Abstract
Bone mineral density (BMD) testing is a key component in the management of patients with osteoporosis. Dual-energy X-ray absorptiometry (DXA) can be used to diagnose osteoporosis, assess fracture risk, and monitor changes in bone mineral density (BMD) over time. Quality control, acquisition, analysis, interpretation, and reporting of DXA studies require training and experience for the DXA technologist and interpreter. Poor quality DXA reports may result in inappropriate patient care decisions that can be costly and sometimes harmful to patients. This chapter will discuss the basic principles of DXA scanning, how to collect local reference data, falls risk, and the role of healthcare professionals (physicians, radiographer, as well as practice and osteoporosis nurse specialist) in the DXA scanning service. It will expand to discuss reporting of DXA scans for both adults and children as well as errors in standard practice. Glossary is included in the chapter including examples of preassessment questionnaires as well as the elements to be considered when reporting DXA scans. The objective is to provide the responsible healthcare professional with sufficient information and guidance so that the most informed management decision can be made.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Bone mineral density (BMD) testing is a key component in the management of patients with osteoporosis. Dual-energy X-ray absorptiometry (DXA) is a quantitative radiological procedure for measuring the bone mineral density (BMD), a major determinant of bone strength (1). Indeed, assessing BMD by DXA is a component of osteoporosis treatment guidelines in several countries all over the world [7,8,9,6]. However, DXA measurements are used not only to diagnose osteoporosis but also to monitor changes in BMD over time and estimate fracture risk and are often integral to therapeutic intervention recommendations. The World Health Organization (WHO) has established DXA as the best densitometric technique for assessing BMD in postmenopausal women and based the definitions of osteopenia and osteoporosis on its results. Furthermore, current guidance on fracture risk assessment adopted by the WHO (the fracture risk assessment algorithm (FRAX)) [7] includes femoral neck BMD measurement by DXA as an important risk factor input for fracture risk probability assessment. DXA also has applications beyond BMD testing (Table 10.1), including vertebral fracture assessment (12), analysis of body composition (13), hip structural analysis (14), and trabecular bone score determination (15). Furthermore, physicians rely on DXA measurements to manage patients with skeletal disorders.
Poor quality DXA acquisition/analysis and/or incorrect reporting of the results may result in the ordering of unnecessary diagnostic procedures, failing to order the required tests, or inappropriately starting, stopping, or changing treatment. Such errors in clinical practice are unfortunately common, sometimes costly, and potentially harmful to patients (16–21). DXA scans in growing children and adolescents are particularly challenging, and errors are common with respect to both data acquisition and interpretation (22). These errors can lead to the inappropriate initiation of therapeutic agents, many of which have unknown side effects in pediatric patients, and other inappropriate management decisions.
This chapter will discuss the basic principles of DXA scanning, how to collect local reference data, falls risk, and the role of healthcare professionals (physicians, radiographer, as well as practice and osteoporosis nurse specialist) in the DXA scanning service. It will expand to discuss reporting of DXA scans for both adults and children as well as errors in standard practice. Glossary is included in the chapter including examples of preassessment questionnaires as well as the elements to be considered when reporting DXA scans. The objective is to provide the responsible healthcare professional with sufficient information and guidance so that the most informed management decision can be made.
Basic Principles of DXA Scanning
Basically, DXA is a quantitative radiological procedure for measuring bone mineral density. Several different types of DXA systems are available, but they all operate on similar principles. A radiation source is aimed at a radiation detector placed directly opposite to the site to be measured. The patient is placed on a table in the path of the radiation beam. The source/detector assembly is then scanned across the measurement region. The attenuation of the radiation beam is determined and is related to the BMD [9, 10]. However, based on the fact that DXA scanners use two X-ray energies in the presence of three types of tissue, namely, bone mineral, lean tissue, and adipose tissue, there are considerable errors arising from the inhomogeneous distribution of adipose tissue in the human body [11]. Earlier studies [26,27,14] suggested that BMD measurement errors are in the range of 5–8%.
DXA technology can measure virtually any skeletal site; however, in standard practice, the clinical use has been focused on the lumbar spine, proximal femur, forearm, and total body [15]. DXA systems are available either as full table systems (capable of multiple skeletal measurements, including the spine and hip) or as peripheral systems (limited to measuring the peripheral skeleton). Because of their ability to measure the BMD at skeletal sites of greatest clinical interest, full table DXA systems are the current clinical choice for osteoporosis assessment. Peripheral DXA systems are characterized by being portable and less expensive than full table systems, yet they are more frequently used for screening and early risk assessment; but they cannot be used to monitor response to therapy. Spine and proximal femur scans represent the majority of the clinical measurements performed using DXA. Most full table DXA systems are able to perform additional scans, including lateral spine BMD measurements, body composition study, vertebral morphometry, measurements of children and infants BMD, assessment of bone around prosthetic implants, small animal studies, and measurements of excised bone specimens. However, for children measurement, the exam should be undertaken by clinicians skilled in interpretation of scans in children in centers that have an adapted pediatric software [16]. A glossary of DXA terminology and common acronyms is provided in Table 10.2 [16].
Best Practice of DXA
Over time, densitometer calibration may change due to degradation of the components (e.g., X-ray tube and detector), moving the instrument to a different location, or a variety of other factors. The skills of a DXA technologist may improve with experience or worsen over time, or a highly proficient technologist may leave and be replaced by one who is less skilled. Similarly, a physician involved may be dedicated to very high DXA quality or may view DXA as a sideline to other responsibilities. For all of these reasons, the reliability of DXA measurements and reports is sometimes in doubt, thereby having potential adverse effects on the management of patients [16, 17, 19].
In order to compare serial BMD studies on the same device, precision assessment conducted according to well-recognized standards is necessary to calculate the precision error and least significant change (LSC). Precision error is inherent in the BMD measurement itself and is largely dependent on the skill of the technologist in placing the patient in the same position for different scans. Precision represents the reproducibility of the BMD measurement and is typically calculated by measuring BMD in 15 patients 3 times or 30 patients twice on the same day, repositioning the patient after each scan. The least significant change (LSC), a value that is derived from the precision calculation, is the smallest BMD change that is statistically significant with a 95% level of confidence. Unfortunately, many DXA facilities have not done precision assessment, and quantitative comparison of BMD measurements cannot, therefore, be performed. Furthermore, there is often a lack of adherence to manufacturers’ recommendations for device maintenance and quality control, and the education and training of bone densitometry technologists and interpreters vary widely. For all these reasons, mistakes in BMD testing are commonly seen, sometimes with adverse effects on patient care [19].
How to Collect Local Reference Data
As the standardization of the diagnosis of osteoporosis is with a single reference database as outlined by WHO criteria, local reference values are primarily valuable for body composition analysis and in younger (pediatric) populations for determining Z-scores. Local reference values can be defined as either “healthy,” “representative,” or “normal.” Unfortunately, there are no standard definitions for these terms. For example, the BMDCS study is a healthy cohort that excluded all children with bone disease, children taking any medications that may affect bone density, children with multiple fractures, etc. [18]. The NHANES III study is a representative cohort of women recruited randomly by postal code throughout the USA, regardless of health status [19].
This guide for obtaining normative ranges was modeled after an investigator’s guide used by one of the manufacturers. The number of subjects and the age distributions have been based on statistical justifications. If the investigator deviates substantially from this protocol, statistical power and relevance may be lost, especially if collecting fewer numbers. The following describes the procedures for adult reference data collections. The investigator will need to recruit a minimum of 300 participants for each group desired, separated by sex and ethnicity. For example, adequately describing two distinct ethnic groups for both sexes requires 1200 participants (i.e., 50 subjects for each decade, sex, and ethnicity between 20 and 80 years old). The investigator will also need to capture all biological information. A QC phantom scan needs to be performed at least on the days that the subject is scanned but preferably three times a week to daily. The measurements and regions of interest (ROIs) the investigator acquires are dependent on their needs. If the need is exclusively for bone density, assessment in adults, spine, hip, and forearm DXA is appropriate. For body composition studies, whole body needs to be included. Each site is measured once for each subject, and the results are recorded on the Case Record Form (CRF). The Case Record Form (CRF) can then be sent to a statistician for analysis [20].
