillary endothelium include transferrin receptor (TfR) (Pardridge et al. 1987), low-density lipoprotein receptor (Ueno et al. 2010), insulin receptor (IR), and nicotinic acetylcholine receptors (Pardridge et al. 1985; Vu et al. 2014). Targeting with endogenous ligands as well as ligands based on phage display or structure-guided design can be exploited for receptor-mediated transcytosis.
An example of this is GRN1005, an angiopep-2 peptide conjugated to paclitaxel, which gets across the BBB via transcytosis using the lipoprotein receptor-related protein 1 (LRP1) (Kurzrock et al. 2012; Drappatz et al. 2013). Another example is 2B3-101, which is a pegylated liposome conjugated with glutathione and actively transported across the BBB. This formulation showed enhancement in the uptake and delivery when compared to the conventional doxorubicin liposomal formulation (Gaillard et al. 2014). T7, targeting TfR1, has been investigated to deliver antisense oligonucleotides to gliomas (Kuang et al. 2013; Zong et al. 2014).
Monoclonal antibodies (mAbs) are another class of molecules that are being currently investigated to inhibit tumor growth driver pathways. Bevacizumab, targeting VEGF, as mentioned earlier received accelerated FDA approval for newly diagnosed and recurrent GBM. Cetuximab, another mAb targeted to EGFR failed to show survival benefit in a phase II trial (Neyns et al. 2009). Antibodies, being large (~150 kDa) molecules, do not generally cross the BBB and hence despite showing effectiveness in case of peripheral tumors need enhanced delivery mechanisms to cross the BBB and be effective in case of brain tumors (Zhang and Pardridge 2001; St-Amour et al. 2013). With recent advances in antibody engineering and use of antibody fragments, the structure of these large molecules is being exploited to modify and utilize different domains to promote receptor-mediated transcytosis. TfRs as well as IRs have been shown to be widely used targets for therapeutic antibodies as well as nanocarriers linked to antibodies for brain delivery (Boado et al. 2010; Kim et al. 2019a, b). In a recently published study, a nanocarrier loaded with p53 gene therapy, decorated with anti-TfR1 single-chain variable fragments, SGT-53, showed success in GBM preclinical models and has moved into clinical trials (Kim et al. 2019a, b). In another study from AbbVie, dual-variable-domain IgG molecules with dual affinity (TfR for receptor mediated transcytosis and HER2 for HER2+ brain tumors) have been developed for precision targeting (Karaoglu Hanzatian et al. 2018).
7.5 Antibody Drug Conjugates (ADCs)
ADCs are composed of an antibody acting as a targeting agent linked to cytotoxic compounds to enable their delivery into the cells. Ado-trastuzumab emtansine (T-DM1) is an ADC which is trastuzumab (mAb targeting HER2) linked to the maytansinoid DM-1 (microtubule inhibitor) using a stable linker (Lambert and Chari 2014). A series of studies have shown prolonged progression free survival as well as treatment effect in case of breast cancer brain metastases using T-DM1 (Bartsch et al. 2015; Keith et al. 2016; Okines et al. 2018; Ricciardi et al. 2018). Depatuxizumab mafodotin (ABT-414) is composed of an antibody targeted to cells with EGFR amplifications and releases monomethyl auristatin F (microtubule toxin). ABT-414 was studied in phase II trials for recurrent GBM in combination with TMZ; however, the phase III trial was halted as no overall survival benefit was observed (Van Den Bent et al. 2020). Other EGFR targeting ADCs, ABBV-221 and ABBV-321, are being evaluated in phase I trials for GBM (NCT02365662, NCT03234712).
7.6 Immunotherapy
Immunotherapy involves harnessing the body’s own immune system to identify, target, and kill tumor cells. This approach is particularly effective in tumors with high tumor mutational burden but has not been effective in brain tumors despite their highly heterogenous nature (Liu et al. 2020). A variety of immunotherapies are being explored for brain tumors using multiple strategies—checkpoint inhibition, utilizing chimeric t-cell receptors, dendritic cell, and peptide vaccines as well as using viral vectors for gene therapy. However, none of these have been approved for treatment. The reader is directed to a comprehensive review of these strategies as well as their challenges in the following reviews (Lyon et al. 2017; Liu et al. 2020).
7.7 Development of Radiosensitization Strategies with Current Standard of Care
DNA damage response signaling pathways play a critical role in DNA repair and cell survival following radiation therapy, and the inhibition of these pathways could augment the cytotoxicity associated with radiation providing a sensitizing effect. DNA damage occurs continually through various mechanisms. Environmental factors such as ultraviolet (UV) radiation, x-rays, and smoking, as well as endogenous factors, including replication errors, reactive oxygen and nitrogen species, and hydrolysis of bases are some examples through which DNA damage may occur (Hoeijmakers 2009). High proliferation rates inherent to tumor cells may also lead to an amplification of errors and DNA damage. Evolution has led to the development of complex cellular mechanisms that detect and repair such defects, and these have been collectively termed the DNA damage response (DDR) (Harper and Elledge 2007). Several pathways have been identified within the DDR, each distinct in their mechanism of repairing DNA. Core DDR pathways include nonhomologous end joining (NHEJ), homologous recombination, base excision repair, nucleotide excision repair, mismatch repair, and interstrand cross-link repair (Lord and Ashworth 2012). These pathways are activated by a cascade of events initiated by DNA damage sensor proteins that engage signaling networks and regulate cell cycle progression allowing for DNA repair to occur (O’Connor 2015). An active DDR machinery is essential for the healthy physiology of the cell, ensuring its survival, and is an important mechanism of resistance to cytotoxic approaches. Accordingly, the inhibition of the DDR in tumor cells provides an excellent therapeutic opportunity (Sun et al. 2018).
The response to DNA damage will be different depending on the cell cycle status providing a varied range of cell cycle pathways for targeting for the sensitizing effect. For example, cells in G1 will not have sister chromatid DNA available as an undamaged template and therefore will be dependent upon NHEJ pathways for the repair of DSBs. In addition, there are important differences in the primary roles of checkpoints at different stages of the cell cycle and in the DDR factors that are involved. For example, the G1/S checkpoint allows the repair of DNA damage prior to the start of DNA replication in order to remove obstacles to DNA synthesis, and key DDR factors regulating this checkpoint include ATM, CHK2, and p53. The intra-S phase checkpoint proteins ATR, CHK1, DNA-PK, and WEE1 can delay replication origin firing to provide time to deal with any unrepaired DNA damage that has occurred, thus preventing under-replicated DNA regions being taken beyond S-phase. The activities of the G2/M checkpoint proteins including CHK1, MYT1, and WEE1 lead to an increase in phosphorylated CDK1, thereby keeping it in its inactive state and delaying mitotic entry. The G2/M checkpoint really represents the last major opportunity for preventing DNA damage being taken into mitosis where unrepaired DSBs and under-replicated DNA may result in mitotic catastrophe and cell death (Castedo et al. 2004). Recent analyses suggest that there are at least 450 proteins integral to DDR (Pearl et al. 2015), and the choice of optimal drug targets within DDR will be based on what type of DNA damage repair is to be inhibited and where in the cell cycle that damage is likely to occur. Major drug development efforts are being directed to take the DDR inhibitors into the clinic as radiation and chemotherapy sensitizers.
7.8 Modification of Tight Junctions at the BBB
A selective disruption of the BBB followed by administration of anticancer agents provides for a promising approach to enhance drug delivery to the brain in the treatment of brain tumors. Various techniques have been employed to cause transient BBB disruption, as briefly discussed below.
7.8.1 Osmotic Disruption of the BBB
The administration of hypertonic solutions causes disruption of the BBB due to shrinkage of endothelial cells, leading to the alteration of tight junctions between them, thereby allowing paracellular movement of drugs. This method was first proposed by Rapoport et al. in 1972 and later was translated to the clinic with the first phase I clinical trial in 1979 (Rapoport et al. 1972; Levin et al. 1979). The hypertonic solution of 1.4 M mannitol infusion is FDA approved for administration to patients for transient BBB disruption (Neuwelt 1980). Other agents investigated include saline, arabinose, urea, lactamide, and a variety of radiographic contrast agents (Kroll et al. 1998). In a clinical study in the 1980s by Neuwelt et al., improved survival and long-term remission were observed in patients with primary CNS lymphoma following osmotic BBB disruption plus methotrexate (Neuwelt 1980). Agents in addition to methotrexate that have been used in the clinic with osmotic BBB disruption include etoposide, cyclophosphamide, carboplatin, and melphalan. The transient BBB disruption followed by administration of anticancer agents has been employed as a strategy to overcome brain drug delivery limitations (Rapoport 2000; Kemper et al. 2004). However, this approach is invasive, and complex to perform and is associated with adverse effects (Bellavance et al. 2008).
