Abstract
Neoadjuvant immune checkpoint inhibition therapy has significantly advanced the management of patients with muscle-invasive bladder cancer. However, response rates to neoadjuvant immune checkpoint inhibition therapy are similar to platinum-based neoadjuvant chemotherapy (NAC), suggesting intrinsic tumor biology plays an important role in treatment response. To improve patient selection to neoadjuvant checkpoint inhibitor therapy, molecular profiling of primary and treated tumor tissue becomes essential. With this knowledge, biomarker development is facilitated, as is our understanding of the mechanisms of tumor resistance to immune therapy. While there are numerous ongoing clinical trials in the neoadjuvant setting, in this chapter we focus on four, including ABACUS (atezolizumab), PURE-01 (pembrolizumab), NABUCCO (ipilimumab with nivolumab), and MDACC (durvalumab with tremelimumab). For each study, we evaluate the use of immunohistochemistry, RNA gene expression, and DNA sequencing as candidate biomarkers for predicting response. Finally, we draw parallels from profiles collected post-therapy tumor tissues for each study, providing key insights on how the tumor landscape is impacted by immune therapy-based systemic treatment regimens.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Muscle-invasive bladder cancer
- Neoadjuvant immune therapy
- Clinical trials
- Immunohistochemistry
- RNA expression
- Molecular subtypes
- DNA sequencing
- Biomarkers
Introduction
Muscle-invasive bladder cancer (MIBC) is an aggressive disease with limited treatment options. For the approximate 25–30% of patients who present with MIBC, the recommended treatment option is neoadjuvant cisplatin-based chemotherapy (NAC) followed by pelvic lymph node dissection and removal of the bladder (radical cystectomy; RC) [1, 2]. Despite this aggressive treatment regimen, the 5-year overall survival rate is only approximately 55% from the time of surgery, highlighting an unmet clinical need for better patient stratification and improved therapeutic intervention [3]. Patients who are ineligible for NAC are recommended to proceed to immediate cystectomy [4], where the outcomes for these patients are poor [1, 5]. For these reasons, there is a significant unmet need for improved patient stratification and additional treatment options for both cisplatin-eligible and cisplatin-ineligible patients.
Immune checkpoint blockade (ICB) has emerged as a promising therapy for metastatic urothelial carcinoma, with several checkpoint inhibitor drugs been approved in the second-line setting for patients who have progressed with cisplatin-based chemotherapy [6,7,8,9,10]. The application of IBC in earlier disease stages is also being investigated, with atezolizumab and pembrolizumab having received approval for use in the first-line setting for patients who are cisplatin ineligible and are PD-L1 positive [11]. The higher mutational rates in primary bladder cancer tumors [12, 13], coupled with significant immune infiltration levels [14, 15], make checkpoint inhibitors a rational and attractive avenue of neoadjuvant therapy.
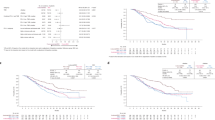
There are numerous ongoing clinical trials evaluating the use of checkpoint inhibitors in the neoadjuvant setting (Fig. 4.1). These clinical trials have showed pathological response rates comparable to platinum-based chemotherapy ranging between 31% and 46% [16,17,18,19,20,21,22,23]. Unfortunately, these lower positive responses mean most patients are not receiving benefit from neoadjuvant checkpoint therapy, further emphasizing the need to improve our understanding of the mechanisms driving treatment response. Moreover, treatment decisions are becoming increasingly complex as novel immune and targeted therapies are developed and approved, where they provide compelling alternatives to current standard of care therapies, such as chemotherapy, radiation therapy, and radical cystectomy. With these challenges in mind, the development and application of biomarkers will be instrumental to improving patient selection, ultimately driving immune therapy toward standard of care.
Unfortunately, many of the clinical trials to date have limited biomarker-associated data or the data is generated using inconsistent methodologies, making a direct comparison between trials challenging. The data available for post-treatment radical cystectomy specimens is also limited, leaving a rather large knowledge gap around the impact of immune therapy on tumor biology and resistance mechanisms. One advantage of the neoadjuvant setting is access to untreated primary tumor tissue, which can facilitate biomarker discovery for key endpoints including pathological response and patient outcomes [24]. Moreover, access to matched patient tumor tissue post-treatment can provide key data to facilitate the characterization of resistance mechanisms. Finally, detailed characterization of post-treatment tissues can provide a foundation to begin to inform adjuvant treatment decisions. Although studies comparing tumor tissue pre- and post-treatment are limited, the available data is intriguing, with the emerging trends for each of these trials providing key insights into neoadjuvant checkpoint therapy.
In this chapter, we discuss the molecular characterization of MIBC tumors treated with systemic IBC, focusing on biomarker discovery opportunities where tumor tissue was profiled before and after therapy. We will focus our discussion on four major clinical trials including ABACUS (atezolizumab), PURE-01 (pembrolizumab), NABUCCO (ipilimumab), and MDACC (neoadjuvant durvalumab plus tremelimumab) [16,17,18,19], illustrating the similarities from the perspective of biomarkers in MIBC.
The ABACUS Trial: Neoadjuvant Atezolizumab
The ABACUS trial is a single-arm, phase 2 study that investigated the use of two cycles of neoadjuvant atezolizumab (anti-PD-L1) for operable MIBC (cT2-4aN0M0), including patients who were ineligible for cisplatin-based chemotherapy [19]. Of the 95 patients recruited, 88 were assessable for the primary endpoint which was complete pathological response at radical cystectomy surgery. With 27 out of 88 patients (31%) achieving a complete pathological response, the trial met the primary endpoint and showed a 1-year relapse-free survival of 79%, with a median follow-up of 13.1 months. For this study, tumor tissue was profiled from untreated TURBT samples and matched post-atezolizumab radical cystectomy samples (ClinicalTrials.gov Identifier: NCT02662309).