Demographics, medical history, and drug therapies should be noted on a completed patient information questionnaire as shown in Fig. 10.1. There is some debate as to the statistical method used to evaluate reference data. The simplest analysis is to calculate a population mean and SD for each 10-year age group. Z-scores can then be generated by comparing a patient’s measure to the decade reference values. Others have suggested that a quinquennial analysis of the means offers better resolution for separating pre- and postmenopausal women than other fitting approaches [21]. Regression models can be used to achieve more age resolution and stability in the Z-score values through each decade. Several approaches can be used; nonlinear and piecewise linear models have been used in the past. For a nonlinear model, the measure is plotted against age. The highest order regression (i.e., age, age2, age3) yielding a significant improvement over the next lower order regression model should be considered as the basis for the final reference data equation. Z-scores are then calculated using this equation to generate the measure mean and SD for the patient’s age. The SEE is used for the average SD across the entire age range (the SEE is an example of a root mean square error. The SEE tells us something about the accuracy of the predictions). However, this assumes that the distributions around the mean values are normal.
The most sophisticated approach is to take skew into account in the distributions around the mean values. Cole has developed a model and software that calculate percentile curves without assumptions of how normal the distribution is. This method, called LMS, is a fitting procedure that employs three cubic splines to generate centile estimates for age or size-related growth [22]. T. Cole offers a free program to perform this type of analysis (http://homepage.mac.com/tjcole/FileSharing1.html). The L curve, a Box–Cox power transformation of the measured variable, characterizes skewness; the M curve is the median for the measure (e.g., aBMD); and the S curve represents the CV (coefficients of variation) of the measure. Z-scores and centiles can be generated from the L, M, and S values. To obtain a Z-score for an individual subject, the following equation is used:
where the measurement represents the result from a DXA scan (aBMD, BMC, PCTFM, etc.) and L, M, and S are age-specific values. Similarly, the centiles for age are obtained using the equation:
where L, M, and S are for the required age and sex and Z is the standard normal deviate for the corresponding centile (e.g., for the 50th centile, Z = 0). Examples of this type of reference data curve are the CDC growth charts (the CDC growth charts are used for children age 2 years and older in the USA) [23] and the children’s aBMD and BMC reference data curves by Kalkwarf [18].
Role of Healthcare Professionals in the DXA Scanning Service
The physician in charge
The physician who is responsible for supervising a DXA facility, interpreting the DXA results, and signing off on the report must have sufficient training to assure that the data are correct and that interpretation and reporting conform to current standards in the field [38]. Expert opinion recommends providing referring clinicians with precise interpretation of all DXA scan results and subsequent guidance for patient management. Current practice is inconsistent, and guidance may be vague, so that the many specialists (including nurses, GPs, gerontologists, gynecologists, orthopedic surgeons, etc.) who are involved in referring patients for bone densitometry may be unclear as to how best to act on the results. Skills, knowledge about, and interest in the significance of DXA findings and which investigations and interventions are appropriate vary across these different disciplines.
Globally, requirements for training, performing, and interpreting DXA scans by healthcare professionals are variable [24]. Local regulation in the USA does not require any specific qualifications for DXA interpretation [25], despite the important technical aspects of the test. US Medicare regulations only require some qualifications of supervising physicians in independent diagnostic testing facilities [26], but not in hospital facilities or private clinical practices. In Canada, three provinces currently have a requirement for International Society for Clinical Densitometry (ISCD) certification for physicians who are reporting or supervising a DXA facility. In Brazil, certification by the Brazilian College of Radiology and Diagnostic Imaging (Colégio Brasileiro de Radiologia e Diagnóstico por Imagem) is required for any physician to perform DXA acquisition, analysis, and reporting.
Many scans are reported by registered healthcare professionals (e.g., radiologists, radiographers, physicians, nurses, etc.), whether medically qualified or not, who may not have direct experience in the management of osteoporosis and metabolic bone disease. Furthermore, many reporting healthcare professionals have not had formal training in DXA methodology or image interpretation and do not themselves operate a scanner. They therefore need to be made aware of the subtleties of interpretation; the significance of artifacts and abnormalities; and the importance of correct positioning when comparing scans [27]. In addition, there may be a need to make the referrer aware of other factors in the patient’s clinical history that may modulate the patient’s fracture risk or that may influence the application of clinical guidance or the necessity for further investigations or follow-up scans. Hence, there is a need to identify and address the educational and training needs of healthcare professionals in this area and for a standard to be established to set the learning outcomes.
Practice nurses and general practitioners
In the primary care setting, practice nurses play an essential part in the delivery of quality primary care, and due to the increasing shift of care from acute to primary, they have a growing responsibility in management of long-term conditions including osteoporosis. Effective fracture prevention is best addressed via a whole system response to the challenge of identifying fragility fractures. Practice nurses and general practitioners are well placed to identify fragility fractures, assess patients for osteoporosis, treat them, and monitor their adherence to treatment, thereby preventing further disabling and costly fractures. The role the practice nurses in the primary care setting was outlined by the royal osteoporosis society [28].
Identifying patients at risk of osteoporosis is one of the tasks that can be handled by practice nurses, who can screen patients for risk factors for osteoporosis, including family history, low BMI, coeliac disease, rheumatoid arthritis, smoking, or heavy drinking. Similarly, with the relevant knowledge, practice nurses can identify patients treated with medications that put them at greater risk of osteoporosis such as steroids, antiepileptic drugs, as well as hormone antagonist/depletion therapies used for breast cancer treatments such as aromatase inhibitors and prostate cancer drugs. Similarly, practice nurses and general practitioners can play a part in low-trauma fracture prevention by identifying all people over 50 years of age with a fracture in their practice and referring them to a fracture liaison service (FLS) for osteoporosis assessment. This should include all fragility fractures excluding face and skull. If a practice nurse sees a patient who has had a fragility fracture after the age of 50 who has not had a DXA scan or an assessment for osteoporosis, then this should be flagged up for consideration. The general practitioner or practice nurse can conduct both an online FRAX assessment and a dietary assessment for calcium intake, refer the patient for a DXA scan if appropriate, or start bone-sparing medication. Where the patient is complex, and where oral treatments have not been tolerated or successful, they can be referred to rheumatology or the local fracture liaison service (FLS).
Furthermore, practice nurses can play a vital role in the identification of osteoporotic vertebral fractures in primary care where most vertebral fractures will present as acute onset back pain with no obvious trauma. Without an assessment for osteoporosis, these fractures are otherwise easily missed. Action to identify and treat vertebral fractures by the practice nurse can quickly modify the patient’s risk of future debilitating fractures. If a practice nurse reviewed a patient with risk factors for osteoporosis, acute onset of back pain, and no obvious trauma and/or loss of height or receives a CT/MRI or X-ray report that highlights a vertebral fracture, then it should be highlighted to the GP as a matter of priority for assessment. The patient should be sent for a DXA scan.
Lastly, follow-up of all patients to check adherence to treatment is central, both to achieving best practice standards and realizing the clinical and cost benefits of fracture prevention. Practice nurses are well placed to do this, especially for complex patients and where there is no fracture liaison service (FLS) in place. Patients will benefit from a good working relationship between their practice nurse and the local osteoporosis service or fracture liaison service (FLS).
On the other hand, setting up specialized nurse-led osteoporosis in the hospitals/secondary care was also reported to be of value for rapid assessment and management of patients living with osteoporosis, particularly those who sustain acute fractures. An earlier study revealed that adopting specialized nurse-led osteoporosis vertebral fracture service identified patients at risk, allowed for accurate diagnosis, and shortened the time of assessment and management [29].
Radiographers
Radiographers working as part of a DXA service should have a robust knowledge of the DXA scanning techniques, risks, pitfalls, as well as national guidance for best practice. Furthermore, radiographers are required to bring particular skills to DXA and osteoporosis services. In addition to acquiring images, they have a responsibility for safeguarding adults and children. Some patients present with special requirements such as mobility difficulties; therefore, radiographers need to understand the principals of safe manual handling to protect themselves and others. DXA services may be provided in remote or mobile locations, and radiographers should understand the challenges presented by lone working in terms of the safety and well-being of themselves and their patients [30].
