Abstract
Neuroendocrine tumors of the thymus (TNETs) are rare and can be associated with multiple neuroendocrine neoplasia type 1 syndrome. TNETs are traditionally classified using the World Health Organization criteria into low-grade typical carcinoids, intermediate-grade atypical carcinoids, and two high-grade malignancies: large cell neuroendocrine carcinoma and small cell carcinoma. One-third of patients with TNET are asymptomatic. TNETs are associated with poor survival and high risk of recurrence. Complete and radical resection of TNET is recommended.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Neuroendocrine tumors
- Thymic neuroendocrine tumor
- Thymus
- Thymectomy
- Minimally invasive thymectomy
- Multiple endocrine neoplasia type 1
Case Presentation
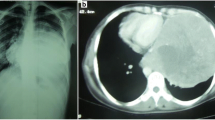
A 25-year-old man with a history of asthma and Poland syndrome underwent chest CT in 2016 owing to chest pain, dyspnea on exertion, and headache. An anterior mediastinal mass measuring 15 cm was discovered, associated with incomplete obstruction of the superior vena cava (◘ Fig. 25.1). A transthoracic needle biopsy of the mass was performed. The cytological description of the mass was consistent with the presence of trabecular growth pattern and rosette formation. Immunohistochemical staining was positive for synaptophysin, chromogranin A, CD56, and NSE, with a Ki-67 index of 5%, consistent with the diagnosis of atypical carcinoid tumor of the thymus. A 6-fluoro-(18F)-L-3,4-dihydroxyphenylalanine (18F-DOPA) positron emission tomography (PET)/CT showed no extrathymic metastases. Complete thymectomy was then performed by hemiclamshell thoracotomy with resection of the right phrenic nerve. A large, well-circumscribed tumor was found without any invasion into the adjacent structure. Final pathology revealed an atypical carcinoid tumor with Ki-67 index between 10% and 20%. This tumor was classified as stage IIB based on TNM classification (7th edition) and Masaoka classification, due to infiltration of the perithymic fat, and pT2R0. Surgical treatment was complemented by adjuvant radiotherapy (50 Gy). However, there was a recurrence 3 years later with cervical and mediastinal lymph node metastases, which was confirmed with needle biopsy vand Ga-68-labeled dodecanetetraacetic acid-tyrosine-3-octreotate (DOTATATE) PET/CT. Complete left lateral neck dissection (by cervicotomy) with left mediastinal lymph node dissection (by VATS) was then performed. Thirteen of 41 lymph nodes were positive for metastatic disease. Immunohistochemistry showed absence of SSTR2 and PDL1 expression. Whole-genome sequencing showed the presence of MEN1 mutation. Ten months later, the patient presented with new lymph node, as well as lung, and bone metastases (◘ Fig. 25.2). Systemic treatment with lutetium (177Lu) oxodotreotide was initiated which stabilized the patient’s condition.
Questions
-
1.
What are the epidemiological characteristics of TNET?
-
1.
TNET is a rare tumor in patients with the MEN1 syndrome but is a common tumor of the thymus.
-
2.
TNET is predominant in males and in patients with smoking history.
-
3.
Phenotype-genotype correlation in patients with MEN1 mutations is low.
-
4.
Twenty-five percent of thymic carcinoids are associated with the MEN1 syndrome.
-
(a)
Only 1) and 4) are correct.
-
(b)
Only 1) and 2) are correct.
-
(c)
Only 2), 3), and 4) are correct.
-
(d)
Only 2) is correct.
-
(e)
All are correct.
-
(a)
-
1.
-
2.
Which imaging test(s) or serum marker(s) is/are used when thymic NET is suspected?
-
1.
Serum chromogranin A
-
2.
Chest MRI
-
3.
Presence of MEN1 mutations
-
4.
Ga-18 DOTATATE PET/CT
-
(a)
Only 1) is correct.
-
(b)
Only 2) and 4) are correct.
-
(c)
Only 3) is correct.
-
(d)
Only 4) is correct.
-
(e)
All are incorrect.
