Abstract
This chapter discusses the relevant surgical anatomy to consider when approaching a chordoma of the thoracic spine. The challenges associated with tumors in this region are unique in some ways and shared in others. One of the unique features of thoracic spine chordomas is that some of the tumors, like distal sacral tumors, can be managed from a posterior-only approach. However, combinatorial posterior and anterior approaches are still very common and often safer. The purpose of this chapter is to discuss relevant anatomy that must be considered with either approach. A case example is shown to help further illustrate the anatomy and to prompt the reader to consider various factors when approaching these tumors operatively.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
This chapter discusses the relevant surgical anatomy to consider when approaching a chordoma of the thoracic spine. The challenges associated with tumors in this region are unique in some ways and shared in others. One of the unique features of thoracic spine chordomas is that some of the tumors, like distal sacral tumors, can be managed from a posterior-only approach. However combinatorial posterior and anterior approaches are still common and often safer. The purpose of this chapter is to discuss relevant anatomy that must be considered with either approach. A case example is shown to help further illustrate the anatomy and to prompt the reader to consider various factors when approaching these tumors surgically.
Thoracic Spine Vascular Anatomy
The aorta holds a dominant position in the vascular anatomy of the thorax. The position relative to the spine and tumor must be considered closely . Thoracic chordomas can compress the thoracic aorta but it is rare in the primary setting for invasion into the adventitia. In general, one can develop a plane between the chordoma and the aorta. The segmental vessels coming off the aorta at each level must be appreciated and appropriately managed to prevent uncontrolled bleeding. The arch of the aorta has several important large branches including the brachiocephalic trunk on the far right, the common carotid artery and then the subclavian artery on the left. These vessels can be a variable during an anterior approach toward upper thoracic chordomas. They are typically not an issue posteriorly. While the arteries are clearly important, they are somewhat more resistant to injury due to their robust muscular layers. The most frequent injuries that occur to these large arteries are related to the avulsion of the smaller segmental vessels. If this occurs, it is usually during the removal of the tumor . A chordoma that abuts these large vessels should be looked upon with suspicion, especially in revision settings if someone has had high-dose radiation therapy. While a plane is typically developed even in this setting, there are circumstances where a chordoma can invade into the lining of the large arterial vessels. In these cases, one must decide whether or not to remove the vessel and replace it with the help of cardiothoracic surgery or to accept a close or positive margin. In the revision setting , we often plan for large vessel reconstruction to increase the change of obtaining negative margins, but this is necessary in only a subset of cases.
The azygos system is a venous drainage system that is often underappreciated. This is potentially due to its smaller caliber relative to the neighboring aortocaval system. However, it is the azygos system that is more likely to be associated with bleeding than the arterial system. The azygos system typically contains a larger azygous vein on the right side of the spine and a smaller hemi-azygos vein on the left side. These veins are the continuation of ascending lumbar veins as well as subcostal veins. The azygos system begins at the caudal end of the thoracic spine (T12). As the azygos system proceeds caudally it collects segmental, subcostal vessel contributions. Toward the arch of the aorta, the azygos cranes over the right main bronchus posteriorly and eventually anastomoses with the superior vena cava. The origin and the course of the azygos system and the presence of its associated accessory hemi-azygos vein are quite variable. Close inspection of the preoperative imaging can help to delineate the caliber and number of these vessels in each case. They must be carefully considered preoperatively and contended with intraoperatively to avoid large volume and potentially catastrophic blood loss. The azygos vessels are easily avulsed during resection or passage of instruments in the thoracic spine.