A DXA scan generally takes 15 to 20 minutes, with the standard World Health Organization (WHO) recommended sites for measurement being the lumbar spine, unilateral or bilateral proximal femoral, and, in some cases, the forearm [31]. The use of DXA vertebral fracture assessment (VFA) scans provide a low-dose visual assessment of vertebrae from the fourth thoracic vertebra (upper spine) to the level of the fourth or fifth lumbar vertebra (lower spine) for fractures in patients meeting scan criteria [32, 33]. Since a much lower dose of ionizing radiation is used for VFA scans in comparison to thoracolumbar spine radiographs, these scans can be undertaken on those who present clinical risk(s) for osteoporosis, even in the absence of a strong clinical suspicion of fracture [34].
Consistent positioning and technique are of particular importance in DXA to ensure reproducibility, accuracy, and precision for patients having follow-up scans. Radiographic positioning is a tactile skill, and radiographers should be aware of consent [35] and chaperone [36] policies and procedures. Practical aspects of the exposure such as pillow height and patient leg height as well as post processing techniques all influence the diagnostic result. Radiographers need to understand avoidable and unavoidable artifacts and the impact these may have on BMD. From time to time, DXA images may demonstrate incidental findings that require action. Radiographers should view the DXA images and should have the knowledge, skills, and competence to follow the correct procedure for communication of findings in accordance with the reporting standards [37].
Falls Service
Falls and osteoporosis go hand in hand to result in fractures, and as such, a falls prevention agenda needs to be high on the priority list for the healthcare professionals dealing with bone health issues as well as service managers. Tendency to fall has been identified as a predominant non-skeletal predictor of fragility fractures in the elderly [38]. It has been reported that about 90% of hip fractures involve falls [39]. Kaptoge et al. [40] found in the prospective multinational European Prospective Osteoporosis Study (EPOS) that BMD appeared to be less important in explaining variations in incidence of upper limb fractures in women across diverse populations in Europe, compared with the effect of location-specific risks of falling and factors that may be associated with the likelihood of falling. The nature of the fall likely determines the type of fracture, while bone density and factors that increase or attenuate the force of impact of the fall determine whether a fracture will occur when a faller lands on a particular bone [39]. The majority of falls in old age likely result from a combination of factors relating to aging and poor health, such as decrease in muscle strength and function, gait disorders, and loss of balance [41]. Epilepsy, use of seizure medication, Parkinson’s disease, and wearing corrective lenses are factors that tend to be associated with increased risk of pelvis fracture in men and women [42].
Identifying frequent fallers and referral to appropriate services is a key addition to the scanning and diagnostic services. Setting up integrated “Osteoporosis and Falls” services would help to manage those patients at high risk of falls and prevent further fractures [38]. Making every contact count (MEEC), which is an evidence-based approach to improving people’s health and well-being by helping them change their behavior, can be used as a framework to underpin the bone health service [44]. Identifying falls risk factors, early in the management pathway, help protecting them and preventing further falling over. Patients can be screened for falls risk. Several questionnaires have been developed and are available [45, 46]. As a result of widening the focus in fracture prevention to include both osteoporosis and falls, some centers implemented a combined fracture and falls risk in one referral form for DXA scanning [47], which would also be included in the DXA scan reporting as recommendations for high falls risk management.
DXA Scanning in Standard Clinical Practice
Referring for DXA Scanning
BMD consultation requests should include patient demographics, the indication for BMD testing, factors of relevance to the scan assessment (joint replacement, bone surgery, or bone disease in scan regions), osteoporosis medication history, factors of relevance to fracture risk determination in patients 50 years of age or older (fragility fracture history, glucocorticoid history), and any other pertinent medical information [63,64,50]. History of recent fractures in the last 2 years is also important to highlight the probability of imminent fracture risk. On referring a patient for DXA, the FRAX® tool should be used to estimate the patient’s 10-year fracture probability to decide whether DXA referral would be helpful. Even if the fracture risk is very high, it is helpful to know BMD in order to assess how well the patient is likely to respond to drug therapy and as a baseline to monitor progress. In most cases, it is clinically appropriate and feasible to send a patient over the age of 75 years for a DXA scanning. It is also advisable to include the falls risk as well as the possibility of sustaining an imminent fracture risk [51]. An example of a comprehensive DXA scan referral form is shown in Fig. 10.1.
On follow-up scans done on patients receiving osteoporosis drug therapy, it is particularly helpful if BMD requests indicate the scan year of primary interest for comparison, with details of current osteoporosis drug therapy and duration [52, 53]. While this level of information is often not provided, a thorough patient history from the referring physician is to be encouraged [63,64,50].
Pre-scan Assessment
DXA is contraindicated in patients for whom it is unlikely to alter clinical decisions, as well as in women who are or might be pregnant. If the patient has received recent radio-opaque contrast material or radioactive compounds, DXA should be postponed until such material no longer represents a potential confounding factor. Calcium supplements should not be taken on the same day before the DXA procedure, as an unabsorbed calcium tablet located in a scanned area might affect the BMD measurement. A patient whose weight exceeds the limit for the DXA table (typically about 130 kg for older instruments; 180–200 kg for others) should not be put on the table in case of damage to the table frame or injury to the patient. Therefore, the patient should be screened before having the DXA scan carried out. Patient questionnaires are usually the best approach for pre-scanning assessment. A template questionnaire that acquires the appropriate information necessary for BMD testing in adults (defined as those 18 years of age or over) is presented in Fig. 10.2. This can either be filled in by the patients while sitting in the waiting area or posted to the patient to be completed either online or paper format [54, 55]. The questionnaire should then be checked by trained facility staff. Alternatively, history can be directly taken by facility staff. The specific items on the questionnaire are intended to collect the minimum information needed to analyze a BMD scan and determine absolute fracture risk in those aged 50 years and over [48, 49]. Additional history items that are of relevance to individual patients should also be collected, such as menopausal history, medication history, and illnesses [57,58,44].
Reporting DXA Scans
Acquisition and accurate interpretation of bone densitometry scans are necessary first steps towards any clinical assessment process. The DXA report fulfils the role of transmitting data clearly to the clinician. A timely, concise, and informative report is essential to relay the DXA findings and to avoid costly and potentially dangerous misinterpretations by physicians unfamiliar with densitometry data.
Reports generated using the DXA manufacturer’s proprietary software have advanced significantly since X-ray-based bone densitometers were widely marketed in the late 1980s. Typically, these reports provide basic patient demographic data and a graphical image of the skeletal scan, as well as numeric data for bone area (BA), bone mineral content (BMC), and bone mineral density (BMD) for each region (and sub-regions). Additionally, the patient’s BMD data are compared with reference data derived from healthy controls to generate standard deviation scores: Z-scores represent comparisons with age-matched norms and T-scores comparisons with young adults.
Regardless of the age of the subject, most of the standard software provided by the manufacturer automatically reports both the T-scores and the resulting diagnoses of osteopenia or osteoporosis, as established by the World Health Organization (WHO) [1, 2]. The software-generated reports appear to provide a comprehensive clinical evaluation of the results sufficient to estimate risk for osteoporosis. However, interpretation based solely on these computer-generated reports is inappropriate and often misleading when interpreting the DXA results. It is crucial that the software generated report be modified and supplemented by a formal written report provided by an expert experienced in interpreting densitometry outcomes.
Report Targets
The clinical DXA report has six main purposes (Table 10.3). Typically, the report is sent only to the referring physician. However, some knowledgeable families may also request a copy of the report; therefore, it is best to provide definitions of all technical and clinical terminology used and to provide an objective, non-judgmental review.
Similar to other clinical reports, the technical DXA report has basic elements (Table 10.4), which include (1) patient demographics, (2) a brief medical history, (3) test results, (4) technical comments, and (5) interpretation and recommendations. Each element will be described in detail below, and data that are typically included in each section are elucidated. The formal report and advice regarding management should be written and signed by a qualified, knowledgeable experienced physician in the field [55].
Demographics
Typically, the report includes basic patient demographics and anthropometrics. Demographics should include patient name, date of birth, gender, healthcare number/hospital number or other identifier, height, weight, scan date, report date, name of the referring physician, name of the reporting physician, and BMD facility name and location [49, 50]. Weight and height should be measured at the BMD facility [48, 49]. It is very important to document patient height and weight because DXA measures “areal” and not true volumetric BMD. Neither values reported by the patient nor measurements provided by other medical practitioners should be used, other than in exceptional circumstances where it is not possible to carry out the measurements (such as if the patient cannot stand). If height or weight data were not measured directly by the BMD facility, this should be indicated in the report.
