Abstract
This chapter examines evidence-based prevention of behavioral disorders related to marijuana use, focusing on the psychoactive compound tetrahydrocannabinol. This chapter summarizes diagnostic criteria for harmful patterns of marijuana use and definitions for identifying problems with use. Based on evidence for increasing subsequent harm and marijuana use disorders, the chapter examines prevention opportunities to reduce early age use and frequent adult use. The international trend for increasing prevalence of use is examined, together with the major driver of this trend – marijuana legalization. Evidence-based prevention programs and policies are reviewed at the universal and targeted levels. The potential for stepped care prevention models is outlined, together with lessons learned to date for implementation of prevention approaches. An important lesson emerging from the studies summarized in this chapter is that available evidence from the nations and states that have legalized marijuana use for medicinal or recreational use shows a clear and causal contribution to harm. This chapter emphasizes the importance of countering the popular misconception that marijuana legalization may reduce harms related to marijuana use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cannabis
- Cannabis disorder
- Drug use
- Epidemiology
- Marijuana harms
- Marijuana consequences
- Prevention
- Substance abuse
- Substance disorder
- Treatment
11.1 Definition/Diagnostic Criteria
Marijuana refers to the psychoactive compound tetrahydrocannabinol [THC] derived from the cannabis plant. In what follows, we focus on THC but also provide some information on other compounds derived from the cannabis plant or through chemical synthesis, collectively known as cannabinoids.
The legal status of marijuana is rapidly changing. At the international level, it has been an illicit drug for half a century with most countries signatories to the United Nations convention that defines illicit drugs. Because it has been the most widely used illicit drug, with relatively low acute harms, and because some cannabinoids appear to have therapeutic benefits, a popular movement has been successful in legalizing marijuana use in a growing number of states and nations (Hall et al., 2019).
This section describes the consequences and harms associated with different patterns of marijuana use behaviors, to provide a basis for establishing diagnostic criteria to guide prevention. Although we focus on THC, the effects of other cannabinoids are also briefly discussed.
There is variation in the patterns of marijuana use that have been associated with harms. Psychiatric guidelines recognize marijuana (cannabis) use disorder as a diagnostic category (Compton et al., 2019). This is assessed using indicators such as frequency, tolerance, and time spent using or getting over effects. In what follows, we note there is increasing evidence that frequent use (monthly or more frequent use) of marijuana may increase the risk of disorders, be harmful to mental health, and have long-term adverse intergenerational effects on the offspring of users.
Longitudinal studies have identified early age marijuana use as a predictor of progression to frequent and daily adolescent use (e.g., Scholes-Balog et al., 2020). This has led to the target of preventing any use of marijuana through childhood and adolescence. In their review of available epidemiological data, Hall et al. (2019) note that adolescents who use cannabis are at greater risk than adults of developing disorders, cognitive impairment, leaving school early, progressing to other illicit drug use, and mental health problems (including schizophrenia, affective disorders, and suicidal thoughts).
A comprehensive literature review (National Academies of Sciences, Engineering, and Medicine, 2017) established that there have been relatively few studies of the longitudinal consequences of marijuana use. Longitudinal studies face the difficulty that marijuana is often used in combination with other drugs (polydrug use). For example, among young Australians, we found that approximately 8.2% reported polydrug use, including cannabis use, and that this subgroup of drug users reported higher levels of psychological distress than adolescents who typically consumed alcohol only (Kelly et al., 2015). It is often difficult in longitudinal studies to estimate the dose of marijuana being used. Chan et al. (2017) observed that very-high-potency THC products like butane hash oil have more significant associations with mental health problems and health risk behaviors, including depressed mood and polydrug use, than herbal cannabis. These issues increase the difficulty of answering questions of the consequences of marijuana use required for clinical guidelines.
In their review, Hall et al. (2019) note that epidemiological studies have tended to focus on the adverse health effects of daily marijuana use, with clear evidence of harm for this pattern of use. Silins et al. (2014) integrated data from three large longitudinal studies from Australia and New Zealand. After adjusting for other predictors, daily marijuana use before age 17 years consistently predicted a range of adult outcomes including reductions in high school completion, and adult degree attainment and increases in cannabis dependence, other illicit drug use, and suicide attempts.
There is evidence that adult frequent marijuana use (monthly or more frequent) is a risk factor for mental health problems. A large epidemiological study combined data from the US National Survey of Drug Use and Health (NSDUH) with geographically linked community surveys (Reece & Hulse, 2020a). From 2011 to 2016, state-level marijuana use in the past month (a measure of frequent use) was causally associated with higher rates of mental health problems indicated by any mental illness, major depressive illness, serious mental illness, and suicidal thinking. In explaining their effects, these authors note laboratory studies that show that cannabinoid exposure leads to adverse psychiatric outcomes by adversely impacting neural stem cell activity, which reduces neuroplasticity, resulting in premature brain aging. These authors note that these destructive neuro-cellular mechanisms not only apply to THC but also to other cannabinoids including cannabidiol and cannabichromene.
