Abstract
Musculoskeletal regenerative medicine encompasses strategies for the regeneration of bone, cartilage, tendon, ligament, muscle, fat, and other connective tissues. Perhaps the greatest unmet need is cartilage preservation, repair, and regeneration. Most of the reported approaches in regenerative medicine for chondral defects and osteoarthritis (OA) have been based on adult stem cells, but pluripotent stem cells also merit a consideration as potential cell sources with their advantage in plasticity and unlimited expansion potential. While embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) are similar to each other in almost all cellular characteristics, iPSCs are preferred to ESCs because iPSCs do not have religious and ethical issues and autogenous iPSCs are free from the risk of immune rejection unlike ESCs. While iPSCs were first induced using either retrovirus or lentivirus, non-integrating vectors are currently preferred for the generation of iPSCs. Several methods to differentiate ESCs/iPSCs toward chondrocytes have been developed. iPSCs may become a useful cell source for regenerative therapies for chondral defects and OA, provided that safe and reliable ways of producing iPSC-derived chondrocytes are established. One of the unique characteristics seen from in vitro chondrogenic differentiation of iPSCs is the low expression of hypertrophic markers. This may indicate that iPSC-derived chondrocytes have a more stable phenotype, unlike mesenchymal stromal cells (MSCs). Also, in vivo studies on iPSC treatment to joints of small animals demonstrated enhanced survival and engraftment of implanted cells after several months. This may increase the chance of articular cartilage regeneration and durable matrix synthesis, rather than primarily paracrine effects on endogenous cells. Further investigations in larger animal models are necessary for a more accurate assessment of the efficacy and safety of in vivo implantation of iPSCs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pluripotent stem cells
- Embryonic stem cells
- Induced pluripotent stem cells
- Cartilage regeneration
- Musculoskeletal tissue
- Osteoarthritis
1 Introduction
Recent advances in regenerative medicine for the musculoskeletal system indicate that stem cell therapies may evolve into an established treatment for many musculoskeletal tissues. The most challenging and potentially important is the preservation of cartilage tissue, reversal of degenerative change, or regeneration of cartilage tissue in chondral defects and osteoarthritis (OA). While most of reported approaches have been based on adult stem cells that have limited potential for expansion, pluripotent stem cells also merit a consideration as potential cell sources. Embryonic stem cells (ESCs), derived from the inner cell mass of the blastocyst [1, 2], and the cells in the germinal ridge of the embryo [3] had been thought to be the only type of known pluripotent cells, until the seminal work of Yamanaka [4] showed that adult cells can be activated to revert to a pluripotent state, generating induced pluripotent stem cells (iPSCs).
ESCs can be expanded almost infinitely, and not undergoing senescence, as typically seen in adult stem cells. However, the derivation of ESCs from the early embryos raises ethical concern, and the inherent immunogenicity associated with allograft transplantation continues to pose limitations for the clinical applications [1,2,3]. iPSCs are induced by reprogramming somatic cells with forced expression of specific transcription factors [5, 6]. iPSCs are similar to the ESCs in gene expression, surface markers, cell morphology, proliferation potential, pluripotency, and several other aspects [7, 8]. However, as iPSCs can be derived from autologous somatic cells of candidate recipients, iPSCs do not involve such religious and ethical issues as in ESCs and are free from the risk of immune rejection [9, 10].
In this chapter, iPSC generation, chondrogenic induction of iPSC, and reported in vivo application of iPSCs for cartilage regeneration and OA treatment are presented and reviewed from the author’s perspectives.
2 Generation of iPSCs
2.1 Methods Used to Reprogram Somatic Cells into iPSCs
iPSCs were first generated from dermal fibroblasts in vitro by retroviral transduction and forced expression of genes of four transcription factors Oct-4, Sox-2, Klf-4, and c-Myc also called Yamanaka factors [5, 6]. These four factors were identified by testing numerous combinations of 24 factors that are plentifully expressed in ESCs. These factors reprogram the nuclei of somatic cells to make them pluripotent. These cells generated teratomas which contained tissues from all three germ layers, when transplanted into immunodeficient mice, indicating their pluripotency [11].
Theoretically, any actively dividing somatic cell type may be reprogrammed. Therefore, iPSCs have been induced from various somatic cells [5, 6, 12,13,14]. Skin fibroblast has been the most frequently used cells for reprogramming due to efficiency, safety, and minimal morbidity in harvesting cells. On the other hand, the easy accessibility and even lower harvesting invasiveness of blood cells can make them further attractive cellular sources [15]. The efficiency in reprogramming for iPSC generation varies with different somatic cell sources. While reprogramming efficiency is quite important in investigating reprogramming and its mechanism in the laboratory setting, it may not be a critical variable when generating iPSCs for clinical application. In this case, selection of the optimal iPSC clones and documentation of their safety and quality become more important.
In the beginning, iPSCs were induced using either retrovirus [5] or lentivirus [6]. However, these viral vectors are associated with insertional mutagenesis and tumor formation due to the random integration of transgenes [16, 17]. Therefore, non-integrating vectors, such as adenovirus [18] and Sendai virus [19], are currently preferred for the generation of iPSCs. Adenovirus has a low efficiency and kinetics, while the Sendai virus shows fairly efficient transduction. In addition, nonviral methods to generate integration-free iPSCs have been developed, including plasmids [20], recombinant proteins [21, 22], mRNAs [23], episomal vectors [24], and piggybacks [25, 26]. Even small molecule combinations are known to induce iPSCs [27, 28].