Immunohistochemistry
Baseline PD-L1 positivity was assessed on immunohistochemistry (IHC) , using SP142 assay at the ≥5% immune cell staining threshold. For pretreated tumor tissue, PD-L1 staining intensity (immune cells or tumor) was not significantly correlated with outcome, suggesting initial immune infiltration of primary tumor tissue does not predict long-term therapeutic benefit. However, PanCK-CD8 IHC analysis revealed that high baseline presence of intraepithelial CD8+ cells was significantly associated with a complete pathologic response rate of 40%. High levels of immune infiltration appeared to facilitate regression at the primary tumor site, resulting in effective local control as measured by pathological response, but these correlates may be less meaningful for predicting the metastatic potential and ultimately patient outcome.
The PanCK-CD8 scoring method allowed for a granular assessment of the immune infiltration in the pretreatment tumor tissue, resulting in the classification of the ABACUS tumors into three distinct CD8+ immune phenotypes, including desert, excluded, and inflamed [25]. The desert phenotype indicates little to no immune staining positivity, coupled with resistance to atezolizumab. The excluded phenotype is characterized by stromal infiltration, where immune cells accumulate on the tumor periphery but have not penetrated the tumor tissue. Finally, the inflamed phenotype indicates a high level of immune infiltration within the tumor tissue. In the metastatic MIBC setting, earlier studies have reported the inflamed phenotype was associated with response to atezolizumab [25]. The ABACUS study, despite a high occurrence of inflamed tumors, did not report an improved response rate for this phenotype. However, dual CD8 and granzyme B (GZMB) staining was positively associated with response, suggesting the quality of the immune infiltration, beyond CD8 expression, is relevant when determining outcomes within the inflamed immune phenotype. A correlation with response was not seen for the excluded or desert immune phenotypes.
Comparing TURBT tissue to treated RC tissue, significantly increased levels of CD8, PD-L1, and FAP were observed, indicating increased immune activity in the treated tumor tissue. Moreover, dynamic changes to the immune phenotypes occurred with therapy, with five patients changing from excluded to inflamed and four from an inflamed to excluded phenotype.
RNA-Based Molecular Biomarkers
The ABACUS study also conducted RNA-seq gene expression analysis to explore several response categories. Global gene expression patterns were compared before and after treatment in patients with stable disease, finding higher immune signature scores and immune gene expression in posttreated tissues. These data were consistent with the IHC results, where increased staining for immune markers was observed post-therapy. The RNA-seq expression data was also analyzed in the context of a predefined eight-gene (IFNG, CXCL9, CD8A, GZMA, GZMB, CXCL10, PRF1, and TBX21) cytotoxic T-cell transcriptional signature (tGE8), revealing a significant increase in signature scores for responders, compared to patients with stable disease and/or relapse. As with the IHC data, higher levels of immune infiltration in pretreated tissue quantified by RNA-based immune gene signatures correlated with response to atezolizumab.
With respect to RNA-based molecular subtyping, the ABACUS study used the 2012 Lund taxonomy to classify the pre- and post-tumors into five molecular subtypes UroA, GU, Inf, UroB, and SCCL [26]. While in the metastatic setting the Lund subtypes were found to correlate with outcome after treatment with atezolizumab, this was not the case in the neoadjuvant setting pretreatment [19]. After treatment, the majority (14/15, 93%) of responding tumors were classified as the “infiltrated” molecular subtype. Importantly, treated tumors classified as infiltrated had increased levels of angiogenesis, stromal and immune infiltration, and with decreased cellular proliferation [19]. These expression-based patterns may potentially reflect reorganization of the tumor microenvironment, as responding tumors also showed upregulation of extracellular matrix and collagen formation signatures. It is tempting to speculate these features reflect tumor “scarring” or wound healing, a concept which will be explored in detail in the PURE-01 study section (1.3). Importantly, higher angiogenesis signature scores suggest anti-angiogenesis drugs (VEGFR inhibitors) may be a promising candidate for the adjuvant treatment post-atezolizumab.
DNA-Based Molecular Biomarkers
Biomarkers, including tumor mutational burden (TMB) and DNA damage repair (DDR) gene alterations, have previously been reported to correlate with outcomes in the metastatic setting of bladder cancer [27]. However, in the ABACUS study, associations with pathologic response were not observed for neoadjuvant atezolizumab [19]. Exploratory analyses found that responding tumors had increased DNA amplification levels for the 11q13.3 locus, which includes the FGFR3, FGF19, and CCND1 genes. With the recent approval of fibroblast growth factor (FGF)-targeted therapy for bladder cancer, these results may imply the justification for future trials combining atezolizumab with additional targeted therapy [28]. However, FGF pathway activity has not been consistently linked to increased response rates with checkpoint inhibitors, as discussed below.
When comparing TMB and DNA mutations pre- and post-atezolizumab, consistent DNA alterations were not revealed, suggesting an absence of clonal evolution within the relatively short time span of neoadjuvant atezolizumab therapy. This contrasts with data from the neoadjuvant chemotherapy setting, where pressure from platinum-based therapy induced rapid clonal evolution [29]. Considering these results together, the data from the ABACUS study suggest that entire populations of tumor subclones are eliminated with therapy, while with chemotherapy, additional mutations are induced, facilitating a rapid tumor evolution and the emergence of new dominant subclones. However, the time frames between each treatment differ greatly, with 5.6 weeks between atezolizumab and surgery compared to the approximate 12 weeks required to complete chemotherapy. There may be insufficient time to account for all but the most aggressive tumor regrowth in the former time span.
