Abstract
Chronic kidney disease (CKD) is increasingly recognised as a public health problem. This chapter introduces how the definition for CKD was developed. Causes of CKD as known to date are discussed and include recent findings on the importance of acute kidney injury (AKI). The chapter covers key epidemiological concepts as applied to renal epidemiology including incidence, prevalence, screening and how routinely collected data may be of use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points of the Chapter-
1.
When considering risk factors of kidney disease, longitudinal data that investigate incidence of disease may be more useful than cross-sectional data assessing prevalence.
-
2.
There is to date no firm evidence supporting blanket screening for kidney disease irrespective of underlying cause in the general population. However, for specific forms of kidney disease, there may be benefits of testing and early identification, for example, amongst people with diabetes.
-
3.
Urinary testing for albuminuria is infrequently done in primary care, yet albuminuria is a key risk factor for poor health outcomes.
1 Introduction
Abnormalities of kidney function or structure lasting more than 3 months are considered as chronic kidney disease (CKD). CKD is then classified further into categories of risk and severity of function loss based on albuminuria and eGFR. The cause of kidney disease should be recorded as well, though only a subset of people in the general population are investigated as to the cause of their kidney function loss. Typically, people in the general population present with a decreased glomerular filtration rate (GFR less than 60 ml/min per 1.73 m2). Urinary testing is infrequently done in general practice, and structural kidney problems are often only picked up during abdominal ultrasounds carried out for other reasons; hence, patients present less often with gross proteinuria or structural abnormalities.
CKD is increasingly recognised as worldwide health problem. This chapter reviews the epidemiology of CKD. As CKD is a silent disease and often asymptomatic until the presence of established renal failure, there are limited data on its natural history. This chapter aims to put the available data from routine health care and renal registries into context and discusses why screening for CKD has not been established in many health settings.
2 Incidence and Prevalence Explained Using Renal Replacement Therapy Data
Incidence of renal replacement therapy captures how many new people start chronic RRT per unit time (typically years) per million population. ◘ Figure 65.1 shows the change in the UK RRT incidence since 1990. The initial rise in incidence rate in the over 65 age group, which occurred due to acceptance of elderly for RRT, has plateaued, but there appears to be an upward trend in incidence rate in individuals between 45 and 65 years of age [1].
Prevalence refers to how many patients are on RRT at a given point in time. Prevalence data are affected by how many people start dialysis (incidence) and by how long people survive on RRT. Trends of prevalence are therefore much harder to interpret as there are a range of factors that impact on incidence of RRT and factors that impact on survival on RRT, both of which may affect total prevalence figures. For example, in the UK, prevalence has increased each year by ~3–4%. When comparing RRT incidence with prevalence data over time, it becomes apparent that this yearly increase in prevalent patient numbers on dialysis has been mainly driven by improved survival and a larger surviving proportion of transplant patients because in the same time period, there has been an overall stable incidence of new RRT patients (◘ Fig. 65.2) [2].
Prevalence data are useful to quantify costs to the health system; however, incidence data are more useful to understand underlying factors associated with increases in dialysis or transplant take-on over time.
2.1 Limitations of Using RRT Data
Most renal registries record and report the incidence of RRT for patients who have started and survived RRT for at least 90 days as these patients are assumed to have irreversible or established end-stage renal disease (ESRD). This 90-day rule originated in the USA where the government starts to pay for dialysis of patients when they are deemed to be chronic. Many other renal registries adopted the same rule to collect their national data to allow for international comparisons. However, collecting data only on people who survived more than 90 days on dialysis means that this measure does not capture the information of the incidence of dialysis, and it does not tell us how many patients in the population needed acute or chronic dialysis. Not every patient who needs dialysis may get started on dialysis, and not every patient started on dialysis will survive for 90 days. When making international comparisons of RRT incidence, investigators therefore have to make a series of assumptions with regard to the referral and availability of RRT, people with CKD stage 5 being started on dialysis, reversibility of the kidney problem, survival in the first 90 days of the dialysis (numerator) and the population (denominator).
