Abstract
-
The ganglion is the most common soft tissue mass of the hand and wrist.
-
The advantages of their arthroscopical treatment include greater motion, improved cosmesis, and the possibility of identifying/treating other intraarticular pathology.
-
Both dorsal and volar ganglia can be treated arthroscopically.
-
Treatment limitations include inconsistent identification of the ganglion stalk which may lead to.
-
Unnecessary debridement of uninvolved tissue.
-
Midcarpal and radiocarpal soft tissue anatomy is mandatory during arthroscopic ganglion treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Arthroscopy ganglion
- Arthroscopy volar ganglion
- Arthroscopy dorsal ganglion
- Methylene blue
- Scapholunate ligament
1 Background
Dorsal wrist ganglions are mucinous benign tumors that arise at the level of the dorsal scapholunate ligament (SLL). Sometimes these are easily visible and palpable under the skin, close to the extensor carpi radialis brevis (ECRB) distal tendon insertion. Even in those cases, their origin is at the SLL level. Sometimes the ganglion is not visible under the skin and it is difficult to palpate, so-called occult dorsal ganglia.
1.1 Surgical Anatomy
Dorsal SLL reaches the midcarpal joint (Fig. 112.1) and is in contact with the Dorsal Intercarpal Ligament (DIC) that connects the dorsal aspect of the scaphoid and the triquetrum (Fig. 112.2). The dorsal capsuloligamentous scapholunate septum (DCSS) attaches the dorsal wrist capsule to the dorsal SLL and the DIC. The DCSS separates the dorsal radiocarpal and the dorsal midcarpal joint spaces (Fig. 112.3). The SLL, DIC, and the DCSS have a biomechanical role in scapholunate joint stabilization. Preserving all of them during dorsal ganglions excision may be beneficial.
Dorsal aspect of a right cadaver specimen wrist. Dorsal wrist capsule between the distal aspect of the radiotriquetral ligament (***) and the carpometacarpal joints have been removed. Dorsal scapholunate ligament (*) is aligned with the 3/4 portal and it is intimately related to the Dorsal Intercarpal Ligament (DIC) (**). Some dorsal ganglia that originate at the dorsal SLL ligament can be palpated between the distal tendons of the extensor carpi radialis brevis (ECRB) and extensor carpi radialis longus (ECRL) muscles. R radius, U Ulna
Left radiocarpal joint space. The scope is in 6R portal. The needle enters the joint through the 3/4 portal. The dorsal capsuloligamentous scapholunate septum (DCSS) connects the SLL with the dorsal capsule (1). At this level, the DCSS is the roof of the dorsal radiocarpal joint space (L Lunate, S scaphoid)
All ganglions are mucinous collections secondary to a lesion of proper ligament or Sharpey fibers. In order to treat them, both the ganglion stump and the underlying degenerative ligament tissue and fibers must be excised. The risk of this tissue excision is an iatrogenic lesion of the dorsal SLL. The main advantage of arthroscopic ganglion excision technique is that the ganglion and its stump origin can clearly be seen and debrided while avoiding unnecessary sacrifice of healthy tissue.
Partial SLL ligament lesions associated with dorsal ganglion development may lead to SLL dynamic dysfunction. The advantage of arthroscopic dorsal ganglion excision technique is the opportunity to be able to directly check SLL mechanical properties, and to associate an SLL augmentation technique when dorsal SLL is partially torn.
Volar radiocarpal ganglion stumps mainly arise between volar radiocarpal ligaments (Fig. 112.4). Most volar ganglion pedicle stumps are found at the interval between radioscaphocapitate and long radiolunate ligaments (Fig. 112.5). Some volar ganglia arise through the interval between short and long radiolunate ligaments (Fig. 112.6).
