Abstract
Biomechanical behaviour of rotator cuff allows for the articular stability and, at same time, for the humeral motion. Tears of rotator cuff altered the normal biomechanics of the shoulder, leading to functional impairments. Several rotator cuff repair and treatment strategies have been proposed, with the aim to fully restore the biomechanics of the injured shoulder. To understand the biomechanical features of the normal rotator cuff and the mechanical consequences of rotator cuff tears and their repair treatment is mandatory, in order to better address this kind of shoulder pathology. This chapter provides an overview of the normal and torn rotator cuff biomechanics, followed by a description of the mechanical characteristics and effect of the main repair strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Although the rotator cuff tears are more common in older individuals, this kind of pathology also frequently affects athletes and young workers engaged in repetitive overhead activities. The rotator cuff is a complex musculotendinous unit, which plays a major role in glenohumeral joint stability and mobilization. Injuries of the rotator cuff can lead to significant functional impairment, resulting in time loss from sport and competition, and, in the more advanced stages, in trouble in performing daily activities. Therefore, fully understand the biomechanical features of rotator cuff tears and repair is crucial to better manage and address the injuries of rotator cuff. This chapter provide an overview of the normal and injured rotator cuff biomechanics, followed by literature evidence and considerations about the biomechanical concept of the rotator cuff repair.
2 Biomechanical Properties of the Rotator Cuff
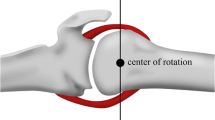
Rotator cuff is composed by the tendons of four muscles: the supraspinatus, the infraspinatus, the teres minor and the subscapularis. These muscles create compressive forces to stabilize the glenohumeral joint and generate torque to move the humerus [1]. In particular, the compressive and antagonistic forces of the subscapularis anteriorly and infraspinatus and teres minor posteriorly, imparts a compression on the humeral head into the glenoid, with a mechanism known as “concavity compression” [2] (Fig. 11.1). This tendinous connection, with the addition of ligaments and bone factors, allows for the articular stability and, at same time, for the humeral motion with respect to the scapula, defining the role for tendons as specific active restraints during the shoulder movement [3]. The wide range of motion of glenohumeral joint is allowed by the variety of rotational moments of the cuff muscles, whose tendons insert continuously around the humeral head. The force and the torque that a muscle can generate vary with the position of the joint: at the extremes of the range of motion, the muscles of the rotator cuff are weaker, because they are fully contracted or extended, while the maximal force is in the midrange of their pretension [4]). The supraspinatus has a major role in humeral elevation at higher glenohumeral angles, while at lower angles the deltoid contribution is higher. The subscapularis and infraspinatus also play a role in abduction during internal and external humeral rotation [5]. During the arm motion, movements of the scapulothoracic joint are associated with those of glenohumeral joint, performing a complex and coordinated pattern of motions that Codman defined the “scapulohumeral rhythm” [6]: while under the 90° of humeral elevation scapular and clavicular motion are minimal, beyond the 90° there is upward rotation, posterior tilting and external rotation of the scapula to allow for the full range of motion in the upper extremity [7].
As in the shoulder there is not a fixed axis of rotation, the functions of the shoulder muscles must be balanced, working together to produce a net torque and neutralize opposed elements: the superior portion of the cuff and the deltoid neutralize the adduction of the latissimus dorsi during pure internal rotation, the posterior cuff and the posterior deltoid muscles neutralize the internal rotation moment of the anterior deltoid during forward elevation without rotation [5].
The tendons of the rotator cuff are subjected to complex tension loads. Compressive loads stress the cuff between the humeral head and the coracoacromial arch: in vivo subacromial pressure values of 8 mmHg at rest, 39 mmHg at 45° of flexion and 56 with the arm in elevated position with 1 Kg weight held in the hand were reported [8]. Concentric and eccentric tension loads are produced in abduction against resistance and in active resistance to downward respectively [8].
3 Biomechanics of Rotator Cuff Tears
3.1 Mechanical Factors in Rotator Cuff Tears
Rotator cuff tear aetiology is multifactorial: the role of extrinsic factors, which have been classically considered among the causes of rotator cuff tears, takes alongside to that of intrinsic factors, such as biologic degeneration and deficit of vascularisation [3]. The extrinsic theory dominated the pathophysiology of the rotator cuff tears and the impingement syndrome for decades. In 1931, Meyer suggested that tears of the rotator cuff could develop secondary to attrition due to the friction between the rotator cuff and the under surface of the acromion [9]. In the 1972, Neer introduced the theory of subacromial impingement, describing it as a mechanical phenomenon corresponding to impingement of the rotator cuff tendon beneath the anterior-inferior acromion [10]. Neer observed that this condition affected mainly the supraspinatus tendon insertion on the greater tuberosity, and that occurred when the shoulder was placed in forward flexion and external rotation. Moreover, he observed that this condition presupposed an anatomic irregularity of the acromion and the presence of bony spurs in the site of coracoacromial ligament insertion on the acromion [10]. The correlation between the acromial shape and the cuff disease was supported by subsequent cadaveric studies, in which a higher prevalence of full-thickness tears of the rotator cuff was noted in association with the hooked or type III acromion [11, 12]. However, later, acromial impingement was found not to be the primary cause of rotator cuff tears [3, 5, 13]: it resulted associated with changes on the bursal side of the rotator cuff tears which is less frequently affected than the intra-tendinous or articular side [14], and the acromioplasty procedures did not avoid the occurrence of rotator cuff tears, leading to damage of tendons in 20% of cases [15]. Furthermore, the morphology of the acromion seemed to be secondary to pathology of the bursal side of the cuff [16, 17]: the cuff degeneration lead to produce an acromial hook, which results in a greater load on the coracoacromial arch producing traction spurs in the coracoacromial ligament [18, 19]. A contact between rotator cuff and the coracoacromial arch was also reported in normal shoulders in both cadaveric studies and healthy human subject, suggesting that the contact phenomenon between the coracoacromial arch and the rotator cuff was not a pathological but a physiological condition [20, 21].
