Abstract
Thalassemia major (TM) is a hereditary disease caused by defective globin synthesis. Because of the significant increase in life expectancy, these patients are suffering from various health conditions, including endocrinopathies and low bone mineral density. The aim of the present study was to investigate the correlation between clinical and biochemical parameters as well as to identify possible relations in a genotype to phenotype pattern. Sixty-four patients with TM (32 men and 32 women) participated in a cross-sectional study design. The patients were recruited from “Aghia Sofia” Children’s Hospital. Clinical and biochemical parameters were evaluated as well as specific mutations were identified. We have found significant correlations between biochemical parameters and iron chelation, hormone replacement treatment as well as TM genotype and hematocrit and T-score. To conclude, the current study showed that clinical parameters of TM patients correlate significantly with both biochemical factors and genotypical patient parameters. Our present study showed that there is a connection between genotype and phenotype as, for example, the identified relation between hematocrit and T-scores and TM-specific mutations. This connection indicates that there is still much more to learn about the role of mutations not only in the disease itself but also in the underlying comorbidities.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Thalassemia is the most frequent single-gene syndrome, affecting approximately 270 million patients worldwide. Their main clinical manifestation concerns the aberrant production of hemoglobin chains and in particular the expression of the alpha and beta hemoglobin chains. All human hemoglobin chain genes have a similar structure. They consist of about 1500 nucleotides and have three exons and two introns (IVS). The regions responsible for the connection between the heme and the alpha and beta chains are located in exon 2. There are at least three loci that regulate gene expression and are in the 200–300 bp promoter region before the “CAP site.” These sequences are the “TATA box” (about 30 bp) and the “CCAAT box” (between 70 and 90 bp), while the CACCC and CCGCCC sequences are located even farther [1,2,3].
Hemoglobin genes are located in two gene clusters. The first cluster concerns the hemoglobin genes for the alpha chain, which is located near the telomeric end of the short arm of the chromosome 16 (16p13.3, GenBank NG 000006). It also contains one embryonic gene of the zeta chain (HBZ or Zeta2), two genes for the alpha chain (HBA2, HBA1, or alpha2, alpha1), three pseudo-genes (HBZps, HBD, HBA1PS or pseta-zeta1, pseta-alpha2, pseta-alpha1), and the gene for the theta chain, whose functionality is still unknown [4, 5].
More than 80 different mutations have been identified worldwide,Footnote 1 causing an alpha thalassemia syndrome. The majority of these mutations cause deficits or even complete removal of the hemoglobin chains. Mutations concern sequence changes or complete removal of hemoglobin gene regions, while point mutations are rarer.
In particular for the beta thalassemia major (TM), more than 200 mutations have been identified.Footnote 2 Unlike alpha thalassemia, the majority of mutations in beta thalassemia are point mutations, which include single base replacement, deletions, or insertions of a small number of nucleotides. Mutations that limit the synthesis of beta hemoglobin chains are known as beta+ mutations, while those which completely abolish the hemoglobin synthesis are referred to as beta0 mutations. Most mutations result in increased erythrocyte production with decreased cell volume (Mean Corpuscular Volume (MCV) = 60–70 fl), as well as reduced mean cell hemoglobin (Mean Corpuscular Hemoglobin (MCH) = 19–23 pg). Point mutations responsible for beta TM are categorized with respect to the affected mechanism of beta globin synthesis. Mutations that affect transcription of globin genes are located either in the conserved regions of the beta gene promoter (e.g., TATA locus, CCAAT locus, or CACCC loci) or in the 5′-UTR region [1,2,3].
Thus, the characterization and identification of more than 200 mutations that are responsible for the pathogenesis of beta TM have greatly contributed toward the understanding of the molecular basis of TM. At the same time, this acquired knowledge has created the basis for the implementation of prevention programs for the eradication of this genetic disease [4, 5]. Nevertheless, TM syndromes still remain a major health problem around the world. The great diversity of the disease, in concordance with other genetic or environmental factors, constitutes the treatment of TM a challenging task. It is easy to understand that understanding of the molecular basis of TM syndromes is imperative in order to create more efficient treatments.