2.2 Epigenetic Signature of iPSCs
Although the hiPSCs fundamentally share the properties of hESCs, there is evidence that their differentiation to a lineage related to their origin is more facilitated [64], probably due to residual epigenetic memory [7, 29].
iPSCs repeat errors in DNA methylation during the reprogramming process [30], though it has not been proven whether these epigenetic abnormalities are the result of cellular reprogramming itself or of the iPSC induction methods. While this has posed concerns about the safety and stability of the iPSCs, ESCs and iPSCs showed very few consistent differences in the gene expression profiles [31]. Also, the different epigenetic signatures observed initially in the iPSCs dissipate with prolonged passaging, suggesting that cell-specific memory may not be functionally relevant [29]. The origin of primary cells may also influence the reprogramming and differentiation thereafter. Rim et al. [32] reprogrammed hiPSCs from four different types of primary cells such as dermal fibroblasts (DF), peripheral blood mononuclear cells (PBMC), cord blood mononuclear cells (CBMC), and OA fibroblast-like synoviocytes (OAFLS). Established hiPSCs were differentiated into chondrogenic pellets. All told, the relative rank of expression of cartilage-specific markers was CBMC > DF > PBMC > FLS. On the other hand, Nasu et al. [33] generated genetically matched human iPSCs from different origins using bone marrow stromal cells and dermal fibroblasts of the same donor. Global gene expression profile, DNA methylation status, and the chondrogenic and osteogenic differentiation properties of each lineage were analyzed. After cell autonomous and induced differentiation, each iPSC clone exhibited various differentiation properties, which did not correlate with the cell of origin.
3 Induction of Chondrogenesis from iPSCs
Several methods to differentiate ESCs/iPSCs toward chondrocytes have been developed. These methods can be interchangeably used for both ESCs and iPSCs. ESCs and iPSCs can be expanded almost indefinitely due to their capacity for self-renewal [33, 34]. With enhanced efficiency and low cost of induction, iPSCs may become a useful cell source for regenerative medicine for chondral defects and OA, provided that safe and reliable ways of producing chondrocytes from these cells are established [12].
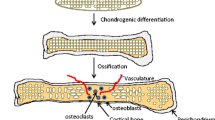
To employ the iPSC technology for cartilage regeneration, it is very important to understand the normal developmental processes of chondrocytes. Cartilage formation is regulated by a number of signal transduction pathways that regulate a series of events, including condensation of mesenchymal cells and nodule formation followed by chondrogenic differentiation, the hallmark of which is the expression of Sox-9. Several critical signaling molecules regulate this process, including soluble factors such as transforming growth factor beta (TGF-β), Wnt and cell adhesion molecules, bone morphogenetic proteins (BMPs), and fibroblast growth factors (FGFs). These factors activate essential targets to initiate and maintain chondrocyte phenotypes [35]. Induction of chondrogenesis from iPSCs is not yet standardized, with several different methods showing variable results. Protocols for chondrogenic differentiation of ESCs/iPSCs are grouped into four categories [36].
-
1.
Co-culture with primary chondrocytes either in direct [37] or indirect ways [33, 38].
- 2.
-
3.
Through generation of intermediate induced mesenchymal stromal cells (iMSCs) and subsequent differentiation into chondrocytes [41, 42].
-
4.
Direct chondrogenic differentiation using chondro-inductive factors [43, 44].
3.1 Co-Culture with Primary Chondrocytes
Co-culture takes advantage of paracrine factors secreted from the chondrocytes that can stimulate the differentiation of iPSCs into chondrocytes [34, 36]. On the other hand, co-culture conditions may increase the risk of contamination by other undesired cells [45]. The direct co-culture [38] has higher risk of contamination compared to the indirect co-culture [33, 37].
This strategy was reported by Wei et al. using human healthy chondrocytes [34] and Qu et al. using bovine articular chondrocytes [46]. Adding BMPs or other TGF-β family molecules to the culture medium may improve the quality of chondrogenic differentiation [47].
3.2 Via Embryoid Body Formation
Chondrogenic differentiation of iPSCs via EB formation is the most commonly used approach to obtain hiPSC-derived chondrocytes [48]. The process involves the formation of EBs, allowing auto-induction (spontaneous differentiation) of MSC-like cells as fibroblastic outgrowths from the EBs, followed by induction of chondrogenic differentiation of the MSCs [39]. The main disadvantages of this method are the potential for unpredictable differentiation, heterogeneous cell populations, and low efficiency. EB’s three-dimensional (3D) structure is similar to that in the early post-implantation embryo; thus the cells in the EB can differentiate into cells of three germ layers [49]. However, several groups employed this strategy with some success [50,51,52,53].
3.3 Through Intermediate iMSC
In this strategy, iPSCs are stimulated exogenously to differentiate into an MSC-like population (iMSC), followed by differentiation to chondrocytes. As this method directly generates MSCs, it can limit the spontaneous differentiation of iPSCs into undesired cell types, even though these iMSCs may be more prone to differentiate into fibro- and hypertrophic cartilage [34, 36].
