Abstract
X-linked adrenoleukodystrophy (ALD) is the most common inborn error of peroxisomal beta-oxidation, caused by pathogenic variants in the ABCD1 gene, affecting the functioning of a protein responsible for the transportation of very long-chain fatty acids (VLCFA) into the peroxisome. This defect results in the accumulation of VLCFA in different tissues, specially the central nervous system, suprarenal glands, and testis. There is no genotype-phenotype correlation, and affected families have a noticeable intrafamilial variability. Several different clinical presentations have been described for men with ALD, including a pre-symptomatic state, cerebral demyelinating ALD, adrenomyeloneuropathy (AMN), Addison’s disease, and a spinocerebellar subtype. The lifetime risk of Addison’s disease in ABCD1 carriers is about 80%. Virtually all men and up to 80% of heterozygous women develop AMN. Women present with milder and usually later-onset myelopathy than men. Neuroimaging carries diagnostic and prognostic implications. The diagnosis is based on the biochemical analysis of VLCFA plasma levels (although less sensitive in women), and/or genetic testing. A newborn ALD screening is now available. There is no cure, but early hematopoietic stem cell transplantation can arrest brain demyelination in appropriate candidates. Preventing Addisonian crisis is a mainstay in patient management, through corticosteroid replacement. Symptomatic treatment for AMN is primarily based on relieving spasticity and pain.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Adrenoleukodystrophy
- Peroxisomal disorders
- Leukoencephalopathies
- Demyelinating diseases
- Adrenomyeloneuropathy
- Addison’s disease
- Adrenal insufficiency
- Ataxia
- Spasticity
- Spastic paraparesis
- Fatty acids
- ABCD1 gene
Patient Vignette
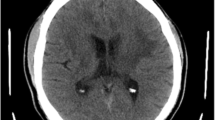
A 28-year-old man with a 5-year history of progressive spastic paraparesis of unknown etiology, with comorbid sphincter and sexual dysfunction, was brought to the emergency department (ED) because of a 3-day history of marked exacerbation of spasticity in his lower limbs, followed by two syncopal episodes, emesis, vegetative symptoms, and finally psychomotor agitation. At the ED he was noted to be agitated and confused. He had no fever, but his vital signs were remarkable for hypotension and tachycardia. Brain CT and CSF analysis were unremarkable. His clinical picture progressed with persistent hypotension, hypoglycemia, hyponatremia, hyperkalemia, and a low cortisol level. Suprarenal insufficiency was confirmed, and he was started on steroid replacement, along with correction of hypoglycemia and electrolyte imbalance. While his mentation slowly improved, his spasticity with severe spasms persisted. Neurological and general evaluation during admission was remarkable for hyperpigmented skin and gums, frontotemporal alopecia (Fig. 27.1), cognitive slowness, spastic paraparesis-dystonic syndrome, and mild ataxia with hypermetric saccades, mild dysmetria, dysdiadochokinesia, and dyssynergia, with generalized hyperreflexia and bilateral Babinski signs. His MRI showed signal changes in parieto-occipital deep white matter and splenium of the corpus callosum (Fig. 27.2). Based on the clinical and radiological characteristics, along with elevated very long-chain fatty acid (VLCFA) levels, X-linked adrenoleukodystrophy was confirmed.
Introduction
X-linked adrenoleukodystrophy (ALD) is both the most common inborn error of metabolism of peroxisomal beta-oxidation and the most frequent monogenetically inherited demyelinating disorder [1]. In the United States, the estimated overall minimum frequency is about 1:21,000 for hemizygote men and 1:14,000 for heterozygote women [2]. Now that newborn screening has been implemented in some parts of the world, the true prevalence could be even higher [3]. It is an X-linked hereditary disease caused by pathogenic variants in the ATP-binding cassette, subfamily D, member 1 (ABCD1) gene, located on chromosome Xq28, that codes for the peroxisomal half-transporter of CoA-activated very long-chain fatty acids (VLCFA), responsible for the transportation of VLCFA into the peroxisome [4, 5]. Deficiency of the enzyme very long-chain acyl CoA synthetase (ligase) results in accumulation of endogenous and exogenous saturated VLCFA (fatty acyl chain length of ≥22 carbons), particularly tetracosanoic (C24:0) and hexacosanoic acid (C26:0), mainly in the nervous system, the adrenal cortex, and the Leydig cells in the testes [4, 6].
There is no genotype-phenotype correlation, and there is often marked intrafamilial variability. Clinically, ALD can present with a wide spectrum of neurological and endocrine manifestations. Six main phenotypes among men hemizygotes have been reported. The more prevalent phenotypes are adrenomyeloneuropathy (AMN) and the cerebral form of ALD with a childhood, adolescent, and adult age of presentation. Less frequent phenotypes include pure Addison’s disease, spinocerebellar ataxia, and asymptomatic subtypes [1]. Heterozygous women develop an AMN phenotype with a later onset and somewhat milder presentation.
 X-linked adrenoleukodystrophy is the most common inherited peroxisomal disorder, caused by mutations in the ABCD1 gene, resulting in the accumulation of VLCFA mainly in the nervous and endocrine systems. There is no genotype-phenotype correlation. It may present with adrenal insufficiency, progressive brain demyelination, or myelopathy, in different combinations.
X-linked adrenoleukodystrophy is the most common inherited peroxisomal disorder, caused by mutations in the ABCD1 gene, resulting in the accumulation of VLCFA mainly in the nervous and endocrine systems. There is no genotype-phenotype correlation. It may present with adrenal insufficiency, progressive brain demyelination, or myelopathy, in different combinations.
Pathophysiology
ABCD1 is widely expressed in many different tissues, and VLCFA levels are highly elevated in almost all tissues. The exact mechanism by which VLCFA are toxic to cells and why cells of the adrenal cortex, testes, and the peripheral and central nervous system are especially vulnerable remains to be resolved [7]. An explanation for the demyelination in the cerebral ALD subtype could be the myelin sheath instability from VLCFA excess in the lipid membrane. High levels of VLCFA could also be cytotoxic to oligodendrocytes and microglia contributing to the demyelination process [8]. Cerebral inflammation is mediated by oxidative stress, activation of macrophages, microglial apoptosis, and endothelial dysfunction, which ultimately damages the blood–brain barrier [9].