Right cadaver specimen wrist. The upper arrow shows the interval between the radioscaphocapitate (1) and the long radiolunate (2) ligaments. The lower arrow indicates the interval between the long (2) and the short (3) radiolunate ligaments. (S scaphoid bone, L lunate bone, R radius); (4) Testut Ligament (profundus radioscaphoid ligament)
Less frequently, a ganglion can originate from the scaphotrapeziotrapezoid (STT) joint or flexor carpi radialis (FCR) distal tendon sheath.
2 Indications and Contraindications
-
Primary arthroscopic ganglionectomy is indicated only when symptoms appear. Patients may complain of pain, loss of strength, or reduced range of motion (ROM) of the wrist. The pros and cons of surgery can be discussed with the patient in case of unacceptable aesthetics due to ganglion size.
-
Arthroscopic ganglionectomy is also indicated in ganglion recurrence, especially when the primary procedure has been through open surgery, and could have created an iatrogenic intraarticular ligament lesion.
There are no specific contraindications for this procedure. Local infection and surgeon inexperience are contraindications for this procedure.
3 Surgical Technique
3.1 Preoperative Planning
Magnetic resonance imaging (MRI) can assist in identification of the pedicle and cyst wall location and help to plan the surgery, as the resection of the ganglion must be performed at the origin of the pedicle stump (Table 112.1).
-
Some occult ganglia have the cyst wall in the radiocarpal joint; others in the midcarpal joint.
-
Some dorsal and volar ganglia have a cyst wall in the extracapsular space; others are only intraarticular.
-
Some extraarticular ganglia are multi-lobulated. These MRI findings do not contraindicate arthroscopic ganglionectomy, but may suggest the need to perform a direct trans-cyst approach.
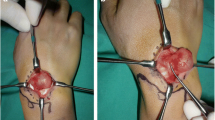
3.2 Ultrasound-Guided Volar Ganglion Methylene Blue Injection
Volar radiocarpal ganglion pedicles can arise between different volar radiocarpal ligaments. Ultrasound guided injection of 1 cc methylene blue into the ganglion before traction is applied to the wrist facilitating identification of the correct ligament interval which must be debrided (Figs. 112.7 and 112.8).
3.3 Box Theory
The wrist is like a box which can be reached through many different portals. The distance between our instrument and camera should be as long as possible to facilitate the instruments maneuverability. Therefore, depending on the ganglion location, different portals must be used. Figure 112.9 shows the usual portals for each type of ganglion excision.
The wrist box concept. Depending on the ganglion pedicle and cyst wall locations, the useful portals will vary in each case. To treat an occult radiocarpal joint ganglion (G), the scope should be introduced through the 6R portal (2) and the instruments through the 1/2 portal (3). To treat a large dorsal radiocarpal ganglion, the scope should be introduced through a volar portal (6) and the shaver through the 6R (2) or the 1/2 (3) portal. When the ganglion cyst wall has been removed, we should introduce the scope in 6R (2) and the shaver in the 1/2 portal to resect the pedicle stump at the dorsal aspect of the dorsal SLL. To treat a large dorsal extraarticular radiocarpal joint ganglion, the scope should be introduced through a volar portal (6) and the shaver through the 6R (2) or the 1/2 (3) portals to resect the capsule around the ganglion pedicle without damaging the radiotriquetral ligament or the dorsal intercarpal ligament (DIC) (see Fig. 112.2). To treat a dorsal midcarpal ganglion, the scope should be introduced in the MCU portal (5) and the instruments through the MCR (4) portal. A volar midcarpal portal can also be used to introduce the scope and facilitate the instruments maneuverability. To treat a volar radiocarpal ganglion, the scope should be introduced through the 6R portal (2) and the instruments through the 3/4 Portal (1)
3.4 Local Anesthesia
In most patients, the procedure can be done under local anesthesia. Each portal area is subcutaneously injected with 1 cc of epinephrine 1/100,000-lidocaine 2% solution, 30 min before starting the surgical procedure. Local anesthesia allows control of extensor tendons and flexor pollicis longus integrity after dorsal capsulectomy is performed in extraarticular dorsal ganglions or after volar radiocarpal ganglionectomy. Intraarticular surgical procedures are painless; nevertheless, if the patient informs of intraarticular pain or if synovectomy triggers some annoying bleeding, injection of epinephrine-lidocaine solution into the joint can be performed.
