Abstract
The goal of economic evaluation is to determine whether a new or updated intervention maximizes health benefits to children and families for every dollar spent compared to the standard of care. In this chapter the basic concepts and methods of economic evaluation are introduced, including cost item identification, measurement and valuation; description of modelling approaches, study perspective and time horizon; and definitions of cost effectiveness and cost utility analyses. This chapter also includes a review of studies that evaluated the cost-effectiveness of Early Intensive Behavioral intervention (EIBI) in autism spectrum disorder (ASD). While the economic evaluations of EIBI are scarce, existing studies show that EIBI can be costly, but may result in cost savings to a public payer due to a reduction in the use of services such as special education or adult assistance programs. None of the studies which reported both incremental costs and outcomes was conducted alongside an observational study or an RCT. Prospective research should be conducted to evaluate the long-term effectiveness of alternative EIBI programs with clearly defined comparator and control groups, collection of resource use across different service sectors, and with preference-based health-related quality of life assessment incorporated in the design.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Economic evaluation
- EIBI
- Early intensive behavioural intervention
- Cost-effectiveness analysis
- Funding decision-making
Introduction
Should Early Intensive Behavioral Intervention (EIBI) be administered to all children with autism spectrum disorder (ASD) or just those most severely affected? What type of EIBI approach should be used? Should speech-language services and parent delivery models be integrated into the EIBI program? These are the kinds of questions that ASD policymakers are grappling with as the incidence of ASD climbs. Regrettably, there is not an unlimited supply of money to pay for all potentially beneficial services. An efficient allocation of resources requires that a choice be made among services options. It is the goal of health economic evaluation to determine which option is the most economically efficient, i.e., that maximizes benefits to children and families for every dollar spent. Every dollar invested in a particular program or service takes a dollar away from the next best possible use of that money, thus poor allocation of budgets results in waste and lost benefits. In this chapter the basic concepts and methods of economic evaluation are introduced and studies that have evaluated the cost-effectiveness of EIBI in ASD are presented and reviewed. Finally, suggestions for expanding and improving economic evaluation of EIBI are proposed.
Defining Economic Evaluation
An economic evaluation is defined as a comparison of two or more interventions in terms of both costs and health consequences. In the comparison of interventions, the inputs are the costs associated with resources consumed. With respect to ASD, these resources can be related to health, education, social services and community services. These are weighed against the outputs, which are the improvements in health, function, quality of life or other dimensions observed as a consequence of consuming the relevant resources. Simply measuring the volume of resources, such as the number of days spent with a behavioural therapist, or what this costs, is never the endpoint in an economic evaluation. The goal is to determine whether these resources resulted in improvement in health status, and whether that improvement represents good value for money.
In economic evaluation, typically a new or updated treatment approach is compared to standard care. One or more comparators must always be stipulated in economic evaluation. Thus, the costs and consequences of the new treatment are measured in comparison to the standard care and possibly other treatment alternatives. The two most common analytic approaches to economic evaluation are cost-effectiveness analysis (CEA) and cost-utility analysis (CUA). CEA measures outcomes in natural health units. Examples at the person-level include scores on functional measures such as the Vineland Adaptive Behavior Scales, 2nd Edition (VABS-II), a measure of child adaptive behaviour in communication, daily living skills, motor and socialization domains (Sparrow et al., 2005). At the population level, an outcome might be the number of cases successfully treated with the EIBI program of interest. The precise choice of outcome measure may vary between studies, complicating comparisons between them. The problem of disparate outcomes is solved by using a common metric. In CUA, the quality-adjusted life year (QALY) is used. The QALY is a composite measure that considers not only the life years achieved for any given intervention, but also the health-related quality of life that the person experiences during those life years. The health-related quality of life effects are used as a weight to adjust the observed life expectancy. Knowing there is an improvement in quality-adjusted life years, not just the number of life years, is an important consideration when making an allocation decision. A significant advantage of the QALY is that it allows comparisons not only across different studies, but across different patient groups and therapeutic areas. For that reason it is considered a universal outcome measure and is recommended by economic evaluation guidelines (CADTH, 2017; Neumann et al., 2017). Despite the allure of the universal metric, CUAs are often difficult to carry out in children with ASD as available measures may not have the appropriate performance characteristics or sensitivity to detect clinically important changes.
If compared to standard care a new intervention is more costly and not as effective, then it is dominated by standard care and is clearly not a worthy investment. If the intervention saves money and results in better outcomes compared to standard care, then it is surely worth adopting. The remaining scenarios are the ones for which economic evaluation is most critical—when the intervention is less costly but also less effective or when the intervention is more costly but also more effective than standard care.