There is evidence that frequent adult marijuana use is harmful to the next generation. The offspring of frequent adult marijuana users have higher rates of congenital abnormalities (Reece & Hulse, 2020b) and adverse mental health problems including autism and ADHD symptoms (Reece & Hulse, 2020a). Geographic differences in rates of frequent adult marijuana use in Canada have been associated with higher rates of congenital abnormalities including cardiovascular defects, Down’s syndrome, and gastroschisis (a birth defect of the belly wall) (Reece & Hulse, 2020b). Reece and Hulse also describe how neurobiological effects of THC and other cannabinoids explain these intergenerational harms.
11.2 Prevalence and Age of Onset
In what follows, we summarize what is known of patterns of marijuana use in different age groups and countries. In their review, Hall et al. (2019) summarize international patterns of marijuana use, noting that in 2015 around 4% of the global adult population used marijuana. Use was more common in North America and high-income countries in Europe and Oceania than in low- and middle-income countries. In the intervening years, cannabis use increased in low- and middle-income countries but remained low in Asia.
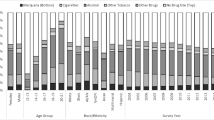
In high-income countries, population rates of marijuana use have until recent decades tended to peak in the late 20s and then declined slowly from age 30 (Compton et al., 2007). However, since 2008, cannabis use in the USA has tended to extend longer into the 30s (Hall et al., 2019). Hall et al. (2019) note that the THC content of the marijuana that is used has increased in past decades in the USA and Europe, from around 5% to more than 15%. Compton et al. (2019) analyzed data from US National Surveys on Drug Use and Health (NSDUH) collected from 2002 to 2017, noting that marijuana use increased from 10.4% to 15.3%, while daily/near daily use increased from 1.9% to 4.2%. Despite these rises, the past year prevalence of marijuana use disorders remained stable at around 1.5%.
Presently, marijuana remains by far the most used illicit drug among adolescents and young people (Kelly et al., 2018). The Monitoring the Future (MTF) survey provides annual epidemiological trend estimates of the prevalence of marijuana use among young people (early age use) in the USA (Miech et al., 2020). Surveys of the last year of secondary school (grade 12 students) reveal that lifetime use peaked in 1979 when 60.4% reported use. Since that time lifetime use declined until 1992 to 32.6% and then increased to 49.6% in 1997. In 2019, 43.7% of US grade 12 students reported lifetime use.
In Europe, similar surveys to the MTF have been n implemented. In Central Europe, past year prevalence of marijuana use among young adults (up to 34 years of age) varies from 10% in Belgium to 22% in France (EMCDDA, 2016). In Australia, around 12% of 14–17-year-olds have used cannabis in the previous year (Weier et al., 2016).
11.3 Risk Factors
In efforts to prevent harmful patterns of marijuana use, risk factors are identified based on evidence that they act as independent predictors of behavior targets in longitudinal and epidemiological research studies. Although protective factors are often defined as the reverse of risk factors, they are more clearly differentiated as characteristics that buffer, mediate, or moderate the influence of risk factors, thereby reducing the likelihood of later problems such as frequent marijuana use (Catalano et al., 1996; Toumbourou & Catalano, 2005). Resilience researchers have identified several protective factors by studying children who have avoided adversity after being exposed to difficult childhood experiences such as parental mental illness or extreme poverty (Catalano et al., 1996).
Longitudinal studies typically show a developmental behavioral sequence whereby marijuana use begins with a first experience and then progresses to more frequent use, which in turn increases the risk of marijuana use disorders (Toumbourou & Catalano, 2005). This developmental behavioral sequence has a neurobiological substrate and social relationship overlay. Neuroadaptation begins from the first exposure to marijuana use observable from higher doses being required over time to experience similar levels of intoxication. Laboratory studies show that neuroadaptation caused by both marijuana and other cannabinoid use is associated with destructive neuro-cellular changes that weaken neurological stem cell activity and therefore reduce brain plasticity (Reece & Hulse, 2020a, b). These changes in part explain the behavioral progression from marijuana use to disorder symptoms such as narrowing of life interests and aspirations. These behavioral and neurological changes also associate with social relationship overlays whereby peer, intimate, family, and community relationships are attenuated to accommodate changes such as increasing time spent in marijuana use.
Neonates are extremely vulnerable to destructive neurobiological changes following in utero exposure to maternal use of marijuana and other cannabinoids. Laboratory studies show the destructive neuro-cellular changes that arise through both marijuana and other cannabinoid use are transmitted to offspring (Reece & Hulse, 2020a, b).
Risk factors for harmful patterns of marijuana use tend to show variation across communities and are often contrasted with structural and societal determinants such as marijuana policies and laws that affect large population aggregations but show differences across states and nations (Toumbourou et al., 2014). Reviews of longitudinal and program evaluation studies identify risk factors for early age marijuana use across a range of child and adolescent development settings.
The review paper by Hawkins et al. (1992) was influential in organizing what was known to that point of developmental risk and protective factors for youth drug use, including marijuana use. Subsequent reviews have confirmed their conclusion that predictors are evident at the individual level and within the family, school, peer, and community ecological settings (Toumbourou & Catalano, 2005).