Integrating Biomarkers to Refine the Molecular Diagnosis in the ABACUS Study
In the metastatic MIBC setting, biomarkers like TMB, DDR gene alterations, and PD-L1 staining have all shown promising utility for predicting benefit from atezolizumab [27]. However, these biomarkers did not correlate with treatment response in the context of neoadjuvant atezolizumab in the ABACUS study [19]. Nonetheless, preliminary biomarker data suggests that quantifying preexisting immune infiltration, using either RNA-based signatures or IHC staining, holds promise for predicting pathological response after neoadjuvant checkpoint inhibition with atezolizumab. However, simply quantifying the levels of immune infiltrates may be insufficient, as the type or quality of immune infiltrate may improve response prediction even further, particularly for the inflamed phenotype, suggesting an important avenue of biomarker discovery. Notably, when comparing pre- and post-atezolizumab tumor tissues, an increase in angiogenesis and stromal gene expression for responding tumors was revealed, suggesting a scarring or wound-healing phenotype in a significant proportion of cases, which has significant implications for targeted adjuvant therapies. Taken together, future standardization for the application of these promising biomarkers is warranted, in order to validate them as response predictors in the context of neoadjuvant anti-PD-L1 treatment.
The PURE-01 Trial: Neoadjuvant Pembrolizumab
In the PURE-01 trial (single arm, phase 2), 143 cisplatin-eligible MIBC patients (cT2-T4aN0M0) were enrolled and treated with 3 cycles of neoadjuvant pembrolizumab (anti-PD-1) [30, 31]. Of the 143 treated patients, 55 (38.5%) showed a complete pathologic response (ypT0N0) at radical cystectomy. The median follow-up of 23 months, corresponded with 12- and 24-month event-free survival rates of 84.5% and 71.7%, respectively [30] (ClinicalTrials.gov Identifier: NCT02736266).
Immunohistochemistry
PD-L1 positivity was determined by IHC using the 22C3 assay and the combined positive score (CPS), defined as the percentage (≥10%) of PD-L1-expressing tumor and infiltrating immune cells relative to the total number of tumor cells. Within the PURE-01 cohort, PD-L1 positivity was significantly associated with complete pathologic response at radical cystectomy [31], which directly contrasts the ABACUS data. However, while both studies investigate neoadjuvant checkpoint inhibitors, there are numerous differences which confound direct comparisons, including differences in the assay (SP142 vs 22C3), treatment (anti-PD-L1 vs anti-PD-1) or patient inclusion (cisplatin ineligible vs eligible). Notably, CD8 IHC analysis for matched pre- and post-pembrolizumab samples in PURE-01 revealed an increase of CD8+ cells infiltrating the tumor stroma, consistent with observations from the ABACUS study where a 78% increase in median values for intraepithelial CD8 expression was noted. However, unlike ABACUS, PURE-01 did not report an association of pretreatment CD8 IHC positivity with pathologic response.
RNA-Based Molecular Biomarkers
In the PURE-01 study, gene expression data was analyzed for 84 TURBT specimens collected pre-therapy using whole-transcriptome microarrays [18]. Molecular subtyping was used to classify the PURE-01 cohort into subtypes according to the consensus, TCGA and GSC (genomic subtyping classifier) models, with the latter consisting of a luminal, luminal-infiltrated, basal, claudin-low, and neuroendocrine-like molecular subtypes [32, 33]. Pathological response to pembrolizumab was not significantly associated with molecular subtypes, which was consistent with previous studies for atezolizumab and NAC, where molecular subtypes did not predict response [19, 33]. Notably, basal-like tumors did have favorable response rates averaging around 65%, differing slightly with each subtyping model. Downstaging was observed for 17/26 (65.4%) for both the TCGA and consensus basal squamous subtypes and for 7/11 (63.3%) for the GSC claudin-low subtype [18]. The basal squamous and claudin-low subtypes differ in that the basal squamous encompasses all basal tumors, regardless of immune or stromal infiltration, while the claudin-low are more restrictive, encompassing basal tumors with higher immune infiltration and activity.
Integrating immune-associated IHC data with the molecular subtypes revealed that PD-L1 combined positive score on IHC was higher for basal-type tumors compared to the other subtypes. These data were consistent with immune gene signatures, including the generalized immune190 signature, which also showed higher scores for basal-type tumors. Moreover, basal-type tumors had higher gene expression for select immune-associated genes, including CD274, PDCD1, and CD8A. The immune190 signature and three additional immune hallmark signatures, IFNγ, IFNα, and inflammatory response, were all significantly associated with pathological complete response after receipt of pembrolizumab. These data are in alignment with the observations from the ABACUS trial, which found that preexisting immune infiltrates were key for predicting response to therapy.
There were several notable associations of molecular subtypes and immune gene signatures with patient outcome in PURE-01. In the first gene expression profiling study for PURE-01, the GSC claudin-low subtype had exceptional recurrence-free survival, with 0/11 events in 24 months [18]. In contrast, with NAC, the claudin-low patients had high rates of disease progression, suggesting neoadjuvant pembrolizumab is a highly favorable treatment option for these patients. When additional outcome data became available, the event-free survival rates remained extremely favorable, with only a single event in 14 patients over 24 months [30]. The basal-type tumors from the TCGA and consensus model were not significant for either RFS or EFS, in the initial or expanded study, respectively. However, when the basal-type tumors were subset according to the median immune190 signature scores, a significant association with RFS was identified [18]. These data suggest that immune infiltration and intrinsic subtype may both play a role in predicting long-term benefit from pembrolizumab.