The Research Question
The first step in an economic evaluation is to specify a research question which flows from a problem identified by a relevant stakeholder such as clinical or policy decision-maker and addresses a gap in existing evidence. Begin by:
-
Identifying a gap in the evidence base
-
Stating the study purpose and rationale
-
Identifying the target knowledge user audience
-
Posing a clear research question in terms of costs, outcomes, comparators, perspective and target population
Costing
An economic evaluation weighs the additional costs of a new intervention against any added benefits, compared to standard care. While ‘benefits’ may be represented in terms of a single effectiveness variable such as QALYs, the cost consists of many cost item variables, all of which must be properly combined to accurately represent the costs of individuals receiving an intervention. The costing process is comprised of these steps often requiring extensive data collection (Jacobs & Roos, 1999):
-
1.
Cost item identification
-
2.
Cost item measurement
-
3.
Valuation
Cost Item Identification
The cost items that are included in an economic evaluation are broadly grouped into three categories: (1) direct ASD care-related costs; (2) direct patient/family (out-of-pocket) costs and (3) indirect costs. It is important to know about consumption of all ASD-related services used during the period of EIBI that may affect the outcomes of interest. Unlike the majority of health economic evaluations, studies in ASD require enumeration of resources that are not only related to healthcare (e.g. developmental pediatrician), but also to education (e.g. classroom support workers), community services (e.g. special education daycare programs) and social services (e.g. parent respite) (Genereaux et al., 2016; Ungar et al., 2018; Volden et al., 2015). Depending on how ASD programs are structured, families are likely to incur direct out-of-pocket costs to receive services or may have some services covered by insurance. Out-of-pocket costs can be considerable and pose a financial burden for some families over a short or long interval (Barrett et al., 2012; Horlin et al., 2014). A large out-of-pocket expenditure burden may influence how families choose health and other types of services and it’s therefore important that these cost items not be overlooked. The third category of cost items are the indirect costs, also referred to as productivity costs. In addition to paying out-of-pocket for some or all ASD services, parents and other caregivers can miss time from work and other activities to attend to the child with ASD. These time losses can be substantial (Tsiplova et al., 2019). Examples of cost items included in an economic evaluation of EIBI are listed in Table 1.
Cost Item Measurement
For every cost item, two variables are relevant: the volume of use and the unit price. Cost item measurement refers to collecting the necessary data related to both volume of use and price for each item. Accurately measuring volumes of resource use across multiple sectors requires a valid tool with sufficient breadth to capture relevant services and resources. The tool should also capture how the service is paid for, such as by a publicly subsidized program, private insurance or out-of-pocket. It is often expedient to consider “piggy-backing” an economic evaluation onto a planned clinical trial of a new EIBI treatment and administer the tool alongside other clinical trial instruments. Prospective data collection may be supplemented by retrospective data collection from patient charts and health plan administrative databases.
Unit prices for identified resources can often be obtained from existing sources such as fee schedules for physicians and clinical psychologists and drug formularies. The tool used to collect resource use data should also collect the prices paid by parents for goods and services purchased out-of-pocket. In collecting and assigning prices to cost items, one must be aware of the difference between prices and charges. The best value for prices is the one that represents the true value, or opportunity cost of the good or service, before any mark-ups or taxes are added.
Omitting indirect or time costs from an economic evaluation can bias the result if these costs are significant, such as in the case of parents caring for their children with ASD. It is preferable to collect these data prospectively from parents, with repeated assessments as needed. Just as prices represent the value of goods and services, in the human capital approach, wages represent the value of time (Liljas, 1998). Using reported wages to value time losses may affect the validity of the findings if time loss contributes significantly to total cost. An alternative approach is to value reported time losses by average national statistical wages. These data, stratified by age, sex and occupation, may be available from national census data sources.
Cost Valuation
When stochastic data have been collected for each study participant i, cost valuation begins at the level of the individual. The cost of each item is valued by multiplying price (p) by person-level resource use, or quantity (qi). For indirect costs, the unit price is represented by hourly or daily wage and the quantity of resource use by the parent or caregiver’s hours or days lost. Once the volumes and prices for all items are determined, a vector of total costs per person can be calculated as follows:
The total cost for participant i equals the sum of price multiplied by quantity for all cost items j, where the range of j extends from 1 through n cost items. With a total cost per person, descriptive statistics can be determined including mean and standard deviation of the total costs for each comparator group. Additional statistics, such as median, interquartile range and minimum and maximum are also informative, particularly when cost data are not normally distributed. Differences in the mean cost per patient between groups can be tested for statistical significance using an inferential test that is appropriate for the data.
In addition to descriptive statistics on total costs per person for each group, it may be useful to compare the mean costs per person for each major cost item or category, such as EIBI costs, health services costs, or educational costs. Another useful descriptive statistic is the percent contribution of each major cost category to total costs.
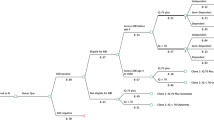
The above discussion of cost valuation assumes that stochastic data are available for individual study subjects. For many economic evaluations this is not the case, and instead costing proceeds based on a hypothetical, well described cohort of children with ASD. For cost item measurement and valuation, probabilities of use of each of the cost items are determined for strata that represent different outcomes, such the sub-groups of children representing different levels of severity (and hence consume different volumes of resource use). Probabilities are obtained from the literature and a decision model is built using the principles of decision analysis (Drummond et al., 2015).