7.8.2 Focused Ultrasound
Focused ultrasound (FUS) is based on a concentration of acoustic energy onto a focal area that results in BBB disruption. Microbubble (MB)-enhanced FUS involves the oscillation of MBs in the presence of FUS to cause BBB disruption. These microbubbles are FDA approved for use as contrast agents in ultrasound imaging and in the context of drug delivery and are used to lower the energy threshold for BBB disruption (Timbie et al. 2015). This approach is local, transient, and reversible and has demonstrated improvements in delivery and efficacy of anticancer agents in glioma models (Liu et al. 2014; Deng et al. 2019). The delivery of small molecules like TMZ, doxorubicin, and 1,3-bis (2-chloroethyl)-1-nitrosourea (BCNU) to large molecules like bevacizumab and trastuzumab as well as cell therapy, viral therapy, and nanoparticle delivery has been facilitated by FUS with microbubbles in glioma and brain metastases (Meng et al. 2018; Bunevicius et al. 2020). Also, significant downregulation of localized P-gp expression with no apparent damage to brain endothelial cells was observed, suggesting the potential use of MB-FUS for targeted brain delivery of drugs that are liable to efflux by P-gp (Cho et al. 2016). However, the long-term effect of FUS on the brain microvasculature has not been investigated. A thorough investigation of safety due to repeated FUS treatments as well as safe and appropriate ultrasound settings has to be conducted for drug delivery applications. The reader is guided to two comprehensive reviews for the use of FUS in brain tumors and the ongoing clinical trials (Meng et al. 2018; Bunevicius et al. 2020).
7.8.3 Photodynamic Therapy Approaches
Photodynamic therapy (PDT) involves the administration of a photosensitizing agent that localizes in the tumor followed by photoactivation that can result in a direct inhibitory effect on tumor cells and also a localized disruption of BBB that can aid in the delivery of other anticancer agents to the brain tumor (Akimoto 2016). An early report of PDT was by Perria et al. that utilized a hematoporphyrin derivative injected i.v. as a sensitizing drug with a helium-neon laser to trigger the photodynamic process (Perria et al. 1980). First-generation photosensitizers include hematoporphyrin and its derivatives. Chlorins (talaporfin sodium and temoporfin) and 5-aminolevulinic acid (5-ALA) are examples of second-generation photosensitizers that were developed to be more potent. 5-ALA is the most commonly used photosensitizer due to its high oral bioavailability, favorable safety profile, and preferential accumulation in malignant gliomas (Mahmoudi et al. 2019). The recent FDA approval of 5-aminolevulinic acid (5-ALA) for fluorescence-guided resection (FGR) of tumors has generated immense interest in leveraging this agent as a means to administer photodynamic therapy (PDT). The joint clinical application of fluorescence-guided surgery (FGS) and PDT confers the ability to both visualize tumor cells and selectively destroy them. Clinical studies of PDT using porfimer sodium, talaporfin sodium, 5-ALA, boronated porphyrin, and temoporfin in GBM have been reported (Cramer and Chen 2020). Third-generation photosensitizers were developed for enhanced tumor cell selectivity achieved through the conjugation of modifiers including nanoparticles and antibodies (Allison and Sibata 2010). Lack of clear efficacy in overall survival, technical limitations in light delivery, and photosensitizer design as well as unclear safety profiles of varied photosensitizers have hindered the impact that PDT can have in brain tumor treatment. Exploration of novel photosensitizer agents and safe photosensitization strategies in brain tumors is warranted for incorporation of PDT into current standard of care (Cramer and Chen 2020).
7.9 Local Delivery Methods
Local drug administration directly into the CNS has been employed as a strategy to precisely deliver drug to the target site in the brain. These local delivery methods include biodegradable wafers placed in the tumor cavity post resection, convection-enhanced delivery (CED), and intrathecal delivery into CSF cavities (Blakeley 2008; Calias et al. 2014).
7.9.1 Biodegradable Wafers
Polymer-based biodegradable wafers have been available for patients with brain tumors as one of the earliest treatment options with Gliadel (BCNU/carmustine) approved by the FDA in 1996 for recurrent high-grade gliomas. These wafers are placed in the tumor cavity post resection for sustained drug release over a few days and have also been considered for improving drug delivery to brain tumors post resection. This approach provides local control of disease but is limited by the modest distribution of BCNU away from the resection cavity. Gliadel has also been used in patients with brain metastases where patients with single brain metastases underwent surgical resection followed by Gliadel implantation and whole brain radiation treatment (Ewend et al. 2007). In an effort by Domb et al., co-loading of BCNU and TMZ within poly(lactic acid-glycolic acid) (PLGA) wafers in rat glioma models led to a 25% enhancement in survival (Shapira-Furman et al. 2019). Lee et al. developed a novel material and device technology consisting of a flexible, sticky, and biodegradable wireless device loaded with doxorubicin for controlled intracranial delivery using mild-thermal actuation. In mouse and canine models of GBM, this device showed tumor volume suppression and improved survival indicating its potential to be translated to humans utilizing a variety of other potent anticancer agents for intracranial delivery (Lee et al. 2019). A major challenge for this technology is to ensure biocompatibility and biodegradation in a reasonable time period, as incompletely biodegraded material can lead to inflammatory responses in patients. The success of these therapies is limited due to their inability to reach to the invasive and dense tumor cells due to poor diffusion characteristics (Wolinsky et al. 2012).
7.9.2 Convection-Enhanced Delivery
Convection-enhanced delivery (CED) is a bulk-flow (hydrostatic pressure differential)-driven invasive technique that affords the continuous delivery of small and large molecular weight compounds into the brain parenchymal tissue through infusion catheters implanted during surgery (Debinski and Tatter 2009). It was first proposed by Bobo et al. in 1994 for the delivery of macromolecules to the brain (Bobo et al. 1994). Two phase III trials were initiated in participants with GBM. One trial utilizing Tf-CRM107 was aborted, with data available from a phase II trial (Weaver and Laske 2003). The other phase III trial, the PRECISE trial, compared the infusion of citredekin besudotox (PE38QQR) with recombinant human interleukin-13 delivered by CED. The study did not reveal statistically significant improvement in survival for patients with recurrent GBM (Kunwar et al. 2010). CED is being widely studied in preclinical and clinical studies for GBM as well as diffuse intrinsic pontine glioma (DIPG) (Vogelbaum and Aghi 2015; Zhou et al. 2016). Limitations of CED include limited area of distribution, requirement of surgery, and increased risk of neurotoxicity due to elevated intracranial pressure (Blakeley 2008). The brain tissue near the catheter may receive effective drug delivery, but the concentrations can decrease steeply as the distance from the catheter tip increases due to competing forces of convective flow through brain parenchyma and drug diffusion into capillaries. One problem with any local drug delivery technique is that molecules with a high permeability or active efflux liability efficiently clear from the brain tissue into blood capillaries following local brain delivery. This phenomenon, the “sink effect,” can influence the volume of brain tissue captured for drug distribution. The brain, a highly perfused organ, has a dense capillary network; therefore, the probability of drug diffusion into the capillary bed can be high, depending on the physicochemical characteristics of the compound (Lonser et al. 2015). Thus, the selection of a suitable drug candidate that has minimal liability for the sink effect and optimization of delivery parameters (such as infusion parameters for CED) to capture the required brain tissue volume (e.g., brain tumor) are critical to achieve beneficial responses with local delivery methods.
7.9.3 Intrathecal Delivery
Intrathecal (IT) administration typically refers to the infusion of drug into the subarachnoid space in the lumbar region. Intrathecal chemotherapy is administered directly into the lumbar thecal sac via lumbar puncture or infused into the lateral ventricle through a subcutaneous reservoir and a ventricular catheter (Ommaya reservoir), thus allowing the drug to distribute into the target sites via diffusion. A phase I trial using implanted ventricular catheter has been reported where chlorotoxin was coupled with the radioisotope 131I (131I-TM-601) infusing radioactive therapy into the tumor resection cavity via an Ommaya reservoir in patients with recurrent malignant glioma (Mamelak et al. 2006). In cases of breast cancer brain metastases, studies employing intrathecal administration of rituximab, trastuzumab alone, and with other cytotoxic agents like methotrexate and cytarabine have been reported (Perissinotti and Reeves 2010; Oliveira et al. 2011; Niwińska et al. 2015; Mack et al. 2016). IT administration suffers from a variety of drawbacks, like limited drug delivery to tumors despite high CSF concentrations, slow rate of drug diffusion, and rapid CSF turnover compared to rate of diffusion leading to rapid clearance of drugs. In addition, the idea that high CSF concentrations correspond to high drug levels in the brain and tumor have led to an impediment in the advancement of IT therapies (Pardridge 2016).
8 How Much Is Enough? Drug Pharmacokinetic-Pharmacodynamic (PK-PD) Relationships in Brain Tumors
The intricate architecture of the CNS as well as the complex tumor microenvironment necessitates careful application of pharmacokinetic principles in the determination of drug distribution to brain tumors and, hence, understanding the PK→PD→Efficacy relationship. A schematic depicting the relationship between PK→PD→Efficacy of novel drug molecules to be used for clinical translation is depicted in Fig. 24.6.
