Abstract
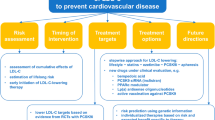
Multiple epidemiological, experimental, genetic, and interventional trials have unequivocally established that low-density lipoprotein (LDL) is a causal risk factor for the initiation and progression of atherosclerosis. LDL-cholesterol (LDL-C) is a key goal for primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD) according to international guidelines. To achieve this, the 2019 American College of Cardiology/American Heart Association Guideline on the primary prevention of cardiovascular disease emphasizes the importance of adopting a healthy dietary pattern. This guideline document suggests that rather than focus on specific micronutrients, it may be more important to consider dietary patterns for the prediction and mitigation of cardiovascular disease risk. Current evidence suggests that adopting a healthy dietary pattern that includes fruits, vegetables, whole grains, nuts, legumes and, optionally, low-fat dairy and fish, and reduced consumption of red and processed meats, is a useful approach to lowering LDL-C. Here, we briefly review the role of LDL in the genesis of atherosclerosis, the importance of lowering LDL-C for primary and secondary prevention of ASCVD, and approaches to LDL-C lowering with dietary interventions and medical therapy. This chapter also evaluates the current evidence of different dietary patterns such as the Dietary Approaches to Stop Hypertension (DASH) diet, the Mediterranean diet, and plant-based vegetarian diets, with a specific focus on their impact on LDL-C.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atherosclerotic cardiovascular disease
- Low-density lipoprotein-cholesterol
- Hypercholesterolemia
- Dietary fat
- Dietary pattern
Introduction
Low-Density Lipoprotein and Atherosclerosis
Atherosclerosis is a complex process that involves many factors, but the cholesterol-rich apolipoprotein B (apoB)-containing lipoproteins have emerged as the chief initiating and driving factor. Cholesterol and triglycerides, water-insoluble lipids, require protein-containing complexes called lipoproteins for solubilization in the aqueous plasma and for transport to tissue. ApoB is the major structural protein (apolipoprotein) found on atherogenic lipoproteins and serves as the scaffold for lipidation and as a ligand for receptor binding. The five major atherogenic lipoproteins include chylomicron remnants, very-low-density lipoprotein, intermediate-density lipoprotein, low-density lipoprotein (LDL), and lipoprotein(a). Although LDL is the principle atherogenic lipoprotein, largely due to its relatively high plasma concentrations relative to other lipoproteins, other apoB-containing lipoproteins (up to about 70 nm in diameter) also play a role in the initiation and progression of atherosclerosis [1]. LDL particles penetrate the arterial endothelial cell lining, especially in the presence of endothelial dysfunction, and enter the subendothelial space where they interact with positively charged intimal proteoglycans to become retained in the arterial wall [2]. The subendothelial retention of apoB-containing lipoprotein particles leads to a complex interplay between metabolic and inflammatory processes that leads to the initiation of an atheroma. Early atherogenesis can be impacted by many factors including hyperlipidemia, lipoprotein influx, lipoprotein modification, turbulent blood flow, and alterations in the endothelium, smooth muscle cells, and matrix. According to the response-to-retention hypothesis of early atherogenesis, lipoprotein retention is an absolute prerequisite for lesion development and appears to be sufficient in the majority of circumstances to provoke otherwise normal cellular and matrix elements to participate in a stream of events leading to atherosclerosis [3].
Importance of Lowering LDL Cholesterol for Primary Prevention of Cardiovascular Disease
Data from numerous observational studies suggest that, even in the absence of other risk factors, severe hypercholesterolemia (e.g., LDL-cholesterol [LDL-C] ≥ 190 mg/dL) is associated with significantly increased risk for atherosclerotic cardiovascular disease (ASCVD) [4]. One of the earlier trials evaluating the efficacy of decreasing cholesterol in reducing the risk of coronary heart disease (CHD) was the LRC-CCPT (Lipid Research Clinics Coronary Primary Prevention Trial), including 3806 asymptomatic middle-aged men. The study revealed that treatment with bile acid sequestrant cholestyramine was associated with a 20% reduction in LDL-C with an associated 19% reduction in the incidence of CHD [5]. In the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), treatment with lovastatin reduced LDL-C by 25% compared to placebo and reduced the incidence of first acute major coronary events after 5.2 years [6]. The (HOPE)-3 (Heart Outcomes Prevention Evaluation) trial studied the effect of statins in 12,705 intermediate-risk, ethnically diverse participants without cardiovascular disease [7]. Rosuvastatin reduced LDL-C level by 27% compared to the placebo at 5 years. Treatment with rosuvastatin resulted in a 24% reduction in the primary composite outcome of death from CVD, non-fatal myocardial infarction, or non-fatal stroke. The JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial, included 17,802 men and women free of cardiovascular disease at baseline with LDL-C levels <130 mg/dL and high-sensitivity C-reactive protein levels ≥2.0 mg/L and randomized them to rosuvastatin 20 mg daily vs. placebo. Rosuvastatin reduced LDL-C levels by 50% and significantly reduced the incidence of a first major cardiovascular event by 44% [8]. It is clear from the evidence that there is a significant benefit associated with LDL-C lowering in the primary prevention of ASCVD (Table 13.1).