The PURE-01 study also profiled 26 radical cystectomy samples collected post-pembrolizumab [34]. These samples were compared to a cohort of post-chemotherapy radical cystectomy samples (n = 133) and to a cohort of radical cystectomy samples without systemic therapy (n = 94). The gene expression profiles for these samples had several consistencies with each other but also with the ABACUS study. First, in all three cohorts, regardless of systemic therapy, there were numerous cases classified as stroma-rich by the consensus model [15]. As this subtype is defined by high stromal and immune cell infiltration, these data have interesting parallels to the enrichment for the “infiltrated” subtype in the post-atezolizumab RC samples from the ABACUS study. The PURE-01 RC study defined these tumors as “scar-like,” represented by high stromal marker expression, higher angiogenesis activity, and lower levels of proliferation, which is directly in alignment with the reports from ABACUS. Second, after NAC or surgery alone, there was a good representation of basal and luminal tumors, which contrasted with the post-pembrolizumab subtypes. In PURE-01, there was a poor representation of basal-type tumors (4/26) compared to luminal tumors (9/26). Moreover, the scar-like tumors post-pembrolizumab also showed expression of many luminal markers, differing from the other two cohorts. Given luminal tumors tend to be immune desert phenotype, it is tempting to speculate that the resistant tumors collected post-pembrolizumab represent an intrinsic resistance mechanism of luminal tumors, represented by a higher ratio of luminal tumors post-pembrolizumab. However, the sample sizes in the PURE-01 study are small, so these observations require further data to corroborate this hypothesis.
DNA-Based Molecular Biomarkers
The interim study results for PURE-01 reported that patients with higher tumor mutational burden (TMB) had a significant pathologic response to pembrolizumab [JCO ref]. As additional study data became available, however, follow-up reports found TMB was neither significantly associated with complete response (p = 0.06) [18] nor did TMB appear to significantly predict event-free survival outcomes on multivariable analyses (p = 0.2) [30].
The PURE-01 study also investigated the mutational status in the exons of 395 cancer-associated genes and select introns from 31 genes that are frequently rearranged in cancer. Of these, only PBRM1 mutations were found to have a significant association with complete response, although this was no longer significant after multiple hypothesis testing. Furthermore, the observed associations between DDR and RB1 gene alterations were weakened after multivariable adjustments for TMB. These data suggest that mutational status at either the individual gene level or whole genome level is not a significant predictor of response to pembrolizumab.
The ABACUS study found that several genes involved in the fibroblast growth factor (FGF) pathway were amplified in responding tumors [19]. Interestingly, increased FGF pathway activity tends to be associated with tumors of the luminal subtype, which are also typically immune-depleted [13, 15, 33] and therefore would not be predicted to have good response to therapy [10]. To attempt to reconcile these discrepancies, multiple fibroblast growth factor receptor-3 (FGFR3) genomic alterations (GA) were investigated as candidates for predicting response to pembrolizumab in PURE-01 [35]. In this study, FGFR3 mutations, gene expression, and pathway activity were all investigated. In addition, using a molecular signature based on long noncoding RNA expression, a subgroup of luminal tumors with excellent prognosis and amplified FGFR3 activity was identified and evaluated. Only higher FGFR3 gene expression was found to have a significant association with lower rates of complete response, but this is likely balanced by multiple clinical and biological factors. Further study is warranted, and until such time, it was not recommended to exclude patients with FGFR3-altered tumors from neoadjuvant immune checkpoint therapy.
Integrating Biomarkers to Refine the Molecular Diagnosis in the PURE-01 Study
The PURE-01 study was an important clinical trial moving pembrolizumab into the cisplatin-eligible neoadjuvant MIBC setting. As was observed with the ABACUS study, preexisting immune infiltration was a significant predictor of response to therapy, indicating immune infiltration is a common link to predict responses to atezolizumab or pembrolizumab. However, the nature of the intrinsic subtype may also be relevant as claudin-low tumors had exceptional outcomes with pembrolizumab. Splitting basal-like tumors by immune190 signature scores revealed similar outcomes, indicating basal features with high immune infiltration may have the most favorable response to pembrolizumab. Comparatively, traditional biomarkers used to predict response to immune therapy, such as TMB and PD-L1 IHC, were significantly associated with pathological response but not with outcome. These data would suggest that local control of the primary tumor may be informed using these tools, but more advanced RNA-based signatures would be preferred for predicting long-term benefit. Finally, the prevalence of luminal and scar-like tumors expressing luminal makers in the PURE-01 radical cystectomy cases suggests that luminal tumors may have an intrinsic resistance to pembrolizumab or that clones of the luminal subtype may be selected for during therapy.
The NABUCCO Trial: Neoadjuvant Ipilimumab with Nivolumab
The NABUCCO study evaluated a combination of two immune checkpoint inhibitors, ipilimumab (anti-CTLA4) and nivolumab (anti-PD1), in the neoadjuvant setting [16]. The study endpoint was the feasibility to resect within 12 weeks from initiation of treatment. This study was a single-arm, phase 1 feasibility trial including 24 patients with locoregionally advanced (cT2-4aN0-3M0) urothelial carcinoma. With all patients in the NABUCCO trial undergoing surgical resection, 23/24 patients received surgery within 12 weeks, therefore meeting the primary endpoint of the study. Of the 24 included patients, 11 (46%) had a pathological complete response, and 14 (58%) had no remaining invasive disease (pT0N0 or pTisN0/pTaN0). The median postoperative follow-up was 8.3 months (ClinicalTrials.gov Identifier: NCT03387761).
Immunohistochemistry
Like the PURE-01 study, baseline PD-L1 IHC was performed using the 22C3 assay and the combined positive score (CPS). The pathological complete response rate was higher (73%) for PD-L1-positive tumors compared to PD-L1-negative tumors (33%), but this was not significant (p = 0.15). Quantitative multiplex immunofluorescence was used to analyze correlations between baseline CD8+ T-cell density and treatment response, as was done in the ABACUS trial. There was no correlation with combination anti-PD1 and anti-CTLA4 immunotherapy, suggesting this regimen has the potential to induce pathologic response, irrespective of preexisting CD8 levels. Multiplex immunofluorescence was also used to establish CD20+ B-cell counts, revealing stromal B-cell counts were significantly increased in nonresponding tumors compared to responding tumors. Of note, the presence of increased B cells in nonresponders was irrespective of preexisting CD8+ T-cell immunity. Finally, multiplex immunofluorescence was also used to quantify the dynamics of tertiary lymphoid structures (TLS). Although baseline TLS was not associated with treatment response, comparison of pre- and post-therapy tissue specimens did show an enrichment in TLS among tumors that responded to therapy. Further analysis of the TLS dynamics indicated that regulatory T cells were reduced in TLS upon treatment. Since TLS are ectopic lymphoid formations generally found in inflamed, infected, or tumoral tissues [36], these findings could potentially be in alignment with the scarring phenotypes observed on post-therapy specimens from the PURE-01 and ABACUS studies.