Spinal Cord Blood Supply
The thoracic region spinal cord blood supply is derived primarily from the aorta and in some cases from the subclavian vessels . The anterior spinal artery (ASA) is the main blood supply to the ventral thoracic cord parenchyma. The aorta supplies the anterior spinal artery through radiculo-medullary branches. There are fewer radiculo-medullary arteries in the thoracic spine (one to four is typical) and less collateralization of the blood supply in the thoracic spine. In addition, the distance between these arteries is greater in the thoracic spine. Furthermore, there is little communication between the central and peripheral regions of the thoracic spinal cord. The dominant radiculo-medullary artery in the thoracic spine is termed the artery of Adamkiewicz. It arises from the aorta and enters the spinal cord from the left in most cases between T9 and T-12. The artery of Adamkiewicz gives off a hairpin shaped, descending branch, and a smaller branch that ascends. The ASA in the thoracic spine is in continuity throughout the spinal cord in this region but the caliber of the ASA fluctuates depending upon the region of the cord. Areas supplied by a vessel of diminutive caliber are more at risk for vascular insult [1].
Iatrogenic vascular injury to the thoracic spinal cord was closely studied during the advent and subsequent evolution of thoraco-abdominal aortic aneurysm (TAAA) repair. TAAA was at one point associated with spinal cord ischemia in up to 32% of cases [2, 3]. This finding initially led some vascular surgeons to reconstruct the segmental spinal arteries to their graft to help prevent the risk of cord ischemia. Subsequent research in this area has improved our understanding of spinal cord blood supply. For instance, loss of the artery of Adamkiewicz by itself is not associated with cord ischemia in all cases. Cord ischemia is multifactorial and also partly based on patient factors such as renal and vascular disease as well as perioperative hemodynamic fluctuations [2]. Several studies have noted the importance of maintaining an elevated mean arterial pressure to perfuse the spinal cord. Additionally, the insertion of intrathecal drains to control the intrathecal pressure and facilitate a gradient between the mean arterial pressure (MAP) became commonplace in TAAA. Several studies noted that cord ischemia often occurred in a delayed fashion up to several days after an operation [3]. Cord ischemia was found to be associated with drops in MAP and increases in intrathecal pressure, which further illustrates the importance of maintaining this pressure gradient.
The number of segmental vessels that are occluded or ligated during tumor resection is an important determinant for spinal cord perfusion. One study in the thoracic surgery literature investigated cases in which four or more segmental vessels were occluded by a vascular stent. They included eight cases, and in six of the eight cases, the dominant radiculo-medullary vessel was occluded. The authors noted intraoperatively that two of the eight patients had changes in their motor evoked potentials. However, both of these cases responded to increasing the MAP. This small series of patients did not report any occurrence of postoperative paraplegia [4].
As described in Chap. 13, the role of the artery of Adamkiewicz has been investigated in the setting of en bloc resection (EBR) in the thoracic spine. In a case series of 15 patients, the authors removed the artery of Adamkiewicz as well as the cephalad and caudal adjacent segmental vessels bilaterally [5]. No cases demonstrated postoperative neurologic changes in this series. This clinical study corresponds with an animal study using a canine model performed by the same authors. The anatomy is notably different in canines as the dominant radiculo-medullary vessel typically occurs at L5. The authors reported a change in spinal cord blood flow after removing the dominant radiculo-medullary vessel along with the adjacent two vessels. However, none of the canine subjects demonstrated neurologic compromise afterward [6, 7]. Yet, despite this evidence, it should not be a foregone conclusion that removing the dominant radiculo-medullary vessel along with the adjacent two segmental vessels is safe. As mentioned in Chap. 13, the authors report anecdotal experience of postoperative neurologic deficits attributable to ischemia. In the author’s experience, patients with spinal cord compression or deformation of the spinal cord with preoperative neurologic deficits are at higher risk and the spinal cord is not in a stable physiologic state in this setting. Furthermore, a patient with preexisting renal and/or vascular disease may be more at risk for developing cord ischemia. The non-zero risk of an ischemic event with resection and catastrophic clinical sequelae warrants a thorough discussion with the patient preoperatively. Close monitoring of the MAP is an important component and is recommended in the perioperative setting. In our institution, we utilize the intensive care unit (ICU) in between staged procedures and for 48–72 hours postoperatively to ensure the MAP remains adequate. In certain cases where the risk of cord ischemia is felt to be high, an intrathecal drain is placed in order to more fully control the pressure gradient. It is important to consider preoperative angiography in patients where spondylectomy is considered, particularly at the cord level. The results of angiography can help inform intraoperative and postoperative management. In addition, the results of angiography can help guide preoperative risk discussions with patients and families.