Importance of Lowering LDL Cholesterol for Secondary Prevention of Cardiovascular Disease
Many large clinical trials assessed the impact of LDL-C lowering in patients with known CVD. In the 4S (Scandinavian Simvastatin Survival Study), 4444 patients with known CHD were randomly assigned to simvastatin (10–40 mg daily) or placebo [9]. At the end of 5.4 years, simvastatin reduced LDL-C level by 35%. Treatment with simvastatin resulted in a 42% reduction in coronary mortality and a 35% reduction in major coronary events. More recently, non-statin therapies were evaluated in patients with ASCVD in the IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). This study enrolled 18,144 patients with a recent acute coronary syndrome (within 10 days of enrollment) and randomly assigned participants to receive simvastatin 40 mg plus ezetimibe 10 mg or simvastatin 40 mg daily plus placebo. The median time–weighted average LDL-C level during the study was 53.7 mg/dL in the simvastatin/ezetimibe group as compared with 69.5 mg/dL in the simvastatin monotherapy group [10]. At the conclusion of the study, there was a 6.5% proportional reduction in major cardiovascular events (cardiovascular death, non-fatal MI, unstable angina requiring hospitalization, coronary revascularization ≥30 days after randomization, or non-fatal stroke) with combination therapy compared to simvastatin/placebo. The study concluded that reducing LDL-C to levels below previous targets provided additional benefit (e.g., even lower LDL-C is even better). The discovery of proprotein convertase subtilisin/kexin type 9 (PCSK9) and the recent development and approval of the PCSK9 inhibitors have transformed our understanding of lipoprotein metabolism and our ability to manage patients with hypercholesterolemia and/or ASCVD. The FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) trial assessed the efficacy of evolocumab when added to statin therapy in patients with clinically evident ASCVD [11]. In total, 27,564 participants with ASCVD and LDL-C levels of 70 mg/dL or higher who were on optimized statin therapy were randomly assigned to receive evolocumab (either 140 mg every 2 weeks or 420 mg monthly) or placebo. After a median follow-up of 2.2 years, treatment with evolocumab, as compared with placebo, led to a reduction in LDL-C from a median baseline value of 92–30 mg/dL corresponding to 59% reduction. There was a significant 15% reduction in the risk of the primary composite endpoint of cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina, or coronary revascularization with evolocumab treatment above and beyond background optimal medical therapy. Several meta-analyses have also suggested similar cardiovascular benefits with an intensive lowering of LDL-C in patients with ASCVD [12,13,14]. In conclusion, the totality of the evidence indicates that reducing plasma LDL-C level is an integral component of secondary prevention of ASCVD (Table 13.2).
Impact of Diet on LDL-C
Dietary Fat and LDL
The relationship between macronutrient intake in the diet and plasma LDL-C concentrations is well known. Historically, there was an emphasis on the reduction of total dietary fat intake. In aggregate, clinical studies have failed to reveal a favorable impact on CVD by taking this approach [15]. However, it is now understood that the specific type of fat is far more critical in influencing plasma lipids and CVD outcomes [16].
Dietary Cholesterol
The main sources of dietary cholesterol are egg yolks. The other major sources include dairy products, shrimp, beef, pork, and poultry. A systematic review and meta-analysis of randomized controlled trials exploring the quantitative effect of egg consumption on serum lipid concentrations demonstrated that compared with non-egg-consumers, consumption of eggs increased LDL-C by 5.5 mg/dL [17]. However, the consumption of eggs also increased HDL-C, and there was no effect on the LDL-C: HDL-C ratio. A meta-analysis of 13 randomized controlled trials investigating the impact of dietary cholesterol interventions on serum LDL-C showed a significant increase in LDL-C when comparing intervention with control doses of dietary cholesterol [18]. The “National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia” recommend limiting cholesterol intake to <200 mg/day to maintain a cardioprotective eating pattern [19]. It is important to note that intestinal absorption of cholesterol is variable with both hyper- and hypo-absorbers. Some individuals show little or no increases in LDL-C in response to a higher intake of dietary cholesterol, while others show responses well above the average [19, 20]. Dietary Guidelines for Americans (2015–2020) do not limit the consumption of dietary cholesterol to 300 mg per day in contrast to the 2010 Dietary Guidelines [21]. However, the guideline suggests that limiting dietary cholesterol is an integral part of building a healthy eating pattern. It is particularly important that individuals with inherited hypercholesterolemia (e.g., familial hypercholesterolemia) continue to limit dietary cholesterol intake.
Saturated Fatty Acids
High concentrations of saturated fatty acids are found in red meat, dairy products, and plant-derived products such as palm kernel oil and coconut oil. Saturated fats increase LDL-C through different mechanisms (Fig. 13.1). However, issues related to saturated fats and their impacts on LDL-C are considerably more nuanced. The LDL-C raising effect of saturated fatty acids progressively increases as the chain length of saturated fat diminishes. Specifically, lauric acid (C12:0) is more potent than myristic acid (C14:0) and palmitic acid (C16:0) in increasing LDL-C. On the other hand, lauric acid has also been shown to increase high-density lipoprotein (HDL)-cholesterol (HDL-C), though the clinical significance of this effect is unclear [22]. The DELTA (Dietary Effects on Lipoproteins and Thrombogenic Activity) study compared the average American diet containing 15% of total calories from saturated fat to a low saturated fat diet containing 6.1% of total calories from saturated fat. The lower saturated fat diet was associated with an 11% reduction in LDL-C as compared to the typical American diet [23]. However, the evidence suggests that the effect of saturated fatty acids on LDL-C is modified by the food source within which they are consumed [24]. A randomized controlled trial of 49 participants demonstrated that cheese consumption was associated with lower LDL-C when compared with butter intake of equal fat content [25]. A meta-analysis of 36 randomized control trials of red meat consumption in comparison with other diets exhibited no significant difference in plasma LDL-C concentration [26]. Similarly, evidence has suggested that a higher intake of processed meat is associated with a neutral or increased risk of CVD, while dairy products have a neutral or beneficial effect on CVD [16]. Evidence, as provided in these examples, has called into question the recommendation to keep total saturated fat consumption below 10% of total calories. In fact, many experts suggest evaluating the quality of dietary nutrients, components, and patterns rather than a rigid reliance on absolute proportions of macronutrients [27].