Weight can be measured with either a mechanical or an electronic scale that is medical grade. Facilities are encouraged to use wall-mounted height measuring devices, referred to as stadiometers, and to use standardized positioning of patients. It is also encouraged that three height measurements be made, with repositioning between each measurement, and the average used as the height value. The reason for this is that, just as with bone density quantitation, height measurements have significant precision error and this is minimized by averaging several assessments [56, 57] (in some centers, this height measurement methodology is a recommendation and is not a requirement for accreditation).
The demographic and anthropometric data are helpful in determining if body size is sufficiently above or below the expected range to warrant adjusting DXA results. If warranted, there are a number of recommendations for how to attempt to correct BMD for the size effects [59].
Medical History Used for Risk Determination
The report should include a brief summary of the clinical history relevant to the patient’s medical status and the interpretation of the scan. This might include the primary medical diagnosis; history of low-trauma fractures, particularly in the last 2 years; history of underlying medical condition or the use of medications known to affect BMD (e.g., antiepileptics and glucocorticoid therapy); mobility status and falls risk; endocrine abnormalities; pubertal status; surgical-induced menopause; bone age; and family history of osteoporosis [48, 49]. Physical activity level, dietary history, and use of vitamin or mineral supplements may also be useful.
Clinical information included in the referral form for DXA scanning improves both the acquisition and the interpretation of bone densitometry. Ideally, the relevant patient’s medical history should be obtained and recorded directly from the referring physician. This would be ideal when there is a local bone health service set up. Ideally, there should be an agreed referral form for DXA scan service (e.g., that shown in Fig. 10.1) [58]. The form should include (1) the reason for referring (e.g., for diagnosis of osteoporosis or monitoring of therapy); (2) indication for DXA scanning; (3) other health problems/medications that might affect the patient’s bone mineral density; (4) the main items of fracture risk score (e.g., FRAX) highlighting which fracture risk does the patient have; and (5) the patient’s falls risk. This will facilitate the process of reporting and assessment of the patient’s probability of having another fracture. However, in several occasions, patients are referred for bone densitometry assessment from a variety of clinical departments not familiar with the request form, and pre-scanning relevant medical history may not be readily available. Consequently, a registration questionnaire should be ready at the time of the DXA procedure to be completed by the patient. The technician should review the questionnaire paying attention to details surrounding fracture history, medication and supplement usage, and family history of osteoporosis.
If, for some reason, the questionnaire cannot be adequately completed at the time of examination (e.g., because of a language barrier or difficulty to read or hear), the form can be faxed/emailed to the referring clinic for completion by a qualified staff member familiar with the patient after the DXA procedure is completed.
Test Results
Care must be taken in all technical aspects of how scanning is performed, including adherence to manufacturer protocols, proper positioning, sub-region assignment, bone tracing, determination of regions of interest, and quality assurance [49, 50, 59]. A minimum of two skeletal sites should be scanned and reported. The usual sites would be the lumbar spine and the proximal femur [60].
For each skeletal site that is assessed, BMD, BMC, T-score, and Z-score should be included. The ISCD currently recommends calculating T-scores using a uniform sex-matched (white) young adult database for patients of all ethnicities in the USA, recognizing that other countries might use alternative databases according to local requirements [61]. Regarding Z-scores, the ISCD recommends databases that are matched for sex, ethnicity, and age. Although there is no established standard for using or not using weight adjustment for Z-scores, the evidence seems to favor not using weight adjustment [62].
For each skeletal site with a valid scan, reported density results should include absolute BMD (in g/cm2 to 3 decimal places) and either T-score (to one decimal place) for those 50 years or older or Z-score (to one decimal place) for those under 50 years of age [63] (Table 10.4). For women, T-scores and Z-scores should be derived using the manufacturer’s white female reference database. Similarly, for men over age 50 years, T-scores used for diagnostic classification should be derived using a white male reference database; the femoral neck T-score used for risk determination should be derived from a white female reference database, while the spine T-score used to alter the risk category from low to moderate if the value is ≤ −2.5 should be derived from a white male reference database. For men under age 50 years, Z-scores should be derived using a white male reference database. The reference databases and versions should be specified in the report [62].
When analyzing the lumbar spine, L1–L4 should be used unless the decision is made to exclude one or two vertebrae because of technical artifacts. A minimum of two vertebrae should be used. Interpretation should not be based on a single vertebra [49, 59]. If a report includes graphical representation of results, the graph must present data and reference curves for the vertebrae, actually, used in interpretation. Consideration can be given to excluding a particular vertebra if the T-score of that vertebra is more than one standard deviation greater than the T-score of the vertebra with the next highest value [64]. It is not mandatory that a high-density vertebra be excluded, but it should be evaluated for causes of artifact and a decision made as to whether it should be retained in the vertebral analysis.
For the proximal femur, the left side should be measured unless it is not available and invalid or the right hip was previously measured [49]. Results should be reported for the total hip and femoral neck. If either the spine or hip site is not available or invalid because of artifact, another body site should be substituted. The non-dominant forearm is the site of choice, and the one-third (or 33%) radius should be reported [59]. If the non-dominant forearm is not available or is invalid, the dominant side may be used. If the wrist cannot be measured, total body BMD can be assessed. The head may be included or excluded when analyzing the scan. If the head is excluded, this should be noted in the report. If the spine cannot be measured, and neither forearm nor total body measurements are available, bilateral hip measurements may be made. The two hip measurements should be reported separately, not as an averaged value [64]. When applying hip data to determine the diagnostic category or fracture risk category, the lowest of the relevant values from the two sides should be used. For patients whose weight exceeds the limit of the DXA equipment, bilateral forearm studies may be done unless one side is not available or invalid, although it will not be possible to determine fracture risk [63, 64].
Technical Notes
The report should consider future DXA scanning and allow comparisons with previous and future densitometry studies. Therefore, it should include sufficient information regarding how the DXA was performed and interpreted. Given the fact that there are intrinsic differences between the variable DXA scanners, and the software used for BMD assessment, the manufacturer and model of the instrument should be specified (e.g., Hologic Delphi A/Lunar iDXA). Similarly, the software mode used to acquire and analyze the scan should also be provided (e.g., auto low-density, low-density spine [LDS] software). If the reference data used in the calculation of Z-scores were different from the manufacturer’s normative data, it is important that this also be documented.
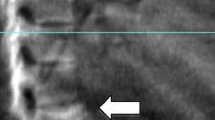
Careful visual review of each scan, prior to the preparation of the report, should be considered to ensure that artifacts do not affect the data recorded (Fig. 10.3). The report should outline any technical matters encountered during the scanning process. Documentation is important, both for the initial interpretation of the DXA scan and to alert the DXA technologist to these effects in future scan acquisitions. These might include noticeable scoliosis, degenerative disease, vertebral compression fractures, or nonremovable metal artifacts (Table 10.5). Scans with motion artifacts or removable metal objects (e.g., metal from the underwire or clasp of a bra, a belt buckle, a pant zipper, or a belly button ring) should not be reported. These scans should be repeated before the patient leaves the clinic [65].
Diagnostic Category
The diagnostic category is determined using the lowest T-score (for individuals 50 years of age or older) or Z-score (for individuals under 50 years of age) from the available results for the lumbar spine, total hip, femoral neck, one-third (or 33%) radius, and total body (2). The trochanteric region and Ward’s region of the proximal femur are not to be used (16). T-scores or Z-scores for diagnostic categorization should be derived using a white female reference database for women and a white male reference database for men. The original WHO criteria are stated in Table 10.6.
The WHO criteria should not be applied to other bone density measures, including QCT of the spine or hip, peripheral densitometry systems using ultrasound, DXA, or other technologies that scan the fingers, metacarpals, or heels [31].