Whether very elderly patients or those with other chronic conditions such as HIV, malignancy or severe cardiovascular disease are offered RRT depends to a large extent on available resources, national legislation with respect to life-prolonging therapy in the face of chronic disease and the degree of renal knowledge and ethical opinions of treating doctors.
3 Defining the Incidence and Prevalence of CKD in a Population
The term CKD covers a number of primary disease processes that result in structural and/or functional kidney abnormalities persisting for at least 3 months. There have been various staging systems over time. A widely used version was from NFK-KDOQI which subdivided CKD into five stages according to the eGFR. This staging was later superseded by the KDIGO CKD staging system (◘ Fig. 65.3) which was based on solid epidemiological information on how single time point eGFR and albuminuria test results relate to later risk of cardiovascular disease and incidence of ESRD.
Composite ranking for relative risks by GFR and albuminuria (KDIGO 2009). (Reproduced with permission from Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group [3])
The incidence of CKD is much harder to ascertain than the incidence of RRT. In order to measure ‘incidence of CKD’, i.e. true new CKD cases in a perfect epidemiological cohort study, one would need to exclude those with CKD at baseline from our follow-up study. The follow-up requires re-measuring kidney function at regular time points on every participant using the exact same assay each time. This assumes a perfect measurement of CKD, but as we discuss below, this is not feasible. In order to have enough observations to understand the risk factors for incident ESRD, a very large study would be needed. For a million population in the UK, there would be about 150 incident RRT cases per year, so the cost of a proper research study just to define CKD incidence, and how this relates to RRT incidence, is prohibitive. To date, there is no universal screening for kidney disease in the general population at pre-specified time points in life. Due to the use of changing creatinine assays over time and testing of kidney function at irregular intervals according to patient need, the use of routine data is therefore challenging and relies on some untestable assumptions.
3.1 Limitations of Using CKD Definition and Staging
The biggest problem of the NKF-KDOQI system was that it did not reflect the true risk of who progresses to RRT and, of those identified, who has a treatable kidney problem. As mentioned before, pooled population-based studies looking at risks for ESRD and death in international studies provided evidence which led to the KDIGO staging of CKD to include albuminuria as an independent risk factor for RRT and low GFR; indeed, albuminuria is an equally strong or potentially stronger predictor of the risk of RRT than eGFR (◘ Fig. 65.3). This is now firmly reflected in the risk system [3, 4] – a person with persistent albuminuria who has an eGFR >60 ml/min/1.73 m2 has the same risk of ending up on dialysis as a person with already reduced eGFR but no albuminuria. However, in practice, the largest group of patients to come to clinical attention with CKD are those with reduced GFR (stages 3–5), for many of whom the causes are multifactorial, and for whom it is unclear whether detecting CKD has any implications on specialised kidney care. Most people with CKD stages 3–5 benefit from agressive cardiovascular risk management, as their risk of dying from cardiovascular disease is very high. The vast majority of these patients are frail elderly people who are traditionally managed by general practitioners and geriatricians. Unfortunately, the many patients with proteinuria/albuminuria and maintained renal function who may merit relatively more attention because there is a greater potential to prevent progression are often not detected as they are not tested for albuminuria.