8.1 Drug in Plasma Versus Drug in the Brain Versus Drug in Tumor
The drug concentrations in blood or plasma are routinely measured as surrogates for concentrations at the site of action due to ease of sampling. While drug concentration in the systemic circulation may somewhat reflect the concentration at the site of action when the target is in a peripheral, more accessible tissue, their use as a surrogate for brain drug concentrations can be misleading and even more so for tumor drug concentrations. This is particularly important in the context of the brain when compared to other organs due to the presence of the BBB, which can severely restrict drug distribution to the target site in the brain (Hawkins et al. 2010). The misconception that drug delivery to brain tumors is not impeded by the BBB due to disruption of the tumor vasculature has been furthered by studies that fail to consider the invasive nature of brain tumors. These studies use the “tumor core” concentrations to indicate effective drug delivery to the tumor (Blakeley et al. 2009; Grossman et al. 2013; Sarkaria et al. 2018). The BBB in the tumor core is often leaky, and therefore delivery to the tumor core alone is insufficient to improve patient outcomes, since the invasive cells remain untreated (Sarkaria et al. 2018). These differences in BBB integrity at the tumor core, tumor rim (area of tumor infiltration adjacent to the core), and in the normal brain have been depicted in Fig. 24.7. Concentrations in the tumor core can be inadequate to predict a useful concentration–response relationship, and an “adequate” concentration achieved around the invasive cells is critical for improved response. Accepting the importance of drug delivery across an intact BBB into the brain is the first critical step to develop novel therapies for brain tumors (Agarwal et al. 2012; Sarkaria et al. 2018).
The current standard of care for the treatment of brain tumors involves radiation (a highly BBB penetrant treatment) that can have serious long-term side effects that range from cognitive decline to other serious effects like blindness, local tumor recurrence, and radiation-associated tumor (Amelio and Amichetti 2012). Therefore, understanding the importance of spatial differences in BBB permeability on drug levels, particularly those drugs that are radiation sensitizers, in various regions of the CNS, and the periphery, is a critical factor in the assessment of novel therapies.
8.2 Utilizing Appropriate Preclinical Models to Determine Effective Drug Concentration
Slow progress in the approval of novel therapeutics for the treatment of brain tumors can be attributed to two major factors: (1) inadequate, that is, non-predictive, in vitro systems and (2) the use of preclinical models that fail to address critical aspects of the tumor in the patient (Aldape et al. 2019). A useful in vivo system should include the heterogeneity of BBB permeability and genetic makeup of the tumors. For instance, many patient-derived xenograft (PDXs) orthotopic models of brain tumors can recapitulate genetic drivers and invasive growth leading to vast differences in BBB permeability to drug treatment and as such will enable a more predictive assessment of the benefit of new treatments. Development of PDXs and genetically engineered mouse models (GEMMs) are often suitable for this use. Defining the preclinical spectrum of response for novel agents/therapies across a representative panel of genetically diverse brain tumors with the necessary complexity in the tumor microenvironment including the condition of the BBB can provide important information and guide optimal clinical drug development.
8.3 Impact of Drug Binding in Brain Tumor Treatment
Crucial to the efficacy of any antitumor agent is adequate exposure of target cells to effective concentrations of active drug. However, reducing toxicity to normal cells often depends on limiting exposure to active drug. Many drugs are highly bound in both plasma and in brain tissue. The free drug hypothesis states that the driving force concentration for distribution into tissues is the free concentration in the blood (Dubey et al. 1989; Hammarlund-Udenaes et al. 2008). Therefore, in addition to determining the total brain-to-plasma ratio (Kp, a tissue partition coefficient) of drug molecules, their binding in plasma, brain, and tumor tissues must be evaluated in order to determine tumor exposure to free drug. New therapies will only be effective if they are able to penetrate the BBB and elicit their effects in the tumor cells. Therefore, in addition to a pharmacokinetic assessment of total drug (bound plus unbound) delivery to the brain and the tumor regions, free brain partitioning of the drugs, defined as Kpuu, must also be determined (Fridén et al. 2009, 2011; Loryan et al. 2013). The reader is directed at the review article by Hammarlund-Udenaes et al. for an extensive description of factors to be considered for the rate and extent of delivery to the brain (Hammarlund-Udenaes et al. 2008). Knowledge of drug pharmacokinetics combined with drug binding in plasma and brain, as well as tumor tissues, can help explain the concentration effect relationship with respect to binding as a determinant of an effective drug concentration.
8.4 Dosage Regimen Design for Achieving Target Drug Concentration and Desired Pharmacodynamic (PD) Effect
A comprehensive understanding of drug distribution into tumor and normal tissues, and associated pharmacodynamic effects, is critical for defining which drugs to move forward into phase I dose-seeking studies. It is therefore important for novel treatment options to define key parameters, such as the determinants of free- and bound-drug exposure in plasma, normal brain, and brain tumor as described above, and to relate these metrics to a dose range associated with an effective endpoint, that is, tumor growth reduction, progression free survival, and overall survival. Although new combination drug regimens have generated excitement in the field and initial positive responses, they ultimately fail to demonstrate efficacy due to drug resistance mechanisms and limited brain delivery (Gottesman 2002; Trédan et al. 2007; Van Den Bent et al. 2009; Chamberlain et al. 2014; Sarkaria et al. 2018). These failures can be attributed to not only pharmacokinetic and drug delivery aspects but also pharmacodynamic or cellular mechanism responses within the tumor cells that can compensate for targeted antitumor mechanisms (Wang et al. 2008). These PD-based treatment failures can also be attributed to inadequate drug levels within the brain tumors that in turn lead to poor efficacy. Brain metastases as well as GBM have been shown to have extensive intra- and intertumoral heterogeneity in terms of genetic composition and protein expression. This genetic heterogeneity as well as the heterogeneity in drug distribution contribute to wide ranging responses to drug therapy (Perus and Walsh 2019). Therefore, as mentioned above, the determination of free drug levels within the tumor as well as normal brain is essential to understand if exposures associated with efficacious pharmacodynamic responses can be achieved in and around the tumor where invasive cancer cells are present (Laramy et al. 2017). All these considerations lead to the establishment of a therapeutic window, a key consideration when developing novel treatments for brain tumors. Time-dependent responses of pharmacodynamic biomarkers in response to a dosage regimen are critical and can drive the design of monotherapy and combination treatments. Therefore, PK-PD modeling efforts for novel agents using the predictive preclinical models are being explored to guide dosage regimen selection in humans (Sharma et al. 2012, 2013; Li et al. 2017). Optimizing dose as well as timing is necessary in predicting pharmacodynamic effects, and decisions to move forward with efficacy testing in phase II/III trials then can be made by a combined understanding of drug potency, mechanism of action, PD effects, and drug distribution to invasive tumor.
9 Conclusions
Despite improvements in the management of cancers over the last decade, treatments for brain tumors have not seen significant advances. A diagnosis of either primary or metastatic brain tumor is associated with a grim prognosis and none of the currently available therapies have long-term efficacy. The diffuse and infiltrative nature of these tumors, their location within the brain, and the highly heterogenetic makeup with a variety of mutations make it even more difficult to design effective therapeutics. In this chapter, we describe different drug delivery approaches for the treatment of brain tumor. These drug delivery approaches include both systemic and local delivery options. Key considerations in the PK→PD→Efficacy relationships have been included to inform the development of effective treatments for brain tumors. It is clear that consideration of drug delivery to the brain tumor needs to be incorporated at all levels of research and development in an effort to discover effective treatments.
10 Points for Discussion
-
What factors may be limiting successful clinical translation of therapies demonstrating positive preclinical results in animal models of primary and metastatic brain cancer?
-
Contrast similarities and differences in the standard of care for primary and metastatic brain cancer?
-
List at least four hurdles to developing new drug delivery strategies for chemotherapeutics targeted to brain cancers.
-
Describe at least two ways in which P-gp/BCRP expression is upregulated in brain cancer and at least two ways in which P-gp/BCRP expression may be pharmacologically downregulated.
-
List several reasons why small molecule inhibitors of P-gp/BCRP have not yet been successfully applied for the clinical enhancement of chemotherapeutic brain exposure.
-
Describe at least three methods where brain endothelial cell tight junction integrity can be altered to deliver circulating drugs to brain tumors and describe how they are thought to work. Also discuss limitations, safety issues, and drawbacks associated with each method.
-
Describe at least three methods for local delivery of drugs to brain tumors and describe how they are thought to work. Also discuss limitations, safety issues, and drawbacks associated with each method.
-
Discuss the following concepts and their impact on our understanding of PK→PD→efficacy relationships with respect to the effective treatment of brain tumors:
-
differences in BBB integrity at the tumor core, tumor rim, and in the normal brain
-
major factors associated with preclinical models that have limited development and approval of novel therapeutics for the treatment of brain tumors
-
drug binding in plasma and brain and the difference between Kp and Kpuu
-
common reasons behind PD-based treatment failures
-
References
Abe T et al (1998) Expression of multidrug resistance protein gene in patients with glioma after chemotherapy. J Neurooncol. https://doi.org/10.1023/A:1005954406809
Achrol AS et al (2019) Brain metastases. Nat Rev Dis Primers. https://doi.org/10.1038/s41572-018-0055-y
Agarwal S et al (2012) Breast cancer resistance protein and P-glycoprotein in brain cancer: two gatekeepers team up. Curr Pharm Des. https://doi.org/10.2174/138161211797440186
Akimoto J (2016) Photodynamic therapy for malignant brain tumors. Neurol Med Chir. https://doi.org/10.2176/nmc.ra.2015-0296
Aldape K et al (2019) Challenges to curing primary brain tumours. Nat Rev Clin Oncol. https://doi.org/10.1038/s41571-019-0177-5
Alifieris C, Trafalis DT (2015) Glioblastoma multiforme: pathogenesis and treatment. Pharmacol Therapeutic. https://doi.org/10.1016/j.pharmthera.2015.05.005
Allison RR, Sibata CH (2010) Oncologic photodynamic therapy photosensitizers: a clinical review. Photodiagnosis Photodyn Ther. https://doi.org/10.1016/j.pdpdt.2010.02.001
Amelio D, Amichetti MA (2012) Radiation therapy for the treatment of recurrent glioblastoma: an overview. Cancer. https://doi.org/10.3390/cancers4010257
Amsbaugh, M. J. and Kim, C. S. (2019) Cancer, brain metastasis, StatPearls.