Zou et al. [54] derived iMSCs from human iPSCs by culturing the iPSCs in MSC differentiation medium containing DMEM-low glucose and 10% fetal bovine serum, followed by serial trypsinization-based passaging. For chondrogenic differentiation, pellets were formed and cultured in chondrogenic medium containing TGF-β3. Similarly, other groups reported other approaches involving direct induction of hMSCs under specific cell culture conditions, followed by chondrogenic differentiation with TGF-β3 [55] or TGF-β3 and BMP2 [56]. Another strategy for generating MSCs from iPSCs utilized specific coatings during cell culture. Liu et al. reported a one-step method to derive MSC-like cells from hiPSCs using plates coated with fibrillar type I collagen. This thin layer of collagen fibrils on the plates successfully stimulated the derivation of MSC-like cells [57].
3.4 Direct Differentiation Using Growth Factors
This approach, also known as directed differentiation, is grounded on mimicking the events during the embryo development [17, 48]. Using different mixtures of defined factors at different developmental stages, a defined protocol to direct differentiation of the pluripotent stem cells toward the chondrocytes was reported [44]. Cheng et al. [49] successfully applied an iPSC protocol that had been developed for the direct differentiation of hESCs toward chondrocytes. This protocol involves the use of different growth factors including activin-A, Wnt3a, FGF2, BMP4, neurotrophin-4, and growth differentiation factor 5 (GDF5) in a timed sequence at specific concentrations. This protocol is also applied by Saito et al. to differentiate hiPSCs with similar results [58]. Protocol of Yamashita et al. [59] includes initially differentiating hiPSCs into mesodermal cells and then culturing them in chondrogenic medium containing TGF-β1, BMP2, GDF5, and ascorbic acid. Thereafter, chondro-induced cells are sorted according to type II collagen expression and cultured in 3D. Protocol of Borestrom et al. [14] comprises a 3D pellet pre-differentiation followed by monolayer expansion of chondrogenic progenitors. These progenitors are subsequently cultured in a second chondrogenic 3D pellet and differentiated into chondrocytes using chondrogenic medium containing growth factors.
It is not yet clear which is the best method for deriving chondrocytes from iPSCs as each reported protocol used different iPSC lines derived from different somatic cell types, has different genetic backgrounds, and employed different reprogramming methods [47, 60]. One of the unique characteristics seen in in vitro chondrogenic differentiation of iPSCs is the low expression of hypertrophic markers such as type X collagen and alkaline phosphatase [61,62,63]. The difference can be attributed to the heavier methylation of promotor sites of hypertrophic genes [63]. Lower expression of hypertrophic markers may mean that chondrocytes derived from iPSCs have stable phenotypes, unlike chondroid cell-derived traditional MSC populations. If true, this may represent a profound advantage for iPSCs as a cell source for the regeneration of articular cartilage.
4 The Use of iPSCs for Cartilage Regeneration
iPSCs can be a promising cell source for cartilage tissue engineering because plenty of accessible and autologous cells are available iPSC fabrication. iPSCs bypass ethical concerns and overcome the limited proliferation potential of adult cells such as MSCs or chondrocytes [64]. hiPSC-derived chondrocytes are more similar to juvenile chondrocytes. Cartilage from juveniles has more anabolic activity and is less antigenic than those from adults [65,66,67]. This reduced antigenicity may imply that cartilaginous tissue derived from a single allogeneic hiPSC or hESC clone could be used for many patients. This, in turn, could allow greater flexibility in iPSC clone selection and control the quality and lower the clinical cost of this regenerative cell therapies.
To apply iPSCs for cartilage repair, efficient and reproducible protocols to differentiate iPSCs toward chondrocytes are necessary. While a number of protocols for chondrogenic differentiation are described, so far there is no general agreement on the best approach to obtain chondrocytes from iPSCs. It is premature to state that iPSCs are better than MSCs for cartilage regeneration. On the other hand, iPSCs can resolve several issues, including cell number, accessibility, engraftment, or phenotype loss with passaging.
A number of in vivo preclinical assessments have been reported testing the use of iPSC-derived cells to treat chondral defects and OA. Zhu et al. [68] investigated the repair of cartilage defects in osteoarthritic rats with hiPSC-derived chondrocytes. 106 chondro-induced hiPSCs were injected into chemical OA-induced knees of rats. After 15 weeks transplantation, no immune responses were observed, micro-CT showed improvement of subchondral plate integrity, and histological examinations demonstrated articular cartilage matrix production. Rim et al. tested the repair potential of human iPSC-derived chondrocytes in a rat osteochondral defect model. hiPSC-derived chondrocytes were either implanted as pellets or injected into the joint. Both transplanted chondrogenic pellets and chondrocytes had positive effects in the osteochondral defect rat model. Detection of human proteins in the joints proved that the cells were successfully delivered and retained in the defect [62].