Segmental Nerve Roots
Each of the paired segmental nerve roots of the thoracic spine exits the spinal canal under the pedicle of their vertebral body with the same numbering. As such, the first thoracic segmental nerve root leaves the spine under the pedicle of the T1 vertebral body. The C8 segmental nerve root leaves the spine between C7 and T1. These nerve roots must be carefully managed in the case of upper thoracic chordoma. They are both functional nerve roots and can lead to significant hand dysfunction if damaged or sacrificed. This must be discussed with the patient in advance. Both C8 and T1 contribute to multiple motor endpoints in the upper limb. However, the most profound changes seen after removing these segmental nerve roots are in hand function where the loss of intrinsic and finger flexion can be profound and debilitating. It is important to recognize that inadvertent and irreparable damage to nerve roots is possible even in the absence of frank injury. Extensive dissection of the nerve roots can devascularize and lead to similar dysfunction seen in overt ligation. The use of radiation therapy can potentiate the dysfunction through pain and upper extremity swelling . The remaining thoracic nerve roots from T2 through T12 also contain important motor function. However, removing these segmental nerve roots leads to less disability than observed at C8 and T1. Resection of the remaining segmental nerve roots leads to numbness in their distribution, but it can also lead to dysesthetic pain. In addition, the work of breathing may change depending on how many segmental nerve roots are removed and the degree of intercostal muscle dysfunction. Resection of nerve roots in the lower thoracic spine may lead to changes in the flank musculature and lead to the appearance of a hernia. Dyesthesia related to nerve root resection can create challenges with acute postoperative pain and progress to chronic pain. The patient is aware of this potential outcome in advance of surgery. The segmental nerve roots also serve as the conduit for the segmental arterial and venous supply to the spinal cord as described in the previous section.
Relevant Osseous Anatomy
Each of the 12 thoracic vertebrae typically has an associated rib. The rib articulates with the transverse process as well as the vertebral body. If EBR is considered, it is usually necessary to remove a portion of singular or multiple ribs . From a posterior approach, one can identify large segments of the ribs if the trapezius and latissimus musculature is gently elevated from the dorsal aspect of the ribs. It is important to consider these muscular structures when one is dissecting far lateral on the ribs because they may be necessary for flap coverage in the future. Depending upon the exposure that is necessary and the position of the tumor, it is often possible to leave a portion of the proximal aspect of the rib in place. Leaving the articulation of the rib with the vertebral body and the transverse process in its original position can simplify the approach. Transection of the rib lateral to the transverse process followed by a second transection further lateral allows removal of the rib and access to the thoracic spine from a posterior approach.
The ribs can be an important source of non-vascularized autogenous graft. However, one can also use a vascularized rib for reconstructive purposes. During the approach to the spine, one must keep this in mind if a vascular reconstruction is needed. Posterior vascular reconstruction using a rib is possible and it has the advantage of not requiring anastomosis since the rib is left attached to its segmental vessel. The ribs chosen for these purposes are typically cephalad or caudal to the primary levels of the tumor since the segmental vessels are typically removed from the ribs to access the tumor. Further discussion of this will occur later in this chapter during the case example.
The osseous anatomy of the vertebral bodies from T1 through T12 is better covered in a general spine textbook. The preoperative plan should involve scrutiny of imaging for any morphometric deviation in the patient’s anatomy. This includes the shape and dimensions of the pedicles as well as the size of the vertebral bodies. Evaluating bone density and considering preoperative radiation therapy is important and has implications for reconstruction efforts. It is not uncommon to have a poor bone structure in patients who are being treated for cancer and this is particularly true if a patient has undergone radiation therapy. If bone quality is of concern, then one might consider alternative forms of instrumentation such as laminar hooks. This is also a consideration if the pedicle anatomy is such that a standard pedicle screw will not be possible.