At the societal and community level, socioeconomic disadvantage is a characteristic that is consistently associated with developmental problems for neonates, children, and adolescents. In addition to socioeconomic disadvantage, several sets of community risk factors influence early age marijuana exposure (e.g., Catalano et al., 1996; Toumbourou et al., 2014) including normative expectations and acceptance of marijuana use and availability.
The International Youth Development Study (IYDS) is a cross-nationally matched longitudinal study that uses the Communities That Care Youth Survey to monitor risk factors and youth health behaviors (Rowland et al., 2019a). Longitudinal analyses of cross-nationally matched analyses of the IYDS data showed a wide range of adolescent (age 12) family, peer-group, school, and community risk factors were predictive of marijuana use (past month) 1 year later, in both US and Australian adolescents (Hemphill et al., 2011). At the family level, unique multivariate predictors included less positive family management practices (e.g., permissive parenting styles, lower relationship quality), higher levels of family conflict, a family history of substance use, and parental attitudes more favorable toward both drug use and antisocial behavior. Higher levels of attachment to both the mother and father, as well as greater opportunities and rewards for prosocial involvement within the family environment, showed protective effects.
Hemphill et al. (2011) found that similar risk and protective factors predicted both marijuana and other forms of substance use. These findings parallel research findings on the association of family and parenting factors with other types of substance use, including early use of tobacco and alcohol. For example, low emotional closeness to parents predicts tobacco use cross-sectionally and longitudinally (Kelly et al., 2011; Kelly, 2012) and alcohol use cross-sectionally and longitudinally (Kelly et al., 2011, 2012). Poor parental supervision is more associated with adolescents who show early and steep rises in alcohol use compared to those who show limited and stable growth trajectories that more strongly predicts early and strong escalation in alcohol use relative to use (Chan et al., 2013). These findings suggest that efforts to reduce social environmental risk factors for early age marijuana use are likely to also reduce other substance use problems.
A consistent observation in prevention science is that risk factors have a cumulative impact. The more risk factors that are present and the longer they persist over time, the greater the subsequent developmental impact (e.g., Toumbourou et al., 2014). There is no single risk factor that fully explains developmental problems; rather, these problems can be regarded as having complex causes involving influences and interaction of multiple risk and protective factors. For example, low emotional closeness to parents and poor supervision may serve to increase the likelihood of engagement with drug-using peer networks during the pubertal stage of development, and major school transitions may heighten this risk (Kelly et al., 2012; Li et al., 2014).
One heuristic proposed to describe the cumulative effect of risk factors is to use the analogy of a snowball (Toumbourou & Catalano, 2005). According to this view, risk factors that emerge early in life (e.g., maternal marijuana use) can lead to subsequent risk factors that tend to “adhere” and accumulate as a consequence of the experience of earlier problems (e.g., child disability, child-onset behavior problems, school failure).
Social and economic mobility patterns in competitive market economies have increased socioeconomic differentials and led to a situation whereby children experiencing snowball risk trajectories tend to be disproportionately clustered within disadvantaged geographic communities and schools (Reece & Hulse, 2020a; Toumbourou et al., 2014). Using this analogy, the solution is to invest within these targeted areas to prevent the potential for an avalanching snowball by building protective solutions and reducing early life risk factors. For example, by increasing illicit drug laws and their enforcement, it may be possible to reduce the availability and normative acceptance of marijuana and to in this way encourage adults to reduce regular marijuana use before they conceive, in this way preventing the sequence of events that can result in the cumulative escalation of risk for future generation.
In many cases, the cumulative effect of risk is more temporal and can be better described with the analogy of a snowstorm (Toumbourou & Catalano, 2005; Toumbourou et al., 2014). According to this view, a healthy child without protective clothing can be put at risk by temporal events such as exposure to extreme weather. If such unprotected exposure continues for long enough, adverse health outcomes can result. Where the adolescent has low protective factors (such as parents being unavailable to supervise activities or poor relationships with teachers) in a community with high rates of marijuana use and availability, the likelihood of the adolescent using marijuana increases. The protective advantages of positive relationships with adults suggest there is potential to protect health within risky social environments by increasing healthy adult relationships or other protective factors (analogous to providing warm clothing and shelter in stormy weather). From this perspective, solutions lie in improving social environments (by increasing protective social relationships) through the course of development (Catalano et al., 1996; Toumbourou et al., 2014).
The cumulative effect of risk across social environments for the initiation of different patterns of adolescent marijuana use has been demonstrated in an Australian longitudinal study (Scholes-Balog et al., 2020). Scholes-Balog et al. (2020) reported the cumulative effect of risk across family, peer, and community factors, accounting for early (childhood) substance use (cigarette, alcohol and illicit drug use, and drinking until drunk), predicted early adolescent-onset marijuana use. The cumulative effect of risk within the family and early adolescent substance use also predicted late adolescent-onset occasional marijuana use (relative to non-marijuana users).