Further bone features has been associated with injuries of the rotator cuff; a glenohumeral joint with a higher acromial coverage index, which is the ratio between the distance from the glenoid plane to the acromion and the distance from the glenoid plane to the lateral aspect of the humeral head, is associated with an increased risk of rotator cuff tear [22]. The angle between the line connecting the inferior border to the superior border of the glenoid fossa, and a second line connecting the inferior border of the glenoid fossa to the most inferolateral point of the acromion, represents the critical shoulder angle (CSA) (Fig. 11.2). Since it combines the measurement of the glenoid inclination and the lateral extension of the acromion, CSA has been used to predict the presence of degenerative cuff tears [23]. In a biomechanical simulation model, a larger CSA has been shown to increase the supraspinatus tendon load at low degrees of abduction compared to a control with a normal CSA [24].
The mechanism of rotator cuff fatigue damage starts with isolated changes in microstructures and develops into severe matrix disruption and kinked deformation; this degeneration, in addition to biological changes due to aging and overuse, predispose the tendons to failure [3]. Studies of torn rotator cuff tendons have revealed that degenerative changes also appear medially from the tear, indicating the presence of degeneration before the tear occurs [25, 26]. In particular, the critical zone of the rotator cuff, localized at 1 cm medially to the supraspinatus insertion in the tuberculus major, resulted to have a decreased vascularisation [27]. This feature, associated with increased local pressure during humeral elevation and abduction, may be related with the degeneration process, predisposing the tendons to failure [3].
In patients who require to achieve a large range of external rotation, such as throwers, defects of the deep surface of the rotator cuff are common. Among these patients, the mechanism of cuff injury is explained by the abutment of the edge of the glenoid against the under surface of the supraspinatus tendon at the extreme of the external rotation [5].
Rotator cuff tears typically start at the deep surface of the supraspinatus tendon, close to the long head of the biceps. This site is subject to greater loads, even at rest. The complex and coordinated actions of the rotator cuff muscles are coupled in a manner that produces increased strain on the surrounding tendons when a tear in one tendon occurs. For this reason, a tear of one tendon in the rotator cuff could potentially lead to an increased risk for injury in the remaining muscles, determining a pattern that induces the tear progression and extension [28]. The loads are concentred at the margin of the tear, facilitating the extension of the defect. A tear of 60% of the tendon thickness increases of 23.8% the tensile strain in the posterior tendon [29]. Tears of the articular side of the infraspinatus increase the strain in the middle and superior portions of the supraspinatus. Subsequently, the defects of supraspinatus propagate posteriorly through the reminder of the supraspinatus and the infraspinatus [5].
3.2 Biomechanical Effects of Rotator Cuff Tears
Tears in the rotator cuff result in altered glenohumeral joint mechanics and are frequently associated with loss of strength and stability of the shoulder. However, clear evidence about the relationship between the tear features and the functional outcomes still lack. The superior translation of the humeral head represents the most important biomechanical consequence of the rotator cuff tears, and the main radiograph signs of massive cuff deficiency. Large-to-massive tears may lead to rotator cuff tear arthropathy, which implies the development of progressive glenohumeral and acromiohumeral arthritis secondary to the tear, associated with joint pain and reduced humeral elevation [30, 31].
When the dynamic function of rotator cuff is compromised by a tear, the external rotation and the elevation are primarily decreased. Burkhart introduced the concept of the rotator cuff cable [32], a thickened area of the rotator cuff tendon which inserts anteriorly between the anterior insertion of the supraspinatus and superior half insertion of subscapularis, and posteriorly near the inferior insertion of infraspinatus tendon. Burkhart noted that rotator cuff tears that did not involve the cable, such as supraspinatus tears alone, were functional and biomechanically intact, because the cable remained intact [33].
