Abstract
Computed tomography (CT) is a digital radiological modality which has been classified as the largest source of medical radiation exposure. In this study, we estimated the effective dose to patients undergoing CT examinations using information obtained from DICOM images, including tube current, patient size and positioning, collimation etc. The custom code was used to calculate the conversion factors between an effective dose and air kerma length product. Their values are 0.0232 mSv/(mGy cm) and 0.0263 mSv/(mGy cm), for male and female patients, respectively. The effective dose for the whole-body CT is estimated to be 8.7 mSv.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Computed tomography (CT) is a digital radiological modality that has certainly made the biggest change in diagnostic radiology since the discovery of x-rays. Previous planar radiological methods hid the third dimension of the human body, so a large number of morphological changes in the body could not be noticed. Despite its benefits, CT examination is always accompanied by radiation exposure of the patient.
Concerns about radiation risk due to CT examinations are rising in both the medical physics community and the general public. Cohort studies investigating stochastic effects of radiation exposure from CT scans are being still being published [1, 2]. CT imaging and interventional procedures have been classified as the largest source of medical radiation exposure. The effective dose in CT-guided interventions can easily exceed 100 mSv [3]. National Council on Radiation Protection and Measurements (NCRP) Report 184 estimates that effective dose per capita in the United States of America is 1.45 mSv [4, 5]. The value has not changed much since 2010, indicating that the rapid increase in collective effective dose from CT examinations that happened since the introduction of multislice CT scanners has stopped [6]. We could argue that the same trend is being witnessed in other nations on a similar healthcare level.
Many institutions are actively developing dose control programs to make more responsible use of computed tomography and to avoid unnecessary exposure to ionizing radiation [7,8,9]. Such programs automatically extract values relevant for direct assessment of patient exposure from patient dosimetry reports, such as volume computed tomography air kerma index CVOL or CT air kerma-length product PKL,CT, and monitor changes in their value over time.
However, these values are related to measurements on the dosimetry phantom and do not provide information on the actual patient dose, and therefore cannot be compared to doses in other diagnostic modalities or different patient sizes.
One way to solve this problem is to convert CVOL to organ doses using conversion factors labeled h. These factors have been shown to be exponentially dependent on body diameter. For organs that are fully covered by the primary radiation beam, the h factors do not depend much on the scan parameters and the CT device model [10]. These properties suggest the need to incorporate conversion factors h into direct patient exposure assessment programs to allow control of organ doses for individual patients. Several research groups have examined how changes in tube current affect dose and conversion factors [11,12,13,14,15,16,17,18].
There are significant differences in the implementation of tube current modulation (TCM) technology among different manufacturers of CT devices. Some manufacturers aim to provide a unique image noise for all body regions and patient sizes, while others aim to reduce the dose for the patient by allowing slightly higher noise for larger patients [19]. New technologies allow organ-based TCM which is capable of anterior and total dose reduction with minimal loss of image quality [20].
The dependence of the h factor on the modulation schemes was investigated in the study of Li et al. which focused on examinations of the thorax, abdomen, and pelvis, which are examinations in which TCM is most commonly used. In the conclusion of this paper, it was pointed out that ignoring the modulation of the anode current when estimating the dose to a patient can lead to errors reaching values in the order of 200% [10].
However, the dose estimate also depends on the selected modulation strength, the choice of scanning protocol, such as minimum and maximum anode current, and the current modulation method itself, which is based on the patient’s scans and is a trade secret from the CT manufacturer. Taking all the above into account, it is impossible to give a universal way of estimating the effective dose and the dose to individual organs using the mean value CVOL.