Griffin et al. have typed the cells in the perivascular cuffs [10]. Fifty-nine percent were T cells, 24% B cells, and 11% monocytes/macrophages. Fifty-eight percent of the T cells were T4, and 27% T8, while 15% could not be classified. This pattern was similar to that found in the CNS during a cellular immune response, which suggested that an aspect of injury in ALD is likely immunologically mediated [10, 11]. In AMN cases, the current pathogenic hypotheses suggest that impaired mitochondrial function, subsequent oxidative stress, and energy depletion contribute to a noninflammatory dying-back axonopathy of the spinal cord that involves the descending corticospinal tracts in the thoracic and lumbosacral regions and ascending posterior columns in the cervical region [4]. The mechanism of adrenal gland injury in ALD is not well understood. VLCFA are known to accumulate in the zona fasciculata and reticularis of the adrenal cortex, and the chronic accumulation of VLCFA is thought to lead to cytotoxic effects and ultimately apoptosis with atrophy of the adrenal cortex [12].
See Fig. 27.3 for the pathophysiological aspects of ALD.
Pathophysiological aspects of ALD. LCFA long-chain fatty acids, VLCFA very long-chain fatty acids, ALD adrenoleukodystrophy, AMN adrenomyeloneuropathy. (Adapted from [4])
Clinical Presentations
Neuropsychiatric Manifestations
ALD has been defined as a disorder with many different phenotypes (Table 27.1). In addition, presenting phenotypes may not be static, and their clinical state may change over time. Patients with ALD are classically asymptomatic at birth [7]. AMN, the combination of myelopathy and peripheral neuropathy, has a near 100% lifetime penetrance. Virtually all men and up to 80% of heterozygous women develop myelopathy [13]. Consequently, there is a high risk for children and adult asymptomatic patients to develop neurological deficits, and for AMN men to develop cerebral demyelination [14]. Although myelopathy may present during adolescence, it typically develops between 20 and 40 years of age. The earliest symptoms are usually urge incontinence, followed by a gradually progressive gait disorder due to spastic paraparesis and sensory ataxia. An axonal peripheral sensorimotor neuropathy is present on electrophysiological testing, but this is frequently overlooked because of the coexisting myelopathy. The age of onset and rate of progression of AMN symptoms are highly variable [7]. In a prospective cohort of men with AMN, Huffnagel et al. determined a median time from onset of myelopathy to the use of a walking aid of 13 years (95% CI 9.1–16.9 years) [15]. Patients with pure AMN, with normal brain MRI, have a better prognosis compared with other phenotypes. Their neuropsychological profile is typically normal except for mild deficits in psychomotor speed and visual memory [16].
According to van Geel et al. after a mean follow-up period of 10 ± 5 years, 19% of adult patients with AMN without symptoms of cerebral involvement developed cerebral ALD, with a mean survival of 2.3 ± 1.9 years after the first manifestation of cerebral disease [14]. Studies have shown that more than 80% of women heterozygous carriers develop a milder AMN phenotype than men, usually after the age of 40. According to some recent reports, AMN can occur in women in their 20s [17]. Signs of dementia, behavioral or visual disturbances, occur in 1–3% of heterozygous women and adrenal insufficiency in only 1% [18]. A prospective cohort study in 42 men with ALD and 32 controls demonstrated that the spinal cord cross-sectional area of patients is smaller compared to healthy controls and correlates with severity of myelopathy as measured by the expanded disability status scale, severity scoring system for progressive myelopathy, and vibration sense scores [19].
There are several reports of ALD presenting as pure familial spastic paraparesis [20], in some cases presenting with an autosomal dominant pedigree [21], or recessive pattern in others [22]. Urinary and bowel symptoms are common in men with AMN and in ABCD1 variant female carriers. According to Hofereiter et al., in a case series of 19 males with AMN and 29 female carriers, overactive bladder symptoms were reported in 100% of males and 86% of females. Moderate to severe bowel dysfunction was noted in 21% and 10% of males and females, respectively [23]. In a retrospective chart review based on 39 ALD adult patients (28 female carriers), Gomery et al. reported urinary symptoms in 64% of men and 68% of women and bowel symptoms in 44% of men and 64% of women. The most common symptoms included urinary urgency (28% of males, 50% of females), urinary incontinence (41% of males, 57% of females), and constipation (36% of males, 39% of females), as well as urinary frequency and urinary hesitancy in males (both 38%) [24]. Although the precise mechanism is still unclear, severe autonomic dysfunction has also been reported, characterized by orthostatic hypotension, sexual dysfunction [25], and autonomic neuropathy [26].
According to Chen et al., among unrelated Taiwanese patients with adult-onset cerebellar ataxia, ALD accounts for 0.85% (1/118) of the patients with molecularly unassigned hereditary ataxia and 0.34% (1/296) of the patients with sporadic ataxia with autonomic dysfunction. In this cohort, white matter hyperintensities in the corticospinal tracts and in the cerebellar hemispheres were strongly associated with ALD rather than other ataxias [27]. Cerebral demyelination is estimated to occur in about 40% of male ALD patients before the age of 18 years but is well documented to occur also in adulthood [14].
The symptoms associated with cerebral ALD depend on the site of the initial lesions. In children and adolescent boys, the first symptoms are usually cognitive deficits, hyperactive behavior, emotional lability, and decline in school performance [1]. These symptoms are frequently initially attributed to attention deficit hyperactivity disorder, which can delay the diagnosis of ALD. When lesions progress, pyramidal tract signs, central visual impairment, apraxia, astereognosis, auditory impairment, and sometimes seizures occur [1, 28]. Demyelination involving the visual tracts occurs typically months to years after the diagnosis of childhood cerebral ALD, manifesting as progressive visual loss followed by optic atrophy. In a report of 15 childhood cerebral ALD patients, there were strabismus in 10 cases, pale optic discs in 7 cases, macular pigmentary changes in 3, optic nerve hypoplasia in 1, and cataracts in 1 [29]. A pathological examination revealed accumulation of bi-leaflet inclusions in optic nerve macrophages, retinal neurons, and macrophages [30].