Aronica E et al (2005) Localization of breast cancer resistance protein (BCRP) in microvessel endothelium of human control and epileptic brain. Epilepsia 46(6):849–857
Arvanitis CD et al (2018) Mechanisms of enhanced drug delivery in brain metastases with focused ultrasound-induced blood–tumor barrier disruption. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1807105115
Barani IJ, Larson DA (2015) Radiation therapy of glioblastoma. Cancer Treat Res. https://doi.org/10.1007/978-3-319-12048-5_4
Bartsch R et al (2015) Activity of T-DM1 in Her2-positive breast cancer brain metastases. Clin Exp Metastasis. https://doi.org/10.1007/s10585-015-9740-3
Basit S et al (2017) European journal of medicinal chemistry first macrocyclic 3rd-generation ALK inhibitor for treatment of ALK / ROS1 cancer: clinical and designing strategy update of lorlatinib. Eur J Med Chem 134:348–356. https://doi.org/10.1016/j.ejmech.2017.04.032. Elsevier Masson SAS
Bastien JIL, McNeill KA, Fine HA (2015) Molecular characterizations of glioblastoma, targeted therapy, and clinical results to date. Cancer. https://doi.org/10.1002/cncr.28968
Bauer TM et al (2020) Brain penetration of lorlatinib: cumulative incidences of CNS and non-CNS progression with lorlatinib in patients with previously treated ALK-positive non-small-cell lung cancer. Target Oncol. https://doi.org/10.1007/s11523-020-00702-4
Baumert C, Hilgeroth A (2012) Recent advances in the development of P-gp inhibitors. Anticancer Agents Med Chem. https://doi.org/10.2174/1871520610909040415
Bellavance MA, Blanchette M, Fortin D (2008) Recent advances in blood-brain barrier disruption as a CNS delivery strategy. AAPS J. https://doi.org/10.1208/s12248-008-9018-7
Bhagavathi S, Wilson JD (2008) Primary central nervous system lymphoma. Arch Pathol Lab Med. https://doi.org/10.1043/1543-2165-132.11.1830
Bhardwaj RK et al (2006) The functional evaluation of human peptide/histidine transporter 1 (hPHT1) in transiently transfected COS-7 cells. Eur J Pharm Sci. https://doi.org/10.1016/j.ejps.2005.09.014
Bhatia P et al (2012) Breast cancer resistance protein (BCRP/ABCG2) localises to the nucleus in glioblastoma multiforme cells. Xenobiotica. 2012/03/10 42(8):748–755. https://doi.org/10.3109/00498254.2012.662724
Bi WL, Beroukhim R (2014) Beating the odds: extreme long-term survival with glioblastoma. Neuro Oncol. https://doi.org/10.1093/neuonc/nou166
Blakeley J (2008) Drug delivery to brain tumors. Curr Neurol Neurosci Rep. https://doi.org/10.1007/s11910-008-0036-8
Blakeley JO et al (2009) Effect of blood brain barrier permeability in recurrent high grade gliomas on the intratumoral pharmacokinetics of methotrexate: a microdialysis study. J Neurooncol. https://doi.org/10.1007/s11060-008-9678-2
Bleau AM et al (2009) PTEN/PI3K/Akt pathway regulates the side population phenotype and ABCG2 activity in glioma tumor stem-like cells. Cell Stem Cell 4(3):226–235. https://doi.org/10.1016/j.stem.2009.01.007
Boado RJ et al (2010) IgG-single chain Fv fusion protein therapeutic for Alzheimer’s disease: expression in CHO cells and pharmacokinetics and brain delivery in the Rhesus monkey. Biotechnol Bioeng. https://doi.org/10.1002/bit.22576
Brennan CW et al (2013) The somatic genomic landscape of glioblastoma. Cell. 2013/10/15 155(2):462–477. https://doi.org/10.1016/j.cell.2013.09.034
Bruzzone MG et al (2012) CT and MRI of brain tumors. Q J Nucl Med Mol Imaging
Bui K et al (2016) The effect of quinidine, a strong P-glycoprotein inhibitor, on the pharmacokinetics and central nervous system distribution of naloxegol. J Clin Pharmacol. https://doi.org/10.1002/jcph.613
Bunevicius A, McDannold NJ, Golby AJ (2020) Focused ultrasound strategies for brain tumor therapy. Oper Neurosurg. https://doi.org/10.1093/ons/opz374
Calias P et al (2014) Intrathecal delivery of protein therapeutics to the brain: a critical reassessment. Pharmacol Therapeutic. https://doi.org/10.1016/j.pharmthera.2014.05.009
Cardoso FL, Brites D, Brito MA (2010) Looking at the blood-brain barrier: molecular anatomy and possible investigation approaches. Brain Res Rev. Elsevier B.V 64(2):328–363. https://doi.org/10.1016/j.brainresrev.2010.05.003
Castedo M et al (2004) Cell death by mitotic catastrophe: a molecular definition. Oncogene. https://doi.org/10.1038/sj.onc.1207528
Castro M et al (2001) High-affinity sodium-vitamin C co-transporters (SVCT) expression in embryonic mouse neurons. J Neurochem. https://doi.org/10.1046/j.1471-4159.2001.00461.x
Chamberlain MC et al (2014) A phase 2 trial of verubulin for recurrent glioblastoma: a prospective study by the brain tumor investigational consortium (BTIC). J Neurooncol. https://doi.org/10.1007/s11060-014-1437-y
Chen JS et al (2006) EGFR regulates the side population in head and neck squamous cell carcinoma. Laryngoscope. 2006/03/17 116(3):401–406. https://doi.org/10.1097/01.mlg.0000195075.14093.fb
Cho HS et al (2016) Localized down-regulation of P-glycoprotein by focused ultrasound and microbubbles induced blood-brain barrier disruption in rat brain. Sci Rep. Nature Publishing Group 6(May):1–10. https://doi.org/10.1038/srep31201
Chowdhary S, Chamberlain M (2013) Bevacizumab for the treatment of glioblastoma. Expert Rev Neurother. https://doi.org/10.1586/14737175.2013.827414
Cloughesy TF, Cavenee WK, Mischel PS (2014) Glioblastoma: from molecular pathology to targeted treatment. https://doi.org/10.1146/annurev-pathol-011110-130324
Cooray HC et al (2002) Localisation of breast cancer resistance protein in microvessel endothelium of human brain. Neuroreport. https://doi.org/10.1097/00001756-200211150-00014
Cordon-Cardo C et al (1989) Multidrug-resistance gene (P-glycoprotein) is expressed by endothelial cells at blood-brain barrier sites. Proc Natl Acad Sci 86:695–698. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC286540/pdf/pnas00242-0297.pdf
Cramer SW, Chen CC (2020) Photodynamic therapy for the treatment of glioblastoma. Front Surg. https://doi.org/10.3389/fsurg.2019.00081
Davis ME (2016) HHS public access. 20(5):1–14. https://doi.org/10.1188/16.CJON.S1.2-8.Glioblastoma
de Trizio I et al (2020) Expression of P-gp in glioblastoma: what we can learn from brain development. Curr Pharm Des. https://doi.org/10.2174/1381612826666200318130625
Debinski W, Tatter SB (2009) Convection-enhanced delivery for the treatment of brain tumors. Expert Rev Neurother. https://doi.org/10.1586/ern.09.99
Delattre JY et al (1988) Distribution of brain metastases. Arch Neurol. https://doi.org/10.1001/archneur.1988.00520310047016
Demeule M et al (2001) Expression of multidrug-resistance p-glycoprotein (MDR1) in human brain tumors. Int J Cancer 93:62–66
Dempke WCM et al (2015) Brain metastases in NSCLC-are TKIs changing the treatment strategy? Anticancer Res
Deng Z, Sheng Z, Yan F (2019) Ultrasound-induced blood-brain-barrier opening enhances anticancer efficacy in the treatment of glioblastoma: current status and future prospects. J Oncol. https://doi.org/10.1155/2019/2345203
Drappatz J et al (2013) Phase I study of GRN1005 in recurrent malignant glioma. Clin Cancer Res 19(6):1567–1576. Available at: http://clincancerres.aacrjournals.org/content/19/6/1567.abstract
Dubey RK et al (1989) Plasma binding and transport of diazepam across the blood-brain barrier. No evidence for in vivo enhanced dissociation. J Clin Investig. https://doi.org/10.1172/JCI114279
Durant ST et al (2018) The brain-penetrant clinical ATM inhibitor AZD1390 radiosensitizes and improves survival of preclinical brain tumor models. Sci Adv. https://doi.org/10.1126/sciadv.aat1719
Eisenblaetter T, Galla H-J (2002) A new multidrug resistance protein at the blood–brain barrier. Biochem Biophys Res Commun 293:1273–1278
El-Osta A et al (2002) Precipitous release of methyl-CpG binding protein 2 and histone deacetylase 1 from the methylated human multidrug resistance gene (MDR1) on activation. Mol Cell Biol 22(6):1844–1857. https://doi.org/10.1128/mcb.22.6.1844-1857.2002
Emery IF et al (2017) Expression and function of ABCG2 and XIAP in glioblastomas. J Neurooncol. 2017/04/23 133(1):47–57. https://doi.org/10.1007/s11060-017-2422-z
Eskilsson E et al (2018) EGFR heterogeneity and implications for therapeutic intervention in glioblastoma. Neuro Oncol. 2017/10/19 20(6):743–752. https://doi.org/10.1093/neuonc/nox191