-
(a)
-
1.
-
3.
Which of the following clinical presentation(s) is/are most commonly seen in patients with thymic NET?
-
1.
Skin flushing
-
2.
Chest pain
-
3.
Diarrhea
-
4.
Moon face
-
5.
Absence of symptoms
-
(a)
Only 1), 2), and 3) are correct.
-
(b)
Only 2) and 5) are correct.
-
(c)
Only 2) is correct.
-
(d)
Only 5) is correct.
-
(e)
All are correct.
-
(a)
-
1.
-
4.
Which of the following factors negatively influence the survival of patients with thymic NET?
-
1.
The histological grade
-
2.
Incomplete radical surgical resection
-
3.
Thymectomy by video-assisted thoracic surgery
-
4.
Thymectomy by sternotomy
-
(a)
Only 1) is correct.
-
(b)
Only 4) is correct.
-
(c)
Only 1), 2), and 3) are correct.
-
(d)
Only 1) and 2) are correct.
-
(e)
All are correct.
-
(a)
-
1.
-
5.
Which statement(s) regarding the management of thymic NET is/are correct?
-
1.
Active surveillance with MRI every 3 months is recommended for early-stage tumors.
-
2.
Multidisciplinary management of thymic tumors is recommended.
-
3.
Centers with expertise in thoracic and cardiovascular surgery are recommended for management of patients with thymic NET.
-
4.
Complete and radical resection of the tumor is recommended if the tumor is resectable.
-
(a)
Only 1) is correct.
-
(b)
Only 2) is correct.
-
(c)
Only 2) and 4) are correct.
-
(d)
Only 2), 3), and 4) are correct.
-
(e)
All are correct.
-
(a)
-
1.
-
6.
Which statement(s) regarding thymic surgery is/are correct?
-
1.
A transcervical approach should always be performed in patients with thymic NET associated with the MEN1 syndrome.
-
2.
Thymectomy including perithymic fat is the standard of care surgical approach for thymic tumors.
-
3.
Surgery by minimally invasive approach can always be performed.
-
4.
Thymectomy by sternotomy is an obsolete procedure.
-
(a)
Only 2) is correct.
-
(b)
Only 1) and 2) are correct.
-
(c)
Only 3) and 4) are correct.
-
(d)
All are correct.
-
(a)
-
1.
-
7.
The benefits of minimally invasive surgery as compared to open procedures are as follows:
-
1.
Reduced operative time
-
2.
Reduced intraoperative blood loss
-
3.
Shorter hospital stay
-
4.
Lower rate of cancer recurrence at 5 years
-
5.
Lower rate of postoperative pneumonia
-
(a)
Only 4) is correct.
-
(b)
Only 1) and 3) are correct.
-
(c)
Only 2), 3), and 5) are correct.
-
(d)
Only 2) and 5) are correct.
-
(e)
All are correct.
-
(a)
-
1.
-
8.
Radiotherapy is currently used as follows:
-
1.
In association with chemotherapy
-
2.
As adjuvant treatment for patients with positive margins
-
3.
As palliative treatment in case of vena cava syndrome
-
4.
In all cases with MEN1 syndrome
-
(a)
Only 1) is correct.
-
(b)
Only 2) is correct.
-
(c)
Only 2) and 3) are correct.
-
(d)
Only 4) is correct.
-
(e)
All are correct.
-
(a)
-
1.
-
9.
Which statement(s) regarding the prognosis of thymic NET is/are correct?
-
1.
The Masaoka staging system is specific to predict the prognosis.
-
2.
Reported 10-year survival rate for atypical carcinoid thymic tumors is 30%.
-
3.
Patients with TNET secondary to the MEN1 syndrome have better prognosis with a 10-year survival rate of 90% as compared to sporadic cases.
-
4.
Recurrence is frequent.
-
(a)
Only 1) and 4) are correct.
-
(b)
Only 1) is correct.
-
(c)
Only 2) and 4) are correct.
-
(d)
Only 3) is correct.
-
(e)
All are correct.