Study Perspective
The cost items to be included in an economic evaluation are determined by the payer perspective of the analysis. The choice of perspective should consider the research question and the target audience. As information about EIBI cost-effectiveness is used by ASD program decision-makers to determine whether to pay for a new service or intervention, a public payer perspective (including health, education and other publicly subsidized services) is a common approach. It may be appropriate to take a wider perspective that encompasses costs incurred by the public payer as well as by private third party insurers. In jurisdictions where the target population may be mostly uninsured, or when families bear a substantial portion of intervention costs, then a patient or family perspective is also appropriate.
Not included in any of the conventional perspectives are the indirect costs. Time losses incurred to parents and caregivers are included only in a societal perspective. For a decision that affects a large health planning region, such as the number and location of EIBI delivery sites, the principal decision-maker is the ASD program manager. While this decision-maker may be principally concerned with the program’s budget and expenditures, the decision-maker must recognize that depending on the location of these services, parents may have to travel long distances to have their children receive care, incurring out-of-pocket costs as well as indirect productivity costs. Including a societal perspective alongside other perspectives can be highly informative and is recommended (Ungar, 2010). How cost items are mapped to different payer perspectives is indicated in Table 1.
Outcome Measurement
The choice of effectiveness measure may represent the goals of the intervention, such as VABS-II domains or other functional measures. While CEAs enable the specification of a variety of outcomes, effective EIBI can have significant impacts on a child’s health-related quality of life (HRQoL). There is a wide array of structured psychometrically valid HRQoL instruments available. These instruments typically consist of a series of closed-ended questions grouped in domains such as physical functioning, emotion, cognitive function, social interactions, and general health.
When HRQoL is expected to be an important outcome in a prospective economic evaluation, it is ideal to measure it with a valid preference-based instrument. A preference-based instrument elicits an individual’s utility, or preference, for a given health state, based on the classic conceptual domains of HRQoL. These utilities are then applied as weights to a child’s life expectancy for the calculation of QALYs (Drummond et al., 2015). As described above, QALYs are a universal and therefore, a powerful outcome measure. Because differences in QALYs between groups will be observed as long as the quality of life effects are present, QALYs can be performed even when life expectancy is not expected to change. It should also be noted that utility is difficult to ascertain in certain vulnerable populations, such as young children with ASD or cognitive impairment. The researcher must rely on a proxy reporter in these cases, such as a parent, who may have an imperfect perception of the individual’s health state preferences (Ungar, 2011).
In a study comparing two preference-based HRQoL instruments in children with ASD, the Health Utilities Index (HUI)3 was more sensitive and responsive to clinical changes in adaptive and cognitive function compared to the Quality of Well-Being scale (Tilford et al., 2012). While preference-based instruments are increasingly becoming available to generate utilities for pediatric health states, including pediatric-specific measures (Stevens, 2011; Wille et al., 2010), the wide heterogeneity in presentation of symptoms in children with ASD makes it challenging to assign utility weights for particular health states compared to other pediatric conditions (Payakachat et al., 2012). While generic instruments are useful for comparing quality-of-life effects across diverse populations, they may be too blunt to detect small but clinically important changes in function. Incorporating both a generic and a disease-specific quality of life measure into a prospective study is therefore often a useful strategy.
Time Horizon
In designing an economic evaluation, one must also specify the duration of time for measurement of costs and health consequences. Although the period of EIBI coincides with a child’s pre-school years, an effective program may demonstrate long-lasting benefits experienced over the lifetime though reduced need for educational supports and social services, greater workforce participation, and greater functional independence during the adult years. A mismatch between the timing of costs and timing of benefits of EIBI can be problematic for ASD program decision-makers who wish to support EIBI investment. Analysts must distinguish between costs and outcomes that occur today versus those that are deferred into the future. This is handled by applying a discount rate to costs and outcomes when they are measured over a year or more. The same constant rate should be applied to both costs and consequences and this rate is typically 1–5%, reflecting society’s rate of positive time preference (CADTH, 2017).
It becomes clear that when long time horizons are needed, the ability to collect all necessary long-term data on resource use and outcomes becomes extremely challenging. Good quality data can come from longitudinal cohorts of children with ASD exposed to different types of EIBI programs provided that sufficient details regarding the EIBI programs and other resources used are collected in addition to outcomes.
Cost-Effectiveness Analysis
As described at the start of this chapter, a cost-effectiveness analysis is a full economic evaluation whereby both costs and consequences of programs or treatments are examined, the outcomes are measured in natural units (e.g., VABS-II score) and are common to all comparators. The results of a CEA are expressed as the incremental cost per unit of effectiveness, e.g. dollars per unit of improvement in adaptive function.