Fracture Risk
The absolute fracture risk category should be reported for men and women 50 years of age and older. The current WHO guidelines for diagnosing and treating osteoporosis are based on a comprehensive fracture risk model WHO “FRAX.” The WHO FRAX algorithm estimates the likelihood for a person to break a hip or other major bone due to low bone mass or osteoporosis over a period of 10 years. The National Osteoporosis Foundation (NOF) has prepared a clinician’s guide to osteoporosis that discusses the details of the FRAX model and the use of fracture risk versus BMD alone (http://www.nof.org/professionals/NOF_Clinicians%20_Guide.pdf). In summary, the major recommendations to the clinician regarding the diagnosis of osteoporosis are outlined in Table 10.7 [66]. The WHO FRAX model is the most common tool used to assess for the fracture risk. Although it was noted that the WHO FRAX algorithm pertains only to individuals that have not been treated for osteoporosis, other studies revealed that in women currently or previously treated for osteoporosis, the FRAX tool can be used to predict fracture probability. Osteoporosis treatment does not annul prediction of fractures. FRAX tool could be of value in guiding clinicians towards the need for continuation or withdrawal of treatment [67].
Interpretation
A narrative section on the interpretation and implications of BMD results should be provided. This should not be a simple restatement of data. The reporting physician should integrate the available information on the patient’s specific risk factor, fracture risk probability, falls risk, as well as current medication (when appropriate). Guidance as to therapeutic considerations can also be provided within the context of the local/international osteoporosis guidelines and up to the degree appropriate to the knowledge and experience of the reporting physician [48, 49].
Follow-Up Recommendation
A recommendation should be included for the timing of the next DXA study. The timing of serial testing should be driven by the expected rate of bone loss. The intention of serial monitoring is to provide a sufficient period of time for anticipated changes in density to exceed the precision error of the DXA method, which also renders a stable density informative measure [59].
A guide for the follow-up period is provided in Table 10.8, although this needs to be applied in the context of local recommendations. When indicating recommended timing of the subsequent BMD test, consideration should be given to specifying the year of recommended follow-up rather than a time interval, as this makes the report more readily implementable by referring physicians. For follow-up periods under 2 years, the month of recommended follow-up could also be included.
Limitations
Any structural abnormalities, anatomical variants, artifacts, suboptimal positioning, or other issues impacting on scan reliability and interpretation need to be considered when interpreting BMD results. A judgment needs to be made as to whether these issues render results invalid or impact on the interpretation. Some sources of artifact are preventable, and care should be taken to assess these prior to scanning (such as metal on clothes or in pockets, or recent barium or nuclear medicine studies), either to remove the source of artifact or postpone the scan to a future date. Sources of artifact relevant to the scan should be noted in the report. Skeletal size can affect BMD readings, with larger bones producing falsely high values and smaller bones producing falsely low values [64]. There is no accepted means of correcting for skeletal size, but height or weight outside the normal range should be noted and should be considered in the interpretation of results. Components of the first-time and follow-up adult DXA report are shown in Table 10.9.
Follow-Up Adult BMD Report
It is common to have follow-up DXA scans requested. This step should reflect the need to have a new scan, which should be also reflected in the repeat BMD report. Consequently, the follow-up adult BMD report should include, in addition to all the components of a first-time adult report, specific new items such as changes in density, statistical parameters relating to measurement error, aspects of interpretation relating density changes to the clinical situation, and definitions relevant to follow-up.
Follow-Up Referral Form
The referral should include the reason for repeating the BMD testing and whether it is to monitor response to therapy or change in the patient’s status, e.g., sustaining a fracture. Developing a recent fracture should be highlighted as an imminent fracture risk. Also, the form should include any change in the patient medical status, whether he developed a new medical disorder or taking medication that might affect the bone health status. The referring physician should also highlight if the patient has started taking medication to improve his bone mineral density status and the duration of treatment. Fracture risk probability, without BMD, can also be carried out by the referring physician and recorded in the referral form.
Demographics
Any significant change in height recorded at the BMD facility should be noted. In particular, loss of height exceeding 2 cm over 3 years or less should be emphasized, as this amount of change in height has been shown to have a high predictive value for incident vertebral fractures which might have developed during the monitoring period. Consequently, this may be an indication to do spine radiographs or vertebral morphometry to assess for vertebral fractures [48, 57].
Change in the patient’s body weight is another demographic parameter to note, as this may represent an artifactual change in BMD values. Though there is no consensus as to what is the threshold of change in body weight that can be flagged as being of potential importance as a source of artifact, some physicians suggested the use of percentage change in weight, whereas others recommended the use of absolute change in weight. A suggested threshold is 10% change in weight over the monitoring period. However, each reporting physician must define a weight change threshold and adopt it in all serial reporting, applying it to each pair of BMD measurements for which change in BMD is reported [68].
Fracture Risk Category
All men and women aged 50 years and above should have the absolute fracture risk category reported, regardless of therapy that might be taking. If bone-active drug therapy is currently prescribed and taken by the patient, the fracture risk category should be provided, but the report should include a statement indicating that the risk may be lower than calculated if osteoporosis drug therapy is effective [49, 67].
Changes in Density
Whenever possible, when serial BMD assessments are carried out, it is always preferable to use the same DXA machine. In concordance, it is highly recommended that positioning and sub-region assignment must be consistent [59]. Also, the same reference population database should be used for serial studies when possible [64]. If the reference database has to be changed, this should be noted in the report. The description of change in the BMD should include the absolute density change (in g/cm2, to 3 decimal places) and percentage change (to 1 decimal place) [52]. Percentage change must be derived using absolute density (g/cm2), not T-scores or Z-scores. An annualized rate of change should be reported, though it may be optional in some locations. The skeletal sites for which changes in density are to be reported are the lumbar spine (using whichever vertebrae are considered valid, with a minimum of two vertebrae) and the total proximal femur (this include neck of the femur and total hip). Other hip sub-regions should not be used. If either the spine or hip is not available, it is permissible to report changes at a single site. If the forearm or total body BMD is being monitored in lieu of the spine or hip, change can be reported for the one-third (or 33%) proximal radius or for the total body BMD. It must be recognized that the change profile at these sites may not be in parallel with changes at the spine and hip and may not correlate as well with drug responses. This will need to be addressed in the interpretation section [69].
Changes in BMD must be reported in relation to (1) the first baseline study on file, (2) the most recent previous BMD study, and (3) the study done closest to the initiation of the current clinical medical management/medication (if any), if this can be confirmed. The latter BMD change is the one of greatest importance for patients on drug therapy; it is also relevant to patients who adopted lifestyle changes and/or started nutritional supplements for bone health. Ideally, the study of primary interest for comparison should be indicated on the requisition by the referring physician, but if it is not provided, the reporting physician is responsible for obtaining this information from the patient’s history [52, 64].
On comparison to previous scans, statistical significance must be reported for each BMD skeletal site, indicating whether the difference is considered significant at a 95% level of confidence [50]. The manufacturer’s software determination of statistical significance should not be the one to be used (2). Each facility must determine the precision error for each DXA machine and for each skeletal site (including forearm and total body if these sites are measured by the facility and are used for serial monitoring) using the least significant change (LSC) methodology and using this value when determining statistical significance. It is permissible to apply results derived from precision testing on one side (forearm or hip) to serial scans done using the opposite side of the body. A follow-up BMD report should state the least significant change (LSC) in absolute values (g/cm2 to 3 decimal places) for each skeletal site for which change is reported. Whenever possible, the same instrument should be used for serial studies on an individual patient. Comparisons between measurements done on different machines can be made only if inter-machine precision between the two devices has been determined [59, 64].
Interpretation
The clinical implications of the change in BMD or fracture risk must be incorporated into the interpretation section of the report [49, 50]. This is of greatest importance for patients receiving osteoporosis drug therapy, where BMD is often being used to assist in monitoring management outcomes. The primary BMD outcome of interest in this circumstance is the net change in density from the time that the current therapeutic regimen was initiated [53].
In general, net gain in BMD is considered positive drug effect while net loss of density is considered as evidence of drug failure. Secondary changes in the BMD profile that may differ from the net change on a drug regimen, such as a change from the most recent prior study, also need to be considered in the interpretation. For serial studies in those not on osteoporosis drug therapies, there are similar implications for the effects of nutritional supplements, lifestyle changes, and exercise regimens [70].
So far, there is insufficient data to define the relationship between the amount of loss in BMD and the resulting change in fracture risk. Rather, the implications of density loss and any changes in the fracture risk probability should be discussed in the interpretation of results. Components of follow-up DXA scan report in adult are shown in Table 10.9.