3.5 Dry Arthroscopy
Dry arthroscopy is preferred to avoid intraarticular soft tissue swelling which can difficult the vision of the ganglion pedicle. Ensure that the valves of the arthroscope sheath are always open to allow free circulation of air and prevent capsular collapse and loss of visualization. Occasionally insert some saline to prevent shaver tamponade.
3.6 Preliminary Systematic Examination
An initial diagnostic assessment of both radiocarpal and midcarpal joint spaces should be performed in every case and a sequence from radial to ulnar, and volar to dorsal should be followed. The integrity of the triangular fibrocartilage complex (TFCC), volar lunotriquetral ligament, dorsal and volar scapholunate ligaments, three volar radiocarpal ligaments, and joint dorsal and volar capsule must be assessed.
3.7 Occult Dorsal Ganglion Cysts
These are located adjacent to dorsal SLL and can arise proximally, into the radiocarpal joint space or distally, into the midcarpal joint space.
-
The arthroscope is introduced into the 3–4 portal to establish the 6R portal under direct intraarticular vision. The scope is then redirected to the 6-R portal.
-
Establish, subsequently, the 1–2 portal under direct intraarticular control. Insert the hook through the 1–2 portal.
-
Find the scapholunate interosseous membrane with the hook and follow it in a distal direction (Fig. 112.10) until the dorsal SLL is clearly seen. If the dorsal capsule (C) collapses the space, it can be pull-out with the hook or with a 1-0 suture entering through the 6R portal and exiting through the 3–4 portal.
-
If the ganglion cyst is in the radiocarpal joint, it will be clearly seen at this moment (Fig. 112.11) with its stump emerging from the dorsal SLL ligament (Fig. 112.12).
-
The shaver is then inserted into the 1–2 portal. The complete ganglion and his stalk can then be shaved; the d-SLL and DCSS should be preserved if the shaver is correctly directed under direct vision control from the 6R portal.
-
The arthroscope is introduced into the MCU portal to establish the MCR portal under direct intraarticular vision. Instrumentation is through the MCR portal.
-
Find the scapholunate interosseous joint space with the hook and direct it dorsally. It will get hooked over the dorsal SLL ligament that can be, at this moment, palpated and strained. At its dorsal portion, the hook will be able to palpate the distal surface of the DCSS and the DIC at its dorsal aspect.
-
If the ganglion cyst is in the midcarpal joint, it will be clearly seen (Fig. 112.13) and its stump can be clearly visualized emerging between the dorsal aspect of the SLL ligament and the volar aspect of the DIC (Fig. 112.14).
-
The shaver is then be inserted into the MCR portal to completely shave the ganglion and his stalk, preserving the SLL, the DCSS, and the DIC, under direct vision control from the MCU portal.
-
The ganglion stalk may be thin and long: in these cases, it emerges at the radiocarpal dorsal aspect of the SLL, pierces the DCSS distally and the cyst wall can be found in the midcarpal joint. This is the reason why both radiocarpal and midcarpal joint space arthroscopies should always be performed during arthroscopic ganglionectomy.
Radiocarpal joint space arthroscopy of a right wrist. Scope is in 6R portal. The hook is in the 1–2 portal. The hook is in most distal dorsal portion of the interosseous membrane (IM) between the scaphoid (S) and the lunate (L), and is pointing the dorsal capsuloligamentous scapholunate septum (DCSS). (C dorsal capsule)
Radiocarpal joint space arthroscopy of a right wrist. Scope is in 6R portal. The radiocarpal occult ganglion stalk (St) emerges besides the dorsal scapholunate ligament (SLL). The ganglion (G) is just under the dorsal capsuloligamentous scapholunate septum (DCSS). (IM interosseous scapholunate membrane, L lunate bone)
3.8 Non-occult Dorsal Intracapsular Ganglion Cysts
The stump arises at the dorsal SLL but they are bulky (non-occult). Most of them are in the radiocarpal joint (Fig. 112.15).