Case Example
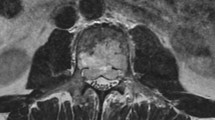
The following case example is meant to illustrate some of the difficulties posed by an upper thoracic tumor. A 66-year-old woman had a cough for several months and presented to her primary care doctor, which prompted further imaging. Figure 9.1 demonstrates a chest radiograph revealing a widened mediastinum, which then led to a magnetic resonance image (MRI). Figure 9.2 demonstrates a T2-sequence hyperintense mass on MRI at the level of the third thoracic vertebrae. Note this corresponds to the level of the aortic arch . A subsequent biopsy confirmed chordoma as the pathology. Figure 9.2 also demonstrates that the esophagus is being compressed by the mass, which is depicted by a white arrow in the figure. Anterolateral to the esophagus is the aortic arch. Compression of the esophagus complicates the patient’s management in two ways. First, if one were to consider radiation therapy alone for treatment of this mass, which some patients may opt for, this would have a low probability of success. The position of the esophagus would mandate a lower dose of radiation to this region. A suboptimal dose of radiation , which would spare esophageal injury, would not be able to control the tumor. For that reason, surgery with or without radiation therapy is a better option in this situation. Although the appearance on imaging may give the impression that the tumor is growing into the esophagus, it is more likely that the esophagus is being compressed rather than invaded. Figure 9.3 reveals that the mass involves portions of three vertebrae (T2–T4) and contacts a total of five vertebrae (T1–T5). This observation lays the foundation for the spondylectomy. In this case, our plan was to transect through the vertebral body above and below the main 3 impacted vertebrae. This patient has a robust azygos vein reversing along the right side of the vertebral bodies. Figure 9.4 demonstrates the large caliber azygos vein as well as many of the segmentals coming off of the azygos and traveling along the lateral border of the vertebral bodies. It is important to characterize the venous structures in the planned operative field as these will need to be managed during the approach. Preoperative angiography revealed that the dominant radiculo-medullary artery enters the spinal cord along the left side through the T9 segmental nerve root (Fig. 9.5).
This sagittal T2-weighted image reveals the azygos vein (horizontal arrow) as it ascends the right side of the anterolateral thoracic spine. The vertical arrow reveals the segmental vessels coming from the azygos. An appreciation of the segmental vessels is crucial when one is planning en bloc spondylectomy
Stage one of the operation involved a posterior approach with instrumentation as well as the development of a plane circumferentially around the vertebrae above and below the level of the tumors [8, 9]. Figure 9.6 reveals the blunt dissection that is performed in order to develop a plain dorsal to the great vessels of the thoracic spine and ventral to the vertebral body. In the thoracic spine, several ribs must be removed to develop these planes . The amount of rib removed is determined based on the size of the tumor and the space needed to adequately and safely access the tumor. Typically, 5–7 centimeters lateral to the costotransverse joint is enough rib removal to allow access. When dissecting around the dorsal convexity of the ribs, one eventually begins to visualize the mid-portion of the rib both caudally and in the cephalad direction. At these levels, one can see Sharpey’s fibers where the intercostal musculature inserts into the ribs. The intercostal muscle and the associated Sharpey’s fibers can be removed sharply. Once these areas have been carefully released gentle blunt dissection can occur typically in the extra plural compartment. Gentle release of the adventitial tissue deep to the rib can be done bluntly. Once the rib has been mobilized it can be transected and removed. The rib is an important structure and can be used for structural grafting or morselized for autograft. During the process of removing the ribs, the segmental subcostal neurovascular bundle is also isolated. Depending upon the planned reconstruction, these intercostal vessels can be used for vascularized rib graft. However, in most cases, the segmental nerve artery and vein are removed to allow access to the thoracic cavity for spondylectomy. Once the ribs have been removed at the level of the tumor and typically one level above and below on both sides, then one can begin to bluntly elevate the pleural tissue off the lateral border of the vertebrae. With a gentle retraction of the lung tissue, the segmental vessels coming off the azygos system and the aorta can be identified. These segmental vessels can be ligated and gently elevated away from the vertebral body. This allows for blunt dissection ventral to the vertebral body and dorsal to the great vessels. It is important to fully develop the plane between the vessels and the vertebral body.