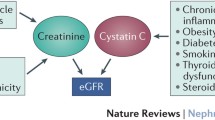
The second issue is accuracy of measuring estimated GFR. The traditional indirect measure of GFR in clinical practice was the 24 h creatinine clearance. These 24 h urine collections are subject to substantial measurement error and not feasible in large studies. NHANES III was the first population-based survey that assessed renal impairment using a serum creatinine-based formula that had been validated for the US kidney patient population [5]. The typical eGFR formula requires simple input data such as the age, gender and ethnicity, in addition to serum creatinine. Because creatinine is a product of the endogenous muscle metabolism, these calculations assume the presence of a stable muscle mass. An investigation in standardisation of creatinine assays showed that the type of assay plays a role for an estimated GFR >60 ml/min per 1.73 m2. Each of the available eGFR formulae has its own biases, e.g. the MDRD formula overestimates presence of CKD in older women and has not been validated in older age groups [6]. The CKD-EPI formula is thought to perform better in Western populations [7] but does not appear to work in less well-nourished populations in other parts of the world, and using the ‘race’ adjustment in the formula has been shown to lead to unintended health inequalities. The measurement error around an eGFR measurement ranges from ±20 ml/min relative to the gold-standard GFR measurement (with worse errors when eGFR is >60 ml/min), and so any survey using eGFR data will be imprecise by default [8]. Most epidemiologic studies only use a single time point eGFR, and the reported risk associations are to some degree affected by non-differential misclassification. Non-differential misclassification means that the observed associations for eGFR and spot urine or dipstick measurements will be imprecise and not capture true kidney function and true albuminuria perfectly. Hence, research studies underestimate the true degree of risk associations for the true underlying kidney function/damage. This is not a major problem for clinical practice as we use repeats of these imperfect test results to reduce measurement error for an individual patient. Of note is that the current KDIGO classification system is based on these imperfect test results.
Overall, despite above criticisms – in comparison with pure serum creatinine measurements and 24 h collections of urine, serum creatinine-based GFR estimates and urinary albumin/creatinine or protein/creatinine ratios seem to perform well to detect the presence of kidney disease.
4 What Influences Prevalence of CKD and Incidence of ESRD?
Many community-based surveys in the USA, the UK and elsewhere have highlighted that the prevalence of CKD is much higher than previously appreciated and appears to be increasing especially in countries with a rising prevalence of diabetes, hypertension, cardiovascular disease and obesity. An updated NHANES survey which used ACR >_ 30mg/g and GFR <60 ml/min/1.73 m2 showed that the prevalence of CKD in the USA has increased over the last 10 years by a factor of approximately 1.3; increases in prevalence of microalbuminuria were explained by increases in BMI, diagnosed diabetes and hypertension; however, only parts of the overall decrease in GFR were explained by the same factors. Cross-sectional data suggest that proteinuria has different prevalence in different ethnicities and that these differences already exist in childhood. Hispanic patients with CKD seem to have a faster decline of GFR when compared to non-Hispanic whites, when adjusting for diabetes. Whether these ethnic differences in albuminuria and proteinuria and disease progression are a function of a certain lifestyle or due to genetic differences remains unclear.
Most countries have similar CKD prevalence estimates but very different RRT incidences. For example, in the USA, the incidence of 90-day RRT is 340 pmp; in the UK, approximately 150 pmp; and in Germany, 180 pmp – again highlighting that CKD prevalence and RRT incidences are not measuring the same entity. Within the USA, the prevalence of CKD as measured by MDRD eGFR has remained stable over 10 years, whilst incidence of RRT increases in the same time period with a disproportionate number of patients with diabetic ERF [9]. In Caucasian populations, variation of RRT incidences is a function of the variation of differing age structures in the population. If this variation is removed via age/sex standardisation and restriction to those under 65 to account for a potential referral bias by age, then the residual variation is partially explained by varying RRT incidence of diabetic nephropathy [10].
5 Referral of Patients with CKD
CKD prognosis consortium data (◘ Fig. 65.4) shows that there are many more patients within primary care than seen by a nephrologist in secondary or tertiary care. It is very evident that for every 100 patients seen in primary care, there were 10 seen in clinics, and only 1 survives and reaches ESRD. To date, we do not know who this one survivor will be who will reach ESRD. This means that a renal physician’s perspective of ‘late referral’ may in parts be true, but certainly there are plenty of people in the community who had many other problems in addition to CKD.