-
(a)
-
1.
-
10.
A 20-year-old patient presented with the MEN1 syndrome and primary hyperparathyroidism. Chest CT did not reveal any thymic masses. Which statement(s) is/are correct?
-
1.
Performing a prophylactic transcervical thymectomy during a parathyroidectomy surgery for primary hyperparathyroidism is sufficient to prevent TNET.
-
2.
A prophylactic transcervical thymectomy can be performed during a parathyroid surgery for primary hyperparathyroidism with routine pathological evaluation of the thymus for thymic pathology.
-
3.
A minimally invasive complete thymectomy could be performed during surgery for primary hyperparathyroidism to avoid the risk of TNET.
-
4.
Transcervical thymectomy is currently not necessary during surgery for primary hyperparathyroidism.
-
(a)
Only 1) is correct.
-
(b)
Only 2) is correct.
-
(c)
Only 3) is correct.
-
(d)
Only 4) is correct.
-
(e)
Only 2) and 3) are correct.
-
(a)
-
1.
1 Introduction
Neuroendocrine tumors of the thymus (TNETs) are rare. They account for approximately 5% of all tumors of the mediastinum and 0.4% of all neuroendocrine tumors [1,2,3]. The reported incidence of TNET is 0.02/100,000 population per year and shows male predominance (male-to-female ratio of 3:1) [2]. Although most TNETs are sporadic, some are associated with multiple neuroendocrine neoplasia type 1 syndrome (TNETs-MEN1), thymoma, or thymic carcinoma [1, 4, 5]. In a prospective study of 85 patients, Gibril et al. showed that 8% of patients with the MEN1 syndrome developed TNET [6]. In the American/European series, TNET-MEN1 occurs predominantly in male patients (10:1) [7]. However, the genotype-phenotype correlations in patients with the MEN1 syndrome are reported to be lower in TNET than in pulmonary neuroendocrine tumors (PNET) [8,9,10,11]. TNET in patients with the MEN1 syndrome is associated with a higher risk of death (hazard ratio [HR] = 4.64, 95% CI = 1.73–12.41) than in patients without the MEN1 syndrome [12].
Thoracic NETs (pulmonary and thymic) are often referred to as foregut NETs. TNET and PNET are traditionally classified using the same World Health Organization (WHO) criteria into low-grade typical carcinoids (TC), intermediate-grade atypical carcinoids (ACs), and two high-grade malignancies: large cell neuroendocrine carcinoma (LCNEC) and small cell carcinoma (SCC). However, TNET and PNET have clinicopathological and genetic differences. For example, AC and LCNEC are the most frequent subtypes in the thymus, whereas TC and SCC are prevalent in the lung. The WHO classification is based on morphology. However, other classifications have been proposed based on mitotic count and Ki-67 index [13] or a morphomolecular grading system using a copy number instability (CNI) score [14].
2 Clinical Presentation
One-third of patients with TNET are asymptomatic, and tumors are discovered incidentally. Local symptoms, such as chest pain, cough, and respiratory distress, occur in about half of patients. Superior vena cava syndrome and hoarseness can occur depending on the extent of the tumor. Liver, bone, and lung metastases are often found. TNET can be accompanied by paraneoplastic syndromes, such as Cushing’s syndrome, hypertrophic osteoarthropathy, or ectopic acromegaly. Carcinoid syndrome is rare [15].
Due to the higher risk of death associated with TNET, screening for thymic tumors is required every 1–3 years in patients with the MEN1 syndrome using thoracic (low-dose) computed tomography (CT) or magnetic resonance imaging (MRI) [16]. Since patients with foregut NET often lack aromatic amino acid decarboxylase, which is necessary to convert tryptophan to serotonin, urinary serotonin or 5-HIAA measurement is not routinely recommended for screening and/or diagnosis of TNET.