Given the range of risk and protective factors, the social development model (SDM) has been proposed to organize knowledge of how risk and protective factors work together to predict marijuana use and related problems. The SDM is an explicit developmental theory of health behavior that has been well supported in empirical tests during childhood, adolescence, and young adulthood. The SDM proposes that social relationships are critical proximal influences that affect health behaviors, including marijuana use. Social relationships can conversely encourage either healthy (prosocial) or unhealthy behavior, depending on the norms and standards of the relationship influence. The development of social relationship bonds are in turn affected by more distal factors related to interaction opportunities; social, emotional, and cognitive skills; and the rewards experienced from social interactions. The SDM provides a basis for coherently evaluating health behavior influences in a range of child, adolescent, and adult social contexts.
The SDM theorizes that liberalizing marijuana laws changes key risk factors including social acceptability, perceived prevalence, risk, and availability (Kosterman et al., 2016). Fischer et al. (2020) summarize what is known of patterns of use and harms following state and national legalization of marijuana use. They observe that legalization has reduced the perceived risk and increased the normative acceptance of marijuana use among young people and adults. Legalization has been associated with a reduced price of marijuana, increased availability, and higher potency products.
Available studies show increases in use Marijuana: risk factors among adults following legalization, in line with SDM predictions. For example, a large epidemiological study combining data across geographic areas in the USA from 2011 to 2016 found state legalization changes caused increases in frequent use. These increases have in turn caused increases in mental health problems across large state populations (Reece & Hulse, 2020a).
11.4 Review of Evidence-Based Prevention
Evidence-based prevention can be defined based on programs or policies that result in reduced early age use, frequent use, or marijuana use disorders. To identify preventative interventions, we searched for literature reviews of program evaluation studies that had rigorous randomized trial and quasi-experimental or epidemiological designs. As outlined in the SDM, prevention effects operate within a social ecological setting context and may be disrupted in locations where the legalization of marijuana use results in community norms that are accepting of marijuana use for medical or recreational use.
11.5 Effective Screening
In community settings, screening includes epidemiological surveillance using instruments such as the Communities That Care Youth Survey to monitor population patterns of marijuana use and risk and protective factors, which can be targeted in prevention (Rowland et al., 2019b). Rowland et al. (2019b) reported similar risk and protective factors predicted community rates of adolescent marijuana use in both Australia and the Netherlands. These findings tend to confirm the validity and utility of the Communities That Care Youth Survey as a community surveillance instrument for monitoring population patterns of marijuana use and risk and protective factors (Hemphill et al., 2011). In Australia, the Communities That Care Youth Survey has been used successfully to guide community coalitions to reduce community rates of adolescent marijuana use and other substance use (Toumbourou et al., 2019).
Evidence from systematic literature reviews suggests that screening assessments for youth marijuana use in settings such as secondary schools (Carney et al., 2016), tertiary education institutions, or health services can be combined with brief interventions (typically one to five counseling sessions) to encourage reduction in use (Tanner-Smith et al., 2015). In their systematic review, Tanner-Smith et al. (2015) included 13 studies and demonstrated a small significant effect in reducing marijuana use. Brief counseling interventions included strategies such as motivational interviewing, goal setting, and relapse prevention. Similar effects have been demonstrated in one study implemented in the secondary school setting (Carney et al., 2016).
Screening and brief counseling strategies have also been incorporated in some online and telehealth interventions offered in tertiary education settings (Gulliver et al., 2015). However, there have been insufficient studies to assess the impacts on marijuana use.
Faced with rising rates of marijuana use following legalization, employers and injury prevention agencies have expressed concerns about potential increases in marijuana-related occupational injuries (Smith et al., 2018). Screening surveys in Colorado of occupations where workers have responsibility for their own safety or the safety of others (e.g., construction and extraction, farming, fishing, and forestry and healthcare support) reveal around 16% of workers report frequent marijuana use. Although biological screening (e.g., urine testing) is feasible in workplace injury prevention (Price, 2014), the legal status of marijuana use poses challenges to the mandatory application of such screening procedures.
11.6 Universal, Indicated, and Selective Prevention
Prevention refers here to strategies or programs that avert or delay the onset or escalation of marijuana use toward frequent use and use disorders that are implicated as causes of mental health and next-generation problems. Prevention responses can be classified as universal where they apply to an entire population, selective, or indicated where they target groups with elevated risk. This conceptualization of prevention addresses the progression from risk factor to behavior within populations (Toumbourou et al., 2014).
For the prevention of early age marijuana use, there is evidence that universal interventions are effective where they focus on improving child social-emotional competence and/or healthy social development environments at the school and/or community level. The effectiveness of interventions of this type concurs with evidence of social developmental risk factors in the early onset of marijuana use.
Policies and laws are an important community-level factor that influence population levels of marijuana use. There is evidence that the legalization of marijuana for medical and recreational use in US states has acted as a risk factor for harmful use. Reece and Hulse (2020a) present a causal analysis which implicates US state legalization as a direct cause of increasing rates of frequent marijuana use across US states, which in turn has caused increased population rates of mental health problems. The increase in population rates of frequent adult marijuana use is predicted to increase rates of congenital damage to the next generation (Reece & Hulse, 2020b).
