Abstract
Occipital neuralgia is a condition that is caused by irritation or pressure on the occipital nerves. The pain can be sharp, jabbing, or shock like and is felt in the back of the head and neck. There are various treatments including occipital nerve blocks. This chapter will provide a brief overview of the condition, treatment options, as well as a description of the occipital nerve block technique.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction: Occipital Neuralgia
-
Occipital neuralgia is a type of headache characterized by piercing, throbbing, or electric-shock-like chronic pain in the upper neck, back of the head, and behind the ears, usually on one side of the head [1].
-
The International Headache Society defines occipital neuralgia as a unilateral or bilateral paroxysmal shooting or stabbing pain in the posterior part of the scalp in the distribution of the greater, lesser, or third occipital nerve, sometimes accompanied by diminished sensation or dysesthesia in the affected area [2].
-
Etiology of occipital neuralgia can include cervical instability, trauma, compression due to vascular abnormalities and mass lesions, due to arthrosis, sclerosis, osteolytic lesions, and Chiari I malformation. Surgeries at the cranio-cervical junction and upper cervical spine may also cause this syndrome.
-
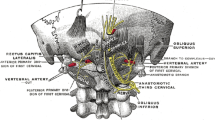
Diagnostic criteria: (1) Occipital headache associated with tenderness over the affected nerve branches. (2) Trigger points at the emergence of the greater occipital nerve or in the distribution of C2. (3) Pain improved by local anesthetic block of the affected nerve(s) (Fig. 50.1).
Treatment
-
Conservative : non-pharmacologic options include heat/cold application, cognitive behavioral therapy, and massage. Pharmacologic options may be preferred by patients over injections or may be used in settings where practitioners are unable to provide occipital nerve blocks. Oral agents have not been systematically studied for their efficacy in occipital neuralgia. Gabapentinoids, tricyclic antidepressants, and baclofen have all been used given their efficacy in other craniocervical pain syndromes. Similarly, carbamazepine has been used for paroxysmal occipital pain.
-
Occipital nerve blocks are often the treatment of choice. They may be diagnostic and therapeutic. Pain relief can last from days to months. They may be performed with or without steroid. The procedure can be repeated as needed, unless steroid is used.
-
Botulinum toxin type A injections and peripheral nerve stimulation have been studied in small cases series.
-
Surgical decompression of occipital nerve in refractory cases.
Anatomy (Fig. 50.1)
-
The greater occipital nerve (GON) arises from dorsal primary rami of C2 (with occasional contribution from C3).
-
GON passes through the semispinalis and trapezius musculature just inferior to the superior nuchal line, then continues alongside the occipital artery superiorly above the fascia and below the galea.
-
The lesser occipital nerve (LON) arises from the ventral primary rami of C2 and C3.
-
LON passes superiorly and laterally from the occiput to the lateral edge of the sternocleidomastoid muscle.
-
LON innervates the scalp in the lateral area of the head posterior to the ear.
-
The third occipital nerve originates from the third cervical spinal nerve, perforates the trapezius muscle, and supplies sensation to the upper posterior neck and lower occipital region of the scalp, medial to the greater occipital nerve territory.
Greater and Lesser Occipital Nerve Block Indications
-
Diagnostic and therapeutic purpose
-
Occipital headaches (occipital neuralgia)
-
Neck pain felt in the upper back of the neck, potentially referring to the occiput, temporal, forehead, and retrobulbar regions of the head.
-
Can be considered in
-
Chronic headaches
-
Cervicogenic headaches
-
Greater and Lesser Occipital Nerve Block Contraindications
-
Coagulopathy
-
Allergies to any of the local anesthetics
-
Infection of the scalp
-
Cervical instability or acute fracture
-
Arnold-Chiari syndrome
Greater and Lesser Occipital Nerve Block Technique
Landmark Based
Landmarks (Fig. 50.2) [3]
-
1.
External occipital protuberance
-
(a)
Midline occipital highest point (inion) on the posterior-inferior occiput of the skull
-
(b)
Insertions for both the nuchal ligament and the trapezius
-
(a)
-
2.
Mastoid process
-
(a)
Posterior to the external acoustic meatus
-
(a)
-
3.
Draw a line between the external occipital protuberance and mastoid process
-
(a)
GON lies 2/3 along the line, close to the occiput
-
(b)
LON lies 1/3 along the line, closer to the mastoid process
-
(a)
Procedure
-
Patient in seated or supine position, neck fully flexed
-
Locate the external occipital protuberance (see above)
-
For GON, injection site is often identified as a point of maximal tenderness and in approximately 2/3 along the line (close to occiput) between the external occipital protuberance and mastoid process.