The unit of analysis for costs and outcomes is often the child. When the measure of effectiveness is a proportion, such as the percent of children achieving a clinically significant response, it can be easier for decision-makers to interpret the analysis if the costs and outcomes are scaled to a group of 100 or 1000 patients.
The point estimates of the means for each treatment group are represented in an incremental cost-effectiveness ratio (ICER):
The numerator of the ICER is the difference in mean costs between the experimental intervention and standard care (or another comparator). The denominator expresses the difference in mean outcomes between comparators. By subtracting the mean values for costs and outcomes of standard care from the intervention, one can determine the added or incremental costs associated with the intervention per unit of added or incremental benefit achieved. ICERs therefore allow the direct comparison of two comparators in terms of costs and outcomes. If data on life expectancy and utility related to treatments are available, then a CUA that examines the incremental cost per QALY gained can be conducted.
A separate analysis should be conducted for each payer perspective (public payer, family, societal) whereby the total cost estimate is varied. It may also be useful to conduct separate analyses for hypothetical sub-groups of children that are clinically distinct, e.g. by age group, diagnostic sub-type or presence of comorbid conditions. The analysis inputs would then be customized for these sub-groups.
Uncertainty
Economic evaluations require large amounts of accurate data. In the case of missing or uncertain data, assumptions are needed. For example, if behavioural therapist salaries are not available for the jurisdiction where the work is being performed, then wages from a neighboring region or a similar profession may be used with the assumption that the values are similar. When data on the frequency of longer term outcomes, the magnitude of quality of life improvements or other variables are not available, a panel of experts might be convened to provide estimates based on their practices. However, consulting experts should only be considered if consensus is anticipated based on their depth of knowledge and experience. If there is too much uncertainty, it may not be possible to conduct a reliable analysis.
Assumptions may be needed for the point estimate of a variable or for the upper and lower bounds that are used to indicate the precision of the point estimate. For every study, a researcher must state all assumptions explicitly, with a rationale for the values used in the analysis. Sensitivity analysis is employed to assess the sensitivity of the incremental costs, incremental effects and the ICER to changes in the underlying assumptions.
Advanced probabilistic techniques can be used which directly incorporate uncertainty into the analysis. In a probabilistic analysis, a point estimate and a range, often the 95% confidence intervals or standard deviations, are specified for every variable, along with a distribution (e.g. normal, beta, gamma, log-normal, uniform) (Briggs et al., 2006). Through Monte Carlo simulation, the data are sampled 5000 times or more. Each iteration produces values for incremental costs, incremental benefits and ICERs. From the 5000 samplings of the data, a probability that the intervention is cost-effective can be deduced. This is essentially the proportion of ICERs that demonstrate the intervention to be more effective and less costly than the standard care alternative.
Because of the inherent uncertainty in economic evaluation, the results of sensitivity analyses are as important as presenting the primary results. Sensitivity analyses convey additional important evidence that allows the target user to judge their confidence in the allocation decision that flows from the findings.
Synthesis, Reporting and Knowledge Translation
The final step is to ensure that the evidence gets into the hands of the decision-makers who need it. Ideally these individuals, representing clinical, institutional or jurisdictional decision-makers, will be involved as a partner from the first step of articulating the research question. Reporting back closes the loop to provide the necessary evidence.
Often the decision-maker wishes to determine whether a new intervention is cost-effective, i.e. make a value-for-money decision, under varying thresholds for willingness-to-pay. A decision-maker may have a higher or lower threshold for willingness-to-pay for any given intervention depending on the jurisdiction, societal values regarding the health gains and who is incurring them, and the available budget.
To determine the net monetary benefit of an intervention, a decision-makers’ willingness-to-pay threshold, say $50,000 for a QALY gain, is assigned. If a new intervention yields QALY gains that when converted to dollars with the selected threshold yield more benefits than costs, then the intervention is deemed cost-effective. If the willingness-to-pay for a QALY gain is very high, then there is a high probability than the monetary health benefits will exceed the costs.
The issue of generalizability to other populations or other jurisdictions must also be addressed, particularly if the final report is widely disseminated. Any plans to update the analysis, for example, in the event that novel approaches to EIBI are introduced, should be described.
In a society with complex health, education and social service systems, families of children with ASD expect the very best in care. This includes timely access to state-of-the-art treatments and services. At the same time, the North American population is aging and consuming more health care while growing economic pressures put constraints on public spending. In the widening gap between the demand for high quality ASD services and the availability of limited resources to deliver that care, opportunistic inequities can arise. The answer is not to spend more on services, but to increase efficiency and consume only the resources that have demonstrated benefits. Health economic evaluation helps to reduce inequity and inefficiency by producing evidence that allows decision-makers to make allocation decisions that maximize benefits for dollars spent.