Polyunsaturated Fatty Acids
Omega-3 (ω-3) and Omega-6 (ω-6) fatty acids are polyunsaturated fatty acids (PUFAs) as they contain more than one cis double bond in the long-carbon fatty acid chain. Unlike saturated and monounsaturated fats, humans cannot synthesize PUFA because they lack desaturase enzymes necessary to insert a cis double bond at the n-3 and n-6 positions of a fatty acid. Hence, PUFA are considered essential fatty acids. Dietary ω-3 PUFA include eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and α-linolenic acid (ALA). Oily fish such as herring, salmon, sardines, oysters, and tuna are the richest dietary sources of EPA and DHA. Flaxseed, chia seed, and walnuts are the primary dietary sources of ALA. Most studies investigating the effect of ω-3 PUFA on plasma lipids are notable for the consistent triglyceride-lowering properties of EPA and DHA, particularly at high doses (4 grams per day). On the other hand, ω-3 PUFA have shown either no effect or a slight increase in LDL-C [28]. A 2018 Cochrane systematic review of 79 RCTs revealed no beneficial effect of EPA, DHA, or ALA on LDL-C [29]. However, most studies demonstrated an increase in mean LDL particle size without an increase in LDL particle number [29]. This shift toward large LDL particles may confer cardiovascular benefit, as small dense LDL (sdLDL) particles have relatively greater atherogenic potential [30]. Mechanisms by which sdLDL may facilitate atherogenesis are illustrated in Fig. 13.2.
The main dietary ω-6 PUFA are linoleic acid (LA) and arachidonic acid (AA). LA is found in vegetable oils such as safflower oil, sunflower oil, and corn oil, as well as nuts and seeds. AA is present in small amounts in eggs , meat, and poultry. A meta-analysis of 27 RCTs suggested a beneficial effect of LA on LDL-C [31]. A Cochrane systematic review of 19 RCTs, including 6461 participants, demonstrated that replacing dietary saturated fatty acids with ω-6 PUFA lowered total blood cholesterol. Still, there was no evidence of LDL-C reducing benefits [32].
Monounsaturated Fatty Acids
In contrast to PUFA , monounsaturated fatty acid (MUFA) contains only one cis double bond. The primary source of MUFA includes dairy products, red meat, and plant-based oil, including olive oil. MUFA is also found in avocados, peanut butter, and other nuts and seeds. An RCT of 58 participants tested the effect of replacing saturated fat with MUFA or PUFA [33]. At the end of the study period, the serum LDL-C level decreased by 18% in those on the MUFA diet and by 13% in those on the PUFA diet. The study concluded that a diet rich in MUFA was as efficacious as a diet rich in PUFA in lowering LDL-C. In the OmniHeart (Optimal Macronutrient Intake Trial to Prevent Heart Disease) study, replacing saturated fat with MUFA led to a significant decrease in LDL-C [34]. A similar reduction in LDL-C was observed in a meta-analysis of 27 trials investigating the replacement of saturated fat with MUFA [31].
Trans Fatty Acids
There are two main sources of trans fatty acids (TFA) . Naturally occurring TFA can be found in small amounts from meat and dairy products. However, the major dietary source is synthetic TFA found in processed foods. The partial hydrogenation of unsaturated fat found in vegetable oil leads to the formation of TFA. This process is used by the food industry to increase the shelf-life of processed foods and to enhance flavor. A meta-analysis of 32 clinical trials demonstrated that a high intake of industrial TFA lead to increases in serum LDL-C [35]. Another meta-analysis of 12 randomized controlled trials on isocaloric replacement of saturated fat or cis unsaturated fats with TFA revealed that the consumption of TFA increases LDL-C as compared with the consumption of an equal number of calories from saturated or cis unsaturated fats [36]. Given their harmful effects on atherogenic lipid levels, systemic inflammation, and ASCVD, the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease recommended minimizing the consumption of TFA [37].
In summary, dietary cholesterol is associated with increased LDL-C. The effect of saturated fat on LDL-C is modulated by the food source. EPA and DHA may not reduce LDL-C but could confer CVD protection through increasing LDL size and triglyceride lowering. Replacement of saturated fat with MUFA seems to have a beneficial effect on LDL-C. The consumption of TFA has been consistently shown to increase LDL-C (Table 13.3).
Dietary Sugars and LDL
The major source of added sugar among US adults aged 20 and overcomes from sugar-sweetened beverages such as fruit-flavored drinks, sodas, and sports drinks [38]. Low-calorie sweetened beverages and 100% fruit juices are frequently considered as a healthier alternative to sugar-sweetened beverages. A cross-sectional analysis from the National Health and Nutrition Examination Survey (NHANES) demonstrated that intake of added sugar was positively associated with higher LDL-C [39]. A prospective cohort of the Coronary Artery Risk Development in Young Adults (CARDIA) Study demonstrated that higher consumption of sugar-sweetened beverages was associated with increased risk of high LDL-C at 20 years [40]. A longitudinal study from the FOS (Framingham Offspring Study) and GEN3 (Generation Three) cohorts examined the association of sugar-sweetened beverages, low-calorie sweetened beverages, and fruit juice consumption with changes in the lipid profile [41]. The study demonstrated that the regular consumption of sugar-sweetened beverages was associated with decreased HDL-C and increased triglycerides. Moreover, recent low-calorie sweetened beverage consumption was associated with increased LDL-C. Sugar-sweetened beverages are sweetened primarily with fructose, sucrose, or high-fructose corn syrup (HFCS) [42]. A meta-analysis of 19 controlled feeding trials indicated that there was a dose–response relationship between fructose consumption and LDL-C [43]. Fructose intake >100 g/day significantly increased LDL-C by 11.6 mg/dL. A 2-week parallel-arm trial, including a total of 187 participants, demonstrated that consumption of beverages containing 10%, 17.5%, or 25% of energy requirements from HFCS produced significant linear dose-response increase fasting LDL cholesterol [44]. Hence, the 2019 ACC/AHA Guideline and the Dietary Guidelines for Americans (2015–2020) recommend minimizing or entirely eliminating sugar-sweetened beverage consumption [21, 37].