Radiocarpal joint space arthroscopy of a right wrist. The scope is in 6R portal. Although the ganglion emerges from the dorsal aspect of the SLL, its bulky cyst invades all the dorsal intracapsular aspect of the joint. In this case, trying to reach the stump before shaving the cyst can be difficult. Nevertheless, after cyst shaving, the SLL should be located to cautiously debride any degenerative ligament fibers at its level
Although the ganglion emerges from the dorsal aspect of the SLL, its bulky cyst invades all the dorsal intracapsular aspect of the radiocarpal joint. In this case, trying to reach the stump before shaving the cyst can be difficult. Nevertheless, after cyst removal with the shaver, the SLL should be reached following the steps mentioned above, to carefully debride any degenerative ligament fibers at this level. Radiofrequency is not recommended: SLL is richly innervated and heat can damage the mechanoreceptors contained in its ligament fibers.
3.9 Non-occult Dorsal Extracapsular Ganglion
The stump arises at the dorsal SLL but the ganglion emerges into the extracapsular space and becomes palpable. Most of these are in the radiocarpal joint. They become extraarticular through the 3–4 portal area, at the distal margin of the radiotriquetral ligament. Less frequently they are midcarpal ganglions which exit the joint at the proximal margin of the DIC ligament.
-
During excision, the intraarticular steps reviewed above have to be combined with a dorsal 1 cm2 capsulectomy. We perform a cyst-sparing portal technique but we usually pass a 18–22-gauge needle through the cyst into the joint at the level of the stalk, to better identify the area where the capsulectomy has to be done; this typically will be at the 3–4 interval. In the same way, we usually introduce the scope in a volar portal to ensure that the capsulectomy preserves the radiotriquetral ligament (in the radiocarpal joint) (Fig. 112.16) or the dorsal intercarpal ligament (in the midcarpal joint).
-
We usually scope from the volar central portal which was described by Fernando Corella. This portal allows vision of both radiocarpal and midcarpal joints, without any volar ligament damage (Fig. 112.17).
-
Dorsal capsulectomy is performed until visualization of the extensor tendons (usually one of the Extensor Digitorum Communis or occasionally ECRB tendon).
The volar central portal described by Corella F. et al. allows access to both radiocarpal and midcarpal joints (yellow circles). It is centered on the lunate, with the volar structures at risk protected by the tendons. It is a reproducible and safe portal that allows radiocarpal and midcarpal joints inspection through one single incision centered between both wrist creases
3.10 Volar Ganglion Cysts
Their stump arises in the volar aspect of the wrist through the volar radiocarpal joint space and is usually associated with a ligament area degeneration. The ligament degeneration is sometimes difficult to appreciate until synovectomy of the dorsal aspect of the volar radiocarpal ligaments has been completed (Fig. 112.18). Intra-lesional methylene blue injection may help to identify the proper ligament interval where the cyst stump is located, as the cysts are not visible from inside the joint.
-
The arthroscope is introduced through 3–4 portal and instrumentation is through the 1–2 portal.
-
The ligament interval and the cyst stump are identified with the hook probe.
-
The shaver should be introduced to debride the ligament degenerative area and to drain the cyst capsule contents (Fig. 112.19).
-
External digital pressure over the cyst helps to pour away the cyst contain into the joint.
-
The cyst capsule is not removed. The patient should be informed preoperatively that a swelling or tumor will persist at the area for 3 weeks; this is the remnant cyst capsule and will slowly disappear.