2 Materials and Methods
In this study, the effective dose and the dose to individual organs in wholebody CT were estimated using tube current values extracted from the header of DICOM images. In the process of data collection, a software has been designed that can extract tube current values from tomographic images, apply conversion factors, and use readily available Monte Carlo data from CTVoxDos software to estimate the effective dose to the patient. CTVoxDos software dose estimations are based on the scheme of Schlattl et al. [15, 21, 22]. In this study we used voxel computational phantoms RCP-AM and RCP-AF, which correspond to an average male and female body, respectively. Body mass and height of RCP-AM is 73 kg and 177.6 cm, respectively, while for RCP-AF these values are 60 kg and 168.4 cm. To examine the influence of these values on E we followed this basic idea:
-
–
obtain conversion factors ki(zi) between the effective dose per slice Ei(zi) and CVOL from CTVoxDos;
-
–
obtain Ii(zi) from DICOM images for a group of patients that performed whole-body CT;
-
–
interpolate values of Ii(zi) to match positions zi on the phantom, and adjust for different body parts proportions;
-
–
calculate CVOL,i from tube current using nCVOL;
-
–
multiply the obtained value with slice width ∆z and divide with pitch factor p;
-
–
calculate the effective dose as:
 (1)
(1)
Although there might be other convenient solutions to get the values of tube current from DICOM images, we used the command-line software dicom2 (Sebastien Barre, 2007), as an accessory for our own code. Visual Basic in Microsoft Access was used to run dicom2, store collected data, perform necessary calculations, as well as to organize results.
3 Results and Discussion
Table 1 shows the height (m), body mass (kg) and age of the patients included in this study. Twenty-eight out of 53 patients (52.8%) were female and 25 male (47.2%). Average height of patients was 1.72 m (σ = 0.10 m) with body mass of 74 kg (σ = 16 kg). Most of the patients were normally sized according to the WHO classification of body mass index. Height of patients does not differ significantly from computational phantom size. According to the two-tailed one sample t-test, p-values for males and females are 0.5379 and 0.1422, respectively. Body mass, however, is slightly higher, with p-values equal to 0.0003 and 0.0214 for male and female patients, respectively.
The median age of the female patient group was 53 years (IQR = 28y) which did not significantly differ (Mann-Whitney U test, p = 0.358) from the median age of male patients, which was 57 years (IQR = 14y).
Within the statistical data processing, the analysis of the correlation between certain quantities was performed. As the body mass index increases, so does the anode current, and thus the CVOL and PKL,CT (Table 2). The obtained results were expected and confirm that the software that modulates the anode current adjusts the scan parameters to match patient body size.
The average value of CVOL is 3.0 mGy (IQR = 2.0 mGy), and the tube current read for images is 65.8 mA (IQR = 45.6 mA). The statistically significant correlation was found between tube current I and CVOL, which is shown in the Fig. 1. The figure confirms the theoretical linear relationship between the tube loading (product of anode current and exposure time, PIt) and air kerma, which is in this case represented by CVOL.
Using software developed for this study, data on scanning parameters were obtained that cannot be read directly from the device console or the process would take a very long time. Values of table position z and anode current I were loaded from the header of a series of DICOM files (tomographic images). A series of transformations have been performed for z to match specific positions on the computational phantom and adjust for different body parts proportions.
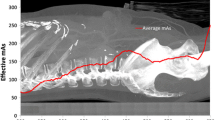
The final results (z vs. median I) are presented in the figure, where shaded areas represent the interval between 1st and 3rd quartile (Fig. 2).
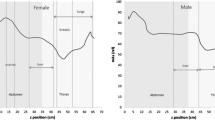
The anode current is greatest in the pelvic region when the pelvic and hip bones are in the beam. The current is the lowest in the head region. However, we notice that the value of I increases unexpectedly near the scalp. The reason for this is the inability of the software to estimate the adequate value of the anode current when single projection radiograph (SPR or scout) does not cover the entire patient head. Due to the lack of input data at the beginning of the scan, software resorts to a solution that will certainly give a picture of satisfactory quality. Hence, the tube current is increased to its maximum permissible value. Figure 3 shows the effective dose E to patients after whole-body CT vs. PKL,CT for males and females. The conversion factor k can be read from the equations describing the linear regression curves. For male patients k = 0.0232 mSvmGy−1cm−1, and for female patients k = 0.0263 mSvmGy−1cm−1.