In their international literature review, Fischer et al. (2020) note several harms that have increased in states and nations that have legalized cannabis use. These include increases in cannabis-related hospitalizations (e.g., emergency room visits, trauma incidents, calls to poison control centers), including cases involving children, as well as increases in treatment-seeking for cannabis use disorders. Fischer et al. (2020) also summarize evidence that marijuana-related road fatalities have increased in association with legalization. These trends align with evidence that frequent marijuana use increases the risk of road accidents (Asbridge et al., 2012).
In nations where marijuana remains illegal, there is early evidence that community-level interventions may be able to prevent child and adolescent marijuana use. Community-level prevention frameworks, such as Communities That Care, which address the cumulative effect of risk across multiple social contexts, have been recommended for preventing early marijuana use (Scholes-Balog et al., 2020). Communities That Care is a five-phase training process that assists the formation and strategic action of community coalitions (e.g., comprised of community workers, local health services, schools, youth agencies, and police). These coalitions are guided to use knowledge from social developmental ecological theories and prevention science. An observational study in Australia associated the implementation of Communities That Care with reductions in adolescent reports of marijuana use (Toumbourou et al., 2019). The strength of a community coalition approach is that it fortifies the skills and resources of communities to address adolescent risks in a manner that is sustainable and flexible (Rowland et al., 2013; Kelly et al., 2020).
A variety of systematic literature reviews note the potential for school-level universal interventions to prevent marijuana use in countries where marijuana is illegal. In their Cochrane review, Faggiano et al. (2014) summarize evidence for universal school-based interventions in preventing marijuana and illicit drug use. Social competence approaches were found to be effective when compared to usual curricula or no intervention in preventing school-age marijuana use. Four studies were included that had assessed effects at less than 12-month follow-up and one study after 12 months. In their systematic review, Hodder et al. (2017) also identified universal school-based resiliency interventions (teaching social-emotional competency) as an effective strategy for preventing marijuana and other illicit drug use.
Cochrane reviews note some promise for family interventions to prevent early age marijuana use, in contexts where marijuana is illegal (Gates et al., 2006). Three family interventions (Focus on Families, Iowa Strengthening Families Program, and Preparing for the Drug-Free Years) were identified in a Cochrane review as having at least one study demonstrating effects in preventing marijuana use (Gates et al., 2006).
Although the current review focuses on THC, it is possible that some cannabinoids may be associated with therapeutic effects. Hall et al. (2019) summarize evidence regarding the effectiveness of cannabinoids for medicinal use. Their evidence suggests that cannabinoids might be effective in treating anxiety symptoms. They also note there is reasonable evidence that medical quality cannabis preparations and cannabinoids modestly reduce the symptoms of chronic pain, epilepsy, and nausea and vomiting.
11.7 Stepped Care Prevention Model: Role of PCP (Primary Care Provider) and BCP (Behavioral Care Provider)
Based on the information summarized in earlier sections, there are several possibilities for stepped care prevention models. In what follows, we distinguish different models for locations where marijuana use remains illegal versus those where it is has been legalized for medical or recreational use.
In all settings, it is important to promote an accurate understanding of the patterns of marijuana use that are harmful, such that they warrant intervention. Unfortunately, there continues to be public confusion as to the effects of marijuana, with many unaware of the harms. In localities where marijuana is legally available, the SDM predicts that there is likely to be an erroneous assumption that because marijuana use is normal, it is in fact safe. Within the stepped care prevention models, there is a hierarchy of more assertive and active responses available for service agencies including (a) watchful waiting, (b) psychoeducation, (c) biblio-prevention, (d) e-health prevention tools, (e) groups, and (f) individual services. In the sections that follow, we consider the evidence base for each of these possible responses as they relate to the prevention of early age and frequent marijuana use.
-
(a)
Watchful waiting may be applicable within the period that elapses between experimental marijuana use and the development of problems that may lead users to seek help. As early age marijuana use is typically not associated with readily observable problems such as violence or injuries, watchful waiting may fail to detect and intervene to prevent the development of frequent use and subsequent life-disrupting consequences including educational failure, marijuana use disorders, illicit drug use, and mental health problems (Silins et al., 2014).
As it applies to frequent adult marijuana use in localities where marijuana use has been legalized, watchful waiting is leading to increasing numbers approaching health services seeking assistance (Fischer et al., 2020). The problem with this strategy is that health services do not have the capacity or resources to assist the increasingly large numbers with intractable disorders (Fischer et al., 2020), mental health problems (Reece & Hulse, 2020a), and disabled children (Reece & Hulse, 2020b) that are projected to be increasingly caused by legalization.
-
(b)
Psychoeducation is effectively used as one component in universal programs in settings such as schools to prevent early age marijuana use (e.g., Faggiano et al., 2014) and as a component in screening and brief counseling interventions to reduce frequent and disordered use (e.g., Tanner-Smith et al., 2015). While psychoeducation is a necessary component, evaluation studies suggest it is not a sufficient stand-alone component compared to critical elements such as the building of social-emotional competence skills (Hodder et al., 2017).
