Abstract
When possible, preservation of the epiphysis in tumors of the proximal tibia is a good option to avoid arthroplasty or arthrodesis in immature patients. Cañadell’s technique (epiphysiolysis before resection of metaphyseal sarcomas) was designed for preserving the joint and most of the growth plate, thus avoiding future complications such as loosening or wear, limb length discrepancy, and revision surgeries (Cañadell J, Forriol F, Cara JA, J Bone Joint Surg Br. 76:127–132, 1994). Distraction-epiphysiolysis makes resection easier by providing a safe margin; only a diaphyseal osteotomy is needed. The reconstruction with autologous bone provides better long-term results. In this case, we used the contralateral tibia and fibula.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bone sarcoma
- Biological reconstruction
- Epiphysiolysis
- Cañadell’s technique
- Autograft
- Osteosarcoma
- Ewing Sarcoma
1 Basic Clinical History
A 4-year-old girl presented to our Department in 2003 after amputation was advised elsewhere because of diagnosis of proximal tibia Ewing’s sarcoma with continuous pain and swelling in her left knee. She had been treated with a standard protocol of chemotherapy with a good response. X-ray showed a sclerotic lesion with periosteal reaction in the proximal metaphysis of the tibia. No distant metastases were found. MRI showed a metaphyseal lesion with soft tissue mass, but no invasion of the epiphysis, making this patient suitable for Cañadell’s technique [1, 2]. After neoadjuvant chemotherapy, the tissue mass disappeared.
2 Preoperative Images
See Fig. 28.1.
3 Preoperative Problem List
To decide:
-
(a)
Is the articular joint affected?
-
(b)
Is the epiphysis free of tumor?
-
(c)
Is the extensor mechanism affected?
-
(d)
Is the growth plate able to continue growing after treatment?
-
(e)
Given the possibilities of complications, is it worthy to preserve this limb?
4 Treatment Strategy
-
First stage: Placing a monolateral external fixator for physeal distraction at a rate of 1 mm/day until the growth plate breaks (usually 8–10 days). Hospitalization is not needed in this step. We usually advise the parents that the patient will have pain and schedule the follow-up X-ray and surgery 10–15 days after placing the fixator.
-
Second stage: Resection and biological reconstruction: en-bloc resection is performed by doing a diaphyseal osteotomy and the reconstruction is done with nonvascularized autograft from the contralateral tibia and fibula. The joint, the extensor mechanism, and growth plate are preserved. The grafts are stabilized with the same external fixator.
5 Basic Principles
-
Growth plate can be a barrier to tumoral spread in selected cases.
-
Preoperative planning is mandatory with an actual MRI previous to surgery. Imaging methods are very reliable in assessing whether the growth plate and the epiphysis are free of tumor.
-
The insertion of the patellar tendon in the anterior tibia tuberosity is retained in the epiphysis as the growth plate lies inferior in the anterior zone.
-
Family cooperation is needed for the external fixator care.
-
Rehabilitation is started in 48 h.
6 Photos and Imaging During Treatment
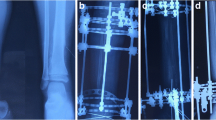
See Figs. 28.2, 28.3, 28.4, 28.5.
(a, b) Intraoperative picture of the resection. Diaphyseal osteotomy is performed. The metaphyseal “osteotomy” is already done. You just have to cut the perichondrium with a knife. A small layer of growth plate at the metaphyseal side is a safe margin of resection, whilst most of the physis remain together with the epiphysis inside the patient. Subsequent histopathological analysis showed 100% of necrosis. No radiation was employed
X-ray just before removing the external fixation confirming graft healing. Reconstruction was done with autologous tibia and fibula from the contralateral leg and temporarily stabilized with the same external fixator. She continued with the external fixator 4 months until healing of the graft. In this short period of time, you can see the formation of new bone from the preserved growth plate and the donor site occurring
7 Technical Pearls
-
1.
External Fixation [3]:
-
Selection of pins and frame according to bone size.
-
External fixator is placed in a usual manner (medial) in the tibia: epiphyseal pins have to be introduced under fluoroscopy avoiding the growth plate and avoiding the tumor. Diaphyseal pins should be placed far away from the tumor. We used regular Schanz pins. In this particular case, no postoperative chemotherapy was given. Most cases of Cañadell’s technique needed the initial fixator for a period between 10 and 15 days.
-
Additional surgery on the proximal tibiofibular joint is not necessary because distraction is usually about 1 cm.
-
The rate of distraction is crucial (1 mm/day) to achieve a type I epiphysiolysis according to Salter and Harris’ classification [4, 5].
-
-
2.
Resection
-
Proximal “osteotomy” is already done by the distraction, you only need to perform the diaphyseal osteotomy. Most of the growth plate remains together with the retained epiphysis. The small layer of growth plate covering the metaphysis is a safe margin (healthy tissue) by definition.
-
-
3.
Reconstruction
-
In the long-term follow-up, an autograft is the best option for intercalary reconstruction in small tumors such as this. The donor site will rebuild by itself in young children.