Dietary Fibers and LDL
Dietary fibers represent the indigestible part of plant foods. Dietary fibers are classified based on their solubility in water as soluble fibers or insoluble fibers. They are mainly found in vegetables, fruits, oats, nuts, barley, and legumes. Dietary fibers are also available as supplements that contain psyllium, methylcellulose, and wheat dextrin. A meta-analysis of 67 randomized controlled trials evaluating the effect of soluble fibers on plasma lipids found that soluble fiber consumption of 1 g/day was associated with approximately a 2 mg/dL reduction of LDL-C [45]. A randomized control trial of 68 patients evaluated the LDL-C lowering effect of psyllium added to simvastatin [46]. The study found that the addition of 15 g of daily psyllium fiber to 10 mg simvastatin/day achieved a similar 36% LDL-C reduction to that achieved with 20 mg simvastatin/day. A more recent meta-analysis of 28 randomized controlled trials evaluating the effects of psyllium on LDL-C found that the supplementation of 10.2 g/day of psyllium reduced the LDL-C by an average of 12.9 mg/dL. The National Lipid Association (NLA) and the 2016 ACC Expert Consensus Decision Pathway (ECDP), recommend the incorporation of soluble dietary fiber as a dietary adjunct for lowering LDL-C in patients with dyslipidemia [19, 47].
Phytosterols and LDL
Plant sterols and plant stanols are commonly referred to as phytosterols (plant-based sterols) that are similar in structure to cholesterol. Phytosterols are found in foods of plant origin, including vegetable oils, nuts, whole grains, seeds, and legumes. There are also dietary supplements fortified with phytosterols available commercially. Numerous studies have demonstrated the beneficial effects of the consumption of foods enriched with free or esterified forms of phytosterols on LDL-C [48, 49]. A meta-analysis of 124 studies examining the LDL-C lowering effect of phytosterols demonstrated that the consumption of 0.6–3.3 g/day of phytosterols was associated with a 6–12% reduction in LDL-C in a dose-response fashion [50]. In one meta-analysis including 15 trials, phytosterols consumption of 1.8–6 g/day in patients treated with statins was associated with 11.7 mg/dL lower LDL-C compared with a statin alone [51]. The NLA and the 2016 ACC ECDP, recommend considering the use of phytosterols as a part of lifestyle modification to reduce LDL-C for primary and secondary prevention of ASCVD [19, 47].
Dietary Patterns and LDL
The 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease placed a significant emphasis on the benefits of a healthy diet [37]. In the following section, we will review some of the dietary patterns associated with improvements in the lipid profile, including LDL-C.
DASH Diet
The DASH (Dietary Approaches to Stop Hypertension) trial was an outpatient controlled feeding study including 459 participants who were randomized to either a control dietary pattern, similar to an average American diet or two experimental diets: FV (fruits, vegetable) diet or the DASH diet [52]. The FV dietary pattern contained more fruit, vegetables, and whole grains and fewer sweets but had macronutrient content similar to that of the control diet. The DASH diet was a combination of dietary patterns, and compared with the control and FV diet, it was higher in protein and calcium and lower in saturated fat, total fat, and cholesterol. At the end of 8 weeks, the DASH diet, compared with the control diet, led to a significantly lower mean LDL-C level (−10.7 mg/dL), which represented a 9% net reduction [53]. The DASH-Sodium trial was a multicenter, randomized feeding trial, where participants were randomly assigned to a typical American control diet or the DASH diet, each prepared with three levels of sodium [54]. The study revealed that compared with the control diet, the DASH diet significantly lowered LDL-C. Further improvement in LDL-C was found when part of the carbohydrate content in the DASH diet was replaced with either unsaturated fat or protein in the OmniHeart trial [34]. The OmniHeart was a randomized, three-period crossover design comparing the effect of three healthful diets on serum lipids and blood pressure. The three diets included a carbohydrate-rich diet, similar to the DASH diet, a protein-rich diet, and a diet rich in unsaturated fat. The study demonstrated that the DASH diet decreased mean LDL-C by an absolute 11.6 mg/dL from baseline. Compared with the DASH diet, the protein-rich diet, but not the diet rich in unsaturated fat, significantly lowered LDL-C levels.
Mediterranean Diet
The Mediterranean dietary pattern represents the dietary habits of populations bordering the Mediterranean Sea. While there is considerable regional variation in the Mediterranean diet, perhaps more appropriately referred to as the Mediterranean pattern, there are some general similarities found in this dietary pattern. This diet is enriched in fruits, vegetables, complex carbohydrates, including whole grains, nuts, and seeds [55, 56]. Olive oil is a principal source of fat in this diet. Also, the typical Mediterranean diet is low in animal fat and simple sugars. The Med-RIVAGE (Mediterranean Diet, Cardiovascular Risks, and Gene Polymorphisms) study, including 212 participants with moderate CVD risk, demonstrated a beneficial effect on LDL-C with the Mediterranean-type diet [57]. The Indo-Mediterranean Diet Heart Study randomized 1000 patients with angina pectoris, myocardial infarction, or surrogate risk factors for CVD to receive either a diet rich in whole grains, fruits, vegetables, walnuts, and almonds or the Step 1 NCEP (National Cholesterol Education Program) diet. At the end of 2 years, both groups demonstrated a significant reduction in LDL-C. However, the effect was greater in the Mediterranean diet group [58]. A recent meta-analysis including 30 randomized control trials, including 12,461 participants comparing the Mediterranean dietary intervention versus usual care or another dietary intervention (e.g., low-fat, the traditional diet of that country, national recommendations/disease-specific guidance, and vegetarian), demonstrated that the Mediterranean diet produced small beneficial or no effect on LDL-C levels [59]. The PREDIMED (Prevención con Dieta Mediterránea) study is the largest randomized control study to evaluate the health effects of the Mediterranean diet on 7447 subjects at high risk for cardiovascular disease [60]. The participants were assigned to one of three diets: a Mediterranean diet supplemented with extra-virgin olive oil, a Mediterranean diet supplemented with mixed nuts, or a control diet (low-fat diet). The original trial, which was published in 2013, demonstrated a beneficial effect of the Mediterranean diet supplemented with extra-virgin olive oil or nuts on major cardiovascular events. However, it was retracted after identifying protocol deviations, including enrollment of household members without randomization, assignment to a study group without randomization of some participants at 1 of 11 study sites, and apparent inconsistent use of randomization tables at another site. After the omission of 1588 participants whose study-group assignments were known or suspected to have departed from the protocol, the results did not change [61]. A random subsample of 210 individuals from the PREDIMED study revealed that the Mediterranean diet supplemented with extra-virgin olive oil led to a statistically significant absolute 10.5 mg/dL decrease of LDL-C level. Moreover, measures of LDL oxidation and LDL particle size were improved in participants randomized to the Mediterranean diet supplemented with extra-virgin olive oil compared to the low-fat diet [62]. The Mediterranean diet supplemented with nuts exhibited similar trends but did not reach statistical significance.