As aforementioned, TM is a hereditary disease, which is a result of defective globin synthesis [6, 7]. Patients suffering from TM are depended on frequent blood transfusion causing iron overload and are in need of several medications. The combination of transfusion and chelation therapy extended the life expectancy of TM patients. Thus, many health conditions, usually present in the aging general population, are becoming also common in TM patients [8]. In particular, some endocrinopathies are present in these patients, and among them low bone mineral density has become a topic of wide interest. Low bone mineral density (BMD) has also become a significant topic of interest. While severe bone deformities characterizing untreated TM patients are, nowadays, rarely seen, both low bone mineral density and disruption of bone architecture are observed in increased prevalence, in part due to the increasing age of TM patients [8].
During the past decades, literature data have shown that treatment of hypogonadism in patients with TM contributes to improve BMD as well as other comorbidities [9]. However, it is well known that bone remodeling takes place throughout the entire lifespan and is not dependent only on gonadal hormones. Moreover, the discovery of receptor activator of nuclear factor-κB ligand (RANKL), a tumor necrosis factor-family member, and its decoy receptor osteoprotegerin (OPG) widened the therapeutic spectrum. An imbalance of the RANKL/OPG ratio has been described in both postmenopausal women and β-thalassemia major-induced osteoporosis [10]. Several factors known to participate in other diseases have been found to play a significant role in TM. For example, RANKL and its decoy receptor osteoprotegerin (OPG) are known for its role in BMD but also for its role in TM [11, 12]. Besides their role in the osteoporotic patient, an imbalance of the RANKL/OPG ratio has been described in both postmenopausal women and β-thalassemia major-induced osteoporosis [11, 12]. Another example of identified factors, previously heterogeneous to TM, is the role of sclerostin in bone remodeling of TM patients. Sclerostin inhibits bone formation both in vitro and in vivo by directly reducing proliferation and differentiation of osteoblasts via the canonical Wnt signaling pathway. Sclerostin is thought to act by binding to the low-density lipoprotein receptors 5 and 6 and thus inhibit Wnt-catenin signaling [13]. A monoclonal antibody to sclerostin (Scl-Ab) has been developed that can inhibit the activity of sclerostin and therefore stimulate bone formation [14]. Patients with homozygous inactivating mutations of the SOST gene develop sclerosteosis, a rare genetic disorder characterized by undetectable level of serum sclerostin, very high bone mass phenotype, and nerve entrapment due to the excessive bone formation. Heterozygous carrier for the mutation individuals has increased bone mineral density and lowered fracture risk. This discovery has led to the hypothesis that sclerostin-neutralizing agents might mimic the heterozygous carrier condition and be efficacious in reversing bone loss in osteoporosis [15]. Clinical trials, furthermore, showed that anti-sclerostin agents increase bone formation and decrease bone resorption. One-year treatment with this anti-sclerostin agent in postmenopausal women with osteoporosis resulted in a lower risk of vertebral and clinical fractures than in the placebo-treated group [16].
Thus it is apparent that the TM patient is not only affected by the severity of the primary disease but also by a plethora of other comorbidities, which also consist significant health risks. In that sense, it is important for studies to investigate the understanding of the disease in a more complete and perhaps more systemic manner. The present work attempts to analyze the clinical and genotype data of a TM patient cohort in order to identify correlational patterns among them.
2 Materials and Methods
2.1 Patients and Study Design
In a previous study we have reported a cross-sectional study of 64 patients with TM. Follow-up of those patients was performed for the documentation of fracture incidence as well as for the effects of TM on bone metabolic factors [12]. Patients were collected from the Thalassemia Unit of “Aghia Sofia” Children’s Hospital during the period of July 2016 until March 2017. All patients are transfused every 2–3 weeks, in order to maintain a pre-transfusion hemoglobin >9.5 g/dl. Initially, 74 patients with TM were recruited; however, two patients have withdrawn consent, four patients passed away, and four patients were lost to follow-up. Thus, the remaining 64 subjects (mean age 40.86 ± 5.43 years, 32 men and 32 women) were evaluated with DXA of the lumbar spine and femoral neck. All 64 subjects were diagnosed for TM with standard hemoglobin electrophoresis and HPLC. Mutations were detected with the PCR methodology (LightCycler 480, Roche GmbH) and were further sequenced and screened for mutations known to be present in TM. Patients had either normal gonadal function or were under hormone replacement treatment for hypogonadism (ntotal = 21; 32.8%; nmen = 9; 28.1%; nwomen = 12; 37.5%) and were regularly receiving calcium carbonate and vitamin D supplementation. Only one woman and one man were on oral bisphosphonates, while three men were on denosumab. If a patient received only one medication (either nutritional supplementation or hormonal treatment), he or she is considered to be in a monotherapy.