An atypical spontaneous “arrested” clinical course of cerebral ALD has been described, without evidence of imaging, neurological, or neuropsychological deterioration for many years after the initial symptoms [5, 31]. All three patients reported by Korenke et al. showed typical first symptoms and neuroimaging alterations of cerebral ALD between 7 and 11 years, with a subsequent arrest of neurologic deterioration for 5 to 12 years; none developed impaired visual or auditory function. This stable clinical course was supported by serial neuroimaging studies, with gadolinium enhancement observed only in the first MRI examination of one of these patients [31]. Some authors warned that it may still reactivate many years later [7].
In adult cerebral ALD, initial symptoms are often psychiatric, especially if the lesions are located in the frontal lobes, and can resemble depression, mania, or psychosis [13]. A review by Rosebush et al. found that 19 of 34 cases (56%) were reported to have psychiatric symptomatology. However, a detailed psychiatric assessment was provided only in 13, and the earliest reported symptom was a change in behavior or personality. Twelve of those 13 patients had symptoms of mania, including disinhibition, emotional lability, increased spending, hypersexuality, and perseveration. In addition, five of these patients were also psychotic. Unfortunately, many of the patients were treatment-resistant and appeared to have an aggressive course [32].
See Fig. 27.4 for the clinical spectrum and natural history of ALD.
Endocrine Dysfunction
X-linked ALD is the most frequent genetic cause of Addison’s disease [37]. However, in regions where neonatal screening has not been established, there is a high prevalence of unrecognized adrenocortical insufficiency in ABCD1 pathological variant children carriers [38]. Primary adrenal insufficiency is characterized by high levels of adrenocorticotropic hormone (ACTH) and low cortisol level. The lifetime prevalence of adrenal insufficiency in ALD is about 80%. The cumulative probability of adrenal insufficiency is highest at the age of 10 years (46.8%) and remains prominent until 40 years of age (an additional 28.6%), decreasing substantially thereafter (an additional 5.6%) [39]. The incidence of adrenal insufficiency varies according to phenotype (see Table 27.1). According to van Geel et al. in a retrospective analysis in 35 of 70 patients with AMN, adrenocortical insufficiency was diagnosed before ALD, and in 33 patients dysfunction was diagnosed after ALD [14]. Sato et al. in a case report have shown that the demand for cortisol is extremely high in advanced adult-onset cerebral ALD. Even with mild infection, because cortisol secretion is limited in these patients, the risk of relative adrenal insufficiency despite normal serum cortisol levels warrants proactive administration of steroids when hyponatremia or hypoglycemia develops [40].
Patients with chronic adrenal insufficiency often have fatigue, anorexia, nausea, vomiting, loss of appetite, poor weight gain or weight loss, and abdominal symptoms. In an acute adrenal crisis, patients may present with hypotension, hypoglycemia, altered mental status, vomiting, and syncope, in addition to chronic symptoms. Salt wasting (hyponatremia and hyperkalemia) is less common with ALD, but patients are described to have impaired aldosterone response to ACTH stimulation and require mineralocorticoid replacement. Hyponatremia may also be present with severe cortisol deficiency, as there may be water retention due to a lack of cortisol inhibition of vasopressin secretion [36]. Corresponding with the relative sparing of the zona glomerulosa from VLCFA accumulation, mineralocorticoid function typically is less affected than glucocorticoid function [12].
Hypogonadism is noticed most frequently after neurologic or adrenal symptoms, but testicular dysfunction has been reported before the appearance of neurologic or adrenal symptoms. In a retrospective report of 26 men with ALD, 46% reported decreased libido and 58% had erectile dysfunction [41]. A prospective controlled study of 49 men with AMN revealed an 82% incidence of testicular dysfunction (elevated gonadotropins or low testosterone/luteinizing hormone ratio), and 54% with erectile dysfunction [42].
 Adrenal insufficiency may be absent
at the time of ALD diagnosis. In suspected cases, monitoring adrenal function is extremely important in order to secure the diagnosis and prevent Addisonian crisis.
Adrenal insufficiency may be absent
at the time of ALD diagnosis. In suspected cases, monitoring adrenal function is extremely important in order to secure the diagnosis and prevent Addisonian crisis.
Dermatologic Signs
Early-onset androgenetic alopecia despite hypogonadism and a diffuse reduction in scalp hair and the eyelashes are the main patterns of alopecia described in these patients [43]. Increased skin pigmentation may also be observed as a result of elevations of melanocyte-stimulating hormone, a byproduct of ACTH production. Common areas to note hyperpigmentation include palmar creases, axillae, genitalia, areolae, scars, gums, and the posterior helix of the ear [36]. After adrenarche, loss of pubic and axillary hair due to accumulation of VLCFA in the zona reticularis of the adrenal cortex and consequent poor androgen production may also be noted [36].
Radiologic Findings
Frequently, CT scan shows a symmetric hypodensity bilateral in parieto-occipital white matter with involvement of the splenium of the corpus callosum and enhancement seen along the anterior edge of hypodensity. MRI demonstrates T2/FLAIR hyperintense signal in the same areas as that on CT scan with hypo-intense signal on T1. There is no evidence of restricted diffusion or blooming on susceptibility-weighted images. Histopathologically, in brain lesions of cerebral ALD cases, three distinct zones of white matter involvement are seen. The inner zone is represented by scarring, while the intermediate inflammatory zone is represented by perivascular inflammatory cells and demyelination. Finally, a zone of ongoing demyelination is situated at the periphery, where myelin is breaking down in the absence of inflammation [44]. These areas are also observed in contrast MRI images, where the intermediate zone shows contrast enhancement in the “leading edge” due to ongoing inflammation [45].
Different radiological patterns have been recognized among patients with cerebral ALD: pattern 1, white matter in the parieto-occipital lobe or splenium of corpus callosum; pattern 2, white matter in the frontal lobe or genu of corpus callosum; pattern 3, primary involvement of frontopontine or corticospinal projection fibers without affecting the periventricular white matter; pattern 4, primary involvement of cerebellar white matter; and pattern 5, combined but separate initial involvement of frontal and parieto-occipital white matter. Whereas 80% of patients under 10 years of age presented with pattern 1, the overall frequency of this pattern was somewhat less common in older patients. For the group as whole, 137 (66%) patients presented with pattern 1, 32 (15.5%) with pattern 2, 24 (12%) with pattern 3, 2 (1%) with pattern 4, and 5 (2.5%) with pattern 5. The pattern 1 and 5 groups were on average the youngest, whereas patterns 2 and 4 presented mostly during adolescence, and pattern 3 during adulthood. Progression rates for patterns 1 and 2 were relatively rapid and similar, whereas progression in pattern 3 patients was slow. The progression in pattern 5 patients was extremely rapid [33].