Plant-Based Vegetarian Diet
There are many variations to the vegetarian diet, including the pescovegetarian diet (seafood with or without eggs and dairy), lactovegetarian diet (dairy), lacto-ovo-vegetarian diet (eggs and dairy), and vegan diet (no animal products). A plant-based vegetarian diet incorporates vegetables and fruits as well as whole grains, beans, legumes, nuts, and seeds. The Oxford Vegetarian Study was an observational study of 11,040 participants residing in the United Kingdom and revealed that vegans exhibited lower LDL-C compared to meat-eaters [63]. One of the earliest trials to examine the impact of lifestyle changes on the progression of coronary atherosclerosis was the Lifestyle Heart Trial, which was a randomized controlled trial conducted from 1986 to 1992, including 48 patients with moderate to severe coronary heart disease [64]. The participants in the experimental group were prescribed an intensive lifestyle program that included adhering to a vegetarian diet in addition to other lifestyle modifications (smoking cessation, exercise, and stress management). After 1 year, LDL-C levels decreased by 40% in the experimental group compared to a 1.2% decrease in LDL-C in the control group. In a crossover experiment, Cooper et al. examined the effects of a lactovegetarian diet in 15 healthy, nonsmoking physicians and medical students [65]. The participants were randomly assigned to a low-saturated fat vegetarian diet or a “typical American diet.” Compared to the omnivorous diet, participants consuming the vegetarian diet experienced a 14.7% decrease in LDL-C. In the GEICO (Government Employees Insurance Company) study, 291 participants with a body mass index (BMI) ≥25 kg/m2 and/or a previous diagnosis of Type 2 diabetes were randomized to either a low-fat vegan diet or a group without any dietary changes [66]. After 18 weeks, LDL-C was reduced by 8.1 mg/dL for the participants consuming a low-fat vegan diet compared with only 0.9 mg/dL reduction in LDL-C in the control group. Another randomized control trial investigated the impact of a low-fat vegan diet on cardiovascular risk factors in 99 individuals with Type 2 diabetes [67]. The participants were randomized to a low-fat, low-glycemic index vegan diet or to the American Diabetes Association (ADA) diet. After 22 weeks, the participants consuming a vegan diet experienced a 21.2% reduction in LDL-C compared to a 10.7% reduction in those consuming the ADA diet. It is important to note that the benefits of the vegetarian diet could be due to specific components of the diet with lipid-lowering properties. The “portfolio” diet is a vegan diet with emphasis on plant sterols, soy foods, viscous fibers, and almonds. In a randomized control trial of 25 individuals with hyperlipidemia, participants were randomized to either a portfolio diet or a lacto-ovo-vegetarian diet [68]. At the end of the trial, LDL-C was reduced by 12.1% in the participants assigned to a lacto-ovo-vegetarian diet while the portfolio diet led to a 35% reduction in LDL-C. Another study examining the impact of the portfolio diet enrolled 45 hyperlipidemic individuals to determine whether the portfolio diet leads to cholesterol reduction similar to statins [69]. The participants were randomly assigned to either a low-fat diet, a low-fat diet plus lovastatin, or a vegetarian portfolio diet. Interestingly, the portfolio diet group and the low-fat diet plus statin group demonstrated significant and comparable reductions in LDL-C. A 2017 meta-analysis, including 49 studies (30 observational studies and 19 clinical trials), demonstrated that compared to the omnivorous diet, the plant-based vegetarian diet lowered LDL-C by 15–30% [70]. The CARDIVEG (Cardiovascular Prevention With Vegetarian Diet) was the first randomized control trial assessing the effects of a lacto-ovo-vegetarian diet compared to a Mediterranean diet on CVD risk factors [71]. After 3 months of dietary intervention, compared with the Mediterranean diet, the vegetarian diet led to a significant reduction in LDL-C. The plant-based vegetarian diets may reduce serum LDL-C through multiple mechanisms [72]. The plant-based vegetarian diet, including fruits, vegetables, whole grains, legumes, nuts, and various soy products, contain a number of phytochemicals including plant sterols and/or stanols, phytoestrogen, and flavonoids [73]. The beneficial effect of plant sterols/stanols and flavonoids is likely related to inhibition of cholesterol absorption in the small intestine [74]. The phytoestrogen content of soy facilitates plasma LDL-C reduction through an increase in the excretion of bile acids with concomitant increased LDL receptor expression on hepatocytes [75]. Phytoestrogens can also inhibit the oxidation of LDL [76].