Ewend MG et al (2007) Treatment of single brain metastasis with resection, intracavity carmustine polymer wafers, and radiation therapy is safe and provides excellent local control. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-06-2095
Fokas E, Steinbach JP, Rödel C (2013) Biology of brain metastases and novel targeted therapies: time to translate the research. Biochim Biophys Acta Rev Cancer. https://doi.org/10.1016/j.bbcan.2012.10.005
Fox E, Bates SE (2007) Tariquidar (XR9576): a P-glycoprotein drug efflux pump inhibitor. Expert Rev Anticancer Ther. https://doi.org/10.1586/14737140.7.4.447
Fridén M et al (2009) Development of a high-throughput brain slice method for studying drug distribution in the central nervous system. Drug Metab Dispos. https://doi.org/10.1124/dmd.108.026377
Fridén M et al (2011) Measurement of unbound drug exposure in brain: modeling of pH partitioning explains diverging results between the brain slice and brain homogenate methods. Drug Metab Dispos. https://doi.org/10.1124/dmd.110.035998
Gadgeel S et al (2018) Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALKþ) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol. https://doi.org/10.1093/annonc/mdy405
Gaillard PJ et al (2014) Pharmacokinetics, brain delivery, and efficacy in brain tumor-bearing mice of glutathione pegylated liposomal doxorubicin (2B3-101). PLoS One. https://doi.org/10.1371/journal.pone.0082331
Gampa G et al (2020) Influence of transporters in treating cancers in the CNS. In: Drug efflux pumps in cancer resistance pathways: from molecular recognition and characterization to possible inhibition strategies in chemotherapy. https://doi.org/10.1016/b978-0-12-816434-1.00009-7
Gil ES et al (2009) Quaternary ammonium β-cyclodextrin nanoparticles for enhancing doxorubicin permeability across the in vitro blood-brain barrier. Biomacromolecules. https://doi.org/10.1021/bm801026k
Ginguene C et al (2010) P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2) localize in the microvessels forming the blood-tumor barrier in ependymomas. Brain Pathol. 2010/04/22 20(5):926–935. https://doi.org/10.1111/j.1750-3639.2010.00389.x
Gottesman MM (2002) Mechanisms of cancer drug resistance. Annu Rev Med. https://doi.org/10.1146/annurev.med.53.082901.103929
Grossman R et al (2013) Microdialysis measurement of intratumoral temozolomide concentration after cediranib, a pan-VEGF receptor tyrosine kinase inhibitor, in a U87 glioma model. Cancer Chemother Pharmacol. https://doi.org/10.1007/s00280-013-2172-3
Hammarlund-Udenaes M et al (2008) On the rate and extent of drug delivery to the brain. Pharm Res. https://doi.org/10.1007/s11095-007-9502-2
Han SR et al (2015) Effect and mechanism of peroxisome proliferator-activated receptor-gamma on the drug resistance of the U-87 MG/CDDP human malignant glioma cell line. Molecular Mol Med Rep 12(2):2239–2246. https://doi.org/10.3892/mmr.2015.3625
Harmsen S et al (2013) PXR-mediated P-glycoprotein induction by small molecule tyrosine kinase inhibitors. Eur J Pharm Sci 48(4–5):644–649. https://doi.org/10.1016/j.ejps.2012.12.019
Harper JW, Elledge SJ (2007) The DNA damage response: ten years after. Mol Cell. https://doi.org/10.1016/j.molcel.2007.11.015
Hartz AMS, Mahringer A et al (2010a) 17-beta-Estradiol: a powerful modulator of blood-brain barrier BCRP activity. J Cereb Blood Flow Metab 30(10):1742–1755. https://doi.org/10.1038/jcbfm.2010.36
Hartz AMS, Madole EK et al (2010b) Estrogen receptor beta signaling through phosphatase and tensin homolog/phosphoinositide 3-kinase/Akt/glycogen synthase kinase 3 down-regulates blood-brain barrier breast cancer resistance protein. J Pharmacol Exp Ther 334(2):467–476. https://doi.org/10.1124/jpet.110.168930
Hawkins BT et al (2010) The blood-brain barrier / neurovascular unit in health and disease. Neurobiol Dis. Elsevier B.V 64(1):13–25. https://doi.org/10.1016/j.brainresrev.2010.05.003
Heffron TP (2016) Small molecule kinase inhibitors for the treatment of brain cancer. J Med Chem:10030–10066. https://doi.org/10.1021/acs.jmedchem.6b00618
Heffron TP et al (2016) Discovery of clinical development candidate GDC-0084, a brain penetrant inhibitor of PI3K and mTOR. ACS Med Chem Lett. https://doi.org/10.1021/acsmedchemlett.6b00005
Hellmann-Regen J et al (2012) Retinoic acid as target for local pharmacokinetic interaction with modafinil in neural cells. Eur Arch Psychiatry Clin Neurosci 262(8):697–704. https://doi.org/10.1007/s00406-012-0309-8
Hoeijmakers JHJ (2009) DNA damage, aging, and cancer. N Engl J Med. https://doi.org/10.1056/NEJMra0804615
Huang FF et al (2013) Inactivation of PTEN increases ABCG2 expression and the side population through the PI3K/Akt pathway in adult acute leukemia. Cancer Lett. 2013/04/23 336(1):96–105. https://doi.org/10.1016/j.canlet.2013.04.006
Huang J et al (2014) Regenerating gene family member 4 promotes growth and migration of gastric cancer through protein kinase B pathway. Int J Clin Exp Med 7(9):3037–3044
Huisman MT et al (2003) Assessing safety and efficacy of directed P-glycoprotein inhibition to improve the pharmacokinetic properties of saquinavir coadministered with ritonavir. J Pharmacol Experiment Therapeutic. https://doi.org/10.1124/jpet.102.044388
Hunt Bobo R et al (1994) Convection-enhanced delivery of macromolecules in the brain. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.91.6.2076
J.G., P.-L et al (2011) Temozolomide in elderly patients with newly diagnosed glioblastoma and poor performance status: An ANOCEF phase II trial. J Clin Oncol. https://doi.org/10.1200/JCO.2011.34.8086LK. http://onesearch.unifi.it/openurl/39UFI/39UFI_Services?&sid=EMBASE&issn=0732183X&id=doi:10.1200%2FJCO.2011.34.8086&atitle=Temozolomide+in+elderly+patients+with+newly+diagnosed+glioblastoma+and+poor+performance+status%3A+An+ANOCEF+phase+II+trial&stitle=J.+Clin.+Oncol.&title=Journal+of+Clinical+Oncology&volume=29&issue=22&spage=3050&epage=3055&aulast=P%C3%A9rez-Larraya&aufirst=Jaime+G%C3%A1llego&auinit=J.G.&aufull=P%C3%A9rez-Larraya+J.G.&coden=JCOND&isbn=&pages=3050-
Jackson S et al (2016) The effect of regadenoson-induced transient disruption of the blood-brain barrier on temozolomide delivery to normal rat brain. J Neurooncol. 2015/12/03 126(3):433–439. https://doi.org/10.1007/s11060-015-1998-4
Jackson S et al (2017) The effect of regadenoson on the integrity of the human blood–brain barrier, a pilot study. J Neurooncol. https://doi.org/10.1007/s11060-017-2404-1
Jackson S et al (2018) The effect of an adenosine A2A agonist on intra-tumoral concentrations of temozolomide in patients with recurrent glioblastoma. Fluid Barrier CNS. 2018/01/16 15(1):2. https://doi.org/10.1186/s12987-017-0088-8
Johnson RA, Ince TA, Scotto KW (2001) Transcriptional repression by p53 through direct binding to a novel DNA element. J Biol Chem. 2001/05/15 276(29):27716–27720. https://doi.org/10.1074/jbc.C100121200
Karaoglu Hanzatian D et al (2018) Brain uptake of multivalent and multi-specific DVD-Ig proteins after systemic administration. MAbs. https://doi.org/10.1080/19420862.2018.1465159
Keith KC et al (2016) Activity of trastuzumab-emtansine (TDM1) in HER2-positive breast cancer brain metastases: A case series. Cancer Treat Commun. https://doi.org/10.1016/j.ctrc.2016.03.005
Kemper EM et al (2004) Modulation of the blood-brain barrier in oncology: therapeutic opportunities for the treatment of brain tumours? Cancer Treat Rev. https://doi.org/10.1016/j.ctrv.2004.04.001
Kim DG, Bynoe MS (2015) A2A Adenosine Receptor Regulates the Human Blood-Brain Barrier Permeability. Mol Neurobiol. 2014/09/30 52(1):664–678. https://doi.org/10.1007/s12035-014-8879-2
Kim DG, Bynoe MS (2016) A2A adenosine receptor modulates drug efflux transporter P-glycoprotein at the blood-brain barrier. J Clin Invest. 2016/04/05 126(5):1717–1733. https://doi.org/10.1172/JCI76207
Kim M et al (2018) Barriers to effective drug treatment for brain metastases: a multifactorial problem in the delivery of precision medicine. Pharm Res. https://doi.org/10.1007/s11095-018-2455-9
Kim M et al (2019a) Brain distribution of a panel of epidermal growth factor receptor inhibitors using cassette dosing in wild-type and ABCB1/ABCG2-deficient mice. Drug Metab Dispos. https://doi.org/10.1124/dmd.118.084210