The slope or linear regression coefficients (a) can be used to convert PKL,CT to effective dose E after whole-body CT. For male patients, it has the value of 0.0232 mSvmGy−1cm−1, and for females 0.0263 mSvmGy−1cm−1. We should have in mind that this method is valid only for one protocol of one CT manufacturer. There is no universal conversion factor for all protocols and all CT device manufacturers [23]. It should be noted that the tube current values drop to minimum in the leg region. Hence, the average CVOL is lower than the value observed in the regions of radiosensitive organs. Depending on the protocol, these differences can have significant impact on the overall conversion factor.
Other methods of obtaining the conversion factor can be found in the literature for devices that use anode current modulation. In the study of Kawaguchi et al. for CT devices Toshiba Aquilion 64 and Aquilion RXL, the doses obtained did not differ significantly from the doses obtained via PKL,CT conversion factor [24].
To estimate the final value of effective dose to patients undergoing whole body CT, we used the obtained conversion factors, multiplied them with average PKL,CT for male and female patients, and calculated the average between two. Finally, the effective dose for whole-body CT is estimated to be 8.7 mSv, which is comparable to values found in the literature [25,26,27].
4 Conclusions
This study has shown that more accurate estimation of effective dose to patients undergoing CT examinations could be done using information obtained from DICOM images, including tube current, patient size and positioning, collimation etc. We managed to extract necessary data and calculate the required conversion factors using the custom code which ran images taken from 53 patients. The obtained conversion factor between an effective dose and PKL,CT is 0.0232 mSvmGy−1cm−1 and 0.0263 mSvmGy−1cm−1, for male and female patients, respectively. The effective dose for whole body CT is estimated to be 8.7 mSv.
References
Huang, R., Liu, X., He, L., Zhou, P.K.: Dose-Response 18(2) (2020). https://doi.org/10.1177/1559325820923828. PMID: 32425727
Pearce, M.S., Salotti, J.A., Little, M.P., McHugh, K., Lee, C., Kim, K.P., Howe, N.L., Ronckers, C.M., Rajaraman, P., Craft, A.W., Parker, L., Berrington de González, A.: Lancet 380(9840), 499 (2012). https://doi.org/10.1016/S0140-6736(12)60815-0
Arellano, R., Yang, K., Rehani, M.: Eur. Radiol. 1–6 (2020)
NCRP, Report no. 184 – medical radiation exposure of patients in the United States. Technical Report, National Council on Radiation Protection and Measurements, Bethesda, MD (2019)
Mettler, F.A., Mahesh, M., Bhargavan-Chatfield, M., Chambers, C.E., Elee, J.G., Frush, D.P., Miller, D.L., Royal, H.D., Milano, M.T., Spelic, D.C., Ansari, A.J., Bolch, W.E., Guebert, G.M., Sherrier, R.H., Smith, J.M., Vetter, R.J.: Radiology 295(2), 418 (2020). https://doi.org/10.1148/radiol.2020192256. PMID: 32181730
Einstein, A.J.: Radiology 295(2), 428 (2020). https://doi.org/10.1148/radiol.2020200200. PMID: 32186459
Cook, T.S., Zimmerman, S., Maidment, A.D., Kim, W., Boonn, W.W.: J. Am. Coll. Radiol. 7(11), 871 (2010)