Kotaka et al. [69] investigated the effect of magnetically labeled iPSCs (m-iPSCs) delivered into an osteochondral defect by magnetic field on the repair of articular cartilage. The histologic grading score was significantly better in the treatment group compared to the control group. m-iPSCs maintained pluripotency, and the magnetic delivery system proved useful and safe for cartilage repair using iPSCs. Xu et al. [70] evaluated the use of MSCs derived from hiPSCs for the regeneration of cartilage defects in a rabbit model. Cartilage defects were made in the patellar grooves of New Zealand white rabbits. MSCs were generated from hiPSCs via a step of EB formation. Following flow cytological analysis, the hiPSCs-MSCs were plated onto poly(lactic-co-glycolide) and then transplanted into the cartilage defects in the experimental group. At 6 weeks, cartilage-like tissue was observed in the experimental group but not in the control or scaffold implantation groups. Chijimatsu et al. [56] investigated the feasibility of MSC-like cells originated from iPSCs via neural crest cells (NCCs) for osteochondral repair. Initially, MSC-like cells derived from iPSC-NCCs (iNCCs) were generated and characterized in vitro. When iNCC-derived tissue-engineered constructs were implanted into rat osteochondral defects, the implanted cells remained alive at the implanted site, whereas they failed to repair the defects, with only scarce development of osteochondral tissue in vivo. Our group implanted human iPSCs-derived chondrocytes into immunosuppressed rats. Cartilage was regenerated in the defects created in the articular cartilage of these rats, without any teratoma or tumor formation, suggesting that iPSC-derived chondrocytes are a promising source of cells for transplantation (Fig. 30.1) [63].
To investigate whether chondro-induced hiPSCs promote cartilage repair, hiPSCs in either pellet state or alginate hydrogel were implanted in the osteochondral defects created on the patellar groove of immunosuppressed rats, and the status of the created defects was observed 12 weeks after implantation. The defects treated with chondro-induced hiPSC implantation were repaired with smooth, glistening, firm tissue, while the control defects showed raw surface with or without thin fibrous covering tissue (a). Histological appearance revealed good restoration of the articular surface albeit with reduced amount of proteoglycans compared with adjacent normal cartilage in the defects treated with hiPSC-pellets (group 3) or hiPSC-alginate hydrogel (group 4). On the other hand, the control defects (group 1) and defects treated with alginate alone (group 2) showed little evidence of cartilage regeneration (b). Immunohistochemistry for human nuclear antigen in groups 3 and 4 revealed that the majority of cells inside the regenerated cartilage were implanted hiPSCs and that hiPSCs successfully engrafted in the created defect (c). The macroscopic score was significantly better in groups 3 and 4 than that in groups 1 and 2 (P < 0.05). Groups 3 and 4 also had a significantly better histological score than group 1 (P < 0.05, d). Bar represents mean ± SE. N = 6, *P < 0.05 (reproduced with permission from Ko et al., Biomaterials. 2014 Apr;35(11):3571–81)
It remains to be proven that chondrogenically differentiated hiPSCs can definitely generate articular cartilage that are equal to natural hyaline cartilage in vivo. Further, in order to minimize the risk of teratoma in in vivo implantation, undifferentiated cells should not be left behind after the differentiation of iPSCs into chondrocytes. It should be also remembered that the reprogramming process in iPSCs can add another potential risk of tumor formation not present in ESCs. The efficacy and safety of such transplantation remain to be investigated in larger animal models, to provide a more accurate assessment of the repair capacity of iPSCs [71].
Of note, in vivo studies of iPSC treatment to regenerate cartilage in osteochondral defects or OA have demonstrated the survival and engraftment of implanted or injected chondro-induced iPSCs for several months. This is distinctly different from MSCs which mostly disappear from the joint within 1–3 weeks [62, 63]. While those results are very encouraging and approach the original concept of cell therapy, corroboration of this finding is necessary in large animal models of longer follow-up.
5 Strategy for Clinical Application: iPSC Banking
While patient-specific iPSCs are a possibility with huge advantages, individual preparation of iPSCs under good manufacturing practice (GMP) guidelines can be expensive. To tackle this issue, allogeneic clinical iPSC cell line banks should be considered for lowering the cost of iPSC therapy [72, 73]. iPSC banks can be set up with samples from homozygous donors for common HLA types. Chondro-induced iPSCs with an HLA type that matches the patient’s HLA types can be selected from the iPSC bank and used for transplantation. It is much less difficult to prepare homozygous HLA hiPSCs than hESCs. Individuals who bear homozygous HLA types and are willing to donate their somatic cells for iPSC generation are far more easily found than embryo donors for ESC generation [72].
The avascular nature of cartilage provides some protection against host immune response to some extent compared with other tissues. It is evidenced from reports that transplanted cartilage from unrelated donors elicits little acute or chronic immune response [64, 74]. Allogeneic cartilage has been transplanted in a large number of patients without matching for HLA types and without the administration of immunosuppressive drugs. The allogeneic transplantation of particulated juvenile articular cartilage has also shown good clinical results [75].
Thus, it may be possible to transplant iPSC bank-derived chondrocytes with less optimal HLA matching compared with other cell types. However, it remains to be seen how much of HLA matching is required for successful allogeneic transplantation of cartilage or chondrocytes [76].
6 Direct Conversion to Chondrocytes Without the Need for iPSCs
Somatic cells can be directly converted to another type without going through the generation of iPSCs. Cell type conversion has been demonstrated in some cell types. The transduction of fibroblasts with MyoD results in conversion into myoblasts [77]. Fibroblasts can be converted into neurons by the forced expression of Ascl1, Brn2, and Myt1l [78]. Also, cardiomyocytes can be generated from fibroblasts by forced expression of Gata4, Mef2c, and Tbx5 [79].