Kim SS et al (2019b) A tumor-targeting nanomedicine carrying the p53 gene crosses the blood–brain barrier and enhances anti-PD-1 immunotherapy in mouse models of glioblastoma. Int J Cancer. https://doi.org/10.1002/ijc.32531
Kondo S et al (1996) mdm2 gene mediates the expression of mdrl gene and P-glycoprotein in a human glioblastoma cell line. Br J Cancer 74:1263–1268
Korshunov A et al (1999) Prognostic value of immunoexpression of the chemoresistance-related proteins in ependymomas: an analysis of 76 cases. J Neurooncol 45:219–227
Kroll RA et al (1998) Improving drug delivery to intracerebral tumor and surrounding brain in a rodent model: a comparison of osmotic versus bradykinin modification of the blood-brain and/or blood-tumor barriers. Neurosurgery. United States 43(4):879
Kuang Y et al (2013) T7 peptide-functionalized nanoparticles utilizing RNA interference for glioma dual targeting. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2013.07.019
Kunwar S et al (2010) Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol. https://doi.org/10.1093/neuonc/nop054
Kuppens IELM et al (2007) A phase I, randomized, open-label, parallel-cohort, dose-finding study of elacridar (GF120918) and oral topotecan in cancer patients. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-06-2414
Kurzrock R et al (2012) Safety, pharmacokinetics, and activity of GRN1005, a novel conjugate of angiopep-2, a peptide facilitating brain penetration, and paclitaxel, in patients with advanced solid tumors. Mol Cancer Ther. https://doi.org/10.1158/1535-7163.MCT-11-0566
Laack NN, Brown PD (2004) Cognitive sequelae of brain radiation in adults. Semin Oncol. https://doi.org/10.1053/j.seminoncol.2004.07.013
Lambert JM, Chari RVJ (2014) Ado-trastuzumab emtansine (T-DM1): an antibody-drug conjugate (ADC) for HER2-positive breast cancer. J Med Chem. https://doi.org/10.1021/jm500766w
Laramy JK et al (2017) Heterogeneous binding and central nervous system distribution of the multitargeted kinase inhibitor ponatinib restrict orthotopic efficacy in a patient-derived xenograft model of glioblastoma. J Pharmacol Exp Ther. https://doi.org/10.1124/jpet.117.243477
Lee SY (2016) Temozolomide resistance in glioblastoma multiforme. Genes and Diseases. https://doi.org/10.1016/j.gendis.2016.04.007
Lee J et al (2019) Flexible, sticky, and biodegradable wireless device for drug delivery to brain tumors. Nat Commun. https://doi.org/10.1038/s41467-019-13198-y
Levin AB, Duff TA, Javid MJ (1979) Treatment of increased intracranial pressure: a comparison of different hyperosmotic agents and the use of thiopental. Neurosurgery. https://doi.org/10.1227/00006123-197911000-00005
Li J et al (2017) Quantitative and mechanistic understanding of AZD1775 penetration across human blood-brain barrier in glioblastoma patients using an IVIVE-PBPK modeling approach. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-17-0983
Lim M et al (2019) Innovative therapeutic strategies for effective treatment of brain metastases. Int J Mol Sci. https://doi.org/10.3390/ijms20061280
Lin X, DeAngelis LM (2015) Treatment of brain metastases. J Clin Oncol. https://doi.org/10.1200/JCO.2015.60.9503
Liu HL et al (2014) Combining microbubbles and ultrasound for drug delivery to brain tumors: current progress and overview. Theranostics. https://doi.org/10.7150/thno.8074
Liu Q, Tong X, Wang J (2019) Management of brain metastases: history and the present. Chin Neurosurg J. https://doi.org/10.1186/s41016-018-0149-0
Liu EK et al (2020) Novel therapies for glioblastoma. Curr Neurol Neurosci Rep. https://doi.org/10.1007/s11910-020-01042-6
Lonser RR et al (2015) Convection-enhanced delivery to the central nervous system. J Neurosurg. https://doi.org/10.3171/2014.10.JNS14229
Lord CJ, Ashworth A (2012) The DNA damage response and cancer therapy. Nature. https://doi.org/10.1038/nature10760
Loryan I, Fridén M, Hammarlund-Udenaes M (2013) The brain slice method for studying drug distribution in the CNS. Fluid Barrier CNS. https://doi.org/10.1186/2045-8118-10-6
Löscher W, Potschka H (2005) Blood-brain barrier active efflux transporters: ATP-binding cassette gene family. NeuroRx: J Am Soc Experiment NeuroTherapeutic 2(1):86–98. https://doi.org/10.1602/neurorx.2.1.86
Lyon JG et al (2017) Engineering challenges for brain tumor immunotherapy. Adv Drug Deliv Rev. https://doi.org/10.1016/j.addr.2017.06.006
Mack F et al (2016) Therapy of leptomeningeal metastasis in solid tumors. Cancer Treat Rev. https://doi.org/10.1016/j.ctrv.2015.12.004
Mahmoudi K et al (2019) 5-aminolevulinic acid photodynamic therapy for the treatment of high-grade gliomas. J Neurooncol. https://doi.org/10.1007/s11060-019-03103-4
Mamelak AN et al (2006) Phase I single-dose study of intracavitary-administered iodine-131-TM-601 in adults with recurrent high-grade glioma. J Clin Oncol. https://doi.org/10.1200/JCO.2005.05.4569
Mani S et al (2005) Activation of the steroid and xenobiotic receptor (human pregnane X receptor) by nontaxane microtubule-stabilizing agents. Clin Cancer Res 11(17):6359–6369. https://doi.org/10.1158/1078-0432.CCR-05-0252
Mani S, Dou W, Redinbo MR (2013) PXR antagonists and implication in drug metabolism. Drug Metab Rev 45(1):60–72. https://doi.org/10.3109/03602532.2012.746363
Marroni M et al (2003) Relationship between expression of multiple drug resistance proteins and p53 tumor suppressor gene proteins in human brain astrocytes. Neuroscience. https://doi.org/10.1016/S0306-4522(03)00515-3
McClelland S et al (2018) Application of tumor treating fields for newly diagnosed glioblastoma: understanding of nationwide practice patterns. J Neurooncol. https://doi.org/10.1007/s11060-018-2945-y
McNeill KA (2016) Epidemiology of brain tumors. Neurol Clin. https://doi.org/10.1016/j.ncl.2016.06.014
Meng Y et al (2018) Low-intensity MR-guided focused ultrasound mediated disruption of the blood-brain barrier for intracranial metastatic diseases. Front Oncol. https://doi.org/10.3389/fonc.2018.00338
Munoz JL et al (2014) Temozolomide induces the production of epidermal growth factor to regulate MDR1 expression in glioblastoma cells. Mol Cancer Ther 13(10):2399–2411. https://doi.org/10.1158/1535-7163.Mct-14-0011
Murthy R et al (2018) Tucatinib with capecitabine and trastuzumab in advanced HER2-positive metastatic breast cancer with and without brain metastases: a non-randomised, open-label, phase 1b study. Lancet Oncol. https://doi.org/10.1016/S1470-2045(18)30256-0
Murthy RK et al (2020) Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. https://doi.org/10.1056/NEJMoa1914609
Nakanishi T, Ross DD (2012) Breast cancer resistance protein (BCRP/ABCG2): its role in multidrug resistance and regulation of its gene expression. Chin J Cancer 31(2):73–99. https://doi.org/10.5732/cjc.011.10320
Nakanishi T, Shiozawa K, Hamburger AW (2006) Bcrp expression is functionally upregulated by epidermal growth factor receptor (EGFR, ERBB1) mediated signaling in human ovarian cancer cell lines, but not in human breast cancer cell lines. AACR Meeti Abstract 146
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep. https://doi.org/10.1007/s11912-011-0203-y
Neuwelt EA (1980) Reversible osmotic blood-brain barrier disruption in humans: implications for the chemotherapy of malignant brain tumors. Neurosurgery:204. https://doi.org/10.1097/00006123-198008000-00018
Neyns B et al (2009) Stratified phase II trial of cetuximab in patients with recurrent high-grade glioma. Ann Oncol. https://doi.org/10.1093/annonc/mdp032
Niwińska A, Rudnicka H, Murawska M (2015) Breast cancer leptomeningeal metastasis: The results of combined treatment and the comparison of methotrexate and liposomal cytarabine as intra-cerebrospinal fluid chemotherapy. Clin Breast Cancer. https://doi.org/10.1016/j.clbc.2014.07.004
O’Connor MJ (2015) Targeting the DNA damage response in cancer. Mol Cell. https://doi.org/10.1016/j.molcel.2015.10.040
Oberoi RK et al (2016) Strategies to improve delivery of anticancer drugs across the blood-brain barrier to treat glioblastoma. Neuro-Oncology:27–36. https://doi.org/10.1093/neuonc/nov164
Okines A et al (2018) Development and responses of brain metastases during treatment with trastuzumab emtansine (T-DM1) for HER2 positive advanced breast cancer: A single institution experience. Breast J. https://doi.org/10.1111/tbj.12906