Li, X., Zhang, D., Liu, B.: Am. J. Roentgenol. 196(6), W781 (2011)
Christianson, O., Li, X., Frush, D., Samei, E.: Med. Phys. 39(11), 7131 (2012)
Li, X., Segars, W.P., Samei, E.: Phys. Med. Biol. 59(16), 4525 (2014)
Huda, W., Ogden, K.M., Khorasani, M.R.: Radiology 248(3), 995 (2008)
van Straten, M., Deak, P., Shrimpton, P.C., Kalender, W.A.: Med. Phys. 36(11), 4881 (2009)
Angel, E., Yaghmai, N., Jude, C.M., DeMarco, J.J., Cagnon, C.H., Goldin, J.G., McCollough, C.H., Primak, A.N., Cody, D.D., Stevens, D.M., et al.: AJR. Am. J. Roentgenol. 193(5), 1340 (2009)
Angel, E., Yaghmai, N., Jude, C.M., DeMarco, J.J., Cagnon, C.H., Goldin, J.G., Primak, A.N., Stevens, D.M., Cody, D.D., McCollough, C.H., et al.: Phys. Med. Biol. 54(3), 497 (2009)
Schlattl, H., Zankl, M., Becker, J., Hoeschen, C.: Phys. Med. Biol. 55(20), 6243 (2010)
Khatonabadi, M., Zhang, D., Mathieu, K., Kim, H.J., Lu, P., Cody, D., DeMarco, J.J., Cagnon, C.H., McNitt-Gray, M.F.: Med. Phys. 39(8), 5212 (2012)
Khatonabadi, M., Kim, H.J., Lu, P., McMillan, K.L., Cagnon, C.H., DeMarco, J.J., McNitt-Gray, M.F.: Med. Phys. 40(5), 051903 (2013)
Rupcich, F., Badal, A., Kyprianou, I., Schmidt, T.G.: Med. Phys. 39(9), 5336 (2012)
Kalra, M.K., Maher, M.M., Toth, T.L., Schmidt, B., Westerman, B.L., Morgan, H.T., Saini, S.: Radiology 233(3), 649 (2004). https://doi.org/10.1148/radiol.2333031150. URL https://bit.ly/Q2x7Mr
Mussmann, B., Mørup, S., Skov, P., Foley, S., Brenøe, A., Eldahl, F., Jørgensen, G., Precht, H.: Radiography (2020). https://doi.org/10.1016/j.radi.2020.04.011
Schlattl, H., Zankl, M., Becker, J., Hoeschen, C.: Phys. Med. Biol. 57(20), 6309 (2012)
Fehrmann, M.L., Schegerer, A., Werncke, T., Schlattl, H.: Radiat. Prot. Dosimetry 190(1), 71 (2020). https://doi.org/10.1093/raddos/ncaa070
Christner, J.A., Kofler, J.M., McCollough, C.H.: Am. J. Roentgenol. 194(4), 881 (2010)
Kawaguchi, A., Matsunaga, Y., Kobayashi, M., Suzuki, S., Matsubara, K., Chida, K.: Radiat. Prot. Dosimetry 167(4), 562 (2014). https://doi.org/10.1093/rpd/ncu340
Alkhybari, E.M., McEntee, M.F., Brennan, P.C., Willowson, K.P., Kench, P.L.: J. Med. Imag. Radiat. Oncol. 63(3), 291 (2019). https://doi.org/10.1111/1754-9485.12857
Sabri, A.S.A., Wong, J.H.D.: J. Phys.: Conf. Ser. 1248, 012006 (2019). https://doi.org/10.1088/1742-6596/1248/1/012006
Sato, T., Saito, Y., Saito, N., Ooba, M.: Nihon Hoshasen Gijutsu Gakkai zasshi 73(4), 258—266 (2017). https://doi.org/10.6009/jjrt.2017_jsrt_73.4.258
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Beganović, A., Stabančić-Dragunić, S., Odžak, S., Skopljak-Beganović, A., Jašić, R., Sefić-Pašić, I. (2021). Estimation of Effective Doses to Patients in Whole Body Computed Tomography with Automatic Tube Current Modulation Systems. In: Badnjevic, A., Gurbeta Pokvić, L. (eds) CMBEBIH 2021. CMBEBIH 2021. IFMBE Proceedings, vol 84. Springer, Cham. https://doi.org/10.1007/978-3-030-73909-6_86
Download citation
DOI: https://doi.org/10.1007/978-3-030-73909-6_86
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73908-9
Online ISBN: 978-3-030-73909-6
eBook Packages: EngineeringEngineering (R0)