Ketogenic Diet
The ketogenic diet is a high-fat, low-carbohydrate diet that has generated a lot of interest and has led to a great deal of debate, especially regarding its safety and long-term effects on cardiovascular health [77]. There are many versions of a ketogenic diet with a different ratio of macronutrients. In general, the typical ketogenic diet consists of 70–80% calories from fat, 10–20% calories from protein, and 5–10% from carbohydrate. The ketogenic diet causes the body to break down fat into ketones, which becomes the primary source of energy. The hypothesized favorable mechanisms of ketosis include appetite suppressant action of the ketone bodies, increased lipolysis, and greater metabolic efficiency in consuming fats [78]. A randomized control trial of 30 normal-weight, healthy individuals, assessed the impact of the ketogenic diet on LDL-C. The participants were assigned to either a ketogenic diet or a habitual diet for 3 weeks. There was a 44% increase in LDL-C among the participants allocated to the ketogenic diet at the end of 3 weeks, while LDL-C remained unchanged in the control group [79]. Similarly, several meta-analyses also demonstrated deleterious effects on plasma LDL-C associated with the ketogenic diet [80,81,82].
Intermittent Fasting
Intermittent fasting (IF) includes different eating patterns such as time-restricted feeding, alternate-day fasting, and 5:2 intermittent fasting (fasting 2 days each week) [83]. The exact underlying mechanism of the potentially beneficial effects of IF is not entirely understood but may involve bolstering cellular stress resistance and metabolic switching [84]. In a single-arm, paired-sample trial, 19 participants with metabolic syndrome underwent 10 h of time-restricted feeding for 12 weeks [85]. At the end of 12 weeks, participants observed a significant reduction in LDL-C (−12 ± 19 mg/dL [−11%], p = 0.016), and this effect was independent of weight loss. Another study examined the effect of alternate-day fasting on CVD risk factors in obese individuals. The study enrolled 16 individuals who completed the 10-week trial consisting of three phases: (1) a 2-week control phase, (2) a 4-week weight loss/alternate-day fasting controlled food intake phase, and (3) a 4-week weight loss/alternate-day fasting self-selected food intake phase. At the study conclusion, there was a 25% reduction in LDL-C. Several other studies have also demonstrated the LDL-C lowering effect of IF [86,87,88].
Conclusion
LDL is in the causal pathway of ASCVD, and, as such, it is the primary target of therapy in all major international guidelines. Lifestyle modifications, including the adoption of a healthy dietary pattern, remain paramount in the prevention and management of ASCVD. The focus has shifted from restricting the total fat intake to a focus on the quality of specific types of fat as a means to reduce LDL-C and mitigate the risk of ASCVD. In general, the effect of dietary fat on LDL-C is complex. Moreover, humans consume food that contains different types and ratios of macronutrients like fats rather than eating in isolation. In recognition of the complexity of the impact of isolated nutrients on LDL-C, it is crucial to focus on a healthy dietary pattern. The totality of the evidence suggests that any dietary pattern that incorporates more vegetables, fruits, whole grains, and nuts optimizes LDL-C lowering and is associated with improved cardiovascular outcomes (Table 13.4).
References
Boren J, Williams KJ. The central role of arterial retention of cholesterol-rich apolipoprotein-B-containing lipoproteins in the pathogenesis of atherosclerosis: a triumph of simplicity. Curr Opin Lipidol. 2016;27(5):473–83.
Tabas I, Williams KJ, Boren J. Subendothelial lipoprotein retention as the initiating process in atherosclerosis - update and therapeutic implications. Circulation. 2007;116(16):1832–44.
Williams KJ, Tabas I. The response-to-retention hypothesis of early atherogenesis. Arterioscler Thromb Vasc Biol. 1995;15(5):551–61.
Perak AM, Ning H, de Ferranti SD, Gooding HC, Wilkins JT, Lloyd-Jones DM. Long-term risk of atherosclerotic cardiovascular disease in US adults with the familial hypercholesterolemia phenotype. Circulation. 2016;134(1):9–19.
The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251(3):351–64.
Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279(20):1615–22.
Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2021–31.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207.
Pedersen TR, Kjekshus J, Berg K, Haghfelt T, Faergeman O, Thorgeirsson G, et al. Randomized trial of cholesterol-lowering in 4444 patients with coronary-heart-disease – the Scandinavian Simvastatin Survival Study (4s). Lancet. 1994;344(8934):1383–9.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–22.
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart J, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425–35.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Mills EJ, O’Regan C, Eyawo O, Wu P, Mills F, Berwanger O, et al. Intensive statin therapy compared with moderate dosing for prevention of cardiovascular events: a meta-analysis of > 40 000 patients. Eur Heart J. 2011;32(11):1409–U138.
Harcombe Z, Baker JS, DiNicolantonio JJ, Grace F, Davies B. Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis. Open Heart. 2016;3(2):e000409.
Siri-Tarino PW, Chiu S, Bergeron N, Krauss RM. Saturated fats versus polyunsaturated fats versus carbohydrates for cardiovascular disease prevention and treatment. Annu Rev Nutr. 2015;35:517–43.
Rouhani MH, Rashidi-Pourfard N, Salehi-Abargouei A, Karimi M, Haghighatdoost F. Effects of egg consumption on blood lipids: a systematic review and meta-analysis of randomized clinical trials. J Am Coll Nutr. 2018;37(2):99–110.
Berger S, Raman G, Vishwanathan R, Jacques PF, Johnson EJ. Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis. Am J Clin Nutr. 2015;102(2):276–94.
Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6):S1–S122.
Griffin JD, Lichtenstein AH. Dietary cholesterol and plasma lipoprotein profiles: randomized-controlled trials. Curr Nutr Rep. 2013;2(4):274–82.
US Department of Health and Human Services; US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th ed. Washington, DC: US Dept of Health and Human Services; December 2015. http://www.health.gov/DietaryGuidelines. Accessed Aug 2020.
Mensink RP, Zock PL, Kester ADM, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77(5):146–55.
Ginsberg HN, Kris-Etherton P, Dennis B, Elmer PJ, Ershow A, Lefevre M, et al. Effects of reducing dietary saturated fatty acids on plasma lipids and lipoproteins in healthy subjects: the DELTA Study, protocol 1. Arterioscler Thromb Vasc Biol. 1998;18(3):441–9.
Astrup A, Dyerberg J, Elwood P, Hermansen K, Hu FB, Jakobsen MU, et al. The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010? Am J Clin Nutr. 2011;93(4):684–8.