Loes et al. proposed a 34-point brain MRI severity score for cerebral ALD, derived from location and extent of involvement, and the presence of focal and/or global atrophy [46]. This scale is used as a disease progression monitoring tool, with a score <4 considered very early stage, a score 4–8 representing early stage, a score 9–13 representing late stage, and a score of >13 representing advanced disease [47]. Its combination with the radiological pattern, presence of contrast enhancement, and age helped predict progression of lesions [47, 48]. Currently the “Loes scale” is the main radiological criteria used to determine viability for hematopoietic stem cell transplantation in cerebral ALD, with a score ≤ 8 points showing a higher likelihood of benefiting from this treatment [48].
In the pure form of AMN, imaging is dominated by spinal cord atrophy primarily affecting the thoracic cord [28, 49]. Imaging of the brain is either normal or demonstrates only minor abnormalities in the pyramidal tracts traversing the brainstem and internal capsules [28]. On the other hand, patients with AMN may have signs of concealed “arrested” cerebral ALD on MRI, which can help point to a diagnosis of AMN [5]. Liberato et al. described the brain MRI findings in 47 boys with asymptomatic ALD. They reported that 28/47 cases showed brain lesions. Among these cases, 22 had contrast enhancement [50].
Diagnosis
According to a case series reported by van Geel et al., the mean delay in diagnosis of all cases, from the time of onset of symptoms, was almost 10 years; delay was 17 years in adults with initial symptoms of adrenocortical insufficiency [51]. However, this reality is expected to change, because since 2006 a newborn screening test for ALD, using liquid chromatography-tandem mass spectroscopy (LC-MS/MS) measurement of C26:0-lysophosphatidylcholine (C26:0-LPC) in dried blood spot, has been available and already implemented in some regions [3]. This strategy allows pre-symptomatic identification of patients with ALD, close monitoring, and early intervention with hematopoietic stem cell transplantation and adrenal hormone therapy, thereby avoiding the devastating consequences of cerebral ALD and Addisonian crisis, respectively [52].
Usually, when the diagnosis of ALD is suspected based on clinical characteristics and/or brain imaging, plasma VLCFA levels are determined. VLCFA are elevated in almost all male ALD cases irrespective of age, disease duration, metabolic status, or clinical symptoms [53]. Most laboratories measure the concentration of total hexacosanoic acid (C26:0) in dried blood spots, the most frequently used parameter, and its ratio to tetracosanoic (C24:0) and docosanoic (C22:0) acids [11, 54]. The latter remains basically unchanged in plasma samples of ALD [53] (Table 27.2).
If ALD is suspected in a woman, the testing strategy should additionally include mutation analysis of the ABCD1 gene for the correct identification of heterozygous ALD females, because 15% of women with ALD have normal plasma VLCFA levels [9]. Family screening follows the same recommendations [28]. Plasma VLCFA levels strongly depend on dietary intake of VLCFA, for example, by the consumption of peanuts. Thus, blood leucocytes provide an alternative for confirmation of the diagnosis. Following the development of the whole blood spot LC-MS/MS, it has been shown that the C26:0-LPC assay accurately diagnoses males with ALD, and notably offers an accurate diagnostic test for women with ALD, with a reported sensitivity of 100% in 49 females and 126 controls [56].
VLCFA are similarly increased in other peroxisomal disorders such as the Zellweger syndrome spectrum or single enzyme defects of peroxisomal beta-oxidation (acyl-CoA oxidase deficiency and D-bifunctional protein deficiency). Hence mild atypical or late-onset variants of these diseases must be considered in the differential diagnosis, although other peroxisomal disorders can usually be excluded by measuring phytanic acid and plasmalogen levels [53].
In addition to the identification of female carriers and confirmation of the diagnosis in male patients, analysis of ABCD1 gene variants is also valuable to characterize ALD kindreds and for prenatal diagnosis [53]. To date, more than 849 non-recurrent ABCD1 mutations have been described, of which 46% are missense mutations [57]. The reported de novo mutation rate ranges from 5% to as high as 19% [58]. As an X-linked inherited disorder, all daughters of an affected male are obligate carriers, whereas his sons can never be affected. When a woman carries the gene for ALD, there is a 50% probability for each pregnancy that the gene is transmitted to a son or daughter. The frequency of de novo mutations in the index case is estimated to be around 4%, which indicates that the ABCD1 mutation occurred in the germ line. There is evidence of gonadal or gonosomal mosaicism in less than 1% of patients, which means an increased risk of an additional affected offspring. On occasions when no mutations can be detected by DNA sequence analysis, methods such as quantitative polymerase chain reaction, multiple ligation-dependent probe amplification, or Southern blot analysis have been used for recognition of large deletions, duplications, or chromosomal rearrangements [53]. Other tests should include serum ACTH and baseline cortisol levels (24-hour urine cortisol and A.M. and P.M. serum levels). If either is abnormal, an ACTH stimulation test should be performed to evaluate adrenal reserve. The adrenocortical insufficiency in ALD can be life-threatening if not treated, and all patients with ALD should have a regular reassessment of adrenocortical function if the initial results are normal. Routine adrenal testing every 4 to 6 months until 10 years of age, annual testing thereafter until 40 years of age, and solely on-demand testing in case endocrine symptoms manifest from age 41 years onward are recommended [39]. See Fig. 27.5 for a general guide to the diagnosis of X-ALD patients and their management.
