Abstract
Sigmoid colostomy is performed for temporary or permanent fecal diversion in order to provide the most distal possible stoma. This chapter describes the creation of a sigmoid colostomy in its variations as to surgical access and the types of construction. The emphasis is on appropriate indications, the surgical strategies, and safe techniques to avoid complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Indications
-
A sigmoid colostomy as the sole procedure is performed for temporary or permanent fecal diversion when the stoma should be as distal as possible to minimize the impact on fluid balance.
-
Specific indications for sigmoid colostomy include obstructing rectal or anal cancer, severe pelvic floor dysfunction (fecal incontinence, fecal outlet obstruction), pelvic trauma, recto-urinary or rectovaginal fistulas, perianal or rectal Crohn disease, and congenital anomalies.
-
The laparoscopic approach is preferred in absence of contraindications as it allows the surgeon to readily mobilize the sigmoid to reach the abdominal wall, verify the correct orientation, or to use a different solution (transverse colostomy, ileostomy), should the sigmoid colon prove not be suited for diversion.
Contraindications
Sigmoid (as opposed to other locations):
-
Previously eliminated sigmoid loop (e.g., after rectosigmoid resection).
-
Acute or chronic pathology in the left lower quadrant.
-
Superobesity: a transverse colostomy may be more likely to reach to the skin without tension.
Laparoscopy:
-
Patients with severe cardiac and restrictive pulmonary disease for whom the carbon dioxide pneumoperitoneum and Trendelenburg position may impair the cardiac output or create intolerable acidosis.
-
Severe intraabdominal adhesions.
-
Bleeding disorders.
-
Pregnancy (the enlarged uterus can obstruct the view).
Preoperative Preparation
-
Study the patient’s history and verify the diagnosis and appropriate indication by clinical, radiographic, or endoscopic means.
-
Review preoperative images if available (CT scans, plain x-ray films, contrast enemas).
-
Mark the site for the stoma: this is mandatory for elective stoma creations.
-
Educate the patient about stoma function and lifestyle modifications.
-
Routine antibiotic prophylaxis (unless therapeutic indication for active infection).
Pitfalls and Danger Points
-
Poorly selected stoma location
-
Short sigmoid mesentery with risk for stoma retraction
-
Narrow fascial opening with risk of stoma necrosis or outlet obstruction
-
Wide fascial opening with risk of prolapse, or peristomal herniation
-
Obesity
-
Maturing the “wrong end” of the colon as a result of bowel orientation confusion
-
Ureteral injury
-
Previous surgeries and pathologies that limit the sigmoid colon mobility
Operative Strategy
Choice of Procedure and Site
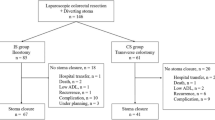
A sigmoid colostomy or a loop ileostomy is the preferred alternative to a transverse colostomy for the majority of elective situations. Under urgent/emergency circumstances, when a Hartmann type resection is performed, the creation of the end colostomy may follow similar principles except it is preceded by a bowel resection and/or damage control. In selecting the right location and type of stoma, it is important to consider all past, current, and future interventions that may interfere with the current creation or which may be handicapped by the new stoma.
Identification of an optimal stoma site will reduce local complications such as skin erosion, stoma trauma, and retraction. Use all positions (standing, supine, and sitting) to mark the stoma site. Ideally this should lie on a vertical line within the boundaries of the rectus muscle. Remember that in obese patients, a comparably much higher (cephalad) stoma site needs to be selected as the pannus may shift downward and bury a classical “left lower quadrant” location.
Creation of a loop colostomy may jeopardize the marginal artery blood flow and potentially devascularize the distal colon. This again is critical when considering a stoma proximal to a previous anastomosis.
Access
The segment of intestine chosen for the ostomy formation must reach to the skin without tension, and the mesentery must not be twisted during stoma formation. Even though the sigmoid can in some cases be directly pulled up through a small single-incision open approach (sometimes termed a “trephine” colostomy), that cannot be anticipated from outside. In fact not infrequently, the sigmoid is less mobile than one would expect, and the laparoscopic approach allows for safe mobilization under direct view to achieve adequate reach.
Type of Fecal Diversion