Economic Evaluations of Early Intensive Behavioural Intervention
To illustrate the application of economic evaluation methods to interventions in ASD, a review of key studies evaluating the cost-effectiveness of EIBI as well as studies comparing costs of early intervention programs was conducted. The methods and results of each study included in the review are summarized in Tables 2 and 3, respectively.
The reported target population was primarily children with ASD, but occasionally included children with unspecified developmental delay. Eligible age ranges were 2–6 years of age (i.e. preschool aged children) for most studies. Two studies that assessed the Early Start Denver Model (ESDM) included children aged 15–30 months (Penner et al., 2015; Cidav et al., 2017). The cost savings or outcome gains of EIBI were estimated until age of retirement (65 years), with some studies having a much shorter time horizon: 2 years (Tsiplova et al., 2019), follow-up to 6 years (Cidav et al., 2017) and 4–22 years (Chasson et al., 2007). Of the eight studies reviewed, five were cost analyses with no outcomes reported and three reported the incremental changes in both costs and outcomes. The latter CEA studies used a decision analysis approach. Costs were measured from a public payer perspective in all studies, while societal costs were additionally estimated in four studies and only one study measured costs to families (Tsiplova et al., 2019). Among all studies, the breadth of sectors considered was wide and included costs associated with health, educational and community services. The authors of the three cost-effectiveness analyses measured outcomes as dependency-free life years gained to age 65. No study conducted a cost utility analysis.
Several studies (Jacobson et al., 1998; Motiwala et al., 2006; Chasson et al., 2007; Peters-Scheffer et al., 2012) calculated representative costs of EIBI and other related autism services and in some studies modified published efficacy rates of EIBI (Lovaas, 1987) to estimate long-term cost savings of EIBI per child with ASD per unit of functional improvement. It was assumed that children with ASD who received EIBI would be more likely to achieve normal to semi-dependent functioning compared to children with did not receive EIBI and therefore would require less continued ASD services, such as special education, respite services and other child and adult support programs.
The total costs savings of EIBI and comparators varied due to study differences in model time horizons, types of costs included, settings and efficacy rates. In Motiwala et al. (2006), the authors used published estimates of both direct and indirect costs of EIBI and other ASD services, including adult care, and showed that an expansion of EIBI program to all eligible children in Ontario, Canada was dominant, resulting in cost savings to the public sector (over $45 million in 2003 CAD) and gains in dependency-free life years of 4.5 years per person compared to no EIBI, and gains of 2.8 years per person compared to EIBI provision for severely affected individuals until age 65 years. Using IQ as a measure of dependency and including both direct and indirect costs, (Penner et al., 2015) showed that the pre-diagnosis intensive ESDM with or without parental involvement administered to toddlers aged 15–36 months with undifferentiated developmental concerns was cost-effective compared to status quo treatment. From a societal perspective, the pre-diagnosis ESDM was dominant, resulting in $45,000 (2015 CAD) in savings per person and an additional 0.53 dependency-free life years compared to the status quo. Another cost-effectiveness analysis from the same research team (Piccininni et al., 2017) examined whether reducing or eliminating wait times for EIBI in Ontario, Canada could result in cost savings and gains in dependency-free life years. The authors found that compared with a current wait time of 32 months, eliminating wait time was the least costly and most effective strategy, resulting in cost savings of $52,976 (2017 CAD) and more than $267,000 (2017 CAD) per individual over the lifetime (to age 65 years) from both public and societal perspectives, respectively and resulted in an incremental benefit of 2.52 dependency-free life years. However, this study failed to account for the significant costs that would be required to expand capacity to reduce or eliminate the wait time.
The review identified two cost analyses which were conducted prospectively alongside a randomized controlled trial (RCT) or as an observational study. In Cidav et al. (2017), authors used data from an RCT of children with ASD aged 18–30 months who were assigned to either ESDM delivered for 2 years or the usual community care and who were followed until 6 years of age. During the intervention, parent-reported health-related costs were higher for the ESDM group. Post-intervention, total ASD-related service costs were significantly lower due to reduced use of applied behavioural analysis (ABA)/EIBI, speech therapy, and occupational/physical therapy services, resulting in cost savings of about $19,000 (2017 USD) per child. In a prospective observational study comparing two provincial EIBI programs in New Brunswick and Nova Scotia, Canada, researchers collected multi-sectoral service use and cost data from parents for 12 months prior to and during a first year of EIBI (Tsiplova et al., 2019). The authors found significant differences between New Brunswick and Nova Scotia with respect to the utilization of services and costs to families, the public sector and society. The annual costs of EIBI per child were estimated to be $29,015 (2017 CAD) in New Brunswick and $90,200 (2017 CAD) in Nova Scotia. The program in Nova Scotia, while more expensive, was delivered in family homes and daycare and included speech language therapy services, which reduced out-of-pocket, travel and productively losses for the families in Nova Scotia relative to families in New Brunswick. The wait times for EIBI were shorter in New Brunswick than in Nova Scotia, which meant that most parents in Nova Scotia sought and used extensive services prior to receiving EIBI.