Differential Diagnosis
In children with cerebral ALD, the main differential diagnoses are other childhood-onset leukodystrophies. The mnemonic “LACK Proper Myelin” may help clinicians to remember the main differential diagnoses among demyelinating leukodystrophies in the childhood (L, Leigh’s disease; A, Alexander’s disease and adrenoleukodystrophy; C, Canavan’s disease; K, Krabbe’s disease; P, Pelizaeus-Merzbacher disease; M, metachromatic leukodystrophy) [59]. Remarkably, as mentioned, VLCFA are also increased in other peroxisomal disorders, such as Zellweger syndrome, neonatal adrenoleukodystrophy, and infantile Refsum disease, but these disorders have a different clinical presentation and are rarely confused with ALD [11].
Adults with cerebral ALD should be differentiated from other demyelinating diseases, such as multiple sclerosis, but other adult-onset leukoencephalopathies should also be considered. The spinocerebellar form of ALD could mimic sporadic ataxias such as multiple system atrophy or adult-onset hereditary ataxias. Moreover, AMN could also present with ataxic features. Therefore, ALD should also be considered in the differential of ataxias. However, the most important differential diagnoses in patients with AMN are probably the many causes of spastic paraparesis. As mentioned, the presence of brain MRI abnormalities, family history, and the evidence of adrenal insufficiency could help in suspecting the diagnosis, although the diagnosis must still be considered even in the absence of these elements.
 Adult ALD patients may present with atypical phenotypes, such as pure spastic paraparesis mimicking familial spastic paraparesis, or ataxia-dysautonomia syndrome mimicking other neurodegenerative diseases.
Adult ALD patients may present with atypical phenotypes, such as pure spastic paraparesis mimicking familial spastic paraparesis, or ataxia-dysautonomia syndrome mimicking other neurodegenerative diseases.
Treatment
Currently used therapies for ALD include hormone replacement therapy, dietary therapy with Lorenzo’s oil, and hematopoietic cell transplantation.
Patients with adrenal abnormalities should be referred to an endocrinologist, as glucocorticoid and mineralocorticoid treatment should be monitored. Glucocorticoid therapy must be initiated in all patients with confirmed adrenal insufficiency. A recent clinical practice guideline on the treatment of primary adrenal insufficiency suggests the use of hydrocortisone (15–25 mg) or cortisone acetate (20–35 mg) in two or three divided oral doses per day. The highest dose should be given in the morning at awakening, the next either in the early afternoon (2 hours after lunch; two-dose regimen) or at lunch, and in the afternoon (three-dose regimen). As an alternative, prednisolone (3–5 mg/d), administered orally once or twice daily, is suggested. In patients with severe adrenal insufficiency symptoms or adrenal crisis, immediate therapy with intravenous hydrocortisone at an appropriate stress dose prior to the availability of the results of diagnostic tests is recommended [60]. Initiation of mineralocorticoid replacement therapy has been suggested only after clinical and/or biochemical evidence of mineralocorticoid deficiency [12].
Lorenzo’s oil is a formula of unsaturated fatty acids (glycerol trioleate C18:1 and glyceryl trierucate C22:1 in a 4:1 ratio); this formula may inhibit elongation of saturated fatty acids [1, 61]. Lorenzo’s oil combined with a VLCFA-poor diet has been shown to be helpful in normalizing plasma levels of VLCFA [61]. This combined therapy failed to arrest disease progression of AMN and pre-symptomatic patients in an open trial [62]. In an open single-arm trial of asymptomatic ALD patients with normal brain MRI, Moser et al., using Lorenzo’s oil combined with a moderate fat restriction diet, showed a reduced risk of developing MRI abnormalities and an association between the development of MRI abnormalities and a plasma C26:0 levels [63]. Other studies of untreated boys reported similar conversion rates as those reported on Lorenzo’s oil. There is no consistent evidence of disease-modifying effects of Lorenzo’s oil in AMN, nor a role in reducing the risk of brain lesions in cerebral ALD. A group of experts recommend that “the use of Lorenzo’s oil should only be undertaken by centers that have the ability to provide monitoring with MRI, nutritional guidance, and the ability to measure VLCFA and other essential fatty acids. Other centers consider the efficacy of Lorenzo’s oil unproven and do not recommend its use” [57].
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only therapeutic approach that can potentially arrest the neuroinflammatory demyelinating cerebral process of X-ALD in boys, particularly if the procedure is performed when patients have no neuropsychiatric compromise and limited extension of demyelinating lesions on brain MRI. After the transplantation procedure, demyelinating lesions may extend for 12 months to 18 months, and then their progression arrests. This interval is likely caused by the slow substitution of brain microglia with bone marrow-derived cells. Similar benefits of allogeneic HSCT have been demonstrated in adults with cerebral ALD. In already symptomatic patients, unfortunately, this procedure has not been shown to be effective in stopping the demyelinating process. More importantly, it can accelerate neurologic deterioration. Furthermore, allogeneic HSCT is associated with risks of graft-versus-host disease and prolonged immune deficiency, particularly in adults, and not all ALD patients have donors despite the availability of cord blood [64].
In practice, for the children up to 12 years of age, HSCT is mainly reserved for patients who present first with Addison’s disease or who are identified during genetic counseling, and in whom repeated brain MRI can detect the appearance of the beginning signs of cerebral demyelination. For adults, most transplanted patients were patients who initially had AMN and in whom repeated brain MRI detected early signs of cerebral demyelination.
Increased muscle tone is often severe and difficult to treat. Aggressive treatment is essential, since it causes pain, which in turn aggravates spasticity as well as dystonia in a vicious feedback circle that not only causes suffering but seriously lowers the quality of life of both the patient and his family. Symptomatic treatment is primarily the approach to spasticity, dystonia, and other complications in patients with ALD. Intrathecal baclofen seems to be effective for boys with the cerebral form of ALD with spasticity-dystonia who have not responded adequately to oral medication. It also can be considered as an early option in such cases in the hopes of preventing further complications [65]. Other therapeutic approaches remain under investigation.
 High VLCFA level is the standard biomarker for diagnosis in males, although less reliable in females. Genetic testing is available. Early hematopoietic stem cell transplantation can arrest brain demyelination/inflammation. However, there is no known cure for adrenomyeloneuropathy. Treatment is focused on hormone replacement and symptomatic treatment of spasticity.
High VLCFA level is the standard biomarker for diagnosis in males, although less reliable in females. Genetic testing is available. Early hematopoietic stem cell transplantation can arrest brain demyelination/inflammation. However, there is no known cure for adrenomyeloneuropathy. Treatment is focused on hormone replacement and symptomatic treatment of spasticity.