An intraoperative photograph as well as an artistic rendition with the Penrose drain in place. The Penrose drain is placed in the plane and bluntly dissected as demonstrated in Fig. 9.6. In this figure, the threadwire saws are passed through the Penrose drain, which is serving as a conduit
Once the blunt dissection has been carried out the vertebrae can be osteotomized above and below the tumor. At our center, we often utilize threadwire saws to complete the osteotomy. We generally pass these during the posterior portion of the surgery and then utilize their cutting function during the anterior portion of the surgery, which was performed in this case. Figures 9.7 and 9.8 reveal how the Penrose drains are initially passed through the plane created by blunt dissection. The purpose of passing the Penrose drain is to eventually pass the threadwire saws through the Penrose drain. In this way, the Penrose drain acts as a conduit. After the Penrose drain has served its purpose it is removed, leaving the threadwire saws in place (Fig. 9.9). After the threadwire saws have been passed dorsal to the great vessels and ventral to the spinal cord we secure them in the field with clamps. We then performed removal of the posterior vertebral elements . The posterior elements are removed (including the pedicles) where it is safe to do so based on the location of the tumor. Once this is done, we develop a plane ventral to the spinal cord. Development of this plane is done with bipolar electrocautery as well as sharp dissection using dissecting scissors to cut any attachments from the posterior longitudinal ligament to the dura. This is done throughout the ventral surface of the spinal cord at the level of the tumor. It is very important to detach these structures in order to facilitate the removal of the tumor away from the spinal cord in stage two. Once this dissection has been carried out one can safely pass the threadwire saws ventral to the spinal cord as seen in Figs. 9.10 and 9.11. Once the threadwire saws have been safely past circumferentially around the vertebrae they are coiled and sutured together with silk sutures and subsequently sutured to a posterior rod. This is typically done to the rod on the side of the planned anterior approach (usually left) (Fig. 9.12). After the posterior incision is closed and stage one completed, the patient is transferred to the ICU. This level of care allows maintenance of mean arterial pressures and frequent neurologic checks . In addition, we often obtain a CT to help elucidate the final position of the threadwire saws. It is useful to see their position and also their relative trajectory. It is possible to inadvertently pass one of the threadwire saws ventral to a component of the azygos venous system. It is important to recognize this to avoid transection of the vessel during the anterior approach.
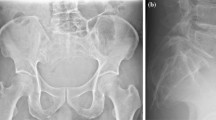
In this example, the patient’s tumor is difficult to access from an anterior approach. While it may have been possible to remove this tumor completely from a posterior approach, we felt that the compression of the esophagus as well as the proximity to segmental vessels off of the arch of the aorta and azygos system made it relatively unsafe to remove this all posteriorly. Therefore, we planned an anterior approach with the help of a thoracic surgeon who performed a sternotomy (Figs. 9.13 and 9.14). Isolation and deflation of the left lung field by the anesthesiologist aided the exposure. We were able to identify and ligate further segmental vessels and develop a plane between the esophagus and the tumor. This allowed us to identify the threadwire saws which had been sutured to the posterior rods. We released the saws by cutting the silk sutures which held them in position. The saws were then placed into their saw handles and a gentle back in forth action with the hands was used to cut through the vertebral bodies (Fig. 9.15). Great care was taken to retract the deflated lung as well as to protect the heart which was directly in the field (Fig. 9.16). Once the vertebrae are cut, the specimen should be relatively mobile . However, there are often soft tissue attachments that were not completely appreciated during the posterior approach. Sharp dissection of these attachments allows delivery of the specimen. Often, there are attachments between the posterior longitudinal ligament and the spinal cord which need to be transected. This can be done by gently rotating