If the purpose of the colostomy is to decompress and vent a colon obstructed by anorectal pathology, a loop colostomy with equal weight openings for the afferent and efferent segment should be created. If the colon is empty but at risk for an obstruction, a small mucous fistula is sufficient to prevent a blowout of the segment distal to the stoma and proximal to the obstruction. If the goal of creating a colostomy is to achieve the most complete diversion of stool from a non-obstructed distal area (reconstruction, fistula, incontinence), the efferent limb can either be closed completely with a stapler or a Prasad-type pseudo-loop colostomy can be created. For the latter, the proximal end is brought out as a functional end colostomy, and a tiny edge of the distal stapler-transected end is either fixed to the afferent limb or brought out as a mini-mucous fistula in the same opening. This construction has the advantage over a true loop that it is less prone to hernia formation and prolapse (but it will require a resection and anastomosis for closure).
Documentation Basics
Coding for surgical procedures is complex. Consult the most recent edition of the AMA’s Current Procedural Terminology book for details (see references at the end). In general, it is important to document:
-
Findings and indication for diversion.
-
Reasoning for choice of type and site.
-
Construction details: loop, Prasad-type, end, Hartmann type.
-
Tacking (or absence) of colon to fascia.
-
Use of stoma bridge.
-
Use of abdominal wall reinforcement.
-
It is important to document technical details when fashioning any type of stoma. This will facilitate the reversal of a temporary stoma.
Operative Technique
When constructing a sigmoid colostomy of any type, place the patient in a modified lithotomy and moderate Trendelenburg position with both arms tucked. Assure ready access to the rectum and have a rigid or flexible sigmoidoscope available.
Incision, Identification, and Mobilization of the Sigmoid Colon
Open—Through Laparotomy
A standard laparotomy allows you to perform a controlled lysis of adhesions, release attachments, and positively identify and mobilize the target segment (as if a resection were to be performed). Once you have verified that it will reach your stoma marking, you can proceed with creating the gap at the colostomy site. This is done in the same fashion as described in the next paragraph, but with the luxury of access from inside as well.
Open—Through Colostomy Site Only
Make a circular incision at the stoma site marking. To make a perfect circle, use the plunger handle of a 60 cc syringe to make an impression on the skin. When no previous laparotomy has been performed, it may—depending on the body habitus—be easy to find the sigmoid colon using this incision. Incise the subcutaneous fat down to the level of the anterior rectus fascia without creating dead space. Make a cruciate incision of 2–4 cm long in either direction on the anterior rectus fascia with electrocautery. Expose the rectus muscle and spread its fibers all the way to the posterior rectus sheath by inserting and opening a clamp, followed by the retractors. Avoid injury to the inferior epigastric vessels; otherwise, suture-ligate them. Enter the abdomen by incising the posterior rectus sheath and peritoneum. This is the colostomy “trephine,” which should be wide enough to accommodate at least 2 fingerbreadths. Feel for adhesions between the anterior abdominal wall and abdominal contents by sweeping the index finger through the incision. If necessary, take them down in a controlled fashion.
Key landmarks to identify the sigmoid colon are the tenia and the epiploic appendages. After entering the peritoneal cavity, push the omentum and hence the transverse colon cephalad from the operative field with a sponge-on-a-stick. Identify the sigmoid colon and gently deliver it through the trephine using a Babcock clamp. Identify the margin of the colon with its mesocolon and open a small defect with electrocautery. Use a tonsil clamp to dissect through the mesocolon and complete a window. Bring a red Robinson or a Penrose drain through the defect and use this as a temporary bridge for the colostomy.
Laparoscopic
As with all laparoscopic procedures, the surgeon, target area, and primary video monitor should all be in one line (Fig. 66.1). The surgeon stands at the right side; the monitor hence will be on left side at the level of the patient’s hip/knee. Access and creation of the pneumoperitoneum are done using an appropriate and safe standard approach starting at the umbilicus: (1) open cut-down (Hasson technique) or (2) Veress needle technique with optical trocar insertion. Two additional ports are inserted under visual control with one in the right lower quadrant and one through the planned stoma site (Fig. 66.2) .