RNA-Based Molecular Biomarkers
Preexisting immunity was also assessed by transcriptomic signatures that also had been shown to have potential utility within the PURE-01 and ABACUS studies. However, neither the baseline IFN-γ, tumor inflammation, nor CD8+ T-cell effector (tGE8) signatures were associated with a complete response, in contrast to the observations from the ABACUS trial. Notably, the use of different immunotherapy drugs, differences in patient populations, and a lack of standardized biomarker platforms may contribute to these inconsistencies. Notably, a TGF-β gene expression signature was found to be associated with nonresponse to ipilimumab/nivolumab, which aligned with the proposed mechanism of resistance in the ABACUS study, where TGF-β-mediated T-cell inhibition was suggested to drive the immune excluded phenotype, which is resistant to atezolizumab [19]. Finally, hierarchical clustering analyses of differentially expressed genes between responders and nonresponders revealed an upregulation for the expression of B-cell-related genes in patients with tumors that did not respond. Of note, expression of these “B-cell genes” positively correlated with B-cell counts on immunofluorescence, confirming the results of the differential gene expression analyses.
DNA-Based Molecular Biomarkers
Despite the small sample size of the NABUCCO trial, tumors achieving complete pathologic response had slightly higher levels of TMB on pretreatment tissue specimen, but this was not a significant difference (p = 0.056). Further analysis of mutations in a set of DDR genes revealed alterations in these genes were more frequently observed for responding tumors. As was observed for the PURE-01 trial, TMB and DDR gene alterations seem to represent promising biomarkers, based on these initial reports. However, thresholds for “high” TMB and DDR are not yet standardized. Importantly, these initial findings warrant further evaluation within an additional representative cohort, should any clinical utility be confirmed.
Integrating Biomarkers to Refine the Molecular Diagnosis in the NAMBUCCO Study
The NAMBUCCO study investigates the addition of anti-CTLA-4 to PD-1 blockade in the neoadjuvant setting for locoregionally advanced MIBC. Unlike the ABACUS and PURE-01, preexisting immune infiltration was not correlated with response. As this is a feasibility study, an expanded trial will be important in better understanding the underlying biology driving response to this combination therapy.
Neoadjuvant Durvalumab with Tremelimumab (MDACC)
The University of Texas MD Anderson Cancer Center (MDACC) initiated the first pilot combination trial of neoadjuvant durvalumab (anti-PD-L1) plus tremelimumab (anti-CTLA-4), recruiting a total of N = 28 patients with “high-risk,” cisplatin-ineligible, operable muscle-invasive bladder cancer [17]. Of note, “high risk” was defined as having features including bulky tumors, variant histology, lymphovascular invasion, hydronephrosis, and/or high-grade upper tract disease. The primary study endpoint for MDACC was safety. Of the 28 patients recruited, 24 patients ultimately underwent cystectomy as per study protocol. From these 24 patients, 9 (37.5%) achieved a complete pathological response, and the relapse-free survival rate was 82.8% at 1 year (ClinicalTrials.gov Identifier: NCT02812420).
Immunohistochemistry
Like the ABACUS trial, PD-L1 immunohistochemistry within the MDACC trial was executed using the E1L3N assay, and like the ABACUS trial, PD-L1 expression did not correlate with treatment response. Multiplex immunofluorescence staining was also used to identify tertiary lymphoid structures (TLS) as in the NABUCCO trial. Although baseline TLS numbers were not associated with treatment response within the NABUCCO trial, the MDACC study results included a higher density of TLS in pretreatment tissue of responders, which corresponded with favorable outcomes. Further characterization of immune cell subsets revealed that responding tumors had significantly higher density of pretreatment B cells, CD4+ T cells, and CD8+ T cells, again suggesting utility for preexisting immune infiltration. Finally, comparing pre- and post-immunotherapy specimen showed an increase in ICOS+CD4+ T cells in posttreatment tumor tissues of responding tumors compared to nonresponders. These observations align with the concept of increased immune infiltration for responding tumors post-therapy, reinforcing the concept of tumor scarring which, at least in part, involves immune cell recruitment [37]. The scarring phenomenon has been proposed (albeit in different contexts) for all three of the previous studies.
RNA-Based Molecular Biomarkers
A four-gene TLS expression signature (POU2AF1, LAMP3, CD79A, and MS4A1) was found to be significantly higher in responding tumors in the MDACC study. However, the tGE8 signature scores were not found to be significantly different when comparing responders to nonresponders. Unfortunately, this signature has only demonstrated significance for predicting response to atezolizumab monotherapy (ABACUS) and lacks clear utility in either the NABUCCO or MDACC trials, suggesting this signature in the context of combination immunotherapy is of minimal utility.
DNA-Based Molecular Biomarkers
Whole exome sequencing for the MDACC trial found that neither TMB nor DDR GA correlated with response to therapy. This study also predefined KRAS, PIK3CA, PBRM1, EFGR, NRAS, APC2, and FGFR mutations as interesting targets for investigation, although none of these were found to have an association with response to therapy in context of this pilot study. Similarly, the ABACUS study explored the fibroblast growth factor (FGF) pathway as a potential region of interest, but neither the PURE-01 nor MDACC trials found this pathway to be predictive of response to immune checkpoint blockade.