It is important to appreciate that as CKD gets worse, the risk profile of patients changes. Whilst most patients with CKD whom a general practitioner detects on screening will die before ever reaching RRT, patients with progressive renal disease who are seen by nephrologists may have been selected and therefore may show a better survival prognosis with consequently more people needing RRT.
Patients who were referred from primary care to renal services and who have CKD stage 4 show higher cumulative risks death or progression to ESRD than those with earlier CKD (◘ Fig. 65.5) [11]. Almost 65% of patients with CKD stage 4 will have either a renal or a cardiovascular event over the ensuing 5 years. As the GFR falls below 20 ml/min per 1.73 m2, the focus moves to treating the advanced CKD complications and planning for RRT.
Age- and sex-adjusted relative risk (RR) of end-stage renal disease (ESRD) and death in the Chronic Renal Impairment in Birmingham Study by baseline estimated glomerular filtration rate. Both the horizontal and vertical axes are shown on a logarithmic scale. The points in the right-hand panel have been adjusted so that the absolute mortality rates they represent are comparable with the absolute ESRD rates represented in the left-hand panel (thus, the point at which the two lines cross is the level of eGFR above which, in the CRIB cohort, the risk of death started to exceed the risk of ESRD). (Reprinted with permission from Landray et al. [11])
6 Understanding CKD Progression and the Issue of AKI
AKI is reported to complicate up to 5% of all hospital admissions. In a study of over five million hospital admissions in the USA, the AKI rate was 14.6 cases per 1000 discharges in 1992 and increased to 36.4 cases per 1000 discharges in 2001 [12] though case identification was incomplete. Applying laboratory definitions of AKI (an acute rise in serum creatinine), much higher incidences of AKI have been observed. In 2003, in a well-defined Scottish region, the incidences of AKI and acute-on-chronic kidney disease (ACKD) were 1811 and 336 per million population (pmp), respectively, each year. The median age for AKI was 76 years and for ACKD was 80.5 years. Sepsis was a precipitating factor in half of these patients [13]. The same authors repeated this study a few years later and found that the AKI incidence had risen to 2147 pmp per year. A higher proportion of patients with AKI were now referred to specialists, and treatment with RRT was almost four times more common. Whether this is due to true increases in AKI due to the changing population structure with more frail older patients being susceptible or whether this is due to increases in better testing for and coding of AKI due to physician awareness needs to be investigated further.
There is increasing evidence that AKI returning to a ‘normal’ baseline may not be benign but significantly predispose to CKD particularly in the context of multiple or severe episodes [14]. It is increasingly appreciated that AKI often occurs in patients with pre-existing CKD – so-called acute-on-chronic kidney disease. This is best thought of as an acute deterioration in renal function occurring in an individual with limited renal reserve, and not all of these acute-on-chronic declines in kidney function are reversible.
In summary, AKI is common, and its incidence appears to be rising in particular in the older population many of whom have CKD. Of course, AKI will impact on any epidemiological study of CKD progression. Emerging data suggest that the concept of ‘slow CKD progression’ through CKD stages 1–5 does not really hold up in the community setting. The idea of slow progression may very well be true for defined well-understood kidney disease entities. However, at the population level, it appears that CKD progression as a continuous phenomenon is not present in older people, whilst the risk of AKI in the context of acute illness is substantive due to a multitude of factors, which require further investigations as to their preventability.
7 Defining an Underlying Cause of CKD: Considerations and Causes Not to Miss
◘ Figure 65.6 shows an approximate breakdown of CKD causes. Within the British white population, recorded primary causes of ESKD include in 20% diabetic nephropathy, in probably more than 15% severe CVD unrelated to diabetes, in 8% polycystic kidney disease and in autoimmune diseases, as, for example, glomerulonephritis or systemic lupus erythematosus (SLE), 30%. Ideally, the primary cause of CKD should be established in every patient, but a substantial percentage (20–30%) of registry returns worldwide have ‘CKD unknown cause’ as the reason for ESRD – partly because patients may present with small kidneys so it is not appropriate or possible for them to undergo a renal biopsy.