This cohort was also screened with dual-energy X-ray absorptiometry (DXA) of the lumbar spine and hip. Osteoporosis was defined according to WHO criteria as a T-score of <−2.5 standard deviations (SD). Data on demographic information (age, gender, other treatment) were also collected. Biochemical factors evaluated included ferritin (ng/ml), 25-hydroxyvitamin D (25ΟΗD) (ng/ml), parathormone (PTH) (ng/lt), calcium (Ca+2) (in urine) (mmol), hematocrit (Ht) (%), DXA (lumbar spine), DXA (hip), free thyroxine (FT4) (ng/dl), thyroid-stimulating hormone (TSH) (mU/ml), luteinizing hormone (LH) (IU/lt), follicle-stimulating hormone (FSH) (IU/ml), testosterone (ng/dl), estradiol (E2) (pg/ml), calcium (Ca+2) (in serum) (mg/dl), and phosphorus (P+4) (mg/dl).
2.2 Measurement of Biomarkers
Blood has been obtained by standard phlebotomy procedures by a trained healthcare personnel. Whole blood has been collected and allowed to clot in serum tubes (Becton Dickinson UK Ltd., Oxfordshire, UK) and processed within 1 h from collection by double centrifugation at 2000 rpm for 10 min for serum separation. Serum was retained into 250 μl RNA/DNA enzyme-free frozen Eppendorf (ThermoFisher Scientific, Foster City, CA, USA) and immediately stored at −80 °C until further processing. Biochemical parameters were measured with a Siemens biochemical analyzer Advia 1800 (Siemens AG, Munich, Germany).
2.3 Statistical Analysis
Continuous data are presented as mean standard deviation (SD) and the categorical data are presented with their frequencies. For comparisons between groups, Student’s t-test and one-way analysis of variance (ANOVA) were performed for the continuous variables, and Chi-square tests were used for the categorical variables. Post hoc comparisons (adjusted with Bonferroni criterion) were also performed when significant differences (p < 0.05) of the biochemical markers in ANOVA tests were identified. The statistical analyses were conducted using the Statistical Package for the Social Sciences version 23. A value of p < 0.05 (two-tailed) was set as the level of significance.
Chi-square test of independence was used to evaluate the association between patients’ characteristics. The characteristics that were found statistically significant were entered in a logistic regression model in order to evaluate the probability of having multiple positive reactions. The modeling of a quantitative variable based on one or more qualitative and quantitative parameters was performed through linear regression. Multiple logistic regression was performed in order to evaluate the probability of having multiple positive reactions. The relative risk (RR), odds ratio (OR), and absolute risk (AR) were calculated.
2.4 Ethics Statement
All experiments were conducted in compliance with the international biomedical study stipulations, with reference to the Declaration of Helsinki of the World Medical Association. All participants gave their written informed consent after a detailed description of the study protocol. This study was approved by the ethical committee of the Medical School of the National and Kapodistrian University of Athens.