Fig. 66.1

Fig. 66.2
Alternatively, you can create the trephine first (as described in the previous section) and insert a mini-gel port with trocar. Two additional trocars are placed under visual control at the umbilicus and the right lower quadrant.
Quickly examine the entire abdomen; then place the patient in Trendelenburg position with left side up 30° to move the small bowel out of the pelvis and expose the sigmoid colon.
Grasp the sigmoid colon with a Babcock clamp through the stoma site trocar (Fig. 66.3). Draw it toward the trocar. If it does not easily reach the anterior abdominal wall, mobilize the sigmoid by freeing up adhesions and releasing the lateral peritoneal attachments (using cautery or an energy device) (Fig. 66.4). Dissect from the inferior lateral part of the sigmoid up to the splenic flexure until there is sufficient mobility for a tension-free colostomy. Create a small window in the mesocolon and slide in a small Penrose drain. Loop it and secure it with a locking laparoscopic grasper. Clearly mark afferent versus efferent limb in any absolute fashion of your preference. For example, place two marking clips proximal and one clip distal to the gap in the mesocolon.

Fig. 66.3

Fig. 66.4
If a Hartmann type colostomy is planned, the bowel can be divided intracorporeally with a laparoscopic stapler (Fig. 66.5). You may have to divide the mesentery a bit more to allow for good mobility. Secure the proximal bowel with a locking atraumatic grasper.

Fig. 66.5
Remove the trocar at the stoma site and create the trephine as described in the previous section. Pause and deflate the pneumoperitoneum. Pull the Penrose drain with the bowel loop up. Reinsufflate the abdomen to confirm the reach, correct position, and rotation of the loop and to verify hemostasis.
Stoma Orientation
If a loop colostomy is created, there is no special need to orient the bowel—as long as it is not unduly twisted. Otherwise and if it was not possible to mark and orient the bowel internally, you must correctly identify afferent versus efferent limb. Gently lift the exteriorized bowel with the Penrose drain. Clamp off the bowel lumen with one click of a non-crushing bowel clamp. Inflate the rectum with a rigid or flexible sigmoidoscope. The distal (efferent) sigmoid loop will inflate. Mark it with a Vicryl suture. Remove the bowel clamp.
Abdominal Wall Reinforcement (Hernia Prevention)
Parastomal hernia formation is inevitable if the stoma remains in place long enough. If the stoma is planned for more than just a short period of time, it may be worthwhile to reinforce the abdominal wall with a biological implant (collagen sheath). Before pulling through the bowel, you may place a rectangular piece with a central cruciate incision anterior to the posterior rectus sheath (behind the rectus muscle). Secure it to that fascia with a few interrupted stitches.
Choice of Bridge
Depending on the patient’s body habitus, a stoma bridge may not always be necessary for a loop sigmoid colostomy. But in many instances, the bridge helps to prevent the bowel from retracting (Fig. 66.6). Analyze your options for the definitive stoma bridge: premanufactured plastic bridges versus large catheter (24 F). The plastic bridges or rods sit on top of the skin where they are fixed with anchoring stitches. They are easy to do and strong, but routinely make it difficult to fit an ostomy bag. A catheter-based bridge can be sutured on the cephalad and caudad end to the dermis, which makes it easier to fit the appliance all the way to the mucocutaneous junction. Once you decide which approach to use, grab the end of that bridge with the temporary bridge clamp and pull/slide it to the other side.

Fig. 66.6
Maturation of Colostomy
Using 2–0 or 3–0 atraumatic Vicryl sutures, circumferentially attach the abdominal wall structures to the colon to prevent spillage of stool into the peritoneal cavity once it is opened. Start in a deeper layer with the rectus sheath, followed by a more superficial layer of dermis to the colon serosa. Tacking the stoma to the abdominal wall does not really increase the difficulty of mobilization during a subsequent closure of the colostomy. If additional incisions (laparoscopy or midline) are present, close these in standard fashion before maturing the stoma.
Loop Colostomy
Make a small colotomy with the scissors and allow the gases to escape. Do not use electrocautery to avoid triggering an explosion of combustive bowel gases. After the initial venting, you can use cautery to extend the incision. Both directions (longitudinal or perpendicular to the bowel axis) have been used. For the former, create a 5- to 6-cm longitudinal incision along the anterior wall of the colon, preferably in the tenia. For the latter, open roughly two thirds of the bowel circumference. Then evert in either case the bowel wall and mature it with interrupted 3–0 PG sutures to the subcuticular layer of the skin (Fig. 66.6). Avoid placing sutures through the skin, as to avoid stich abscesses or granulomas.
Prasad-Type Colostomy
In some cases where relative certainty about fecal diversion with minimized risk of stool overflow is desired, you may choose to fashion a pseudo-loop Prasad-type end colo-colostomy. The proximal and distal side have been closed with a linear-cutting stapler (transection only or with resection). Verify the correct bowel orientation for the proximal and distal stapled ends as there is no room for error. Bring the full diameter of the proximal bowel and the antimesenteric stapled corner of the distal bowel out of the same trephine (described in a previous section). Using with 3–0 PG sutures, tack both the proximal bowel and the distal bowel edge in two layers to (a) the posterior rectus sheath/peritoneum and (b) the dermis. The distal end can either be left closed at the skin edge (pseudo-mucous fistula), or a 2–3 mm opening is created and matured. Once all other incisions are closed, remove the entire staple line of the proximal bowel. Suture the full thickness of the bowel to the subcuticular layer of the skin using 3–0 PG sutures to mature the proximal stoma (Fig. 66.7). If an aperture is created in the distal bowel, place full-thickness sutures between the proximal and the distal apposed bowel walls. Document in detail the technique used to fashion the stoma in the operative note. This is to avoid confusion when the stoma is reversed.