This review illustrates that there is a lack of published economic evaluations of EIBI. To date, studies that reported both incremental costs and outcomes used decision analysis, with none conducted alongside an observational study or an RCT recruiting children with ASD. The review did not include cost-of-illness studies which measured the general costs of health, community, and/or education services for preschool- or school-aged individuals with ASD (Lavelle et al., 2014; Cidav et al., 2013; Peacock et al., 2012; Horlin et al., 2014), since such studies did not focus on EIBI or other early intervention programs and were not comparative.
Methodologic Challenges
EIBI and other applied behavioural analysis approaches to early intervention vary widely in structure, intensity, and duration of treatment (Smith, 2014). The optimal study design for ascertaining effectiveness, as well as cost-effectiveness, of alternative approaches to treatment is an RCT. However, the literature review found that RCTs of EIBI are virtually non-existent. There are many challenges to conducting RCTs in children for any therapeutic indication (Council of Canadian Academies, 2014) and it may be particularly difficult to enroll children with a spectrum disorder such as autism that manifest their symptoms with wide heterogeneity (Reichow et al., 2018). Observing a treatment effect of EIBI in children with ASD would require a very large sample. Moreover, detecting the effects of treatment would require a lengthy observation period that extended at minimum over the preschool years of development. Observational study designs that enroll and continue to observe children with ASD over time may offer advantages with respect to a large sample size and longer follow-up period. However, since children who received EIBI and those did not might differ in terms of clinical and demographic characteristics, collected data would be exposed to potential confounding. In addition, in a longer follow-up, attrition may be substantial. Furthermore, since such studies often compare EIBI programs offered in a community setting, participating children may be accessing services of varying intensity and fidelity. It is essential that in observational studies of EIBI programs, comparator and control group are well defined and data are collected on the intensity and duration of EIBI services. Another challenge that is particularly relevant for economic evaluation relates to the fact that ASD is a condition that is not primarily treated in the health sector. Initial assessment and diagnosis may be performed by a developmental pediatrician or a clinical psychologist, and the primary mode of treatment is behavioural, not biomedical. Parents typically access ASD services and programs in the health, education, community and social service sectors. Prospective studies must use valid tools that can capture the breadth of ASD-related services (Ungar et al., 2018). The wide range of services accessed by parents also points to the need to consider multiple payer perspectives in economic evaluations of EIBI, including the public sector (consisting of health, education, social and community services), the family, to allow for an accounting of the financial burden on families, and society as a whole, so that indirect productivity costs—often substantial for parents and informal care providers—can be included.
The present literature review revealed a preponderance of modeling studies using decision analysis, which are common in economic evaluation. While these designs are expedient and do not require prospective data collection, they are severely constrained by the availability of data on costs and outcomes from published studies. Thus, decision models risk oversimplifying resource use and outcomes for children with ASD, do not allow sub-groups comparisons, and are associated with extensive uncertainty, particularly when constructed over long time horizons. Better quality representations of ASD can be constructed with health-state transition (Markov) models that assign a utility and costs to individual health states, but these data require substantially more input data on health states that change over time compared to decision trees and none such studies were found.
Economic evaluations of EIBI are jurisdictional by design—they aim to synthesize evidence on costs and outcomes to serve a policy decision-maker for a particular region or health plan. The paucity of high quality economic evidence for policy decision-makers has undoubtedly contributed to the wide variation in programs observed across jurisdictions (Volden et al., 2015; L & M Policy Research, 2014). Depending on the geographic region or health plan, the policy question may differ. When multiple jurisdictions or health plans require evidence of EIBI program effectiveness for optimal EIBI program design and delivery, it may be possible to transfer economic results by omitting irrelevant cost items, adjusting the payer and/or performing currency conversion.
Despite these enormous challenges, prospective research should be conducted to evaluate the effectiveness of alternative EIBI program designs, with the collection of resource use and preference-based health-related quality of life data incorporated in the design. Interest in newer naturalistically-based, early-start, and parent-mediated approaches to EIBI is growing and these options may have important impacts on resource use and productivity (Ip et al., 2019; Smith, 2014). Prospective well-designed comparisons of newer approaches to more conventional EIBI are essential. The evidence base for EIBI programs must grow substantially to enable the conduct of high quality economic to inform funding decisions.
Conclusions
The evidence base for economic evaluations of EIBI remains sparse, with an urgent need for high quality prospective evaluations to ensure that allocation of limited public payer or health plan funds are optimized. The challenges of conducting such studies are not trivial, but adherence to basic principles of study design as delineated in this chapter, will greatly facilitate such research.