3 Results
3.1 Descriptive Statistics
3.1.1 Clinical and Demographic Data
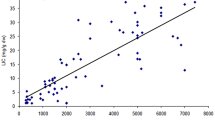
The demographic, clinical, and biochemical characteristics are summarized in Table 1 and the age frequency is presented in Fig. 1. On a total of 64 patients, the male to female ratio was 1:1. The patient’s clinical data with respect to gender are also presented in Table 2. From the total patient cohort, 60.93% (n = 40) received a monotherapy (nutritional supplementation and/or hormonal replacement) and 37.50% (n = 24) received multiple treatments, i.e., nutritional supplementation, hormonal replacement, etc. At the same time 43.75% (n = 28) received hormonal replacement therapy (HRT), while 54.68% did not receive HRT. Almost all patients received chelation therapy (n = 60, 93.75%), while only four were not in chelation therapy at the time of the study (n = 4, 6.25%). Twenty-three patients (35.93%) received also thyroxine treatment, while 60 patients (62.50%) did not receive any thyroxine. Data concerning thyroxine treatment were not available for one patient.
3.1.2 Thalassemia Genotype Frequencies
Patient’s TM genotypic frequencies are presented in Fig. 2. The IVSI-110/IVSI-110 (n = 15) mutation accounted for the 23.44% of all cases, the IVSI-110/CD39 mutation (n = 5) accounted for the 7.81% of all cases, and IVSI-6/IVSI-6 (n = 4), IVSI-110/IVSII-1 (n = 4), and CD39/IVSI-6 (n = 4) mutations accounted for the 18.75% of all cases. In total, the IVSI-110/IVSI-110, IVSI-110/CD39, IVSI-6/IVSI-6, IVSI-110/IVSII-1, and CD39/IVSI-6 mutations accounted for the 50% of all cases. The remaining mutation frequencies were IVSI/beta039 (n = 1, 1.56%), IVSII-745/CD8 (n = 1, 1.56%), CD39/IVSII-745 (n = 1, 1.56%), IVSI-6/delta-beta Lepore (n = 1, 1.56%), IVSI-110/FSC6 (n = 1, 1.56%), IVS1-110/IVSI-1 (n = 1, 1.56%), IVSI-110/delta-beta CORFU (n = 1, 1.56%), IVSI-6/IVSII-745 (n = 1, 1.56%), IVSI-1/IVSI-1 (n = 1, 1.56%), CD39/IVSI-1 (n = 1, 1.56%), CD39/CD39 (n = 1, 1.56%), delta-beta-sic/IVSI-110 (n = 1, 1.56%), IVSI-110/-44bp6del (n = 1, 1.56%), IVS1-110/-87 (n = 2, 3.13%), IVSI-1/CD6 (n = 2, 3.13%), IVSI-110/IVSI-1 (n = 2, 3.13%), IVSI-110/IVSII-745 (n = 3, 4.69%), IVS-110/-87 (n = 3, 4.69%), IVSI-110/CD 6 (n = 3, 4.69%), and IVSI-1/IVSII-1 (n = 3, 4.69%).
3.1.3 Iron Chelation Therapy
The present patient cohort received iron chelation therapy as part of its routine treatment. In particular, 60 patients (93.75%) received chelation therapy and 4 did not receive at the time of the study. From those patients, 25 (39.06%) received deferiprone in combination with deferoxamine mesylate, 23 patients (35.93%) received deferasirox as monotherapy, 1 patient (1.56%) received deferoxamine mesylate as monotherapy, 4 patients (6.25%) received deferasirox and deferoxamine mesylate, and 6 patients (9.37%) received deferiprone as monotherapy.
3.2 Statistical Analysis
No significant differences were found with respect to gender and nutritional supplementation, and no significant differences were found with respect to the administration of a monotherapy or not.
3.2.1 The Effect of Iron Chelation
All patients (except four as reported in the previous sections) received iron chelation therapy, and in particular, we have observed that patients receiving deferasirox in combination with deferoxamine mesylate manifested higher ferritin levels as compared to patients receiving deferasirox as monotherapy (p = 0.00043) (Fig. 3a) as well as patients receiving deferasirox in combination with deferoxamine mesylate manifested higher ferritin levels as compared to patients who received deferiprone as monotherapy (p = 0.0042) (Fig. 3b). Interestingly, we have found that patients receiving deferiprone in combination with deferoxamine mesylate manifested significantly lower levels of FT4 as compared to patients who received deferasirox as monotherapy (p = 0.0052) (Fig. 4).