Oliveira M et al (2011) Complete response in HER2+ leptomeningeal carcinomatosis from breast cancer with intrathecal trastuzumab. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-011-1417-2
Omidi Y, Barar J (2012) Impacts of blood-brain barrier in drug delivery and targeting of brain tumors. Bioimpacts. https://doi.org/10.5681/bi.2012.002
Ostrom QT et al (2014) The epidemiology of glioma in adults: a state of the science review. Neuro Oncol. https://doi.org/10.1093/neuonc/nou087
Ostrom QT et al (2019) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro Oncol. https://doi.org/10.1093/neuonc/noz150
Pan-Weisz TM et al (2019) Patient-reported health-related quality of life outcomes in supportive-care interventions for adults with brain tumors: a systematic review. Psychooncology. https://doi.org/10.1002/pon.4906
Pardridge WM (2016) CSF, blood-brain barrier, and brain drug delivery. Expert Opin Drug Deliv. https://doi.org/10.1517/17425247.2016.1171315
Pardridge WM, Eisenberg J, Yang J (1985) Human blood—brain barrier insulin receptor. J Neurochem. https://doi.org/10.1111/j.1471-4159.1985.tb07167.x
Pardridge WM, Eisenberg J, Yang J (1987) Human blood-brain barrier transferrin receptor. Metabolism. https://doi.org/10.1016/0026-0495(87)90099-0
Parrish KE, Sarkaria JN, Elmquist WF (2015) Improving drug delivery to primary and metastatic brain tumors: strategies to overcome the blood-brain barrier. Clinic Pharmacol Therapeutic:336–346. https://doi.org/10.1002/cpt.71
Pearl LH et al (2015) Therapeutic opportunities within the DNA damage response. Nat Rev Cancer. https://doi.org/10.1038/nrc3891
Perissinotti AJ, Reeves DJ (2010) Role of intrathecal rituximab and trastuzumab in the management of leptomeningeal carcinomatosis. Ann Pharmacother. https://doi.org/10.1345/aph.1P197
Perkins A, Liu G (2016) Primary brain tumors in adults: Diagnosis and treatment. Am Fam Physician
Perria C, Capuzzo T, Cavagnaro G (1980) First attempts at the photodynamic treatment of human gliomas. J Neurosurg Sci
Perus LJM, Walsh LA (2019) Microenvironmental heterogeneity in brain malignancies. Front Immunol. https://doi.org/10.3389/fimmu.2019.02294
Porter KR et al (2010) Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro Oncol. https://doi.org/10.1093/neuonc/nop066
Portnow J et al (2009) The neuropharmacokinetics of temozolomide in patients with resectable brain tumors: potential implications for the current approach to chemoradiation. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-09-1349
Puris E et al (2020) L-Type amino acid transporter 1 as a target for drug delivery. Pharm Res. https://doi.org/10.1007/s11095-020-02826-8
Ramalingam SS et al (2020) Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med. https://doi.org/10.1056/NEJMoa1913662
Rankovic Z (2015) CNS drug design: balancing physicochemical properties for optimal brain exposure. J Med Chem:2584–2608. https://doi.org/10.1021/jm501535r
Rankovic Z (2017) CNS physicochemical property space shaped by a diverse set of molecules with experimentally determined exposure in the mouse brain. J Med Chem:5943–5954. https://doi.org/10.1021/acs.jmedchem.6b01469
Rapoport SI (2000) Osmotic opening of the blood-brain barrier: principles, mechanism, and therapeutic applications. Cell Mol Neurobiol. https://doi.org/10.1023/A:1007049806660
Rapoport SI, Hori M, Klatzo I (1972) Testing of a hypothesis for osmotic opening of the blood-brain barrier. Am J Physiol. https://doi.org/10.1152/ajplegacy.1972.223.2.323
Reungwetwattana T et al (2018) CNS response to osimertinib versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-mutated advanced non-small-cell lung cancer’, Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2018.78.3118
Ricciardi GRR et al (2018) Efficacy of T-DM1 for leptomeningeal and brain metastases in a HER2 positive metastatic breast cancer patient: New directions for systemic therapy - a case report and literature review. BMC Cancer. https://doi.org/10.1186/s12885-018-3994-5
Rick JW et al (2019) Systemic therapy for brain metastases. Crit Rev Oncol Hematol. https://doi.org/10.1016/j.critrevonc.2019.07.012
Riganti C et al (2013) Temozolomide downregulates P-glycoprotein expression in glioblastoma stem cells by interfering with the Wnt3a/glycogen synthase-3 kinase/beta-catenin pathway. Neuro Oncol. 2013/07/31 15(11):1502–1517. https://doi.org/10.1093/neuonc/not104
Sakata S et al (2011) ATP-binding cassette transporters in primary central nervous system lymphoma: Decreased expression of MDR1 P-glycoprotein and breast cancer resistance protein in tumor capillary endothelial cells. Oncol Rep 25(2):333–339. https://doi.org/10.3892/or.2010.1102
Salphati L et al (2012) Targeting the PI3K pathway in the brain - efficacy of a PI3K inhibitor optimized to cross the blood-brain barrier. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-12-0720
Sampath J et al (2001) Mutant p53 cooperates with ETS and selectively up-regulates human MDR1 Not MRP1. J Biol Chem. https://doi.org/10.1074/jbc.M103429200
Sandler A et al (2004) A phase I trial of a potent P-glycoprotein inhibitor, zosuquidar trihydrochloride (LY335979), administered intravenously in combination with doxorubicin in patients with advanced malignancy. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-03-0644
Sarkadi B et al (2006) Human multidrug resistance ABCB and ABCG transporters: participation in a chemoimmunity defense system. Physiol Rev. https://doi.org/10.1152/physrev.00037.2005
Sarkaria JN et al (2018) Is the blood-brain barrier really disrupted in all glioblastomas? A critical assessment of existing clinical data. Neuro Oncol. https://doi.org/10.1093/neuonc/nox175
Shapira-Furman T et al (2019) Biodegradable wafers releasing Temozolomide and Carmustine for the treatment of brain cancer. J Control Release. https://doi.org/10.1016/j.jconrel.2018.12.048
Sharma J, Lv H, Gallo JM (2012) Analytical approach to characterize the intratumoral pharmacokinetics and pharmacodynamics of gefitinib in a glioblastoma model. J Pharm Sci. https://doi.org/10.1002/jps.23283
Sharma J, Lv H, Gallo JM (2013) Intratumoral modeling of gefitinib pharmacokinetics and pharmacodynamics in an orthotopic mouse model of glioblastoma. Cancer Res. https://doi.org/10.1158/0008-5472.CAN-13-0690
Shaw AT et al (2017) Alectinib versus crizotinib in treatment-naive advanced ALK -positive non-small cell lung cancer (NSCLC): primary results of the global phase III ALEX study. J Clin Oncol. https://doi.org/10.1200/jco.2017.35.18_suppl.lba9008
Shawahna R et al (2011) Transcriptomic and quantitative proteomic analysis of transporters and drug metabolizing enzymes in freshly isolated human brain microvessels. Mol Pharm. https://doi.org/10.1021/mp200129p
Shen F et al (2008) Quantitation of doxorubicin uptake, efflux, and modulation of multidrug resistance (MDR) in MDR human cancer cells. J Pharmacol Experiment Therapeutic. https://doi.org/10.1124/jpet.107.127704
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin. https://doi.org/10.3322/caac.21551
Soria JC et al (2018) Osimertinib in untreated EGFR-Mutated advanced non-small-cell lung cancer. N Engl J Med. https://doi.org/10.1056/NEJMoa1713137
Sperduto PW et al (2012) Summary report on the graded prognostic assessment: An accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. https://doi.org/10.1200/JCO.2011.38.0527
Spiegl-Kreinecker S et al (2002) Expression and functional activity of the ABC-transporter proteins P-glycoprotein and multidrug-resistance protein 1 in human brain tumor cells and astrocytes. J Neurooncol 57:27–36
St-Amour I et al (2013) Brain bioavailability of human intravenous immunoglobulin and its transport through the murine blood-brain barrier. J Cereb Blood Flow Metab. https://doi.org/10.1038/jcbfm.2013.160
Stupp R (2019) Changing paradigms in the treatment of brain metastases. J Oncol Pract. https://doi.org/10.1200/JOP.19.00602
Stupp R et al (2008) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma – a critical review. Clinic Med Oncol. https://doi.org/10.1056/NEJMoa043330
Sugawara M et al (2010) Expressions of cytochrome P450, UDP-glucuronosyltranferase, and transporter genes in monolayer carcinoma cells change in subcutaneous tumors grown as xenografts in immunodeficient nude mice. Drug Metab Dispos 38(3):526–533. https://doi.org/10.1124/dmd.109.030668