-
(c)
Biblio-prevention in the form of books and brochures has shown promise as a means of conveying brief behavioral messages to prevent early and frequent marijuana use (Faggiano et al., 2014). They have also been used as a service delivery format in some screening and brief counseling strategies to prevent frequent use (Tanner-Smith et al., 2015).
-
(d)
e-Health prevention tools have been feasible to incorporate in interventions offered in tertiary education settings (Gulliver et al., 2015). However, there have been insufficient studies to assess the impacts on marijuana use.
-
(e)
Groups are effective service delivery formats for the implementation of school-level programs to prevent early age use. Systematic reviews identify classroom (Faggiano et al., 2014; Hodder et al., 2017) and peer-led intervention group programs (Georgie et al., 2016) as effective strategies to prevent early marijuana use.
-
(f)
Individual services are effective service delivery formats for the implementation of brief counseling interventions, which are linked to screening assessments in contexts such as secondary schools (Carney et al., 2016) and tertiary education settings (e.g., Tanner-Smith et al., 2015). Cochrane reviews of interventions for marijuana disorders and frequent use note limited evidence for the use of pharmacotherapies (Nielsen et al., 2019) but some short-term effects for psychosocial interventions (Gates et al., 2016). Psychosocial interventions of around four sessions combining motivational enhancement and cognitive-behavioral therapy reduced frequency of use and severity of dependence posttreatment (Gates et al., 2016).
11.8 Lessons Learned/Implementation
The overview presented in this chapter reveals evidence for prevention opportunities to reduce early age and frequent adult marijuana use. International trends in prevalence show rising rates of use and increased potency of the marijuana that is used. An examination of evidence-based prevention programs and policies suggests legalization as the major policy change that is currently driving increased marijuana use and harm. The potential for stepped care prevention models is outlined. Lessons learned to date are that it is feasible to implement evidence-based prevention approaches. Perhaps the most pertinent lesson from the studies summarized in this chapter is the importance of countering the popular misconception that marijuana legalization may offer benefits for reducing harms related to marijuana use. The available evidence from the nations and states that have legalized marijuana use to date now shows a clear and causal contribution to increase in frequent use and harm.
References
Asbridge, M., Hayden, J. A., & Cartwright, J. L. (2012). Acute cannabis consumption and motor vehicle collision risk: Systematic review of observational studies and meta-analysis. BMJ, 344, e536. https://doi.org/10.1136/bmj.e536
Carney, T., Myers, B. J., Louw, J., & Okwundu, C. I. (2016). Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database of Systematic Reviews, 2016(1), Art. No.: CD008969. https://doi.org/10.1002/14651858.CD008969.pub3
Catalano, R. F., Kosterman, R., Hawkins, J. D., Newcomb, M. D., & Abbott, R. D. (1996). Modeling the etiology of adolescent substance use: A test of the social development model. Journal of Drug Issues, 26(2), 429–455. https://doi.org/10.1177/002204269602600207
Chan, G. C., Kelly, A. B., Toumbourou, J. W., Hemphill, S. A., Young, R. M., Haynes, M. A., & Catalano, R. F. (2013). Predicting steep escalations in alcohol use over the teenage years: Age-related variations in key social influences. Addiction (Abingdon, England), 108(11), 1924–1932. https://doi.org/10.1111/add.12295
Chan, G. C. K., Hall, W., Freeman, T. P., Kelly, A. B., Ferris, J., & Winstock, A. (2017). User characteristics and effect profiles of butane hash oil: Findings across 20 countries. Drug and Alcohol Dependence, 178, 32–38. https://doi.org/10.1016/j.drugalcdep.2017.04.014
Compton, W. M., et al. (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States…. Archives of General Psychiatry, 64, 566–576.
Compton, W. M., Han, B., Jones, C. M., & Blanco, C. (2019). Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug and Alcohol Dependence, 204, 107468. https://doi.org/10.1016/j.drugalcdep.2019.05.008
EMCDDA. (2016). Prevalence maps – Prevalence of drug use in Europe. European Drug Report European Monitoring Centre for Drugs and Drug Addiction; 2016.
Faggiano, F., Minozzi, S., Versino, E., & Buscemi, D. (2014). Universal school-based prevention for illicit drug use. Cochrane Database of Systematic Reviews, 2014(12), Art. No.: CD003020. https://doi.org/10.1002/14651858.CD003020.pub3. Accessed 25 November 2020.
Fischer, B., Daldegan-Bueno, D., & Boden, J. M. (2020). Facing the option for the legalisation of cannabis use and supply in New Zealand: An overview of relevant evidence, concepts and considerations. Drug and Alcohol Review, 39(5), 555–567. https://doi.org/10.1111/dar.13087
Gates, S., McCambridge, J., Smith, L. A., & Foxcroft, D. (2006). Interventions for prevention of drug use by young people delivered in non-school settings. Cochrane Database of Systematic Reviews, 2006(1), Art. No.: CD005030. https://doi.org/10.1002/14651858.CD005030.pub2. Accessed 30 November 2020.