The Tsumaki group [80] reported the generation of induced chondrocytes (iChon) from mouse and human fibroblasts using two reprogramming factors (c-Myc and Klf -4) and one cartilage forming factor (Sox-9). The resulting iChon cells form hyaline cartilage expressing only type II collagen. As iChon cells did not express Nanog, a marker of pluripotent cells, these cells would not theoretically cause teratoma. While in vivo direct conversion for the treatment of OA has not been reported until now, the technique is likely to materialize in the near future with recent advancements in in vivo gene transfer and smart biomaterials. In vivo direct conversion might be applied in vivo to rejuvenate diseased chondrocytes that have lost the chondrocyte phenotypes or to convert synovial or connective tissue progenitors resident in the bone marrow into chondrocytes when used in combination with microfracture. In vivo direct conversion could be a relatively non-invasive method for cartilage regeneration if converting vectors can be applied into the OA lesion topical or arthroscopic placement while excluding exposure and potential reprogramming of synovial tissues.
7 Conclusions
Starting from the initial report by Yamanaka et al. who used retroviral transduction to reprogram somatic cells into iPSCs, numerous methods were developed to generate iPSCs. The efficiency of induction has also greatly improved, which makes patient-derived iPSCs a clinical possibility with decreased cost. An efficient nonviral induction method would greatly enhance the safety of iPSCs. While the attempts for clinical application of iPSCs started with a focus on retinal or neural disease, it has potential applications in cartilage repair and OA if lower cost and impeccable control over cartilage differentiation and safety can be achieved.
The enhanced survival and engraftment are critical for restoring cartilage form and function. As the prime purpose of cell therapy in OA is the improvement of structure in articular cartilage by regeneration, enhanced survival and engraftment would increase the chance of matrix synthesis and cartilage regeneration by the implanted cells, rather than reliance on paracrine effects targeting endogenous cells. On the other hand, unlike adult stem cells, safety issues in terms of teratoma formation from insufficiently differentiated cells pose risk to the use of iPSCs for a nonlethal disease such as OA.
There is relative lack of in vivo investigation of iPSC implantation compared with culture-expanded MSCs. While comparable or even better results were reported in small animals compared with MSCs, it is not known whether the same good results can be obtained in large animals. The efficacy and safety of such transplantation remain to be investigated in larger animal models, which would allow for a more accurate assessment of the repair capabilities of iPSCs.
Take-Home Messages
-
Pluripotent stem cells merit a consideration as potential cell sources for cartilage regeneration with their advantage in terms of unlimited expansion potential.
-
Despite similar cellular characteristics, iPSCs are preferred to ESCs because iPSCs do not have religious and ethical issues and autogenous iPSCs are free from the risk of immune rejection.
-
iPSCs may become a useful cell source for regenerative therapies for chondral defects and OA, provided that safe and reliable ways of producing iPSC-derived chondrocytes are established.
-
Low expression of hypertrophic markers is seen during in vitro chondrogenic differentiation of iPSCs, suggesting a more stable phenotype in iPSC-derived chondrocytes.
-
iPSCs show enhanced survival and engraftment when implanted in vivo, which may increase the chance of articular cartilage regeneration and durable matrix synthesis.
References
Evans MJ, Kaufman MH. Establishment in culture of pluripotential cells from mouse embryos. Nature. 1981;292:154–6.
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7.
Nichols J, Smith A. The origin and identity of embryonic stem cells. Development. 2007;138:3–8.
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–76.
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–20.
Kim K, Doi A, Wen B, Ng K, Zhao R, Cahan P, et al. Epigenetic memory in induced pluripotent stem cells. Nature. 2010;467:285–90.
Huang C, Jiang S-W. Induced pluripotent stem cells (iPSCs): safe and efficient induction strategies. Chin J Biochem Mol Biol. 2012;28:1005–10.
Guha P, Morgan JW, Mostoslavsky G, Rodrigues NP, Boyd AS. Lack of immune response to differentiated cells derived from syngeneic induced pluripotent stem cells. Cell Stem Cell. 2013;12:407–12.
Morizane A, Doi D, Kikuchi T, Okita K, Hotta A, Kawasaki T, et al. Direct comparison of autologous and allogeneic transplantation of iPSC-derived neural cells in the brain of a nonhuman primate. Stem Cell Rep. 2013;1:283–92.
Okita K, Ichisaka T, Yamanaka S. Generation of germline-competent induced pluripotent stem cells. Nature. 2007;448:313–7.
Lee J, Kim Y, Yi H, Diecke S, Kim J, Jung H, et al. Generation of disease-specific induced pluripotent stem cells from patients with rheumatoid arthritis and osteoarthritis. Arthritis Res Ther. 2014;16:R41.
Aasen T, Raya A, Barrero MJ, Garreta E, Consiglio A, Gonzalez F, et al. Efficient and rapid generation of induced pluripotent stem cells from human keratinocytes. Nat Biotechnol. 2008;26:1276–84.
Borestrom C, Simonsson S, Enochson L, Bigdeli N, Brantsing C, Ellerstrom C, et al. Footprint-free human induced pluripotent stem cells from articular cartilage with redifferentiation capacity: a first step toward a clinical-grade cell source. Stem Cells Transl Med. 2014;3:433–47.