-
A single anterolateral incision is performed for obtaining the bone graft. Gentle dissection leaving the periosteum intact is mandatory to help in the regeneration of the donor site. Simple osteotomy of the medial third part of the fibula and a bone window of the external third of the tibia is done. Both bones will self-reconstruct without future intervention. No cast is needed and partial weight bearing is allowed.
-
The same fixator is used, both for physeal distraction and for stabilizing the reconstruction until healing of the graft, thus avoiding damage of the growth plate due to osteosynthesis [6]. In this particular case, the procedure was carried out at the end of chemotherapy, thus reducing the possibilities of tract pin infection. In many other cases, stabilization of the epiphysis to the graft was achieved with 2 k-wires, that were removed after bone healing (3–4 months).
-
With this technique, most of the growth plate can be preserved. However, if radiation is used, no growth at this site can be expected.
-
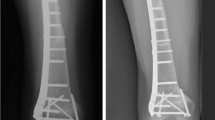
8 Outcome Photos and Imaging
Final X-ray at 21 year old, A corrective osteotomy, new plating and contralateral epiphysiodesis had been performed at 12 year old. Despite the young age at diagnosis (4 year old) and the contact between the tumor and the physis, this patient did not need any lengthening procedure, because her growth plate was preserved
9 Avoiding and Managing Complications
-
Preoperative planning is vital to this technique, an MRI is mandatory to confirm the growth plate is free of tumor and to accurately determine the osteotomy. Crossing the physis by the tumor is a contraindication for this technique.
-
Pathological fracture is a contraindication for physeal distraction unless it heals during neoadjuvant chemotherapy.
-
Pin tract infection is not common with Cañadell’s technique, because the external fixator is usually in place for 10–15 days. In this particular case, this time was superior due to the use of the device not only for distraction but also for stabilization of the graft. This patient had surgery at the end of chemotherapy protocol, so the risk of infection was lower, and she had not to pin tract infection [7].
-
Autograft fractures usually heal with conservative treatment, but in this case, it required osteosynthesis with bone grafting.
-
Small limb length discrepancy can be easily treated with contralateral epiphysiodesis. This patient did not require any other treatment for discrepancy, because her growth plate continued growing after resection of the tumor.
-
Until the fracture developed patient’s growth was as expected. The valgus deformity was subsequent to the fracture. We hypothesize that the valgus deformity in this case was possibly related to Cozen’s phenomenon [8] (proximal tibia fractures in young children tend to develop a late valgus) because we have not encountered this complication in other cases of proximal tibia distraction epiphysiolysis in “older” patients. We therefore corrected this deformity with a subsequent osteotomy.
10 Cross References: List of Other Similar Cases in the Atlas
-
Chap. 1: When and Why Biological/Implant Reconstruction?
-
Chap. 17: Implant Reconstruction of the Femoral Diaphysis—I: Intercalary Femur Prosthesis
-
Chap. 25: Implant Reconstruction of the Distal Femur—III: Expandable Prosthesis
-
Chap. 27: Biological Reconstruction of the Proximal Tibia—I: Pedicled Frozen Autograft
-
Chap. 29: Implant Reconstruction of the Proximal Tibia: Modular Prosthesis and Rotational Gastrocnemius Flap
References
Cañadell J, Forriol F, Cara JA. Removal of metaphyseal bone tumours with preservation of the epiphysis. Physeal distraction before excision. J Bone Joint Surg Br. 1994;76(1):127–32.
San-Julian M, editor. Cañadell’s pediatric bone sarcomas. Heidelberg, New York, London: Springer; 2016.
de Pablos J, Canadell J. Experimental physeal distraction in immature sheep. Clin Orthop Relat Res. 1990;250:73–80.
Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587–622.
Cañadell J, San-Julian M, Cara J, Forriol F. External fixation in tumour pathology. Int Orthop. 1998;22(2):126–30. https://doi.org/10.1007/s002640050223.
Arriola F, Forriol F, Cañadell J. Histomorphometric study of growth plate subjected to different mechanical conditions (compression, tension and neutralization): an experimental study in lambs. J Pediatr Orthop. 2001;10B:334–8.
Brown HK, Schiavone K, Gouin F, Heymann MF, Heymann D. Biology of bone sarcomas and new therapeutic developments. Calcif Tissue Int. 2018;102(2):174–95. https://doi.org/10.1007/s00223-017-0372-2.
Dorman S, Jariwala A, Campbell D. Cozen’s phenomenon: a reminder. Scott Med J. 2013;58(3):e10–3. https://doi.org/10.1177/0036933013496922.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Function 6 years after the first surgery (MP4 16131 kb)
Function 17 years after the first surgery (MP4 16769 kb)
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vázquez-García, B., San-Julián, M. (2022). Biological Reconstruction of the Proximal Tibia—II: Distraction-Epiphysiolysis Before Resectioning of the Tumor. In: Özger, H., Sim, F.H., Puri, A., Eralp, L. (eds) Orthopedic Surgical Oncology For Bone Tumors . Springer, Cham. https://doi.org/10.1007/978-3-030-73327-8_28
Download citation
DOI: https://doi.org/10.1007/978-3-030-73327-8_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73326-1
Online ISBN: 978-3-030-73327-8
eBook Packages: MedicineMedicine (R0)