3 Prognosis
According to the WHO classification of TNET, the reported 5-year survival rate, 10-year survival rate, and median survival time were 100%, 60%, and 126 months, respectively, for TC, and 50%, 30%, and 52 months, respectively, for AC. The reported 5-year survival rate and median survival time was 30% and 21 months, respectively, for LCNEC, and 0% and 13.5 months, respectively, for SCC [11]. According to the Groupe d’Etude des Tumeurs Endocrines (GTE) network, the median survival time of patients with TNET-MEN1 is 9 years and 7 months, and the 10-year survival rate is 36% [12].
There is no established method for staging TNET. The most common method includes the Masaoka system, which was initially established for thymoma. However, neither the Masaoka staging nor the proposed TNM classification suggested by the International Association for the Study of Lung Cancer (IASLC)/International Thymic Malignancy Interest Group (ITMIG) seems relevant for prognosis of TNET [17, 18]. In contrast, histological grade, high proliferative rate (Ki-67 index >10%), incomplete radical surgical resection, and absence of surgical resection seem to be negative prognostic factors [2, 18, 19].
4 Treatment of TNET
TNET should be referred to an experienced medical team. Multidisciplinary management of thymic tumors is recommended. According to the European Society for Medical Oncology and North American Neuroendocrine Tumor Society guidelines, complete and radical resection is recommended, if the tumor is resectable [19, 20].
5 Surgical Details
Centers with expertise in thoracic and cardiovascular surgery are recommended to manage patients with TNET. The completeness of resection (R0) is the most important prognostic factor. Therefore, complete resection of the thymus (thymectomy) is the standard of care for thymic tumors. To evaluate the resectability of the tumor, thoracic MRI might be necessary. However, judgment during surgery is critical for determining invasion of adjacent structures and resectability. The aim of thymectomy is to remove the entire thymus without opening the tumor capsule and the perithymic fat (including cervical, mediastinal, and cardiophrenic fat) between the two phrenic nerves. Anterior lymph node dissection (N1) is also mandatory in thymic cancer [21]. Sometimes, resection of the mediastinal pleura, pericardium, adjacent lung, innominate vein, or phrenic nerve is required to achieve resection with negative margins.
To complete the resection of the thymus (R0), open mediastinal sternotomy and minimally invasive thymectomy (MIT) are usually performed. These different approaches can vary depending on the extent of the tumor, its size, and the experience of the surgeon.
Median sternotomy is the standard for thymomectomy/thymectomy and remains the preferred approach in cases of pleuropulmonary invasion of TNET. It provides excellent exposure to the neck, anterior mediastinum, and thymus. MIT is an increasingly used alternative to the traditional open approach for thymic tumors, especially for small and well-encapsulated tumors, with a similar 10-year recurrence-free survival [22]. In contrast to sternotomy, MIT demonstrates reduced intraoperative blood loss and shorter hospital stays [22, 23]. However, an appropriately designed prospective trial would be required to assess whether MIT is as safe as sternotomy. There is a wide range of MIT procedures used: robot-assisted thoracic surgery (RATS); video-assisted thoracic surgery (VATS) with a left, right, or bilateral approach; subxiphoid single-port VATS; video-assisted transcervical thymectomy; or a hybridization of these procedures [23,24,25,26]. None of these procedures showed any real benefit over the other.
6 Prophylactic Transcervical Thymectomy
Given the frequency of supernumerary parathyroid glands in the thymus, there is a general agreement to perform transcervical thymectomy at the time of surgery for primary hyperparathyroidism in patients with the MEN1 syndrome [27]. This procedure is advocated for resection of ectopic parathyroid glands, for reduction of the rate of persistent and recurrent hyperparathyroidism, and as prophylaxis against development of TNET. However, transcervical thymectomy only partially removes the thymus, mostly the superior thymic horns, leaving behind a significant part of the thymus. Although partial thymectomy is useful in the treatment of hyperparathyroidism, its efficacy in finding or preventing TNET and its impact on patient survival have not been demonstrated [28, 29]. Furthermore, the development of thymic carcinoids has been documented after prophylactic transcervical thymectomy [30]. Due to poor survival associated with TNET and the high risk of recurrence, complete thymectomy (preferentially minimally invasive) in addition to parathyroidectomy for treatment of primary hyperparathyroidism is currently debated. Long-term screening with thoracic imaging is therefore required in patients with the MEN1 syndrome after transcervical thymectomy.