Regarding the abduction torque, the features of rotator cuff tears which could affect the force transmission are the supraspinatus tendon detachment and the retraction of its muscle. In a cadaveric study [34] the effect of different size and shape of the rotator cuff tear on in vitro force transmission was investigated, comparing different size of supraspinatus tendon detachment with a defect of tendon substance and muscle retraction: authors reported that only after detachment of the entire width of the supraspinatus tendon, the transmitted force significantly decreased; this finding support the concept of rotator cable, pointing out that the muscle forces are effectively transmitted by the rotator cuff as long as the rotator cable is intact. Furthermore, in this cadaveric study, the simulated muscle retraction resulted in significantly greater decrease in transmitted force compared with the isolated detachment of the tendon, showing that rotator cuff muscle retraction contributes substantially to loss of shoulder strength following large rotator cuff ruptures [34].
In order to gain more insight in the effect of rotator cuff tear in shoulder biomechanics, the kinematics of the joint with a defect of the cuff was analysed in literature. In particular, the assessment of humeral head position, external humeral rotation, humeral abduction and associated scapulothoracic rotations were investigated, and the findings showed that the shoulder kinematics is associated with rotator cuff tear size [35,36,37]: while isolated tears of supraspinatus had no significant biomechanics consequences, massive cuff tears involving supraspinatus or subscapularis altered significantly the kinematics of the shoulder. In a cadaveric study [36] in which five shoulder specimens were subjected to different loading conditions with sequentially larger anterosuperior cuff tears, a significant increase in anterior-superior and superior translation resulted only after that the anterosuperior tears were extended to the superior half of the subscapularis. No significant biomechanical consequences, in contrast, were reported after isolated tears of supraspinatus. These results support the rotator cuff cable concept, suggesting that the preservation or the loss of the anterior cable attachment represents an important determinant of the biomechanics of anterosuperior rotator cuff tears [36]. In line with these findings, in another cadaveric study, in which the effect of 1 and 3 cm isolated supraspinatus tears on joint kinematics was examined, no significant changes were founded in glenohumeral translation [38].
Regarding the position of humeral head along the superior-inferior and anterior-posterior axis during scapular plane abduction in shoulder with rotator cuff tears, superior migration of humeral head, when the superior shear forces created by the deltoid are no longer effectively opposed, was described in studies employed in vitro static evaluation techniques [39, 40] (Fig. 11.3).
In a dynamic in vivo study, on the other hand, an inferior dynamic translation was founded during scapular plane humeral abduction [41]. During an in vitro simulation of active shoulder kinematics, the effect of three sequential simulated tears affecting the supraspinatus and the subscapularis during the unconstrained glenohumeral abduction was provided [35]: authors founded that, as the size of the simulated cuff tear increased, the plane of elevation became significantly more posterior at all angles of abduction, and the position of humeral head became more anterior for angle of abduction greater than 50°. No differences, on the other hand, were founded regarding the position of humeral head along the superior-inferior axis [35]. In an in vivo study in which a 3D to 2D model-to-image registration techniques was provided [42], a more anterior position of the humeral head centre was founded in shoulder with large-to-massive full-thickness rotator cuff tear than in controls, at internal rotation position during dynamic axial rotation in adducted position. Moreover, authors reported a more medial position of humeral head in patients with rotator cuff tear than in controls at the late phase of dynamic scapular plane abduction [42]. A recent in vivo three-dimensional bone model of ten shoulders with massive rotator cuff tears showed a significantly higher humeral head position under the 40° of abduction angle than the normal contralateral shoulder [43].
Regarding the associated scapular kinematics, Authors of the latter study reported a significant increase of scapular upward rotation in the initial position at 20° of humeral abduction and at the final elevation, over 130° of humeral abduction in shoulders with rotator cuff tears [43]. In another kinematics study, the comparison between patients with massive posterior-superior rotator cuff tear and patients with subacromial pain syndrome associated with intact rotator cuff showed a lower humero-thoracic abduction and forward flexion, associated with a marked increase in scapular upward rotation in the rotator cuff injured group [37]. Furthermore, decline in humeral abduction and increase in scapular upward rotation were founded in simulated massive posterior-superior rotator cuff tear created after a suprascapular nerve block in healthy volunteers [44]. These results about the postero-superior massive tears, since the infraspinatus muscle has a direct impact on the glenohumeral joint and does not directly control scapula-thorax motion, suggested that the increased scapular upward rotation (i.e. scapulo-thorax lateral rotation) should be compensatory in nature [37, 44] (Fig. 11.4).
Scapular associated kinematics in rotator cuff tears. In vivo kinematics studies reported increase in scapular upward rotation (scapula-thorax lateral rotation) associated with a decreased humeral abduction in shoulders with postero-superior massive rotator cuff tears. a: normal cuff; b: injured cuff
4 Biomechanics of Rotator Cuff Repair
The rotator cuff repair must aim to fully restore the anatomy and function of the rotator cuff tendons.
Regarding isolated supraspinatus lesion, the biomechanical effect of repair was seen by Yu et al. [45] only at 10° abduction with 60 N loading with an increase in percent inferior force after repair that may represent greater concavity compression and spacer effect, which are both important functions of the supraspinatus. This same increase was not observed with the deltoid loaded to 90 N, which could be a function of the effect of loading producing an offset between the inferior and superior forces. No changes were seen in the contact area, pressure, or position after repair, suggesting that repair of full-thickness rotator cuff tears does not completely recreate normal glenohumeral biomechanics or that no change existed in the pathologic tear specimens from normal.