There are undoubtedly new renal diseases waiting to be discovered in the CKD population as illustrated by the recent discovery of C5 nephropathy in the Cypriot dialysis population, or the Mesoamerican nephropathy [15, 16]. Some authors refer to an epidemic of primarily tubulointerstitial chronic kidney disease (CKD) of unknown cause which has been acknowledged to cause an enormous number of early deaths in the last two decades in younger inhabitants in agricultural communities in low- and middle-income countries (LMICs) due to unavailability of diagnostic services and RRT. Whether this is one single disease entity of single causation or a mix of different diseases is unknown [17]. Due to the highly politicised nature of this problem as the hypothesised causes are often directly related to the livelihoods of affected populations, it has been difficult to carry out solid epidemiological research into causation. Most studies are cross-sectional and affected by reverse causality (i.e. presence of kidney damage affecting other biomarker assessments and risk factor reporting). There have been occupational cohort studies which often lose many participants over time and do not reflect the underlying populations as most agricultural workers are healthier than the average population (the so-called healthy worker effect). It has been difficult to perform screening tests as the natural history is not well understood, and this kidney disease has not shown association with traditional markers such as hypertension or proteinuria. The existing eGFR formulae have not been validated in affected populations.
In clinical practice, there are advantages to the patient in honing down the differential diagnosis in terms of (a) the possibility of an inheritable condition, (b) recurrent disease and (c) potential on-going treatment for systemic conditions. ► Box 65.1 shows some conditions worth considering in the patient first presenting with CKD in whom the diagnosis is not clear (obstruction and other obvious causes excluded) and a biopsy either non-diagnostic or inappropriate. This is not a comprehensive list, nor are most of these tests appropriate in most patients, but some in the right setting can be very suggestive of the underlying disease.
Aside from known individual causes in selected patients, there are also more population factors to consider. For example, individuals born in developing countries may be at increased risk of chronic kidney disease due to the high prevalence of poor maternal health and malnutrition leading to low birth weight, prematurity and smaller renal reserve. ► Box 65.2 shows the maternal factors affecting birth weight and prematurity [18].
Data from Pakistan suggest that South Asian children have higher blood pressure than white children in the USA, with also a relatively high prevalence of proteinuria. Data from the UK show convincingly that people who have low birth weight and gain weight in early adulthood will have a lower eGFR than people who are overweight in middle or older age [19]. In short, some patients may be preconditioned from birth to later reduced GFR, and superimposition of secondary causes such as hypertension, diabetes or even AKI such as post-streptococcal glomerulonephritis may result in a higher risk of CKD. This temporal delay in having kidney disease related to diabetes may in part be related to ethnicity. For example, South Asian patients seem to have a two to four times faster progression of diabetic nephropathy in comparison to their Dutch counterparts.
8 Prevention and Screening of CKD
According to the World Health Organization, coronary heart disease is now the leading cause of death worldwide with 60% of the global burden of heart disease in low- to middle-income countries. Some say that cardiovascular risk is very high in patients with CKD, which makes a strong argument for screening for CKD. However, from epidemiologic studies, it appears that a large proportion of people with CKD have to do with lifelong exposure to an adverse lifestyle, in particular, obesity. Hence, targeting common cardiovascular risk factors such as smoking, obesity, diabetes and hypertension is likely to prevent at least in parts CKD and development of renal failure.