Li Y, Liu T, Van Halm-Lutterodt N, Chen J, Su Q, Hai Y. Reprogramming of blood cells into induced pluripotent stem cells as a new cell source for cartilage repair. Stem Cell Res Ther. 2016;7:31.
Tapia N, Schöler HR. Molecular obstacles to clinical translation of iPSCs. Cell Stem Cell. 2016;19:298–309.
Augustyniak E, Trzeciak T, Richter M, Kaczmarczyk J, Suchorska W. The role of growth factors in stem cell-directed chondrogenesis: a real hope for damaged cartilage regeneration. Int Orthop. 2015;39:995–1003.
Stadtfeld M, Nagaya M, Utikal J, Weir G, Hochedlinger K. Induced pluripotent stem cells generated without viral integration. Science. 2008;322:945–9.
Ban H, Nishishita N, Fusaki N, Tabata T, Saeki K, Shikamura M, et al. Efficient generation of transgene-free human induced pluripotent stem cells (iPSCs) by temperature-sensitive Sendai virus vectors. Proc Natl Acad Sci U S A. 2011;108:14234–9.
Okita K, Nakagawa M, Hong H, Ichisaka T, Yamanaka S. Generation of mouse induced pluripotent stem cells without viral vectors. Science. 2008;322:949–53.
Zhou H, Wu S, Joo JY, Zhu S, Han DW, Lin T, et al. Generation of induced pluripotent stem cells using recombinant proteins. Cell Stem Cell. 2009;4:381–4.
Kim D, Kim CH, Moon JI, Chung YG, Chang MY, Han BS, et al. Generation of human induced pluripotent stem cells by direct delivery of reprogramming proteins. Cell Stem Cell. 2009;4:472–6.
Warren L, Manos PD, Ahfeldt T, Loh YH, Li H, Lau F, et al. Highly efficient reprogramming to pluripotency and directed differentiation of human cells with synthetic modified mRNA. Cell Stem Cell. 2010;7:618–30.
Yu J, Hu K, Smuga-Otto K, Tian S, Stewart R, Slukvin II, et al. Human induced pluripotent stem cells free of vector and transgene sequences. Science. 2009;324:797–801.
Woltjen K, Michael IP, Mohseni P, Desai R, Mileikovsky M, Hämäläinen R, et al. PiggyBac transposition reprograms fibroblasts to induced pluripotent stem cells. Nature. 2009;458:766–70.
Kaji K, Norrby K, Paca A, Mileikovsky M, Mohseni P, Woltjen K. Virus-free induction of pluripotency and subsequent excision of reprogramming factors. Nature. 2009;458:771–5.
Long Y, Wang M, Gu H, Xie X. Bromodeoxyuridine promotes full chemical induction of mouse pluripotent stem cells. Cell Res. 2015;25:1171–4.
Hou P, Li Y, Zhang X, Liu C, Guan J, Li H, et al. Pluripotent stem cells induced from mouse somatic cells by small-molecule compounds. Science. 2013;341:651–4.
Polo JM, Liu S, Figueroa ME, Kulalert W, Eminli S, Tan KY, et al. Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat Biotechnol. 2010;28:848–56.
Ma H, Morey R, O’Neil RC, He Y, Daughtry B, Schultz MD, et al. Abnormalities in human pluripotent cells due to reprogramming mechanisms. Nature. 2014;511:177–83.
Guenther MG, Frampton GM, Soldner F, Hockemeyer D, Mitalipova M, Jaenisch R, et al. Chromatin structure and gene expression programs of human embryonic and induced pluripotent stem cells. Cell Stem Cell. 2010;7:249–57.
Rim YA, Nam Y, Park N, Jung H, Jang Y, Lee J, et al. Different Chondrogenic potential among human induced pluripotent stem cells from diverse origin primary cells. Stem Cells Int. 2018;2018:9432616.
Nasu A, Ikeya M, Yamamoto T, Watanabe A, Jin Y, Matsumoto Y, Hayakawa K, Amano N, Sato S, Osafune K, Aoyama T, Nakamura T, Kato T, Toguchida J. Genetically matched human iPS cells reveal that propensity for cartilage and bone differentiation differs with clones, not cell type of origin. PLoS One. 2013;8(1):e53771.
Wei Y, Zeng W, Wan R, Wang J, Zhou Q, Qiu S, et al. Chondrogenic differentiation of induced pluripotent stem cells from osteoarthritic chondrocytes in alginate matrix. Eur Cell Mater. 2012;23:1–12.
Matta C, Mobasheri A. Regulation of chondrogenesis by protein kinase C: emerging new roles in calcium signalling. Cell Sign. 2014;26:979–1000.
Tsumaki N, Okada M, Yamashita A. iPS cell technologies and cartilage regeneration. Bone. 2015;70:48–54.
Bigdeli N, Karlsson C, Strehl R, Concaro S, Hyllner J, Lindahl A. Coculture of human embryonic stem cells and human articular chondrocytes results in significantly altered phenotype and improved chondrogenic differentiation. Stem Cells. 2009;27:1812–21.
Hwang NS, Varghese S, Elisseeff J. Derivation of chondrogenically-committed cells from human embryonic cells for cartilage tissue regeneration. PLoS One. 2008;3:e2498.