By the way, when a tear is large, it may sometimes be difficult to bring the torn edges back to the original insertion site of the greater tuberosity. In those cases, a medial shift of the insertion site of the cuff tendon is one of the surgical options. According to biomechanical studies by Yamamoto and those by Liu et al., a medial shift of 17 mm or more should be avoided from the functional point of view because it reduces both the moment arm and the range of shoulder motion [46, 47].
Several biomechanical studies investigated the effect of different angles anchor insertion and inclination in rotator cuff repair, with the aim to achieve greater pullout strength possible. In 1995 Burkhart introduced the deadman theory [48], suggesting that an anchor inserted at 45° may show the greatest pullout strength theoretically. However, biomechanical pullout studies, have shown that anchors inserted at 90°, 135° or between 105° and 135° present the greatest pullout strength [49,50,51], advancing that the deadman theory depends on the friction of the anchors. In a review associated with additional biomechanical studies, Itoi et al. [52] reported that the insertion angle of 90° is the strongest for a threated anchor. Furthermore, authors of this latter study showed that the pullout strength depends on the inclination of the anchor, friction of the anchor–bone interface and quality of bone. In particular, the insertion angle of the suture threated anchor should replicate the angle of applied load to ensure the optimum pullout strength [52]. (Fig. 11.5).
Regarding the rows of the anchor, there are single, double and triple row repair described, with associated different types of stiches configuration. In a cadaveric study, in which a simple single-row repair construct and a linked single-row construct were compared, no significant differences in ultimate load to failure and resistance to gap formation between the simple and the linked single-row construct were founded [53].
Many biomechanical studies have already clarified that the use of transosseous equivalent repair for rotator cuff repair was superior to other techniques such as the single- or dual-row technique in terms of contact area or pressure between the rotator cuff tendon and the footprint, and the initial pullout strength [54,55,56,57]. Using the transosseous equivalent technique, a greater initial fixation strength may be achieved. However, the tendon itself is inherently elastic. Fixing the torn tendon with the transosseous equivalent repair technique, the tendon may lose its inherent elasticity due to the crossover of the strong sutures. The initial strong fixation is needed to avoid pullout failure after surgery. However, the fixation is required only for the first few months. Yamamoto et al. [57] demonstrated that the rotator cuff tendon became stiffer after arthroscopic rotator cuff repair, especially transosseous equivalent repair, by measuring the strain of the supraspinatus tendon using ultrasound elastography. Results showed that the superficial layer of the supraspinatus tendon was stiffer after transosseous equivalent repair than the contralateral side at the final follow up [57]. In addition, their study revealed that a high-stress concentration was observed around the insertion sites of the medial row threads.
The tying of the medial knots during transosseous equivalent repair is controversial. There are several biomechanical reports demonstrating biomechanical improvement (ultimate load, contact pressure, and stiffness) by tying the medial row of a transosseous equivalent repair [58, 59]. Tamboli et al. [60] investigated the effects of bite-size horizontal mattress stitch: whereas a 4-mm bite fixed the tendon more tightly but at the cost of decreased ultimate strength, a 10-mm bite conveyed greater ultimate strength but with increased gap and strain. Authors concluded that for transosseous equivalent repair, large stitches are beneficial because the repaired tendon has a higher strength, and the slightly mobile medial knot can be tightened by lateral fixation.
Anatomic and biomechanical cadaveric studies highlighted the structural and functional relationship between superior shoulder capsule and the articular side of rotator cuff suggesting that articular-sided partial-thickness tears include detachment of the superior shoulder capsule from the greater tuberosity [61, 62]. In a cadaveric study a significant increase of anterior and inferior glenohumeral translation was founded after that a tear of superior capsule was performed, compared with the intact capsule state [62]. Satisfactory results were reported about the repair procedure to manage articular-sided partial-thickness rotator cuff tear [63, 64]. In a cadaveric analysis of the effect of an articular-sided partial supraspinatus and infraspinatus tear during the simulated late-cocking and acceleration phases of throwing, no significant differences in humeral head apex position, internal impingement area or glenohumeral contact pressure were reported compared with the intact condition [65]. In the same study, authors performed a transtendon repair with two anchors providing a significant decrease of external humeral rotation, posterior shift of humeral apex position, decrease of glenohumeral contact pressure at maximum external rotation and decrease of internal impingement area compared with the intact and the torn status during both the two phases of throwing. These results suggested that transtendon repair of an articular-sided partial supraspinatus tear may cause overtightening of the torn tendon and superior capsule, minimizing secondary subacromial and interior impingement, and that careful evaluation of patient individual shoulder laxity should be assessed when the transtendon repair is chosen for address an articular-sided partial tear [65].
4.1 Irreparable Tears
Rotator cuff tears are defined as irreparable when the lesions cannot be repaired primarily to their insertion on the tuberosities with conventional techniques of surgical release/mobilization, because of their size, retraction, and muscle impairment caused by atrophy and fatty infiltration [66].