the specimen while protecting the spinal cord. Figure 9.17 reveals the specimen immediately after it was removed from the field (Fig. 9.17). Figure 9.18 shows an anterior viewpoint of the specimen. One can see the spinal cord in the upper left portion of the image. The heart is designated with the five-pointed star and the deflated lung is designated by the hexagon. Reconstruction of the defect can be carried out in multiple ways. We prefer vascularized bone grafts as described in Chap. 13. Figure 9.19 reveals further complexity associated with an upper thoracic tumor as this shows the vascularized fibular graft delivered into the operative field. One can also see the brachiocephalic artery, which is designated by an arrow and complicated both the extirpation of the tumor and also reconstruction (Fig. 9.19). Figures 9.20 and 9.21 reveal a radiograph of the gross specimen. Gross and microscopic examination of the specimen with our pathologist revealed negative margins (Figs. 9.20 and 9.21). After reconstruction of the defect using a vascularized fibular graft, the anastomosis was carried out using a segmental vessel from the azygos and aortic arch. Postoperative CT scan and standing x-rays are demonstrated in Figs. 9.22 and 9.23. Postoperatively, the patient continues to do well 2 years out from her surgery at the time of this writing. However, one notes several findings from a sagittal balance point of view. She is compensating a positive sagittal balance with pelvic retroversion and hyperlordosis of the lumbar spine. This positive sagittal balance was likely iatrogenic from the reconstruction and not fully appreciated at the time of surgery. Positive sagittal balance has been linked to poor quality of life after en bloc spondylectomy [10].
This intraoperative photograph reveals the relevant anatomy from an anterior perspective once the specimen has been removed. The arrow delineates the spinal cord where one can see the segmental nerve roots have been ligated with zero silk sutures. The five-pointed star is on the heart. The hexagon is on the deflated lung
Abbreviations
- ASA:
-
Anterior spinal artery
- EBR:
-
En bloc resection
- ICU:
-
Intensive care unit
- MAP:
-
Mean arterial pressure
- MRI:
-
Magnetic resonance image
References
Colman MW, Hornicek FJ, Schwab JH. Spinal cord blood supply and its surgical implications. J Am Acad Orthop Surg. 2015;23:581–91.
Crawford ES, et al. Thoracoabdominal aortic aneurysms: preoperative and intraoperative factors determining immediate and long-term results of operations in 605 patients. J Vasc Surg. 1986;3:389–404.
Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ. Experience with 1509 patients undergoing thoracoabdominal aortic operations. J Vasc Surg. 1993;17:357–68; discussion 368–70.
Schurink GW, et al. Assessment of spinal cord circulation and function in endovascular treatment of thoracic aortic aneurysms. Ann Thorac Surg. 2007;83:S877–81; discussion S890–2.
Murakami H, et al. Does interruption of the artery of Adamkiewicz during total en bloc spondylectomy affect neurologic function? Spine (Phila Pa 1976). 2010;35:E1187–92.
Fujimaki Y, Kawahara N, Tomita K, Murakami H, Ueda Y. How many ligations of bilateral segmental arteries cause ischemic spinal cord dysfunction? An experimental study using a dog model. Spine (Phila Pa 1976). 2006;31:E781–9.
Kato S, et al. Effects on spinal cord blood flow and neurologic function secondary to interruption of bilateral segmental arteries which supply the artery of Adamkiewicz: an experimental study using a dog model. Spine (Phila Pa 1976). 2008;33:1533–41.
Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: improvement of the technique and its associated basic background. J Orthop Sci. 2006;11:3–12.
Shah AA, et al. Modified en bloc spondylectomy for tumors of the thoracic and lumbar spine: surgical technique and outcomes. J Bone Joint Surg Am. 2017;99:1476–84.
Massier JRA, et al. Sagittal spinal parameters after en bloc resection of mobile spine tumors. Spine J. 2019;19:1606–12.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tobert, D.G., Shin, J.H., Schwab, J.H. (2021). Surgical Management of Chordoma in the Thoracic Spine. In: Sciubba, D.M., Schwab, J.H. (eds) Chordoma of the Spine. Springer, Cham. https://doi.org/10.1007/978-3-030-76201-8_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-76201-8_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76200-1
Online ISBN: 978-3-030-76201-8
eBook Packages: MedicineMedicine (R0)