Fig. 66.7
End Colostomy
The process is exactly the same as in the previous section except that there is either no distal segment or it is left a blind stump in the abdomen.
Postoperative Care
-
In the operating room, apply an adhesive-type transparent colostomy bag.
-
Antibiotics: Routine coverage for the perioperative 24-hour period. In case of an underlying infection/sepsis, continue respective therapeutic antibiotics for that indication.
-
Intravenous fluids: Maintain adequate fluid until return of bowel function.
-
Diet: Start diet as tolerated.
-
Stoma: Start early stoma teaching to avoid delaying discharge. Leave the bridge in place between 2 and 3 weeks to allow for good healing between the bowel and the abdominal wall.
Complications
-
Peristomal abscess and sepsis is rare. Treatment requires incision and drainage either into the stoma bag or far enough to be outside the waver of the appliance. Massive sepsis may require stoma relocation.
-
Stoma necrosis or retraction, particularly in very obese patients: If the stoma appears dusky or dark, evaluate it by inspecting the mucosa above and below the fascia. If the viability is compromised below the fascia, the stoma needs to be revised immediately. If it only affects the bowel part above the fascia, it will likely stricture; timing of a stoma revision versus takedown can be individualized.
-
Prolapse of both the defunctionalized or the active limb is fairly common in a loop colostomy. It is best managed by restoring intestinal continuity including removal of the original site of obstruction; alternatively, it can be converted into an end or Prasad-type colostomy.
-
Parastomal hernias: The rule rather than the exception.
-
Skin dermatitis from intestinal content leakage.
Further Reading
American Medical Association. Current procedural terminology: CPT ®. Professional ed. Chicago: American Medical Association; 2022. https://www.ama-assn.org/practice-management/cpt.
Cataldo PA. Technical tips for stoma creation in the challenging patient. Clin Colon Rectal Surg. 2008;21:17–22.
Corman ML. Intestinal stomas. In: Corman ML, editor. Bergamaschi RCM, Nicholls RJ, Fazio VW, (Assoc Eds) Corman’s colon and Rectal surgery. sixth ed. Philadelphiaffig: Lippincott Williams & Wilkins; 2012. p. 1396–450.
Kaiser AM. McGraw-Hill Manual Colorectal Surgery. Access Surgery; 2009. Retrieved November 14, 2022, from https://accesssurgery.mhmedical.com/book.aspx?bookID=425.
McGee MF, Cataldo PA. Chapter 55: intestinal stomas. In: Steele SR, Hull TL, Read TR, Saclarides TJ, Senagore AJ, Whitlow CB, editors. The ASCRS textbook of colon and rectal surgery. 3rd ed. New York: Springer; 2016. p. 971–1013.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Spanos, C.P., Kaiser, A.M. (2022). Laparoscopic Versus Open Creation of Sigmoid Colostomy (Loop, Prasad-Type, End). In: Scott-Conner, C.E.H., Kaiser, A.M., Nguyen, N.T., Sarpel, U., Sugg, S.L. (eds) Chassin's Operative Strategy in General Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-81415-1_66
Download citation
DOI: https://doi.org/10.1007/978-3-030-81415-1_66
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81414-4
Online ISBN: 978-3-030-81415-1
eBook Packages: MedicineMedicine (R0)