Sun M, Chen Y, Hu B (2018) The inhibition of DNA damage response contributes to cancer radiotherapy. 5(1):149–156. https://doi.org/10.17554/j.issn.2313-3406.2018.05.47
Sutherlin DP et al (2010) Discovery of (thienopyrimidin-2-yl)aminopyrimidines as potent, selective, and orally available Pan-PI3-kinase and dual Pan-PI3-kinase/mTOR inhibitors for the treatment of cancer. J Med Chem 53(3):1086–1097. https://doi.org/10.1021/jm901284w
Takada T et al (2005) Regulation of the cell surface expression of human BCRP/ABCG2 by the phosphorylation state of Akt in polarized cells. Drug Metab Dispos. 2005/04/22 33(7):905–909. https://doi.org/10.1124/dmd.104.003228
Tanaka Y et al (1994) Ultrastructural localization of P-glycoprotein on capillary endothelial cells in human gliomas. Virchows Arch 425:133–138
Tews DS et al (2000) Drug resistance-associated factors in primary and secondary glioblastomas and their precursor tumors. J Neurooncol 50:227–237
Timbie KF, Mead BP, Price RJ (2015) Drug and gene delivery across the blood-brain barrier with focused ultrasound. J Control Release. https://doi.org/10.1016/j.jconrel.2015.08.059
Toms SA et al (2019) Increased compliance with tumor treating fields therapy is prognostic for improved survival in the treatment of glioblastoma: a subgroup analysis of the EF-14 phase III trial. J Neurooncol. https://doi.org/10.1007/s11060-018-03057-z
Toth K et al (1996) MDR1 P-Glycoprotein Is Expressed by Endothelial Cells of Newly Formed Capillaries in Human Gliomas but Is Not Expressed in the Neovasculature of Other Primary Tumors. Am J Pathol 149:853–858
Tran PN, Klempner SJ (2017) ALK on my mind: Alectinib takes an early lead in managing intracranial disease in non-small cell lung cancer with ALK rearrangements. Ann Trans Med. https://doi.org/10.21037/atm.2017.03.47
Trédan O et al (2007) Drug resistance and the solid tumor microenvironment. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djm135
Uchida Y et al (2011) Blood-Brain Barrier (BBB) pharmacoproteomics: Reconstruction of in vivo brain distribution of 11 P-glycoprotein substrates based on the BBB transporter protein concentration, in vitro intrinsic transport activity, and unbound fraction in plasma and brain. J Pharmacol Experiment Therapeutic. https://doi.org/10.1124/jpet.111.184200
Uchida Y et al (2015) Major involvement of Na + -dependent multivitamin transporter (SLC5A6/SMVT) in uptake of biotin and pantothenic acid by human brain capillary endothelial cells. J Neurochem. https://doi.org/10.1111/jnc.13092
Ueno M et al (2010) The expression of LDL receptor in vessels with blood-brain barrier impairment in a stroke-prone hypertensive model. Histochem Cell Biol. https://doi.org/10.1007/s00418-010-0705-y
Valera ET et al (2007) Quantitative PCR analysis of the expression profile of genes related to multiple drug resistance in tumors of the central nervous system. J Neurooncol. 2007/04/13 85(1):1–10. https://doi.org/10.1007/s11060-007-9382-7
Van Den Bent MJ et al (2009) Randomized phase II trial of erlotinib versus temozolomide or carmustine in recurrent glioblastoma: EORTC brain tumor group study 26034. J Clin Oncol. https://doi.org/10.1200/JCO.2008.17.5984
Van Den Bent M et al (2020) INTELLANCE 2/EORTC 1410 randomized phase II study of Depatux-M alone and with temozolomide vs temozolomide or lomustine in recurrent EGFR amplified glioblastoma. Neuro Oncol. https://doi.org/10.1093/neuonc/noz222
Veringa SJ et al (2013) In vitro drug response and efflux transporters associated with drug resistance in pediatric high grade glioma and diffuse intrinsic pontine glioma. PLoS One. 2013/05/03 8(4):e61512. https://doi.org/10.1371/journal.pone.0061512
Vogelbaum MA, Aghi MK (2015) Convection-enhanced delivery for the treatment of glioblastoma. Neuro Oncol. https://doi.org/10.1093/neuonc/nou354
Vu CU et al (2014) Nicotinic acetylcholine receptors in glucose homeostasis: the acute hyperglycemic and chronic insulin-sensitive effects of nicotine suggest dual opposing roles of the receptors in male mice. Endocrinology. https://doi.org/10.1210/en.2014-1320
Wager TT et al (2010) Moving beyond rules: the development of a central nervous system multiparameter optimization (CNS MPO) approach to enable alignment of druglike properties. ACS Chem Nerosci 1(6):435–449. https://doi.org/10.1021/cn100008c
Wager TT et al (2016) Central nervous system multiparameter optimization desirability: application in drug discovery. ACS Chem Nerosci. https://doi.org/10.1021/acschemneuro.6b00029
Wang S et al (2008) Preclinical pharmacokinetic/pharmacodynamic models of gefitinib and the design of equivalent dosing regimens in EGFR wild-type and mutant tumor models. Mol Cancer Ther. https://doi.org/10.1158/1535-7163.MCT-07-2070
Weaver M, Laske DW (2003) Transferrin receptor ligand-targeted toxin conjugate (Tf-CRM107) therapy of malignant gliomas. J Neurooncol. https://doi.org/10.1023/A:1026246500788
Wei X et al (2014) Brain tumor-targeted drug delivery strategies. Acta Pharm Sin B. https://doi.org/10.1016/j.apsb.2014.03.001
Weller M et al (2015) Glioma. Nat Rev Dis Primers. https://doi.org/10.1038/nrdp.2015.17
Wen PY et al (2020) First-in-human phase i study to evaluate the brain-penetrant PI3K/mTOR inhibitor GDC-0084 in patients with progressive or recurrent high-grade glioma. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-19-2808
Wolinsky JB, Colson YL, Grinstaff MW (2012) Local drug delivery strategies for cancer treatment: gels, nanoparticles, polymeric films, rods, and wafers. J Control Release. https://doi.org/10.1016/j.jconrel.2011.11.031
Wu Y et al (2019) MicroRNA-302c enhances the chemosensitivity of human glioma cells to temozolomide by suppressing P-gp expression. Biosci Rep. 2019/08/15 39(9). https://doi.org/10.1042/BSR20190421
Xu S et al (2013) Targeting receptor-mediated endocytotic pathways with nanoparticles: rationale and advances. Adv Drug Deliv Rev. https://doi.org/10.1016/j.addr.2012.09.041
Yan A et al (2019) CD73 promotes glioblastoma pathogenesis and enhances its chemoresistance via A(2B) adenosine receptor signaling. J Neurosci 39(22):4387–4402. https://doi.org/10.1523/jneurosci.1118-18.2019
Yasuda M et al (2019) The Involvement of Pregnane X Receptor-regulated Pathways in the Antitumor Activity of Cisplatin. Anticancer Res 39(7):3601–3608. https://doi.org/10.21873/anticanres.13507
Zeng Q et al (2015) Discovery and evaluation of clinical candidate AZD3759, a potent, oral active, central nervous system-penetrant, epidermal growth factor receptor tyrosine kinase inhibitor. J Med Chem 58(20):8200–8215. https://doi.org/10.1021/acs.jmedchem.5b01073
Zhang Y, Pardridge WM (2001) Mediated efflux of IgG molecules from brain to blood across the blood-brain barrier. J Neuroimmunol. https://doi.org/10.1016/S0165-5728(01)00242-9
Zhang W et al (2003) Expression and functional characterization of ABCG2 in brain endothelial cells and vessels. FASEB J. https://doi.org/10.1096/fj.02-1131fje
Zhou J et al (2006) Reversal of P-glycoprotein-mediated multidrug resistance in cancer cells by the c-Jun NH2-terminal kinase. Cancer Res 66(1):445–452. https://doi.org/10.1158/0008-5472.CAN-05-1779
Zhou Z, Singh R, Souweidane M (2016) Convection-enhanced delivery for diffuse intrinsic pontine glioma treatment. Curr Neuropharmacol. https://doi.org/10.2174/1570159x14666160614093615
Zong T et al (2014) Enhanced glioma targeting and penetration by dual-targeting liposome co-modified with T7 and TAT. J Pharm Sci. https://doi.org/10.1002/jps.24186
Acknowledgments
This work was supported by the National Institutes of Health [Grants RO1 NS107548, U54 CA210180, U01 CA227954]. The authors would also like to thank the editors of the book for their comments and valuable inputs.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Talele, S. et al. (2022). Drug Delivery to Primary and Metastatic Brain Tumors: Challenges and Opportunities. In: de Lange, E.C., Hammarlund-Udenaes, M., Thorne, R.G. (eds) Drug Delivery to the Brain. AAPS Advances in the Pharmaceutical Sciences Series, vol 33. Springer, Cham. https://doi.org/10.1007/978-3-030-88773-5_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-88773-5_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-88772-8
Online ISBN: 978-3-030-88773-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)