Kawaguchi J, Mee PJ, Smith AG. Osteogenic and chondrogenic differentiation of embryonic stem cells in response to specific growth factors. Bone. 2005;36:758–69.
Yang Z, Sui L, Toh WS, Lee EH, Cao T. Stage-dependent effect of TGF-beta1 on chondrogenic differentiation of human embryonic stem cells. Stem Cells Dev. 2009;18:929–40.
Lian Q, Lye E, Suan Yeo K, Khia Way Tan E, Salto-Tellez M, Liu TM, et al. Derivation of clinically compliant MSCs from CD105þ, CD24- differentiated human ESCs. Stem Cells. 2007;25:425–36.
Drissi H, Gibson JD, Guzzo RM, Xu RH. Derivation and chondrogenic commitment of human embryonic stem cell-derived mesenchymal progenitors. Methods Mol Biol. 2015;1330:65–78.
Tanaka H, Murphy CL, Murphy C, Kimur M, Kawai S, Polak JM. Chondrogenic differentiation of murine embryonic stem cells: effects of culture conditions and dexamethasone. J Cell Biochem. 2004;93:454–62.
Oldershaw RA, Baxter MA, Lowe ET, Bates N, Grady LM, Soncin F, et al. Directed differentiation of human embryonic stem cells toward chondrocytes. Nat Biotech. 2010;28:1187–94.
Lietman SA. Induced pluripotent stem cells in cartilage repair. World J Orthop. 2016;7:149–55.
Qu C, Puttonen KA, Lindeberg H, Ruponen M, Hovatta O, Koistinaho J, et al. Chondrogenic differentiation of human pluripotent stem cells in chondrocyte co-culture. Int J Biochem Cell Biol. 2013;45:1802–12.
Castro-Viñuelas R, Sanjurjo-Rodríguez C, Piñeiro-Ramil M, Hermida-Gómez T, Fuentes-Boquete IM, de Toro-Santos FJ, et al. Induced pluripotent stem cells for cartilage repair: current status and future perspectives. Eur Cell Mater. 2018;36:96–109.
Suchorska WM, Augustyniak E, Richter M, Trzeciak T. Comparison of four protocols to generate chondrocyte-like cells from human induced pluripotent stem cells (hiPSCs). Stem Cell Rev. 2017;13:299–308.
Cheng A, Kapacee Z, Peng J, Lu S, Lucas RJ, Hardingham TE, et al. Cartilage repair using human embryonic stem cell-derived chondroprogenitors. Stem Cells Transl Med. 2014;3:1287–94.
Craft AM, Rockel JS, Nartiss Y, Kandel RA, Alman BA, Keller GM. Generation of articular chondrocytes from human pluripotent stem cells. Nat Biotechnol. 2015;33:638–45.
Umeda K, Zhao J, Simmons P, Stanley E, Elefanty A, Nakayama N. Human chondrogenic paraxial mesoderm, directed specification and prospective isolation from pluripotent stem cells. Sci Rep. 2012;2:455–66.
Lee J, Taylor SE, Smeriglio P, Lai J, Maloney WJ, Yang F, et al. Early induction of a prechondrogenic population allows efficient generation of stable chondrocytes from human induced pluripotent stem cells. FASEB J. 2015;29:3399–410.
Medvedev SP, Grigor’eva EV, Shevchenko AI, Malakhova AA, Dementyeva EV, Shilov AA, et al. Human induced pluripotent stem cells derived from fetal neural stem cells successfully undergo directed differentiation into cartilage. Stem Cells Dev. 2011;20:1099–112.
Zou L, Luo Y, Chen M, Wang G, Ding M, Petersen CC, et al. A simple method for deriving functional MSCs and applied for osteogenesis in 3D scaffolds. Sci Rep. 2013;3:2243.
Nejadnik H, Diecke S, Lenkov OD, Chapelin F, Donig J, Tong X, et al. Improved approach for chondrogenic differentiation of human induced pluripotent stem cells. Stem Cell Rev. 2015;11:242–53.
Chijimatsu R, Ikeya M, Yasui Y, Ikeda Y, Ebina K, Moriguchi Y, et al. Characterization of mesenchymal stem cell-like cells derived from human iPSCs via neural crest development and their application for osteochondral repair. Stem Cells Int. 2017;2017:1960965.
Liu Y, Goldberg AJ, Dennis JE, Gronowicz GA, Kuhn LT. One-step derivation of mesenchymal stem cell (MSC)-like cells from human pluripotent stem cells on a fibrillar collagen coating. PLoS One. 2012;7:e33225.
Saito T, Yano F, Mori D, Kawata M, Hoshi K, Takato T, et al. Hyaline cartilage formation and tumorigenesis of implanted tissues derived from human induced pluripotent stem cells. Biomed Res. 2015;36:179–86.
Yamashita A, Morioka M, Yahara Y, Okada M, Kobayashi T, Kuriyama S, et al. Generation of scaffoldless hyaline cartilaginous tissue from human iPSCs. Stem Cell Reports. 2015;4:404–18.
Lach M, Trzeciak T, Richter M, Pawlicz J, Suchorska W. Directed differentiation of induced pluripotent stem cells into chondrogenic lineages for articular cartilage treatment. J Tissue Eng. 2014;30:5:2041731414552701.