3.2.2 The Effect of Hormone Replacement Therapy (HRT)
Patients who received HRT were significantly older in age as compared to patients that did not receive any HRT (p = 0.042) (Fig. 5a). At the same time patients who received HRT underwent marginally significant less frequently transfusion as compared to patients that did not (p = 0.078) (Fig. 5b). Interestingly, patients with no administration of HRT manifested significantly higher hematocrit levels as compared to those patients that did receive HRT (p = 0.014) (Fig. 5c). Finally, patients under HRT manifested lower T-score in the lumbar spine (p = 0.019) (Fig. 5d), while they did not manifest significant difference with respect to the hip T-score (p = 0.419) (Fig. 5d).
3.2.3 The Effect of Genotype
Additionally, we have investigated the effect of TM genotype in the clinical parameters of our patient cohort. Not many differences were observed with respect to the patients’ genotype in the estimated clinical parameters.
Significant differences were observed with respect to hematocrit and T-score. In particular, patients with the CD39/CD39 mutation manifested significantly higher hematocrit levels as compared to patients with the IVS1-110-87 mutation (p = 8.22 × 10−9) (Fig. 6a). Also, patients with the CD39/IVSI-1 mutations manifested higher hematocrit levels as compared to patients with the IVS1-110/-87 mutation (p = 8.22 × 10−9) (Fig. 6a). Interestingly, significant differences were observed with respect to the lumbar spine and hip T-scores. In particular, patients with the CD39/IVSI-1 mutation manifested higher lumbar spine T-score as compared with patients with the IVSI-110/IVSII-745 mutation (p = 8.7 × 10–9) (Fig. 6b). Further on, patients with the CD39/IVSI-1 mutation manifested similarly higher hip T-score levels as compared to patients with the IVSI-110/IVSII-745 (p = 8.00 × 10−9) (Fig. 6b). Finally, patients with the IVSI-110/CD6 mutation manifested higher hip T-score levels as compared to patients with the IVSI-110/IVSII-747 mutation (p = 8.00 × 10−9) (Fig. 6b).
3.3 Risk Assessment
Several of the previous results have been confirmed by the estimation of risk using the linear regression. In particular, no significant correlation between gender and HRT was observed (OR = 1.5, p = 0.45). Similarly, a marginal significant correlation was observed between gender and thyroxine treatment (OR = 0.34, p = 0.066), meaning that males were more probable to receive thyroxine supplementation as compared to females. Similarly, a significant correlation was observed between the presence of mono-treatment (as defined in the Sect. 2) and HRT. In particular, patients under monotherapy were less likely to receive HRT (OR = 4.5, p = 0.008). On the contrary, there was no significant correlation between monotherapy and thyroxine administration (OR = 0.39, p = 0.11), as well as there was no significant correlation between HRT and thyroxine administration (OR = 0.46, p = 0.19).
4 Discussion
As life expectancy of TM patients increases, comorbidities are becoming more apparent and evident. Prevention and early diagnosis of secondary pathologies are as important as the treatment of the established disease [17]. In the present study we have investigated the relationship between biochemical and clinical markers as well as genotypic characteristics of TM. Our study has highlighted several significant correlations between examined factors, which especially showed that mutations probably do affect the disease outcome.
One of the interesting findings was that iron chelation correlated with the ferritin levels. We have found that combination of iron chelation therapies resulted in higher ferritin levels as compared to iron chelation monotherapy. However, previous studies did not report significant differences in ferritin levels with respect to chelation therapies [18]. Yet, a recent study has shown that treatment of deferasirox vs. deferasirox and deferoxamine resulted in increased ferritin levels for the second treatment respectively [19]. Similarly, our results agreed with an older report, which showed that iron chelation combinatory therapy resulted in higher ferritin levels [20].