Currently, there is no clear evidence showing that ‘screening for CKD’ should be done in all populations. There are several criteria that need to be fulfilled to qualify for screening. The condition should be an important health problem which kidney disease undoubtedly is. Its natural history should be understood – this is the case for people with type 1 diabetes, but less so for the general population where the importance of AKI has only been recognised in the past decade. There should be a recognisable early stage and an acceptable test – this is undoubtedly the case as we have eGFR and albuminuria tests. However, the key criteria to justify screening are that a condition must be treatable, and an outcome prevented, and treatment should be cost-effective. For many forms of common kidney disease, there is no strong evidence that treatment by nephrologists indeed prevents poor outcomes – evidence from a recent hypertension trial suggests that more intensive blood pressure treatment may in fact cause AKI [20]. There is good evidence that detecting and treating albuminuria and hypertension in the context of diabetes delays dialysis and that detecting people requiring referral for dialysis preparation on time may prevent an unplanned start to RRT [21]. However, considering the majority of patients identified in routine primary care, there is no strong evidence that detecting a mildly reduced eGFR in an older person who is already well managed in terms of cardiovascular risk either prevents poor outcomes or is cost-effective.
9 Summary
CKD is common and is associated with an increased risk of cardiovascular disease, mortality, progression to ESRD and AKI. There is very little understanding of the epidemiology of CKD progression in older people. Robust systems for identifying at-risk populations to prevent medication side effects, especially in the setting of acute illness, and higher awareness of albuminuria being a marker for progression to ESRD, may reduce the risk for these patients.
Chapter Review Questions
-
1.
Why do trends on prevalence of RRT provide only limited information on causes of kidney disease?
-
2.
Would you capture the entire population of patients with CKD by applying blood tests?
-
3.
Who is at higher risk of death, a person with eGFR 50 ml/min without albuminuria or a person of the same age and sex with nephrotic syndrome but an eGFR of 88 ml/min?
-
4.
In a given person, by how much can eGFR be wrong relative to the true (but unmeasured GFR) – and does that matter for clinical practice when looking at repeat measurements for that person?
-
5.
Were the guidelines for CKD derived on two measurements of blood/urine more than 3 months apart?
Answers
-
1.
RRT prevalence is not a good measure to use – that is, the number of people on dialysis or living with kidney transplants divided by the total population irrespective of the duration of RRT. The numerator of this figure is the number of patients starting dialysis in that year, plus the number of people that were already on dialysis or living with a kidney transplant in that year, minus the people who died on dialysis or with a transplant. The numerator is affected by a range of factors, which include the causes that drive people to end up on dialysis or with a kidney transplant, but also importantly how long people survive on dialysis or with a transplant which may mask any important associations. It also does not capture people with kidney failure who are treated conservatively.
-
2.
No, CKD is defined by both urine and blood tests.
-
3.
The person with nephrotic syndrome has higher risk of death.
-
4.
eGFR may be ±20 ml/min erroneous, with the error decreasing as GFR declines, i.e. the error is much less in people with advanced CKD, compared to those with normal renal function. However, repeated measurement of eGFR over time in the same patient is meaningful as this will map kidney function change over time, provided the muscle mass/nutrition and fluid status are in a steady state.
-
5.
No, all the risk associations that underlie the guidelines derive from single time point measurements. Clinical populations who are seeking health care are quite different to cohort participants who are in steady state – often patients who seek help are unwell, which will mean that they are not in steady state, and therefore the ‘chronicity’ criterion was introduced based on clinical reasoning. The epidemiological data are clear that a random on-off measurement in steady state informs on risk – a second measurement is not needed.
References
Hole B, Gilg J, Casula A, Methven S, Castledine C. UK renal registry 20th annual report: UK renal replacement therapy adult incidence in 2016. Nephron. 2018;139(suppl1):13–46.
MacNeill S, Ford D, Evans K, Medcalf. UK renal registry 20th annual report: UK renal replacement therapy adult prevalence in 2016. Nephron. 2018;139(suppl1):47–74.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for evaluation and management of chronic kidney disease. Kidney Int. 2013;3(Suppl):1–150.
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80(1):17–28.
Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41(1):1–12.
Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P. Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol. 2005;16(3):763–73.