Pediatric DXA Scanning
The pediatric population is defined as individuals under age 18 years. The components of a first-time pediatric BMD report, in contrast to the adult first-time BMD report, are shown in Table 10.10. In concordance with adults, there are similar components including demographics, machine identification, and limitations [71]. On the other hand, there are differences regarding BMD data and interpretation. This is based on the fact that there are specific definitions which apply to reporting in this age group [72]. There are no guidelines on timing of follow-up studies, so a recommended follow-up date is not mandatory, although may be included at the discretion of the reporting physician. If the referring physician has not relayed the indications for the scan and the relevant medical history, it is possible to ask the patient, parent, or both to complete a brief registration questionnaire at the time of the DXA procedure. Individual pediatric patient should be collected and may include fracture history, medications, and illnesses. Height and weight measurements in younger children require special devices and procedures. If these are not available, it is acceptable in younger children to use values provided by other medical practitioners. If height or weight were not measured directly by the BMD facility, this should be indicated in the report [71].
Diagnostic Category
For each skeletal site that is assessed, BMD, BMC, and BA (BA: bone area) should be included, as should the corresponding BMD Z-score, to enable the clinician to determine if the measured values are within the expected range for age. BMC and BAs are used to calculate estimates of volumetric BMD (i.e., bone mineral apparent density [BMAD]) and should be included in the report. Reporting BMC and BA also allows the clinician to examine subsequent changes due to bone growth. The current standard for reporting the diagnostic category in the pediatric population is based on the lowest adjusted Z-score from the results for the lumbar spine and total body, using either bone mineral content (BMC) or BMD at the discretion of the reporting physician. The T-score is not to be used in pediatric reporting. If either the spine or total body value is not available or invalid, this should be reported as a limitation. Forearm measurements (one-third or 33% site) may be used if either the spine or total body value is not available, but only if a reference population database is available from which forearm Z-scores can be derived. Proximal femur measurements are not to be used to generate the diagnostic category in the pediatric population, although it may be clinically useful to begin measuring hip density in older adolescents in order to start transition into the adult mode of monitoring [71, 73].
Technical Comments
Care must be taken in all technical aspects of how scanning is performed, including adherence to manufacturer protocols, proper positioning, sub-region assignment, bone tracing, determination of regions of interest, and quality assurance. Results should be reported for the lumbar spine and total body, including BMC and BMD for each site. When analyzing the lumbar spine, L1 to L4 should be used unless the decision is made to exclude one or two vertebrae because of technical artifacts [64]. A minimum of two vertebrae should be used. Interpretation should never be based on a single vertebra. If a report includes graphical representation of results, the graph must present data and reference curves for the vertebrae actually used in interpretation. Consideration can be given to excluding a particular vertebra if the Z-score of that vertebra is more than one standard deviation greater than the Z-score of the vertebra with the next highest value. It is not mandatory that the high-density vertebra be excluded, but it should be evaluated for causes of artifact and a decision made as to whether it should be included in the vertebral analysis. In some manufacturers’ databases, Z-scores may not be available if vertebrae are excluded. In this circumstance, it is appropriate to include L1 to L4 in order to generate a Z-score, but the interpretation section must address the accuracy of the spine measurement and the ways in which the Z-score may have been perturbed by the abnormal vertebrae. For the total body measurement, the head may be included or excluded on analyzing the scan [87,88,74]. If the head is excluded, this should be noted in the report. For adolescent patients whose weight exceeds the limit of the DXA equipment, bilateral forearm studies may be done unless one side is not available or invalid, in which case a single side can be measured [71, 72].
For each skeletal site with a valid scan, reported density results should include absolute BMD (in g/cm2 to 3 decimal places), BMD Z-score (to 1 decimal place), and adjusted BMD Z-score (to 1 decimal place) and BMC (in g, to 2 decimal places), BMC Z-score (to 1 decimal place), and adjusted BMC Z-score (to 1 decimal place) [59].
The Z-score adjustment is done to correct for relative skeletal size or maturation. There is no consensus at this time as to the specific adjustment that should be made, so the nature of the adjustment is at the discretion of the reporting physician. Adjustment can be based on height, weight, body mass index, bone area, bone age, pubertal stage, lean body mass, or a combination of these parameters [92,93,79]. The method of adjustment should be noted in the report, and if a multivariable method is used, a published reference should be provided.
The assignment of diagnostic category should be based on the adjusted Z-scores using the BMC Z-score, the BMD Z-score, or the lower of the two, at the discretion of the reporting physician. Some manufacturers provide height or weight corrections as part of the DXA software. For those whose DXA software does not provide such corrections, an approach to correcting for bone age or height age is described in Table 10.10. Each method of correction has limitations and constraints, and these need to be considered in the interpretation [64, 71].
Bone area, corrected bone area, and area Z-scores are not required but can be included at the discretion of the reporting physician [79]. All Z-scores are derived using a white female reference database for girls and a white male database for boys. The reference database and version should be specified in the report. If the reference database that is used to generate Z-scores is not one provided by the manufacturer, a published reference should be provided. Z-scores may not be available for certain skeletal sites at young ages and so do not need to be reported [71].
Follow-Up Pediatric DXA Scanning
The components of a follow-up pediatric BMD report are shown in Table 10.11. A follow-up pediatric BMD report should include all of the components of a first-time pediatric report. In addition, items specific to follow-up also need to be described, including changes in density, statistical parameters relating to measurement error, and aspects of interpretation relating to the changes in density.
Changes in Density
When comparing serial assessments, positioning and sub-region assignment must be consistent [78, 79]. The same reference population database should be used for serial studies whenever possible. If the reference population database must be changed, this should be noted in the report. The description of density change should include the absolute density change (in g/cm2, to 3 decimal places), percentage change (to 1 decimal place, derived using absolute density, not Z-scores), change in Z-score, and change in adjusted Z-score [59, 64]. Annualized rates of change may be reported, but this is optional [79]. The skeletal sites for which changes in density are to be reported are the lumbar spine (using whichever vertebrae are considered valid, with a minimum of two vertebrae) and the total body [71, 72]. If the forearm is being monitored in lieu of the spine or total body, change can be reported for the one-third or 33% proximal radius [78]. It must be recognized that the change profile at the forearm may not parallel changes at the spine and total body and may not correlate as well with drug responses. This will need to be addressed in the interpretation section, if applicable.
Changes in density must be reported in relation to (1) the first study on file and (2) the most recent previous study. Pediatric osteoporosis drug treatment regimens are not well defined, and if information is not provided by the referring physician, it can be difficult to ascertain the timing of the BMD study corresponding to the initiation of a clinical treatment regimen. It is therefore not mandatory at this time that changes be reported in relation to the initiation of treatment. This can be provided at the discretion of the reporting physician if it is felt that an appropriate comparison study can be defined in relation to treatment.
Statistical significance must be reported for each BMD skeletal site comparison, indicating whether the difference is considered significant at a 95% level of confidence. The manufacturer’s software determination of statistical significance is not to be used. Each facility must determine precision error for each DXA machine and for each skeletal site (including forearm if this site is measured by the facility and used for serial monitoring) using the LSC methodology and use this value when determining statistical significance [64]. It is permissible to apply results derived from precision testing of the forearm on one side to serial scans done using the opposite side of the body. Facilities are encouraged to derive precision using pediatric age subjects, particularly facilities that perform only pediatric clinical tests. In the absence of data proving that precision differs between adults and children, however, it is acceptable at this time for all facilities to use precision derived from adult subjects. If precision is derived using adult subjects, this should be noted in the report. A follow-up pediatric BMD report should state the LSC in absolute values (g/cm2 to 3 decimal places for BMD, g to 2 decimal places for BMC) for each skeletal site for which change is reported and for both BMD and BMC. Whenever possible, the same instrument should be used for serial studies on an individual patient. Comparisons between measurements done on different machines can be made only if inter-machine precision between the two devices has been determined [59, 64]. Table 10.12 shows the common mistakes in DXA scanning and BMD assessment.
There is no accepted methodology, so far, for evaluating statistical significance of Z-score differences at different time points. The change in Z-score between comparison BMD studies should be noted. An opinion as to whether the difference is clinically meaningful should be incorporated into the interpretation section. It is not necessary to report changes in either height or weight.
In conclusion, a timely, concise, and informative DXA report is essential to relay densitometry findings and to avoid costly and potentially dangerous misinterpretations by referring physicians unfamiliar with interpreting densitometry data.