In addition to economic evaluations of EIBI, evidence of cost-effectiveness of alternative approaches to ASD screening, ASD assessment and diagnosis, use of genetic testing to aid diagnosis, educational supports and adult interventions are urgently needed. ASD is a lifelong disorder; although costs of pre-school EIBI may appear high to payers, these costs are slight compared to the costs of long-term residential care for the most severely affected during the many decades of adult life (Motiwala et al., 2006). If pre-school EIBI is effective in promoting learning and consequently enabling greater workforce participation and independent living for even a small percentage of moderately and severely affected persons with ASD, then there is the potential for net savings to payers and health plans. But the most-cost effective approach to EIBI remains to be elucidated.
References
Barrett, B., Byford, S., Sharac, J., Hudry, K., Leadbitter, K., Temple, K., Aldred, C., Slonims, V., & Green, J. (2012). Service and wider societal costs of very young children with autism in the UK. Journal of Autism and Developmental Disorders, 42(5), 797–804. https://doi.org/10.1007/s10803-011-1306-x
Briggs, A., Claxton, K., & Sculpher, M. (2006). Decision modelling for health economic evaluation. In Handbooks in health economic evaluation. Oxford University Press.
CADTH. (2017). Guidelines for the economic evaluation of health technologies: Canada (4th ed.). CADTH.
Chasson, G. S., Harris, G. E., & Neely, W. J. (2007). Cost comparison of Early Intensive Behavioral Intervention and special education for children with autism. Journal of Child and Family Studies, 16(3), 401–413. https://doi.org/10.1007/s10826-006-9094-1
Cidav, Z., Lawer, L., Marcus, S. C., & Mandell, D. S. (2013). Age-related variation in health service use and associated expenditures among children with autism. Journal of Autism and Developmental Disorders, 43(4), 924–931. https://doi.org/10.1007/s10803-012-1637-2
Cidav, Z., Munson, J., Estes, A., Dawson, G., Rogers, S., & Mandell, D. (2017). Cost offset associated with Early Start Denver Model for children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 56(9), 777–783. https://doi.org/10.1016/j.jaac.2017.06.007
Council of Canadian Academies. (2014). Improving medicines for children in Canada. The Expert Panel on Therapeutic Products for Infants, Children, and Youth, Council of Canadian Academies.
Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., & Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes (4th ed.). Oxford University Press.
Genereaux, D., Bansback, N., & Birch, P. (2016). Development and pilot testing of a tool to calculate parental and societal costs of raising a child with intellectual disability. Journal of Intellectual & Developmental Disability, 41(1), 11–20. https://doi.org/10.3109/13668250.2015.1087479
Horlin, C., Falkmer, M., Parsons, R., Albrecht, M. A., & Falkmer, T. (2014). The cost of autism spectrum disorders. PLoS One, 9(9), e106552. https://doi.org/10.1371/journal.pone.0106552
Ip, A., Zwaigenbaum, L., & Brian, J. A. (2019). Post-diagnostic management and follow-up care for autism spectrum disorder. Paediatrics & Child Health, 24(7), 461–477. https://doi.org/10.1093/pch/pxz121
Jacobs, P., & Roos, N. P. (1999). Standard cost lists for healthcare in Canada. Issues in validity and inter-provincial consolidation. PharmacoEconomics, 15(6), 551–560. https://doi.org/10.2165/00019053-199915060-00003
Jacobson, J. W., Mulick, J. A., & Green, G. (1998). Cost–benefit estimates for early intensive behavioral intervention for young children with autism—general model and single state case. Behavioral Interventions, 13(4), 201–226. https://doi.org/10.1002/(SICI)1099-078X(199811)13:4<201::AID-BIN17>3.0.CO;2-R
L & M Policy Research. (2014). Autism spectrum disorders (ASD): State of the states of services and supports for people with ASD. Centers for Medicare and Medicaid Services.
Lavelle, T. A., Weinstein, M. C., Newhouse, J. P., Munir, K., Kuhlthau, K. A., & Prosser, L. A. (2014). Economic burden of childhood autism spectrum disorders. Pediatrics, 133(3), e520–e529. https://doi.org/10.1542/peds.2013-0763
Liljas, B. (1998). How to calculate indirect costs in economic evaluations. PharmacoEconomics, 13(1 pt 1), 1–7. https://doi.org/10.2165/00019053-199,813,010-00001
Lovaas, O. I. (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55(1), 3–9. https://doi.org/10.1037/0022-006x.55.1.3
Motiwala, S. S., Gupta, S., Lilly, M. B., Ungar, W. J., & Coyte, P. C. (2006). The cost-effectiveness of expanding intensive behavioural intervention to all autistic children in Ontario. Health Policy, 1(2), 135–151.
Neumann, P. J., Sanders, G. D., Russell, L. B., Siegel, J. E., & Ganiats, T. G. (2017). Cost-effectiveness in health and medicine (2nd ed.). Oxford University Press.