Matsushita K, Mahmoodi BK, Woodward M, Emberson JR, Jafar TH, Jee SH, et al. Comparison of risk prediction using the CKD-EPI equation and the MDRD study equation for estimated glomerular filtration rate. JAMA. 2012;307(18):1941–51.
Giles PD, Fitzmaurice DA. Formula estimation of glomerular filtration rate: have we gone wrong. BMJ. 2007;334(7605):1198–200.
Hallan SI, Coresh J, Astor BC, Asberg A, Powe NR, Romundstad S, et al. International comparison of the relationship of chronic kidney disease prevalence and ESRD risk. J Am Soc Nephrol. 2006;17(8):2275–84.
Group TEIS. Geographic, ethnic, age-related and temporal variation in the incidence of end-stage renal disease in Europe, Canada and the Asia-Pacific region, 1998–2002. Nephrol Dial Transplant. 2002;21(8):2178–83.
Landray MJ, Wheeler DC, Lip GY, Newman DJ, Blann AD, McGlynn FJ, Ball S, Townend JN, Baigent C. Prediction of ESRD and death among people with CKD: the chronic renal impairment in Birmingham (CRIB) prospective cohort study - American Journal of Kidney Diseases (ajkd.org). Am J Kidney Dis. 2004;43(2):244–53.
Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, Himmelfarb J, Collins AJ. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol. 2006;17(4):1135–42.
Prescott GJ, Metcalfe W, Baharani J, Khan IH, Simpson K, Smith WC, MacLeod AM. A prospective national study of acute renal failure treated with RRT: incidence, aetiology and outcomes. Nephrol Dial Transplant. 2007;22(9):2513–9.
Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;53(6):961–73. https://doi.org/10.1053/j.ajkd.2008.11.034.
Gale DP, de Jorge EG, Cook HT, Martinez-Barricarte R, Hadjisavvas A, et al. Identification of a mutation in complement factor H-related protein 5 in patients of Cypriot origin with glomerulonephritis. Lancet. 2010;376(9743):794–801.
Gonzalez-Quiroz M, Pearce N, Caplin B, Nitsch D. What do epidemiological studies tell us about chronic kidney disease of undetermined cause in Meso-America? A systematic review and meta-analysis. Clin Kidney J. 2018;11(4):496–506.
Caplin B, Jakobsson K, Glaser J, Nitsch D, Jha V, Singh A, Correa-Rotter R, Pearce N. International collaboration for the epidemiology of eGFR in low and middle income populations – rationale and core protocol for the disadvantaged populations eGFR epidemiology study (DEGREE). BMC Nephrol. 2017;18(1):1.
Luyckx VA, Brenner BM, Luyckx VA, Brenner BM. Birth weight, malnutrition and kidney-associated outcomes—a global concern. Nat Rev Nephrol. 2015;11:135–49.
Silverwood RJ, Pierce M, Hardy R, Sattar N, Whincup P, Ferro C, Savage C, Kuh D, Nitsch D. Low birth weight, later renal function, and the roles of adulthood blood pressure, diabetes, and obesity in a British birth cohort. Kidney Int. 2013;84(6):1262–70. https://doi.org/10.1038/ki.2013.223.
The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. New Engl J Med. 2015;373:2103–16.
Black C, Sharma P, Scotland G, McCullough K, et al. Early referral strategies for management of people with markers of renal disease: a systematic review of evidence of clinical effectiveness, cost-effectiveness and economic analysis. Health Technol Assess. 2010;14(21):1–184.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Abro, A., Greenhall, G.H.B., Nitsch, D. (2022). Chronic Kidney Disease: Epidemiology and Causes. In: Harber, M. (eds) Primer on Nephrology. Springer, Cham. https://doi.org/10.1007/978-3-030-76419-7_65
Download citation
DOI: https://doi.org/10.1007/978-3-030-76419-7_65
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76418-0
Online ISBN: 978-3-030-76419-7
eBook Packages: MedicineMedicine (R0)