-
Slowly touch periosteum then slightly withdraw needle
-
Aspirate to minimize intravascular injection
-
Inject 1–2 mL of local anesthetic (steroid can be added)
-
For LON, injection site is often identified as a point of maximal tenderness and located 1/3 along the line (closer to the mastoid process) between the external occipital protuberance and mastoid process.
-
Slowly touch periosteum then slightly withdraw needle
-
Aspirate to minimize intravascular injection
-
Injection 1–2 mL of local anesthetic (steroid can be added)
Risks/Complications
-
The most common complications include bleeding, bruising, swelling, and soreness at the site of injection
-
Infection, local anesthetic toxicity
-
Allergic reaction to the medication
-
Nerve injury
-
Seizure from intravascular injection of local anesthetic
-
Headache exacerbation
Clinical Pearls
-
1.
Occipital nerve block (ONB) can be diagnostic and therapeutic
-
2.
ONB is a simple and safe treatment option for occipital neuralgia.
-
3.
Landmark based ONB is simple and safe, though ultrasound guidance can be used (See references [3, 4])
-
4.
In refractory cases, other treatment options include, botulinum toxin injections, radiofrequency ablation, occipital nerve decompression, occipital or spinal cord stimulation
Questions
-
1.
Greater occipital nerve originates primarily from what cervical nerve root
-
A.
C2 ventral rami
-
B.
C2 dorsal rami
-
C.
C3 ventral rami
-
D.
C3 dorsal rami
-
A.
-
2.
Occipital neuralgia typically presents with the following features, except
-
A.
Tenderness over the posterior scalp
-
B.
Aura prior to the pain
-
C.
Pain behind the ear
-
D.
Recurring paroxysmal attacks
-
A.
-
3.
Which of the following is most likely to respond to occipital nerve blocks
-
A.
Migraines
-
B.
Post herpetic neuralgia
-
C.
Cervicogenic headaches
-
D.
Myofascial cervical pain
-
A.
-
4.
Lesser occipital nerves originates primarily from what cervical nerve roots
-
A.
C2 ventral rami
-
B.
C2 dorsal rami
-
C.
C3 dorsal rami
-
D.
none of the above
-
A.
-
5.
The occipital portion of the skull receives sensory innervation from
-
A.
Spinal accessory nerve (nerve XI)
-
B.
Facial nerve (nerve VII)
-
C.
Maxillary branch of trigeminal nerve (nerve V)
-
D.
None of the above
-
A.
Answers
1. B, 2. B, 3. C, 4. A, 5. D
References
www.ninds.nih.gov/disorders/all-disorders/occipital-neuralgia-information-page.
Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
Palamar D, Uluduz D, Saip S, Erden G, Unalan H, Akarirmak U. Ultrasound-guided greater occipital nerve block: an efficient technique in chronic refractory migraine without aura? Pain Physician. 2015;18(2):153–62.
Pingree MJ, Sole JS, O’Brien TG, Eldrige JS, Moeschler SM. Clinical efficacy of an ultrasound-guided greater occipital nerve block at the level of C2. Reg Anesth Pain Med. 2017;42(1):99–104.
Further Reading
Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. J Korean Med Sci. 2016;31(4):479–88.
Greengrass RA, Narouze S, Bendtsen TF, Hadzic A. Cervical plexus and greater occipital nerve blocks: controversies and technique update. Reg Anesth Pain Med. 2019;44(6):623–6. https://doi.org/10.1136/rapm-2018-100261.
Greher M, Moriggl B, Curatolo M, Kirchmair L, Eichenberger U. Sonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissection. Br J Anaesth. 2010;104(5):637–42.
Inan LE, Inan N, Unal-Artık HA, Atac C, Babaoglu G. Greater occipital nerve block in migraine prophylaxis: narrative review. Cephalalgia. 2019;39(7):908–20. https://doi.org/10.1177/0333102418821669. Epub 2019 Jan 6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Habibi, B.A., Kim, C. (2022). Craniofacial Pain: Occipital Neuralgia and Nerve Block. In: Banik, R.K. (eds) Anesthesiology In-Training Exam Review. Springer, Cham. https://doi.org/10.1007/978-3-030-87266-3_50
Download citation
DOI: https://doi.org/10.1007/978-3-030-87266-3_50
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87265-6
Online ISBN: 978-3-030-87266-3
eBook Packages: MedicineMedicine (R0)