References
Berger J, Gärtner J. X-linked adrenoleukodystrophy: clinical, biochemical and pathogenetic aspects. Biochim Biophys Acta, Mol Cell Res. 1763;2006:1721–32.
Bezman L, Moser AB, Raymond GV, Piero Rinaldo, Watkins PA, Smith KD, et al. Adrenoleukodystrophy: incidence, new mutation rate, and results of extended family screening. Ann Neurol [Internet]. 2001;49:512–7. Available from: http://doi.wiley.com/10.1002/ana.101.
Vogel BH, Bradley SE, Adams DJ, D’Aco K, Erbe RW, Fong C, et al. Newborn screening for X-linked adrenoleukodystrophy in New York State: diagnostic protocol, surveillance protocol and treatment guidelines. Mol Genet Metab [Internet]. 2015;114:599–603. Available from: https://doi.org/10.1016/j.ymgme.2015.02.002.
Berger J, Forss-Petter S, Eichler FS. Pathophysiology of X-linked adrenoleukodystrophy. Biochimie [Internet]. 2014;98:135–42. Available from: https://doi.org/10.1016/j.biochi.2013.11.023.
Lin JE, Armour EA, Heshmati A, Umandap C, Couto JJ, Iglesias AD, et al. Pearls & Oy-sters: adolescent-onset adrenomyeloneuropathy and arrested cerebral adrenoleukodystrophy. Neurology. 2019;93:81–4.
Wang A.-G. X-Linked Adrenoleukodystrophy, in: A.-G. Wang (Ed.), Emergency Neuro-Ophthalmology: Rapid Case Demonstrations, Springer Singapore, Singapore, 2018: pp. 137–141. https://doi.org/10.1007/978-981-10-7668-8.
Engelen M, Kemp S, Poll-The BT. X-linked adrenoleukodystrophy: pathogenesis and treatment. Curr Neurol Neurosci Rep. 2014;14:1–8.
Paláu-Hernández S, Rodriguez-Leyva I, Shiguetomi-Medina JM. Late onset adrenoleukodystrophy: a review related clinical case report. eNeurologicalSci [Internet]. Elsevier; 2019;14:62–7. Available from: https://doi.org/10.1016/j.ensci.2019.01.007.
Moser HW, Mahmood A, Raymond GV. X-linked adrenoleukodystrophy. Nat Clin Pract Neurol. 2007;3:140–51.
Griffin DE, Moser HW, Mendoza Q, Moench TR, O’Toole S, Moser AB. Identification of the inflammatory cells in the central nervous system of patients with adrenoleukodystrophy. Ann Neurol. 1985;18:660–4.
Moser HW, Krieger K. Adrenoleukodystrophy: phenotype, genetics, pathogenesis and therapy* dedicated to the memory of Peter Moser. Brain. 1997;120:1485–508.
Zhu J, Eichler F, Biffi A, Duncan CN, Williams DA, Majzoub JA. The changing face of adrenoleukodystrophy. Endocr Rev [Internet]. 2020;1–29. Available from: https://academic.oup.com/edrv/advance-article/doi/10.1210/endrev/bnaa013/5828725.
Kemp S, Huffnagel IC, Linthorst GE, Wanders RJ, Engelen M. Adrenoleukodystrophy - Neuroendocrine pathogenesis and redefinition of natural history. Nat Rev Endocrinol [Internet]. 2016;12:606–15. Available from: https://doi.org/10.1038/nrendo.2016.90.
Van Geel BM, Bezman L, Loes DJ, Moser HW, Raymond GV. Evolution of phenotypes in adult male patients with X-linked adrenoleukodystrophy. Ann Neurol. 2001;49:186–94.
Huffnagel IC, Van Ballegoij WJC, Van Geel BM, Vos JMBW, Kemp S, Engelen M. Progression of myelopathy in males with adrenoleukodystrophy: towards clinical trial readiness. Brain. 2019;142:334–43.
Edwin D, Speedie LJ, Kohler W, Naidu S, Kruse B, Moser HW. Cognitive and brain magnetic resonance imaging findings in adrenomyeloneuropathy. Ann Neurol. 1996;40:675–8.
Azar C, Nadjar Y. First report of young women presenting with severe form of adrenomyeloneuropathy. J Neurol Sci [Internet]. 2019;405:79. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022510X19321860.
Moser HW, Moser AB, Naidu S, Bergin A. Clinical aspects of adrenoleukodystrophy and adrenomyeloneuropathy. Dev Neurosci [Internet]. 1991;13:254–61. Available from: https://www.karger.com/Article/FullText/112170.
Van de Stadt SIW, Van Ballegoij JWC, Labounek R, Huffnagel IC, Kemp S, Nestrasil I, et al. Spinal cord atrophy as a measure of severity of myelopathy in adrenoleukodystrophy., J. Inherit. Metab. Dis. 2020;43:852–60. https://doi.org/10.1002/jimd.12226.
Maris T, Androulidakis EJ, Tzagournissakis M, Papavassiliou S, Moser H, Plaitakis A. X-linked adrenoleukodystrophy presenting as neurologically pure familial spastic paraparesis. Neurology. 1995;45:1101–4.
Shaw-Smith CJ, Lewis SJG, Reid E. X-linked adrenoleukodystrophy presenting as autosomal dominant pure hereditary spastic paraparesis. J Neurol Neurosurg Psychiatry. 2004;75:686–8.
Zhan Z Xiong, Liao X Xin, Du J, Luo Y Ying, Hu Z Ting, Wang J Ling, et al. Exome sequencing released a case of X-linked adrenoleukodystrophy mimicking recessive hereditary spastic paraplegia. Eur J Med Genet [Internet]. 2013;56:375–8. Available from: https://doi.org/10.1016/j.ejmg.2013.04.008.
Hofereiter J, Smith MD, Seth J, Tudor KI, Fox Z, Emmanuel A, et al. Bladder and bowel dysfunction is common in both men and women with mutation of the ABCD1 gene for X-linked adrenoleukodystrophy. JIMD Rep [Internet]. 2015;77–83. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/8904_2015_414.