Right radiocarpal joint arthroscopy. Scope is in 3–4 portal. Degeneration of long radiolunate ligament (LRL) fibers is clearly seen. This degenerative ligament area must be debrided with the shaver introduced into the joint through the 1–2 portal. The volar ganglion is presumably at the volar aspect of this area: the initial introduction of the hook into the interval between the radioscaphocapitate (RSC) and the long radiolunate ligaments combined with a digital pressure on the cyst area should show the presence of some mucinous cyst content (colored in blue if the cyst has previously been injected with methylene blue)
Right radiocarpal joint arthroscopy. Scope is in 3–4 portal; the shaver is in 1–2 portal. Degeneration of long radiolunate ligament (LRL) fibers is clearly seen and must be debrided. The volar ganglion is presumably at the volar aspect of this area: a hook is passed into the interval between the radioscaphocapitate (RSC) and the long radiolunate ligaments and combined with a digital pressure on the cyst area to see some mucinous cyst content (colored in blue if the cyst has previously been injected with methylene blue)
4 Technical Tips
-
Dorsal radiocarpal capsule can be separated from the dorsal aspect of the first carpal row bones by using dorsal traction with a simple 1-0 suture thread or a nitinol wire inserted through the 3–4 portal and exiting through the 6R portal. This maneuver facilitates the dorsal SLL inspection during radiocarpal joint arthroscopy.
-
Radiofrequency is not recommended: heat can damage the extensor tendons in dorsal capsulectomy, SLL innervation in occult ganglionectomy, and median nerve or radial artery in volar ganglion excision.
-
Intermittent saline joint injection is the better system to avoid shaver tamponade and intraarticular soft tissue swelling; half intensity suction is recommended to allow good shaving function without capsule collapse.
-
An accessory instrument portal to insert the hook while the shaver is in action helps to actively protect the SLL, DIC, DCSS, or RTq ligaments from some iatrogenic damage. The assistant becomes a key point.
-
Dorsal capsulodesis should be performed after dorsal ganglion excision if the SLL seems mechanically incompetent during the hook test.
5 Pitfalls
-
Arthroscopic ganglion cyst excision should be performed by those who have basic competency with wrist arthroscopy.
-
Complete resection of the ganglion stalk, synovitis, and redundant cyst capsule is the standard approach for arthroscopic ganglionectomy.
-
Multi-lobulated cyst detected on MRI can also be arthroscopically treated.
-
Aggressive arthroscopic dorsal capsulectomy can result in extensor tendon injury.
-
When performing arthroscopic resection of volar wrist ganglion cyst, the proximity of the major neurovascular structures must be considered: radial artery lesions, injury of the median nerve, and neuropraxia of the superficial radial nerve have been described.
-
Methylene blue should be injected under ultrasound guidance to avoid intraarticular administration.
6 Postoperative Management and Rehabilitation
-
Stitchless closure (steri strips are adequate) and soft splint for 7 days.
-
Edema control of the hand during the first 2 days.
-
Active finger motion is encouraged from the first day.
-
Finger motion (extensor tendons) is checked and all patients are taught active and passive wrist motion after 1 week immobilization. Avoidance of strenuous activities for 4–6 weeks is recommended, except for those with concomitant intraarticular abnormalities.
7 Complications
-
Incomplete cyst excision.
-
Extraarticular edema after dorsal capsulectomy in wet arthroscopy.
-
Dorsal extensor tendon injury or tenosynovitis.
-
Median nerve neuroapraxia.
-
Scapholunate ligament injury.
-
Stiffness.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 ISAKOS
About this chapter
Cite this chapter
Esplugas, M., Lluch, A., Necci, F., Llusa Pérez, M. (2022). Arthroscopic Excision of Dorsal and Volar Ganglion Cysts. In: Bhatia, D.N., Bain, G.I., Poehling, G.G., Graves, B.R. (eds) Arthroscopy and Endoscopy of the Elbow, Wrist and Hand. Springer, Cham. https://doi.org/10.1007/978-3-030-79423-1_112
Download citation
DOI: https://doi.org/10.1007/978-3-030-79423-1_112
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-79422-4
Online ISBN: 978-3-030-79423-1
eBook Packages: MedicineMedicine (R0)