Integrating Biomarkers to Refine the Molecular Diagnosis in the MDACC Study
The MDACC study was similar to NABUCCO, combining an anti-CTLA4 inhibitor (tremelimumab) with an anti-PD-L1 inhibitor (durvalumab). Likewise, this study also included patients with more aggressive disease, with MDACC including patients with variant histology. Like ABACUS and PURE-01, response in MDACC appeared to have correlation with preexisting immune infiltration. However, these data contrast with the findings from NABUCCO, which used a similar combination of checkpoint inhibitors. Further study will be required to reconcile these differences and identify the clinical and biological features which may help predict response to combination anti-CTLA and anti-PD-L1 therapy.
Conclusions and Future Directions
There are several challenges associated with transitioning immune therapy into the neoadjuvant setting, many of which may be mitigated, at least in part, by biomarker-driven approaches [38]. First, the pathological response rates of IBC are comparable to NAC, averaging about 40% overall [39], which raises questions as to whether these patients may have received greater benefit from chemotherapy or radical cystectomy alone. As discussed for PURE-01, patients with a tumor of the claudin-low subtype had exceptional outcomes with pembrolizumab, but comparatively poor outcomes with NAC [18], providing compelling data that molecular subtypes may provide a mechanism to stratify patients to the treatment which would provide the greatest benefit. One caveat to this finding was that the claudin-low tumors did show a significant association with pathological response, which may contradict the data generated in the NAC setting, where complete response was associated with improved survival [2].
This may be an issue associated with radiological tumor assessment, as this has not been standardized for immune therapy in the neoadjuvant setting [38], although multiparametric magnetic resonance imaging has shown promise in this respect [40]. At this time, we have limited information on how immune therapy impacts the biology and phenotype (i.e., volume) of patient tumor, which may confound our ability to connect pathological response and outcomes. There may also be the added effect of the TURBT procedure which until recently has not been considered in molecular profiling studies.
In the PURE-01 study, three molecular subtypes were identified post-pembrolizumab, including luminal, basal, and “scar-like” tumors [34]. The latter, defined largely by higher expression of stromal markers, represented half of the PURE-01 RC samples. Notably, in the ABACUS study, responding tumors were predominantly found to be an infiltrated subtype (Lund 2012 model). Like the “scar-like” subtype, the infiltrated subtype is defined by high levels of stromal and immune infiltration, suggesting a commonality between these two classifications. This scar-like subtype has been suggested to be the result of the impact of TURBT, resulting in a wound healing at the tumor site [34, 41]. Given the high rates of the infiltrated subtype and scar-like in ABACUS and PURE-01, respectively, it is tempting to speculate that TURBT, rather than systemic immune therapy, has a greater impact on local tumor control, while systemic therapy offers metastatic control and improved outcomes. This may explain, at least in part, why certain molecular signatures (i.e., claudin-low subtype) were not significantly associated with response yet were significantly associated with patient outcome. The truth is likely somewhere in between, where local tumor control in terms of pathological response is achieved by a combination of surgery (TURBT) and systemic therapy.
In a recent post-chemotherapy study, four molecular subtypes were identified, including a scar-like subtype and a highly immune-enriched subtype which was not identified in the PURE-01 study [34, 41]. In the ABACUS study, the infiltrated subtype is considered immune-enriched but is also enriched with stromal type cells (i.e., myofibroblasts) [26], where the post-NAC immune subtype did not report stromal infiltration [41]. In both studies, amplified or increased immune activity was also reported for treated tissues in both checkpoint studies, suggesting that a generalized immune response is achieved with either neoadjuvant chemotherapy or immune therapy [18, 19]. In the ABACUS study, the infiltrated subtype was enriched post-pembrolizumab, while luminal (UroA, GU, UroB) and basal (SCCL) tumors were evenly represented [19]. In contrast, tumors collected post-pembrolizumab were enriched with scar-like and luminal subtypes, with basal tumors poorly represented [34]. An important caveat, when considering the molecular subtype cells generated for the ABACUS study, is most molecular subtyping models are trained on untreated tumor tissue (TURBT and/or RC), meaning accuracy of the subtypes on treated tissues is unknown. The subtypes for PURE-01 were generated using consensus clustering, meaning they are not “true” subtype cells by a classifier, but rather groups of tumors that have molecular features consistent with a representative subtype.
In general, preexisting immunity appears to be a reasonable metric to predict response to checkpoint inhibitors. In ABACUS, PURE-01 and MDACC patients with tumors that showed higher levels of immune infiltration, by a variety of assays, had improved responses compared to those with lower immune infiltration [16,17,18,19]. However, the NABUCCO trial did not find a correlation between preexisting immune infiltration and response [16]. This study included patients with more advanced disease, but the small numbers in the trial preclude determining how this may affect any correlation between treatment and response. One of the limitations of using “high immune infiltration” as a method to stratify patients to treatment is the lack of standardization of a threshold or cut point for determining “high.” Another limitation is the range of assays used across the various studies described in this study. To best enable comparison across studies, future trials would ideally include several standardized metrics (i.e., median, quartiles, etc.) and platforms. Another potential option is to standardize the use of molecular subtypes for studies involving gene expression analysis. One advantage of molecular subtypes is the models tend to be categorical, stratifying patients into one of several different subtypes. Several of these molecular subtypes are characterized by higher immune infiltration (i.e., basal or claudin-low) or by a lack of infiltrates (i.e., luminal), suggesting good utility for predicting outcomes, as was demonstrated in the PURE-01 study [18].
Taken together, the ABACUS, PURE-01, NAMBUCCO, and MDACC study, while different in some respects, all provide key biomarker data to further our understanding of which tumor features may be driving response to therapy in the neoadjuvant setting. A commonality among these trials is baseline immunity appears to be predictive of response, except for NABUCCO. However, as an independent biomarker, immune infiltration scores would not facilitate stratification of patients to immune therapy or chemotherapy, which remains the standard of care. Here, molecular subtyping may have greater utility, as different subtypes have now been reported to have varying response to both chemotherapy and immune therapy. After treatment with neoadjuvant immune therapy, there appears to be an enrichment of stromal infiltration, whether defined as an infiltrated subtype [26], scar-like subtype, or increased TLS. Unfortunately, there is no clear pattern for which tumors may adopt such a profile, further emphasizing a need to profile tumor tissue post-therapy. Another advantage of this approach is that the character of the tumor post-therapy may also help to inform adjuvant treatment decisions.