-
Enough information should be provided in the report to allow for comparison to previous and subsequent DXA studies.
-
The technical DXA report typically has five basic elements: (1) patient demographics, (2) a brief medical history, (3) test results, (4) technical comments, and (5) interpretationand recommendations.
-
Medical history information should be obtained ideally from the referring physician, or otherwise from the patient or parent. Key information to include in the report are primary medical diagnosis, use of medications known to affect bone, fracture history and whenavailable, pubertal status, bone age, focused dietary, and physical activity histories.
-
Careful review of the DXA scan images must be made prior to reporting of results toavoid misinterpretation of the findings based on artifacts in the scan field.
References
Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. 1994;4:368–81.
Miller PD, Bonnick SL, Rosen CJ. Consensus of an international panel on the clinical utility of bone mass measurements in the detection of low bone mass in the adult population. Calcif Tissue Int. 1996;58:207–14.
Papaioannou A, Morin S, Cheung AM, et al. 2010 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73.
Kanis JA, McCloskey EV, Johansson H, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57.
Compston J, Bowring C, Cooper A, et al. Diagnosis and management of osteoporosis in postmenopausal women and older men in the UK: National Osteoporosis Guideline Group (NOGG) update 2013. Maturitas. 2013;75:392–6.
Wang M, Bolland M, Grey A. Management recommendations for osteoporosis in clinical guidelines. Clin Endocrinol. 2015;84(5):687–92. https://doi.org/10.1111/cen.13000; (Oxf) Epub.
Kanis JA, Oden A, Johansson H, et al. FRAX(R) and its applications to clinical practice. Bone. 2009;44:734–43.
Fenton JJ, Robbins JA, Amarnath AL, Franks P. Osteoporosis overtreatment in a regional health care system. JAMA Intern Med. 2016;176:391–3.
Blake GM, Fogelman I. DXA scanning and its interpretation in osteoporosis. Hosp Med. 2003;64:521–5.
Blake GM, Fogelman I. Dual energy x-ray absorptiometry and its clinical applications. Semin Musculoskelet Radiol. 2002;6:207–18.
Tothill P, Avenell A. Errors in dual-energy X-ray absorptiometry of the lumbar spine owing to fat distribution and soft tissue thickness during weight change. Br J Radiol. 1994;67:71–5.
Svendsen OL, Hassager C, Skodt V, Christiansen C. Impact of soft tissue on in vivo accuracy of bone mineral measurements in the spine, hip, and forearm: a human cadaver study. J Bone Miner Res. 1995;10:868–73.
Lee DC, Wren TAL, Gilsanz V. Correcting DXA pediatric bone mineral density measurements to account for fat inhomogeneity. ASBMR. 2007;W514
Kuiper JW, van Kuijk C, Grashuis JL, Ederveen AG, Schutte HE. Accuracy and the influence of marrow fat on quantitative CT and dual-energy X-ray absorptiometry measurements of the femoral neck in vitro. Osteoporos Int. 1996;6:25–30.
Hans D, Downs RW Jr, Duboeuf F, Greenspan S, Jankowski LG, Kiebzak GM, et al. Skeletal sites for osteoporosis diagnosis: the 2005 ISCD official positions. J Clin Densitom. 2006;9:15–21.
El Maghraoui A, Roux C. DXA scanning in clinical practice. Q J Med. 2008;101:605–17.
Watts NB. Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int. 2004;15:847–54.
Kalkwarf HJ, et al. The bone mineral density in childhood study: bone mineral content and density according to age, sex, and race. J Clin Endocrinol Metab. 2007;92(6):2087–99.
Looker AC, et al. Proximal femur bone mineral levels of US adults. Osteoporosis Int. 1995;5(5):389–409.
Dual energy X ray absorptiometry for bone mineral density and body composition assessment. IAEA human health series no. 15. International Atomic Energy Agency Vienna, 2010. https://www-pub.iaea.org/MTCD/Publications/PDF/Pub1479_web.pdf. Accessed 3 Nov 2019.
Truscott JG, et al. Variation in lumbar spine and femoral neck bone mineral measured by dual energy X ray absorption: a study of 329 normal women. Br J Radiol. 1993;66(786):514–21.
Cole TJ, Green PJ. Smoothing reference centile curves: the lMS method and penalized likelihood. Stat Med. 1992;11(10):1305–19.
Ogden CL, et al. Centers for disease control and prevention 2000 growth charts for the United States: improvements to the 1977 national center for health statistics version. Pediatrics. 2002;109(1):45–60.
Michael Lewiecki E, Binkley N, Morgan SL, Shuhart CR, Camargos BM, Carey JJ, Gordon CM, Jankowski LG, Lee J-K, Leslie WD, on behalf of the International Society for Clinical Densitometry. Best practices for dual-energy X-ray absorptiometry measurement and reporting: International Society for Clinical Densitometry Guidance. J Clin Densitom. 2016;19(2):127–40.
MultiState Associates Incorporated. Semi-weekly reports to the International Society for Clinical Densitometry on state legislative and regulatory activity relating to DXA or bone density studies. 2006–2015; Data on file.
Centers for Medicare & Medicare Services. 2011 Code of Federal Register. Billing and Enrollment Guideline for PHYS-078 Independent Diagnostic Testing Facilities (IDTF). Available at: https://downloads.cms.gov/medicare-coveragedatabase/lcd_attachments/23448_6/CBGPHYSMED078April09.pdf. Accessed 10 Oct 2019.
Watts NB. Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporosis Int. 2004;15(11):847–54.
Royal osteoporosis society. The role of the practice nurse. https://theros.org.uk/healthcare-professionals/courses-and-cpd/osteoporosis-resources-for-primary-care/practice-nurses/the-role-of-the-practice-nurse/.
El Miedany Y, Gardiner A, El Gaafary M, Toth M. Outcomes of a nurse-led osteoporosis and falls assessment. Br J Nurs. 2006;15(19):1070–6.
The society and college of radiographers. The role of the radiographer in DXA and osteoporosis services. 2018. https://www.sor.org/sites/default/files/document-versions/the_role_of_the_radiographer_in_dxa_and_osteoporosis_services_-_final_proof_0.pdf. Accessed 20 Oct 2019.
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Heal. Organ. - Tech. Rep. Ser. 1994. Available at: http://apps.who.int/iris/bitstream/handle/10665/39142/WHO_TRS_843_eng.pdf?sequence=1&isAllowed=y.
International Society for Clinical Densitometry (ISCD). 2013 ISCD Official Positions – adult. 2013. Available at: https://www.iscd.org/official-positions/2013-iscd-official-positions-adult/. Accessed 20 Oct 2019.
International Society for Clinical Densitometry (ISCD). Reference data – International Society for Clinical Densitometry (ISCD) – Pediatric Resources. 2012. Available at: https://www.iscd.org/resources/pediatric-resources/reference-data/. Accessed 20 Oct 2019.
Kuet K-P, Charlesworth D, Peel NFA. Vertebral fracture assessment scans enhance targeting of investigations and treatment within a fracture risk assessment pathway. Osteoporos Int. 2013;24:1007–14.
Society and College of Radiographers. Obtaining consent: a clinical guideline for the diagnostic imaging and radiotherapy workforce. 2018. Available at: https://www.sor.org/sites/default/files/document-versions/obtaining_consent_170118.pdf. Accessed 20 Oct 2019.
Society and College of Radiographers. Intimate examinations and chaperone policy. 2016. Available at: https://www.sor.org/learning/document-library/intimate-examinations-and-chaperone-policy-0. Accessed 20 Oct 2019.
The Royal College of Radiologists. Standards for interpretation and reporting of imaging investigations; 2nd edition. 2018. Available at: https://www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr181_standards_for_interpretation_reporting.pdf. Accessed 20 Oct 2019.
Gardsell P, Johnell O, Nilsson BE, Nilsson JA. The predictive value of fracture, disease, and falling tendency for fragility fractures in women. Calcif Tissue Int. 1989;45(6):327–30.
Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 1993;41(11):1226–34.
Kaptoge S, Benevolenskaya LI, Bhalla AK, Cannata JB, Boonen S, Falch JA, et al. Low BMD is less predictive than reported falls for future limb fractures in women across Europe: results from the European Prospective Osteoporosis Study. Bone. 2005;36(3):387–98.