Gomery P, Corre C, Eichler F. Urinary and Bowel symptoms in adult patient with adrenoleukodystrophy. Neurology. 2018;90:464.
Zhang Y, Guo D, Tang Y. Autonomic dysfunction in a patient with X-linked adrenoleukodystrophy. Int J Neurosci [Internet]. 2018;128:783–4. Available from: https://doi.org/10.1080/00207454.2017.1405953.
Schulte-Mattler W, Lindner A, Zierz S. Autonomic neuropathy in a patient with adrenomyeloneuropathy. Eur J Med Res. 1996;1:559–61.
Chen YH, Lee YC, Tsai YS, Guo YC, Hsiao CT, Tsai PC, et al. Unmasking adrenoleukodystrophy in a cohort of cerebellar ataxia. PLoS One. 2017;12:1–14.
Engelen M, Kemp S, De Visser M, Van Geel BM, Wanders RJA, Aubourg P, et al. X-linked adrenoleukodystrophy (X-ALD): clinical presentation and guidelines for diagnosis, follow-up and management. Orphanet J Rare Dis. 2012;7:1–14.
Traboulsi EI, Maumenee IH. Ophthalmologic manifestations of X-linked childhood adrenoleulcodystrophy. Ophthalmology. 1987;94:47–52.
Brown FR, Moser HW, Cohen SMZ, Green WR, de la Cruz ZC, Luckenbach MW, et al. Ocular histopathologic studies of neonatal and childhood adrenoleukodystrophy. Am J Ophthalmol. 1983;95:82–96.
Korenke GC, Pouwels PJW, Frahm J, Hunneman DH, Stoeckler S, Krasemann E, et al. Arrested cerebral adrenoleukodystrophy: a clinical and proton magnetic resonance spectroscopy study in three patients. Pediatr Neurol. 1996;15:103–7.
Rosebush PI, Garside S, Levinson AJ, Mazurek MF. The neuropsychiatry of adult-onset adrenoleukodystrophy. J Neuropsychiatry Clin Neurosci [Internet]. 1999;11:315–27. Available from: http://psychiatryonline.org/doi/abs/10.1176/jnp.11.3.315.
Loes DJ, Fatemi A, Melhem ER, Gupte N, Bezman L, Moser HW, et al. Analysis of MRI patterns aids prediction of progression in X-linked adrenoleukodystrophy. Neurology. 2003;61:369–74.
Au LWC, Chan AYY, Mok VCT. Teaching NeuroImages: X-linked adrenoleukodystrophy: spinocerebellar variant. Neurology. 2019;93:E731–2.
Ogaki K, Koga S, Aoki N, Lin W, Suzuki K, Ross OA, et al. Adult-onset cerebello-brainstem dominant form of X-linked adrenoleukodystrophy presenting as multiple system atrophy: case report and literature review. Neuropathology [Internet]. 2016;36:64–76. Available from: http://doi.wiley.com/10.1111/neup.12230.
Burtman E, Regelmann MO. Endocrine dysfunction in X-linked adrenoleukodystrophy. Endocrinol Metab Clin North Am [Internet]. 2016;45:295–309. Available from: https://doi.org/10.1016/j.ecl.2016.01.003.
Aubourg P, Chaussain JL. Adrenoleukodystrophy: The most frequent genetic cause of Addison’s disease. Horm Res. 2003;59:104–5.
Dubey P, Raymond GV, Moser AB, Kharkar S, Bezman LMH. Adrenal insufficiency in asymptomatic long-chain fatty acid screening. J Pediatr. 2005;146:528–32.
Huffnagel IC, Laheji FK, Aziz-Bose R, Tritos NA, Marino R, Linthorst GE, et al. The natural history of adrenal insufficiency in X-linked adrenoleukodystrophy: an international collaboration. J Clin Endocrinol Metab. 2019;104:118–26.
Sato T, Umehara T, Nakahara A, Oka H. Relative adrenal insufficiency in adult-onset cerebral X-linked adrenoleukodystrophy. Neurol Clin Pract [Internet]. 2017;7:398–400. Available from: http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000310.
Assies J, Gooren LJG, Van Geel B, Barth PG. Signs of testicular insufficiency in adrenomyeloneuropathy and neurologically asymptomatic X-linked adrenoleukodystrophy: a retrospective study. Int J Androl [Internet]. 1997;20:315–21. Available from: http://doi.wiley.com/10.1046/j.1365-2605.1997.00066.x.
Brennemann W, Köhler W, Zierz S, Klingmüller D. Testicular dysfunction in adrenomyeloneuropathy. Eur J Endocrinol. 1997;137:34–9.
König A, Happle R, Tchitcherina E, Schaefer JR, Sokolowski P, Köhler W, et al. An X-linked gene involved in androgenetic alopecia: a lesson to be learned from adrenoleukodystrophy. Dermatology. 2000;200:213–8.
Schaumburg H, Poewers J, Raine C, Suzuki K, Richardson E. Adrenoleukodystrophy a clinical and pathological study of 17 cases. Arch Neurol. 1975;32:577–91.
Eichler F, Mahmood A, Loes D, Bezman L, Lin D, Moser HW, et al. Magnetic resonance imaging detection of lesion progression in adult patients with X-linked adrenoleukodystrophy. Arch Neurol. 2007;64:659–64.
Loes DJ, Hite S, Moser H, Stillman AE, Shapiro E, Lockman L, et al. Adrenoleukodystrophy: a scoring method for brain MR observations. Am J Neuroradiol. 1994;15:1761–6.
Turk BR, Moser AB, Fatemi A. Therapeutic strategies in adrenoleukodystrophy. Wien Med Wochenschr. 2017;167:219–26.
Bladowska J, Kulej D, Biel A, Zimny A, Kałwak K, Owoc-Lempach J, et al. The role of MR imaging in the assessment of clinical outcomes in children with x-linked adrenoleukodystrophy after allogeneic haematopoietic stem cell transplantation. Polish J Radiol. 2015;80:181–90.
Resende LL, de Paiva ARB, Kok F, Leite C da C, Lucato LT. Adult leukodystrophies: a step-by-step diagnostic approach. Radiographics. 2019;39:153–68.