Interestingly, we have found that patients under HRT manifested lower hematocrit levels as compared to patients that did not receive HRT. This result indicates that HRT acts as a secondary parameter for the hematologic factors of TM patients. To the best of our knowledge, there are no previous reports concerning the role of HRT on hematocrit in TM patients. Yet, another interesting finding was the fact that patients under HRT manifested lower lumbar spine T-score levels as compared to patients with no HRT, as well as that hip T-score manifested no significant difference. Previous reports demonstrated that TM patients had unbalanced bone turnover with an increased resorption phase. However, it is possible that various and partially unknown pathogenetic factors could be involved in this bone remodeling imbalance. Factors such as an excessive iron accumulation in the cells of the bone marrow that may have altered or provoked defective bone remodeling and osteoblastic activity, desferrioxamine itself, which inhibits DNA synthesis, and low levels of the insulin-like growth factor 1 (IGF-1), a very important anabolic factor for bone, may account for the observed differences among patients [21]. However, it appears that bone remodeling improves only after HRT in combination with anti-osteoporotic treatment [22]. Toward that end, it is important for more studies to highlight the role of HRT and its combination with other treatments for bone remodeling. Also, in a previous study we have shown that patients with TM had a lower percentage of fractures as compared to previous reports [11, 12, 23]. In a recent report by Chen et al. (2018), it was found that cumulative fracture incidence was higher in thalassemia patients when compared to non-thalassemia, but the cohort used was transfusion-naïve patients [24]. On the other hand, Vogiatzi et al. (2006) revealed that fracture incidence in these patients is 12.1%, which is much higher than in our study [23].
One very interesting finding consisted of the role of identified mutation on hematocrit. To the best of our knowledge there are no previous reports on this fact. An older report, however, indicated that TM mutations do affect hematologic parameters, including hematocrit [25]. Furthermore, we have identified mutations that play a possible role in the T-scores of lumbar spine and hip, yet with no evident explanation. There are no other previous reports referring to this phenomenon and thus it consists an interesting subject for further investigation.
4.1 Study Limitations
A limitation of the current study is that the total number of patients included is small, and since the findings were interesting, more patients would be required to extract more solid conclusions. Another limitation is that few TM patients were already receiving treatment for osteoporosis, probably affecting the observed T-scores. Yet, anti-osteoporotic treatment was not to be interrupted due to the increased fracture risk of those patients [26].
4.2 Conclusions
To conclude, the current study showed that clinical parameters of TM patients correlate significantly with both biochemical factors and genotypical patient parameters. Our present study showed that there is a connection between genotype and phenotype as for example the identified relation between hematocrit and T-scores and TM-specific mutations. This connection indicates that there is still much more to learn about the role of mutations not only in the disease itself but also in the underlying comorbidities.
References
Cousens NE et al (2010) Carrier screening for beta-thalassaemia: a review of international practice. Eur J Hum Genet 18(10):1077–1083. https://doi.org/10.1038/ejhg.2010.90
Lee YK et al (2019) Recent progress in laboratory diagnosis of thalassemia and hemoglobinopathy: a study by the Korean Red Blood Cell Disorder Working Party of the Korean Society of Hematology. Blood Res 54(1):17–22. https://doi.org/10.5045/br.2019.54.1.17
Goh SH et al (2005) A newly discovered human alpha-globin gene. Blood 106(4):1466–1472. https://doi.org/10.1182/blood-2005-03-0948
Karponi G, Zogas N (2019) Gene therapy for beta-thalassemia: updated perspectives. Appl Clin Genet 12:167–180. https://doi.org/10.2147/tacg.s178546
Weatherall DJ, Clegg JB (1999) Genetic disorders of hemoglobin. Semin Hematol 36(4 Suppl 7):24–37
Weatherall DJ (1994) The thalassemias. In: Stamatoyannopoulos G, Nienhuis AW, Majerus PW, Varmus H (eds) The molecular basis of blood diseases. WB Saunders, Philadelphia, p 815