With the aim to better address the massive irreparable rotator cuff tears, Burkhart et al. [33] introduced the concept of the “suspension bridge” which lead to the development of the functional partial repair: the repair of the whole subscapularis and the inferior half of infraspinatus, without the complete coverage of the defect, can restore the normal shoulder mechanics, recovering the transverse force couples and a stable fulcrum for glenohumeral kinematics [66].
Several biomechanical studies investigated the influence of the superior capsule reconstruction on the superior stability of the shoulder joint. Superior capsular reconstruction (SCR) potentially improves function by re-centering the humeral head and improving glenohumeral kinematics [67].
Several techniques for performing superior capsule reconstruction have been described, characterized by different type of the graft (fascia lata, extracellular matrix dermal grafts, long head of biceps and tendon allografts), whether performed in an open manner or arthroscopically, the mode of the glenoid and greater tuberosity fixation, and whether the anchors are all inserted before or after passage of the graft [67,68,69,70,71,72,73].
In a cadaveric study involving eight shoulders, Mihata et al. [74] compared the superior translations of the proximal humerus in five conditions: intact rotator cuff, excised supraspinatus, reconstructed supraspinatus using a bridging graft connecting the remnant of the supraspinatus to the greater tuberosity, reconstructed superior capsule with graft attached to the glenoid and the greater tuberosity, reconstructed superior capsule and supraspinatus with the patch [74]. They demonstrated that excising the supraspinatus tendon resulted in a significant increase in the superior translation of the proximal humerus, which was fully restored only when the superior capsule was reconstructed with the graft [74]. Supraspinatus reconstruction with the graft only resulted in a partial restoration of superior translation [74]. In another biomechanical study, Mihata et al. demonstrated an 8 mm thick fascia lata graft resulted in a greater superior stability than a 4 mm thick graft [75]. A significant decrease in superior translation was only witnessed with 8 mm thick graft as compared to the 4 mm thick graft [75].
When performing SCR, it was also reported that addition of posterior side-to-side suturing between the graft and residual infraspinatus tendon increases the superior stability of the proximal humerus [76]. In a biomechanical study, SCR without posterior side-to-side suturing, did not inhibit glenohumeral superior translation, whereas addition of posterior side-to-side suturing resulted in significantly reduced superior translation [76].
The superior rotator cuff and superior capsule reconstruction technique using long head of biceps (LHB) was also proposed and described in literature. In a biomechanical study by Han et al. the superior capsule reconstruction using LHB permitted to reduced humeral head translation and subacromial contact pressure [77]. Moreover, Authors did not find significant differences between the isolated SCR using LHB procedure and the side-to-side repair augmentation associated procedure [77].
Recently, performing acromioplasty with a rotator cuff repair has become a subject of controversy. There have been some clinical reports describing the excellent outcome after cuff repair without acromioplasty [78, 79]. According to the 2011 guidelines published by the American Academy of Orthopaedic Surgeons, [80] the routine acromioplasty is not required at the time of rotator cuff repair. A biomechanical study by Denard et al. [81] demonstrated that a limited acromioplasty, of 3 mm in thickness, might be enough for decompression while preserving the coracoacromial ligament. Because of variations in the distance between the undersurface of the acromion and the cuff surface, the level of acromioplasty should be decided during surgery on a patient specific level.
Although the results of routinely acromioplastic are controversial, Mihata et al., investigating the effects of acromioplasty on shoulder biomechanics associated with superior capsule reconstruction [82], illustrated that adding acromioplasty to SCR with fascia lata significantly decreased the subacromial peak contact area compared to SCR without acromioplasty, without altering the humeral head position, superior translation or subacromial peak contact pressure [82]. Based on their findings the authors suggested that when performing SCR, acromioplasty may help to decrease the postoperative risk of abrasion and tearing of the graft beneath the acromion, without increasing the risk of superior translation [82].
To treat the irreparable rotator cuff tears the subacromial balloon spacers have been proposed. There is limited biomechanical literature on the subacromial balloon spacer and its ability to manage irreparable rotator cuff tears. Literature is also lacking on the appropriate inflation volumes.
The biomechanical study by Singh et al. [83] found out that the 25-mL balloon displaced the humeral head more inferior than the intact condition with a mean difference statistically significant, but it is not likely clinically significant. Their study has some limitations and they only tested static abduction.
5 Conclusions
The rotator cuff tears modify shoulder biomechanics radically. Rotator cuff repair allows to restore biomechanics in order to address the clinical impairment. If the tear is not completely reparable, adding superior capsule reconstruction to partial cuff repair could be a good option for young and active patient without rotator cuff tear arthropathy, with the aim to restore the native shoulder biomechanics.
References
Karduna AR, Williams GR, Williams JL, Iannotti JP. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J Orthop Res. 1996;14(6):986–93.
Soslowsky LJ, Malicky DM, Blasier RB. Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J Shoulder Elb Surg. 1997;6(4):371–9.
Huegel J, Williams AA, Soslowsky LJ. Rotator cuff biology and biomechanics: a review of normal and pathological conditions. Curr Rheumatol Rep. 2015;17(1):476.
Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elb Surg. 1998;7(4):393–6.
Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V. Biomechanics of the rotator cuff: European perspective. Med Sport Sci. 2012;57:10–7.
G. BJ. The Shoulder. By E. A. Codman. Reprint of the 1934 edition. 7 x 6 in. Pp. 513, with 85 figures, 7 plates (2 in colour), some tables and an epilogue of 29 pages. 1965. Brooklyn: G. Miller & Company. Price $17.50. The Journal of Bone and Joint Surgery British volume. 1967;49-B(1):206-.
Provencher CM, Makani A, McNeil JW, Pomerantz ML, Golijanin P, Gross D. The role of the scapula in throwing disorders. Sports Med Arthrosc Rev. 2014;22(2):80–7.
Sigholm G, Styf J, Herberts P. Subacromial pressure during diagnostic shoulder tests. Clin Biomech (Bristol, Avon). 1988;3(3):187–9.
L M. Rupture of the supraspinatus tendon. J Bone Jt Surg. 1937;19:640–2.
Neer CS 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50.
Bigliani LU. The morphology of the acromion and its relationship to rotator cuff tears. OrthopTrans. 1986;10:228.
Zuckerman JD, Kummer FJ, Cuomo F, Simon J, Rosenblum S, Katz N. The influence of coracoacromial arch anatomy on rotator cuff tears. J Shoulder Elb Surg. 1992;1(1):4–14.
Shi LL, Edwards TB. The role of acromioplasty for management of rotator cuff problems: where is the evidence? Adv Orthop. 2012;2012:467571.
Schneeberger AG, Nyffeler RW, Gerber C. Structural changes of the rotator cuff caused by experimental subacromial impingement in the rat. J Shoulder Elb Surg. 1998;7(4):375–80.
Hyvönen P, Lohi S, Jalovaara P. Open acromioplasty does not prevent the progression of an impingement syndrome to a tear. Nine-year follow-up of 96 cases. J Bone Joint Surg Br. 1998;80(5):813–6.
Ozaki J, Fujimoto S, Nakagawa Y, Masuhara K, Tamai S. Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavera. J Bone Joint Surg Am. 1988;70(8):1224–30.
Fukuda H, Hamada K, Nakajima T, Tomonaga A. Pathology and pathogenesis of the intratendinous tearing of the rotator cuff viewed from en bloc histologic sections. Clin Orthop Relat Res. 1994;304:60–7.
Yazici M, Kopuz C, Gülman B. Morphologic variants of acromion in neonatal cadavers. J Pediatr Orthop. 1995;15(5):644–7.
Flatow EL, Soslowsky LJ, Ticker JB, Pawluk RJ. Hepler M, ark J, et al. excursion of the rotator cuff under the acromion. Patterns of subacromial contact. Am J Sports Med. 1994;22(6):779–88.
Yamamoto N, Muraki T, Sperling JW, Steinmann SP, Itoi E, Cofield RH, et al. Contact between the coracoacromial arch and the rotator cuff tendons in nonpathologic situations: a cadaveric study. J Shoulder Elb Surg. 2010;19(5):681–7.
Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA 3rd. Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Joint Surg Am. 2011;93(19):1827–32.
Torrens C, López JM, Puente I, Cáceres E. The influence of the acromial coverage index in rotator cuff tears. J Shoulder Elb Surg. 2007;16(3):347–51.
Moor BK, Röthlisberger M, Müller DA, Zumstein MA, Bouaicha S, Ehlinger M, et al. Age, trauma and the critical shoulder angle accurately predict supraspinatus tendon tears. Orthop Traumatol Surg Res. 2014;100(5):489–94.
Gerber C, Snedeker JG, Baumgartner D, Viehöfer AF. Supraspinatus tendon load during abduction is dependent on the size of the critical shoulder angle: a biomechanical analysis. J Orthop Res. 2014;32(7):952–7.
Castagna A, Cesari E, Garofalo R, Gigante A, Conti M, Markopoulos N, et al. Matrix metalloproteases and their inhibitors are altered in torn rotator cuff tendons, but also in the macroscopically and histologically intact portion of those tendons. Muscles Ligaments Tendons J. 2013;3(3):132–8.
Garofalo R, Cesari E, Vinci E, Castagna A. Role of metalloproteinases in rotator cuff tear. Sports Med Arthrosc Rev. 2011;19(3):207–12.
Rothman RH, Parke WW. The vascular anatomy of the rotator cuff. Clin Orthop Relat Res. 1965;41:176–86.
Andarawis-Puri N, Kuntz AF, Jawad AF, Soslowsky LJ. Infraspinatus and supraspinatus tendon strain explained using multiple regression models. Ann Biomed Eng. 2010;38(9):2979–87.
Yang S, Park HS, Flores S, Levin SD, Makhsous M, Lin F, et al. Biomechanical analysis of bursal-sided partial thickness rotator cuff tears. J Shoulder Elb Surg. 2009;18(3):379–85.
Collins DN, Harryman DT 2nd. Arthroplasty for arthritis and rotator cuff deficiency. Orthop Clin North Am. 1997;28(2):225–39.