Hjerpsted J, Leedo E, Tholstrup T. Cheese intake in large amounts lowers LDL-cholesterol concentrations compared with butter intake of equal fat content. Am J Clin Nutr. 2011;94(6):1479–84.
Guasch-Ferre M, Satija A, Blondin SA, Janiszewski M, Emlen E, O’Connor LE, et al. Meta-analysis of randomized controlled trials of red meat consumption in comparison with various comparison diets on cardiovascular risk factors. Circulation. 2019;139(15):1828–45.
Freeland-Graves JH, Nitzke S, Academy of Nutrition and Dietetics. Position of the academy of nutrition and dietetics: total diet approach to healthy eating. J Acad Nutr Diet. 2013;113(2):307–17.
Oscarsson J, Hurt-Camejo E. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and their mechanisms of action on apolipoprotein Bcontaining lipoproteins in humans: a review. Lipids Health Dis. 2017;16(1):149.
Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018;7:CD003177.
Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43(9):1363–79.
Mensink RP, Katan MB. Effect of dietary fatty acids on serum lipids and lipoproteins. A meta-analysis of 27 trials. Arterioscler Thromb. 1992;12(8):911–9.
Hooper L, Al-Khudairy L, Abdelhamid AS, Rees K, Brainard JS, Brown TJ, et al. Omega-6 fats for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018;7:CD011094.
Mensink RP, Katan MB. Effect of a diet enriched with monounsaturated or polyunsaturated fatty acids on levels of low-density and high-density lipoprotein cholesterol in healthy women and men. N Engl J Med. 1989;321(7):436–41.
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids – results of the OmniHeart randomized trial. JAMA. 2005;294(19):2455–64.
Liska DJ, Cook CM, Wang DD, Gaine PC, Baer DJ. Trans fatty acids and cholesterol levels: an evidence map of the available science. Food Chem Toxicol. 2016;98:269–81.
Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Medical progress – trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354(15):1601–13.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;140(11):E563–E95.
Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. youth, 2011–2014. NCHS Data Brief. 2017(271):1–8.
Welsh JA, Sharma A, Cunningham SA, Vos MB. Consumption of added sugars and indicators of cardiovascular disease risk among US adolescents. Circulation. 2011;123(3):249–57.
Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR, Popkin BM. Drinking caloric beverages increases the risk of adverse cardiometabolic outcomes in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr. 2010;92(4):954–9.
Haslam DE, Peloso GM, Herman MA, Dupuis J, Lichtenstein AH, Smith CE, et al. Beverage consumption and longitudinal changes in lipoprotein concentrations and incident dyslipidemia in US adults: the Framingham Heart Study. J Am Heart Assoc. 2020;9(5):e014083.
Ventura EE, Davis JN, Goran MI. Sugar content of popular sweetened beverages based on objective laboratory analysis: focus on fructose content. Obesity (Silver Spring). 2011;19(4):868–74.
Zhang YH, An T, Zhang RC, Zhou Q, Huang Y, Zhang J. Very high fructose intake increases serum LDL-cholesterol and total cholesterol: a meta-analysis of controlled feeding trials. J Nutr. 2013;143(9):1391–8.
Stanhope KL, Medici V, Bremer AA, Lee V, Lam HD, Nunez MV, et al. A dose-response study of consuming high-fructose corn syrup-sweetened beverages on lipid/lipoprotein risk factors for cardiovascular disease in young adults. Am J Clin Nutr. 2015;101(6):1144–54.
Brown L, Rosner B, Willett WW, Sacks FM. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr. 1999;69(1):30–42.
Moreyra AE, Wilson AC, Koraym A. Effect of combining psyllium fiber with simvastatin in lowering cholesterol. Arch Intern Med. 2005;165(10):1161–6.
Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD Jr, DePalma SM, et al. 2017 focused update of the 2016 ACC expert consensus decision pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2017;70(14):1785–822.
Miettinen TA, Puska P, Gylling H, Vanhanen H, Vartiainen E. Reduction of serum cholesterol with sitostanol-ester margarine in a mildly hypercholesterolemic population. N Engl J Med. 1995;333(20):1308–12.
Katan MB, Grundy SM, Jones P, Law M, Miettinen T, Paoletti R, et al. Efficacy and safety of plant stanols and sterols in the management of blood cholesterol levels. Mayo Clin Proc. 2003;78(8):965–78.
Ras RT, Geleijnse JM, Trautwein EA. LDL-cholesterol-lowering effect of plant sterols and stanols across different dose ranges: a meta-analysis of randomised controlled studies. Br J Nutr. 2014;112(2):214–9.
Han S, Jiao J, Xu J, Zimmermann D, Actis-Goretta L, Guan L, et al. Effects of plant stanol or sterol-enriched diets on lipid profiles in patients treated with statins: systematic review and meta-analysis. Sci Rep. 2016;6:31337.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER 3rd, Lin PH, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Clin Nutr. 2001;74(1):80–9.
Harsha DW, Sacks FM, Obarzanek E, Svetkey LP, Lin PH, Bray GA, et al. Effect of dietary sodium intake on blood lipids – results from the DASH-Sodium trial. Hypertension. 2004;43(2):393–8.
Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferroluzzi A, Helsing E, et al. Mediterranean diet pyramid – a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6):1402s–6s.
Shen J, Wilmot KA, Ghasemzadeh N, Molloy DL, Burkman G, Mekonnen G, et al. Mediterranean dietary patterns and cardiovascular health. Annu Rev Nutr. 2015;35:425–49.
Vincent-Baudry S, Defoort C, Gerber M, Bernard MC, Verger P, Helal O, et al. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or a low-fat diet. Am J Clin Nutr. 2005;82(5):964–71.
Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, et al. Effect of an indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002;360(9344):1455–61.
Rees K, Takeda A, Martin N, Ellis L, Wijesekara D, Vepa A, et al. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2019;3:CD009825.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34.