7 Medical Treatment and Radiotherapy
Adjuvant radiotherapy is currently used in the treatment of incomplete resection, resection with positive margins, and unresectable cases. Systemic treatments include cytotoxic chemotherapy, somatostatin analogs, and everolimus. Systemic treatment may be administered as curative therapy for advanced TNET, as induction therapy to reduce the tumor burden before surgery, as postoperative therapy to reduce the risk of recurrence, and as palliative therapy for unresectable, metastatic, and recurrent TNET. The management of patients with TNET requires multidisciplinary expertise at every step of disease progression.
Answers
1. (c); 2. (e); 3. (b); 4. (d); 5. (d); 6. (a); 7. (c); 8. (c); 9. (c); 10. (e)
References
Strobel P, Marx A, Chan JK, et al. Thymic neuroendocrine tumors. In: Travis WD, Brambilla E, Burke AP, et al., editors. WHO classification of tumors of the lung, pleura, thymus, and heart. Lyon: IARC Press; 2015. p. 234–41.
Gaur P, Leary C, Yao JC. Thymic neuroendocrine tumors: an SEER database analysis of 160 patients. Ann Surg. 2010;251:1117–21.
Filosso PL, Yao X, Ahmad U, et al. Outcome of primary neuroendocrine tumors of the thymus: a joint analysis of the International Thymic Malignancy Interest Group and the European Society of Thoracic Surgeons databases. J Thorac Cardiovasc Surg. 2015;149:103 e2–109 e2.
Rosai J, Higa E, Davie J. Mediastinal endocrine neoplasm in patients with multiple endocrine adenomatosis: a previously unrecognized association. Cancer. 1972;29:1075–83.
Teh BT, Zedenius J, Kytölä S, et al. Thymic carcinoids in multiple endocrine neoplasia type 1. Ann Surg. 1998;228:99–105.
Gibril F, Chen YJ, Schrump DS, Vortmeyer A, Zhuang Z, Lubensky IA, Reynolds JC, Louie A, Entsuah LK, Huang K, Asgharian B, Jensen RT. Prospective study of thymic carcinoids in patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 2003;88:1066–81.
Ye L, Wang W, Ospina NS, et al. Clinical features and prognosis of thymic neuroendocrine tumors associated with multiple endocrine neoplasia type 1: a single-center study, systematic review, and meta-analysis. Clin Endocrinol. 2017;87:706–16.
Teh BT, Hayward NK, Walters MK, et al. Genetic studies of thymic carcinoids in multiple endocrine neoplasia type 1. J Med Genet. 1994;31:261–2.
Zhao J, de Krijger RR, Meier D, et al. Genomic alterations in well-differentiated gastrointestinal and bronchial neuroendocrine tumors (carcinoids): marked differences indicate diversity in molecular pathogenesis. Am J Pathol. 2000;157:1431–8.
Petzmann S, Ullmann R, Klemen H, et al. Loss of heterozygosity on chromosome arm 11q in lung carcinoids. Hum Pathol. 2001;32:333–8.
Strobel P, Zettl A, Shilo K, et al. Tumor genetics and survival of thymic neuroendocrine neoplasms: a multi-institutional clinicopathologic study. Genes Chromosomes Cancer. 2014;53:738–49.
Goudet P, Murat A, Binquet C, Cardot-Bauters C, Costa A, Ruszniewski P, et al. Risk factors and causes of death in MEN1 disease A GTE (Groupe d'Etude des Tumeurs Endocrine) cohort study among 758 patients. World J Surg. 2010;34:249–55.
Pelosi G, Pattini L, Morana G, et al. Grading lung neuroendocrine tumors: controversies in search of a solution. Histol Histopathol. 2017;32:223–41.
Dinter H, Bohnenberger H, Beck J, et al. Molecular classification of neuroendocrine tumors of the thymus. J Thorac Oncol. 2019;8:1472–83.