Hanssens L, Reginster JY. Relevance of bone mineral density, bone quality and falls in reduction of vertebral and non-vertebral fractures. J Musculoskelet Neuronal Interact. 2003;3(3):189–93.
Kelsey JL, Prill MM, Keegan TH, Quesenberry CP Jr, Sidney S. Risk factors for pelvis fracture in older persons. Am J Epidemiol. 2005;162(9):879–86.
El Miedany Y, Toth M. Osteoporosis, fracture prevention and falls risk assessment – closing the gap between treatment guidelines and clinical practice. Eur Musculoskelet Rev. 2011;6(1):7–14.
Varley E, Murfin M. An implementation guide and toolkit for making every contact count. Available at: https://www.england.nhs.uk/wp-content/uploads/2014/06/mecc-guid-booklet.pdf. Accessed 20 Oct 2019.
El Miedany Y, El Gaafary M, Toth M, Palmer D, Ahmed I. Falls risk assessment score (FRAS): time to rethink. J Clin Gerontol Geriatr. 2011;2:21–6.
Wiens CA, Koleba T, Jones CA, Feeny DF. The falls risk awareness questionnaire: development and validation for use with older adults. J Gerontol Nurs. 2006;32(8):43–50.
El Miedany Y, El Gaafary M, Youssef S, Toth M. Osteoporosis, falls and fractures: three confounders in one equation. Development and validity of a new form for assessment of patients referred for DXA scanning. Rheumatology. 2010;49(suppl 1):i80–6.
2010 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 2010; 182:1864–1873.
Lentle B, Cheung AM, Hanley DA, Leslie WD, Lyons D, Papaioannou A, et al. Osteoporosis Canada 2010 guidelines for the assessment of fracture risk. Can Assoc Radiol J. 2011;62:243–50.
American College of Radiology. Practice guideline for the performance of dual-energy x-ray absorptiometry (DXA). Res. 29-2008; Available at: www.acr.org. http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/DXA.pdf. Accessed 20 Oct 2019.
Miedany YE, Gaafary ME, Toth M, et al. OP0216 identification and management of patientsat increased risk of osteoporotic fracture: implementation of imminent risk factor in standard daily practice for bone mineral density assessment and patient management. Ann Rheum Dis. 2019;78:184–5.
Binkley N, Krueger D. What should DXA reports contain? Preferences of ordering health care providers. J Clin Densitom. 2009;12:5–10.
Lewiecki EM, Watts NB. Assessing response to osteoporosis therapy. Osteoporos Int. 2008;19:1363–8.
Bonnick SL, Shulman L. Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med. 2006;19:S25–31.
Siminoski K, O’Keeffe M, Brown JP, Burrell T, Coupland D, Marcel Dumont S, Ganguli N, Hanley DA, Law-Dillabough A, Lévesque J. Bone mineral densitometry reporting. Canadian Association of Radiologists; 2013. https://car.ca/wp-content/uploads/Technical-Standards-for-Bone-Mineral-Densitometry-Reporting-2013.pdf. Accessed 20 Oct 2019.
Siminoski K, Jiang G, Adachi JD, Hanley DA, Cline G, Ioannidis G, et al. Accuracy of height loss during prospective monitoring for the detection of incident vertebral fractures. Osteoporos Int. 2005;16:403–10.
Siminoski K, Warshawski RS, Jen H, Lee K. The accuracy of historical height loss for the detection of vertebral fractures in postmenopausal women. Osteoporos Int. 2006;17:290–6.
el Miedany YM, Gardiner A, Toth M. Development and validation of a referral model for direct access DXA scanning (DADS) for standard clinical practice. Ann Rheum Dis. 2006;65(supplement II):642.
Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, et al. Official positions of the International Society for Clinical Densitometry and executive summary of 2007 ISCD position development conference. J Clin Densitom. 2008;11:75–91.
Blake GM, Fogelman I. An update on dual-energy x-ray absorptiometry. Semin Nucl Med. 2010;40:62–73.
Hillier TA, Cauley JA, Rizzo JH, Pedula KL, Ensrud KE, Bauer DC, et al. WHO absolute fracture risk models (FRAX): do clinical risk factors improve fracture prediction in older women without osteoporosis? J Bone Miner Res. 2011;26:1774–8.
Tamaki J, Iki M, Kadowaki E, Sato Y, Kajita E, Kagamimori S, et al. Fracture risk prediction using FRAX: a 10-year follow-up survey of the Japanese Population-Based Osteoporosis (JPOS) Cohort Study. Osteoporos Int. 2011;22:3037–45.
Leslie WD, et al. Application of the 1994 WHO classification to populations other than postmenopausal Caucasian women: the 2005 ISCD Official Positions. J Clin Densitom. 2006;9:22–30.
Siminoski K, O’Keeffe M, Lévesque J, Hanley D, Brown JP. Canadian Association of Radiologists technical standards for bone mineral densitometry reporting. Can Assoc Radiol J. 2011;62:166–75.
Fung EB, Bachrach LK, Briody JN, Cowell CT. Reporting DXA scan. Reporting DXA results. In: Sawyer AJ, Bachrach LK, Fung EB, editors. Bone densitometry in growing patients. Current clinical practice. Totowa: Humana Press; 2007. p. 127–36.
Physician’s guide to prevention and treatment of osteoporosis, National Osteoporosis Foundation, Washington, D.C. 2008.
Miedany YE, Gaafary ME, Yassaki AE, Youssef S, Nasr A, Ahmed I. Monitoring osteoporosis therapy: can FRAX help assessing success or failure in achieving treatment goals? World J Rheumatol. 2014;4(2):14–21.
Tothill P. Dual-energy x-ray absorptiometry measurements of total body bone mineral during weight change. J Clin Densitom. 2005;8:31–8.
Simonelli C, Adler RA, Blake GM, Caudill JP, Khan A, Leib E, et al. Dual-energy x-ray absorptiometry technical issues: the 2007 ISCD official positions. J Clin Densitom. 2008;11:109–22.
Bonnick SL. Monitoring osteoporosis therapy with bone densitometry: a vital tool or regression towards mediocrity? J Clin Endocrinol Metab. 2000;85:3493–5.
Gordon CM, Bachrach LK, Carpenter TO, Crabtree N, Fuleihan GE, Kutilek S, et al. Dual energy x-ray absorptiometry interpretation and reporting in children and adolescents: the 2007 ISCD pediatric official positions. J Clin Densitom. 2008;11:43–58.
Rauch F, Plotkin H, DiMeglio L, Engelbert RH, Henderson RC, Munns C, et al. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2007 pediatric official position. J Clin Densitom. 2008;11:22–8.
Webber CE, Sala A, Barr RD. Accounting for body size deviations when reporting bone mineral density variables in children. Osteoporos Int. 2009;20:113–21.
Cole JH, Dowthwaite JN, Scerpella TA, van der Meulen MCH. Correcting fan-beam magnification in clinical densitometry scans of growing subjects. J Clin Densitom. 2009;12:322–9.
Smith CM, Coombs RC, Gibson AT, Eastell R. Adaptation of the Carter method to adjust lumbar spine bone mineral content for age and body size: application to children who were born preterm. J Clin Densitom. 2006;9:114–9.
Crabtree NJ, Kibirige MS, Fordham JN, Banks LM, Muntoni F, Chinn D, et al. The relationship between lean body mass and bone mineral content in paediatric health and disease. Bone. 2004;35:965–72.
Zemel BS, Leonard MB, Kelly A, Lappe JM, Gilsanz V, Oberfield S, et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95:1265–73.
The Writing Group for the ISCD. Position development conference: diagnosis of osteoporosis in men, premenopausal women, and children. J Clin Densitom. 2004;7:17–26.
Binkovitz LA, Henwood MJ, Sparke P. Pediatric DXA: technique, interpretation, and clinical applications. Pediatr Radiol. 2008;8:S227–39.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
El Miedany, Y. (2022). Best Practice Recommendations for DXA Scans and Reports. In: El Miedany, Y. (eds) New Horizons in Osteoporosis Management. Springer, Cham. https://doi.org/10.1007/978-3-030-87950-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-87950-1_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87949-5
Online ISBN: 978-3-030-87950-1
eBook Packages: MedicineMedicine (R0)