Gates, P. J., Sabioni, P., Copeland, J., Le Foll, B., & Gowing, L. (2016). Psychosocial interventions for cannabis use disorder. Cochrane Database of Systematic Reviews, 2016(5), Art. No.: CD005336. https://doi.org/10.1002/14651858.CD005336.pub4
Georgie, J. M., Sean, H., Deborah, M. C., Matthew, H., & Rona, C. (2016). Peer-led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11–21 years: A systematic review and meta-analysis. Addiction, 111(3), 391–407. https://doi.org/10.1111/add.13224
Gulliver, A., Farrer, L., Chan, J. K., Tait, R. J., Bennett, K., Calear, A. L., & Griffiths, K. M. (2015). Technology-based interventions for tobacco and other drug use in university and college students: A systematic review and meta-analysis. Addiction Science & Clinical Practice, 10(1), 5. https://doi.org/10.1186/s13722-015-0027-4
Hall, W., Stjepanović, D., Caulkins, J., Lynskey, M., Leung, J., Campbell, G., & Degenhardt, L. (2019). Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet, 394(10208), 1580–1590. https://doi.org/10.1016/S0140-6736(19)31789-1
Hawkins, J. D., Catalano, R. F., & Miller, J. Y. (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112, 64–105.
Hemphill, S. A., Heerde, J. A., Herrenkohl, T. I., Patton, G. C., Toumbourou, J. W., & Catalano, R. F. (2011). Risk and protective factors for adolescent substance use in Washington State, United States and Victoria, Australia: A longitudinal study. Journal of Adolescent Health, 49(3), 312–320. https://doi.org/10.1016/j.jadohealth.2010.12.017
Hodder, R. K., Freund, M., Wolfenden, L., Bowman, J., Nepal, S., Dray, J., Kingsland, M., Yoong, S. L., & Wiggers, J. (2017). Systematic review of universal school-based ‘resilience’ interventions targeting adolescent tobacco, alcohol or illicit substance use: A meta-analysis. Preventive Medicine, 100, 248–268. https://doi.org/10.1016/j.ypmed.2017.04.003
Kelly, A. B. (2012). Perceived father’s care: Protects adolescents from transitions to tobacco use at a highly vulnerable age: A short-term longitudinal study. Mental Health and Substance Use, 5(2), 173–181. https://doi.org/10.1080/17523281.2011.619502
Kelly, A. B., Chan, G. C. K., Toumbourou, J. W., O’Flaherty, M., Homel, R., Patton, G. C., & Williams, J. (2012). Very young adolescents and alcohol: Evidence of a unique susceptibility to peer alcohol use. Addictive Behaviors, 37, 414–419. https://doi.org/10.1016/j.addbeh.2011.11.038
Kelly, A. B., O’Flaherty, M., Toumbourou, J. W., Connor, J. P., Hemphill, S., & Catalano, R. F. (2011). Gender differences in the impact of families on alcohol use: A lagged longitudinal study of pre-teens. Addiction, 106, 1427–1436. https://doi.org/10.1111/j.1360-0443.2011.03435.x
Kelly, A. B., Chan, G. C. K., Mason, W. A., & Williams, J. W. (2015). The relationship between psychological distress and adolescent polydrug use. Psychology of Addictive Behaviors, 29, 787–793. https://doi.org/10.1037/adb0000068
Kelly, A. B., Weier, M., & Hall, W. D. (2018). First use of illicit drugs: The state of current knowledge. In G. Girolamo, P. McGorry, & N. Sartorius (Eds.), Age of onset of mental disorders: Etiopatogenetic and treatment implications. Springer International. isbn 978-3-319-72619-9.
Kelly, A. B., Rowland, B., Kuhn, R. A., Munnings, A. W., & Toumbourou, J. W. (2020). Chapter 7: High school students at risk of exclusion: Systemic approaches to reducing risk factors and strengthening protective factors. In P. Towl & S. A. Hemphill (Eds.), Safe, supportive, and inclusive learning environments for young people in crisis and trauma: Plaiting the rope. Routledge. isbn: 9780367243722. www.routledge.com/Safe-Supportive-and-Inclusive-Learning-Environments-for-Young-People/Towl-Hemphill/p/book/9780367243722
Kosterman, R., Bailey, J. A., et al. (2016). Marijuana legalization and parents’ attitudes, use, and parenting in Washington State. Journal of Adolescent Health, 59(4), 450–456.
Li, H. K., Kelly, A. B., Chan, G. C. K., Toumbourou, J. W., Patton, G. C., & Williams, J. (2014). The association of puberty and young adolescent alcohol use: Do parents have a moderating role? Addictive Behaviors, 39, 1389–1393. https://doi.org/10.1016/j.addbeh.2014.05.006
Miech, R. A., Johnston, L. D., O’Malley, P. M., Bachman, J. G., Schulenberg, J. E., & Patrick, M. E. (2020). Monitoring the future national survey results on drug use, 1975–2019: Volume I, secondary school students (590 pp). Institute for Social Research, The University of Michigan.