Liberato AP, Mallack EJ, Aziz-Bose R, Hayden D, Lauer A, Caruso PA, et al. MRI brain lesions in asymptomatic boys with X-linked adrenoleukodystrophy. Neurology. 2019;92:e1698–708.
van Geel BM, Assies J, Haverkort EB, Barth PG, Wanders RJA, Schutgens RBH, et al. Delay in diagnosis of X-linked adrenoleukodystrophy. Clin Neurol Neurosurg. 1993;95:115–20.
Turk BR, Theda C, Fatemi A, Moser AB. X-linked adrenoleukodystrophy: pathology, pathophysiology, diagnostic testing, newborn screening, and therapies. Int J Dev Neurosci [Internet]. 2019. Available from: https://doi.org/10.1016/j.ijdevneu.2019.11.002.
Wiesinger C, Eichler FS, Berger J. The genetic landscape of X-linked adrenoleukodystrophy: inheritance, mutations, modifier genes, and diagnosis. Appl Clin Genet. 2015;8:109–21.
Hubbard WC, Moser AB, Liu AC, Jones RO, Steinberg SJ, Lorey F, et al. Newborn screening for X-linked adrenoleukodystrophy (X-ALD): validation of a combined liquid chromatography-tandem mass spectrometric (LC-MS/MS) method. Mol Genet Metab [Internet]. 2009;97:212–20. Available from: https://doi.org/10.1016/j.ymgme.2009.03.010.
Steinberg S, Jones R, Tiffany C, Moser A. Investigational methods for peroxisomal disorders. Curr Protoc Hum Genet. 2008;58(1):17.6.1–17.6.23.
Huffnagel IC, van de Beek MC, Showers AL, Orsini JJ, Klouwer FCC, Dijkstra IME, et al. Comparison of C26:0-carnitine and C26:0-lysophosphatidylcholine as diagnostic markers in dried blood spots from newborns and patients with adrenoleukodystrophy. Mol Genet Metab [Internet]. 2017;122:209–15. Available from: https://doi.org/10.1016/j.ymgme.2017.10.012.
Engelen M, Salzman R, Bonnamain V, Kemp S. The ALD mutation database [Internet]. 2019. Available from: https://adrenoleukodystrophy.info/mutations-biochemistry/mutation-statistics.
Horn MA, Retterstøl L, Abdelnoor M, Skjeldal OH, Tallaksen CME. Adrenoleukodystrophy in Norway: high rate of De Novo mutations and age-dependent penetrance. Pediatr Neurol [Internet]. 2013;48:212–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0887899412006789.
Myelin LP. Pediatric radiology originals Dysmyelinating leukodystrophies: “LACK Proper Myelin”. Pediatr Radiol. 1991:477–82.
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364–89.
Moser HW, Moser AB, Hollandsworth K, Brereton NH, Raymond G V. “Lorenzo’s Oil” therapy for X-linked adrenoleukodystrophy: rationale and current assessment of efficacy. J Mol Neurosci [Internet]. 2007;33:105–13. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s12031-007-0041-4.
Aubourg P, Adamsbaum C, Lavallard-Rousseau M-C, Rocchiccioli F, Cartier N, Jambaque I, et al. A two-year trial of Oleic and Erucic Acids (“Lorenzo’s Oil”) as treatment for adrenomyeloneuropathy. N Engl J Med [Internet]. 1993;329:745–52. Available from: http://www.nejm.org/doi/pdf/10.1056/NEJM199309303291401.
Moser HW, Raymond GV, Lu S-E, Muenz LR, Moser AB, Xu J, et al. Follow-up of 89 asymptomatic patients with adrenoleukodystrophy treated with Lorenzo’s Oil. Arch Neurol [Internet]. 2005;62:1073. Available from: http://archneur.jamanetwork.com/article.aspx?doi=10.1001/archneur.62.7.1073.
Cartier N, Aubourg P. Hematopoietic stem cell transplantation and hematopoietic stem cell gene therapy in X-linked adrenoleukodystrophy. Brain Pathol. 2010;20:857–62.
Hjartarson HT, Ehrstedt C, Tedroff K. Intrathecal baclofen treatment an option in X-linked adrenoleukodystrophy. Eur J Paediatr Neurol [Internet]. 2018;22:178–81. Available from: https://doi.org/10.1016/j.ejpn.2017.09.003.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
A 28-year-old man with a 5-year history of progressive spastic paraparesis of unknown etiology, with comorbid sphincter and sexual dysfunction, was evaluated urgently because of a 3-day history of marked exacerbation of spasticity in his lower limbs, followed by two syncopal episodes, emesis, vegetative symptoms, and finally psychomotor agitation. At the ED he was noted to be agitated and confused. He had no fever, but his vital signs were remarkable for hypotension and tachycardia. Brain CT and CSF analysis were unremarkable. His clinical picture progressed with persistent hypotension, hypoglycemia, hyponatremia, hyperkalemia, and a low cortisol level. Suprarenal insufficiency was confirmed, and he was started on steroid replacement, along with correction of hypoglycemia and electrolyte imbalance. While his mentation slowly improved, his spasticity with severe spasms persisted. Neurological and general evaluation during admission was remarkable for hyperpigmented skin and gums, frontotemporal alopecia, cognitive slowness, spastic paraparesis-dystonic syndrome, and mild ataxia with hypermetric saccades, mild dysmetria, dysdiadochokinesia, and dyssynergia, with generalized hyperreflexia and bilateral Babinski signs. His MRI showed signal changes in parieto-occipital deep white matter and splenium of the corpus callosum. Based on the clinical and radiological characteristics, along with elevated very long chain fatty acids (VLCFA) levels, X-linked adrenoleukodystrophy was confirmed (MP4 77805 kb)
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Salles, P.A., Fernandez, H.H. (2022). X-Linked Adrenoleukodystrophy: Addisonian Crisis in a Patient with Spastic Paraparesis-Ataxia Syndrome. In: Frucht, S.J. (eds) Movement Disorder Emergencies. Current Clinical Neurology. Humana, Cham. https://doi.org/10.1007/978-3-030-75898-1_27
Download citation
DOI: https://doi.org/10.1007/978-3-030-75898-1_27
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-75897-4
Online ISBN: 978-3-030-75898-1
eBook Packages: MedicineMedicine (R0)