Soga J, Yakuwa Y, Osaka M. Evaluation of 342 cases of mediastinal/thymic carcinoids collected from literature: a comparative study between typical carcinoids and atypical varieties. Ann Thorac Cardiovasc Surg. 1999;5:285–92.
Thakker RV, Newey PJ, Walls GV, et al. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metab. 2012;97:2990–3011.
Zhao Y, Shi J, Fan L, et al. Evaluation of the proposed International Association for the Study of Lung Cancer (IASLC)/International Thymic Malignancies Interest Group (ITMIG) staging revisions in thymic well-differentiated neuroendocrine carcinoma patients. Eur J Cardiothorac Surg. 2016;49:569–73.
Crona J, Björklund P, Welin S, Kozlovacki G, Oberg K, Granberg D. Treatment, prognostic markers and survival in thymic neuroendocrine tumors. a study from a single tertiary referral center. Lung Cancer. 2013;79:289–93.
Oberg K, Jelic S, ESMO Guidelines Working Group. Neuroendocrine bronchial and thymic tumors: ESMO clinical recommendation for diagnosis, treatment, and follow-up. Ann Oncol. 2009;20:147–9.
Phan AT, Oberg K, Choi J, et al. NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the thorax (includes lung and thymus). Pancreas. 2010;39:784–98.
Bhora FY, Chen DJ, Detterbeck FC, et al. The ITMIG/IASLC Thymic epithelial tumors staging project: a proposed lymph node map for thymic epithelial tumors in the forthcoming 8th edition of the TNM classification of malignant tumors. J Thorac Oncol. 2014;9:S88.
Xie A, Tjahjono R, Phan K, Yan TD. Video-assisted thoracoscopic surgery versus open thymectomy for thymoma: a systematic review. Ann Cardiothorac Surg. 2015;4:495–508.
O'Sullivan KE, Kreaden US, Hebert AE, Eaton D, Redmond KC. A systematic review of robotic versus open and video assisted thoracoscopic surgery (VATS) approaches for thymectomy. Ann Cardiothorac Surg. 2019;8:174–93.
Lemaître PH, Keshavjee S. Uniportal video-assisted transcervical thymectomy. Thorac Surg Clin. 2019;29:187–94.
Zieliński M, Rybak M, Wilkojc M, Fryzlewicz E, Nabialek T, Pankowski J. Subxiphoid video-assisted thoracoscopic thymectomy for thymoma. Ann Cardiothorac Surg. 2015;4:564–6.
Suda T. Robotic subxiphoid thymectomy. J Vis Surg. 2016;22:118.
Montenegro FLM, Neves MC, Lourenço DM Jr, Arap SS, Nascimento CP Jr, Toledo SPA, et al. Thymectomy in the surgical approach to hyperparathyroidism in type 1 multiple endocrine neoplasia. Rev Bras Cir Cab Pesc. 2010;39:174–8.
Powell AC, Alexander HR, Pingpank JF, et al. The utility of routine transcervical thymectomy for multiple endocrine neoplasia 1-related hyperparathyroidism. Surgery. 2008;144:878–83.
Welch K, McHenry CR. The role of transcervical thymectomy in patients with hyperparathyroidism. Am J Surg. 2012;203:292–5. discussion 295–296
Burgess JR, Giles N, Shepherd JJ. Malignant thymic carcinoid is not prevented by transcervical thymectomy in multiple endocrine neoplasia type 1. Clin Endocrinol. 2001;55:689–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bédat, B., Triponez, F. (2021). Neuroendocrine Tumors of the Thymus. In: Shifrin, A.L., Raffaelli, M., Randolph, G.W., Gimm, O. (eds) Endocrine Surgery Comprehensive Board Exam Guide. Springer, Cham. https://doi.org/10.1007/978-3-030-84737-1_25
Download citation
DOI: https://doi.org/10.1007/978-3-030-84737-1_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-84736-4
Online ISBN: 978-3-030-84737-1
eBook Packages: MedicineMedicine (R0)