National Academies of Sciences, Engineering, and Medicine. (2017) The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. www.nationalacademies.org/hmd/Reports/2017/health-effects-of-cannabis-and-cannabinoids.aspx
Nielsen, S., Gowing, L., Sabioni, P., & Le Foll, B. (2019). Pharmacotherapies for cannabis dependence. Cochrane Database of Systematic Reviews, 2019(1), Art. No.: CD008940. https://doi.org/10.1002/14651858.CD008940.pub3
Price, J. W. (2014). Marijuana and workplace safety: An examination of urine drug tests. Journal of Addictive Diseases, 33(1), 24–27. https://doi.org/10.1080/10550887.2014.882729
Reece, A. S., & Hulse, G. K. (2020a). Co-occurrence across time and space of drug- and cannabinoid- exposure and adverse mental health outcomes in the National Survey of Drug Use and Health: Combined geotemporospatial and causal inference analysis. BMC Public Health, 20(1), 1655. https://doi.org/10.1186/s12889-020-09748-5
Reece, A. S., & Hulse, G. K. (2020b). Canadian cannabis consumption and patterns of congenital anomalies: An ecological geospatial analysis. Journal of Addiction Medicine, 14(5), e195–e210. https://doi.org/10.1097/ADM.0000000000000638
Rowland, B., Toumbourou, J. W., Osborn, A., Smith, R., Hall, J., Kremer, P., Kelly, A., Williams, J., & Leslie, E. (2013). A clustered randomised trial examining the effect of social marketing and community mobilisation on the age of uptake and levels of alcohol consumption by Australian adolescents: Study protocol. BMJ Open, 3(1), 1–8.e002423. https://doi.org/10.1136/bmjopen-2012-002423
Rowland, B., Jonkman, H., Steketee, M., Solomon, R., Solomon, S., & Toumbourou, J. W. (2019a). A cross-national comparison of the development of adolescent problem behavior: A 1-year longitudinal study in India, the Netherlands, USA and Australia. Prevention Science. https://doi.org/10.1007/s11121-019-01007-3
Rowland, B., Jonkman, H., Williams, J., Kremer, P., & Toumbourou, J. W. (2019b). Community variation in adolescent cannabis use in Australia and the Netherlands. Addictive Behaviors, 90, 204–209. https://doi.org/10.1016/j.addbeh.2018.10.027
Scholes-Balog, K. E., Hemphill, S. A., Heerde, J. A., Toumbourou, J. W., & Patton, G. C. (2020). Childhood social environmental and behavioural predictors of early adolescent onset cannabis use. Drug and Alcohol Review, 39(4), 384–393. https://doi.org/10.1111/dar.13077
Silins, E., Horwood, J., Patton, G. C., Fergusson, D. H., Olsson, C. A., Hutchinson, D. M., Spry, E., Toumbourou, J. W., Degenhardt, L., Swift, W., Coffey, C., Tait, R. J., Letcher, P., Copeland, J., & Mattick, R. P. (2014). Young adult sequelae of adolescent cannabis use: An integrative analysis across three Australasian Cohorts. Lancet Psychiatry, 1(4), 286–293. https://doi.org/10.1016/S2215-0366(14)70307-4
Smith, R., Hall, K. E., Etkind, P., & Van Dyke, M. (2018). Current marijuana use by industry and occupation – Colorado, 2014–2015. MMWR Morbidity and Mortality Weekly Report, 67(14), 409–413. https://doi.org/10.15585/mmwr.mm6714a1
Tanner-Smith, E. E., Steinka-Fry, K. T., Hennessy, E. A., Lipsey, M. W., & Winters, K. C. (2015). Can brief alcohol interventions for youth also address concurrent illicit drug use? Results from a meta-analysis. Journal of Youth and Adolescence, 44(5), 1011–1023. https://doi.org/10.1007/s10964-015-0252-x
Toumbourou, J. W., & Catalano, R. F. (2005). Predicting developmentally harmful substance use. In T. Stockwell, P. Gruenewald, J. W. Toumbourou, & W. Loxley (Eds.), Preventing harmful substance use: The evidence base for policy and practice (pp. 53–66). Wiley.
Toumbourou, J. W., Olsson, C., Rowland, B., Renati, S., & Hallam, B. (2014). Health Psychology intervention in key social environments to promote adolescent health. Australian Psychologist, 49, 66–74. https://doi.org/10.1111/ap.12043
Toumbourou, J. W., Rowland, B., Williams, J., Smith, R., & Patton, G. C. (2019). Community intervention to prevent adolescent health behavior problems: Evaluation of communities that care in Australia. Health Psychology, 38(6), 536–544. https://doi.org/10.1037/hea0000735
Weier, M., Chan, G. C. K., Quinn, C., Hides, L., & Hall, W. D. (2016). Cannabis use in 14 to 25 year old Australians 1998–2013: Technical report. Centre for Youth Substance Abuse Research, University of Queensland.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Toumbourou, J.W., Heerde, J., Kelly, A., Bailey, J. (2021). Marijuana Use. In: O’Donohue, W., Zimmermann, M. (eds) Handbook of Evidence-Based Prevention of Behavioral Disorders in Integrated Care. Springer, Cham. https://doi.org/10.1007/978-3-030-83469-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-83469-2_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-83468-5
Online ISBN: 978-3-030-83469-2
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)