Diederichs S, Klampfleuthner FAM, Moradi B, Richter W. Chondral differentiation of induced pluripotent stem cells without progression into the endochondral pathway. Front Cell Dev Biol. 2019;7:270.
Rim YA, Nam Y, Park N, Lee J, Park SH, Ju JH. Repair potential of nonsurgically delivered induced pluripotent stem cell-derived chondrocytes in a rat osteochondral defect model. J Tissue Eng Regen Med. 2018;12(8):1843–55.
Ko JY, Kim KI, Park S, Im GI. In vitro chondrogenesis and in vivo repair of osteochondral defect with human induced pluripotent stem cells. Biomaterials. 2014;35:3571–81.
Diekman BO, Christoforou N, Willard VP, Sun HS, Sanchez-Adams J, Leong KW, et al. Cartilage tissue engineering using differentiated and purified induced pluripotent stem cells. Proc Natl Acad Sci U S A. 2012;109:19172–7.
Adkisson HD, Milliman C, Zhang X, Mauch K, Maziarz RT, Streeter PR. Immune evasion by neocartilage-derived chondrocytes: implications for biologic repair of joint articular cartilage. Stem Cell Res. 2010;4(1):57–68.
AdkssonHD MJA, Amendola RL, Milliman C, Mauch KA, Katwal AB, Seyedin M, Amendola A, Streeter PR, Buckwalter JA. The potential of human allogeneic juvenile chondrocytes for restoration of articular cartilage. Am J Sports Med. 2010;38(7):1324–33.
Lee J, Smeriglio P, Chu CR, Bhutani N. Human iPSC-derived chondrocytes mimic juvenile chondrocyte function for the dual advantage of increased proliferation and resistance to IL-1beta. Stem Cell Res Ther. 2017;8(1):244.
Zhu Y, Wu X, Liang Y, Gu H, Song K, Zou X, Zhou G. Repair of cartilage defects in osteoarthritis rats with induced pluripotent stem cell derived chondrocytes. BMC Biotechnol. 2016;16(1):78.
Kotaka S, Wakitani S, Shimamoto A, Kamei N, Sawa M, Adachi N, Ochi M. Magnetic targeted delivery of induced pluripotent stem cells promotes articular cartilage repair stem. Cells Int. 2017;2017:9514719.
Xu X, Shi D, Liu Y, Yao Y, Dai J, Xu Z, et al. In vivo repair of full-thickness cartilage defect with human iPSC-derived mesenchymal progenitor cells in a rabbit model. Exp Ther Med. 2017;14:239–45.
Liu H, Yang L, Yu FF, Wang S, Wu C, Cu C, Lammi MJ, Guo X. The potential of induced pluripotent stem cells as a tool to study skeletal dysplasias and cartilage-related pathologic conditions. Osteoarthr Cartil. 2017;25(5):616–24.
Okita K, Matsumura Y, Sato Y, Okada A, Morizane A, Okamoto S, et al. A more efficient method to generate integration-free human iPS cells. Nat Methods. 2011;8:409–12.
Turner M, Leslie S, Martin NG, Peschanski M, Rao M, Taylor CJ, et al. Toward the development of a global induced pluripotent stem cell library. Cell Stem Cell. 2013;13:382–4.
Chesterman PJ, Smith AU. Homotransplantation of articular cartilage and isolated chondrocytes. An experimental study in rabbits. J Bone Joint Surg Br. 1968;50:184–97.
Farr J, Tabet SK, Margerrison E, Cole BJ. Clinical, radiographic, and histological outcomes after cartilage repair with particulated juvenile articular cartilage: a 2-year prospective study. Am J Sports Med. 2014;42(6):1417–25.
Yamashita A, Tamamura Y, Morioka M, Karagiannis P, Shima N, Nsumaki N. Considerations in hiPSC-derived cartilage for articular cartilage repair. Inflamm Regen. 2018;38:17.
Davis RL, Weintraub H, Lassar AB. Expression of a single transfected cDNA converts fibroblasts to myoblasts. Cell. 1987;51:987–1000.
Vierbuchen T, Ostermeier A, Pang ZP, Kokubu Y, Sudhof TC, Wernig M. Direct conversion of fibroblasts to functional neurons by defined factors. Nature. 2010;463:1035–41.
Ieda M, Fu JD, Delgado-Olguin P, Vedantham V, Hayashi Y, Bruneau BG, et al. Direct reprogramming of fibroblasts into functional cardiomyocytes by defined factors. Cell. 2010;142:375–86.
Outani H, Okada M, Yamashita A, Nakagawa K, Yoshikawa H, Tsmaki N. Direct induction of chondrogenic cells from human dermal fibroblast culture by defined factors. PLoS One. 2013;8:e77365.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 ISAKOS
About this chapter
Cite this chapter
Im, GI. (2022). Pluripotent Stem Cells: Embryonic/Fetal Stem Cells and Induced Pluripotent Stem Cells. In: Filardo, G., Mandelbaum, B.R., Muschler, G.F., Rodeo, S.A., Nakamura, N. (eds) Orthobiologics. Springer, Cham. https://doi.org/10.1007/978-3-030-84744-9_30
Download citation
DOI: https://doi.org/10.1007/978-3-030-84744-9_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-84743-2
Online ISBN: 978-3-030-84744-9
eBook Packages: MedicineMedicine (R0)