Otrock ZK et al (2006) Intravenous zoledronic acid treatment in thalassemia-induced osteoporosis: results of a phase II clinical trial. Ann Hematol 85(9):605–609. https://doi.org/10.1007/s00277-006-0136-y
Dresner Pollack R et al (2000) Bone mineral metabolism in adults with beta-thalassaemia major and intermedia. Br J Haematol 111(3):902–907
Molyvda-Athanasopoulou E et al (1999) Bone mineral density of patients with thalassemia major: four-year follow-up. Calcif Tissue Int 64(6):481–484
Voskaridou E et al (2006) Osteoporosis and osteosclerosis in sickle cell/beta-thalassemia: the role of the RANKL/osteoprotegerin axis. Haematologica 91(6):813–816
Tsartsalis AN et al (2018) The role of biphosphonates in the management of thalassemia-induced osteoporosis: a systematic review and meta-analysis. Hormones (Athens) 17(2):153–166. https://doi.org/10.1007/s42000-018-0019-3
Tsartsalis AN et al (2019) Bone metabolism markers in thalassemia major-induced osteoporosis: results from a cross-sectional observational study. Curr Mol Med 19(5):335–341. https://doi.org/10.2174/1566524019666190314114447
Spatz JM et al (2015) The Wnt inhibitor sclerostin is up-regulated by mechanical unloading in osteocytes in vitro. J Biol Chem 290(27):16744–16758. https://doi.org/10.1074/jbc.M114.628313
McClung MR et al (2014) Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med 370(5):412–420. https://doi.org/10.1056/NEJMoa1305224
van Dinther M et al (2013) Anti-Sclerostin antibody inhibits internalization of Sclerostin and Sclerostin-mediated antagonism of Wnt/LRP6 signaling. PLoS One 8(4):e62295. https://doi.org/10.1371/journal.pone.0062295
Cosman F et al (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375(16):1532–1543. https://doi.org/10.1056/NEJMoa1607948
Reynolds AW et al (2018) Comparison of osteoporosis pharmacotherapy fracture rates: analysis of a MarketScan((R)) claims database cohort. Int J Endocrinol Metab 16(3):e12104. https://doi.org/10.5812/ijem.12104
Bordbar M et al (2019) Effect of different iron chelation regimens on bone mass in transfusion-dependent thalassemia patients. Expert Rev Hematol 12(11):997–1003. https://doi.org/10.1080/17474086.2019.1662721
Eghbali A et al (2019) A 1-year randomized trial of deferasirox alone versus deferasirox and deferoxamine combination for the treatment of iron overload in thalassemia major. Transfus Apher Sci 58(4):429–433. https://doi.org/10.1016/j.transci.2019.03.021
Tanner MA et al (2007) A randomized, placebo-controlled, double-blind trial of the effect of combined therapy with deferoxamine and deferiprone on myocardial iron in thalassemia major using cardiovascular magnetic resonance. Circulation 115(14):1876–1884. https://doi.org/10.1161/circulationaha.106.648790
Soliman A et al (2014) Growth hormone – insulin-like growth factor-I axis and bone mineral density in adults with thalassemia major. Indian J Endocrinol Metab 18(1):32–38. https://doi.org/10.4103/2230-8210.126525
Bhardwaj A et al (2016) Treatment for osteoporosis in people with β-thalassaemia. Cochrane Database Syste Rev 3:CD010429. https://doi.org/10.1002/14651858.CD010429.pub2
Vogiatzi MG et al (2006) Prevalence of fractures among the Thalassemia syndromes in North America. Bone 38(4):571–575. https://doi.org/10.1016/j.bone.2005.10.001
Chen YG et al (2018) Risk of fracture in transfusion-naive thalassemia population: a nationwide population-based retrospective cohort study. Bone 106:121–125. https://doi.org/10.1016/j.bone.2017.10.016
Stefanis L et al (1994) Hematologic phenotype of the mutations IVS1-n6 (T→C), IVS1-n110 (G→A), and CD39 (C→T) in carriers of beta-thalassemia in Greece. Pediatr Hematol Oncol 11(5):509–517. https://doi.org/10.3109/08880019409141689
Allon R et al (2018) How to best predict fragility fractures: an update and systematic review. Isr Med Assoc J 20(12):773–779
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
A, T. et al. (2021). Genotypic and Clinical Analysis of a Thalassemia Major Cohort: An Observational Study. In: Vlamos, P. (eds) GeNeDis 2020. Advances in Experimental Medicine and Biology, vol 1339. Springer, Cham. https://doi.org/10.1007/978-3-030-78787-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-78787-5_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78786-8
Online ISBN: 978-3-030-78787-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)