Biomarker development in the neoadjuvant immune checkpoint setting is ongoing, as are the clinical trials in this setting. The data accumulated to date are promising and suggest that selection of patients using biomarkers is highly feasible and may ultimately facilitate the adoption of neoadjuvant immune therapy as a new standard of care.
References
International Collaboration of T, Medical Research Council Advanced Bladder Cancer Working P, European Organisation for R, Treatment of Cancer Genito-Urinary Tract Cancer G, Australian Bladder Cancer Study G, National Cancer Institute of Canada Clinical Trials G, et al. International phase III trial assessing neoadjuvant cisplatin, methotrexate, and vinblastine chemotherapy for muscle-invasive bladder cancer: long-term results of the BA06 30894 trial. J Clin Oncol. 2011;29(16):2171–7.
Grossman HB, Natale RB, Tangen CM, Speights VO, Vogelzang NJ, Trump DL, et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med. 2003;349(9):859–66.
Advanced Bladder Cancer Overview C. Neoadjuvant chemotherapy for invasive bladder cancer. Cochrane Database Syst Rev. 2005;(2):CD005246.
Reardon ZD, Patel SG, Zaid HB, Stimson CJ, Resnick MJ, Keegan KA, et al. Trends in the use of perioperative chemotherapy for localized and locally advanced muscle-invasive bladder cancer: a sign of changing tides. Eur Urol. 2015;67(1):165–70.
Kim HS, Jeong CW, Kwak C, Kim HH, Ku JH. Pathological T0 following cisplatin-based neoadjuvant chemotherapy for muscle-invasive bladder cancer: a network meta-analysis. Clin Cancer Res. 2016;22(5):1086–94.
Patel MR, Ellerton J, Infante JR, Agrawal M, Gordon M, Aljumaily R, et al. Avelumab in metastatic urothelial carcinoma after platinum failure (JAVELIN solid tumor): pooled results from two expansion cohorts of an open-label, phase 1 trial. Lancet Oncol. 2018;19(1):51–64.
Powles T, O'Donnell PH, Massard C, Arkenau HT, Friedlander TW, Hoimes CJ, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(9):e172411.
Bellmunt J, de Wit R, Vaughn DJ, Fradet Y, Lee JL, Fong L, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015–26.
Sharma P, Callahan MK, Bono P, Kim J, Spiliopoulou P, Calvo E, et al. Nivolumab monotherapy in recurrent metastatic urothelial carcinoma (CheckMate 032): a multicentre, open-label, two-stage, multi-arm, phase 1/2 trial. Lancet Oncol. 2016;17(11):1590–8.
Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, Necchi A, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387(10031):1909–20.
Witjes JA, Bruins HM, Cathomas R, Comperat EM, Cowan NC, Gakis G, et al. European Association of Urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol. 2021;79(1):82–104.
Lv J, Zhu Y, Ji A, Zhang Q, Liao G. Mining TCGA database for tumor mutation burden and their clinical significance in bladder cancer. Biosci Rep. 2020;40(4):BSR20194337.
Robertson AG, Kim J, Al-Ahmadie H, Bellmunt J, Guo G, Cherniack AD, et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell. 2017;171(3):540–56.e25.
Wu Z, Zhu K, Liu Q, Liu Y, Chen L, Cui J, et al. Profiles of immune infiltration in bladder cancer and its clinical significance: an integrative genomic analysis. Int J Med Sci. 2020;17(6):762–72.
Kamoun A, de Reynies A, Allory Y, Sjodahl G, Robertson AG, Seiler R, et al. A consensus molecular classification of muscle-invasive bladder cancer. Eur Urol. 2020;77(4):420–33.
van Dijk N, Gil-Jimenez A, Silina K, Hendricksen K, Smit LA, de Feijter JM, et al. Preoperative ipilimumab plus nivolumab in locoregionally advanced urothelial cancer: the NABUCCO trial. Nat Med. 2020;26(12):1839–44.
Gao J, Navai N, Alhalabi O, Siefker-Radtke A, Campbell MT, Tidwell RS, et al. Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat Med. 2020;26(12):1845–51.
Necchi A, Raggi D, Gallina A, Ross JS, Fare E, Giannatempo P, et al. Impact of molecular subtyping and immune infiltration on pathological response and outcome following neoadjuvant pembrolizumab in muscle-invasive bladder cancer. Eur Urol. 2020;77(6):701–10.
Powles T, Kockx M, Rodriguez-Vida A, Duran I, Crabb SJ, Van Der Heijden MS, et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat Med. 2019;25(11):1706–14.
Hoimes CJ, Adra N, Fleming MT, Kaimakliotis HZ, Picus J, Smith ZL, et al. Phase Ib/II neoadjuvant (N-) pembrolizumab (P) and chemotherapy for locally advanced urothelial cancer (laUC): final results from the cisplatin (C)- eligible cohort of HCRN GU14-188. J Clin Oncol. 2020;38(15_Suppl):5047.
Kaimakliotis HZ, Adra N, Kelly WK, Trabulsi EJ, Lauer RC, Picus J, et al. Phase II neoadjuvant (N-) gemcitabine (G) and pembrolizumab (P) for locally advanced urothelial cancer (laUC): interim results from the cisplatin (C)-ineligible cohort of GU14-188. J Clin Oncol. 2020;38(15_Suppl):5019.