Hernáez Á, Castañer O, Goday A, Ros E, Pintó X, Estruch R, et al. The Mediterranean Diet decreases LDL atherogenicity in high cardiovascular risk individuals: a randomized controlled trial. 2017;61(9):1601015.
Thorogood M, Carter R, Benfield L, McPherson K, Mann JI. Plasma lipids and lipoprotein cholesterol concentrations in people with different diets in Britain. Br Med J (Clin Res Ed). 1987;295(6594):351–3.
Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–7.
Cooper RS, Goldberg RB, Trevisan M, Tsong Y, Liu K, Stamler J, et al. The selective lipid-lowering effect of vegetarianism on low-density lipoproteins in a crossover experiment. Atherosclerosis. 1982;44(3):293–305.
Mishra S, Xu J, Agarwal U, Gonzales J, Levin S, Barnard ND. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: the GEICO study. Eur J Clin Nutr. 2013;67(7):718–24.
Barnard ND, Cohen J, Jenkins DJA, Turner-McGrievy G, Gloede L, Jaster B, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777–83.
Jenkins DJA, Kendall CWC, Marchie A, Faulkner D, Vidgen E, Lapsley KG, et al. The effect of combining plant sterols, soy protein, viscous fibers, and almonds in treating hypercholesterolemia. Metab-Clin Exp. 2003;52(11):1478–83.
Jenkins DJA, Kendall CWC, Marchie A, Faulkner DA, Wong JMW, de Souza R, et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA. 2003;290(4):502–10.
Yokoyama Y, Levin SM, Barnard ND. Association between plant-based diets and plasma lipids: a systematic review and meta-analysis. Nutr Rev. 2017;75(9):683–98.
Sofi F, Dinu M, Pagliai G, Cesari F, Gori AM, Sereni A, et al. Low-calorie vegetarian versus Mediterranean diets for reducing body weight and improving cardiovascular risk profile CARDIVEG study (cardiovascular prevention with vegetarian diet). Circulation. 2018;137(11):1103–13.
Ferdowsian HR, Barnard ND. Effects of plant-based diets on plasma lipids. Am J Cardiol. 2009;104(7):947–56.
deLorgeril M, Salen P, Martin JL, Mamelle N, Monjaud I, Touboul P, et al. Effect of a Mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease – insights into the cardioprotective effect of certain nutriments. J Am Coll Cardiol. 1996;28(5):1103–8.
Tilvis RS, Miettinen TA. Serum plant sterols and their relation to cholesterol absorption. Am J Clin Nutr. 1986;43(1):92–7.
Erdman JW, Comm AN. Soy protein and cardiovascular disease – a statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation. 2000;102(20):2555–9.
Damasceno NRT, Apolinario E, Flauzino FD, Fernandes I, Abdalla DSP. Soy isoflavones reduce electronegative low-density lipoprotein (LDL-) and anti-LDL- autoantibodies in experimental atherosclerosis. Eur J Nutr. 2007;46(3):125–32.
O’Neill B, Raggi P. The ketogenic diet: pros and cons. Atherosclerosis. 2020;292:119–26.
Paoli A. Ketogenic diet for obesity: friend or foe? Int J Environ Res Public Health. 2014;11(2):2092–107.
Retterstol K, Svendsen M, Narverud I, Holven KB. Effect of low carbohydrate high fat diet on LDL cholesterol and gene expression in normal-weight, young adults: a randomized controlled study. Atherosclerosis. 2018;279:52–61.
Bueno NB, de Melo ISV, de Oliveira SL, Ataide TD. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110(7):1178–87.
Dong T, Guo M, Zhang P, Sun G, Chen B. The effects of low-carbohydrate diets on cardiovascular risk factors: a meta-analysis. PLoS One. 2020;15(1):e0225348.
Mansoor N, Vinknes KJ, Veierod MB, Retterstol K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115(3):466–79.
Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG 3rd, et al. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity (Silver Spring). 2018;26(2):254–68.
de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. 2019;381(26):2541–51.
Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2020;31(1):92–104. e5
Most J, Gilmore LA, Smith SR, Han H, Ravussin E, Redman LM. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am J Physiol Endocrinol Metab. 2018;314(4):E396–405.
Lefevre M, Redman LM, Heilbronn LK, Smith JV, Martin CK, Rood JC, et al. Caloric restriction alone and with exercise improves CVD risk in healthy non-obese individuals. Atherosclerosis. 2009;203(1):206–13.
Kroeger CM, Klempel MC, Bhutani S, Trepanowski JF, Tangney CC, Varady KA. Improvement in coronary heart disease risk factors during an intermittent fasting/calorie restriction regimen: relationship to adipokine modulations. Nutr Metab (Lond). 2012;9(1):98.
Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361(9364):1149–58.
Vallejo-Vaz AJ, Robertson M, Catapano AL, Watts GF, Kastelein JJ, Packard CJ, et al. Low-density lipoprotein cholesterol lowering for the primary prevention of cardiovascular disease among men with primary elevations of low-density lipoprotein cholesterol levels of 190 mg/dL or above analyses from the WOSCOPS (West of Scotland Coronary Prevention Study) 5-year randomized trial and 20-year observational follow-up. Circulation. 2017;136(20):1878−+.
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335(14):1001–9.
Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–30.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–107.
Conflicts of Interest
Michael D. Shapiro: reports scientific advisory activities with Amgen, Esperion, and Regeneron as well as consultant activities with Novartis. Parag Anilkumar Chevli: declares no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chevli, P.A., Shapiro, M.D. (2021). Dietary Approaches to Lowering LDL-C. In: Wilkinson, M.J., Garshick, M.S., Taub, P.R. (eds) Prevention and Treatment of Cardiovascular Disease. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-030-78177-4_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-78177-4_13
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-78176-7
Online ISBN: 978-3-030-78177-4
eBook Packages: MedicineMedicine (R0)