Jensen KL, Williams GR Jr, Russell IJ, Rockwood CA Jr. Rotator cuff tear arthropathy. J Bone Joint Surg Am. 1999;81(9):1312–24.
Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder's "suspension bridge". Arthroscopy. 1993;9(6):611–6.
Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10(4):363–70.
Halder AM, O'Driscoll SW, Heers G, Mura N, Zobitz ME, An KN, et al. Biomechanical comparison of effects of supraspinatus tendon detachments, tendon defects, and muscle retractions. JBJS. 2002;84(5):780–5.
Kedgley AE, Mackenzie GA, Ferreira LM, Johnson JA, Faber KJ. In vitro kinematics of the shoulder following rotator cuff injury. Clin Biomech (Bristol, Avon). 2007;22(10):1068–73.
Su W-R, Budoff JE, Luo Z-P. The effect of Anterosuperior rotator cuff tears on Glenohumeral translation. Arthroscopy. 2009;25(3):282–9.
Kolk A, Henseler JF, de Witte PB, van Zwet EW, van der Zwaal P, Visser CPJ, et al. The effect of a rotator cuff tear and its size on three-dimensional shoulder motion. Clin Biomech (Bristol, Avon). 2017;45:43–51.
Mueller AM, Rosso C, Entezari V, McKenzie B, Hasebroock A, Cereatti A, et al. The effect of supraspinatus tears on glenohumeral translations in passive pitching motion. Am J Sports Med. 2014;42(10):2455–62.
Konrad GG, Markmiller M, Jolly JT, Ruter AE, Sudkamp NP, McMahon PJ, et al. Decreasing glenoid inclination improves function in shoulders with simulated massive rotator cuff tears. Clin Biomech (Bristol, Avon). 2006;21(9):942–9.
Mura N, O'Driscoll SW, Zobitz ME, Heers G, Jenkyn TR, Chou SM, et al. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: a biomechanical study. J Shoulder Elb Surg. 2003;12(2):179–84.
Millett PJ, Giphart JE, Wilson KJ, Kagnes K, Greenspoon JA. Alterations in Glenohumeral kinematics in patients with rotator cuff tears measured with biplane fluoroscopy. Arthroscopy. 2016;32(3):446–51.
Kozono N, Okada T, Takeuchi N, Hamai S, Higaki H, Shimoto T, et al. Dynamic kinematics of the glenohumeral joint in shoulders with rotator cuff tears. J Orthop Surg Res. 2018;13(1):9.
Kim D, Lee B, Yeom J, Cha J, Han J. Three-dimensional in vivo comparative analysis of the kinematics of normal shoulders and shoulders with massive rotator cuff tears with successful conservative treatment. Clin Biomech (Bristol, Avon). 2020;75:104990.
McCully SP, Suprak DN, Kosek P, Karduna AR. Suprascapular nerve block disrupts the normal pattern of scapular kinematics. Clin Biomech (Bristol, Avon). 2006;21(6):545–53.
Yu J, McGarry MH, Lee YS, Duong LV, Lee TQ. Biomechanical effects of supraspinatus repair on the glenohumeral joint. J Shoulder Elbow Surg. 2005;14(1 Suppl S):65s–71s.
Yamamoto N, Itoi E, Tuoheti Y, Seki N, Abe H, Minagawa H, et al. Glenohumeral joint motion after medial shift of the attachment site of the supraspinatus tendon: a cadaveric study. J Shoulder Elb Surg. 2007;16(3):373–8.
Liu J, Hughes RE, O'Driscoll SW, An KN. Biomechanical effect of medial advancement of the supraspinatus tendon. A study in cadavera. J Bone Joint Surg Am. 1998;80(6):853–9.
Burkhart SS. The deadman theory of suture anchors: observations along a South Texas fence line. Arthroscopy. 1995;11(1):119–23.
Strauss E, Frank D, Kubiak E, Kummer F, Rokito A. The effect of the angle of suture anchor insertion on fixation failure at the tendon-suture interface after rotator cuff repair: deadman's angle revisited. Arthroscopy. 2009;25(6):597–602.
Clevenger TA, Beebe MJ, Strauss EJ, Kubiak EN. The effect of insertion angle on the pullout strength of threaded suture anchors: a validation of the deadman theory. Arthroscopy. 2014;30(8):900–5.
Green RN, Donaldson OW, Dafydd M, Evans SL, Kulkarni R. Biomechanical study: determining the optimum insertion angle for screw-in suture anchors-is deadman's angle correct? Arthroscopy. 2014;30(12):1535–9.
Itoi E, Nagamoto H, Sano H, Yamamoto N, Kawakami J. Deadman theory revisited. Biomed Mater Eng. 2016;27(2–3):171–81.
Meisel AF, Henninger HB, Barber FA, Getelman MH. Biomechanical comparison of standard and linked single-row rotator cuff repairs in a human cadaver model. Arthroscopy. 2017;33(5):938–44.
Mazzocca AD, Bollier MJ, Ciminiello AM, Obopilwe E, DeAngelis JP, Burkhart SS, et al. Biomechanical evaluation of arthroscopic rotator cuff repairs over time. Arthroscopy. 2010;26(5):592–9.
Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elb Surg. 2007;16(4):461–8.
Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elb Surg. 2007;16(4):469–76.
Yamamoto N, Itoi E. A review of biomechanics of the shoulder and biomechanical concepts of rotator cuff repair. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(1):27–30.
Busfield BT, Glousman RE, McGarry MH, Tibone JE, Lee TQ. A biomechanical comparison of 2 technical variations of double-row rotator cuff fixation: the importance of medial row knots. Am J Sports Med. 2008;36(5):901–6.
Kaplan K, ElAttrache NS, Vazquez O, Chen YJ, Lee T. Knotless rotator cuff repair in an external rotation model: the importance of medial-row horizontal mattress sutures. Arthroscopy. 2011;27(4):471–8.
Tamboli M, Hwang J, McGarry MH, Kang Y, Lee TQ, Mihata T. Biomechanical characteristics of the horizontal mattress stitch: implication for double-row and suture-bridge rotator cuff repair. J Orthop Sci. 2014;19(2):235–41.
Nimura A, Kato A, Yamaguchi K, Mochizuki T, Okawa A, Sugaya H, et al. The superior capsule of the shoulder joint complements the insertion of the rotator cuff. J Shoulder Elb Surg. 2012;21(7):867–72.
Ishihara Y, Mihata T, Tamboli M, Nguyen L, Park KJ, McGarry MH, et al. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elb Surg. 2014;23(5):642–8.
Castagna A, Delle Rose G, Conti M, Snyder SJ, Borroni M, Garofalo R. Predictive factors of subtle residual shoulder symptoms after transtendinous arthroscopic cuff repair: a clinical study. Am J Sports Med. 2009;37(1):103–8.
Shin SJ. A comparison of 2 repair techniques for partial-thickness articular-sided rotator cuff tears. Arthroscopy. 2012;28(1):25–33.
Mihata T, McGarry MH, Ishihara Y, Bui CN, Alavekios D, Neo M, et al. Biomechanical analysis of articular-sided partial-thickness rotator cuff tear and repair. Am J Sports Med. 2015;43(2):439–46.
Novi M, Kumar A, Paladini P, Porcellini G, Merolla G. Irreparable rotator cuff tears: challenges and solutions. Orthop Res Rev. 2018;10:93–103.
Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29(3):459–70.
Hirahara AM, Adams CR. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4(6):e637–41.
Hartzler RU, Burkhart SS. Superior Capsular Reconstruction. Orthopedics. 2017;40(5):271–80.
Narvani AA, Consigliere P, Polyzois I, Sarkhel T, Gupta R, Levy O. The "pull-over" technique for arthroscopic superior capsular reconstruction. Arthrosc Tech. 2016;5(6):e1441–e7.
Petri M, Greenspoon JA, Millett PJ. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc Tech. 2015;4(6):e751–5.
Sutter EG, Godin JA, Garrigues GE. All-arthroscopic superior shoulder capsule reconstruction with partial rotator cuff repair. Orthopedics. 2017;40(4):e735–e8.
Dimock RAC, Malik S, Consigliere P, Imam MA, Narvani AA. Superior capsule reconstruction: what do we know? Arch Bone Jt Surg. 2019;7(1):3–11.
Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40(10):2248–55.
Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effect of thickness and tension of fascia Lata graft on Glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32(3):418–26.
Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44(6):1423–30.
Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: a biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105(2):257–63.
Gartsman GM, O'Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elb Surg. 2004;13(4):424–6.
MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomized controlled trial. J Bone Joint Surg Am. 2011;93(21):1953–60.
Tashjian RZ. AAOS clinical practice guideline: optimizing the management of rotator cuff problems. J Am Acad Orthop Surg. 2011;19(6):380–3.
Denard PJ, Bahney TJ, Kirby SB, Orfaly RM. Contact pressure and glenohumeral translation following subacromial decompression: how much is enough? Orthopedics. 2010;33(11):805.
Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effects of Acromioplasty on superior capsule reconstruction for irreparable supraspinatus tendon tears. Am J Sports Med. 2016;44(1):191–7.
Singh S, Reeves J, Langohr GDG, Johnson JA, Athwal GS. The effect of the subacromial balloon spacer on humeral head translation in the treatment of massive, irreparable rotator cuff tears: a biomechanical assessment. J Shoulder Elb Surg. 2019;28(10):1841–7.
Acknowledgments
Authors would like to express special thanks to Ms. Silvia Bassini for the pictures and graphic support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 ISAKOS
About this chapter
Cite this chapter
Dal Fabbro, G., Serra, M., Carbone, G., Grassi, A., Al-Khelaifi, K., Zaffagnini, S. (2021). Biomechanics of Rotator Cuff Injury and Repair. In: Koh, J., Zaffagnini, S., Kuroda, R., Longo, U.G., Amirouche, F. (eds) Orthopaedic Biomechanics in Sports Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-81549-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-81549-3_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81548-6
Online ISBN: 978-3-030-81549-3
eBook Packages: MedicineMedicine (R0)