Payakachat, N., Tilford, J. M., Kovacs, E., & Kuhlthau, K. (2012). Autism spectrum disorders: A review of measures for clinical, health services and cost-effectiveness applications. Expert Review of Pharmacoeconomics & Outcomes Research, 12(4), 485–503. https://doi.org/10.1586/erp.12.29
Peacock, G., Amendah, D., Ouyang, L., & Grosse, S. D. (2012). Autism spectrum disorders and health care expenditures: The effects of co-occurring conditions. Journal of Developmental and Behavioral Pediatrics, 33(1), 2–8. https://doi.org/10.1097/DBP.0b013e31823969de
Penner, M., Rayar, M., Bashir, N., Roberts, S. W., Hancock-Howard, R. L., & Coyte, P. C. (2015). Cost-effectiveness analysis comparing pre-diagnosis autism spectrum disorder (ASD)-targeted intervention with Ontario’s autism intervention program. Journal of Autism and Developmental Disorders, 45(9), 2833–2847. https://doi.org/10.1007/s10803-015-2447-0
Peters-Scheffer, N., Didden, R., Korzilius, H., & Matson, J. (2012). Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in the Netherlands. Research in Developmental Disabilities, 33(6), 1763–1772. https://doi.org/10.1016/j.ridd.2012.04.006
Piccininni, C., Bisnaire, L., & Penner, M. (2017). Cost-effectiveness of wait time reduction for intensive behavioral intervention services in Ontario, Canada. JAMA Pediatrics, 171(1), 23–30. https://doi.org/10.1001/jamapediatrics.2016.2695
Reichow, B., Hume, K., Barton, E. E., & Boyd, B. A. (2018). Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews, 10. https://doi.org/10.1002/14651858.CD009260.pub3
Smith, T. (2014). Early and intensive behavioral intervention in autism. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (3rd ed., pp. 312–326). Guilford Publications.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland Adaptive Behavior Scales: Second Edition (Vineland II), Survey interview form. Pearson Assessments.
Stevens, K. (2011). Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Applied Health Economics and Health Policy, 9(3), 1–13. https://doi.org/10.2165/11587350-000000000-00000
Tilford, J. M., Payakachat, N., Kovacs, E., Pyne, J. M., Brouwer, W., Nick, T. G., Bellando, J., & Kuhlthau, K. A. (2012). Preference-based health-related quality-of-life outcomes in children with autism spectrum disorders: A comparison of generic instruments. PharmacoEconomics, 30(8), 661–679. https://doi.org/10.2165/11597200-000000000-00000
Tsiplova, K., Ungar, W. J., Flanagan, H. E., den Otter, J., Waddell, C., Murray, P., D’Entremont, B., Léger, N., Garon, N., Bryson, S., & Smith, I. M. (2019). Types of services and costs of programs for preschoolers with autism spectrum disorder across sectors: A comparison of two Canadian provinces. Journal of Autism and Developmental Disorders, 49(6), 2492–2508. https://doi.org/10.1007/s10803-019-03993-3
Ungar, W. J. (2010). Economic evaluation in child health. Oxford University Press.
Ungar, W. J. (2011). Challenges in health state valuation in paediatric economic evaluation: Are QALYs contraindicated? PharmacoEconomics, 29(8), 641–652. https://doi.org/10.2165/11591570-000000000-00000
Ungar, W. J., Tsiplova, K., Millar, N., & Smith, I. M. (2018). Development of the Resource Use Questionnaire (RUQ-P) for families with preschool children with neurodevelopmental disorders: Validation in children with autism spectrum disorder. Clinical Practice in Pediatric Psychology, 6(2), 164–178. https://doi.org/10.1037/cpp0000226
Volden, J., Duku, E., Shepherd, C., Ba, Georgiades, S., Bennett, T., Di Rezze, B., Szatmari, P., Bryson, S., Fombonne, E., Mirenda, P., Roberts, W., Smith, I. M., Vaillancourt, T., Waddell, C., Zwaigenbaum, L., Elsabbagh, M., & Pathways in ASD Study Team. (2015). Service utilization in a sample of preschool children with autism spectrum disorder: A Canadian snapshot. Paediatrics & Child Health, 20(8), e43–e47.
Wille, N., Badia, X., Bonsel, G., Burstrom, K., Cavrini, G., Devlin, N., Egmar, A.-C., Greiner, W., Gusi, N., Herdman, M., Jelsma, J., Kind, P., Scalone, L., & Ravens-Sieberer, U. (2010). Development of the EQ-5D-Y: A child-friendly version of the EQ-5D. Quality of Life Research, 19(6), 875–886. https://doi.org/10.1007/s11136-010-9648-y
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ungar, W.J., Tsiplova, K. (2022). Economic Evaluations of Early Intensive Behavioral Interventions for Autism. In: Matson, J.L., Sturmey, P. (eds) Handbook of Autism and Pervasive Developmental Disorder. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-030-88538-0_29
Download citation
DOI: https://doi.org/10.1007/978-3-030-88538-0_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-88537-3
Online ISBN: 978-3-030-88538-0
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)