Gupta S, Sonpavde G, Weight CJ, McGregor BA, Gupta S, Maughan BL, et al. Results from BLASST-1 (Bladder Cancer Signal Seeking Trial) of nivolumab, gemcitabine, and cisplatin in muscle invasive bladder cancer (MIBC) undergoing cystectomy. J Clin Oncol. 2020;38(6_Suppl):439.
Grande E, Guerrero F, Puente J, Galante I, Duran I, Dominguez M, et al. DUTRENEO trial: a randomized phase II trial of DUrvalumab and TREmelimumab versus chemotherapy as a NEOadjuvant approach to muscle-invasive urothelial bladder cancer (MIBC) patients (pts) prospectively selected by an interferon (INF)-gamma immune signature. J Clin Oncol. 2020;38(15_Suppl):5012.
Rouanne M, Bajorin DF, Hannan R, Galsky MD, Williams SB, Necchi A, et al. Rationale and outcomes for neoadjuvant immunotherapy in urothelial carcinoma of the bladder. Eur Urol Oncol. 2020;3(6):728–38.
Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature. 2018;554(7693):544–8.
Sjodahl G, Lauss M, Lovgren K, Chebil G, Gudjonsson S, Veerla S, et al. A molecular taxonomy for urothelial carcinoma. Clin Cancer Res. 2012;18(12):3377–86.
Powles T, Loriot Y, Ravaud A, Vogelzang NJ, Duran I, Retz M, et al. Atezolizumab (atezo) vs. chemotherapy (chemo) in platinum-treated locally advanced or metastatic urothelial carcinoma (mUC): immune biomarkers, tumor mutational burden (TMB), and clinical outcomes from the phase III IMvigor211 study. J Clin Oncol. 2018;36(6_Suppl):409.
Loriot Y, Necchi A, Park SH, Garcia-Donas J, Huddart R, Burgess E, et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N Engl J Med. 2019;381(4):338–48.
Faltas BM, Prandi D, Tagawa ST, Molina AM, Nanus DM, Sternberg C, et al. Clonal evolution of chemotherapy-resistant urothelial carcinoma. Nat Genet. 2016;48(12):1490–9.
Bandini M, Gibb EA, Gallina A, Raggi D, Marandino L, Bianchi M, et al. Does the administration of preoperative pembrolizumab lead to sustained remission post-cystectomy? First survival outcomes from the PURE-01 study ☆. Ann Oncol. 2020;31(12):1755–63.
Necchi A, Anichini A, Raggi D, Briganti A, Massa S, Luciano R, et al. Pembrolizumab as neoadjuvant therapy before radical cystectomy in patients with muscle-invasive urothelial bladder carcinoma (PURE-01): an open-label, single-arm, phase II study. J Clin Oncol. 2018;36(34):3353–60.
Batista da Costa J, Gibb EA, Bivalacqua TJ, Liu Y, Oo HZ, Miyamoto DT, et al. Molecular characterization of neuroendocrine-like bladder cancer. Clin Cancer Res. 2019;25(13):3908–20.
Seiler R, Ashab HAD, Erho N, van Rhijn BWG, Winters B, Douglas J, et al. Impact of molecular subtypes in muscle-invasive bladder cancer on predicting response and survival after neoadjuvant chemotherapy. Eur Urol. 2017;72(4):544–54.
Necchi A, de Jong JJ, Raggi D, Briganti A, Marandino L, Gallina A, Bandini M, Dabbas B, Davicioni E, Capitanio U, Montorsi F, Seiler R, Wright JL, Lotan Y, Black PC, Gibb EA. Molecular characterization of residual bladder cancer after neoadjuvant pembrolizumab. Eur Urol. 2021;80:149–59.
Necchi A, Raggi D, Giannatempo P, Marandino L, Fare E, Gallina A, et al. Can patients with muscle-invasive bladder cancer and fibroblast growth factor receptor-3 alterations still be considered for neoadjuvant pembrolizumab? A comprehensive assessment from the updated results of the PURE-01 study. Eur Urol Oncol. 2020;S2588-9311(20)30053-5.
Dieu-Nosjean MC, Goc J, Giraldo NA, Sautes-Fridman C, Fridman WH. Tertiary lymphoid structures in cancer and beyond. Trends Immunol. 2014;35(11):571–80.
Dvorak HF. Tumors: wounds that do not heal-redux. Cancer Immunol Res. 2015;3(1):1–11.
Zucali PA, Cordua N, D'Antonio F, Borea F, Perrino M, De Vincenzo F, et al. Current perspectives on immunotherapy in the peri-operative setting of muscle-infiltrating bladder cancer. Front Oncol. 2020;10:568279.
Zargar H, Espiritu PN, Fairey AS, Mertens LS, Dinney CP, Mir MC, et al. Multicenter assessment of neoadjuvant chemotherapy for muscle-invasive bladder cancer. Eur Urol. 2015;67(2):241–9.
Bandini M, Calareso G, Raggi D, Marandino L, Colecchia M, Gallina A, et al. The value of multiparametric magnetic resonance imaging sequences to assist in the decision making of muscle-invasive bladder cancer. Eur Urol Oncol. 2020.
Seiler R, Gibb EA, Wang NQ, Oo HZ, Lam HM, van Kessel KE, et al. Divergent biological response to neoadjuvant chemotherapy in muscle-invasive bladder cancer. Clin Cancer Res. 2019;25(16):5082–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
de Jong, J.J., Gibb, E.A. (2022). Biomarkers Predicting Outcomes Before and After Neoadjuvant Immune Checkpoint Inhibition Therapy for Muscle-Invasive Bladder Cancer. In: Necchi, A., Spiess, P.E. (eds) Neoadjuvant Immunotherapy Treatment of Localized Genitourinary Cancers. Springer, Cham. https://doi.org/10.1007/978-3-030-80546-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-80546-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-80545-6
Online ISBN: 978-3-030-80546-3
eBook Packages: MedicineMedicine (R0)